Abstract
Although a robust association between metabolic dysfunction-associated fatty liver disease (MASLD) and cardiovascular disease (CVD) has been established, the impact of MASLD on CVD risk in young adults has not been fully evaluated. This population-based study included adults aged 20–39 years who underwent health screening examinations from 2009 to 2012 based on Korean National Health Insurance Service database. MASLD was defined as a fatty liver index ≥ 30 without any other cause of steatosis, and presence of one or more cardiometabolic risk factors. The primary outcome was newly developed CVD, including myocardial infarction, ischemic stroke, and congestive heart failure. During the median 10.6 years of follow-up, MASLD was observed in 1,435,659 (25.3%) of the 5,666,728 participants. Cumulative incidence of major adverse cardiovascular events was significantly higher in individuals with MASLD compared those without steatosis (P < 0.001). The adjusted hazard ratio (HR) for myocardial infarction was 1.23 [95% CI (confidence interval): 1.18–1.27] in individuals with MASLD compared to those without steatosis. The HR for ischemic stroke and congestive heart failure were higher in individuals with MASLD compared to those without steatosis (HR, 1.12; 95% CI, 1.07–1.17 and HR, 1.18; 95% CI, 1.15–1.21, respectively]. In the subgroup analysis, the elevated HR for CVD in the MASLD group was prominent among individuals who were female and obese. MASLD was associated with an increased risk of CVD in young adults. These findings highlight the need for early intervention in patients with MASLD before they reach middle to reduce the risk of CVD, particularly among young adults in South Korea.
Similar content being viewed by others
Background
Among the Korean population, the prevalence of obesity among young adults has increased to 30.4% and 41.4% in those in their 20s and 30s, respectively1. Accordingly, the incidence of cardiovascular disease (CVD) in young adults is also increasing2,3. The global age-standardized incidence rate (per 100,000 population) moderately increased from 126.80 in 1990 to 129.85 in 2019 in youths and young adults aged 15–39 years4. CVD in young adults is associated with an associated deterioration in its prognosis, including reduced life expectancy or quality of life5. Considering the importance of economic activity among young people, the impact of long-term complications, and the serious potential loss of quality of life, it is important to identify risk factors and intervene early to prevent CVD in this population. Onset of cardiovascular risk factors in young age is associated with a higher risk of CVD events6.
A recent multinational consensus introduced metabolic dysfunction-associated steatotic liver disease (MASLD) to more accurately reflect the disease’s underlying pathophysiology7. MASLD was defined as the presence of hepatic steatosis in conjunction with one cardiometabolic risk factor and no other discernible cause. Given that MASLD is closely associated with CVD risk factors, such as obesity, insulin resistance, dyslipidaemia, and hypertension, there is an evident significant association between MASLD and CVD. Recently, Wang et al. has reported that young adults with overweight/obesity-related MASLD have a higher risk of developing coronary artery calcification by middle age8. However, the association between MASLD and CVD in young adults has not yet been fully evaluated. Assessing the association between MASLD and CVD in young adults is important for the early prevention and identification of individuals susceptible to CVD. Thus, we aimed to investigate the association between MASLD and CVD outcomes in young adults in a nationally representative South Korean study population.
Methods
Ethics statement
The study protocol was approved by the Institutional Review Board (IRB) of Seoul National University Hospital (IRB no. 2401-130-1505). This study conformed to the ethical guidelines outlined in the Declaration of Helsinki and its later amendments. The requirement for patient informed consent was waived as the data used in this study were anonymised in accordance with confidentiality guidelines.
Data source
The present study obtained data from the Korean National Health Insurance System (NHIS), as published previously9. The NHIS is a national insurer managed by the South Korean government and covers approximately 97% of the South Korean population. The NHIS database contains health records, including demographic data, anthropometric measurements, laboratory tests, lifestyle behaviours, medical diagnostic codes based on the 10th revision of the International Classification of Diseases (ICD-10), and treatment data.
Study population
We analysed the data of 6,891,401 adults aged 20–39 years who underwent health screening examinations between 2009 and 2012. To focus on the primary disease under the new consensus criteria for MASLD, we excluded individuals with concomitant liver disease, excessive alcohol consumption, or cryptogenic SLD who had a distinct etiological background. Thus, individuals with any other competing liver disease (e.g. hepatocellular carcinoma and liver transplantation, n = 622), excessive alcohol consumption (≥ 30 g for men and ≥ 20 g for women of alcohol/day, n = 647,868), concomitant specific liver disease (n = 184,800, Supplementary Table 1), cryptogenic SLD defined as SLD without cardiometabolic risk factors (n = 7,385), history of myocardial infarction (MI) (ICD-10 code I21, I22, n = 21,333), ischaemic stroke (ICD-10 code I63, I64, n = 12,876) or heart failure (ICD-10 code I50, n = 15,662) before the index year. In addition, those with incomplete information (n = 330,334), and those who were newly diagnosed with primary outcomes or who died within 1 year of the health screening (n = 3,793) were excluded from the study. We ascertained outcome events after a lag of 1 year to avoid the reversal of any causal relationship. As a result, data of 5,666,728 young adults were analysed (Supplementary Fig. 1).
Measurement of hepatic steatosis
Although imaging studies or biopsy results are required to define SLD7, they are not included in the NHIS mass screening program. Therefore, the fatty liver index (FLI), a surrogate marker of hepatic steatosis, was used to define SLD. FLI was calculated based on the following equation, using body mass index (BMI), waist circumference (WC), triglyceride (TG), and gamma-glutamyl transferase (GGT) data10. The lower cutoff of FLI ≥ 30 was used in this study11,12.
FLI = [(e0.953 × ln triglyceride + 0.139 × BMI + 0.718 × ln GGT[gamma−glutamyl transferase] + 0.053 × WC[waist circumference] – 15.745) / (1 + e0.953 × ln triglyceride + 0.139 × BMI + 0.718 × ln GGT + 0.053 × WC – 15.745)] × 100.
Definitions of MASLD
MASLD was defined as the presence of SLD without any other cause of steatosis, along with one or more of the following cardiometabolic criteria: (i) BMI ≥ 23 kg/m2 or WC ≥ 90 cm for men and ≥ 85 cm for women13, (ii) blood pressure ≥ 130/85 mmHg or specific antihypertensive drug treatment, (iii) fasting plasma TG ≥ 150 mg/dL or lipid-lowering treatment, (iv) plasma high-density lipoprotein cholesterol < 40 mg/dL for men and < 50 mg/dL for women or specific drug treatment for high cholesterol, and (v) fasting glucose ≥ 100 mg/dL or type 2 diabetes or treatment for type 2 diabetes7.
Study outcomes
The study endpoint was a composite of newly developed major adverse cardiovascular events (MACE), including MI, ischaemic stroke, and heart failure, during the follow-up period. MI was defined as an in-hospital diagnosis using ICD-10 codes I21–22. Ischaemic stroke was defined as a diagnosis during admission using ICD-10 codes I63–64, with at least one claim for brain imaging studies, including magnetic resonance imaging/angiography or computed tomography14. Congestive heart failure was defined as hospitalization with the ICD-10 code I5015. The study population was followed from baseline to the date of clinical events, death, or until December 31, 2021.
Covariates
A standardised self-administered questionnaire was used to collect data at the time of enrolment, as described previously16. Briefly, smoking status (non-smoker, ex-smoker, or current smoker), alcohol consumption (none or mild [< 30 g for men and < 20 g for women per day]), and physical activity were evaluated. Physical activity was assessed by regular exercise defined as ≥ 5 days of 30-min moderate workouts/week or ≥ 3 days of 20-min intense workouts/week. Comorbidities were defined using ICD-10 diagnosis codes, prescription information in the year prior to the health screening, and health screening results. The criteria for hypertension were I10–13 or I15 claim codes with a prescription of antihypertensive medications or a systolic/diastolic blood pressure reading ≥ 140/90 mmHg. The criteria for diabetes were E11–14 claim codes with a prescription of oral antidiabetic drugs or insulin, or a fasting glucose level ≥ 126 mg/dL. The criterion for dyslipidaemia was the E78 claim code in conjunction with lipid-lowering drugs or a total cholesterol level ≥ 240 mg/dL. The estimated glomerular filtration rate (eGFR) was calculated from serum creatinine levels using an equation derived from the Modification of Diet in Renal Disease Study17.
Statistical analysis
Data were presented as means ± standard deviations for normally distributed continuous variables and as proportions for categorical variables (unless otherwise indicated). Comparisons of baseline characteristics were conducted using analysis of variance for continuous variables and chi-square tests for categorical variables.
Incidence rates of CVD were calculated by dividing the number of incident cases by the total follow-up period and are presented as rates per 1,000 person-years (PY). Hazard ratios (HRs) and 95% confidence interval (CI) values for MI, ischaemic stroke, and heart failure according to MASLD were analysed using Cox proportional hazards models. We selected potential prognostic factors a priori based on their clinical relevance and a comprehensive literature review. These factors included age, sex, household income, BMI, smoking, alcohol consumption, regular exercise, total cholesterol, fasting glucose, systemic blood pressure, and eGFR. Stratified analysis was conducted according to age (20–29 vs. 30–39 years), sex, and obesity (BMI < 25 vs. ≥ 25 kg/m2)13. Statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA). Two-sided P-values of < 0.05 were considered the threshold for statistical significance.
Results
Baseline characteristics
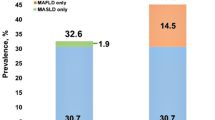
The median follow-up duration was 10.6 (interquartile range, 9.5–11.2) years, and the prevalence of MASLD was 25.3%. The baseline characteristics of individuals according to the presence of MASLD are shown in Table 1. Individuals with MASLD (MASLD group) were older, more likely to be male and current smokers, had higher household income and had higher alcohol consumption and physical activity, compared with those without MASLD (non-MASLD group) (P < 0.001 for all). Additionally, individuals in the MASLD group were more likely to have diabetes, hypertension, and dyslipidaemia than were those in the non-MASLD group (P < 0.001). Most anthropometric and laboratory variables (including BMI, systolic/diastolic blood pressure, fasting glucose, total cholesterol, HDL cholesterol, low-density lipoprotein cholesterol, and TG) were less metabolically favourable in the MASLD group compared with the non-MASLD group (all P < 0.001).
Association of MACE with MASLD
The incidence rates of MACE in young adults were 1.33 and 2.56 per 1,000 PY in the no-MASLD and MASLD groups, respectively. The cumulative crude incidence of MACE was significantly higher in individuals with MASLD compared those without steatosis (P < 0.001, log-rank test) (Fig. 1). In the age- and sex-adjusted model, the HR for MACE was significantly higher in the MASLD group compared to individuals without steatosis (HR, 1.67; 95% CI: 1.65–1.70). In the multivariable-adjusted model, this elevated HR for MACE remained significant (HR, 1.18; 95% CI: 1.16–1.20, Table 2).
Regarding each disease, the HR for MI was 1.23 (95% CI 1.18–1.27) times higher in individuals with MASLD compared to those without steatosis, after multivariable adjustment. Additionally, the HR for ischemic stroke and heart failure were elevated in the MASLD group compared to individuals without steatosis (HR, 1.12; 95% CI, 1.07–1.17 and HR, 1.18; 95% CI, 1.15–1.21, respectively, Fig. 2).
Hazard ratio (95% confidence interval) for cardiovascular event according to MASLD. Adjusted for age, sex, household income, body mass index, smoking, alcohol consumption, regular exercise, total cholesterol, fasting glucose, systolic blood pressure, and estimated glomerular filtration rate. MASLD, metabolic dysfunction-associated steatotic liver disease.
Stratified analysis
We further performed subgroup analyses stratified by age group, sex, and BMI. The increased HR for MACE in the MASLD group was particularly prominent in individuals who were female, and BMI ≥ 25 kg/m2 (P for interaction < 0.05, Fig. 3). Women with MASLD showed higher relative risks for MACE, ischemic stroke, and heart failure versus men, although their risk of MI was slightly lower than that of men. Additionally, individuals with a higher BMI (≥ 25 kg/m2) and MASLD generally exhibited a greater risk for overall cardiovascular events (Table 3).
The association between MASLD and major adverse cardiovascular events in different subgroups: age < 30 vs. ≥30 years; male vs. female; non-obese (BMI < 25) vs. obese (BMI ≥ 25). MASLD, metabolic dysfunction-associated steatotic liver disease; HR, hazard ratio; CI, confidence interval; BMI, body mass index.
Discussion
In this large nationwide population-based cohort study, we demonstrated an association between MASLD and cardiovascular outcomes among young adults using a database of health insurance claims in Korea. The HR of MACE increased significantly in young adults with MASLD compared with those without hepatic steatosis, independent of traditional cardiovascular risk factors. This significant association of MASLD with the risk of CVD remained consistent across different types of MACE, including MI, ischaemic stroke, and heart failure.
The close association between MASLD and CVD outcomes has been previously investigated. A recent study by Lee et al. reported that the cumulative incidence of CVD events, including MI, heart failure, or cardiovascular death, was higher in participants with MASLD than in those without the condition, during a median follow-up of 12.3 years. After multivariable adjustment, the risk of CVD was 1.39 (95% CI 1.38–1.40) times higher in participants with MASLD and associated SLD than in those without the condition18. Another study showed that the risk of MI and stroke was higher among patients with MASLD than among non-MASLD patients (HR, 1.19; 95% CI: 1.15–1.24)19. However, these studies primarily evaluated cohorts with middle-aged individuals and did not focus on younger populations.
This study evaluated the association between MASLD and CVD outcomes in young adults and showed that the incidence of MACE increased significantly in young adults with MASLD compared with those without hepatic steatosis. Our findings are consistent with those of a previous study conducted in China, which reported a significant association between metabolic dysfunction-associated fatty liver disease and heart failure in participants aged < 45 years20. In addition, Swedish children and young adults aged ≤ 25 years with histologically confirmed NAFLD had significantly higher rates of incident MACE, including ischemic heart disease and congestive heart failure, compared with a matched control population21. These findings highlight the importance of early detection and management of CVD risk in young patients with MASLD.
Although the exact pathogenesis of the increased risk of CVD in young adults with MASLD remains unclear, it is believed that increased systemic inflammation, increased sympathetic activity, oxidative stress, and endothelial dysfunction leading to earlier atherosclerosis may contribute to CVD development22. Additionally, the local necro-inflammatory changes of steatohepatitis may exacerbate systemic metabolic inflammation, and concurrent fibrogenesis in both the liver and the myocardium could further contribute to CVD progression23.
When stratified by age, sex, and BMI, the increased HR of MACE in individuals with MASLD was prominent in those who were aged > 30 years, female, and BMI ≥ 25 kg/m2. This increased risk across age groups may be attributed to the cumulative effect of cardiovascular risk factors and the progressive nature of metabolic dysfunction. Moreover, the increased HR of MACE among individuals with obesity reflects the well-established association between obesity and cardiovascular risk factors. Notably, women with MASLD exhibited higher relative risks of MACE, ischemic stroke, and heart failure despite showing a slightly lower risk of MI, compared with men. This observation is consistent with a prior study showing that women with nonalcoholic fatty liver disease (NAFLD) had more CVD events (18% vs. 9%) and mortality (9% vs. 6%) than did men with the same condition24. Furthermore, a recent study reported a higher risk of cardiovascular mortality among young and middle-aged (≤ 60 years) women with NAFLD, compared with their male counterparts25. Additionally, traditional metabolic risk factors, such as type 2 diabetes26, hypertension, and dyslipidemia27, have a stronger effect on CVD risk in women than in men. Unlike the cardiovascular protection conferred by the female sex in the general population28, women with MASLD may lose this advantage owing to their high metabolic burden. Conversely, men tend to engage in more unhealthy lifestyles, including smoking, alcohol consumption, and a high-calorie diet, which are known to contribute to increased CVD morbidity and mortality29, and these factors may obscure the association between conventional metabolic risk factors and incident CVD in men30.
Our study has three major clinical implications. First, identifying MASLD in young patients allows for early detection and intervention, which can help prevent the progression of CVD-related complications later in life. Second, the effective management of MASLD in young patients can improve their quality of life by reducing the risk of CVD complications, improving metabolic health, and potentially preventing other chronic diseases associated with MASLD. Third, given the rising global prevalence of MASLD, addressing the disease in young patients is essential to reduce the overall burden on healthcare systems and improve long-term health outcomes.
However, we acknowledge some limitations of the present work. First, although histological or radiological methods are more accurate for detecting hepatic steatosis than non-invasive biomarkers, we used FLI as a surrogate marker of fatty liver and, thus, did not accurately quantify liver steatosis31. However, the use of FLI has been acknowledged in epidemiologic studies32. Second, because the Korean NHIS database does not include information regarding platelet count or albumin level, we could not assess the degree of liver fibrosis such as the Fibrosis-4 index. Further studies are needed to evaluate the impact of liver fibrosis on CVD risk in MASLD. Third, because of its population-based observational design, our study could not establish a causal relationship, and there might be residual confounding factors. Fourth, to focus on major diseases in the new consensus criteria for MASLD, we excluded individuals with concomitant liver disease, excessive alcohol use, or cryptogenic SLD with distinct etiological backgrounds. Therefore, we could not assess the differential prognosis of the different SLD subgroups. Fifth, it is possible that the evaluated conditions were over- or underestimated because the diagnoses were based on claims data (ICD-10 codes). That is, if the patient does not list all diagnoses in the clinical presentation, but only the main diagnosis. Further research is warranted to validate and elucidate the mechanisms underlying our results. Finally, because we could not assess regional or racial/ethnic diversity, the findings may not generalize to non-Korean populations or regions with different socioeconomic or genetic factors influencing MASLD and CVD risk.
In conclusion, this study demonstrated that MASLD is associated with MACE in young adults, attributable to metabolic dysfunction. These findings underscore the necessity for early intervention in individuals with MASLD prior to reaching middle age to mitigate the risk of CVD.
Data availability
The dataset (NHIS-HEALS) supporting the conclusions of this article is available in the homepage of National Health Insurance Sharing Service [http://nhiss.nhis.or.kr/bd/ab/bdaba021eng.do]. To gain access to the data, a completed application form, a research proposal and the applicant’s approval document from the institutional review board should be submitted to and reviewed by the inquiry committee of research support in NHIS. Currently, use of NHIS data is allowed only for Korean researchers.
Abbreviations
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- CVD:
-
Cardiovascular disease
- eGFR:
-
Estimated glomerular filtration rate
- FLI:
-
Fatty liver index
- HR:
-
Hazard ratio
- ICD-10:
-
International Classification of Diseases,10th revision
- MACE:
-
Major adverse cardiovascular events
- MASLD:
-
Metabolic dysfunction-associated steatotic liver disease
- MI:
-
Myocardial infarction
- NAFLD:
-
Nonalcoholic fatty liver disease
- NHIS:
-
Korean National Health Insurance System
- PY:
-
Person-year
- TG:
-
Triglyceride
- WC:
-
Waist circumference
References
Jeong, S. M. et al. 2023 obesity fact sheet: prevalence of obesity and abdominal obesity in adults, adolescents, and children in Korea from 2012 to 2021. J. Obes. Metab. Syndr. Mar. 30 (1), 27–35. https://doi.org/10.7570/jomes24012 (2024).
George, M. G., Tong, X. & Bowman, B. A. Prevalence of Cardiovascular Risk factors and strokes in younger adults. JAMA Neurol. Jun. 1 (6), 695–703. https://doi.org/10.1001/jamaneurol.2017.0020 (2017).
Arora, S. et al. Twenty Year trends and Sex differences in young adults hospitalized with Acute myocardial infarction. Circulation Feb. 19 (8), 1047–1056. https://doi.org/10.1161/circulationaha.118.037137 (2019).
Sun, J., Qiao, Y., Zhao, M., Magnussen, C. G. & Xi, B. Global, regional, and national burden of cardiovascular diseases in youths and young adults aged 15–39 years in 204 countries/territories, 1990–2019: a systematic analysis of global burden of Disease Study 2019. BMC Med. Jun. 26 (1), 222. https://doi.org/10.1186/s12916-023-02925-4 (2023).
Roth, G. A. et al. Global Burden of Cardiovascular diseases and Risk factors, 1990–2019: Update from the GBD 2019 study. J. Am. Coll. Cardiol. Dec. 22 (25), 2982–3021. https://doi.org/10.1016/j.jacc.2020.11.010 (2020).
Lloyd-Jones, D. M. et al. The coronary artery risk development in young adults (CARDIA) study: JACC Focus Seminar 8/8. J. Am. Coll. Cardiol. Jul 20 (3), 260–277. https://doi.org/10.1016/j.jacc.2021.05.022 (2021).
Rinella, M. E. et al. A multi-society Delphi consensus statement on new fatty liver disease nomenclature. J. Hepatol. Jun. 20 https://doi.org/10.1016/j.jhep.2023.06.003 (2023).
Wang, J. J., Zheng, Z. & Zhang, Y. Association of overweight/obesity and overweight/obesity-related metabolic dysfunction-associated steatotic liver disease in young adults with coronary artery calcification later in life. Diabetes Obes. Metab. Sep. 26 (9), 3860–3867. https://doi.org/10.1111/dom.15733 (2024).
Lee, H., Rhee, T. M., Park, H. E., Han, K. & Choi, S. Y. Association between cumulative metabolic risk exposure and Cardiovascular Disease: a nationwide cohort of over 3.6 million young adults. Eur. J. Prev. Cardiol. Feb. 29 https://doi.org/10.1093/eurjpc/zwae088 (2024).
Bedogni, G. et al. The fatty liver index: a simple and accurate predictor of hepatic steatosis in the general population. BMC Gastroenterol. Nov 2. 6, 33. https://doi.org/10.1186/1471-230X-6-33 (2006).
Chung, G. E. et al. Differential risk of 23 site-specific incident cancers and cancer-related mortality among patients with metabolic dysfunction-associated fatty liver disease: a population-based cohort study with 9.7 million Korean subjects. Cancer Commun. (Lond) Aug. 43 (8), 863–876. https://doi.org/10.1002/cac2.12454 (2023).
Cho, E. J. et al. Fatty Liver Index for Predicting nonalcoholic fatty liver disease in an asymptomatic Korean Population. Diagnostics (Basel) Nov. 29 (12). https://doi.org/10.3390/diagnostics11122233 (2021).
Haam, J. H. et al. Diagnosis of obesity: 2022 update of clinical practice guidelines for obesity by the Korean Society for the Study of Obesity. J. Obes. Metab. Syndr. Jun. 30 (2), 121–129. https://doi.org/10.7570/jomes23031 (2023).
Kim, M. K. et al. Cholesterol variability and the risk of mortality, myocardial infarction, and stroke: a nationwide population-based study. Eur. Heart J. Dec. 21 (48), 3560–3566. https://doi.org/10.1093/eurheartj/ehx585 (2017).
Park, J. et al. The associations of hepatic steatosis and fibrosis using fatty liver index and BARD score with cardiovascular outcomes and mortality in patients with new-onset type 2 diabetes: a nationwide cohort study. Cardiovasc. Diabetol. Apr. 16 (1), 53. https://doi.org/10.1186/s12933-022-01483-y (2022).
Cho, E. J. et al. The association between alcohol consumption and the risk of hepatocellular carcinoma according to glycemic status in Korea: a nationwide population-based study. PLoS Med. Jun. 20 (6), e1004244. https://doi.org/10.1371/journal.pmed.1004244 (2023).
Levey, A. S. et al. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann. Intern. Med. Aug. 15 (4), 247–254. https://doi.org/10.7326/0003-4819-145-4-200608150-00004 (2006).
Lee, H. H. et al. Metabolic dysfunction-associated steatotic liver disease and risk of cardiovascular disease. Gut Feb. 23 (3), 533–540. https://doi.org/10.1136/gutjnl-2023-331003 (2024).
Moon, J. H., Jeong, S., Jang, H., Koo, B. K. & Kim, W. Metabolic dysfunction-associated steatotic liver disease increases the risk of incident cardiovascular disease: a nationwide cohort study. EClinicalMedicine Nov. 65, 102292. https://doi.org/10.1016/j.eclinm.2023.102292 (2023).
Wu, S. et al. Sex and age differences in the Association between Metabolic Dysfunction-Associated fatty liver disease and heart failure: a prospective cohort study. Circ. Heart Fail. Feb. 17 (2), e010841. https://doi.org/10.1161/circheartfailure.123.010841 (2024).
Simon, T. G. et al. Cardiovascular disease risk in paediatric and young adult non-alcoholic fatty liver disease. Gut Mar. 72 (3), 573–580. https://doi.org/10.1136/gutjnl-2022-328105 (2023).
Gulati, R. et al. Jan. Acute Myocardial Infarction in Young Individuals. Mayo Clin Proc. ;95(1):136–156. (2020). https://doi.org/10.1016/j.mayocp.2019.05.001
Armandi, A. & Bugianesi, E. Extrahepatic outcomes of nonalcoholic fatty liver disease: Cardiovascular diseases. Clin. Liver Dis. May. 27 (2), 239–250. https://doi.org/10.1016/j.cld.2023.01.018 (2023).
Allen, A. M. et al. Women with nonalcoholic fatty liver Disease Lose Protection against Cardiovascular Disease: a longitudinal cohort study. Am. J. Gastroenterol. Nov. 114 (11), 1764–1771. https://doi.org/10.14309/ajg.0000000000000401 (2019).
Ren, R. & Zheng, Y. Sex differences in cardiovascular and all-cause mortality in nonalcoholic fatty liver disease in the US population. Nutr. Metab. Cardiovasc. Dis. Jul. 33 (7), 1349–1357. https://doi.org/10.1016/j.numecd.2023.03.003 (2023).
Juutilainen, A. et al. Gender difference in the impact of type 2 diabetes on coronary heart disease risk. Diabetes Care Dec. 27 (12), 2898–2904. https://doi.org/10.2337/diacare.27.12.2898 (2004).
Bai, X. et al. Gender differences in risk factors for ischemic stroke: a longitudinal cohort study in East China. BMC Neurol. May. 23 (1), 171. https://doi.org/10.1186/s12883-024-03678-0 (2024).
Iorga, A. et al. The protective role of estrogen and estrogen receptors in cardiovascular disease and the controversial use of estrogen therapy. Biol. Sex. Differ. Oct. 24 (1), 33. https://doi.org/10.1186/s13293-017-0152-8 (2017).
Meloni, A. et al. Gender differences and cardiometabolic risk: the importance of the risk factors. Int. J. Mol. Sci. Jan. 13 (2). https://doi.org/10.3390/ijms24021588 (2023).
Garcia, M., Mulvagh, S. L., Merz, C. N., Buring, J. E. & Manson, J. E. Cardiovascular Disease in women: clinical perspectives. Circ. Res. Apr. 15 (8), 1273–1293. https://doi.org/10.1161/circresaha.116.307547 (2016).
Fedchuk, L. et al. Performance and limitations of steatosis biomarkers in patients with nonalcoholic fatty liver disease. Aliment. Pharmacol. Ther. Nov. 40 (10), 1209–1222. https://doi.org/10.1111/apt.12963 (2014).
Kim, K. S., Hong, S., Han, K. & Park, C. Y. Association of non-alcoholic fatty liver disease with cardiovascular disease and all cause death in patients with type 2 diabetes mellitus: nationwide population based study. Bmj Feb 13. 384, e076388. https://doi.org/10.1136/bmj-2023-076388 (2024).
Funding
This work was supported by the Korea Medical Device Development Fund grant funded by the Korea government (the Ministry of Science and ICT, the Ministry of Trade, Industry and Energy, the Ministry of Health & Welfare, the Ministry of Food and Drug Safety) (NTIS, KMDF-RnD 1711196788).
Author information
Authors and Affiliations
Contributions
The corresponding authors (Eun Ju Cho and Kyungdo Han) had full access to all study data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Eun Ju Cho and Kyungdo Han. Provision of study materials or patients: Goh Eun Chung, Su Jong Yu, Jeong-Ju Yoo, Yuri Cho. Collection and management of the study data: Kyu Na Lee, Yuri Cho, Jeong-Ju Yoo, Dong Wook Shin. Data analysis and interpretation: Goh Eun Chung, Su Jong Yu, Yuri Cho, Kyu Na Lee, Dong Wook Shin. Manuscript writing: Eun Ju Cho, Goh Eun Chung, Su Jong Yu, Kyungdo Han. Revision and final approval of the manuscript: all authors.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent to participate
The study protocol was approved by the Institutional Review Board (IRB) of Seoul National University Hospital (IRB no. 2401-130-1505). This study conformed to the ethical guidelines outlined in the Declaration of Helsinki and its later amendments. The requirement for patient informed consent was waived as the data used in this study were anonymised in accordance with confidentiality guidelines.
Consent to Publish
All the authors consented to publish work.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chung, G.E., Yu, S.J., Yoo, JJ. et al. Metabolic dysfunction-associated steatotic liver disease increases cardiovascular disease risk in young adults. Sci Rep 15, 5777 (2025). https://doi.org/10.1038/s41598-025-89293-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-89293-6
Keywords
This article is cited by
-
Decoding survival in MASLD: the dominant role of metabolic factors
Diabetology & Metabolic Syndrome (2025)
-
Epidemiological trends and burden of metabolic dysfunction-associated steatotic liver disease in the Middle East and North Africa region: a 32-year analysis of health impact
Journal of Health, Population and Nutrition (2025)