Abstract
Background: Breast cancer is a major global health burden, with hereditary factors such as BRCA1/2 mutations significantly increasing the lifetime risk. This meta-analysis aimed to evaluate the outcomes of selective estrogen receptor modulators (SERMs), tamoxifen, and raloxifene as chemopreventive agents for breast cancer risk reduction in BRCA1/2 mutation carriers. Methods: A meta-analysis was conducted according to the PRISMA guidelines. PubMed, Cochrane Library, and MEDLINE databases were searched for relevant studies published between 2000 and 2024. Case-control studies and observational cohort studies examining the use of tamoxifen/raloxifene in BRCA1/2 carriers were included. Data on the incidence and risk ratios of breast cancer were also extracted. Quality was assessed using the Newcastle-Ottawa Scale (NOS). A random-effects meta-analysis was performed using Review Manager (version 5.4.0). Results: Nine studies (13,676 women) were included. Two studies had low risk, and the remaining seven studies had moderate risk, as assessed by the NOS checklist. Pooled analysis showed tamoxifen/raloxifene decreased breast cancer risk compared to controls (RR 0.80, 95% CI 0.72–0.88, p = 0.04). The risk ratio of breast cancer incidence among BRCA1/2 carriers was reduced after tamoxifen use (RR 1.82, 95% CI 1.48–2.23, p < 0.00001). Subgroup analysis revealed reduced breast cancer risk with SERM use in both BRCA1 (RR 1.51, 95% CI 1.48–1.51) and BRCA2 carriers (RR 1.48, 95% CI 1.40–1.58). The heterogeneity ranged from 51 to 85%, representing high significance and variation in true effect sizes underlying the different included studies. Whereas the heterogeneity among subgroups BRCA1 and BRCA2 was 98%, and the difference was 0%, showing no difference in response to SERM for risk reduction of breast cancer. Conclusion: This meta-analysis provides evidence that tamoxifen and raloxifene significantly reduce the breast cancer risk in women with BRCA1/2 mutations. Chemoprevention efficacy was similar for both BRCA1 and BRCA2 carriers. Further research is needed to validate these findings and to optimize their use in high-risk populations.
Similar content being viewed by others
Introduction
Breast cancer is the most frequent malignancy among women and is a major global burden on the healthcare system1. Approximately 2.3 million new cases and 685,000 deaths due to breast cancer were reported in women in 20202. Hereditary factors play a significant role in the development of breast cancer among women. Some of these genetic predispositions pose a significant lifetime risk of breast cancer3. Among these mutations, BRCA1 and BRCA2 are the most well-known and can lead to breast cancer4,5. The lifetime risk of breast cancer among women who carry the BRCA1 mutation is 45–85%, and the BRCA2 mutation is 40–70%, depending on various environmental as well as genetic factors6,7. The increasing incidence of these genetic mutations (especially BRCA mutations) in the general population, which occurs in 2.5 out of 1000 individuals, emphasizes the need for emergent cancer prevention strategies8. Among these preventive strategies, chemoprevention is an effective method that involves the use of medications for risk reduction in women carrying BRCA mutations9,10. Various chemoprevention therapies are used to reduce breast cancer risk, including aromatase inhibitors (anastrozole and exemestane) and selective estrogen receptor modulators (SERMs) (tamoxifen and raloxifene)11,12. In this study, our key emphasis was on SERMs as a chemopreventive strategy for breast cancer risk reduction.
Two major SERMs, tamoxifen and raloxifene, have long been examined for their role in breast cancer prevention. Both drugs play a pathogenic role by blocking the proliferative effects of estrogen in breast tissue, thus reducing the probability of pathogenesis in hormone receptor-positive breast cancers11,13,14. Among the general population at high risk of breast cancer, tamoxifen has been reported as an effective chemopreventive agent in clinical trials, such as the NSABP P-1 study15,16. Raloxifene is another SERM agent that reduces breast cancer risk; however, it is the least used medication owing to its development for the prevention and treatment of osteoporosis17,18,19.
The use of chemopreventive agents poses a significant challenge for BRCA mutation carriers. In breast cancer prevention, adherence to chemopreventive strategies may be disturbed due to the adverse effects of aromatase inhibitors (AIs) and selective estrogen receptor modulators (SERMs), which lead to high risks of osteoporosis and thromboembolism among patients. Since BRCA-carrier women who are BRCA carriers are at a higher risk of developing breast cancer than the general population. Therefore, SERMs agents such as tamoxifen and raloxifene are effective because of their preventive outcomes. Few previous cohorts and randomized controlled trials (RCTs) have reported the effectiveness of these SERMs among BRCA1 and BRCA2 mutation carrier populations for risk reduction of breast cancer20,21,22. Tamoxifen and Raloxifene inhibit the formation of tumors stimulated by estrogen by blocking estrogen receptors in the breast tissue. In comparison to tamoxifen, raloxifene decreased the risk of advanced breast cancer by 44–49% in the MORE and STAR trials. It also has fewer adverse effects such as a lower risk of endometrial cancer23,24. However, there is a lack of comprehensive analysis on the effectiveness of tamoxifen or raloxifene in reducing breast cancer risk among women who are BRCA1 and BRCA2 mutation carriers. Therefore, this meta-analysis aimed to evaluate the efficacy of tamoxifen and raloxifene as chemopreventive agents for breast cancer risk reduction among BRCA1 and BRCA2 mutation carriers, focusing on both their potential benefits and associated risks. This study aimed to provide a thorough summary of the role of these drugs in the treatment of women with a high genetic risk of breast cancer by analyzing data from studies published between 2000 and 2024.
Methods
Study design
The “Reporting Items for Systematic Review and Meta-Analysis (PRISMA)” guidelines25 were followed for conducting a recent systematic review and meta-analysis to fulfill research aims of evaluating the risk-benefits of tamoxifen or raloxifene as chemoprevention for risk reduction of breast cancer in women who carry BRCA1 or BRCA2 mutations26. Our study is a meta-analysis of previously published case-control and observational studies; therefore, there is no need for an additional ethical review.
Search strategy
A comprehensive literature search was conducted using various electronic databases, including PubMed, Cochrane Library, and MEDLINE, to extract and identify related studies published between 2000 and 2024. The relevant research articles were extracted by using MeSH keywords such as (“risk-benefits” OR “risk prevention” OR “risk reduction” OR “risk assessment”) AND (“Breast neoplasm” OR “Breast cancer” OR “chemoprevention”) AND (“Genetic Predisposition” OR “BRCA1 Gene” OR “BRCA2 Gene”) AND (Tamoxifen OR Raloxifene). Previous meta-analyses and reviews were manually searched to extract and identify additional studies from reference lists.
Eligibility criteria
The eligibility criteria assisted in the selection and screening of research articles after searching electronic databases. Only studies that met the following inclusion criteria were included: 1). Studies have investigated women carrying BRCA1 and BRCA2, 2). Studies have analyzed the female population receiving chemoprevention with tamoxifen or raloxifene 3). Studies involving the incidence of breast cancer and the associated hazard ratio (HR) or relative risk (RR) among tamoxifen or raloxifene users and non-users 4). Case control and observational cohort studies 5). Studies published in English and in full text are available.
However, these studies were excluded 1). The study population consisted of women who were ER-positive or carried risk genes for other cancer types, 2). Studies involving other drugs for the chemoprevention of breast cancer, rather than tamoxifen or raloxifene 3). Studies have discussed other outcomes such as the incidence of prophylactic bilateral mastectomy 4). Studies based on systematic reviews, meta-analyses, comprehensive reviews, narrative reviews, or editorials were excluded. 5). Studies published in languages other than English, and non-full-text papers were excluded.
Data extraction
Two independent reviewers extracted the data using a prespecified table. Data related to demographic information such as authors, year of study, country, study population, sample size, study design, and study follow-up were extracted (Table 1). Information related to primary outcomes, such as the incidence of breast cancer, hazard ratio of breast cancer, and incidence of breast cancer among BRCA1 and BRCA2 carrier women, is shown in Table 2. Discrepancies were resolved by consulting with a third reviewer. The extracted data included the following.
Quality assessment
The Newcastle-Ottawa Scale (NOS) was used to assess the quality of the case-control and cohort studies27. A score of > 7 for included studies was considered low-risk, a score of 5–7 for included studies indicated moderate-risk, and a score of < 5 for included studies indicated high-risk. Any disagreement regarding risk bias assessment was resolved through consensus.
Statistical analysis
All statistical analyses were conducted using Review Manager Software (Cochrane Collaboration, version 5.4.0)28. Statistical significance was set at P < 0.05. Pooled analysis of data was performed for studies with potential heterogeneity using random effects models. Effect sizes are shown as risk ratios (RR) for dichotomous outcomes (e.g., breast cancer incidence). Heterogeneity was evaluated using the I2 statistic, I2 values > 50% indicating significant heterogeneity. Subgroup analyses were conducted according to variables, such as tamoxifen versus non-users and BRCA1 versus BRCA2 mutation carriers.
Results
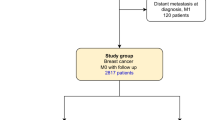
In this study, research articles were selected and screened according to the study aims and title “Risk-benefits assessment of tamoxifen or raloxifene as chemoprevention for risk reduction of breast cancer among BRCA1 and BRCA2 carriers” according to the PRISMA guidelines26. A total of 6,280 research articles were obtained from the above-mentioned electronic databases by using “MeSH” keywords and 4180 duplicates were removed. In accordance with the PRISMA guidelines, only 1509 papers were retrieved after excluding 591 research articles. Among them, only 807 met the eligibility criteria. Only nine studies met the inclusion criteria and were included in this study, as shown in Fig. 1.
Characteristics of included studies
Our study analyzed nine research articles (four prospective cohort studies and five case-control studies) and a total of 13,676 women who carried either BRCA1 or BRCA2 to evaluate the benefits of tamoxifen or raloxifene as chemoprevention for risk reduction of breast cancer using a meta-analysis approach. The main characteristics of the selected studies are presented in Table 1. All the included studies were published between 2000 and 2024. The sample size for some included studies was limited due to the involvement of case-control studies, ranging from 19 to 1504 BRCA1 and BRCA2 female carriers29,30,31,32,33 while the sample size of cohort studies ranged from 432 to 4578 risk carrier women34,35,36,37. The follow-up periods in the included studies ranged from 1 to 10 years.
Quality assessment
Among the nine included studies, two were at low risk30,33 and the remaining seven were at moderate risk29,31,32,34,35,36,37, as shown in Table 3. Most comparisons showed low to moderate evidence quality, and the study’s limitations, inconsistencies, indirectness, and imprecision were the key reasons for the decline in confidence.
Primary outcomes
A. Incidence of breast cancer
All nine included studies reported the incidence of breast cancer among BRCA1/2 carrier women receiving tamoxifen or raloxifene compared to the general population (non-users). The pooled analysis showed that administration of tamoxifen or raloxifene decreased the breast cancer risk as compared to control [RR: 0.80 (95%CI; 0.72 to 0.88], p = 0.04) and heterogeneity reported (I2 = 51%), as shown in Fig. 2. The symmetrical distribution of the risk ratios of the included studies revealed the absence of publication bias (Fig. 3).
B. Risk of breast cancer
Among the nine included studies, six reported the risk ratio of breast cancer among BRCA1/2 carriers receiving tamoxifen or raloxifene. The pooled risk ratio of breast cancer incidence was higher in BRCA1/2 carriers [RR: 1.82 (95% CI; 1.48 to 2.23), p < 0.00001) and heterogeneity reported (I2 = 85%), as shown in Fig. 4. This indicates that tamoxifen use can significantly reduce the risk of breast cancer among BRCA1/2 carriers. The symmetrical distribution of the risk ratios of the included studies revealed the absence of publication bias (Fig. 5).
C. Subgroup analysis for BRCA1 and BRCA2 mutation carriers
Five studies demonstrated the risk ratio of breast cancer incidence among BRCA1 (subgroup 1) and BRCA2 carriers receiving tamoxifen or raloxifene compared with the control rate. A meta-analysis showed that treatment with tamoxifen or raloxifene had reduced the risk of breast cancer incidence (RR = 1.51, 95% CI = 1.48 to 1.54, P < 0.00001) among both subgroups: BRCA1 [RR: 1.51; 1.48 to 1.51] and BRCA2 [RR: 1.48; 1.40 to 1.58], and heterogeneity reported (I2 = 98%), as shown in Figs. 6 and 7.
Discussion
This study aimed to evaluate the risk benefits of tamoxifen or raloxifene as a chemoprevention for breast cancer risk reduction among BRCA1 and BRCA2 carriers by adopting a meta-analysis approach. Through the analysis of nine research articles (four prospective cohort studies and five case-control studies) and 13676 women who carried either BRCA1 or BRCA2, this study reported that tamoxifen or raloxifene as chemoprevention strategies reduced breast cancer risk among BRCA1 and BRCA2 carriers. The primary outcomes of this study were the incidence of breast cancer risk and the risk ratio of breast cancer among BRCA1/2 carrier women receiving tamoxifen or raloxifene compared to controls. The pooled analysis showed that administration of tamoxifen or raloxifene decreased the breast cancer risk [RR: 0.80 (95%CI: 0.72 to 0.88], p = 0.04) and risk ratio of breast cancer incidence among BRCA1/2 carriers after tamoxifen use [RR: 1.82 (95% CI: 1.48 to 2.23], p < 0.00001). The findings of subgroup analysis reported that treatment by tamoxifen or raloxifene had reduced the risk of breast cancer incidence (RR = 1.51, 95% CI = 1.48 to 1.54, P < 0.00001) among both subgroups; BRCA1 [RR: 1.51; (95% CI; 1.48 to 1.51)] and BRCA2 [RR: 1.48 (95% CI: 1.40 to 1.58)]. Among the nine included studies, two were at low risk30,33, and the remaining seven were at moderate risk29,31,32,34,35,36,37, as assessed by NOS.
The findings of this study are consistent with those of previous studies that have demonstrated tamoxifen as an effective chemopreventive strategy for breast cancer in women with BRCA1 and BRCA2 genetic mutations. However, raloxifene, unlike tamoxifen has originally been used for the prevention of osteoporosis in postmenopausal women18,38. Thus, few cohort or case-control studies have reported the outcomes of raloxifene in breast cancer risk reduction among BRCA1 and BRCA2 carrier women39,40. Collectively, the findings of this meta-analysis support the use of SERMs among high-risk populations, especially BRCA1 and BRCA2 carriers41. For instance, Sestak et al.42 reported that tamoxifen reduced the risk of breast cancer in women with BRCA1 and BRCA2 mutations. Furthermore, research on raloxifene in comparable populations has indicated that it is effective in lowering the incidence of breast cancer, although with weaker evidence than that for tamoxifen18,24. The evidence supporting tamoxifen and raloxifene as effective chemopreventive strategies for BRCA1 and BRCA2 carriers was strengthened by the pooled analysis conducted in this study.
Our meta-analysis reported a lower relative risk reduction of 20% in comparison to 40–50% risk reduction of included randomized controlled trials (RCTs) that emerged due to differences in patient populations and study designs. Due to the inclusion of diverse populations from observational studies and case-control studies, the results varied in follow-up durations and baseline risk factors for breast cancer. Additionally, strict eligibility criteria, controlled environments, and higher patient compliance in RCTs resulted in greater risk reduction. Given the variations in breast cancer risk linked to each mutation, subgroup analysis also examined the effectiveness of tamoxifen and raloxifene in carriers of BRCA1 and BRCA2 mutations. The study discovered that, after using tamoxifen or raloxifene, the risk of breast cancer decreased in both BRCA1 and BRCA2 carriers. This result is consistent with earlier studies that found that carriers of BRCA2 mutations also benefit from chemoprevention, even though they have a higher overall chance of developing breast cancer43,44. However, the small variation in risk reduction between the two groups might indicate variable efficacy, which calls for greater research in larger, more focused trials.
In this case, the reported heterogeneity ranging from 51 to 85% indicated a moderate to high level of variability in the effect sizes across the included studies. This suggests that the true effect sizes or the actual impact of the intervention (Selective Estrogen Receptor Modulators, or SERMs) for breast cancer risk reduction vary significantly across different studies. Such variation could be due to differences in the study design, population, or other factors affecting the outcomes. In contrast, the heterogeneity within the BRCA1 and BRCA2 subgroups was reported at 98%, indicating almost complete variability between these two genetic groups. However, the statement that the “difference was 0%” indicates that despite the high heterogeneity, there was no difference in the response to SERMs between women with BRCA1 and BRCA2 mutations in terms of risk reduction for breast cancer. Essentially, the response to SERMs was similar between the two genetic subgroups, although the individual studies contributing to the analysis were highly variable.
The quality of the studies included in the meta-analysis was a crucial factor to consider when evaluating the findings. Based on the Newcastle-Ottawa Scale (NOS), the study found that six of the nine included studies had a moderate risk of bias, whereas two had a low risk. The existence of moderate risk in multiple studies indicates that the results should be carefully observed even though the overall quality of the research is generally good. The stability of the observed effect sizes may be affected by potential biases, particularly in case-control studies.
With enormous benefits, there are a few limitations in this study. First, the number of included studies was limited, which could have affected the reliability and credibility of the findings. Furthermore, not all studies were of high quality or low risk, and several studies were rated as having a moderate risk of bias. This may have affected the outcomes, especially regarding the precision and applicability of the findings. Moreover, the observed heterogeneity among studies may have been caused by differences in the patient characteristics and outcomes of tamoxifen or raloxifene. Lastly, there is a lack of subgroup analyses based on age, postmenopausal and reproductive phases, and other genetic risk factors that may affect the efficacy of tamoxifen for breast cancer risk reduction among BRCA1/2 carrier women.
Because participants may have differing degrees of knowledge regarding their genetic status or treatment history, case-control studies are frequently vulnerable to recall bias, which could affect the accuracy of the reported results. When considering the therapeutic use of these drugs, one should consider the risk profiles of each individual, potential side effects, and long-term effects on quality of life45. Further research is required, particularly in the form of larger randomized controlled trials, to validate these findings and more precisely define the optimal patient populations for each chemoprevention strategy.
Conclusion
Overall, the findings of this meta-analysis showed that tamoxifen or raloxifene can significantly reduce breast cancer risk among women with BRCA1 and BRCA2 mutations. The effectiveness of tamoxifen and raloxifene was similar across the BRCA1 and BRCA2 subgroups in women. Individual risk profiles, the possibility of adverse effects, and long-term implications on quality of life should all be considered when making therapeutic decisions to utilize these medications. More research is required, especially in larger randomized controlled trials, to clearly define suitable patient populations for each chemoprevention approach and to validate these findings.
Data availability
The manuscript includes all the necessary data; related data may be provided on request from the corresponding author/s.
References
Collaborators, G. et al. The global burden of cancer attributable to risk factors, 2010–19: a systematic analysis for the global burden of Disease Study 2019. Lancet 400 (10352), 563–591 (2022).
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Cancer J. Clin. 71 (3), 209–249 (2021).
Behl, T. et al. Understanding the mechanistic pathways and clinical aspects associated with protein and gene-based biomarkers in breast cancer. Int. J. Biol. Macromol. 245, 126595 (2023).
Antunes Meireles, P. et al. Comparing prognosis for BRCA1, BRCA2, and Non-BRCA breast Cancer. Cancers 15 (23), 5699 (2023).
Pourmasoumi, P., Moradi, A. & Bayat, M. BRCA1/2 mutations and breast/ovarian cancer risk: A new insights review. Reprod. Sci. 1–11 (2024).
Antoniou, A. The influence of number and timing of pregnancies on breast cancer risk for women with BRCA1 or BRCA2 mutations. (2018).
Pruthi, S., Heisey, R. E. & Bevers, T. B. Chemoprevention for breast cancer. Ann. Surg. Oncol. 22, 3230–3235 (2015).
van der Kolk, D. M. et al. Penetrance of breast cancer, ovarian cancer and contralateral breast cancer in BRCA1 and BRCA2 families: high cancer incidence at older age. Breast Cancer Res. Treat. 124, 643–651 (2010).
Smith, S. G. et al. Factors affecting uptake and adherence to breast cancer chemoprevention: a systematic review and meta-analysis. Ann. Oncol. 27 (4), 575–590 (2016).
Farkas, A., Vanderberg, R., Merriam, S. & DiNardo, D. Breast cancer chemoprevention: a practical guide for the primary care provider. J. Women’s Health. 29 (1), 46–56 (2020).
Das, A., Lavanya, K. J., Nandini, Kaur, K. & Jaitak, V. Effectiveness of selective estrogen receptor modulators in breast cancer therapy: an update. Curr. Med. Chem. 30 (29), 3287–3314 (2023).
Shieh, Y. & Tice, J. A. Medications for primary prevention of breast cancer. Jama 324 (3), 291–292 (2020).
Das, S., Kulkarni, S., Singh, Y., Kumar, P. & Thareja, S. Selective estrogen receptor modulators (SERMs) for the treatment of ER + breast cancer: an overview. J. Mol. Struct. 1270, 133853 (2022).
Makar, S. et al. Rational approaches of drug design for the development of selective estrogen receptor modulators (SERMs), implicated in breast cancer. Bioorg. Chem. 94, 103380 (2020).
Fisher, B. et al. Tamoxifen for prevention of breast cancer: Report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. JNCI J. Natl. Cancer Inst. 90(18), 1371-1388 (1998).
Wolmark, N. & Dunn, B. K. The role of tamoxifen in breast Cancer Prevention: issues sparked by the NSABP breast Cancer Prevention Trial (P-1). Ann. N. Y. Acad. Sci. 949 (1), 99–108 (2001).
Lippman, M. E. et al. Indicators of lifetime estrogen exposure: effect on breast cancer incidence and interaction with raloxifene therapy in the multiple outcomes of raloxifene evaluation study participants. J. Clin. Oncol. 19 (12), 3111–3116 (2001).
Gennari, L., Merlotti, D., Paola, V. D. & Nuti, R. Raloxifene in breast cancer prevention. Exp. Opin. Drug Saf. 7 (3), 259–270 (2008).
Cummings, S. R. et al. The effect of raloxifene on risk of breast cancer in postmenopausal women: results from the MORE randomized trial. Jama 281 (23), 2189–2197 (1999).
McCowan, C. et al. Cohort study examining tamoxifen adherence and its relationship to mortality in women with breast cancer. Br. J. Cancer. 99 (11), 1763–1768 (2008).
Eggemann, H. et al. Tamoxifen treatment for male breast cancer and risk of thromboembolism: prospective cohort analysis. Br. J. Cancer. 120 (3), 301–305 (2019).
Dew, J., Wren, B. & Eden, J. Tamoxifen, hormone receptors and hormone replacement therapy in women previously treated for breast cancer: a cohort study. Climacteric 5 (2), 151–155 (2002).
Vogel, V. G. et al. Effects of tamoxifen vs raloxifene on the risk of developing invasive breast cancer and other disease outcomes: the NSABP study of tamoxifen and Raloxifene (STAR) P-2 trial. Jama 295 (23), 2727–2741 (2006).
Land, S. R. et al. Patient-reported symptoms and quality of life during treatment with tamoxifen or raloxifene for breast cancer prevention: the NSABP study of tamoxifen and Raloxifene (STAR) P-2 trial. Jama 295 (23), 2742–2751 (2006).
Moher, D. et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Reviews. 4, 1–9 (2015).
Page, M. J. et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Bmj 372 (2021).
Lo, C. K. L., Mertz, D. & Loeb, M. Newcastle-Ottawa Scale: comparing reviewers’ to authors’ assessments. BMC Med. Res. Methodol. 14, 1–5 (2014).
Deeks, J. J. & Higgins, J. P. Statistical algorithms in review manager 5. Stat. Methods Group. Cochrane Collab. 1(11) (2010).
Gronwald, J. et al. Duration of tamoxifen use and the risk of contralateral breast cancer in BRCA1 and BRCA2 mutation carriers. Breast Cancer Res. Treat. 146, 421–427 (2014).
Gronwald, J. et al. Tamoxifen and contralateral breast cancer in BRCA1 and BRCA2 carriers: an update. Int. J. Cancer. 118 (9), 2281–2284 (2006).
Narod, S. A. et al. Tamoxifen and risk of contralateral breast cancer in BRCA1 and BRCA2 mutation carriers: a case-control study. Lancet 356 (9245), 1876–1881 (2000).
King, M-C. et al. Tamoxifen and breast cancer incidence among women with inherited mutations in BRCA1 and BRCA2: National Surgical adjuvant breast and Bowel Project (NSABP-P1) breast Cancer Prevention Trial. Jama 286 (18), 2251–2256 (2001).
Metcalfe, K. et al. Contralateral breast cancer in BRCA1 and BRCA2 mutation carriers. J. Clin. Oncol. 22 (12), 2328–2335 (2004).
Kotsopoulos, J. et al. Tamoxifen and the risk of breast cancer in women with a BRCA1 or BRCA2 mutation. Breast Cancer Res. Treat. 201 (2), 257–264 (2023).
Phillips, K-A. et al. Tamoxifen and risk of contralateral breast cancer for BRCA1 and BRCA2 mutation carriers. J. Clin. Oncol. 31 (25), 3091–3099 (2013).
Phillips, K. et al. Tamoxifen and risk of contralateral breast cancer for BRCA1 and BRCA2 mutation carriers: a combined analysis from the Kathleen Cuningham Foundation Consortium for Research into familial breast Cancer (kConFab), the International BRCA1 and BRCA2 carrier cohort study (IBCCS), and the breast Cancer Family Registry (BCFR). J. Clin. Oncol. 29 (15_suppl), 1500 (2011).
Anderson, C., Nichols, H. B., House, M. & Sandler, D. P. Risk versus benefit of chemoprevention among raloxifene and tamoxifen users with a family history of breast cancer. Cancer Prev. Res. 12 (11), 801–808 (2019).
Chang, M. Tamoxifen resistance in breast cancer. Biomolecules Ther. 20 (3), 256 (2012).
Freedman, A. N. et al. Benefit/risk assessment for breast cancer chemoprevention with raloxifene or tamoxifen for women age 50 years or older. J. Clin. Oncol. 29 (17), 2327–2333 (2011).
Grady, D. et al. Reduced incidence of invasive breast cancer with raloxifene among women at increased coronary risk. J. Natl Cancer Inst. 100 (12), 854–861 (2008).
Moen, M. D. & Keating, G. M. Raloxifene: a review of its use in the prevention of invasive breast cancer. Drugs 68, 2059–2083 (2008).
Sestak, I., Edwards, R., Howell, A. & Cuzick, J. Comparison of side-effect profiles during active treatment versus follow-up in the international breast Cancer intervention study I tamoxifen prevention trial. Breast Cancer Res. 9, 1–2 (2007).
Schrag, D., Kuntz, K. M., Garber, J. E. & Weeks, J. C. Life expectancy gains from cancer prevention strategies for women with breast cancer and BRCA1 or BRCA2 mutations. Jama 283 (5), 617–624 (2000).
Bramley, M. et al. Effects of oestrogens and anti-oestrogens on normal breast tissue from women bearing BRCA1 and BRCA2 mutations. Br. J. Cancer. 94 (7), 1021–1028 (2006).
Peshkin, B. N., Isaacs, C., Finch, C., Kent, S. & Schwartz, M. D. Tamoxifen as chemoprevention in BRCA1 and BRCA2 mutation carriers with breast cancer: a pilot survey of physicians. J. Clin. Oncol. 21 (23), 4322–4328 (2003).
Acknowledgements
This study was supported by the National Key Research and Development Program of China (Grant No. 2019YFE0198800).
Author information
Authors and Affiliations
Contributions
ASSA and NUK did the literature search, extracted the data, analyzed it, and wrote the manuscript. NUK and TC oversaw the data extraction and review of the final manuscript. All authors revised it for important intellectual content.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Alwashmi, A.S.S., Khan, N.U. & Chen, T. Risk-benefits assessment of tamoxifen or raloxifene as chemoprevention for risk reduction of breast cancer among BRCA1 and BRCA2 carriers: a meta-analysis. Sci Rep 15, 6796 (2025). https://doi.org/10.1038/s41598-025-89915-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-89915-z