Abstract
While silk fibroin (SF) obtained from silkworm cocoons is expected to become a next-generation natural polymer, a fabrication method for SF-based artificial nerve conduits (SFCs) has not yet been established. Here, we report a bioresorbable SFC, fabricated using a novel freeze–thaw process, which ensures biosafety by avoiding any harmful chemical additives. The SFC demonstrated favorable biocompatibility (high hydrophilicity and porosity with a water content of > 90%), structural stability (stiffness, toughness, and elasticity), and biodegradability, making it an ideal candidate for nerve regeneration. We evaluated the nerve-regenerative effects of the SFC in a rat sciatic-nerve-defect model, including its motor and sensory function recovery as well as histological regeneration. We found that SFC transplantation significantly promoted functional recovery and nerve regeneration compared to silicone tubes and was almost equally effective as autologous nerve transplantation. Histological analyses indicated that vascularization and M2 macrophage recruitment were pronounced inside the SFC. These results suggest that the unique properties of the SFC further enhanced the peripheral nerve regeneration mechanism. As no SFC has been applied in clinical practice, the SFC reported herein may be a promising candidate for repairing extensive peripheral nerve defects.
Similar content being viewed by others
Introduction
Peripheral nerve injuries often occur as a result of trauma or surgical procedures and lead to significant impairments in daily life due to motor dysfunction, sensory impairment, or neuropathic pain1. Most severe peripheral nerve injuries do not heal spontaneously and require surgical intervention for recovery. For short gaps in nerve continuity, end-to-end nerve suturing is indicated; however, large defects often require nerve transplantation2. The current gold standard for treating large nerve-injury defects is autologous nerve transplantation. However, it presents several drawbacks, such as donor site morbidity, limited graft length, and prolonged surgery times3,4. As alternatives, various artificial nerve conduits have been developed using different materials and fabrication methods5,6, albeit with insufficient nerve-regeneration outcomes.
Artificial nerve conduits need to be optimized for biocompatibility, structural stability, biodegradability, and biosafety5,6,7,8. Biocompatibility with sufficient hydrophilicity and porosity is important to support cell migration and proliferation to allow passage of neurotrophic factors while inhibiting infiltration of exogenous fibroblasts, all of which lead to scar formation6,9,10,11. Structural stability with favorable stiffness, toughness, and elasticity is also required to maintain the luminal structure of the conduit, which is required for axonal guidance. To avoid entrapment-like symptoms as foreign bodies, the conduits need to be biodegradable in the long term and at appropriate degradation rates6. Furthermore, clinical applications require biosafety, and degradation products should be as little cytotoxic and immunogenic as possible8.
To generate an ideal artificial nerve conduit that would meet these requirements, we developed a bioresorbable silk fibroin (SF)-based artificial nerve conduit (SFC) fabricated by a novel freeze–thaw process12. SF is a natural protein, obtained by removing sericin from the cocoons of Bombyx mori silkworm6,13,14. As silk has been widely used for surgical sutures15, SF materials are biocompatible, biodegradable, and biosafe. SF was originally known to support Schwann cell and neuronal attachment during nerve regeneration both in vitro and in vivo without causing cytotoxicity or adverse immune responses16,17,18,19,20,21,22,23.
Several fabrication methods have been reported for the development of nerve conduits using SF, such as freeze-drying, electrospinning, or special freezing techniques, all of which have demonstrated the usefulness of SF materials as nerve conduits24,25,26,27. However, these processes are complicated and require special equipment to configure the precise conditions for production. In addition, these conventional processes require the use of harmful chemicals such as formic acid, polyethylene oxide, or methanol for stabilization16,17,18,19,20,21,22,23. In contrast, our novel fabrication method is simple, and no harmful chemicals or special equipment are required to fabricate porous structures because the procedure is implemented by freezing and thawing aqueous SF solutions, mixed with small amounts of water-miscible organic solvents12. Since the regenerative effects of SF sponges prepared by our freeze–thaw process have already been demonstrated in the cartilage and skin28,29, the SFC is expected to constitute an ideal artificial nerve conduit for extensive peripheral nerve defects, probably owing to its unique physical properties of biocompatibility, structural stability, biodegradability, and biosafety.
Here, we sought to determine the unique physical properties of SFCs fabricated via a novel freeze–thaw process and evaluate their efficacy in inducing peripheral nerve regeneration. We performed quantitative comparisons in vivo and evaluated their motor and sensory function recovery as well as their ability to induce histological regeneration.
Methods
Ethics declaration
This experiment was approved by the Keio University Institutional Animal Care and Use Committee in accordance with institutional guidelines (approval number 17024). The study complied with the ARRIVE guidelines, and all the methodology described in this section was performed according to the relevant guidelines and regulations.
Preparation of the SFC
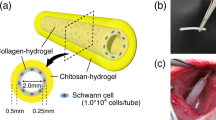
SF was prepared from domestic Bombyx mori silkworm cocoons (Kinsyu x Showa, Atsumaru Holdings Silk Co., Ltd., Kumamoto, Japan). The cocoon was degummed with 0.02 M Na2CO3 at 95–98 °C for 30 min to remove sericin. The obtained SF was dissolved in 9 M LiBr at room temperature, and the solution was dialyzed against pure water to prepare an SF aqueous solution. Then, dimethyl sulfoxide (DMSO, Fujifilm-Wako, Tokyo, Japan) at 1% (v/v) of the final concentration was added to the 8% (w/v) SF aqueous solution. The mixed solution was poured into the mold, which consisted of an aluminum tube (inner diameter: 5 mm; outer diameter: 6 mm) and a polytetrafluoroethylene rod (φ3 mm) with a 3D-printed resin cap (Fig. 1A). The mold was placed in a programmable cooling bath (NCB-3300, EYELA, Tokyo, Japan) with ethanol brine, frozen at − 20 °C for > 8 h, and subsequently kept at room temperature to allow thawing, as previously reported12. The fabricated SFC was removed from the mold and washed with pure water for three days to remove the DMSO. The fabricated SFC had the designed tubular shape (inner diameter: 3 mm; outer diameter: 5 mm) (Fig. 1B).
Fabrication of a silk fibroin conduit (SFC) and transplantation procedures at transected sciatic nerves bearing 13-mm gaps. (A) Mold used for the fabrication of the SFC. (B) Appearance of the SFC. (C) Silicone tube (NC) transplant. (D) Autologous nerve (Auto) transplant. (E) SFC transplant. (F) Sham.
Evaluation of physical properties of the SFC
We prepared SFCs of 10 mm in length and used three SFC samples to perform each of the following tests to evaluate their physical properties.
To evaluate the hydrophilicity of the SFC, we measured the conduit water content. After fully immersing a conduit into distilled water for 24 h, its wet weight was measured after wiping off the excess water. The dry weight of the conduit was measured after it had been vacuum-dried to a constant weight. The water content was calculated using the following formula: Water content (%) = (W0 − W1 / W0) × 100, where W0 and W1 are the weights of the wet and dried SFCs, respectively. Porosity was also evaluated by measuring the SFC pore size. The conduit cross-section was observed via scanning electron microscopy (SEM; JEOL Ltd., Tokyo, Japan) to estimate the average pore size.
The structural stability of the SFC was investigated using a creep meter (RE2-33005B, Yamaden Co., Ltd., Tokyo, Japan) at 25 °C. The compression test was performed by advancing a parallel plate (φ30 mm) attached to the creep meter at a rate of 0.05 mm/s and applying a uniform compressive load perpendicularly to the longitudinal axis of the specimen. Data on force and displacement were recorded at 5-μm intervals to evaluate the stress at 25% or 50% SFC compression. After applying 50% strain to the SFC, the load was immediately removed at a rate of 5 mm/s. The SFC was then left undisturbed for 10 min, after which we measured the diameter height in the direction in which the previously applied load had been measured. The restoration rate of the luminal structure after 50% compression was calculated using the following equation: Restoration rate (%) = (L1 / L0) × 100, where L0 is the initial diameter height in the direction of the load, and L1 is the diameter height in the direction of the load after load application.
Since the SFC is extremely stable in water owing to its fabrication in aqueous solution using our freeze–thaw process12, its biodegradability was assessed by immersion in phosphate-buffered saline (PBS) solution pH7.4 containing protease XIV (Sigma-Aldrich, St Louis, MO, USA) to accelerate its degradation. We prepared PBS solution containing 2.0 U/mL protease XIV, i.e., a highly concentrated enzyme solution compared to the enzyme concentration in the in-vivo environment26. The SFC was incubated in this enzyme solution at 37 °C and observed at days 0, 1, 3, 14, and 28 to assess its structural integrity.
Experimental animals and surgical procedures
Eight-week-old male Sprague Dawley rats (Japan SLC Inc., Shizuoka, Japan) were used to prepare a sciatic-nerve-defect model. All rats were anesthetized by subcutaneous injection of a mixture of three anesthetics (2.5 mg/kg butorphanol, 0.4 mg/kg medetomidine hydrochloride, and 2 mg/kg midazolam). A dorsal longitudinal skin incision was made, and the sciatic nerve was exposed by incising the gluteal fascia and bluntly splitting the gluteal muscle. The sciatic nerve was resected at the middle of the thigh, and its gap was repaired by fixing the nerve stumps 1 mm inside the end of the artificial nerve tube using a horizontal mattress suture of 9–0 monofilament nylon at each end, leaving a 13 mm inter-stump gap. The rats were assigned to four groups as described below (Fig. 1C–F). Rats in the SFC transplantation group received a 15 mm-long SFC filled with only 0.1 M PBS to bridge the gap (SFC group: n = 10). Rats in the negative control group were given a 15-mm-long silicone tube (Taiyo Kogyo, Tokyo, Japan) with an inner diameter of 3 mm and an outer diameter of 5 mm, filled with only 0.1 M PBS to bridge the gap (NC group: n = 10). Rats in the autologous nerve transplantation group underwent a procedure where the 13 mm gap was reconstructed by turning the resected nerve over and bridging it (Auto group: n = 10). Rats in the sham group had their sciatic nerves exposed, without incurring any damage to the nerve (Sham group: n = 10). All nerve suturing procedures required in the NC, SFC, and Auto groups were performed under a surgical microscope. The overlying muscle layers and skin were closed with 5–0 nylon sutures. After 12 weeks of transplantation, peripheral nerve regeneration was assessed electrophysiologically and by measuring the wet gastrocnemius muscle weight. All rats in each group were euthanized and regenerated nerves were harvested at 12 weeks after the transplantation.
Gate tracking analysis
Gate tracking analysis was performed every two weeks after transplantation using the DigiGait System (Rat Specifics, Inc., Framingham, MA, USA). Rats were placed on the transparent board and their footprints were scanned. We measured the sciatic functional index (SFI), which was calculated using the following formula 30: SFI = − 38.3 × (EPL – NPL / NPL) + 109.5 × (ETS – NTS / NTS) − 13.3 × (EIT – NIT / NIT) − 8.8 (EPL: experimental print length, NPL: normal print length, ETS: experimental toe spread, NTS: normal toe spread, EIT: experimental intermediary toe spread, NPL: normal intermediary toe spread).
Motor functional evaluation for ankle motion range and muscle weight
The ankle passive range of motion on the operated limb was measured at 12 weeks after the transplantation in adequately anesthetized rats. Muscle weight recovery was also evaluated at 12 weeks after the transplantation. Bilateral gastrocnemius muscles were harvested, and the muscle recovery was calculated by comparing the wet weights between the experimental and control limbs.
Touch and thermal sensation assessment
To assess tactile and thermal hyperalgesia, the von Fray hair and Hargreaves plantar tests were performed at 12 weeks after the transplantation. In the von Fray hair test, rats were placed in boxes with mesh flooring and allowed to acclimatize for 30 min. Mechanical hyperalgesia was tested by applying gradually increasing pressure to the mid-plantar surface of both hind paws using a nylon monofilament (Semmes–Weinstein Aesthesiometer; Stoelting, Wood Dale, IL, USA). The stimulus was applied manually to the mid-plantar surface of the hind paw and continued until withdrawal31. The up-down method was used to calculate the threshold32. A lower von Frey score indicates increased tactile sensitivity, that is, a weaker stimulus can trigger a response; This phenomenon is typically observed in conditions, such as mechanical allodynia and tactile hyperalgesia, wherein even minor touch causes pain or discomfort32,33. In the Hargreaves plantar test, rats were placed on the glass of the specific apparatus (IITC Life Science, Woodland Hills, CA, USA). The time until withdrawal response after the application of radiant heat to the plantar surface of the hind paw was measured and the average latency across three trials per paw on each side was recorded34. Shorter paw withdrawal latency indicates increased thermal sensitivity or hyperalgesia, wherein the rat experiences pain more quickly33,34.
Electrophysiological study
Electrophysiological evaluation was performed using an electromyography apparatus (MEB-9402; Nihon Kohden, Tokyo, Japan) as previously described35. All rats were adequately anesthetized, their sciatic nerves were re-exposed at 12 weeks after the transplantation, and a supramaximal electrical stimulus (0.2 ms duration) was applied to the intact sciatic nerve proximally 5 mm from the nerve graft. The compound muscle action potential (CMAP) latency and amplitude were measured to evaluate the functional nerve recovery.
Fluorescence immunohistochemistry
Sciatic nerves were harvested from anesthetized rats at 12 weeks post transplantation for histological analysis. Specimens were fixed in 4% PFA in 0.1 M PBS at 4 °C for 24 h and embedded in 15% and 30% sucrose for cryoprotection. Silicone tubes and SFCs surrounding the regenerating nerves were removed during fixation. The specimens were embedded in a frozen section compound (FSC22 Blue; Leica Biosystems, Germany), frozen in liquid nitrogen, and sliced axially at 8-µm thickness using a cryostat (CM3050S; Leica Microsystems, Wetzlar, Germany). After blocking with the blocking solution; Blocking One (Nacalai Tesque, Kyoto, Japan), 20 times diluted with 0.1 M PBS containing 0.2% TritonX-100, the following primary antibodies were applied: rabbit polyclonal anti-neurofilament heavy (NFH) polypeptide antibody (ab8135; 1:500 dilution; Abcam), chicken myelin basic protein polyclonal anti-peptide antibody (MBP88837983; 1:500 dilution; Aves), goat polyclonal anti-mouse and anti-rat CD31 (AF3628; 1:100 dilution; R&D), rabbit polyclonal anti-Iba1 antibody (GtX100042; 1:500 dilution; GeneTex), and goat polyclonal anti-arginase-1 antibody (ab60176; 1:100 dilution; Abcam). Next, the sections were incubated with Alexa Fluor-conjugated secondary antibodies (1:800; Thermo Fisher Scientific), and nuclei were stained with Hoechst 33,258 (94,403, 10 µg/mL; Sigma-Aldrich). The specimens were observed using a fluorescence microscope (BZ-X800; Keyence, Osaka, Japan) or a confocal laser-scanning microscope (LSM780; Carl Zeiss, Jena, Germany). Images were quantitatively analyzed using ImageJ software (National Institute of Health).
Electron microscopic histological analysis
Sciatic nerves from the NC (n = 5), SFC (n = 5), Auto (n = 5), and Sham (n = 5) groups were used for observation via electron microscopy (EM), as previously described36. Samples were dissected and fixed with 2.5% glutaraldehyde in 0.1 M sodium cacodylate buffer (pH 7.4) for 24 h at 4 °C. After 2 h of post-fixation in 1% osmium tetroxide at 4 °C, they were dehydrated using different ratios of ethanol, acetone, and n-butyl glycidyl ether (QY-1, Okenshoji Co. Ltd., Japan), to epoxy resin (epoxy resin: QY-1 equal to 1:3, 1:1, or 3:1) or 100% epoxy resin, before being finally embedded into 100% epoxy resin followed by polymerization at 65 °C for 72 h. Semithin 1-μm and ultrathin 80-nm sections in the axial plane were sliced from resin blocks using an ultramicrotome (UC7, Leica, Germany). The semithin sections were stained with 0.1% toluidine blue and imaged with an ECLIPSE Ci microscope (Nikon, Tokyo, Japan) to quantify the total number and area of axons using ImageJ. Ultrathin sections were prepared on copper grids and silicon wafers, stained with uranyl acetate and lead citrate, and imaged using transmission (JEM-1400Plus, JEOL Ltd.; H-7650, Hitachi High Technology, Tokyo, Japan) and scanning EM (SU6600 and S-3700N, Hitachi; multiSEM505, CarlZeiss, Oberkochen, Germany). For quantitative G-ratio analysis, which is calculated by dividing the axon diameter by the myelin outer diameter, myelinated axons were analyzed from randomized EM images per animal. For > 20% of the entire neural area of each sample, seven randomly selected visual fields were photographed in each sample of the four groups, as previously reported37,38. Myeltracer software was used to measure axon diameter and calculate the G-ratio39.
Statistical methods
All collected data were presented as the mean ± standard error of the mean. The normality of data distribution was confirmed using the Shapiro–Wilk test. Continuous variables were compared using one-way analysis of variance, and Levene’s tests were performed to assess homoscedasticity. Variables with uniform and non-uniform variance were analyzed using the Tukey’s honest significance test and Games–Howell method, respectively. Statistical analyses were performed using SPSS 28.0.1.0 (IBM, Armonk, NY, USA). Statistical significance was set at a p-value of < 0.05.
Results
Physical properties of the SFC
The physical properties of the SFC are presented in Table 1. The water content was sustained at > 90%, and the SFC wall had a microporous structure with approximately 32 ± 7 µm pores (Fig. 2A). These high hydrophilicity and porosity could lead to favorable biocompatibility as a conduit.
The mechanical properties of the SFC are also shown in Table 1. The compression test results allowed us to estimate a stiffness of 1.6 ± 0.5 kPa at 25% and 3.2 ± 0.8 kPa at 50% compression. No conduit collapsed against the compression, and the restoration rate after 50% compression was 98.5% ± 1.0%. These mechanical properties of favorable stiffness, toughness, and elasticity ensure the structural stability of the SFC.
The biodegradability of the SFC was assessed using protease XIV solution (Fig. 2B). The SFCs remained unfragmented and maintained their luminal structures for three days. On day 14, the SFCs were partially degraded and lost their structural integrity. On day 28, the SFCs lost their original structures completely. Considering that the degradation was accelerated under the highly concentrated enzyme solution, we conclude that the SFC biodegradation and resorption from the body require a long period after its transplantation.
Recovery of motor function and sensation
To evaluate the functional recovery of nerve regeneration, gait tracking analysis was performed to calculate the SFI (Fig. 3A). The SFC group showed higher values than the NC group over time. At 12 weeks post transplantation, the SFI for the SFC group was significantly higher than that for the NC group, whereas no significant difference was observed between the SFC and Auto groups (NC: − 86.7 ± 2.7; SFC: − 74.4 ± 3.9; Auto: − 71.7 ± 3.5; Auto: − 8.6 ± 0.5; NC vs. SFC: p = 0.03; NC vs. Auto: p = 0.005; NC vs. Sham: p < 0.001; SFC vs. Auto: p = 0.91; SFC vs. Sham: p < 0.001; Auto vs. Sham: p < 0.001). The ankle passive range of motion was also measured to assess the ankle joint contracture (Fig. 3B). The ankle range of motion in the SFC group was significantly more preserved without contracture compared with that in the NC group, whereas no significant difference was observed between the SFC and Auto groups (NC: 122 ± 4°; SFC: 146 ± 5°; Auto: 148 ± 2°; Sham: 166 ± 1°; NC vs. SFC: p < 0.001; NC vs. Auto: p < 0.001; NC vs. Sham: p < 0.001; SFC vs. Auto: p = 0.98; SFC vs. Sham: p < 0.001; Auto vs. Sham: p = 0.002; Fig. 3C). The von Frey monofilament test and the Hargreaves plantar test were used to assess tactile and thermal hyperalgesia. At 12 weeks after transplantation, the score in the von Frey monofilament test for the SFC group was significantly higher than that for the NC group, with no significant difference compared with the Auto group (NC: 0.36 ± 0.12 g; SFC: 2.70 ± 0.44 g; Auto: 2.93 ± 0.37 g; Sham: 3.74 ± 0.25 g; NC vs. SFC: p < 0.001; NC vs. Auto: p < 0.001; NC vs. Sham: p < 0.001; SFC vs. Auto: p = 0.96; SFC vs. Sham: p = 0.12; Auto vs. Sham: p = 0.29; Fig. 3D). Hargreaves plantar test revealed that the scores for the SFC groups were significantly higher than those for the NC group and comparable to those for the Auto group (NC: 15.4 ± 0.7 s; SFC: 17.7 ± 0.7 s; Auto: 17.8 ± 0.6 s; Sham: 19.7 ± 0.2 s; NC vs. SFC: p = 0.03; NC vs. Auto: p = 0.03; NC vs. Sham: p < 0.001; SFC vs. Auto: p = 1.00; SFC vs. Sham: p = 0.08; Auto vs. Sham: p = 0.10; Fig. 3E). All these results indicate that the SFC transplantation group contributed more to the restoration of motor and sensory functions than did the NC group and performed comparably to the Auto group. However, the NC, SFC, and Auto groups showed less functional recovery compared to the Sham group.
Recovery of motor function and sensation. The silk fibroin conduit (SFC) group showed better nerve recovery than the negative control (NC) group and was comparable to the Auto group. (A) Sciatic functional index (SFI) measured over time post transplantation. The SFI of the SFC group was significantly higher than that of the NC group at 12 weeks post transplantation. (B) Images of the ankle range of motion under anesthesia at 12 weeks, showing ankle joint contracture. (C) The ankle-joint range of motion of the SFC group was significantly more preserved without contracture compared to that of the NC group. (D) The score of the von Frey monofilament test for touch sensation in the SFC group was significantly higher than that in the NC group. (E) The score of the Hargreaves plantar test for thermal sensation in the SFC group was significantly higher than that in the NC group.
Restoration of innervated muscles following nerve regeneration
To characterize the nerve-innervation status of muscles, we evaluated them electrophysiologically. The CMAP latency was not significant different in the NC, SFC, and Auto groups (NC: 2.93 ± 0.28 ms; SFC: 2.51 ± 0.28 ms; Auto: 2.57 ± 0.19 ms; Sham: 1.38 ± 0.07 ms; NC vs. SFC: p = 0.56; NC vs. Auto: p = 0.68; NC vs. Sham: p < 0.001; SFC vs. Auto: p = 1.00; SFC vs. Sham: p = 0.006; Auto vs. Sham: p = 0.003; Fig. 4A). The CMAP amplitude in the SFC group was significantly higher than that in the NC group (NC: 2.8 ± 0.4 mV; SFC: 9.5 ± 1.1 mV; Auto: 15.9 ± 1.4 mV; Sham: 32.7 ± 1.8 mV; NC vs. SFC: p = 0.004; NC vs. Auto: p < 0.001; NC vs. Sham: p < 0.001; SFC vs. Auto: p = 0.005; SFC vs. Sham: p < 0.001; Auto vs. Sham: p < 0.001; Fig. 4B). The extent of muscle atrophy was assessed by calculating the ratio of the gastrocnemius wet weight of the treated to the healthy side at 12 weeks after transplantation (Fig. 4C). The SFC group exhibited less muscular atrophy than the NC group (NC: 0.22 ± 0.16; SFC: 0.39 ± 0.49; Auto: 0.57 ± 0.19; Sham: 1.00 ± 0.06; NC vs. SFC: p < 0.001; NC vs. Auto: p < 0.001; NC vs. Sham: p < 0.001; SFC vs. Auto: p < 0.001; SFC vs. Sham: p < 0.001; Auto vs. Sham: p < 0.001; Fig. 4D). These data indicate that muscle innervation was significantly restored in the SFC group compared with that in the NC group but not to the same extent as in the Auto and Sham groups.
Restoration of innervated muscles following nerve regeneration. The SFC group showed a higher degree of innervated muscle restoration than the NC group but not as much as the Auto group. (A) Electrophysiological evaluation showing no significant differences in the latency of CMAP between the NC, SFC, and Auto groups. (B) The CMAP amplitude in the SFC group was significantly higher than that in the NC group but lower than that in the Auto group. (C) Images of the gastrocnemius of the nerve-transplanted sides (left) and the healthy control sides (right). (D) The SFC group showed less muscular atrophy than the NC group but more atrophy than the Auto group.
Promotion of axonal regeneration after transplantation
To assess the extent of nerve regeneration, histological recovery was evaluated in vivo at 12 weeks post transplantation. The sciatic nerves from each experimental limb were harvested, fixed, and examined using an optical microscope (Fig. 5A). In the SFC group, the luminal structure was preserved, and after the conduit was incised and removed, substantial regenerated tissues were observed inside. In contrast, minimal nerve regeneration was observed in the NC group, consistent with previous reports40,41.
Promotion of axonal regeneration after transplantation. The SFC group showed a greater extent of axonal regeneration than the NC group and was comparable to the Auto group. (A) Representative images of regenerated sciatic nerves at 12 weeks post transplantation. In the SFC group, the luminal structure was maintained. After the conduit was incised and removed, sufficient regenerated tissues were observed inside the conduit. In contrast, minimal nerve regeneration was observed in the NC group. (B) Toluidine blue staining of central axial sections of the regenerated nerves showing that the SFC group exhibited a higher number of regenerated nerve fibers. (C, D) Quantitative analysis of axon count and total axon area showing that the SFC group presented a higher number of regenerated axons than the NC group and was comparable to the Auto group.
In axial toluidine-blue-stained sections corresponding to the center of the regenerated nerve, the SFC group exhibited greater regeneration of the nerve fibers than the NC group, indicating enhanced recovery of a higher number of axons inside the SFC (Fig. 5B). To characterize the regeneration trend, quantitative analyses of axon count and total area were performed. Compared to the NC group, the SFC group showed significant regenerative effects, which were comparable to those in the Auto group in terms of axon count (NC: 288 ± 119; SFC: 4,621 ± 932; Auto: 6,382 ± 483; Sham: 5,853 ± 168; NC vs. SFC: p < 0.001; NC vs. Auto: p < 0.001; NC vs. Sham: p < 0.001; SFC vs. Auto: p = 0.11; SFC vs. Sham: p = 0.38; Auto vs. Sham: p = 0.90; Fig. 5C) and total axon area (NC: 1,675 ± 857 µm2; SFC: 31,900 ± 6,683 µm2; Auto: 45,339 ± 3,220 µm2; Sham: 11,0382 ± 4,154 µm2; NC vs. SFC: p < 0.001; NC vs. Auto: p < 0.001; NC vs. Sham: p < 0.001; SFC vs. Auto: p = 0.14; SFC vs. Sham: p < 0.001; Auto vs. Sham: p < 0.001; Fig. 5D). Thus, SFC transplantation contributes to promoting axonal regeneration. However, the NC, SFC, and Auto groups showed less axonal regeneration compared to the Sham group.
Promotion of myelination after transplantation
We performed immunostaining experiments of axially sliced regenerative nerves for NFH and MBP to assess the degree of nerve regeneration. The SFC group displayed sufficient axonal growth and myelination using light microscopy (Fig. 6A,B). The total myelinated area (MBP-positive area) in the SFC groups was larger than that in the NC group (NC: 3,417 ± 870 µm2; SFC: 56,637 ± 8,540 µm2; Auto: 76,222 ± 3,656 µm2; Sham: 153,915 ± 8,774 µm2; NC vs. SFC: p < 0.001; NC vs. Auto: p < 0.001; NC vs. Sham: p < 0.001; SFC vs. Auto: p = 0.15; SFC vs. Sham: p < 0.001; Auto vs. Sham: p < 0.001; Fig. 6C). To assess the histological recovery microscopically, electron microscopic analysis of the regenerated nerve was performed at 12 weeks after the transplantation (Fig. 6D). Numerous myelinated regenerated axons were observed in the SFC group. The G-ratio in the SFC group was lower than that in the Auto group but significantly higher than that in the NC group (NC: 0.684 ± 0.003; SFC: 0.640 ± 0.003; Auto: 0.616 ± 0.003; Sham: 0.560 ± 0.005; NC vs. SFC: p < 0.001; NC vs. Auto: p < 0.001; NC vs. Sham: p < 0.001; SFC vs. Auto: p < 0.001; SFC vs. Sham: p < 0.001; Auto vs. Sham: p < 0.001; Fig. 6E). Next, the G-ratio (Y-axis) was plotted as a function of the axon diameter (X-axis) and fitted with a linear function (Fig. 6F). The lower the slope of the line, the thicker a myelin sheath was obtained on the larger axon; therefore, the SFC group revealed a thicker myelin formation surrounding larger-diameter regenerated axons than the NC group (fitted linear equation: NC, y = 0.050x + 0.462; SFC, y = 0.045x + 0.513; Auto, y = 0.033x + 0.512; Sham, y = 0.032x + 0.385). These data support the conclusion that SFC transplantation markedly promotes myelination compared to the NC group, although it was not as pronounced as in the Auto and Sham groups.
Promotion of myelination after transplantation. Light and electron microscopic observation of central axial sections of regenerated nerves at 12 weeks post transplantation. The SFC group showed a higher degree of myelination than the NC group but not as much as the Auto and Sham groups. (A, B) Representative low- and high-magnification images of the SFC group using light microscopy, showing regenerated nerves, immunostained for NFH and MBP. (C) The total MBP-positive area of the SFC group was greater than that of the NC group. (D) Representative electron microscopic images of the regenerated nerves. (E) Quantitative analysis of myelination. The G-ratio of the SFC group was significantly higher than that of the Auto and Sham groups but lower than that of the NC group. (F) Axon diameter plotted as a function of the G-ratio with fitted linear equations corresponding to each dataset. The SFC group showed a higher degree of thicker myelination around larger-diameter regenerated axons compared to the NC group.
Promotion of vascularization and macrophage-related immune system after transplantation
To clarify the mechanism underlying the promoted nerve regeneration inside the SFC, quantitative analyses of angiogenesis and macrophage recruitment were performed, since both processes play an important role in nerve regeneration42,43,44,45. To evaluate angiogenesis after transplantation, we performed immunostaining with anti-CD31 antibodies. We observed favorable vascularization around the axon in the SFC group (Fig. 7A). The total CD31-positive area in the SFC group was significantly larger than that in the other groups (NC: 393 ± 232 µm2; SFC: 107,223 ± 11,547 µm2; Auto: 47,677 ± 9,851 µm2; Sham: 23,261 ± 1,468 µm2; NC vs. SFC: p < 0.001; NC vs. Auto: p < 0.001; NC vs. Sham: p = 0.12; SFC vs. Auto: p < 0.001; SFC vs. Sham: p < 0.001; Auto vs. Sham: p = 0.18; Fig. 7B), indicating the presence of potent angiogenic effects inside the SFC.
Promotion of vascularization and macrophage-related immune response after transplantation. The SFC group showed a higher degree of vascularization and M2 macrophage recruitment than the other groups. (A) Representative images of the NC, SFC, Auto, and Sham groups observed using light microscopy, showing the area around the regenerated nerves, immunostained for CD31. (B) The total CD31-positive area of the SFC group was greater than that of the other groups, indicating that the SFC promoted vascularization inside the conduit. (C) Representative images of the NC, SFC, Auto, and Sham groups observed using light microscopy, showing the area around and inside the regenerated nerves, immunostained for Iba1 and arginase-1. (D) The total Iba-1 and arginase-1 double-positive area of the SFC group was greater than that of the other groups, indicating that the SFC promoted M2 macrophage recruitment.
To evaluate the extent of macrophage recruitment and polarization, we performed immunostainings with anti-Iba1 and anti-arginase-1 antibodies, respectively. The SFC group exhibited increased macrophage recruitment, including M2 macrophages, around and inside the regenerated nerve (Fig. 7C). The total Iba1 and arginase-1 double-positive area in the SFC group was also significantly larger than that in the other groups (NC: 4,882 ± 1,966 µm2; SFC: 172,69 ± 27,418 µm2; Auto: 69,779 ± 10,605 µm2; Sham: 18,235 ± 1,215 µm2; NC vs. SFC: p < 0.001; NC vs. Auto: p = 0.02; NC vs. Sham: p = 0.92; SFC vs. Auto: p < 0.001; SFC vs. Sham: p < 0.001; Auto vs. Sham: p = 0.08; Fig. 7D). These results indicates that the SFC transplantation facilitated M2 macrophage recruitment and polarization, which contributed to anti-inflammatory tissue regeneration effects43,46,47.
Discussion
Here, we report the physical properties of SFCs, which were fabricated using our freeze–thaw process, including their high hydrophilicity, porosity, and structural stability, with favorable stiffness, toughness, elasticity, and biodegradability. In a rat sciatic-nerve-defect model, SFC transplantation showed favorable therapeutic effects, both functionally and histologically, compared to silicone tube transplantation. The SFC also exerted nerve-regenerative effects comparable to the autologous nerve, except for the extent of innervated muscle restoration and myelination. As no SFCs have been used in clinical settings worldwide6,48, the SFC reported herein may be a promising candidate for peripheral nerve injury.
In-vitro evaluation of the SFC physical properties indicated that it exhibits favorable biocompatibility with high hydrophilicity and porosity. No SF-based conduit prepared using other conventional fabrication methods has shown all these properties. For example, the freeze-drying method, which consists of a freezing phase and a solvent-removal phase17, results in high porosity with a 100-µm-thick reticulated structure. Electrospinning, another method for fabricating nanofibrous scaffolds, also enables microporous and microfibrous architectures with a porosity of about 300 nm, which mimics the cellular microenvironment18,19,20,21,49. However, both methods require drying for fabrication, which could result in a lower water content of the conduit. By contrast, our freeze–thaw process provides a high-water content of > 90% alongside a microporous structure, which could afford high biocompatibility by facilitating the diffusion and permeation of physiologically active substances. Other fabrication methods, devoid of drying processes, have been reported recently50,51; however, since these use harmful chemical additives for cross-linking or stabilization, the biosafety of nerve conduits cannot be guaranteed. Conversely, the SFC in this study was produced using a novel freeze–thaw process, which ensured biosafety by avoiding any harmful chemicals12. The biosafety of the SF sponges was confirmed by evaluating them according to the guidelines of “Basic Principles of Biological Safety Evaluation Required for Application for Approval to Manufacture Medical Devices” in Japan52.
Although higher water content and porosity of a conduit generally lead to lower mechanical stability53,54,55, the SFC maintained structural stability with enhanced stiffness, toughness, and elasticity. While conventional SF materials have been stabilized by inducing β-sheet silk II formation, high β-sheet scaffolds are often too stiff and suboptimal for soft tissue regeneration50. By contrast, our freeze–thaw process formed metastable helix-dominated crystalline structures of silk I more efficiently than those of silk II12,50, which maintained a favorable mechanical balance among stiffness, toughness, and elasticity in the SFC. The calculated stiffness values also indicate that the SFC has mechanical compatibility with living soft tissues—the stiffness of skin and adipose tissue has been reported to be 0.2–5 kPa56—whereas most conventional SF biomaterials have been weak and fragile57. Furthermore, the SFC is degradable under highly concentrated enzyme conditions, which indicates that the SFC could be biodegradable in the long term. These unique properties of the SFC may meet the ideal conditions for an artificial nerve conduit5,6,7,8.
In vivo, the SFC promoted axon elongation and myelination. SF in nature can provide the minimal requirements for cell adhesion, which is essential for cell integration and regeneration58,59,60. Previous studies showed that silk fiber is cytocompatible with Schwann cells without exhibiting cytotoxicity16 and has the potential to differentiate stem cells to acquire neural phenotypes61. In addition to the original SF characteristics, the SFC showed biocompatibility with high hydrophilicity and porosity, which could promote greater cell affinity and rapid exchange of nutrients, growth factors, and metabolized wastes62,63,64,65,66. Additionally, immunostaining experiments of the SFC did not reveal any detrimental fibroblast permeabilization, which may also be advantageous for nerve regeneration67.
The SFC also enhanced vascularization and M2 macrophage recruitment around the regenerated nerve inside the conduit. Although the mechanisms underlying peripheral nerve regeneration have not been fully clarified, vascularization and M2 macrophage recruitment are known to play an important role42,43,44,45,46,47. When nerve injury occurs, macrophages sense hypoxia at the site of nerve defect, which triggers the rearrangement of vascular endothelial cells and promotes angiogenesis68. Schwann cells then migrate along these blood vessels to form Büngner’s bands, which serve as a scaffold for axonal regeneration45. In addition, macrophages promote remyelination by regulating Schwann cell maturation after nerve injury44—they differentiate into anti-inflammatory M2 macrophages and contribute to the resolution of inflammation and healing by inducing revascularization and Schwann cell migration43,69,70. While the SF material itself promotes angiogenesis and macrophage recruitment in nature71,72,73,74, the SFC biocompatibility with high hydrophilicity and porosity may have promoted the vascularization and macrophage recruitment also through M2 macrophage polarization, probably due to the high cell affinity and permeability of neurotrophic and growth factors62,66. In contrast, the autologous nerve contains endogenous factors including Schwann cells75, and the regenerative mechanism in the autologous nerve transplantation is different from that in the SFC transplantation. Therefore, the Auto group may have exhibited lower levels of angiogenesis and M2 macrophage recruitment compared with the SFC group.
The structural stability of the SFC may also have contributed to nerve regeneration. The SFC exhibited favorable compressive stress (stiffness) without any collapse (toughness) and favorable lumen restoration after compression (elasticity). Furthermore, the SFC maintained adequate patency without rapid degradation for three months after transplantation in vivo. Maintaining luminal patency is essential to retain neurotrophic and growth factors inside the conduit and to promote angiogenesis, macrophage migration, axon elongation, and myelination, depending on the regeneration mechanism described above5,6,7,8. Since collapse or kinking of the conduit may compromise nerve regeneration by causing nerve compression and ischemia53, maintaining a hollow SFC structure with stiffness and toughness may have facilitated peripheral nerve regeneration. However, another favorable property of the SFC is its elasticity. While stiff substrates limit nerve outgrowth, soft substrates exhibit positive effects on nerve regeneration76. Elastic conduits are particularly required around joints or fingers77. The SFC has an appropriate balance of stiffness and elasticity, which may be beneficial for nerve regeneration. Furthermore, its resistance to biodegradation may facilitate nerve regeneration. In general, the nerve conduit durability should scale with the duration of nerve regeneration, and its degradation should be slow enough to maintain structural integrity for axonal guidance78,79. The SFC underwent rapid degradation under a highly concentrated enzymatic solution in vitro; however, in vivo, its luminal structure was maintained during nerve regeneration without significant loss of its original structure. In fact, the SFC degradation rate could be slowed down further by adjusting the concentration of the SF aqueous solution to apply it to longer nerve defects80,81,82. Therefore, the SFC can be modulated to be used for transplantations of peripheral nerves with longer deficits.
Currently, the materials used for commercially available artificial nerves are limited to collagen, polyglycolic acid poly-DL-lactide caprolactone, polyvinyl alcohol, chitosan, and submucosal extracellular matrix, with no SF-based artificial nerve conduits having been applied in clinical settings78. However, the unique properties of the SFC may render it advantageous for peripheral nerve regeneration in clinical practice, owing to its easy and cheap purification processes and its large-scale availability owing to its simple fabrication. We conclude that the SFC may be a promising commercially available transplantation material for peripheral nerve injury.
Although our data provide evidence that our artificial nerve is therapeutically effective, some limitations remain. When considering clinical applications, it is necessary to fabricate longer artificial nerve conduits for larger defects, because of the size limitation of the rats used in this study. Future research should experiment with larger animals to verify the therapeutic effects of the SFC and confirm its biosafety in a more reliable manner before conducting clinical trials in patients with peripheral nerve injury.
In conclusion, we developed a bioresorbable SFC, fabricated using a novel freeze-thaw process, which ensures biosafety by avoiding any harmful chemical additives. The SFC exhibited favorable biocompatibility, structural stability, and biodegradability and demonstrated peripheral nerve-regenerative effects in a rat sciatic-nerve-defect model. The unique properties of the SFC further enhanced the peripheral nerve regeneration mechanism, including vascularization, M2 macrophage recruitment, subsequent axonal elongation, and myelination. As no SFC has been applied in clinical practice, the SFC reported herein is a promising candidate for extensive peripheral nerve defects.
Data availability
All data analyzed during this study are available from the corresponding author on reasonable request.
References
Lee, S. K. & Wolfe, S. W. Peripheral nerve injury and repair. J. Am. Acad. Orthop. Surg. 8, 243–252 (2000).
Panagopoulos, G. N., Megaloikonomos, P. D. & Mavrogenis, A. F. The present and future for peripheral nerve regeneration. Orthopedics 40, e141–e156 (2017).
Gu, X., Ding, F., Yang, Y. & Liu, J. Construction of tissue engineered nerve grafts and their application in peripheral nerve regeneration. Prog. Neurobiol. 93, 204–230 (2011).
Grinsell, D. & Keating, C. P. Peripheral nerve reconstruction after injury: a review of clinical and experimental therapies. Biomed Res. Int. 2014, 698256 (2014).
Yi, S., Xu, L. & Gu, X. Scaffolds for peripheral nerve repair and reconstruction. Exp. Neurol. 319, 112761 (2019).
Fornasari, B. E., Carta, G., Gambarotta, G. & Raimondo, S. Natural-based biomaterials for peripheral nerve injury repair. Front. Bioeng. Biotechnol. 8, 554257 (2020).
Vijayavenkataraman, S. Nerve guide conduits for peripheral nerve injury repair: A review on design, materials and fabrication methods. Acta Biomater. 106, 54–69 (2020).
Sanchez Rezza, A., Kulahci, Y., Gorantla, V. S., Zor, F. & Drzeniek, N. M. Implantable biomaterials for peripheral nerve regeneration-technology trends and translational tribulations. Front. Bioeng. Biotechnol. 10, 863969 (2022).
Alarcón Apablaza, J., Lezcano, M. F., Godoy Sánchez, K., Oporto, G. H. & Dias, F. J. Optimal morphometric characteristics of a tubular polymeric scaffold to promote peripheral nerve regeneration: A scoping review. Polymers 14, 397 (2022).
Liu, X. et al. Influence of substratum surface chemistry/energy and topography on the human fetal osteoblastic cell line hFOB 1.19: Phenotypic and genotypic responses observed in vitro. Biomaterials 28, 4535–4550 (2007).
Carvalho, C. R. et al. Tunable enzymatically cross-linked silk fibroin tubular conduits for guided tissue regeneration. Adv. Healthc. Mater. 7, e1800186 (2018).
Tamada, Y. New process to form a silk fibroin porous 3-D structure. Biomacromolecules 6, 3100–3106 (2005).
Magaz, A. et al. Bioactive silk-based nerve guidance conduits for augmenting peripheral nerve repair. Adv. Healthc. Mater. 7, e1800308 (2018).
Nguyen, T. P. et al. Silk fibroin-based biomaterials for biomedical applications: A review. Polymers 11, 1933 (2019).
Cao, Y. & Wang, B. Biodegradation of silk biomaterials. Int. J. Mol. Sci. 10, 1514–1524 (2009).
Yang, Y. et al. Biocompatibility evaluation of silk fibroin with peripheral nerve tissues and cells in vitro. Biomaterials 28, 1643–1652 (2007).
Yang, Y. et al. Development and evaluation of silk fibroin-based nerve grafts used for peripheral nerve regeneration. Biomaterials 28, 5526–5535 (2007).
Park, S. Y. et al. Functional recovery guided by an electrospun silk fibroin conduit after sciatic nerve injury in rats. J. Tissue Eng. Regen. Med. 9, 66–76 (2015).
Belanger, K. et al. A multi-layered nerve guidance conduit design adapted to facilitate surgical implantation. Health Sci. Rep. 1, e86 (2018).
Xue, C. et al. Electrospun silk fibroin-based neural scaffold for bridging a long sciatic nerve gap in dogs. J. Tissue Eng. Regen. Med. 12, e1143–e1153 (2018).
Alessandrino, A. et al. SilkBridge™: A novel biomimetic and biocompatible silk-based nerve conduit. Biomater. Sci. 7, 4112–4130 (2019).
Carvalho, C. R. et al. Engineering silk fibroin-based nerve conduit with neurotrophic factors for proximal protection after peripheral nerve injury. Adv. Healthc. Mater. 10, e2000753 (2021).
Semmler, L. et al. Silk-in-silk nerve guidance conduits enhance regeneration in a rat sciatic nerve injury model. Adv. Healthc. Mater. 12, e2203237 (2023).
Hu, A., Zuo, B., Zhang, F., Zhang, H. & Lan, Q. Evaluation of electronspun silk fibroin-based transplants used for facial nerve repair. Otol. Neurotol. 34, 311–318 (2013).
Ghaznavi, A. M., Kokai, L. E., Lovett, M. L., Kaplan, D. L. & Marra, K. G. Silk fibroin conduits: a cellular and functional assessment of peripheral nerve repair. Ann. Plast. Surg. 66, 273–279 (2011).
Hu, Z. et al. Stability and biodegradation of silk fibroin/hyaluronic acid nerve conduits. Compos. B Eng. 200, 108222 (2020).
Zhang, Q. et al. Preparation of uniaxial multichannel silk fibroin scaffolds for guiding primary neurons. Acta Biomater. 8, 2628–2638 (2012).
Hirakata, E. et al. Early tissue formation on whole-area osteochondral defect of rabbit patella by covering with fibroin sponge. J. Biomed. Mater. Res. B Appl. Biomater. 104, 1474–1482 (2016).
Hashimoto, T., Kojima, K. & Tamada, Y. Gene expression advances skin reconstruction and wound repair better on silk fibroin-based materials than on collagen-based materials. Materialia 9, 100519 (2020).
Varejão, A. S., Melo-Pinto, P., Meek, M. F., Filipe, V. M. & Bulas-Cruz, J. Methods for the experimental functional assessment of rat sciatic nerve regeneration. Neurol. Res. 26, 186–194 (2004).
Honda, K. et al. Intrathecal alpha2 adrenoceptor agonist clonidine inhibits mechanical transmission in mouse spinal cord via activation of muscarinic M1 receptors. Neurosci. Lett. 322, 161–164 (2002).
Chaplan, S. R., Bach, F. W., Pogrel, J. W., Chung, J. M. & Yaksh, T. L. Quantitative assessment of tactile allodynia in the rat paw. J. Neurosci. Methods 53, 55–63 (1994).
Deuis, J. R., Dvorakova, L. S. & Vetter, I. Methods used to evaluate pain behaviors in rodents. Front. Mol. Neurosci. 10, 284 (2017).
Hargreaves, K., Dubner, R., Brown, F., Flores, C. & Joris, J. A new and sensitive method for measuring thermal nociception in cutaneous hyperalgesia. Pain 32, 77–88 (1988).
Jin, J. et al. Functional motor recovery after peripheral nerve repair with an aligned nanofiber tubular conduit in a rat model. Regen. Med. 7, 799–806 (2012).
Shibata, S. et al. Immuno-electron microscopy and electron microscopic in situ hybridization for visualizing piRNA biogenesis bodies in drosophila ovaries. Methods Mol. Biol. 1328, 163–178 (2015).
Orfahli, L. M. et al. Histomorphometry in peripheral nerve regeneration: Comparison of different axon counting methods. J. Surg. Res. 268, 354–362 (2021).
Ando, M. et al. Long-term outcome of sciatic nerve regeneration using Bio3D conduit fabricated from human fibroblasts in a rat sciatic nerve model. Cell Transplant. 30, 9636897211021356 (2021).
Kaiser, T. et al. MyelTracer: A semi-automated software for myelin g-ratio quantification. eNeuro 8, ENEURO.0558–20.2021 (2021).
Ohbayashi, K. et al. Peripheral nerve regeneration in a silicone tube: effect of collagen sponge prosthesis, laminin, and pyrimidine compound administration. Neurol. Med. Chir. (Tokyo) 36, 428–433 (1996).
Takeya, H. et al. Schwann cell-encapsulated chitosan-collagen hydrogel nerve conduit promotes peripheral nerve regeneration in rodent sciatic nerve defect models. Sci. Rep. 13, 11932 (2023).
Brück, W. The role of macrophages in Wallerian degeneration. Brain Pathol. 7, 741–752 (1997).
Mokarram, N., Merchant, A., Mukhatyar, V., Patel, G. & Bellamkonda, R. V. Effect of modulating macrophage phenotype on peripheral nerve repair. Biomaterials 33, 8793–8801 (2012).
Stratton, J. A. et al. Macrophages Regulate Schwann Cell Maturation after Nerve Injury. Cell Rep., Cell Rep. 24 24, 2561–2572.e6 (2018).
Min, Q., Parkinson, D. B. & Dun, X.-P. Migrating Schwann cells direct axon regeneration within the peripheral nerve bridge. Glia 69, 235–254 (2021).
Mantovani, A. et al. The chemokine system in diverse forms of macrophage activation and polarization. Trends Immunol. 25, 677–686 (2004).
Dervan, A. et al. Biomaterial and therapeutic approaches for the manipulation of macrophage phenotype in peripheral and central nerve repair. Pharmaceutics 13, 2161 (2021).
Kehoe, S., Zhang, X. F. & Boyd, D. FDA approved guidance conduits and wraps for peripheral nerve injury: a review of materials and efficacy. Injury 43, 553–572 (2012).
Wang, Y.-L., Gu, X.-M., Kong, Y., Feng, Q.-L. & Yang, Y.-M. Electrospun and woven silk fibroin/poly(lactic-co-glycolic acid) nerve guidance conduits for repairing peripheral nerve injury. Neural Regen. Res. 10, 1635–1642 (2015).
Li, X. et al. Water-stable silk fibroin nerve conduits with tunable degradation prepared by a mild freezing-induced assembly. Polym. Degrad. Stab. 164, 61–68 (2019).
Gu, X. et al. Pure-silk fibroin hydrogel with stable aligned micropattern toward peripheral nerve regeneration. Nanotechnol. Rev. 10, 10–19 (2021).
Tamada, Y., Kobayashi, K. & Sumi, N. Fibroin sponge safety evaluations. Nippon Silk Gakkaishi 23, 71–73 (2015).
Pawelec, K. M., Hix, J., Shapiro, E. M. & Sakamoto, J. The mechanics of scaling-up multichannel scaffold technology for clinical nerve repair. J. Mech. Behav. Biomed. Mater. 91, 247–254 (2019).
Vijayavenkataraman, S. et al. Electrohydrodynamic jet 3D printed nerve guide conduits (NGCs) for peripheral nerve injury repair. Polymers 10, 753 (2018).
Choi, J.-S. et al. Functional regeneration of recurrent laryngeal nerve injury during thyroid surgery using an asymmetrically porous nerve guide conduit in an animal model. Thyroid 24, 52–59 (2014).
Van Damme, L., Blondeel, P. & Van Vlierberghe, S. Injectable biomaterials as minimal invasive strategy towards soft tissue regeneration—an overview. J. Phys. Mater. 4, 022001 (2021).
Kundu, B., Rajkhowa, R., Kundu, S. C. & Wang, X. Silk fibroin biomaterials for tissue regenerations. Adv. Drug Deliv. Rev. 65, 457–470 (2013).
Sun, W. et al. Viability and neuronal differentiation of neural stem cells encapsulated in silk fibroin hydrogel functionalized with an IKVAV peptide. J. Tissue Eng. Regen. Med. 11, 1532–1541 (2017).
Fernández-García, L. et al. Cortical reshaping and functional recovery induced by silk fibroin hydrogels-encapsulated stem cells implanted in stroke animals. Front. Cell. Neurosci. 12, 296 (2018).
Martín-Martín, Y. et al. Evaluation of neurosecretome from mesenchymal stem cells encapsulated in silk fibroin hydrogels. Sci. Rep. 9, 8801 (2019).
Bojnordi, M. N., Ebrahimi-Barough, S., Vojoudi, E. & Hamidabadi, H. G. Silk nanofibrous electrospun scaffold enhances differentiation of embryonic stem like cells derived from testis in to mature neuron. J. Biomed. Mater. Res. A 106, 2662–2669 (2018).
Oh, S. H. et al. Peripheral nerve regeneration within an asymmetrically porous PLGA/pluronic F127 nerve guide conduit. Biomaterials 29, 1601–1609 (2008).
Kim, J. I., Hwang, T. I., Aguilar, L. E., Park, C. H. & Kim, C. S. A controlled design of aligned and random nanofibers for 3D bi-functionalized nerve conduits fabricated via a novel electrospinning set-up. Sci. Rep. 6, 23761 (2016).
Zhang, M., Li, L., An, H., Zhang, P. & Liu, P. Repair of peripheral nerve injury using hydrogels based on self-assembled peptides. Gels 7, 152 (2021).
Gao, C., Song, S., Lv, Y., Huang, J. & Zhang, Z. Recent development of conductive hydrogels for tissue engineering: Review and perspective. Macromol. Biosci. 22, e2200051 (2022).
Qian, Y., Lin, H., Yan, Z., Shi, J. & Fan, C. Functional nanomaterials in peripheral nerve regeneration: Scaffold design, chemical principles and microenvironmental remodeling. Mater. Today 51, 165–187 (2021).
Oh, S. H. et al. Effect of surface pore structure of nerve guide conduit on peripheral nerve regeneration. Tissue Eng. Part C Methods 19, 233–243 (2013).
Cattin, A.-L. et al. Macrophage-induced blood vessels guide Schwann cell-mediated regeneration of peripheral nerves. Cell 162, 1127–1139 (2015).
Negro, S., Pirazzini, M. & Rigoni, M. Models and methods to study Schwann cells. J. Anat. 241, 1235–1258 (2022).
Zhukauskas, R. et al. Histological comparison of porcine small intestine submucosa and bovine type-I collagen conduit for nerve repair in a rat model. J. Hand Surg. Glob. Online 5, 810–817 (2023).
Wang, C. et al. Silk fibroin enhances peripheral nerve regeneration by improving vascularization within nerve conduits. J. Biomed. Mater. Res. A 106, 2070–2077 (2018).
Meinel, L. et al. The inflammatory responses to silk films in vitro and in vivo. Biomaterials 26, 147–155 (2005).
Wang, Y. et al. Effect of electrospun silk fibroin-silk sericin films on macrophage polarization and vascularization. ACS Biomater. Sci. Eng. 6, 3502–3512 (2020).
Gorenkova, N. et al. The innate immune response of self-assembling silk fibroin hydrogels. Biomater. Sci. 9, 7194–7204 (2021).
Jiang, M., Chen, M. & Liu, N. Interactions between Schwann cell and extracellular matrix in peripheral nerve regeneration. Front. Neurol. 15, 1372168 (2024).
Koch, D., Rosoff, W. J., Jiang, J., Geller, H. M. & Urbach, J. S. Strength in the periphery: growth cone biomechanics and substrate rigidity response in peripheral and central nervous system neurons. Biophys. J. 102, 452–460 (2012).
Rasappan, K., Rajaratnam, V. & Wong, Y.-R. Conduit-based nerve repairs provide greater resistance to tension compared with primary repairs: A biomechanical analysis on large animal samples. Plast. Reconstr. Surg. Glob. Open 6, e1981 (2018).
Chrząszcz, P. et al. Application of peripheral nerve conduits in clinical practice: A literature review. Neurol. Neurochir. Pol. 52, 427–435 (2018).
Houshyar, S., Bhattacharyya, A. & Shanks, R. Peripheral nerve conduit: Materials and structures. ACS Chem. Neurosci. 10, 3349–3365 (2019).
Lu, Q. et al. Degradation mechanism and control of silk fibroin. Biomacromolecules 12, 1080–1086 (2011).
Horan, R. L. et al. In vitro degradation of silk fibroin. Biomaterials 26, 3385–3393 (2005).
Wang, Y. et al. In vivo degradation of three-dimensional silk fibroin scaffolds. Biomaterials 29, 3415–3428 (2008).
Acknowledgements
We appreciate the assistance and instructions provided by Drs M. Ozaki, T. Amemiya, R. Shibata, H. Takeya, Y. Kamata, K. Kajikawa, K. Ago, T. Kitagawa, M. Kawai, S. Hashimoto, T. Shibata, Y. Saijo, Y. Suematsu, T. Yoshida, K. Ito, T. Tanaka, A. Toga, R. Ogaki, Y. Ichihara, and T. Shimizu as well as all members in the Department of Orthopaedic Surgery and Physiology, Keio University School of Medicine, Tokyo, Japan. We also appreciate K. Yasutake, M. Akizawa, T. Kobayashi, and T. Harada for their assistance with the experiments and animal care. This work was supported by the Japan Agency for Medical Research and Development (AMED) [grant number JP24ym0126806] and the Japan Society for the Promotion of Science (JSPS) KAKENHI [grant number JP23K15695].
Author information
Authors and Affiliations
Contributions
Conceptualization, T.M., T.I., H.K., M.S., Y.T., and M.N.; Methodology, T.M., T.I., H.K., T.N., M.S., Y.T., and M.N.; Investigation, T.M., S.S., T.S., M.S., S.N., and Y.T.; Resources, T.I., H.K., N.N., M.S., Y.T., and M.N.; Writing—Original Draft, T.M.; Writing—Review & Editing, T.I., H.K., T.N., Y.K., T.S., N.N., S.S., M.S., Y.T., and M.N.; Supervision, T.M., T.I., H.K., N.N., and M.N.; Project Administration, T.M., T.I., H.K., N.N., M.S., and M.N.; Funding Acquisition, T.M., T.I., H.K., T.S., M.S., and Y.T. All authors read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
A patent application is currently pending for the novel silk fibroin conduit (2023–205384), and T.M., T.I., H.K., T.S., M.S., and Y.T. are listed as inventors of the patent. M.S. and Y.M. report financial support from Charlie Lab Inc. Other authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Matsuo, T., Kimura, H., Nishijima, T. et al. Peripheral nerve regeneration using a bioresorbable silk fibroin-based artificial nerve conduit fabricated via a novel freeze–thaw process. Sci Rep 15, 3797 (2025). https://doi.org/10.1038/s41598-025-88221-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-88221-y