Abstract
Acute appendicitis is a common condition requiring surgical intervention, with a lifetime risk of 7–8%. Differentiating between uncomplicated and complicated appendicitis is essential for appropriate treatment and improved patient outcomes. This study aimed to utilize minimal, non-invasive data to distinguish between these forms of appendicitis, using advanced analytical methods for faster and more precise diagnosis. This retrospective study analyzed acute appendicitis cases from January 2018 to December 2022 at a tertiary care hospital. Data were gathered from 3,045 patients, including demographic details, clinical features, laboratory tests (Red Cell Distribution Width [RDW] and Mean Platelet Volume [MPV]), and imaging results. Patients were classified as having uncomplicated or complicated appendicitis based on surgical and histopathological findings. Statistical analyses, including multivariate logistic regression and ROC curve analyses, were performed using SPSS. Complicated appendicitis was defined based on surgical findings and histopathological criteria, including perforation, abscess formation, or gangrene. Uncomplicated appendicitis was defined as inflammation confined to the appendix without evidence of perforation or abscess. The study population comprised 1,869 males (61.37%) and 1,176 females (38.62%), with a mean age of 36.4 years. The mean RDW was 27.81%, and the mean MPV was 8.68 fL. Among the appendectomy cases, 50.7% were acute appendicitis, 10.3% were negative appendectomies, and 38.9% had complicated appendicitis. RDW was significantly higher in acute appendicitis than in negative cases (t = 2.45, p = 0.02) and even higher in complicated cases (t = 3.78, p = 0.001). MPV was highest in complicated appendicitis, consistent with increased inflammation severity (t = 2.56, p = 0.01). The sensitivity and specificity of RDW for identifying complicated appendicitis were 0.85 and 0.75, respectively, and for MPV, they were 0.80 and 0.70. Univariate logistic regression identified male sex and appendix diameter as significant predictors of complicated appendicitis. In multivariate analysis, appendix diameter remained significant (p = 0.01), and male sex approached significance (p = 0.06). The optimal cutoff for appendix diameter to differentiate appendicitis types was 10 mm, with an AUC of 0.82. RDW, MPV, and appendix diameter provide a reliable method for distinguishing between uncomplicated and complicated appendicitis. Combining these biomarkers enhances diagnostic accuracy and enables precise risk stratification for better patient management.
Similar content being viewed by others
Introduction
Acute appendicitis is one of the most common causes of acute abdominal pain, and it requires surgical intervention. With a lifetime risk of approximately 7–8%, appendicitis represents a significant global healthcare concern. It is most prevalent in individuals aged 10–30 years, although it can occur at any age1. The condition is characterized by inflammation of the appendix, a small tube-like organ attached to the large intestine, which can lead to severe complications if not promptly treated2.
The prevalence of acute appendicitis varies worldwide but remains consistently high in developed countries. Approximately 300,000 appendectomies are performed annually in the United States alone. The male-to-female ratio was approximately 1.4:1, with males having a slightly higher incidence. Notably, the incidence of appendicitis tends to be lower in non-white populations, suggesting that genetic and environmental factors play a role in its development3.
Early and accurate diagnosis of acute appendicitis is crucial to prevent complications, such as perforation, which can lead to peritonitis and sepsis. The clinical diagnosis of appendicitis is often challenging because of the overlap of its symptoms with those of other abdominal conditions4. Typical symptoms include right lower quadrant pain, nausea, vomiting, and fever; however, these can vary significantly among patients. The accuracy of clinical diagnosis without supportive imaging is reported to be approximately 75–80%, which underscores the need for reliable diagnostic tools.
Distinguishing between uncomplicated and complicated appendicitis is vital to determine an appropriate treatment strategy. Uncomplicated appendicitis, characterized by inflammation confined to the appendix without perforation, can often be managed with antibiotics alone and, in some cases, may resolve spontaneously. In contrast, complicated appendicitis, which involves perforation, abscess formation, or generalized peritonitis, typically requires urgent surgical interventions5.
The differentiation between these two forms is essential because it guides clinical decision-making and affects patient outcomes. Misclassification can lead to unnecessary surgery or delayed treatment, increasing the risk of complications. RDW and MPV were chosen as the focus of this study due to emerging evidence suggesting their association with inflammatory and thrombotic processes, which are critical in appendicitis pathophysiology. RDW reflects red blood cell distribution changes due to systemic inflammation, while MPV indicates platelet activation, a key component of the immune response6. Despite advancements in imaging techniques and biomarker research, the accurate differentiation of appendicitis severity remains a significant clinical challenge. Current diagnostic approaches include clinical scoring systems, laboratory tests, and imaging modalities such as ultrasonography, computed tomography (CT), and magnetic resonance imaging (MRI)7.
Acute appendicitis is a prevalent condition with significant implications for patient health and the healthcare system. Early and easy minimally invasive diagnosis is critical to prevent complications. Ongoing research is aimed at improving the accuracy of distinguishing between uncomplicated and complicated appendicitis by exploring advanced analytical methods.
Materials and methods
Study design and setting
This study was a retrospective analysis of acute appendicitis cases over a five-year period from January 2018 to December 2022. Data were collected from a single tertiary care hospital, ensuring a consistent and controlled clinical environment.
Ethics approval
Since our study is retrospective, human ethics and consent to participate were not required from individual participants, and patient confidentiality was strictly maintained. Ethics approval for this study was obtained from the Ethics Committee of HaydarpaşaNumune Training and Research Hospital (Approval Number: 247665561/07.2024). Informed consent was waived by the HaydarpaşaNumuneEğitimveAraştırmaHastanesi Ethics Committee as the study was retrospective.
Patient selection
The study included patients diagnosed with acute appendicitis who underwent surgical intervention between January 2018 and December 2022. Patients with incomplete medical records, missing laboratory data (e.g., RDW, MPV), or unavailable imaging results were excluded (n = 455). These exclusions were necessary to ensure data accuracy but may introduce selection bias by limiting the sample to cases with complete documentation. The diagnosis was based on clinical evaluation, laboratory tests, and imaging studies. Cases were categorized as uncomplicated or complicated appendicitis based on surgical findings and postoperative histopathological reports. Exclusion criteria included patients with incomplete medical records, those with alternative diagnoses that were initially suspected of appendicitis, and those who did not undergo surgery or were lost to follow-up.
Data collection
The following parameters were collected from electronic medical records:
Demographic Data: Age, sex, and ethnicity. Clinical Features: Symptoms at presentation, duration of symptoms, and physical examination findings. Imaging Findings: Results of ultrasound, CT tomography, and MRI where applicable. Ultrasonography was the primary imaging modality used to measure appendix diameter. In cases where ultrasound findings were inconclusive, CT was employed for confirmation. Measurements were standardized, and inter-observer reliability was maintained by ensuring that all imaging was reviewed by experienced radiologists. Appendix diameter measurements were analyzed to determine their diagnostic accuracy for complicated appendicitis. A receiver operating characteristic (ROC) curve analysis was performed to identify the optimal cutoff value for diagnosing appendicitis severity. The area under the curve (AUC) was calculated to assess the performance of this marker. Surgical Findings: Patients were classified as having uncomplicated or complicated appendicitis based on clinical, surgical, and histopathological findings. Uncomplicated appendicitis was defined as inflammation confined to the appendix without evidence of perforation or abscess. Complicated appendicitis included cases with perforation, abscess formation, or gangrene as identified during surgery or confirmed histopathologically.
Laboratory Tests: Red Cell Distribution Width (RDW) and Mean Platelet Volume (MPV) were the primary laboratory values analyzed in this study, as they were identified as potential non-invasive markers for predicting appendicitis severity. Other laboratory values such as white blood cell count (WBC), neutrophil-to-lymphocyte ratio (NLR), and C-reactive protein (CRP) were also collected; however, these were not included in the current analysis due to our focus on novel and less commonly studied markers. If required, additional analysis for these variables can be provided as supplementary material.
Statistical analysis
Continuous variables are expressed as mean ± standard deviation (SD) or medians with interquartile ranges (IQR), as appropriate. Categorical variables are summarized as frequencies and percentages. Differences between the groups (uncomplicated vs. complicated appendicitis) were assessed using the chi-square test or Fisher’s exact test for categorical variables. For continuous variables, comparisons were made using the independent samples t-test or Mann–Whitney U test, depending on the normality of the data distribution.
Multivariate logistic regression analysis was conducted to identify independent predictors of complicated appendicitis. Variables with a p-value < 0.05 in univariate analysis were included in the multivariate model. Results are presented as coefficients, standard errors, z-values, p-values, odds ratios (OR), and 95% confidence intervals (CI).
Receiver Operating Characteristic (ROC) curve analysis was performed to identify the optimal cutoff values for RDW and MPV in predicting complicated appendicitis. The area under the curve (AUC) was calculated to assess diagnostic accuracy, and sensitivity and specificity values were recorded for each threshold. The optimal cutoff values were determined using the Youden index.
Statistical analyses were performed using SPSS, with significance set at p < 0.05. Handling of missing data was addressed by conducting a complete case analysis to ensure consistency and reliability of the results. Variables for multivariate analysis were selected based on univariate analysis with a significance threshold of p < 0.10. Model validation included tests for multicollinearity, assessment of goodness-of-fit using the Hosmer-Lemeshow test, and evaluation of logistic regression assumptions. These steps were implemented to ensure the robustness and accuracy of the statistical models used.
Ethical considerations
The study protocol was reviewed and approved by the Institutional Review Board of Haydarpasa Research and Traning Hospital, 247,665,561, 03.07.2024. Patient confidentiality was maintained by anonymizing the data. Given the retrospective nature of the study, the requirement for informed consent was waived by the IRB.All methods in this study were performed in accordance with the relevant guidelines and regulations, as approved by the HaydarpaşaResearch and Training Hospital Ethics Committee. The study adhered to the principles outlined in the Declaration of Helsinki.
Results.
Demographic and frequency data of the patients
The research examined the outcomes of 3045 cases, comprised of 1869 males (61.37%) and 1176 females (38.62%). The average age was 36.40 years, 15–80 years). The mean RDW was 27.81% (range, 14.7–44.2%). The average MPV was 8.68 femtoliters (fL) (ranging from 6.6 to 10.3 fL). The mean appendix diameter was 8.70 mm (ranging, 6.0 to 15.0 mm).
The diagnostic distribution post-surgery for 3045 appendectomy cases revealed the following: acute appendicitis was diagnosed in 1544 cases, representing 50.7% of the total, with a sex distribution of 782 males (50.7%) and 762 females (49.3%). Negative appendectomy was found in 314 patients (10.3%), including 162 males (51.6%) and 152 females (48.4%). A complicated perforated appendix was observed in 1187 cases, accounting for 38.9% of the cases, with 644 males (54.3%) and 543 females (45.7%). In the multivariate logistic regression analysis, male gender showed a trend toward being a risk factor for complicated appendicitis (p = 0.06), but this did not reach statistical significance.
The comparison of RDW and MPV across different pathology groups
For 3045 appendectomy cases, when examining the RDW and MPV values according to diagnosis, it was found that the highest MPV value was in the complicated group, while the lowest RDW value was observed in the negative patient group. The RDW and MPV values according to acute appendicitis diagnosis are presented in Table 1.
The study revealed that RDW was significantly higher in acute appendicitis than in negative appendicitis (t = 2.45, p = 0.02) and even more so when comparing acute appendicitis to complicated cases (t = 3.78, p = 0.001). MPV was highest in the complicated appendicitis group, consistent with increased inflammation severity (t = 2.56, p = 0.01). Although the difference in MPV between acute and negative appendicitis approached statistical significance (t = 1.89, p = 0.06), it did not reach the conventional threshold for statistical significance. The results are presented in Table 1.
The statistical comparison of Red Cell Distribution Width (RDW) and Mean Platelet Volume (MPV) between different types of appendicitis reveals significant findings. RDW values were notably higher in acute appendicitis compared to negative appendectomy cases, indicating its potential as a marker for acute inflammation. Additionally, RDW was significantly elevated in complicated appendicitis cases compared to both acute appendicitis and negative appendectomy, suggesting its effectiveness in identifying more severe cases. MPV also showed significant differences between complicated and acute appendicitis, as well as between complicated and negative appendectomy cases, though its role was less pronounced than RDW. Overall, the results suggest that RDW, and to a lesser extent MPV, can be useful biomarkers for distinguishing between uncomplicated and complicated appendicitis. The results are presented in Table 2.
The ROC curve analysis identified a cutoff value of 12 for RDW, which demonstrated a sensitivity of 85% and specificity of 75% for detecting complicated appendicitis (AUC = 0,82). Similarly, a cutoff value of 9 for MPV showed a sensitivity of 80% and specificity of 70% (AUC = 0,78). These thresholds were determined as the optimal points for distinguishing complicated appendicitis (Table 3).
Logistic regression analysis of predictors for complicated appendicitis
Univariate logistic regression analysis identified factors that were significantly associated with complicated appendicitis. Sex (male) and appendix diameter showed a significant association with a coefficient of 0.57, a standard error of 0.27, a z-value of 2.12, and a (p = 0.03, p = 0.01, respectively). The odds ratios and 95% confidence intervals for each variable are listed in Table 4.
Multivariate logistic regression analysis identified independent predictors of complicated appendicitis. Gender (male) remained a significant predictor with a coefficient of 0.52, standard error of 0.28, z-value of 1.87, and p-value of 0.06, approaching the threshold for significance. Appendix diameter remained a significant predictor (p = 0.01). The odds ratios and 95% confidence intervals for each variable are listed in Table 5.
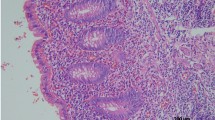
Diagnostic performance of appendix diameter in differentiating appendicitis types
The analysis of appendix diameter for distinguishing between acute appendicitis and complicated appendicitis identified an optimal cutoff value of 10 mm. The sensitivity or true-positive rate was approximately 0.80, indicating a high probability of correctly identifying cases of complicated appendicitis. The specificity or true negative rate was approximately 0.70, suggesting a moderate ability to correctly identify noncomplicated cases. The area under the ROC curve (AUC) was 0.82, reflecting the good overall performance of appendix diameter as a diagnostic tool (Fig. 1).
Discussion.
This study highlights the critical roles of RDW and MPV as valuable biomarkers for differentiating between uncomplicated and complicated appendicitis. In addition, the identification of male sex and appendix diameter as significant predictors of complicated appendicitis can be incorporated into clinical decision-making algorithms. This can enhance the early identification of patients at risk for complicated appendicitis, facilitate timely and appropriate interventions, and potentially reduce the incidence of adverse outcomes such as perforation and abscess formation.
The use of RDW and MPV as part of a diagnostic algorithm could facilitate quicker and more accurate identification of patients at risk of complicated appendicitis. The results demonstrated that RDW values were significantly higher in patients with acute appendicitis than in those without appendicitis. Furthermore, RDW values were even higher in patients with complicated appendicitis, indicating a progressive increase in RDW with the severity of appendicitis. This finding is consistent with those of previous studies, such as those by Krzyzak and Mulrooney1, which suggest that inflammation and subsequent changes in red cell distribution are more pronounced in complicated cases.
The MPV values followed a similar trend, with the highest values observed in complicated appendicitis cases. This indicates that platelet activation and volume increase as the severity of the condition increases. The notable difference in MPV between acute and complicated appendicitis supports the potential utility of MPV as a marker of appendicitis severity. Although the difference in MPV between acute and negative appendicitis approached statistical significance, it did not meet the conventional threshold, suggesting that MPV may be more sensitive to the severity of inflammation than the presence of appendicitis alone. This is contrary to some studies that claim MPV values ineffective in distinguishing the complicated and uncomplicated form of appendicitis8,9.
Statistical analysis revealed that RDW and MPV have substantial diagnostic value, with sensitivity and specificity values supporting their use in clinical settings. An RDW threshold of 12 and an MPV threshold of 9 provided good sensitivity and specificity for identifying complicated appendicitis, making these biomarkers useful tools for early diagnosis and risk stratification.
These findings align with existing literature that underscores the importance of appendix diameter in appendicitis evaluation5,10. Larger appendix diameters are consistently associated with a higher risk of complications, reinforcing the validity of this metric as a diagnostic criterion. The ROC curve further supports the utility of appendix diameter, providing a visual representation of its diagnostic performance and the trade-offs between sensitivity and specificity.
Univariate logistic regression analysis identified male sex and appendix diameter as the significant predictors of complicated appendicitis. Specifically, being male was associated with an increased risk of complicated appendicitis, and an OR of 1.76 further highlights the increased likelihood of complicated appendicitis in male patients. Additionally, appendix diameter was found to be a significant predictor, with an OR of 1.20, suggesting that larger appendix diameters are strongly associated with complicated appendicitis. In contrast, age, RDW, and MPV were not significantly associated in univariate analysis. Although RDW and MPV are valuable biomarkers, their predictive power for complicated appendicitis was not significant in this model, with p-values of 0.80 and 0.38, respectively.
Multivariate logistic regression analysis was performed to identify the independent predictors of complicated appendicitis by controlling for potential confounders. In this analysis, male sex and appendix diameter remained as significant predictors. Male sex approached significance, indicating that it was a near-significant independent predictor of complicated appendicitis. Appendix diameter is a robust predictor. These findings suggest that larger appendix diameter is a consistent and significant independent predictor of complicated appendicitis, underscoring the importance of accurate imaging and measurement in clinical practice. The persistent significance of the male sex in the multivariate analysis also highlights the potential role of sex-specific biological factors in the progression of appendicitis.
Identification of male sex and appendix diameter as significant predictors of complicated appendicitis has important clinical implications. While male gender showed a trend toward being associated with complicated appendicitis (p = 0.06), this finding did not achieve statistical significance. This suggests that while there may be a possible association, further studies are needed to confirm this relationship. These factors can be incorporated into clinical decision-making algorithms to enhance the early identification of patients at risk of complicated appendicitis. This, in turn, can facilitate timely and appropriate interventions, potentially reducing the incidence of adverse outcomes, such as perforation and abscess formation.
Additionally, the findings underscore the importance of using a combination of demographic, clinical, and imaging data to improve the diagnostic accuracy. Although RDW and MPV are useful biomarkers, their predictive value may be enhanced when combined with other significant predictors, such as appendix diameter. This combined approach can enhance patient outcomes by providing timely and appropriate treatment strategies.
The diagnostic performance of appendix diameter in distinguishing between uncomplicated and complicated appendicitis was a key finding of this study. The analysis revealed that an optimal cutoff value of 10 mm for the appendix diameter can significantly aid in the differentiation process, with notable implications for clinical practice.
ROC curve analysis demonstrated good overall diagnostic accuracy. High sensitivity is crucial for ensuring that patients with complicated appendicitis receive timely and appropriate intervention, thereby reducing the risk of severe complications, such as perforation and peritonitis. The specificity indicated a moderate ability to correctly identify non-complicated appendicitis cases, which is equally important for avoiding unnecessary surgical interventions. The specificity value suggests that 70% of patients without complicated appendicitis were correctly classified, reducing the likelihood of overtreatment and its associated risks. The use of the appendix diameter as a diagnostic tool is advantageous because of its non-invasive nature and ease of measurement through imaging modalities such as ultrasound and CT scans. Incorporating appendix diameter into clinical protocols can enhance the accuracy of appendicitis diagnosis and help in stratifying patients based on the severity of their condition. These findings align with existing literature that underscores the importance of appendix diameter in appendicitis evaluation11,12. Larger appendix diameters are consistently associated with a higher risk of complications, reinforcing the validity of this metric as a diagnostic criterion. The ROC curve further supports the utility of appendix diameter, providing a visual representation of its diagnostic performance and the trade-offs between sensitivity and specificity. For instance, studies by Teng et al.2 and Di Saverio et al.3 have similarly highlighted the role of imaging in improving diagnostic accuracy and aiding in the differentiation of appendicitis severity. These studies support the integration of appendix diameter measurements into routine clinical practice for improved patient management.
Study limitations
This study has several limitations. First, the retrospective design may introduce selection bias, as cases with incomplete data were excluded (n = 455). This could limit the generalizability of the findings to all patients with appendicitis. Second, the reliance on medical records for data collection poses a risk of information bias, as some variables may not have been consistently documented. Third, confounding factors such as the timing of symptom onset, blood sample collection, and surgery were not uniformly recorded and may influence outcomes. Future prospective studies should address these limitations by employing standardized data collection protocols and including a broader patient population to enhance generalizability.
Future research directions
The findings of this study provide a foundation for further exploration of non-invasive biomarkers, such as RDW and MPV, in the assessment of appendicitis severity. Future prospective studies and randomized controlled trials are recommended to validate the diagnostic accuracy of these markers and their integration into clinical workflows. Additionally, the role of appendix diameter, as measured by imaging modalities, warrants further investigation in larger, diverse populations to confirm its predictive value. Combining these biomarkers with established clinical scoring systems, such as the Alvarado score, may improve diagnostic precision and decision-making in both high- and low-resource settings. Moreover, longitudinal studies assessing the impact of these tools on patient outcomes and healthcare costs could offer valuable insights into their practical utility.
Conclusion
This study sheds light on the diagnostic potential of RDW, MPV, and appendix diameter in differentiating between uncomplicated and complicated appendicitis. Incorporating these biomarkers into clinical guidelines can improve the accuracy and efficiency of appendicitis management, ultimately leading to improved patient outcomes. RDW values exceeding 12 indicate good sensitivity and specificity for detecting complicated appendicitis, making it a reliable marker for distinguishing between the two types of appendicitis. Additionally, an MPV value of 9 provides sensitivity and specificity for identifying complicated appendicitis, with higher MPV values indicating increased severity of inflammation. Finally, an optimal cutoff value of 10 mm for appendix diameter is effective in differentiating between uncomplicated and complicated appendicitis, with larger diameters associated with a higher risk of complications.
Combining these biomarkers improves the diagnostic accuracy. While RDW and MPV offer significant diagnostic value individually, their predictive power is further enhanced when combined with appendix diameter measurements. This multimodal approach enables more precise risk stratification and timely intervention, potentially reducing the likelihood of adverse outcomes such as perforation and abscess formation. To incorporate these findings into clinical practice, clinicians can use the RDW, MPV, and appendix diameter as part of a diagnostic algorithm to quickly and accurately identify patients at risk of complicated appendicitis. This integration supports clinical decision making, helps avoid unnecessary surgeries, and ensures that patients receive appropriate care promptly.
Data availability
Dr.Mehmet Torune-mail: [email protected] (In case of any queries or requests for data related to this study, please contact).
References
Krzyzak, M. & Mulrooney, S. M. Acute appendicitis review: background, epidemiology, diagnosis, and treatment. Cureus 12(6) (2020).
Teng, T. Z. J., Thong, X. R., Lau, K. Y., Balasubramaniam, S. & Shelat, V. G. Acute appendicitis—advances and controversies. World J. Gastrointest. Surg. 13 (11), 1293 (2021).
Di Saverio, S. et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J. Emerg. Surg. 15, 1–42 (2020).
Akbulut, S. et al. An investigation into the factors predicting acute appendicitis and perforated appendicitis. Turk. J. Trauma. Emerg. Surg. /Ulusal Travma ve Acil Cerrahi Dergisi 27 (4) (2021).
Skjold-Ødegaard, B. & Søreide, K. The diagnostic differentiation challenge in acute appendicitis: how to distinguish between uncomplicated and complicated appendicitis in adults. Diagnostics 12 (7), 1724 (2022).
Nacenta, S. B., Sanz, L. I., Lucas, R. S., Depetris, M. & Chamorro, E. M. Update on acute appendicitis: typical and untypical findings. Radiología (English Edition) 65, S81–S91 (2023).
Erkent, M., Karakaya, E. & Yücebaş, S. C. A new approach to the management of acute appendicitis: decision tree method. Am. J. Emerg. Med. 54, 142–146 (2022).
Lietzén, E. et al. Is preoperative distinction between complicated and uncomplicated acute appendicitis feasible without imaging? Surgery 160 (3), 789–795 (2016).
Beecher, S. M., Hogan, J., O’Leary, D. P. & McLaughlin, R. An appraisal of inflammatory markers in distinguishing acute uncomplicated and complicated appendicitis. Dig. Surg. 33 (3), 177–181 (2016).
Kim, T. H. et al. Predictive factors to distinguish between patients with non-complicated appendicitis and those with complicated appendicitis. Ann. Coloproctol. 31 (5), 192 (2015).
Geerdink, T. et al. Validation of a scoring system to distinguish uncomplicated from complicated appendicitis. J. Surg. Res. 258, 231–238 (2021).
Echevarria, S. et al. Typical and atypical presentations of appendicitis and their implications for diagnosis and treatment: a literature review. Cureus 15 (4) (2023).
Funding
We wish to confirm that no funding was received for this work from any organization, grant, or other financial support. This research and all associated activities were supported entirely by the institutional and personal resources of the authors.
Author information
Authors and Affiliations
Contributions
Dr. Mehmet TORUN and Dr. Deniz KOL contributed to the study conception, design, material preparation, data collection, and analysis. Dr. Hakan Özdemir, Dr.İsmail Ege Subaşı and Dr. Mehmet Ali Özbay provided the methodology framework and was instrumental in interpreting the results and drafting the manuscript.For any queries or data requests regarding this study, please contact Dr.Mehmet Torun at [email protected].
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Torun, M., Subaşı, İ.E., Özbay, D.K. et al. Utilizing non-invasive biomarkers for early and accurate differentiation of uncomplicated and complicated acute appendicitis: a retrospective cohort analysis. Sci Rep 15, 6177 (2025). https://doi.org/10.1038/s41598-025-90591-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-90591-2