Abstract
To investigate the correlation between the density and volume of epicardial adipose tissue(EAT)and acute coronary syndrome (ACS). This study included 355 subjects (mean age: 60.65 ± 9.67 years; 54.65% male), comprising 175 patients with ACS and 180 without ACS. Propensity score matching was applied to balance the variables between the two groups, resulting in 96 successfully matched pairs. Clinical data, epicardial adipose tissue volume (EATV), and epicardial adipose tissue density (EATD) were compared. Independent factors influencing ACS were identified using logistic regression analysis, and the predictive ability of each variable was evaluated using receiver operating characteristic (ROC) curves. Systolic blood pressure, EATV, EATD, fasting blood glucose, triglycerides, and high-sensitivity C-reactive protein were significantly elevated in the ACS group compared with the non-ACS group (all p < 0.05). Spearman correlation analysis revealed a moderate positive correlation between EATV and BMI (r = 0.444, p < 0.001), while EATD showed a weak negative correlation with age (r = -0.177, p = 0.014) and a weak positive correlation with EATV (r = 0.239, p = 0.001). Univariable regression analysis demonstrated that both EATV (OR: 2.018, 95% CI: 1.334–3.052) and EATD (OR: 5.341, 95% CI: 3.293–8.663) were associated with ACS. After adjusting for other risk factors, logistic regression model confirmed that EATV (adjusted OR: 1.892, 95%CI: 1.211–2.955) and EATD (adjusted OR: 6.942, 95%CI: 3.875–12.437) were independent predictors of ACS (both p < 0.001), with EATD showing the highest predictive value (AUC = 0.859). This study identifies a close relationship between EAT and ACS, highlighting EATD and EATV as independent influencing factors for ACS. Among them, EATD demonstrated a stronger predictive value for ACS than both traditional risk factors and EATV.
Similar content being viewed by others
Introduction
Acute coronary syndrome (ACS) encompasses a spectrum of conditions resulting from acute myocardial ischemia. It is characterized by an insidious onset, rapid progression, potential complications, and high mortality rates1,2,3. Identifyling and understanding the factors that contribute to the development and progression of ACS are critical for reducing its morbidity and mortality. Coronary artery disease (CAD), the primary underlying cause of ACS, results from the accumulation of lipids, calcium, and other substances within the coronary arteries. This leads to arterial narrowing or blockage, restricting blood flow to the heart and manifesting as angina pectoris, unstable angina, myocardial infarction, or ischemic heart failure4.
One of the major contributors to the pathogenesis of CAD and ACS is epicardial adipose tissue (EAT). Surrounding the coronary arteries, EAT secretes various cytokines and adipokines that can induce inflammation and promote myocardial remodeling, playing a pivotal role in the progression of CAD5. Researches have shown that EAT is an independent risk factor not only for CAD but also for atrial fibrillation, emphasizing its broader impact on cardiovascular health6,7,8. Inflammatory processes within EAT are strongly associated with the progression of coronary plaques, with increased EAT volume (EATV) correlating with more vulnerable plaque characteristics9.
Accurately quantifying the characteristics of EAT could enhance risk stratification and facilitate targeted therapies for patients with CAD and ACS. Recent advances in imaging technology now enable precise measurement of EAT volume and density. Although many studies have explored the relationship between EAT thickness and ACS, as well as its association with coronary artery vulnerability6,9,10,11, there is limited research examining the relationship between EATV, EAT density (EATD), and their combined effects on ACS.
This study aims to address this gap by comparing EATV and EATD between patients with and without ACS. Using data from 192 patients, we analyze the correlations of these characteristics with ACS. The findings of this research may have significant clinical implications, potentially improving diagnostic accuracy and guiding more effective management strategies for patients at risk of ACS.
Data and methods
General data
A total of 355 patients (mean age: 60.65 ± 9.67 years; 54.65% male) diagnosed with CAD were recruited from the Second Hospital of Hebei Medical University between November 2023 to April 2024. According to the 2023 ESC guidelines for the management of ACS1, ACS is defined as acute myocardial infarction (ST-elevation or non-ST-elevation) or unstable angina. Non-ACS refers to CAD that does not involve acute coronary events, including stable angina, asymptomatic CAD, and microvascular angina. Inclusion criteria: (1) All participants were diagnosed by cardiovascular physicians; (2) Coronary computed tomography angiography (CCTA) images were complete for all participants. Exclusion criteria: (3) Participants allergic to iodinated contrast agents; (4) Participants with severe liver or kidney dysfunction or coagulation disorders; (5) Participants with malignant tumors, rheumatic immune diseases, or acute and chronic infections; (6) Participants with mental disorders that hindered their cooperation during the examinations. Of the 355 patients, 175 were included in the ACS group, and 180 were included in the non-ACS group. The ACS group was designated as the study group, while the non-ACS group served as the control group. Propensity score matching(PSM) was employed to balance baseline characteristics between the two groups. The covariates selected for PSM included age, body mass index (BMI), gender, smoking history, family history of CAD, alcohol consumption history, hypertension, diabetes, and hyperlipidemia. These variables were chosen due to their established role as traditional cardiovascular risk factors influencing both ACS occurrence and EAT characteristics. Matching was conducted to minimize confounding effects and ensure more precise analysis of the relationship between EAT volume and density, and ACS. Propensity scores were calculated using logistic regression, and logit-transformed scores were matched using the nearest neighbor method in a 1:1 ratio with a caliper of 0.2. This resulted in 96 successfully matched pairs, with an average age of 60.71 ± 9.4 years and 56.8% male participants. The study protocol was approved by the Ethics Committee of the Second Hospital of Hebei Medical University and adhered to the ethical principles outlined in the 1975 Declaration of Helsinki. The ethics Approval number is 2021-R485. Written informed consent was obtained from all participants prior to their inclusion in the study.
Methods
Clinical data collection
A resident physician collected clinical data from the participants, including gender, age, height (cm), weight (kg), smoking status (smoker or non-smoker), alcohol consumption history (drinker or non-drinker), family history of CAD (present or absent), and underlying conditions such as hypertension, type 2 diabetes, and hyperlipidemia. Venous blood biochemical indicators were also recorded, including glycated hemoglobin, fasting blood glucose, triglycerides, high-density lipoprotein (HDL), low-density lipoprotein (LDL), total cholesterol, apolipoprotein A, apolipoprotein B, high-sensitivity C-reactive (hs-CRP), neutrophils, and lymphocytes. Additionally, baseline systolic and diastolic blood pressure, left ventricular ejection fraction (LVEF) as assessed by cardiac ultrasound, and BMI were recorded. BMI was calculated by dividing weight (kg) by the square of height (m²). Hypertension was defined as systolic blood pressure ≥ 140 mmHg, a diastolic blood pressure ≥ 90mmHg, or ongoing treatment with antihypertensive medications. Diabetes mellitus was defined as fasting blood glucose level ≥ 200 mg/dL or treatment with hypoglycemic medications. Hyperlipidemia was defined as total cholesterol ≥ 220 mg/dL, triglycerides ≥ 150 mg/dL, LDL ≥ 160 mg/dL, HDL ≤ 40 mg/dL, or ongoing treatmen with lipid-lowering medications.
Fasting venous blood biochemical test
Fasting venous blood samples (5 mL) were collected from patients via the antecubital vein in the early morning. Biochemical indices were analyzed using AU2700 Olympus automatic biochemical analyzer (Olympus France, Rungis, France).
CCTA scanning process
CCTA examinations were conducted using a dual-source CT scanner (Somatom Defnition Flash, Siemens Healthcare, Forchheim, Germany). Depending on heart rate control, either prospective or retrospective electrocardiogram-gated scan modes were utilized as necessary. The scanning parameters were as follows: detector collimation, 2 × 128 × 0.6 mm; slice thickness, 0.5 mm; tube current, 200 ~ 400 mAs; tube voltage, 100 ~ 120 kV (adjusted according to BMI); and gantry rotation time, 0.28 s. The scanning range extended from the pulmonary artery bifurcation to 1 cm below the diaphragm, with the region of interest was within on the root of the ascending aorta. The CCTA protocol consisted of non-contrast scan followed by a contrast-enhanced scan. To minimize respiratory artifacts, all patients underwent breath-holding training prior to the scan. Nonionic contrast medium (Iopamidol, 370 mg I/ml, Jiangsu Hengrui Pharmaceutical Co., Ltd, China) was administered intravenously via the antecubital vein at a rate of 5 ml/s, followed by 40 ml of saline flush. The volume of contrast agent was adjusted according to the patient’s weight. For patientss with heart rates exceeding 65 beats/ min before the scan, an intravenous beta-blocker (metoprolol, 5–20 mg, Astrazeneca Pharmaceuticals Ltd, Sweden) was administered. Additionally, 0.4 mg of sublingual nitroglycerin was given 5 min before the CTA examination.
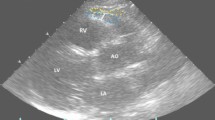
Quantitative CT measurement of EAT
Post-processing was performed on a dedicated off-line workstation (Multimodality Workplace, syngoMMWP VE32B, Siemens Healthineers). Axial images with a slice thickness of 0.75 mm were used for the analysis. CCTA images were independently analyzed by two experienced radiologists blinded to the patient’s identities. In cases of discrepancies between the two measurements, a third senior physician conducted further measurements to reach a consensus. EAT was defined as the adipose tissue located between the myocardium and the visceral pericardium, with a predefined attenuation threshold range of -190 Hounsfield Units (HU) to -30 HU. EATV was defined as the sum of all adipose tissues within this range, while EATD referred to the average attenuation value of all adipose tissues within the same range. The anatomical boundaries for EAT measurement were precisely defined as follows: the superior boundary is at the level of the pulmonary artery trunk, and the inferior boundary is at the junction between the diaphragm and the heart, corresponding to the apex of the left ventricle. The epicardial boundary was manually delineated every 3–5 slices, from the pulmonary trunk to the apex of the left ventricle. Voxels within the area of interest that met the defined attenuation threshold were quantified, and the software automatically calculated the average EATV and EATD values. (VE32B, Siemens Healthcare GmbH; Fig. 1).
EAT volume and density measurement diagram. (A) Manual delineation of epicardial adipose tissue boundaries layer by layer, with the pink area showing the range of epicardial adipose tissue that meets the fat threshold; (B) EAT volume and average density values automatically calculated using Volume software.
Statistical methods
All statistical analyses were performed using IBM SPSS Statistics for Windows, version 25.0. (IBM Corporation, Armonk, NY, USA). Categorical data were presented as frequencies (percentages) and compared between groups using the χ2 test. Continuous variables were first tested for normality using the Kolmogorov-Smirnov test. Variables following a normal distribution were expressed as mean ± standard deviation (‾χ ± SD ) and compared between the ACS and the non-ACS group using the independent samples t-test. For variables not conforming to a normal distribution, data were expressed as median and interquartile range (M, [Q1-Q3]) and compared using the nonparametric rank test Mann-Whitney U test. Spearman correlation analysis was used to assess the relationships among EATV, EATD, age, and BMI. Logistic regression analysis was used to identifyindependent risk factors for the occurrence of ACS. The Forward Selection (Likelihood Ratio) method was employed in the logistic regression model. Receiver operating characteristic (ROC) curve analysis was conducted to evaluate the predictive value of the variables for ACS. To ensure the reliability of EAT measurements, both inter-observer and intra-observer reliability evaluations were conducted, and the intraclass correlation coefficient (ICC) was calculated to assess measurement consistency. Additionally, Python software was used to compute the standardized mean difference (SMD) of the variables before and after PSM, enabling an evaluation of covariate balance between two groups. GraphPad Prism 8.0 (GraphPad, USA) software was utilized for data visualization. A p-value of < 0.05 was considered statistically significant for all analyses.
Results
Comparison of baseline data between two groups
The inter-observer ICCs for EATV and EATD were 0.954 and 0.829, respectively, while the intra-observer ICCs were 0.855 and 0.897, respectively, demonstrating excellent measuremen consistency (Table 1). The covariate balance test before and after PSM is presented in Table 2.
The demographics and baseline characteristics of patients in both groups are summarized in Table 1. Among the 92 matched pairs of subjects, the mean age was 60.71 + 9.4 years, and 109 (56.8%) were males, including 58 (53.2%) males in the ACS group and 51 (46.8%) males in the non-ACS group. Systolic blood pressure, EATV, EATD, fasting blood glucose, CRP, and triglyceride levels were significantly higher in the ACS group compared with the non-ACS group (all p < 0.05). In contrast, no statistically significant differences were observed between the two groups in age, BMI, smoking status, history of CAD, alcohol consumption, hypertension, diabetes mellitus, hyperlipidemia, HDL, LDL, diastolic blood pressure, lymphocytes, neutrophils, and LVEF (all p > 0.05; Table 3).
Correlation analysis between EATD, EATV, age, and BMI
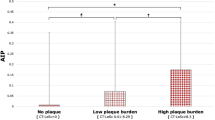
EATD showed a weak negative correlation with age (r = -0.177, p = 0.014) and a weak positive correlation with EATV (r = 0.239, p = 0.001). EATV demonstrated a moderate positive correlattion with BMI (r = 0.444, p < 0.001). No significant correlation was observed between EATD and BMI, nor between EATV and age (all p > 0.05; Fig. 2).
Logistic regression model for predicting the ACS
Univariable regression analysis identified both EATV and EATD as significant risk factors for ACS, with OR and 95%CI of 1.892(1.211–2.955)and 6.942 (3.875–12.437), respectively. Using the forward LR method, regression analysis was performed on all variables, and the final model retained four variables. After adjusting for other risk factors, EATV and EATD remained independent risk factors for ACS. Both EATV and EATD consistently exhibited strong and robust associations with ACS (Table 4.).
EATD, EATV, and age, triglyceride in predicting the ACS
Tthe predictive efficacy of EATD, EATV, and triglycerides for the occurrence of ACS was evaluated using ROC curve analysis. The predictive abilities of EATD, EATV, and triglycerides are summarized in Table 3. The area under the curve (AUC) for EATD was 0.859, which was higher than that for EATV (AUC = 0.717) and triglycerides (AUC = 0.635). The sensitivity and specificity of EATD in predicting ACS were 91.74% and 41.7%, respectively, with a cut-off value was − 111.50HU. (Table 5; Fig. 3).
Discussion
This study demonstrated that both EATV and EATD were significantly higher in patients with ACS compared to those without ACS. These findings underscore the potential role of EAT in the occurrence and progression of ACS. The moderate positive correlation between EATV and BMI supports the association between EATV and obesity, as well as its link to CAD. Furthermore, the weak correlations between EATD and age, and between EATD and EATV, suggest that EATD may be influenced by multiple factors, including age and the extent of adipose tissue accumulation. The logistic regression analysis identified EATV and EATD as independent factors influencing ACS, with EATD demonstrating a more substantial impact. The higher predictive accuracy of EATD (AUC = 0.859) compared to traditional risk factors and EATV highlights its potential as a valuable tool for early diagnosis and risk assessment of ACS. These findings suggest that, beyond traditional cardiovascular risk factors, the measurement of EAT characteristics may provide novel insights into the pathophysiology of ACS and improve risk stratification.
EAT is is widely recognized as closely associated with CAD12,13. Due to its anatomical proximity to the coronary arteries, EAT can directly influence coronary artery health through various mechanisms. This close positioning enables EAT to affect local vascular inflammation and plaque stability, potentially triggering acute coronary events5. EAT is a metabolically active tissue that secretes both pro-inflammatory cytokines, such as tumor necrosis factor-alpha (TNF-α), interleukin-6 (IL-6), and monocyte chemoattractant protein-1 (MCP-1), and anti-inflammatory cytokines, such as adiponectin14. As the volume of EAT increases, its secretion of pro-inflammatory cytokines rises while the production of anti-inflammatory factors diminishes. These inflammatory mediators can diffuse or come into direct contact with the coronary artery wall, exacerbating local inflammatory responses. This inflammation contributes to endothelial cell dysfunction, reduced nitric oxide bioavailability, heightened oxidative stress, and vascular inflammation, thereby promoting the formation and instability of coronary plaques. In addition to these biochemical effects, immune cells infiltrating EAT, such as macrophages and T cells, play a crucial regulatory role. Studies have shown that the polarization state of macrophages in EAT (classified into M1 and M2 types) significantly influences coronary artery health14,15. M1 macrophages exhibit pro-inflammatory effects, whereas M2 macrophages have anti-inflammatory and reparative functions. Dysfunctional EAT is characterized by an increased proportion of M1 macrophages and decreased proportion of M2 macrophages, which intensifies local inflammation and increase plaques instability- key factors in the development of ACS. A large-scale study by Shan D et al. involving over 1,000 participants, demonstrated that higher EATV is significantly associated with the presence of high-risk atherosclerotic plaques, independent of traditional risk factors suce as age and BMI16. EAT can promote lipid accumulation within the arterial wall, enlarging the lipid cores of plaques. Additionally, EAT secretes matrix metalloproteinases (MMPs), which degrade the fibrous cap of plaques, rendering them more prone to rupture. This structural and biochemical impacts underscore the role of EAT as a critical determinant of CAD progression and acute coronary events. Consequently, EATV serves as a specific predictor of coronary plaque vulnerability.
Moreover, excessive accumulation of EAT can also exert mechanical pressure on adjacent coronary arteries, thereby altering the local hemodynamic environment. This mechanical pressure may lead to coronary artery narrowing and reduced blood flow, increasing the risk of localized ischemia. Additionally, a meta-analysis of over 6,600 patients reported that individuals with myocardial infarction exhibited EAT levels approximately 37% greater than those without such events. This finding suggests that elevated EAT levels play a critical role in the pathogenesis of acute myocardial infarction17. These results indicate that quantifying EAT could serve as an effective tool for assessing ACS risk. Uygur B pointed out that high EAT volume can be used for risk stratification of major adverse cardiovascular events (MACE), and patients with high EATV can choose more aggressive risk reduction strategies18.
This study found that EATD was elevated in patients with ACS, likely due to several factors: Firstly, an increase in pro-inflammatory cytokines within EAT enhances the infiltration of inflammatory cells and activates inflammatory responses. The increased EATD in CT images might reflect a higher ratio of hyperdense inflammatory components to hypodense fatty components, indicating adverse metabolic activity., This metabolic activity can lead to the production of inflammatory mediators and cytokines, which which exert localized effects on coronary arteries, promoting coronary atherosclerosis, plaque instability, and the development of ACS19,20. Some studies 21,22 suggest that the increase in EATD may be attributed to the presence of immaturely differentiated adipocytes within EAT. These adipocytes are characterized by low lipid content and a propensity to stimulate the release of inflammatory factors and angiogenesis. This process results in an accumulation of cellular components, thereby increasing EATD. Secondly, in ACS patients, the functionality of EAT adipocytes is compromised, with a higher proportion of immature adipocytes. These immature adipocytes, distinguished by smaller cytoplasms and larger nuclei, inherently contribute to the higher EATD due to their greater cellular density23. Lastly, EAT may undergo fibrosis under chronic inflammatory conditions, involving the deposition of collagen fibers and extracellular matrix components, further elevating tissue density. However, Franssens et al. found that EATD reflects pathological changes and is associated withACS, but noted that lower EATD correlates with high-risk coronary plaques, which contradicts our findings24. The potential reasons for these inconsistencies are as follows: (1) Differences in patient populations. The patients in our study were primarily diagnosed with ACS and may be in the acute phase of inflammation. Acute inflammation may lead to increased EATD25,26, whereas low-density EAT in chronic CAD patients is typically associated with lipid accumulation24,27. (2) Impact of imaging techniques and measurement parameters. The CT scanning parameters used in our study, such as tube voltage, contrast agent protocols, and reconstruction algorithms, may differ from those in other studies, potentially influencing EATD measurements. Furthermore, variations in segmentation thresholds for EATD (e.g., -190 to -30 HU) and differences in measurement methodologies across studies may also contribute to the discrepancies observed. (3) Complex relationship between EATD and plaque characteristics. Although lower EATD is generally associated with high-risk coronary plaques28, acute plaque rupture and localized inflammation in ACS patients may elevate EATD. This suggests that the relationship between EATD and cardiovascular risk is dependent on the stage of the disease and the activity of coronary plaques.
The increase in EAT density and volume serves as independent predictive factors for ACS, primarily through mechanisms such as enhanced inflammatory responses11, metabolic dysregulation9, and fibrosis24. Additionally, research by Franssens et al. demonstrated that EAT contributes to tissue remodeling and alterations in local hemodynamics, further linking EAT characteristics to the instability of coronary plaques24. The close relationship between EAT and ACS underscores the need for further research to determine whether these findings could influence treatment strategies. While EATD demonstrates a higher predictive value for ACS compared with traditional risk factors and EATV, it is essential to evaluate how this can guide clinical practice in providing more personalized treatment approaches for ACS patients.
EAT is a significant source of reactive oxygen species (ROS), which contribute to oxidative stress within the coronary microenvironment. The high metabolic activity of EAT generates ROS that damage endothelial cells and enhance the oxidation of LDL. Oxidized LDL plays a critical role in the development of atherosclerotic plaques, rendering them more prone to rupture. This oxidative modification of LDL and the subsequent inflammatory response are key drivers of plaque instability, a hallmark of ACS. Leptin secreted by EAT promote myocardial injury associated with metabolic syndrome by activating the protein kinase C (PKC)/reduced nicotinamide adenine dinucleotide phosphate (NADPH) oxidase/reactive oxygen species (PKC/NADPH oxidase/ROS) signaling pathway., This pathway contributes to mitochondrial oxidative stress, apoptosis, and inflammatory responses, further exacerbating plaque vulnerability29. Collectively, these factors position EAT as a significant biological markers for predicting the risk of ACS. Understanding these mechanisms not only enhances clinical risk assessment but also paves the way for novel intervention strategies. Franssens et al.24 highlighted the potential role of EATD as a potent biomarker of cardiovascular risk, suggesting that it might be a more sensitive than EATV. Oikonomou et al.30 demonstrated that the perivascular fat attenuation index is highly predictive of cardiac mortality, with elevated values indicating increased risks of both cardiac-specific and all-cause mortality. Recently, quantitative measurements of EAT obtained through CCTA have been integrated into artificial intelligence (AI) models for cardiovascular risk stratification31. These models have shown superior utility in predicting MACE compared to plaque characteristics alone. Analyzing EAT attenuation derived from CT imaging emerges as a safe, valuable, and specific non-invasive method for identifying coronary inflammation and high-risk plaques. EAT may enhance risk assessment for ACS, and its parameters should be considered as a complementary tool in clinical decision-making. Further research is required to elucidate its potential role in developing personalized treatment strategies for ACS patients.
In addition, SBP, FBG, hs-CRP, and triglyceride levels were significantly elevated in ACS group compared with the control groups. These traditional cardiovascular risk factors were more pronounced in the ACS group. It is well established that elevated blood glucose and CRP levels are common among hospitalized patients with ACS. Hypertension is recognizedas one of the primary risk factors for ACS32. It causes damage to the coronary artery endothelium, thereby promoting the formation and progression of atherosclerotic plaques. Over time, persistent hypertension accelerates arteriosclerosis, increasing the likelihood of plaque rupture and thrombosis, which can precipitate acute coronary events. A substantial body of evidence hasconfirmed the association between hyperglycemia, acute myocardial infarction, and poor prognosis33,34,35. Hyperglycemia contributes to endothelial dysfunction, often accompanied by insulin resistance and metabolic syndrome, which collectively promote atherosclerosis. Moreover, diabetic patients frequently exhibita chronic inflammatory state characterized by elevated levels of CRP and other inflammatory markers. This persistent inflammation accelerates atherosclerosis progression and increases the vulnerability of s arterial plaques to rupture. Studies have shown that hs-CRP is not only merely an inflammatory marker but also plays a critical role in the pathogenesis of atherosclerotic cardiovascular disease (ASCVD) and ACS. Elevated hs-CRP levels are strongly associated with plaque instability, post-myocardial infarction inflammatory responses, and a higher mortality risk36. Çağdaş et al. reported that a systemic inflammatory state, as indicated by decreased albumin, elevated CRP level, and increased CRP-to-albumin ratio, is closely related to severe CAD37. Consequently, hs-CRP serve as a a valuable indicator for assessing ACS risk. Elevatedtriglyceride levels have also been shown to significantly increase the risk of myocardial infarction, particularly in patients with additionalr cardiovascular risk factors such as high BMI, LDL-C, and elevated blood glucose levels38. First, high triglyceride levels increase the number of LDL and very low-density lipoprotein (VLDL) particles, which are prone to depositing in the arterial walls and promoting atherosclerosis. This results in coronary artery narrowing or complete blockage, triggering ACS. Second, a scientific statement from the American Heart Association emphasized that hypertriglyceridemia increases the risk of cardiovascular events by promoting inflammatory responses and enhancing endothelial dysfunction. These processes facilitate the formation and instability of atherosclerotic plaques39. Third, elevated triglyceride levels are often associated with insulin resistance and metabolic syndrome, both of which are significant risk factors for ACS. Thus, hypertriglyceridemia not only contributes to atherosclerosis but also exacerbates other underlying metabolic and inflammatory conditions, further amplifying cardiovascular risk. In summary, high triglycerides are a major risk factors for ACS, acting through mechanisms that include promoting atherosclerosis, inducing inflammatory responses, and exacerbating metabolic dysfunction.
Correlation analysis revealed a moderate positive correlation between EATVand BMI, consistent with existing literature, which supports a direct relationship between an individual’s overall fat mass and the accumulation of EAT. As BMI increases, greater fat deposition is observed around the heart, contributing to increased EAT volume. EATD exhibited a weak correlation with both age and EATV, suggesting that EATD may be influenced by a combination of factors. With advancing age, changes in tissue characteristics of EAT, such as fibrosis or changes in cellular metabolism, may affect its density. Additionally, an increase in fat volume does not necessarily correspond to proportional increase in density. This discrepancy may be attributed to variations in the size, number, and distribution of adipocytes within the tissue.
Limitations
This study has several limitations that should be acknowledged. First, due to its cross-sectional design, the study cannot establish a causal relationship between EAT and ACS. Longitudinal studies are necessary to investigate how changes in EAT over time influence ACS development and progression. Second, although propensity score matchingPSM was employed to balance baseline characteristics, factors such as genetic predisposition, lifestyle, and diet were not controlled for and may impact both EAT and ACS risk. Future studies should consider a broade range of potential confounding variables to enhance the robustness of the findings. Third, as this study was conducted at a single center, the generalizability of the results to other populations or healthcare settings is limited. Multi-center studies with diverse cohorts are needed to validate these findings. Fourth, the assessment of EATV and EATD relied on s imaging techniques that may be subject to variability and measurement errors. Standardizing imaging protocols and using advanced technologies could enhance the accuracy and consistency of EAT measurements. Finally, while the study included a relatively large overall sample size, the number of successfully matched pairs was comparatively y small. Future research with larger sample sizes would provide more precise estimates and strengthen the statistical power of the analysis.
Conclusions
This study demonstrates a significant association between EAT characteristics and ACS, with both EATV and EATD identified as independent predictors. EATD, in particular, exhibited superior predictive accuracy, suggesting its potential utility as a novel biomarker for early diagnosis and risk stratification of ACS. The mechanisms linking EAT to ACS likely involve inflammatory pathways, metabolic disturbances, and local effects on coronary arteries, contributing to plaque instability and acute coronary events. However, the cross-sectional nature of this study and potential confounding warrant further investigation. Future longitudinal, multi-center studies with larger and more diverse cohorts are essential to validate these findings and clarify causal relationships. Such efforts could refine risk stratification models and guide the development of personalized treatment strategies for ACS patients, integrating EAT metrics into clinical decision-making.
Data availability
The data supporting the findings of this study are available in its supplementary information files.
References
Byrne, R. A. et al. 2023 ESC guidelines for the management of acute coronary syndromes. Eur. Heart J. 12 (38), 3720–3826. https://doi.org/10.1093/eurheartj/ehad191 (2023).
Bergmark, B. A. et al. Acute coronary syndromes. Lancet 399 (10332), 1347–1358. https://doi.org/10.1016/S0140-6736(21)02391-6 (2022).
Dani, S. S. et al. Trends in premature mortality from acute myocardial infarction in the United States, 1999 to 2019. J. Am. Heart Assoc. 11 (1), e021682. https://doi.org/10.1161/JAHA.121.021682 (2022).
Fox, K. A. A. et al. The myth of ‘stable’ coronary artery disease. Nat. Rev. Cardiol. 17 (1), 9–21. https://doi.org/10.1038/s41569-019-0233-y (2020).
Napoli, G. et al. Epicardial and pericoronary adipose tissue, coronary inflammation, and acute coronary syndromes. J. Clin. Med. 21 (12(23), 7212. https://doi.org/10.3390/jcm12237212 (2023).
Jehn, S. et al. Epicardial adipose tissue and obstructive coronary artery disease in acute chest pain: The EPIC-ACS study. Eur. Heart J. Open. 17 (3), oead041. https://doi.org/10.1093/ehjopen/oead041 (2023).
Couselo-Seijas M, Rodríguez-Mañero M, González-Juanatey JR, et al. Updates on epicardial adipose tissue mechanisms on atrial fibrillation. Obes Rev. 2021, 22(9):e13277. doi: 10.1111/obr.13277.
Conte, M. et al. Epicardial adipose tissue and cardiac arrhythmias: Focus on atrial fibrillation. Front. Cardiovasc. Med. 30, 9:932262. https://doi.org/10.3389/fcvm.2022.932262 (2022).
Kawabata, Y. et al. Association of microluminal structures assessed by optical coherence tomography with local inflammation in adjacent epicardial adipose tissue and coronary plaque characteristics in fresh cadavers. Circ. J. 25 (2), 329–335. https://doi.org/10.1253/circj.CJ-22-0299 (2023).
Mohamed, W. et al. Ethnic disparities and its association between epicardial adipose tissue thickness and cardiometabolic parameters. Adipocyte 13 (1), 2314032. https://doi.org/10.1080/21623945.2024.2314032 (2024).
Shan, D. et al. Epicardial adipose tissue volume is associated with high risk plaque profiles in suspect CAD patients. Oxid. Med. Cell. Longev. 12, 2021:6663948. https://doi.org/10.1155/2021/6663948 (2021).
Conceição, G., Martins, D. & Miranda, M. Unraveling the role of epicardial adipose tissue in coronary artery disease: partners in crime? Int. J. Mol. Sci. 23 (22), 8866. https://doi.org/10.3390/ijms21228866 (2020).
Panda, S. et al. Can epicardial and pericardial adipose tissue volume predict the presence and severity of coronary artery disease? Pol. J. Radiol. 26, 87:e348–e353. https://doi.org/10.5114/pjr.2022.117968 (2022).
Doukbi, E. et al. Browning epicardial adipose tissue: friend or foe? Cells. 14, 11(6):991. (2022). https://doi.org/10.3390/cells11060991
Liberale, L., Dallegri, F., Montecucco, F. & Carbone, F. Pathophysiological relevance of macrophage subsets in atherogenesis. Thromb. Haemost. 5 (1), 7–18. https://doi.org/10.1160/TH16-08-0593 (2017).
Shan, T., Dou, D. & Yang, G. Epicardial adipose tissue volume is associated with high risk plaque profiles in suspect CAD patients. Oxid. Med. Cell. Longev. 12, 2021:6663948. https://doi.org/10.1155/2021/6663948 (2021).
Hendricks, S. et al. Epicardial adipose tissue is a robust measure of increased risk of myocardial infarction - a meta-analysis on over 6600 patients and rationale for the EPIC-ACS study. Med. (Baltim). 100 (52), e28060. https://doi.org/10.1097/MD.0000000000028060 (2021).
Uygur, B. et al. Epicardial adipose tissue volume predicts long term major adverse cardiovascular events in patients with type 2 diabetes. Turk. Kardiyol Dern Ars. 49 (2), 127–134 (2021).
Yuvaraj, J. et al. Pericoronary adipose tissue attenuation is associated with high-risk plaque and subsequent acute coronary syndrome in patients with stable coronary artery disease. Cells 10 (5), 1143. https://doi.org/10.3390/cells10051143 (2021).
Parisi, V. et al. Imbalance between interleukin-1β and interleukin-1 receptor antagonist in epicardial adipose tissue is associated with non St-segment elevation acute coronary syndrome. Front. Physiol. 5, 11:42. https://doi.org/10.3389/fphys.2020.00042 (2020).
Antonopoulos, A. S. et al. Detecting human coronary inflammation by imaging perivascular fat. Sci. Transl Med. 12 (398), eaal2658. https://doi.org/10.1126/scitranslmed.aal2658 (2017).
Koenen, M. et al. Obesity, adipose tissue and vascular dysfunction. Circ. Res. 2 (7), 951–968. https://doi.org/10.1161/CIRCRESAHA.121.318093 (2021).
Marcelin, G., Gautier, E. L. & Clément, K. Adipose tissue fibrosis in obesity: Etiology and challenges. Annu. Rev. Physiol. 10, 84:135–155. https://doi.org/10.1146/annurev-physiol-060721-092930 (2022).
Franssens, B. T. et al. Relation between cardiovascular disease risk factors and epicardial adipose tissue density on cardiac computed tomography in patients at high risk of cardiovascular events. Eur. J. Prev. Cardiol. 24 (6), 660–670. https://doi.org/10.1177/2047487316679524 (2017).
Mahabadi, A. A. et al. Cardiac computed tomography-derived epicardial fat volume and attenuation independently distinguish patients with and without myocardial infarction. PLoS One. 12 (8), e0183514. https://doi.org/10.1371/journal.pone.0183514 (2017).
Monti, C. B. et al. CT-derived epicardial adipose tissue density: Systematic review and meta-analysis. Eur. J. Radiol. 143, 109902. https://doi.org/10.1016/j.ejrad.2021.109902 (2021).
Goeller, M. et al. Epicardial adipose tissue density and volume are related to subclinical atherosclerosis, inflammation and major adverse cardiac events in asymptomatic subjects. J. Cardiovasc. Comput. Tomogr. 12 (1), 67–73. https://doi.org/10.1016/j.jcct.2017.11.007 (2018).
Lu, M. T. et al. Epicardial and paracardial adipose tissue volume and attenuation - association with high-risk coronary plaque on computed tomographic angiography in the ROMICAT II trial. Atherosclerosis 251, 47–54. https://doi.org/10.1016/j.atherosclerosis.2016.05.033 (2016).
Chen, H. et al. Epicardial adipose tissue-derived leptin promotes myocardial injury in metabolic syndrome rats yhrough PKC/NADPH Oxidase/ROS pathway. J. Am. Heart Assoc. 12 (15), e029415. https://doi.org/10.1161/JAHA.123.029415 (2023).
Oikonomou, E. K. et al. Non-invasive detection of coronary inflammation using computed tomography and prediction of residual cardiovascular risk (the CRISP CT study): A post-hoc analysis of prospective outcome data. Lancet 15 (392(10151), 929–939. https://doi.org/10.1016/S0140-6736(18)31114-0 (2018).
West, H. W. et al. Deep-learning for epicardial adipose tissue assessment with computed tomography: Implications for cardiovascular risk prediction. JACC Cardiovasc. Imaging. 16 (6), 800–816. https://doi.org/10.1016/j.jcmg.2022.11.018 (2023).
Williams, B. et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur. Heart J. 1 (33), 3021–3104. https://doi.org/10.1093/eurheartj/ehy339 (2018).
Zheng, Y., Ley, S. H. & Hu, F. B. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat. Rev. Endocrinol. 14 (2), 88–98. https://doi.org/10.1038/nrendo.2017.151 (2018).
Paolisso, P. et al. Hyperglycemia, inflammatory response and infarct size in obstructive acute myocardial infarction and MINOCA. Cardiovasc. Diabetol. 20 (1), 33. https://doi.org/10.1186/s12933-021-01222-9 (2021).
Cosentino, F. et al. ESC scientific document group. 2019 ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur. Heart J. 7 (2), 255–323. https://doi.org/10.1093/eurheartj/ehz486 (2020).
Lawler, P. R. et al. Targeting cardiovascular inflammation: Next steps in clinical translation. Eur. Heart J. 1 (1), 113–131. https://doi.org/10.1093/eurheartj/ehaa099 (2021).
Çağdaş, M. et al. Assessment of Relationship between C-Reactive protein to albumin ratio and coronary artery disease severity in patients with acute coronary syndrome. Angiology 70 (4), 361–368 (2019).
Jiao, Z. Y. et al. Correlation of triglycerides with myocardial infarction and analysis of risk factors for myocardial infarction in patients with elevated triglyceride. J. Thorac. Dis. 10 (5), 2551–2557. https://doi.org/10.21037/jtd.2018.04.132 (2018).
Miller, M. et al. Triglycerides and cardiovascular disease: A scientific statement from the American Heart Association. Circulation 24 (20), 2292–2333. https://doi.org/10.1161/CIR.0b013e3182160726 (2011).
Acknowledgements
The authors express their sincere gratitude to all the study participants and patients who contributed to this research. The authors also extend their appreciation to the the radiology technologists and technicians for their invaluable assistance in patient enrollment and data collection for this study.
Funding
None.
Author information
Authors and Affiliations
Contributions
GZ collected clinical data and drafted part of the manuscript. ZY, YY, XY, XL contributed to data collection and patient evaluation. HZand JL provided expert consultation and revise suggestions. GZ conceptualized the study and drafted the manuscript. All authors reviewed, provided details comments on drafts, and contributed to the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhihong, G., Yuqiang, Z., Linyi, J. et al. Correlation analysis between epicardial adipose tissue and acute coronary syndrome. Sci Rep 15, 3015 (2025). https://doi.org/10.1038/s41598-025-87594-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-87594-4