Abstract
Fine particulate matter 2.5 (PM2.5) is a prevalent atmospheric pollutant that is closely associated with asthma. Elderly patients have a high incidence of asthma with a long course of illness. Our previous studies revealed that exposure to PM2.5 diminishes lung function and exacerbates lung damage in elderly rats. In the present study, we investigated whether PM2.5 exposure influences susceptibility to allergic asthma in elderly rats. Brown-Norway elderly rats were treated with ovalbumin (OVA) for different durations before and after PM2.5 exposure. The results from pulmonary function tests and histopathology indicated that early exposure to allergens prior to PM2.5 exposure increased susceptibility to airway hyperresponsiveness and led to severe lung injury in elderly asthmatic rats. Cytokine microarray analysis demonstrated that the majority of cytokines and chemokines were upregulated in OVA-treated rats before and after PM2.5 exposure. Cytological examination showed no change in eosinophil (EOS) counts, yet the amounts of neutrophils (NEU), white blood cells (WBC), lymphocytes (LYM), and monocytes (MON) in the lung lavage fluid of OVA-treated rats were significantly higher than those in control rats before and after PM2.5 exposure, suggesting that PM2.5 affects noneosinophilic asthma in elderly rats. ELISA results from the plasma and lung lavage fluid revealed that the levels of IgG1, IgE, IgG2a and IgG2b were significantly elevated in OVA-treated rats, whereas the level of IgG2b in the lung lavage fluid was significantly lower in rats treated with OVA prior to PM2.5 exposure compared to those treated afterward. A non-targeted metabolomic analysis of plasma identified 202 metabolites, among which 31 metabolites were differentially abundant. Ten metabolites and 11 metabolic pathways were uniquely detected in OVA-treated rats before PM2.5 exposure. Specifically, there were positive or negative correlations between the levels of Th2-associated cytokines (IL-4, IL-5, and IL-13) and six metabolites in the OVA-treated group before PM2.5 exposure, whereas the levels of IL-4 and IL-5 were negatively correlated with five metabolites in the OVA-treated group after PM2.5 exposure. Our findings suggest that PM2.5 exposure could influence the susceptibility of allergic asthma in response to allergens in elderly rats, potentially through changes in plasma metabolites.
Similar content being viewed by others
Introduction
Asthma is a common respiratory disease with complex pathophysiological alterations, affecting approximately 334 million people worldwide across all age ranges. It is also considered a heterogeneous disease in children and adults1. Asthma is generally recognized as an inflammatory disease of the airways that is characterized by airway remodeling and airway dysfunction. The hallmark feature of asthma is airway hyperresponsiveness (AHR). Allergens, infections, tobacco smoke and generalized eosinophilia can predispose individuals to chronic airway inflammation, leading to airway obstruction and AHR2. There is growing evidence that allergies are essential in the pathogenesis of asthma, and different types of allergens are associated with the development and severity of asthma3.
Fine particulate matter 2.5 (PM2.5) is known as the most prevalent air pollutant in developing countries, and exposure to PM2.5 is associated with an increased risk of asthma attacks4. PM2.5 is characterized by a small particle size and large specific surface area, so it can enter the smallest airways5,6. The main toxic mechanisms of PM2.5-induced pulmonary harm include oxidative stress, inflammatory dysregulation, impaired pulmonary immunity and epithelial‒mesenchymal transition (EMT)7.
Asthma is often considered to be the most common disease among children, but the prevalence of asthma in elderly people is increasing as the population ages8. The higher prevalence of asthma among older adults than younger individuals can be explained by the cumulative incidence of asthma. The morbidity and mortality of asthma are reportedly greater in elderly people than in younger people9,10. Asthma was found to be prevalent but underappreciated among middle-aged and elderly people in China. The estimated prevalence of asthma among Chinese people aged ≥ 45 years in 2018 was 2.16% (95% CI 1.96–2.38)11. The prevalence of asthma has been on the rise over the past three decades in China, from 0.69% in 1984 to 5.30% in 2021. In a recent report, the pooled prevalence of asthma was estimated to be 2.20% (95% CI: 1.96–2.47%) and Meta-analysis subgroups indicated that the elderly people have a higher prevalence of asthma12.
Our previous study revealed that PM2.5 exposure reduces lung function and dramatically damages lung tissue in older rats. In this study, we aimed to investigate the effects of PM2.5 exposure on susceptibility to allergic asthma in elderly rats. We used ovalbumin (OVA) and aluminum hydroxide [Al(OH)3] to establish an allergic asthma model because Al(OH)3 is a commonly used adjuvant to promote the development of a Th2 immune response to OVA. Experimental design and grouping were shown in Fig. 1.We observed phenotypes of allergic asthma and analyzed differentially abundant metabolite levels in the plasma at different sensitization times before and/or after PM2.5 exposure in elderly rats. This study will be helpful for further understanding the effects of PM2.5 exposure on susceptibility to allergic asthma in elderly people.
Experimental design and grouping. Brown‒Norway male rats (62–64 weeks old) were divided into four experimental groups: Sa, normal saline control group; AS, asthma model group; PO, PM2.5 + OVA; OPO, OVA + PM2.5 + OVA, n = 6 for each group. In the sensitization stage, the rats were sensitized by subcutaneous injection of OVA/Al (OH)3 for 5 days on week 6. In the excitation stage, 5% OVA was added to the air atomizer to achieve excitation on week 8.
Results
Effects of PM2.5 exposure on AHR and lung function in elderly rats
The enhanced pause (Penh) is thought to be an important detection indicator, which can reflect the extent of AHR in patients with asthma. As shown in Fig. 2A, the value of Penh was greater in the AS model group than in the Sa control group (P < 0.05), indicating the success of the allergic asthma model. We observed that the Penh values in both the PO group and the OPO group were significantly greater after excitation than those in the AS model group or the Sa control group (P < 0.001), with a higher Penh value in the OPO group than in the PO group (P < 0.05). We then tested the lung function of the elderly rats in the different groups at 0, 4, and 8 weeks (both before and after excitation). The results demonstrated that the respiratory rates (f) of the rats in both the PO and OPO groups significantly increased on week 4 (P < 0.05) and week 8 after excitation (P < 0.01) in contrast to those of the AS model group and the Sa control group (Fig. 2B). The tidal volume (TVb) in both the PO and OPO groups significantly decreased (P < 0.001) compared with that in the AS model group or the Sa control group (Fig. 2C), although there was no obvious difference in the respiratory rate or tidal volume between the PO group and the OPO group.
Effects of PM2.5 exposure on AHR and lung function in elderly rats. (A) Penh values, (B) respiration rates, (C) tidal volume. 8 (a) represents before excitation on week 8, and 8 (b) represents after excitation on week 8. The data are presented as the mean ± SD (n = 4). *P < 0.05, **P < 0.01, ***P < 0.001 vs. Sa group. #P < 0.05, ##P < 0.01, ###P < 0.001 vs. As group. &P < 0.05 vs. PO group.
Effects of PM2.5 exposure on lung injury in elderly rats
We performed hematoxylin and eosin (H&E) staining of rat lung tissues from the different groups. Compared with those in the Sa group, the lung tissues in the As group had a small amount of serous fluid and inflammatory cell exudates (mainly macrophages) in the alveoli. Compared with those in the As group, the number of alveolar plasma cells and inflammatory cells (mainly macrophages) in the PO and OPO groups increased, and bronchial epithelial cell secretion increased due to hemorrhage phenomena. Notably, PM2.5 exposure exacerbated lung injury in asthma, indicating that there were more pronounced alterations in the OPO group than in the PO group (Fig. 3).
Effects of PM2.5 exposure on lung injury in elderly rats. Optical three images of H&E-stained lung tissues for each group are shown, and histopathological changes were observed in the different groups obtained from three different rats (n = 3). The green arrows represent macrophages, and the red arrows represent bleeding. (200 × magnification, scale bars = 100 μm).
Effects of PM2.5 exposure on cytokines and chemokines in elderly rats
H&E staining revealed inflammatory cell infiltration in the lung tissue after PM2.5 exposure, so we further measured the levels of 23 cytokines and chemokines in the lung lavage fluid. As shown in Fig. 4, the levels of most cytokines and chemokines, including tumor necrosis factor (TNF)-α, interleukin (IL-1α, IL-1β, IL-2, IL-4, IL-5, IL-6, IL-10, IL-12, IL-13, IL-17 A), interferon (IFN)-γ, colony-stimulating factor (G-CSF, M-CSF), monocyte chemoattractant protein-1 (MCP-1), monocyte chemotactic protein (MIP-1α, MIP-3α), and recombinant C-C motif chemokine 5 (RANTES), significantly increased, whereas the VEGF levels significantly decreased in both the PO and OPO groups compared with those in the AS model group or the Sa control group. IL-18 and granulocyte‒macrophage colony‒stimulating factor (GM‒CSF) levels were increased in the PO group compared with those in the AS group and OPO group, indicating that there was a significant difference between the PO group and OPO group. Only the IL-7 and growth-regulated oncogene (GRO)/keratinocyte chemoattractant (KC) levels did not differ among these groups.
Effects of PM2.5 exposure on routine blood tests and immunoglobulins in elderly rats
We further analyzed alterations in routine blood tests and immunoglobulins in different groups. In the blood samples, there was a significant difference in the number of leukocyte (WBC) and lymphocyte (LYM) between the PO group and the OPO group, but most blood indicators showed no changes among these groups. In lung lavage fluid, there was no difference in the number of WBC and LYM between the PO group and OPO group, but the number of WBC and LYM in the PO group and OPO group was greater than that in the As group. In addition, the number of neutrophil (NEU) and monocyte (MON) was significantly greater in the PO and OPO groups than in the Sa or As groups. Red blood cell (RBC) and blood platelet (PLT) were greater in the PO group than in the Sa and As groups, revealing a significant difference in RBC between the PO group and the OPO group. However, the number of eosinophils (EOS) did not differ among these groups (Fig. 5).
Effects of PM2.5 exposure on blood cells in the blood and lung lavage fluid of rats. (A) Blood samples, (B) lung lavage fluid. The data are presented as the mean ± SD (n = 6). *P < 0.05, **P < 0.01, ***P < 0.001 vs. Sa group. #P < 0.05, ##P < 0.01, ###P < 0.001 vs. As group. &P < 0.05, &&P < 0.01 vs. PO group.
It is known that immunoglobulins play critical roles in allergen-induced asthma. ELISA results from the plasma and lung lavage fluid revealed that the levels of IgG1, IgE, IgG2a and IgG2b in the AS group were significantly greater than those in the Sa group. Notably, the plasma levels of IgG1 and IgG2c were significantly lower in the OPO group than in the PO group, whereas the level of IgG2b in the lung lavage fluid was significantly lower in the OPO group than in the PO group (Fig. 6).
Effects of PM2.5 on immunoglobulins in the plasma and lung lavage fluid of rats. (A) Plasma samples, (B) lung lavage fluid. The data are presented as the mean ± SD (n = 6), *P < 0.05, **P < 0.01, ***P < 0.001 vs. Sa group. #P < 0.05, ##P < 0.01, ###P < 0.001 vs. As group. &P < 0.05, &&P < 0.01 vs. PO group.
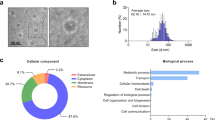
Effects of PM2.5 exposure on metabolites in the plasma
Metabolomics can reflect local and systemic changes in or dysregulation of pathogens, and metabolite changes caused by metabolic pathway disruptions may be related to changes in airway inflammation, airway obstruction, and mucus production in asthma13. Therefore, we performed a non-targeted metabolomic analysis of rat plasma. Metabolites in the plasma samples were detected via UPLC‒Q‒TOF‒MS, and 202 metabolites were pooled and identified. We compared the difference in metabolites between the PO group and the As group and between the OPO group and the As group to analyze the effects of different sensitization times under PM2.5 exposure. A total of 31 differentially abundant metabolites were screened (Fig. 7A). Compared with those in the As group, 18 metabolites were downregulated and 3 metabolites were upregulated in the PO group, whereas 8 metabolites were downregulated and 6 metabolites were upregulated in the OPO group. We found that four common metabolites, namely, L-proline, cis-aconitate, citric acid and 3-indoleactonitrile, were downregulated in both the PO group and the OPO group. Notably, 10 metabolites were detected only when the OPO group was compared with the As group.
Next, we analyzed the metabolic pathways, and a total of 14 and 20 metabolic pathways were enriched in the PO group (Fig. 7B) and OPO group (Fig. 7C), respectively. There were 9 metabolic pathways that were altered in both the PO and OPO groups, whereas 11 metabolic pathways, such as the citrate cycle (TCA cycle), diabetic cardiomyopathy, glycine, serine and threonine metabolism, and tryptophan metabolism, were detected only in the OPO group compared with the As group.
Screening and characterization of differentially abundant metabolites in the plasma of rats with different sensitization times under PM2.5 exposure. (A) Cluster heatmap analysis of differentially abundant metabolites showing the differences in metabolites between the AS group and the PO group (PS) and between the As group and the OPO group (PPS). U represents upregulation, and D represents downregulation. (VIP value > 1, P value < 0.05, fold change > 2 or < 0.5). (B) Analysis of the metabolic pathways when the As group was compared with the PO group. (C) Analysis of the metabolic pathways when the As group was compared with the OPO group. n = 6.
Finally, we performed correlation analysis between inflammatory factors and metabolites in both the PO group (Fig. 8A) and the OPO group (Fig. 8B) relative to As group, respectively. Because the Th2 cell-mediated inflammatory response plays an important role in asthma, we selected cytokines (IL-4, IL-5, and IL-13) secreted by Th2 cells for correlation analysis. The results revealed that IL-4 and IL-5 were negatively correlated with 5 metabolites, including L-valine, cis-aconitate, D-gluconate, citraconic acid and indole-3-pyruvic acid, in the PO group, whereas they were negatively correlated with cis-aconitate and citraconic acid in the OPO group. Specifically, there were positive correlations between the levels of Th2-associated cytokines (IL-4, IL-5, and IL-13) and the levels of 4 metabolites, erucamide, cholecalciferol, erucic acid and argininosuccinic acid, in the OPO group but not in the PO group.
Correlation analysis between Th2 cell-secreted inflammatory factors and metabolites in the plasma of rats exposed to PM2.5. (A) Correlation analysis between inflammatory factors (IL-4 and IL-5) and five metabolites on the basis of spearman rank in the PO group relative to As group. (B) Correlation analysis between inflammatory factors (IL-4, IL-5, and IL-13) and six metabolites on the basis of spearman rank in the OPO group relative to As group. Blue indicates a negative correlation, and red indicates a positive correlation. #P < 0.05, ##P < 0.01 vs. As group.
Discussion
Asthma is thought to be a heterogeneous and multifactorial disease, which can be caused by a combination of genetic and external factors. Notably, environmental factors are important for the occurrence of asthma. PM2.5 in air is one of the major environmental risks of asthma because it can enter the lungs and be deposited in the airways because of its small particle size14. In the present study, we demonstrated the effects of PM2.5 on various asthma phenotypes in elderly rats exposed to allergens prior to PM2.5 exposure and after PM2.5 exposure, indicating that PM2.5 exposure enhances susceptibility to allergic asthma in elderly rats.
Allergic asthma is the most common type of asthma, and accounts for 50-80% of asthma cases15. Allergic asthma is believed to have hypersensitivity and typical symptoms, triggered by allergens such as pet dander, dust mites, pollen, and food items. Many patients are diagnosed with asthma in childhood or adolescence, so asthma is often overlooked as a respiratory disease in aged patients, resulting in elderly people with asthma being undertreated16. In rat models of OVA-induced asthma, OVA is a well-known allergen, and when it is used with Al(OH)3 to immunize rats, it induces asthma through Th2-mediated inflammatory responses, exhibiting characteristics such as airway inflammation, AHR, and airway remodeling17. Therefore, in this study, we used OVA Al (OH)3 to establish an asthma model to investigate whether early exposure to allergens prior to PM2.5 exposure can increase the susceptibility of elderly rats and aggravate the development of asthma (Fig. 1). In our study, the results revealed that the Penh value of the OPO group was significantly greater than that of the PO group, whereas the Penh values of both the PO and OPO groups were significantly greater than those of the Sa and As groups (Fig. 2), indicating that early exposure to allergens prior to PM2.5 exposure increased susceptibility to AHR in elderly asthmatic rats.
Asthma is a chronic inflammatory disease of the airways in which multiple types of cells, including macrophages, granulocytes, T cells, and non-immune cells, act together to play important roles in the pathogenesis of asthma18,19. Here, we observed a number of macrophages in H&E-stained lung tissues from rats in the PO and OPO groups (Fig. 3). In response to allergens, macrophages secrete TNF-α, IFN-γ and interleukins. Our results revealed that the levels of TNF-α, IFN-γ, IL-1α, IL-1β, IL-2, IL-4, IL-5, IL-6, IL-10, IL-12, IL-13, and IL-17 A were elevated in the PO and OPO groups (Fig. 4), suggesting that macrophage dysfunction plays a particularly significant role in asthma pathogenesis when elderly rats are exposed to PM 2.5.
In asthma, Th2-type immune responses involve cytokines such as IL-4, IL-5, and IL-13, which stimulate epithelial cells, smooth muscle cells, and fibroblasts, leading to airway hyperresponsiveness and remodeling20,21. These cytokines play a central role in the pathogenesis of asthma. In addition to Th2 cytokines, non-Th2 cytokines such as IL-10 and IL-17 are also associated with the severity of asthma22. These factors may play a significant role in non-Th2 asthma. IL-17 A, a cytokine associated with Th17 cells, contributes to airway remodeling by increasing neutrophil infiltration, mucus cell metaplasia, and smooth muscle mass. Increased expression of IL-17 A is associated with the severity of asthma23. There is a complex regulatory network among inflammatory factors, which play a key role in the development of asthma. In this study, we observed that the levels of IL-4, IL-5, IL-13, IL-10 and IL-17 A significantly increased in both the PO and OPO groups compared with AS and Sa control group (Fig. 4), indicating the effects of PM2.5 on Th2-type cytokines and non-Th2 cytokines, as well as association with the severity of asthma.
In the present study, we used Brown-Norway elderly rats (62–64 weeks old, male) that did not exhibit a clear induction of IL-4/5/13 in AS model group after OVA challenge, which might be due to several factors including immunosenescence and crosstalk of signaling pathways24,25,26. There is evidence that IL-4 and IL-13 inhibit the migration and effector functions of neutrophils through IL-4R signaling, which may affect the induction of IL-4/5/13 in asthma models27. Studies have shown that in the rat acute lung injury model induced with bacteria, VEGF levels are reduced after excitation 4 h and 24 h28. In this study, samples were collected 24 h after excitation using OVA for subsequent analysis. Therefore, we speculate that the decrease in VEGF levels may be due to acute lung injury caused by the process of OVA elicitation. An imbalance of T cells has been reported to play pivotal roles in asthma pathogenesis29. In response to allergens, naïve T (Tn) cells are activated by macrophages and tend to differentiate into various cells, such as T helper (Th) 1, Th2, Th17, Th22, Th9, and regulatory T (Treg) cells. Th1 cells generate IL-2 and IFN-γ, promoting type 1 immunity. Th2 cells are directly triggered by airway epithelial-derived cytokines, which subsequently secrete Th2-associated cytokines (IL-4, IL-5, and IL-13). Th17 cells produce IL-17 A, IL-17 F, and IL-22, which have proinflammatory effects on neutrophil recruitment and activation30. The results of this study revealed that the levels of IL-2, IFN-γ, IL-4, IL-5, IL-13, and IL-17 A were elevated in the PO and OPO groups (Fig. 4), indicating that these cytokines might contribute to the inflammatory response in elderly rats with asthma when exposed to PM2.5.
Macrophage polarization disrupts the balance of classically activated (M1)/alternatively activated (M2) macrophages in asthma31,32. IFN-γ and TNF-α stimulate M1 macrophages, whereas IL-4, IL-13, and IL-10 activate M2 macrophages33,34. M1 macrophages produce Th1-associated cytokines (TNF-α, IL-1β, IL-2, IL-6, and IL-12), Th17-associated cytokines (IL-23 and IL-27) and MCP-135. M1 macrophages exacerbate Th1-type and Th17-type inflammatory responses associated with neutrophilic infiltration, oxidative damage, and AHR36,37. The immune complex promotes M2b macrophage activation, participating in Th2-type immune regulation and the expression of TNF-α, IL-1β, IL-6, and IL-10. In our study, the levels of IFN-γ, TNF-α, IL-1β, IL-2, IL-6, IL-4, IL-13, IL-10 and IL-12 were elevated in the PO and OPO groups (Fig. 4), indicating that crosstalk between macrophages and T cells is involved in asthma pathogenesis in elderly rats exposed to PM2.5.
Asthma can be divided into eosinophilic and noneosinophilic asthma, on the basis of inflammatory cell patterns in airway secretions38. Eosinophilic asthma accounts for most severe asthma cases, but neutrophilic asthma or a mixture of the two types can also present a severe asthma phenotype39. Clinical studies have shown that patients with noneosinophilic asthma do not have symptoms of increased eosinophils, and patients are usually older at the time of onset35. In our study, cytological analysis revealed that the number of EOS did not change, whereas the amounts of NEU, WBC, LYM, and MON in the lung lavage fluid of the rats significantly increased after PM2.5 exposure (Fig. 5), suggesting that PM2.5 affects noneosinophilic asthma in elderly rats. The increase in the number of WBC indicated that the rats had developed allergies after provocation due to the contributions of NEU and LYM.
A number of reports have demonstrated the role of allergen-specific immunoglobulins (IgE, IgG, IgA) in allergic diseases. IgE plays an essential role in type I immediate allergic responses and mediates the activation of allergen-specific T cells as well as the release of inflammatory mediators, whereas allergen-specific IgG and IgA compete with IgE for binding to allergens40,41. In mice, high levels of IL-4 and IgG1 responses are usually associated with Th2 responses, whereas high levels of IFN-γ, IgG2a, IgG2b and IgG2c are thought to reflect Th1 responses42. In our study, the results revealed that IgE, IL-4, IgG1, IFN-γ, IgG2a and IgG2b were elevated in the PO group compared with those in the Sa group, indicating that exposure to PM2.5 induced a mixture of Th1 and Th2 responses in elderly rats with asthma. In contrast to the Sa group, IgG1 was increased in the PO group but not in the OPO group, although IgG2a was elevated in both the PO and OPO groups (Fig. 6), implying that early exposure to sensitizers prior to PM2.5 might influence the effect of PM2.5 exposure on Th2 responses in asthma.
Alterations in various metabolites in biological fluids reflect the physiological state of normality and disease. Therefore, we investigated the effects of different sensitization times on plasma metabolites in elderly rats with asthma after exposure to PM2.5. A total of 202 metabolites were identified, and 31 differentially abundant metabolites were screened. Our results revealed significant reductions in the levels of four differentially differentiated metabolites in the PO and OPO groups, namely, L-proline, cis-Aconitate, citric acid and 3-indoleactonitrile (Fig. 7). L-Proline is involved in arginine metabolism. Studies have shown that arginase may play a role in chronic airway remodeling through the formation of L-ornithine and the downstream production of polyamines and L-proline, which are involved in the processes of cell proliferation and collagen deposition43. Upon macrophage activation, cis-Aconitate, an intermediate product of the tricarboxylic acid cycle, is converted to itaconic acid in the mitochondrial matrix. In studies of asthmatic mice, allergens were shown to induce the production of itaconate by lung macrophages, which acts on immune cells inside and around the cells. Itaconic esters secreted into airways inhibit signal transducer and activator of transcription 1 (STAT1) phosphorylation in CD4 + T cells, resulting in decreased production of Th2-type cytokines (IL-4, IL-5, and IL-13)44. The role of citraconic acid and 3-indoleactonitrile in asthma has been well documented, implying that they might play a role in asthma induced by PM2.5 exposure.
Current research suggests that asthma is associated with a shift in cellular metabolism to increased aerobic glycolysis while also exhibiting substantial changes in fatty acid and amino acid metabolism45. In addition, asthma-related amino acid changes are also enriched in pathways, leading to increased airway inflammation46. Various metabolic pathways related to energy metabolism, macromolecular biosynthesis and redox signaling are differentially modulated in asthma47. Compared with those in the PO group, a total of 20 metabolic pathways were changed in the OPO group. Notably, 11 metabolic pathways, such as the citrate cycle (TCA cycle), diabetic cardiomyopathy, glycine, serine and threonine metabolism, and tryptophan metabolism, were detected only when the OPO group was compared with the As group. We suppose that these metabolic pathways might be affected by early exposure to sensitizers prior to exposure to PM2.5.
It is reported that a metabolic imbalance was linked to the pathogenesis of asthma48. Recent report revealed that plastic pollution derivatives aggravated allergic asthma in mice, involving lung cell ferroptosis and metabolomics49. We note that IL-4 and IL-5 were negatively correlated with five metabolites, including L-valine, D-gluconate, citraconic acid, cis-aconitate and indole-3-pyruvic acid, in the PO group (Fig. 8A). L-valine is an essential branched chain amino acid, playing a role in immune metabolism50. The antioxidant properties of D-gluconate may have potential positive effects in alleviating asthma symptoms, particularly in reducing oxidative stress and regulating immune responses51. Citraconic acid has anti-inflammatory effects and modulates cell metabolism in immunomodulatory process52. As an anti-inflammatory metabolite, cis-aconitate regulates macrophage metabolic remodeling and inflammation by inhibiting succinate dehydrogenase53. Indole-3-pyruvic acid is involved in the production of tryptophan metabolites that mediate the anti-inflammatory function of cytokine-primed human muscle stem cells54. We speculate that these metabolites may indirectly and negatively affect IL-4 and/or IL-5-related inflammatory processes in OVA-treated rats after exposure to PM2.5.
Th2-associated cytokines (IL-4, IL-5, and IL-13) were positively correlated with 4 metabolites, namely, enrucamide, cholecalciferol, eucolic acid and argininosuccinic acid, whereas they were negatively correlated with cis-Aconitate and citraconic acid in the OPO group (Fig. 8B). It is reported that the antidepressant and anti-anxiety effects of erucamide may be related to the regulation of the hypothalamus-pituitary-adrenal (HPA) axis55. The activation of the HPA axis can affect the production and release of inflammatory factors. As a fatty acid, erucic acid may indirectly affect immune cell signaling by affecting the lipid composition and function of cell membranes, including potentially affecting the IL-4 signaling pathway56. Argininosuccinic acid increases the production of reactive oxygen species, causes lipid peroxidation and protein oxidation, and induces oxidative stress in the developing rat brain57. Argininosuccinic acid participates in the fourth step of the urea cycle, with being cleaved to arginine by argininosuccinic acid lyase. Aberrant arginine catabolism represents a novel asthma paradigm and alterations of the arginine metabolome play a role in the pathogenesis of asthma58. In this study, there are positive correlations between the levels of Th2-associated cytokines (IL-4 and IL-13) and the level of argininosuccinic acid, indicating the potential involvement of argininosuccinic acid in the pathogenesis of asthma in OVA-treated rats before and after PM2.5 exposure. Cholecalciferol, also known as vitamin D3, has been a subject of interest in relation to asthma due to its potential immunomodulatory role in the immune system, which also links to inflammation-induced epithelial changes seen in asthma59. Randomized controlled trials have suggested that vitamin D supplementation can prevent asthma exacerbations in older adults with severe vitamin D deficiency60. Vitamin D3 can affect the differentiation and activity of T cells, especially in regulating Th1/Th2 balance. Vitamin D3 alleviates airway inflammation in asthma by promoting the secretion of IL-10 and inhibiting the secretion of IL-461. Therefore, these metabolites may have potential influence on the production and activity of ILs such as IL-4, IL-5 and IL-13 in the pathogenesis of asthma in OVA-treated rats before and after PM2.5 exposure. According to reports in literature, the mechanisms in the correlation between metabolites and Th2 cytokines in the immune response of asthma may be explained by oxidative stress, immunomodulation and signaling pathways.
Conclusion
PM2.5 exposure enhanced AHR, reduced lung function, caused lung damage, and aggravated lung inflammation in elderly rats with asthma. Early exposure to sensitizers prior to PM2.5 could affect the effects of PM2.5 exposure on AHR, lung tissue injury, and the levels of some cytokines and immunoglobulins in aged rats with asthma, possibly through changes in plasma metabolites. Further research is needed to determine whether multiple sensitizers during PM2.5 exposure can increase the susceptibility of older rats to asthma.
Materials and methods
Animal grouping and experimental process
Brown-Norway rats (62–64 weeks old, male) were purchased from Beijing Vital River Laboratory Animal Technology Company and raised under SPF conditions in the animal house of the Northern Center of the Institute of Laboratory Animal Sciences, CAMS&PUMC. The experimental animals were separated into the following four groups: normal saline group (Sa, n = 6), Asthma group (As, n = 6), PM2.5 exposure + OVA sensitization one time (PO, n = 6) and PM2.5 exposure + OVA sensitization two times (OPO, n = 6).
We collected PM2.5 from Shijiazhuang using previously described method and stored it at 4 degrees62. We used an air atomizer to expose rats to PM2.5 or saline. The Sa group was exposed with 5 ml normal saline for 15 min with an air atomizer once in the morning and once in the afternoon for 8 weeks. The As group was exposed to normal saline for 8 weeks by the same method as the Sa group. At 6 weeks, rats were sensitized by subcutaneous injection of 0.4 ml OVA + Al (OH)3 for 5 days, and 14 days after sensitization, 5% OVA was added to the air atomizer, which was inhaled for 10 min to complete excitation. The PO group was exposed with 5 ml PM2.5 for 15 min with an air atomizer once in the morning and once in the afternoon for 4 weeks, and the rats were exposed to normal saline for the last 4 weeks by the same method. At 6 weeks, the rats were sensitized and stimulated using the abovementioned method. Moreover, the OPO group was exposed to PM2.5 for 4 weeks, and it is worth noting that the OPO group was initially stimulated by the same method for 5 days before the start of the experimental, sensitized again at 6 weeks, and completed the by inhalation of OVA 14 days later.
All methods were performed in accordance with the relevant guidelines and regulations. The rats were euthanized via intraperitoneal injection of pentobarbital sodium at a dosage of 30 mg/kg, followed by blood collection from the femoral artery in the abdominal region. The collected blood was divided into two parts which were as follows: one portion added with the EDTA-K2 anticoagulant was used for the cytological analysis; and the other part was collected using an anticoagulant tube and centrifuged immediately at 4000 rpm/min for 5 min. Plasma was the resulting supernatant, which was then stored at − 80 °C for ELISA detection and metabolomic research. Following ligation of the lungs, 8 ml of cold, sterile PBS was inserted into the airway, then washed 3 times, and lung lavage fluid was collected and test for cytokine levels and immunoglobulin content test and cytological analysis. Rats’ ipsilateral lungs were removed for hematoxylin-eosin (H&E) histologically analysis (LEICA, CV5030, Germany).
Lung function tests
We used a Whole Body Plethysmography (DSI-BUXCO, USA) to test lung function in rats. Place the rats in turn into the detection chamber and close the lid tightly, let them acclimatize to the chamber for 5 min before starting to collect data. Each rat was placed in individual chamber for 2 h at 0, 4 w and 8 w (no excitation and OVA excitation), and basal readings were obtained and averaged for a 3-min period. Then, export the data to analyze inspiratory time (Ti) and tidal volume (Tvb). Penh values were measured on week 8.
Sample collection
After pulmonary function tests, rat lung tissue, lung lavage fluid, and blood were collected using the previously described method for subsequent hematoxylin-eosin (H&E) histological analysis (LEICA, CV5030, Germany), cytological analysis, detection of inflammatory cytokines, immunoglobulin levels, and metabolomics analysis. (Zhao et al., 2023).
Cytokine analysis
According to the manufacturer’s instructions, we used the Bio-Plex system (Bio-Rad, USA) to measure cytokine levels in the lung lavage fluid. The cytokines selected and detailed procedures are presented in the previous publication (Guo et al., 2023).
Detection of the immunoglobulin (ig) content
ELISA was used for immunoglobulin detection and the antibodies were specific for the detected protein. Rat Immunoglobulin E (IgE) ELISA Kit (BIOFINE, FU-D1034), IgG1 (BIOFINE, FU-D1511), IgG2a (BIOFINE, FU-D1513), IgG2b (BIOFINE, FU-D1514) and IgG2c (BIOFINE, FU-D1512) were purchased. The contents of IgE, IgG1, IgG2a, IgG2b and IgG2c in rat lung lavage fluid and plasma were detected according to the instructions.
In details, plasma and lung lavage fluid were centrifuged at 3000 rpm for 30 min/10 min, then we collected the supernatant. The samples were diluted in a 1:4 ratio. Add 50 µL standard solution to the standard well, and add 50 µL diluted sample to the sample well. Subsequently, add 100 µl HRP-labeled detection antibody and incubate at 37 °C for 60 min. After incubation, discard the liquid and blot dry, and wash 5 times with wash solution. Then add 50ul of substrate A and B to each well, and incubate at 37 °C for 15 min in the dark. After incubation, add 50 µl stop solution and measured the OD value at 450 nm.
Cytological analysis
We used the ADVIA 2120i hematology analyzer (Siemens Healthineers, USA) for cytological analysis of blood and lung lavage fluid. The metrics that selected for detection are as previously published63.
Metabolomic analysis of plasma
The collected plasma samples were slowly thawed at 4 °C and then added to pre-cooled methanol/acetonitrile/aqueous solution (2:2:1, v/v), vortex mixing, low temperature sonication for 30 min, and then they were left at -20 °C for 10 min, 14,000 g centrifugation for 20 min (4 °C), and vacuum drying of the supernatant. For mass spectrometry analysis, 100 µL of acetonitrile in water (acetonitrile: water = 1:1, v/v) was added to remix, vortexed, and centrifuged at 14,000 g at 4 °C for 15 min. The supernatant was injected for analysis. Subsequently, we performed ultra-performance liquid chromatography-tandem high-resolution mass spectrometry (LC-MS) analysis (Thermo Fisher Dionex U3000 UHPLC/QE plus, USA) based on a previously published article (Guo et al., 2023).
Statistical analysis
We performed statistical analyses using SPSS 26.0 software and data visualization was done using GraphPad Prism (version 9.0) software in pulmonary function tests, cytological analysis, cytokine and immunoglobulin detection. One-way analysis of variance (ANOVA) and the least significant difference (LSD) method were used for data analysis. For statistical analysis of metabolomics, we used both univariate (Student’s t-test and fold change analysis) and multivariate (principal component analysis and orthogonal partial least squares discriminant analysis) methods. The variable projection importance (VIP) scores > 1 and p-value < 0.05 and fold change > 2 or < 0.5 were used to screen for significantly differential metabolites. All graphs are created with GraphPad Prism (version 9.0) or R software. All results were presented as mean ± standard deviation (SD). A significant level of P < 0.05 was considered statistically significant.
Data availability
All data generated or analyzed during this study can be obtained by contacting with corresponding authors.
References
Szefler, S. J. & Dakhama, A. New insights into asthma pathogenesis and treatment. Curr. Opin. Immunol. 23, 801–807. https://doi.org/10.1016/j.coi.2011.07.014 (2011).
Gans, M. D. & Gavrilova, T. Understanding the immunology of asthma: pathophysiology, biomarkers, and treatments for asthma endotypes. Paediatr. Respir. Rev. 36, 118–127. https://doi.org/10.1016/j.prrv.2019.08.002 (2020).
Pham, D. L., Le, K. M., Truong, D. D. K., Le, H. T. T. & Trinh, T. H. K. Environmental allergen reduction in asthma management: an overview. Front. Allergy 4, 1229238. https://doi.org/10.3389/falgy.2023.1229238 (2023).
Liu, K., Hua, S. & Song, L. PM2.5 exposure and Asthma Development: the key role of oxidative stress. Oxid. Med. Cell. Longev. 2022, 3618806. https://doi.org/10.1155/2022/3618806 (2022).
Li, R., Zhou, R. & Zhang, J. Function of PM2.5 in the pathogenesis of lung cancer and chronic airway inflammatory diseases. Oncol. Lett. 15, 7506–7514. https://doi.org/10.3892/ol.2018.8355 (2018).
Hou, T., Zhu, L., Wang, Y. & Peng, L. Oxidative stress is the pivot for PM2.5-induced lung injury. Food Chem. Toxicol. 184, 114362. https://doi.org/10.1016/j.fct.2023.114362 (2024).
Silva, T. D., Alves, C., Oliveira, H. & Duarte, I. F. Metabolic dysregulations underlying the pulmonary toxicity of atmospheric fine particulate matter: focus on energy-producing pathways and lipid metabolism. Air Qual. Atmos. Health 15, 2051–2065. https://doi.org/10.1007/s11869-022-01236-6 (2022).
Gillman, A. & Douglass, J. A. Asthma in the elderly. Asia Pac. Allergy 2, 101–108. https://doi.org/10.5415/apallergy.2012.2.2.101 (2012).
Bennett, G. H. et al. Risk factors and clinical outcomes associated with fixed airflow obstruction in older adults with asthma. Ann. Allergy Asthma Immunol. 120, 164–168e161. https://doi.org/10.1016/j.anai.2017.10.004 (2018).
Hsu, J., Chen, J. & Mirabelli, M. C. Asthma morbidity comorbidities, and modifiable factors among older adults. J. Allergy Clin. Immunol. Pract. 6, 236–243e237. https://doi.org/10.1016/j.jaip.2017.06.007 (2018).
Wan, J., Zhang, Q., Li, C. & Lin, J. Prevalence of and risk factors for asthma among people aged 45 and older in China: a cross-sectional study. BMC Pulm. Med. 21, 311. https://doi.org/10.1186/s12890-021-01664-7 (2021).
Yu, J., Xu, L., Han, A. & Xie, M. The epidemiology of asthma in Mainland China: a systematic review and meta-analysis. BMC Public. Health 24, 2888. https://doi.org/10.1186/s12889-024-20330-1 (2024).
Barosova, R., Baranovicova, E., Hanusrichterova, J. & Mokra, D. Metabolomics in Animal models of Bronchial Asthma and its translational importance for clinics. Int. J. Mol. Sci. 25, 586. https://doi.org/10.3390/ijms25010459 (2023).
Zhang, Y., Yin, X. & Zheng, X. The relationship between PM2.5 and the onset and exacerbation of childhood asthma: a short communication. Front. Pediatr. 11, 1191852. https://doi.org/10.3389/fped.2023.1191852 (2023).
Akar-Ghibril, N., Casale, T., Custovic, A. & Phipatanakul, W. Allergic endotypes and phenotypes of Asthma. J. Allergy Clin. Immunol.: Pract. 8, 429–440. https://doi.org/10.1016/j.jaip.2019.11.008 (2020).
Teodorescu, M. et al. Asthma Control and its relationship with obstructive sleep apnea (OSA) in older adults. Sleep Disord. 2013, 251567. https://doi.org/10.1155/2013/251567 (2013).
Thakur, V. R., Khuman, V., Beladiya, J. V., Chaudagar, K. K. & Mehta, A. A. An experimental model of asthma in rats using ovalbumin and lipopolysaccharide allergens. Heliyon 5, e02864. https://doi.org/10.1016/j.heliyon.2019.e02864 (2019).
Russjan, E. & Kaczyńska, K. Murine models of hapten-induced asthma. Toxicology 410, 41–48. https://doi.org/10.1016/j.tox.2018.09.001 (2018).
Li, W. J. et al. Lipid metabolism in asthma: Immune regulation and potential therapeutic target. Cell. Immunol. 364, 104341. https://doi.org/10.1016/j.cellimm.2021.104341 (2021).
Takayama, G. et al. A novel component of subepithelial fibrosis of bronchial asthma downstream of IL-4 and IL-13 signals. J. Allergy Clin. Immunol. 118, 98–104. https://doi.org/10.1016/j.jaci.2006.02.046 (2006). Periostin.
Woodruff, P. G. et al. T-helper type 2–driven inflammation defines major subphenotypes of Asthma. Am. J. Respir. Crit Care Med. 180, 388–395. https://doi.org/10.1164/rccm.200903-0392OC (2009).
Huang, A. X., Lu, L. W., Liu, W. J. & Huang, M. Plasma inflammatory cytokine IL-4, IL-8, IL-10, and TNF-α levels correlate with pulmonary function in patients with Asthma-Chronic Obstructive Pulmonary Disease (COPD) Overlap Syndrome. Med. Sci. Monit. 22, 2800–2808. https://doi.org/10.12659/msm.896458 (2016).
Zhou, T. et al. Associations between Th17-related inflammatory cytokines and asthma in adults: a case-control study. Sci. Rep. 7, 15502. https://doi.org/10.1038/s41598-017-15570-8 (2017).
Shankar, A., McAlees, J. W. & Lewkowich, I. P. Modulation of IL-4/IL-13 cytokine signaling in the context of allergic disease. J. Allergy Clin. Immunol. 150, 266–276. https://doi.org/10.1016/j.jaci.2022.06.012 (2022).
Xian, Z. et al. Effects of imperatorin on airway remodelling in asthmatic mice through TGF-β1/Smad3 and PI3K/Akt signaling pathways. Chin. Pharmacol. Bull. 34, 1719–1724 (2018).
Al-Alawi, M., Hassan, T. & Chotirmall, S. H. Transforming growth factor β and severe asthma: a perfect storm. Respir. Med. 108, 1409–1423. https://doi.org/10.1016/j.rmed.2014.08.008 (2014).
Impellizzieri, D. et al. IL-4 receptor engagement in human neutrophils impairs their migration and extracellular trap formation. J. Allergy Clin. Immunol. 144, 267–279. https://doi.org/10.1016/j.jaci.2019.01.042 (2019). .e264.
Maitre, B. et al. Vascular endothelial growth factor synthesis in the acute phase of experimental and clinical lung injury. Eur. Respir. J. 18, 100–106. https://doi.org/10.1183/09031936.01.00074701 (2001).
Zhu, X. et al. The role of T cells and macrophages in asthma pathogenesis: a new perspective on mutual crosstalk. Mediat. Inflamm. 2020, 7835284 (2020). https://doi.org/10.1155/2020/7835284 (2020).
Li, X. M., Peng, J., Gu, W. & Guo, X. J. TCDD-Induced activation of Aryl Hydrocarbon receptor inhibits Th17 polarization and regulates non-eosinophilic Airway inflammation in Asthma. PLoS One 11, e0150551. https://doi.org/10.1371/journal.pone.0150551 (2016).
Murray, P. J. et al. Macrophage activation and polarization: nomenclature and experimental guidelines. Immunity 41, 14–20. https://doi.org/10.1016/j.immuni.2014.06.008 (2014).
Murray, P. J. Macrophage polarization. Annu. Rev. Physiol. 79, 541–566. https://doi.org/10.1146/annurev-physiol-022516-034339 (2017).
Mantovani, A. et al. The chemokine system in diverse forms of macrophage activation and polarization. Trends Immunol. 25, 677–686. https://doi.org/10.1016/j.it.2004.09.015 (2004).
Gordon, S. Alternative activation of macrophages. Nat. Rev. Immunol. 3, 23–35. https://doi.org/10.1038/nri978 (2003).
Jiang, Y. et al. Classification of non-acute bronchial asthma according to allergy and eosinophil characteristics: a retrospective study. Allergy Asthma Clin. Immunol. 17, 89. https://doi.org/10.1186/s13223-021-00546-1 (2021).
Bosco, M. C. Macrophage polarization: reaching across the aisle? J. Allergy Clin. Immunol. 143, 1348–1350. https://doi.org/10.1016/j.jaci.2018.12.995 (2019).
Karta, M. R. et al. LPS modulates rhinovirus-induced chemokine secretion in monocytes and macrophages. Am. J. Respir Cell. Mol. Biol. 51, 125–134. https://doi.org/10.1165/rcmb.2013-0404OC (2014).
Baines, K. J., Simpson, J. L., Bowden, N. A., Scott, R. J. & Gibson, P. G. Differential gene expression and cytokine production from neutrophils in asthma phenotypes. Eur. Respir J. 35, 522–531. https://doi.org/10.1183/09031936.00027409 (2010).
Quaedvlieg, V., Henket, M., Sele, J. & Louis, R. Cytokine production from sputum cells in eosinophilic versus non-eosinophilic asthmatics. Clin. Exp. Immunol. 143, 161–166. https://doi.org/10.1111/j.1365-2249.2005.02968.x (2006).
Gould, H. J. et al. The biology of IGE and the basis of allergic disease. Annu. Rev. Immunol. 21, 579–628. https://doi.org/10.1146/annurev.immunol.21.120601.141103 (2003).
Pillai, P. et al. Allergen-specific IgE is not detectable in the bronchial mucosa of nonatopic asthmatic patients. J Allergy Clin Immunol 133, 1770–1772 e1711. https://doi.org/10.1016/j.jaci.2014.03.027 (2014).
Ahlborg, N., Ling, I. T., Holder, A. A. & Riley, E. M. Linkage of exogenous T-cell epitopes to the 19-kilodalton region of Plasmodium Yoelii merozoite surface protein 1 (MSP1(19)) can enhance protective immunity against malaria and modulate the immunoglobulin subclass response to MSP1(19). Infect. Immun. 68, 2102–2109. https://doi.org/10.1128/IAI.68.4.2102-2109.2000 (2000).
Benson, R. C., Hardy, K. A. & Morris, C. R. Arginase and arginine dysregulation in asthma. J. Allergy (Cairo). 2011, 736319. https://doi.org/10.1155/2011/736319 (2011).
Michalaki, C., Albers, G. J. & Byrne, A. J. Itaconate as a key regulator of respiratory disease. Clin. Exp. Immunol. 215, 120–125. https://doi.org/10.1093/cei/uxad127 (2024).
Goretzki, A., Zimmermann, J., Rainer, H., Lin, Y. J. & Schülke, S. Immune metabolism in TH2 responses: new opportunities to improve allergy treatment—disease-specific findings (part 1). Curr. Allergy Asthma Rep. 23, 29–40. https://doi.org/10.1007/s11882-022-01057-8 (2023).
Luo, J. et al. Metabolism characteristics of Mycoplasma pneumoniae infection in Asthmatic Children. Allergy Asthma Immunol. Res. 14, 713–729. https://doi.org/10.4168/aair.2022.14.6.713 (2022).
Xu, S., Panettieri, R. A. Jr. & Jude, J. Metabolomics in asthma: a platform for discovery. Mol. Aspects Med. 85, 100990. https://doi.org/10.1016/j.mam.2021.100990 (2022).
Ho, W. E. et al. Metabolomics reveals altered metabolic pathways in experimental asthma. Am. J. Respir. Cell Mol. Biol. 48, 204–211. https://doi.org/10.1165/rcmb.2012-0246OC (2013).
Wei, H. et al. Mechanisms of exacerbation of Th2-mediated eosinophilic allergic asthma induced by plastic pollution derivatives (PPD): a molecular toxicological study involving lung cell ferroptosis and metabolomics. Sci. Total Environ. 946, 174482. https://doi.org/10.1016/j.scitotenv.2024.174482 (2024).
Keegan, A. D., Leonard, W. J. & Zhu, J. Recent advances in understanding the role of IL-4 signaling. Fac. Rev. 10, 71. https://doi.org/10.12703/r/10-71 (2021).
Rohatgi, N. et al. Biochemical characterization of human gluconokinase and the proposed metabolic impact of Gluconic Acid as determined by Constraint Based Metabolic Network Analysis. PLOS ONE 9, e98760. https://doi.org/10.1371/journal.pone.0098760 (2014).
Chen, F. et al. Citraconate inhibits ACOD1 (IRG1) catalysis, reduces interferon responses and oxidative stress, and modulates inflammation and cell metabolism. Nat. Metabolism 4, 534–546. https://doi.org/10.1038/s42255-022-00577-x (2022).
Shi, X. et al. The signaling pathways and therapeutic potential of itaconate to alleviate inflammation and oxidative stress in inflammatory diseases. Redox Biol. 58, 102553. https://doi.org/10.1016/j.redox.2022.102553 (2022).
Zuo, M. et al. IL4I1-catalyzed tryptophan metabolites mediate the anti-inflammatory function of cytokine-primed human muscle stem cells. Cell. Death Discovery 9, 269. https://doi.org/10.1038/s41420-023-01568-x (2023).
Li, M. M., Jiang, Z., Song, L. Y., Quan, Z. S. & Yu, H. L. Antidepressant and anxiolytic-like behavioral effects of erucamide, a bioactive fatty acid amide, involving the hypothalamus–pituitary–adrenal axis in mice. Neurosci. Lett. 640, 6–12. https://doi.org/10.1016/j.neulet.2016.12.072 (2017).
Kazmi, I. et al. Review of the potential pharmacological role of erucic acid: a monounsaturated omega-9 fatty acid. Naunyn. Schmiedebergs Arch. Pharmacol. 397, 3663–3674. https://doi.org/10.1007/s00210-023-02875-x (2024).
Seminotti, B., da Silva, J. C., Ribeiro, R. T., Leipnitz, G. & Wajner, M. Free radical scavengers prevent argininosuccinic acid-Induced oxidative stress in the brain of developing rats: a new adjuvant therapy for argininosuccinate lyase deficiency? Mol. Neurobiol. 57, 1233–1244. https://doi.org/10.1007/s12035-019-01825-0 (2020).
Morris, C. R. Arginine and asthma. Nestle Nutr. Inst. Workshop 77, 1–15. https://doi.org/10.1159/000351365 (2013).
Maes, K., Serré, J., Mathyssen, C., Janssens, W. & Gayan-Ramirez, G. Targeting vitamin D deficiency to limit exacerbations in respiratory diseases: utopia or strategy with potential? Calcif. Tissue Int. 106, 76–87. https://doi.org/10.1007/s00223-019-00591-4 (2020).
Camargo, C. A. et al. Effect of monthly vitamin D supplementation on preventing exacerbations of asthma or chronic obstructive pulmonary disease in older adults: post Hoc analysis of a randomized controlled trial. Nutrients 13, 859 (2021).
Minton, K. Vitamin D shuts down T cell-mediated inflammation. Nat. Rev. Immunol. 22, 1–1. https://doi.org/10.1038/s41577-021-00663-3 (2022).
Guo, J. et al. The temporal characteristics of the disruption of gut microbiota, serum metabolome, and cytokines by silica exposure in Wistar rats. Ecotoxicol. Environ. Saf. 252, 114580. https://doi.org/10.1016/j.ecoenv.2023.114580 (2023).
Zhao, L. et al. PM(2.5) exposure promotes asthma in aged Brown-Norway rats: implication of multiomics analysis. Ecotoxicol. Environ. Saf. 263, 115393. https://doi.org/10.1016/j.ecoenv.2023.115393 (2023).
Acknowledgements
We are grateful for the untargeted metabolomics analysis service for plasma provided by Shanghai Applied Protein Technology.
Funding
This research was supported by the National Natural Science Foundation of China (82070103), the National Key R&D Program of China (2022YFF0710803, 2021YFF0703400) and the CAMS Innovation Fund for Medical Science (CIFMS, 2021-I2M-1-036), Fundamental Research Funds for the Central Universities (3132023528) and the Nonprofit Central Research Institute Fund of the Chinese Academy of Medical Sciences, grant numbers 2023-PT180-01.
Author information
Authors and Affiliations
Contributions
Lianlian Zhao: Methodology, Investigation, Writing – original draft, Data curation.Xiaoling Ding: Formal analysis, interpreted the data and collected references.Li Zhou: Performed the experiments; analyzed and interpreted the data.Chenchen Song performed the experiments.Taisheng Kang: Performed the experiments.Yanfeng Xu analyzed and interpreted the data.Yunpeng Liu performed the experiments.Yunlin Han: Performed the experiments.Wenjie Zhao performed the experiments.Boxiang Zhang: Performed correlation analysis and construct correlation matrixDan Xu: Funding acquisition, supervision, and writing-review editing.Jianguo Guo: Conceptualization, Funding acquisition, Project administration, Supervision, Writing-review editing.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The Institute of Laboratory Animal Sciences, Chinese Academy of Medical Sciences & Peking Union Medical College’s Institutional Animal Care and Use Committee approved this study (approval no. QC 20012) and agreed to carry out relevant animal experiments. In the course of the experiment, to ensure the implementation of the experimental animal welfare, ethical measures were taken. The study is reported in accordance with ARRIVE guidelines.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhao, L., Ding, X., Zhou, L. et al. Effect of PM2.5 exposure on susceptibility to allergic asthma in elderly rats treated with allergens. Sci Rep 15, 5594 (2025). https://doi.org/10.1038/s41598-025-90261-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-90261-3