Abstract
Moderate/severe anemia [hemoglobin (Hb) < 10 g/dL] is recommended to be treated in patients with renal anemia. However, the optimal therapeutic target for Hb levels in patients with heart failure (HF) is unknown. This study aimed to investigate the impact of severity of anemia, especially moderate/severe anemia, associated with renal dysfunction (RD: eGFR < 60 mL/min/1.73 m2) in HF patients. We analyzed 1,608 HF patients from the Japanese Cardiac Registry of Heart Failure in Cardiology (JCARE-CARD) database. Patients were classified based on the severity of admission anemia in the presence/absence of RD. Patients with RD and anemia were older, more likely to be female, and had a history of HF admission. The composite outcome was higher in RD and moderate/severe anemia (adjusted hazard ratio:2.120, 95% CI:1.559–2.881, p < 0.001) compared to RD and non/mild anemia (Hb ≥ 10 g/dL), non-RD and moderate/severe anemia, and non-RD and non/mild anemia (reference). During hospitalization, 6% and 10% of patients had improving and worsening RD and/or moderate/severe anemia, respectively. These status changes were associated with the post-discharge outcomes in HF patients. Moderate/severe anemia has a prognostic impact in HF patients with RD and may be an appropriate therapeutic target in HF.
Similar content being viewed by others
Introduction
Anemia is a common comorbidity in patients with heart failure (HF) and an independent risk factor for long-term outcomes.1,2,3,4,5,6,7,8 In addition to anemia, renal dysfunction (RD) is a significant risk factor in both acute and chronic HF.9,10,11 HF, anemia, and RD interact negatively, resulting in the cardio-renal-anemia syndrome (CRAS).12,13,14,15 However, the therapeutic strategies for anemia and RD in HF have not been established.
In patients with chronic kidney disease (CKD) who had hemoglobin (Hb) levels below 10 g/dL had a worse prognosis compared to those with Hb levels between 10 and 12 g/dL. On the other hand, administration of erythropoiesis-stimulating agents (ESAs) targeting Hb ≥ 13 g/dL increased the risk of cardiovascular events.16,17,18 Recent studies demonstrated no significant difference in renal outcomes between patients with Hb 9–11 g/dL and 11–13 g/dL.19,20 These findings raise the possibility that the appropriate cutoff for anemia may be around 10 g/dL. In fact, a recent Japanese guideline for CKD recommends maintaining Hb levels between 10–12 g/dL with Hb < 10 g/dL as the therapeutic target. With respect to HF, the RED-HF trial demonstrated that administration of an ESA targeting Hb ≥ 11 g/dL did not improve the prognosis of HF patients and instead increased thrombosis in HF patients.21 As in CKD, maintaining Hb levels in the normal range may not be beneficial in HF patients with anemia. However, the impact of the severity of anemia, especially Hb < 10 g/dL, associated with RD in HF patients has not been fully elucidated. In particular, the therapeutic target range of Hb levels in HF remains unknown.
The status of RD and anemia can change during hospitalization for HF. Therefore, their management is critical not only in outpatients with HF but also in patients hospitalized for HF. Most studies on HF and anemia have evaluated Hb levels at the time of HF admission. To our knowledge, only a few studies have reported short-term changes in Hb levels in HF.22,23 The information on changes in anemia severity associated with RD during HF hospitalization may be useful in the management of CRAS.
The Japanese Cardiac Registry of Heart Failure in Cardiology (JCARE-CARD) prospectively studied the characteristics and treatments of a large sample of patients hospitalized with HF at teaching hospitals in Japan from January 2004 to June 2005 and the outcomes including death and rehospitalization were followed until 2007.24 The JCARE-CARD database is useful for studying the transitional status of anemia and RD during HF hospitalization. The aim of the present study was to analyze the prognostic impact of anemia severity, especially Hb < 10 g/dL, associated with RD on mortality and rehospitalization, as well as the changes in RD and anemia, in patients due to worsening HF by using the JCARE‐CARD database.
Results
Impact of admission anemia severity on long-term outcomes in HF patients with RD
In the JCARE database, 1,608 patients were identified to have creatinine and Hb levels at admission. Of these, 569 patients had normal renal function (eGFR ≥ 60 ml/min/1.73 m2) and 1,039 patients had RD (eGFR < 60 ml/min/1.73 m2) (Table 1).
In patients with normal renal function, 344 (60%), 169 (30%), and 56 (10%) had non-anemia (Hb ≥ 13.0 g/dL in males, ≥ 12.0 g/dL in females), mild anemia (Hb ≥ 10.0 g/dL, < 13.0 g/dL in males, ≥ 10.0 g/dL, < 12.0 g/dL in females), and moderate/severe anemia (Hb < 10 g/dL), respectively (Table 1). According to the severity of anemia, patients were older and more likely to be female and have valvular heart disease, higher creatinine levels, smaller LV diameters, and higher a LVEF. Consistently, patients with moderate/severe anemia had more HFpEF (Supplementary Fig. 1). Hb levels in non- (14.2 ± 1.4 g/dL vs. 14.4 ± 1.5 g/dL, P = 0.119), mild (11.4 ± 0.8 g/dL vs. 11.4 ± 0.8 g/dL, P = 0.983), and moderate/severe anemia groups (8.6 ± 1.1g/dL vs. 8.8 ± 1.4 g/dL, P = 0.171) were similar between patients with and without RD.
The mean post-discharge follow-up was 698 ± 349 days. The composite of all-cause death or HF rehospitalization and HF rehospitalization did not differ between these groups (Fig. 1A and C). All-cause death was higher in patients with mild and moderate/severe anemia than in those without anemia (Fig. 1B). In Cox hazard analysis, the composite of all-cause death or HF rehospitalization and HF rehospitalization in mild anemia group (aHR 0.970, 95% CI 0.619–1.497) and moderate/severe anemia group (aHR 1.424, 95% CI 0.758–2.560) was compared with the non-anemia group (Table 2).
Long-term outcomes according to severity of anemia in the presence or absence of RD on admission among HF patients. Kaplan–Meier, event-free curves free from all-cause death or rehospitalization (A and D), all-cause death (B and E), and rehospitalization due to worsening HF (C and F) in HF patients with and without RD (eGFR < 60 ml/min/1.73 m2) according to Hb levels on admission; normal Hb (Hb ≥ 13.0 g/dL in males, ≥ 12.0 g/dL in females), mild anemia (Hb ≥ 10.0 g/dL, < 13.0 g/dL in males, ≥ 10.0 g/dL, < 12.0 g/dL in females), moderate severe anemia (Hb < 10.0 g/dL).
Among patients with RD, 372 (41%), 326 (36%), and 196 (23%) had non-anemia, mild anemia, or moderate/severe anemia, respectively. Like those with normal renal function, patients with lower Hb levels were older and likely to be more female and had valvular heart disease, higher creatinine levels, smaller LV diameters, higher LVEF (Table 1), and more HFpEF (Supplementary Fig. 1). However, these patients were less likely to be prescribed beta-blockers, ACEi/ARB, and MRA. The mean post-discharge follow-up was 584 ± 376 days. The composite of all-cause death or HF rehospitalization, all-cause death, and HF rehospitalization were higher in patients with mild anemia than in patients without anemia and the highest in patients with moderate/severe anemia among groups (Fig. 1D–F). In Cox hazard analysis, the composite of all-cause death or HF rehospitalization and HF rehospitalization was higher in moderate/severe anemia group (aHR 1.717, 95% CI 1.257–2.343, P < 0.001) compared with non-anemia group (Table 2). The same trends were observed for all-cause death and HF rehospitalization (Table 2).
These results suggest that the severity of anemia has a greater impact on long-term outcomes in HF patients with RD than in those with normal renal function.
Impact of moderate/severe anemia associated with RD on long-term outcomes in HF patients
A recent guideline for CKD defines moderate/severe anemia (Hb < 10 g/dL) as a therapeutic target in patients with renal anemia. To investigate the impact of moderate/severe anemia associated with RD on admission in HF patients, we analyzed four groups: non-RD and non/mild anemia, RD and non/mild anemia, non-RD and moderate/severe anemia, and RD and moderate/severe anemia (Table 3). Patients with RD and moderate/severe anemia were older, more female, and more likely to have s severe NYHA functional class, previous HF admission, ischemic and valvular heart diseases, hyperuricemia, previous myocardial infarction, higher BNP levels, and lower prescription rates of beta-blocker, ACEi/ARB, and MRA. On the other hand, patients with RD had the highest prevalence of HFpEF among all groups. Hb levels were comparable in patients with non-RD and moderate/severe anemia and those with RD and moderate/severe anemia (8.8 ± 1.4 g/dL vs. 8.6 ± 1.1 g/dL, P = 0.171) as described above. On the other hand, patients with RD and moderate/severe anemia had lower eGFR levels compared with those with RD and non/mild anemia (30.2 ± 15.0 g/dL vs. 41.6 ± 12.6 g/dL, P < 0.001).
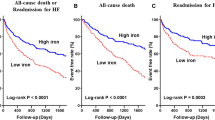
In-hospital death was occurred in 91 patients (non/mild anemia:11, RD:45, moderate/severe anemia, RD and moderate/severe anemia:31). In a multivariate logistic analysis, BMI and systolic BP were negatively associated with in-hospital death, while RD and RD with moderate/severe anemia were positively associated with it (odds ratio (OR) 5.412, 95%CI 2.007–15.431, P < 0.001) (Supplementary Table 1). The composite of all-cause death or HF rehospitalization increased in the order of non-RD and non/mild anemia, RD and non/mild anemia, non-RD and moderate/severe anemia, and RD and moderate/severe anemia (Fig. 2A). The same pattern was observed in all-cause death and HF rehospitalization (Fig. 2B and C). In Cox hazard analysis, the composite of all-cause death or HF rehospitalization (aHR 2.120, 95% CI 1.559–2.881, P < 0.001), all-cause death (aHR 3.340, 95% CI 2.154–5.251, P < 0.001), and HF rehospitalization (aHR 2.212, 95% CI 1.559–2.881, P < 0.001) were the highest in patients with RD and moderate/severe anemia (Table 4).
Long-term outcomes according to the presence of RD and/or moderate/severe anemia on admission among HF patients. Kaplan–Meier, event-free curves free from all-cause death or rehospitalization (A), all-cause death (B), and rehospitalization due to worsening HF (C) in HF patients with/without RD (eGFR < 60 ml/min/1.73 m2) and no/mild anemia (Hb ≥ 10.0 g/dL) or moderate/severe anemia (Hb < 10.0 g/dL). Group 1; non-RD and non/mild anemia, Group 2; RD and non/mild anemia, Group 3; non-RD and moderate/severe anemia, Group 4; RD and moderate/severe anemia.
We also analyzed the impact of RD and moderate/severe anemia in each HF type. These outcomes were greatest in patients with RD and moderate/severe anemia in HF with reduced ejection fraction (HFrEF) (Supplementary Fig. 2), HF with mildly reduced EF (HFmrEF) (Supplementary Fig. 3), and HF with preserved EF (HFpEF) (Supplementary Fig. 4). The presence of RD and moderate/severe anemia was independently associated with the composite of all-cause death or HF rehospitalization (Supplementary Table 2).
These findings suggest that RD and moderate/severe anemia have a synergistic effect on poor outcomes in HF patients.
Changes in RD and anemia during HF hospitalization
During HF hospitalization, the status of RD and anemia can change. Thus, we examined changes in RD and anemia from admission to discharge in each group (non-RD and non/mild anemia defined as group 0 [383 patients], RD and non/mild anemia defined as group 1 [606 patients], non-RD and moderate/severe anemia defined as group 2 [45 patients], and RD and moderate/severe anemia defined as group 3 [211 patients]) (Fig. 3A). Most patients in each group did not change their status (non-RD and non/mild anemia: 88%, RD and non/mild anemia: 83%, non-RD and moderate/severe anemia:83%, and RD and moderate/severe anemia: 75%). In non-RD and non/mild anemia group at admission, 12% of patients had moved on to other groups at discharge. In RD and non/mild anemia group on admission, 12% transitioned to non/mild anemia, 5% progressed to moderate/severe anemia or RD with moderate/severe anemia. In non-RD and moderate/severe anemia patients on admission, 7%, 8%, and 1% transitioned to RD and moderate/severe anemia, non-RD and moderate/severe anemia, and non-RD and non/mild anemia, respectively. In RD and moderate/severe anemia patients on admission, 14%, 8%, and 1% moved on to non-RD and moderate/severe anemia, RD and non/mild anemia, and non-RD and non/mild anemia, respectively. Overall, 6% of patients’ condition worsened, while 10% improved during their HF hospitalization.
Changes in RD and anemia during HF hospitalization. (A) Changes in RD and anemia from admission to discharge. Group 1; non-RD and non/mild anemia, Group 2; RD and non/mild anemia, Group 3; non-RD and moderate/severe anemia, Group 4; RD and moderate/severe anemia. (B) Kaplan–Meier, event-free curves free from all-cause death or rehospitalization according to changes in RD and anemia.
In Kaplan–Meier analysis (Fig. 3B), the composite of all-cause death or HF rehospitalization was lowest in patients who moved from group 0 to group 0, and highest in those who moved from group 3 to group 3. Surprisingly, whereas patients who transitioned from group 0 to group 3 tended to have worse outcomes, those who transitioned from group 3 to other groups had better outcomes.
In the logistic regression model, predictors of transition to Group 3 were ischemic etiology, valvular etiology, systolic BP, Hb (OR 0.678, 95%CI 0.489–0.941, P = 0.020) and eGFR levels (OR 0.962, 95%CI 0.938–0.986, P = 0.020) (Table 5). On the other hand, transition to Group 0 was predicted by Hb (OR 1.316, 95%CI 1.148–1.509, P < 0.001), eGFR (OR 1.040, 95%CI 1.022–1.058, P < 0.001) and LVEF (OR 1.025, 95%CI 1.005–1.046, P = 0.012) (Table 5).
We then investigated the association between the increase in Hb levels and prognosis in patients with non/mild and moderate/severe anemia, respectively. We analyzed 1,026 patients who had Hb values on admission and discharge. Of 839 patients with non/mild anemia, 72 had increased Hb values during hospitalization, but 767 did not (ΔHb: 0.47 ± 0.32 vs -0.25 ± 0.56, p < 0.0001). There was no trend toward improved prognosis with improved anemia (Supplementary Fig. 5A). Of 187 cases of moderate/severe anemia, whereas 27 had increased Hb levels, 160 did not (ΔHb: 0.45 ± 0.29 vs -0.47 ± 1.40, p < 0.001). Patients with increased Hb levels during hospitalization tended to have a better prognosis, although not significantly, compared to those without it (Supplementary Fig. 5B).
Discussion
In this study, we found that the severity of anemia was more strongly associated with poor outcomes in HF patients with RD than in those without RD. Furthermore, moderate/severe anemia (Hb < 10 g/dL) and RD (eGFR < 60 ml/min/1.73 m2) had a similar and additive effect on the prognosis of HF patients. In addition, changes in anemia and RD levels during hospitalization were associated with post-discharge outcomes in HF patients. These findings provide important insights into the management of HF patients with anemia.
In general, the presence of cardiovascular risk factors tends to be more frequent in males. However, patients with anemia and/or RD were more likely to be females than males (Tables 1 and 3). This may be due to the fact that females are more likely to be older than males in this study. In addition, the lower prescription rate of beta-blocker might also be associated with age.
Numerous studies have shown that anemia is strongly associated with a poor prognosis in HF patients.1,2,3,4,5,6,7,8 However, the Japanese guideline on diagnosis and treatment of acute and chronic HF in 2017 did not describe an effective treatment for anemia in HF.25 In particular, the optimal therapeutic range for Hb levels remains unknown. A recent Japanese guideline for CKD recommends Hb < 10 g/dL as the therapeutic target. Therefore, in this study, we focused on the impact of Hb < 10 g/dL in HF patients. Mild anemia (Hb ≥ 10.0 g/dL, < 13.0 g/dL in males, ≥ 10.0 g/dL, < 12.0 g/dL in females) affected all-cause mortality but not the composite of all-cause death or HF rehospitalization and HF rehospitalization among HF patients without RD. On the other hand, mild anemia was associated with the composite outcome, all-cause mortality, and HF rehospitalization in HF patients with RD (Fig. 1 and Table 2). One of the reasons for this difference could be the small number of patients without RD compared to those with RD. However, at least, this study shows the relevance of anemia in RD rather than anemia in normal renal function.
While patients with moderate/severe anemia had the worst prognosis regardless of RD, the risk of adverse outcomes was higher in patients with RD than in those without RD (Table 2). In addition, Hb levels in each anemia severity class were comparable in patients with and without RD. In particular, Hb levels in moderate to severe anemia without/with RD were same (8.8 ± 1.4 g/dL and 8.6 ± 1.1 d/dL, respectively) (Table 1). These findings suggest that RD exacerbates adverse effects of anemia in HF patients regardless of Hb levels. Anemia and CKD are known to have an additive effect on poor outcomes in HF patients.12,15 However, the impact of anemia severity has not been understood. In this study, moderate/severe anemia and RD had a similar impact on the composite of all-cause death or HF rehospitalization, all-cause death, and HF rehospitalization (Table 4). In addition, moderate/severe anemia and RD had an additive negative effect on long-term outcomes in HF patients (Table 4). Furthermore, the combination of moderate/severe anemia and RD was linked to poorer outcome in all HF types (HFrEF, HFmrEF, and HFpEF). The worsening effects of the combination of moderate/severe anemia and RD are thought to be complicated. For example, the depleting treatment with a good response leads to a worsening of renal function and an improvement in anemia. However, in this study, only a few HF patients had improved anemia. This may be because the changes in Hb values during hospitalization is small. In fact, of 839 patients with non/mild anemia, 72 had increased Hb values during hospitalization, but 767 did not (ΔHb: 0.47 ± 0.32 vs -0.25 ± 0.56, p < 0.0001). Of 187 cases of moderate/severe anemia, whereas 27 had increased Hb levels, 160 did not (ΔHb: 0.45 ± 0.29 vs -0.47 ± 1.40, p < 0.001). In general, the period hospitalization in Japan is longer than that in western countries. We speculate that Hb values increase immediately after depletive treatment, and then other factors, such as worsened renal dysfunction, negatively affect anemia status during hospitalization. From another perspective, eGFR levels in HF patients with moderate/severe anemia and RD are likely to be lower than in patients with RD alone. Therefore, moderate/severe anemia in HF patients with RD requires intensive treatment. Several previous studies have demonstrated that elevated Hb levels at or above normal are detrimental not only in CKD but also in HF patients.16,17,18,21,26 Based on ours and previous findings, a therapeutic range of Hb at 10–12 g/dL may be appropriate even in HF patients, as recommended by the Japanese CKD guideline in 2023.
The timing of treatment for anemia is also important. Hb levels may fluctuate with RD during HF hospitalization. A rapid increase in Hb during the early phase of HF hospitalization was independently associated with a favorable outcome.22 Patients with acute Hb drop in levels during HF hospitalization had poor outcomes.23 However, the baseline Hb levels in these studies were 12.6 g/dL and 11.4 g/dL, respectively. Short-term changes in Hb levels in patients with moderate/severe anemia have not been investigated. Our findings have implications for this point. Changes from non/mild to moderate/severe anemia, with or without RD, were associated with a poor prognosis (Fig. 3B). In addition, Hb and eGFR levels predict worsening and improving anemia and RD (Table 3). Intriguingly, LVEF was an independent positive predictor of improving anemia and RD, suggesting that anemia and RD may be more likely to improve in patients with HFpEF. Patients with increased Hb levels during hospitalization tended to have a better prognosis than those without it (Supplementary Fig. 5B). The lack of statistically significant differences may be due to the sample size. Among patients from group 0 to group 1, 2, or 3, there was only one patient who transited group 0 to group 3 during hospitalization (data not shown). The other patients transited from group 0 to group 1 or 2. Thus, we cannot fully elucidate the characteristics of patients who transited group 0 to group 3. We need to investigate this issue in larger cohorts. However, our findings indicate that the prevention and treatment of moderate/severe anemia during hospitalization may be effective in improving outcomes for HF patients.
Regardless of the presence or absence of anemia, intravenous iron therapy was associated with improved exercise capacity and a lower risk of HF hospitalization and cardiovascular death in HF patients.27,28 However, intravenous iron therapy for HF was uncommon in 2004–2005. Thus, intravenous iron administration appears to have little or no effect in this study. Recently, hypoxia-inducible factor prolyl hydroxylase (HIF-PH) inhibitors have been used to treat renal anemia.29,30 A randomized controlled study is currently underway to determine the safety and efficacy of a HIF-PH inhibitor in patients with HF and renal anemia is ongoing.31 The effect of anemia treatment with HIF-PH inhibitors on prognosis in HF patients with and without renal anemia should be prospectively investigated in the future.
Study limitations
This study has several potential limitations that should be acknowledged. First, this study did not collect data on anemia treatment, such as ESAs, iron supplements, or blood transfusions. The effects of these treatments could not be excluded. Second, serum iron, ferritin, transferrin saturation, and erythropoietin levels were not determined in this study. Iron deficiency and renal anemia could not be properly diagnosed. The etiology of anemia might also have a significant prognostic impact, rather than just the Hb values. However, numerous previous studies have demonstrated that Hb levels are negatively correlated with prognosis in HF patients without investigating the cause of anemia.1,2,3,4,5,6,7,8 Like these studies, we focused on the severity of anemia in this study. Third, the JCARE-CARD is a previous study, in which patients were registered from January 2004 to June 2005 and the outcomes, including death and rehospitalization, were followed until 2007. At this time, neither sodium-glucose co-transporter 2 (SGLT2) inhibitors, ARNI (valsartan/sacubitril), ivabradine, nor HIF-PH inhibitors were used. Thus, the effect of improved medical management on patients with anemia and RD remains uncertain in this study. Extrapolation of our results to current clinical practice requires caution. Nonetheless, this study demonstrates the impact of moderate/severe anemia associated with CKD on HF patients, in addition to the relationship between these diseases. Furthermore, our data may provide reference points or a basis for investigating the effectiveness of improved treatments in the future. Forth, nutritional indicators such as albumin might affect the prognosis of HF patients with or without RD. However, our database did not contain serum albumin levels. Fifth, the exact cut-off point of moderate-severe anemia in terms of its impact on heart failure is still unknown. To elucidate this point, we need further investigations (for example, the cubic-spline analysis of clinical outcomes and Hb values) in a larger cohort. Finally, there may be unmeasured biases that affect the results. In particular, the effect of changes in Hb and eGFR over the follow-up period on long-term outcomes is unclear. To address these concerns, further investigation in larger-scale, more recent studies is needed. Furthermore, prospective studies are required to determine optimal Hb levels and how to improve anemia to improve prognosis in HF patients.
Conclusion
Moderate/severe anemia associated with RD had a negative impact on the prognosis of HF patients. The management of anemia and RD, particularly during HF hospitalization, is critical for HF patients. Further studies are needed to elucidate the impact of the etiology of anemia and the effect of recent advances in treatment in HF patients with anemia and RD.
Methods
Patient selection
Clinical data was collected from the JCARE‐CARD database. The baseline data includes (i) demographics; (ii) cause of HF; (iii) precipitating cause; (iv) co‐morbidities; (v) complications; (vi) clinical status; (vii) laboratory data; (viii) electrocardiographic and echocardiographic findings; and (ix) treatment including discharge medications. The discharge laboratory data were also collected. Follow‐up data was collected at least 1 year after the index admission. Patients with both Hb and creatinine levels at admission were selected.
Definition of anemia and renal dysfunction
Anemia was defined as a Hb level of < 13.0 g/dl in males and < 12.0 g/dl in females, based on World Health Organization criteria.2 Furthermore, mild and moderate/severe anemia were defined as Hb levels of ≥ 10.0 g/dl, < 13.0 g/dl in males and < 12.0 g/dl in females, and < 10.0 g/dl in both genders as same as previous studies.32,33,34 RD was defined as an estimated glomerular filtration rate (eGFR) < 60 mL/min/1.73 m2 based on stages of CKD.10.
Outcomes
The primary outcome of this study was a composite of all‐cause death or HF rehospitalization. Secondary outcomes were all‐cause death, HF rehospitalization, and in-hospital death.
Statistical analysis
Patients with mild anemia (Hb ≥ 10.0 g/dl, < 13.0 g/dL in males; Hb ≥ 10.0 g/dl, < 12.0 g/dL in females) and moderate/severe anemia (Hb < 10 g/dL) were compared with those without anemia (Hb ≥ 13.0 g/dL in males, ≥ 12.0 g/dL in females) according to RD. Patient characteristics, such as age, gender, New York Heart Association (NYHA) functional class, previous HF admission, echocardiographic data, co‐morbidities, previous procedures, and therapeutic agents, were compared using Pearson χ2 test for categorical variables and Student’s t‐test, or Wilcoxon rank sum test for continuous variables, as appropriate. Results were presented as mean ± SD or median with interquartile range (IQR). The cumulative incidence of outcomes was estimated using the Kaplan–Meier method and a Cox proportional hazards model including clinically relevant covariates. Adjusted hazard ratios (aHRs) were calculated using the Cox regression model and presented with a 95% confidence interval (CI) and P value. Covariates were selected based on previous studies investigating prognostic factors for HF patients.35,36 In detail, demographics (age, sex, BMI), previous HF admission, causes of heart failure (ischemic, hypertensive, dilated cardiomyopathy, valvular heart disease), medical history (hypertension, stroke, smoking, chronic atrial fibrillation or flutter), NYHA functional class, LVEF, and medication use (ACE inhibitor or ARB, β-blocker, MRA, digitalis) were selected. In-hospital death rates and predictors of group transition were assessed using the logistic regression model. In addition to factors shown above, blood pressure and heart rate were included as covariates. All tests were two-tailed with P < 0.05 indicating statistical significance. All analyses were conducted using JMP Pro (version 14.2.0, SAS Institute, Cary, North Carolina).
Ethical statement
This study protocol was designed to ensure compliance with the Declaration of Helsinki and the Guidelines for Epidemiological Research published by the Japanese Ministry of Health, Labour and Welfare. The original study protocol was approved by the Institutional Review Board (IRB) of Kyushu University. Because this study investigated a nationwide administrative database (unconnectable anonymized data), we could not obtain informed consent from each patient. The IRB of Kyushu University approved the waiver of informed consent. As a result, we announced our research on our website for a certain period of time instead of obtaining informed consent.
Availability of data and materials
The data for this article were obtained from a national database of JCARE-CARD. Derived data from this study will be made available upon reasonable request to the corresponding author.
References
Groenveld, H. F. et al. Anemia and mortality in heart failure patients a systematic review and meta-analysis. J. Am. Coll. Cardiol. 52, 818–827 (2008).
Hamaguchi, S. et al. Anemia is an independent predictor of long-term adverse outcomes in patients hospitalized with heart failure in Japan. A report from the Japanese Cardiac Registry of Heart Failure in Cardiology (JCARE-CARD). Circ J. 73, 1901–8 (2009).
Anand, I. S. et al. Anemia and change in hemoglobin over time related to mortality and morbidity in patients with chronic heart failure: Results from Val-HeFT. Circulation. 112, 1121–1127 (2005).
Ezekowitz, J. A., McAlister, F. A. & Armstrong, P. W. Anemia is common in heart failure and is associated with poor outcomes: Insights from a cohort of 12 065 patients with new-onset heart failure. Circulation. 107, 223–225 (2003).
Valeur N, Nielsen OW, McMurray JJ, Torp-Pedersen C, Kober L and Group TS. Anaemia is an independent predictor of mortality in patients with left ventricular systolic dysfunction following acute myocardial infarction. Eur. J. Heart Fail. 8, 577–584 (2006).
Szachniewicz, J. et al. Anaemia is an independent predictor of poor outcome in patients with chronic heart failure. Int J Cardiol. 90, 303–308 (2003).
Kalra, P. R. et al. Haemoglobin concentration and prognosis in new cases of heart failure. Lancet. 362, 211–212 (2003).
Grigorian Shamagian, L. et al. Anaemia is associated with higher mortality among patients with heart failure with preserved systolic function. Heart. 92, 780–784 (2006).
Ezekowitz, J. et al. The association among renal insufficiency, pharmacotherapy, and outcomes in 6,427 patients with heart failure and coronary artery disease. J. Am. Coll. Cardiol. 44, 1587–1592 (2004).
Hamaguchi, S. et al. Chronic kidney disease as an independent risk for long-term adverse outcomes in patients hospitalized with heart failure in Japan. Report from the Japanese Cardiac Registry of Heart Failure in Cardiology (JCARE-CARD). Circ. J. 73, 1442–7 (2009).
Heywood JT, Fonarow GC, Costanzo MR, Mathur VS, Wigneswaran JR, Wynne J, Committee ASA and Investigators. High prevalence of renal dysfunction and its impact on outcome in 118,465 patients hospitalized with acute decompensated heart failure: a report from the ADHERE database. J. Card. Fail. 2007;13:422–30.
Herzog, C. A., Muster, H. A., Li, S. & Collins, A. J. Impact of congestive heart failure, chronic kidney disease, and anemia on survival in the Medicare population. J. Card. Fail. 10, 467–472 (2004).
Anand, I. et al. Anemia and its relationship to clinical outcome in heart failure. Circulation. 110, 149–154 (2004).
Silverberg, D. S., Wexler, D., Iaina, A. & Schwartz, D. The interaction between heart failure and other heart diseases, renal failure, and anemia. Semin. Nephrol. 26, 296–306 (2006).
Klip, I. T. et al. The additive burden of iron deficiency in the cardiorenal-anaemia axis: scope of a problem and its consequences. Eur. J. Heart Fail. 16, 655–662 (2014).
Singh, A. K. et al. Correction of anemia with epoetin alfa in chronic kidney disease. N. Engl. J. Med. 355, 2085–2098 (2006).
Drueke, T. B. et al. Normalization of hemoglobin level in patients with chronic kidney disease and anemia. N. Engl. J. Med. 355, 2071–2084 (2006).
Pfeffer, M. A. et al. A trial of darbepoetin alfa in type 2 diabetes and chronic kidney disease. N. Engl. J. Med. 361, 2019–2032 (2009).
Hayashi, T. et al. Darbepoetin alfa in patients with advanced CKD without diabetes: randomized, controlled trial. Clin. J. Am. Soc. Nephrol. 15, 608–615 (2020).
Tsuruya K, Hayashi T, Yamamoto H, Hase H, Nishi S, Yamagata K, Nangaku M, Wada T, Uemura Y, Ohashi Y, Hirakata H and Investigators R-CS. Renal prognoses by different target hemoglobin levels achieved by epoetin beta pegol dosing to chronic kidney disease patients with hyporesponsive anemia to erythropoiesis-stimulating agent: a multicenter open-label randomized controlled study. Clin. Exp. Nephrol. 2021;25:456–466.
Swedberg, K. et al. Treatment of anemia with darbepoetin alfa in systolic heart failure. N. Engl. J. Med. 368, 1210–1219 (2013).
van der Meer, P. et al. The predictive value of short-term changes in hemoglobin concentration in patients presenting with acute decompensated heart failure. J. Am. Coll. Cardiol. 61, 1973–1981 (2013).
Lopez, C. et al. Impact of acute hemoglobin falls in heart failure patients: A population study. J. Clin. Med. 9, 1869 (2020).
Tsutsui, H. et al. Clinical characteristics and outcome of hospitalized patients with heart failure in Japan. Circ. J. 70, 1617–1623 (2006).
Tsutsui H, Isobe M, Ito H, Ito H, Okumura K, Ono M, Kitakaze M, Kinugawa K, Kihara Y, Goto Y, Komuro I, Saiki Y, Saito Y, Sakata Y, Sato N, Sawa Y, Shiose A, Shimizu W, Shimokawa H, Seino Y, Node K, Higo T, Hirayama A, Makaya M, Masuyama T, Murohara T, Momomura SI, Yano M, Yamazaki K, Yamamoto K, Yoshikawa T, Yoshimura M, Akiyama M, Anzai T, Ishihara S, Inomata T, Imamura T, Iwasaki YK, Ohtani T, Onishi K, Kasai T, Kato M, Kawai M, Kinugasa Y, Kinugawa S, Kuratani T, Kobayashi S, Sakata Y, Tanaka A, Toda K, Noda T, Nochioka K, Hatano M, Hidaka T, Fujino T, Makita S, Yamaguchi O, Ikeda U, Kimura T, Kohsaka S, Kosuge M, Yamagishi M, Yamashina A, Japanese Circulation S and the Japanese Heart Failure Society Joint Working G. JCS 2017/JHFS. Guideline on diagnosis and treatment of acute and chronic heart failure - digest version. Circ. J. 2019(83), 2084–2184 (2017).
Go, A. S. et al. Hemoglobin level, chronic kidney disease, and the risks of death and hospitalization in adults with chronic heart failure: The Anemia in Chronic Heart Failure: Outcomes and Resource Utilization (ANCHOR) Study. Circulation. 113, 2713–2723 (2006).
Ponikowski P, Kirwan BA, Anker SD, McDonagh T, Dorobantu M, Drozdz J, Fabien V, Filippatos G, Gohring UM, Keren A, Khintibidze I, Kragten H, Martinez FA, Metra M, Milicic D, Nicolau JC, Ohlsson M, Parkhomenko A, Pascual-Figal DA, Ruschitzka F, Sim D, Skouri H, van der Meer P, Lewis BS, Comin-Colet J, von Haehling S, Cohen-Solal A, Danchin N, Doehner W, Dargie HJ, Motro M, Butler J, Friede T, Jensen KH, Pocock S, Jankowska EA and investigators A-A. Ferric carboxymaltose for iron deficiency at discharge after acute heart failure: a multicentre, double-blind, randomised, controlled trial. Lancet. 2020;396:1895–1904.
Kalra PR, Cleland JGF, Petrie MC, Thomson EA, Kalra PA, Squire IB, Ahmed FZ, Al-Mohammad A, Cowburn PJ, Foley PWX, Graham FJ, Japp AG, Lane RE, Lang NN, Ludman AJ, Macdougall IC, Pellicori P, Ray R, Robertson M, Seed A, Ford I and Group IS. Intravenous ferric derisomaltose in patients with heart failure and iron deficiency in the UK (IRONMAN): an investigator-initiated, prospective, randomised, open-label, blinded-endpoint trial. Lancet. 400, 2199–2209 (2022).
Chen, N. et al. Roxadustat for anemia in patients with kidney disease not receiving dialysis. N. Engl. J. Med. 381, 1001–1010 (2019).
Singh AK, Carroll K, McMurray JJV, Solomon S, Jha V, Johansen KL, Lopes RD, Macdougall IC, Obrador GT, Waikar SS, Wanner C, Wheeler DC, Wiecek A, Blackorby A, Cizman B, Cobitz AR, Davies R, DiMino TL, Kler L, Meadowcroft AM, Taft L, Perkovic V and Group A-NS. Daprodustat for the treatment of anemia in patients not undergoing dialysis. N. Engl. J. Med. 2021;385:2313–2324.
Iso, T. et al. Daprodustat for anaemia in patients with heart failure and chronic kidney disease: A randomized controlled study. ESC Heart Fail. 9, 4291–4297 (2022).
Kiec-Kononowicz, K., Stypula, E., Krupinska, J. & Cebo, B. Pharmacological properties of 3-aminoalkyl and amide derivatives of 5,5-diphenylhydantoin. Pol. J. Pharmacol. Pharm. 37, 693–699 (1985).
Prezioso, F. A. Spirituality in the recovery process. J. Subst. Abuse Treat. 4, 233–238 (1987).
Hashimoto, K. et al. Burden of mild (<13 g/dl) anemia in patients with atrial fibrillation (a report from a multicenter registry with patient-reported outcomes). Am. J. Cardiol. 157, 48–55 (2021).
Perea-Armijo J, Lopez-Aguilera J, Gonzalez-Manzanares R, Pericet-Rodriguez C, Castillo-Dominguez JC, Heredia-Campos G, Roldan-Guerra A, Urbano-Sanchez C, Barreiro-Mesa L, Aguayo-Cano N, Delgado-Ortega M, Crespin-Crespin M, Ruiz-Ortiz M, Mesa-Rubio D, Osorio MP and Anguita-Sanchez M. The worsening of heart failure with reduced ejection fraction: The impact of the number of hospital admissions in a cohort of patients. J Clin Med. 2023;12.
Ide, T. et al. Clinical characteristics and outcomes of hospitalized patients with heart failure from the large-scale japanese registry of acute decompensated heart failure (JROADHF). Circ J. 85, 1438–1450 (2021).
Acknowledgements
This study could not have been carried out without the assistance, cooperation, and support of cardiologists in the survey institutions. We thank them for allowing us to obtain the information.
Funding
This research was supported by Japan Agency for Medical Research and Development (AMED) under Grant Number JP24he2202019 (K.A).
Author information
Authors and Affiliations
Contributions
Study conception and design: EN, SM; Leadership: SM; Critical review of study design and oversight of study conduct: SM, KS, TF, SK, TS; Analysis plan: EN, NE, KY, KH; Data acquisition: EN, SM; Statistical analysis: EN, NE, YT, KM; Manuscript preparation: EN, SM; Drafting and revision of the manuscript: EN, SM, NE, TH, SK, KA. All authors made important intellectual contributions during the drafting or revision of the manuscript and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Noda, E., Matsushima, S., Hashimoto, T. et al. Prognostic impact of moderate to severe anemia associated with renal dysfunction in patients with heart failure. Sci Rep 15, 3918 (2025). https://doi.org/10.1038/s41598-025-87650-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-87650-z