Abstract
Symptomatic urethral diverticulum (UD) is a rare disease typically treated with complete surgical resection, which often involves significant trauma and higher postoperative complication rates. This study introduces a surgical concept to convert “Symptomatic” UD into “Asymptomatic” UD. In our study, we retrospectively analyzed 21 symptomatic female UD patients treated at our center between January 2018 and May 2023, collecting baseline demographic and clinical data. All patients underwent diverticulectomy or partial resection and were followed postoperatively. Mean surgery time was 75.67 ± 28.85 min, with an average blood loss of 25.52 ± 10.69 ml. The median hospital stay was 6 days (interquartile range 3.5–7 days), and the median catheterization time was 15 days (interquartile range 14–21 days). According to the Clavien–Dindo classification, most complications were minor (Grade 1 = 2 patients, Grade 2 = 1 patient, above Grade 3a = 1 patient). Pre- and post-operation UDI-6 and QoL questionnaires showed that symptoms involved in Q1–4 all improved after surgery (P < 0.05) and quality of life score also increased (P < 0.05). The "symptom cure rate" reached 76.2%, suggesting that our surgical approach may offer a minimally invasive and effective option for managing UD.
Similar content being viewed by others

Introduction
Female urethral diverticulum (UD) is a rare condition, affecting approximately 1% to 6% of adult women1, while symptomatic UD is even rarer. The classic symptoms of UD—referred to as the “3Ds” (dysuria, dyspareunia, and post-void dribbling)—are observed in only 5% of cases2. Due to the lack of typical symptoms, many clinicians fail to consider the diagnosis of UD and thus neglect related auxiliary examinations, leading to misdiagnosis and mistreatment.
Diagnostic methods for UD include post-void magnetic resonance imaging (MRI)3, urethrocystography, computed-tomographic voiding urethrography (CTU), and transvaginal ultrasound. The primary treatment remains surgical resection of the diverticulum. Certain complex cases of UD, characterized by deep ___location, multilocular structures, or circumferential configurations, pose significant challenges for complete resection. Attempting full removal in such cases can result in severe complications, including bleeding, urethral sphincter damage, urethral stricture, and urethrovaginal fistula. Approximately 10–60% of patients with UD also have stress urinary incontinence (SUI)4. Some patients are implanted with a synthetic mesh, resulting in erosion of the synthetic mesh, infection, and no relief of symptoms5.
In this study, we conducted a retrospective analysis of symptomatic UD cases managed at our center, with a focus on complex cases. We also introduce the treatment concept and surgical methods aimed at transforming symptomatic UD into asymptomatic UD, potentially reducing surgical trauma and associated complications.
Results
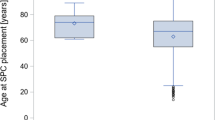
A total of 21 patients with symptomatic UD were included in the study, with a mean age of 50.38 ± 8.96 years. Symptom duration ranged from 12 to 25 months, with a median of 18 months. In our study, the most common symptom was postvoid dribbling (n = 16), followed by frequency (n = 13) and 10 patients had SUI. Other detailed clinical information of the patients was provided in Table 1.
A Limited LNS C3 grading system was used to summarize the characteristics of UD including the ___location, number, size, and configuration, communication, and continence (Table 2). According to the grading system, we can make a preliminary assessment of the complexity of UD and the ease of operation. As mentioned in “Methods”6, there were a total of 19 cases of complex UD in our study. Figure 1 shows the representative MRI, urethrogram and pelvic CT after urethrography.
Representative MR, urethrogram and pelvic CT after urethrography. a Urethrogram of one patient; b Pelvic CT after urethrography showed a horseshoe-shaped UD; c A sagittal MRI T2 weighted image of one patient, UD showed hyperintensity; d A transverse MRI T2 weighted image showed a circumferentially UD. The arrows indicate the urethral diverticula.
All patients underwent surgery under general anesthesia. Mean surgery time was 75.67 ± 28.85 min and mean blood loss was 25.52 ± 10.69 ml. Median hospital stay time was 6 days (interquartile range 3.5–7 days). Median catheterization time was 15 days (interquartile range 14–21 days) and median residual urine after catheter removal was 6 ml (interquartile range 5–10 ml). Clavien–Dindo classification system was used to assess the postoperative complications. 2 patients had Grade 1 postoperative complications (fever) and 1 patient had Grade 2 complication (Overactive bladder after catheterization). Overactive bladder (OAB) symptoms relieved after the administration of M receptor blockers. One patient had wound infection and was classified as a Grade 3a complication. The wound healed after retaining the catheterization again and strengthening the dressing and disinfection.
As mentioned above, all the patients were followed postoperatively. Of the 10 patients with preoperative SUI, only 2 had persistent incontinence after urethral diverticulectomy (2/10, 20%), and the other 8 patients’ symptoms were relieved. Only 1 patient had De novo SUI (1/11, 9.1%) and was cured after oral duloxetine. Fistula and urinary retention occurred in 1 patient respectively accompanied by recurrent urinary tract infections. Dilatation of the urethra was performed and the patient was followed up for one year without dysuria or urinary retention. The patient with urethrovaginal fistula underwent fistula repair and the symptoms disappeared. Overall, “Symptom cure rate” was as high as 76.2%. Although 9 patients had residual diverticulum or recurrence at imaging review, none of them had clinical symptoms. Perioperative characteristics and long-term complications were summarized in Table 3. Pre- and post-operation UDI-6 and QoL questionnaires show that symptoms involved in Q1–4 all improved after surgery (P < 0.05) and quality of life score also increased (P < 0.05) (Table 4).
Discussion
As shown in Table 1, female UD primarily affects older women (mean age, 50.38 ± 8.96 years), which may be linked to estrogen decline and paraurethral gland infections commonly seen in this age group, consistent with previous reports in the literature7. Additionally, symptom duration ranged from 12 to 25 months (median, 18 months), possibly due to the tolerance of Chinese patients to mild symptoms like postvoid dribbling and urinary frequency. Many patients do not seek medical attention until their symptoms are severe enough to affect their quality of life. Typical “3D” symptoms were also rare among the patients in our study. Lack of sexual activity among Asian women over 50 years of age may account for the low prevalence of “dyspareunia”. The proportion of patients with postvoid dribbling or pus is high due to our familiarity with the disease and targeted inquiry. Pelvic pain, vaginitis and recurrent urinary tract infections or urgency may be caused by combined infection after UD.
In this study, 10 patients presented with concurrent stress urinary incontinence (SUI). UD-related SUI may be a clinical artifact, potentially stemming from one of the following mechanisms: intrinsic sphincter deficiency due to UD-induced distortion of the sphincter unit, urge urinary incontinence caused by infectious UD, or sudden drainage of the diverticulum fluid content during increased intrabdominal pressure (cough, straining, etc.)8. Currently, whether to perform anti-incontinence surgery at the time of urethral diverticulum resection is still controversial. Sarah E. Bradley et al. reported that autologous pubovaginal fascial sling (APVS) was performed at the time of urethral diverticulectomy to improve symptoms of urinary incontinence9. However, this method is traumatic and difficult for urologists and gynecologists to master, which increases the risk of de novo urinary incontinence and fistula. Placing a synthetic sling while diverticulectomy may lead to infection and fistula, so it’s avoided or even forbidden by most surgeons. Early in 2014, pre-existing urodynamically proven SUI resolves in 50% of patients after excision of the diverticulum with Martius labial fat pad interposition without the need for further treatment 9. Natalie Jacox et al. reported that 14 (56%) of the 25 patients with resolution of previously existing SUI postoperatively had no concomitant slings, and it is possible that the scarring from the surgical incision site may have provided adequate support for the urethra to prevent leakage of urine10. We agree with this view and use modified figure-of-eight sutures during the surgical procedure. Our study showed that 8 (80%) of the 10 patients’ pre-existing SUI disappeared without concomitant anti-incontinence surgery.
For diagnosis, transvaginal ultrasound is our preferred examination method, offering a cost-effective and convenient option for outpatient screening11. As a recommended examination before surgery, postvoiding MRI is of great help in judging the size, position and configuration of diverticulum, as well as the surgical approach, degree of difficulty, and possible postoperative complications 12. Seth et al. identified risk factors based on MRI findings for de novo SUI as diverticulum larger than 3–4 cm, proximal ___location of the UD, and horseshoe or circumferential configuration13. Videourodynamics was only recommended for UD with SUI and not available in many primary medical institutions14. We found that the diagnostic sensitivity of CTU and voiding urography was not high, and some diverticula were not visualized.
Traditional surgical methods advocate complete exposure and resection of the diverticulum. To prevent urethrovaginal fistula, some surgeons use a right Martius graft on a vascular pedicle to fill the defect after diverticulum excision in the prone position. In our clinical practice, we have found that the trauma of complete exposure of complex UD is large, and some patients need to expand the incision or even split the pubis15, which leads to more bleeding and damages the proximal urethral sphincter, reasulting in De novo SUI. Although the diverticulum was completely removed, the symptoms increased or worsened after the operation. For distal urethral lesions, the transvaginal marsupialization technique introduced by Spence and Duckett has been noted to reduce operative time, minimize blood loss, and lower recurrence rates16,17. However, it is critical to avoid overly extending the incision proximally, as this could lead to vaginal voiding or potential injury to the proximal and distal sphincteric mechanisms, resulting in de novo SUI. Another noteworthy complication associated with this procedure is the potential formation of a pseudoseptum between the urethra and anterior vaginal wall in sexually active women, which may cause dyspareunia. Consequently, the Spence-Duckett technique is generally reserved for select cases of UD affecting the distal third of the urethra and is infrequently utilized in clinical practice18. In our approach, we applied a modified surgical procedure with multi-layer, misplaced figure-of-eight sutures to improve patient symptoms and reduce risks of de novo SUI and vaginal fistula. Table 3 showed that mean surgery time was 75.67 ± 28.85 min, and mean blood loss was only 25.52 ± 10.69 ml (no blood transfusions). Clavien–Dindo classification showed that there was no postoperative complications above grade 3b. Long-term outcomes showed that “Symptom cure rate” was as high as 76.2% and only 1 patient had De novo SUI (1/11, 9.1%). Although 9 patients had residual diverticulum or recurrence at imaging review, the patients changed from symptomatic UD to asymptomatic UD probably due to electrocautery of the diverticulum wall and closure of the diverticulum ostium. Our concept and surgical procedure might be more suitable for proximal UD and complex UD.
As female UD is a rare condition, and symptomatic UD is even rarer, only 21 patients met the inclusion criteria at our center between January 2018 and May 2023. We acknowledge that the small sample size may reduce the statistical power and increase the risk of error. Further studies with larger cohorts and multicenter collaboration are necessary to validate and generalize our findings.
Conclusion
This study presents a novel concept to convert “Symptomatic” UD into “Asymptomatic” UD which can reduce surgical trauma and postoperative complications. Although the current study shows that the results are optimistic and that patients benefit, prospective studies with larger sample sizes and controlled studies of different surgical methods are still needed.
Methods
Patients
The study is approved by our Institutional Review Board (Clinical trial identifier: 2024644) and is performed in accordance with relevant guidelines. We confirm that informed consent was obtained from all participants and/or their legal guardians. We retrospectively collected the clinical data of 21 symptomatic female UD patients who underwent diverticulectomy from January 2018 to May 2023. Baseline demographic and clinical data were recorded. All the patients had at least one clinical symptom, such as SUI, recurrent urinary tract infection, postvoid dribbling, vaginal wall mass, dysuria, and so on. Asymptomatic UDs should be excluded.
For the patients included, at least one of MRI, CTU, cystourethrography, or transvaginal ultrasound was performed to determine the size, ___location, and structure of the diverticulum. And then, a Limited LNS C3 (___location, number, size, and configuration, communication, and continence) grading system was used to classify the UD19. UD located unilaterally (left or right) was classified as simple and was regarded as complex when it was proximally located, loculated, larger than 3 cm in diameter, associated with prior pelvic or vaginal surgery, or horseshoe-shaped or circumferentially enfolds the urethra on a transverse image, multiple diverticula6. In addition, PVR and Qmax were conducted to identify neurogenic bladder or bladder outlet obstruction (BOO). Patients with radiographic suspicion of urethral diverticula carcinoma were excluded from the study and received antineoplastic therapy.
Surgical methods
All surgeries were conducted under general anesthesia. Cystourethroscopy was used to identify the ostium of the UD with the patient in the lithotomy position. Upon locating the ostium, its position was marked on the anterior vaginal wall, and a guide wire could be placed for guidance (Fig. 2a.). For some proximal or complex UD, the patient may be changed to the prone position for easy exposure of the field of view (Fig. 2b.).
A n-shaped, anterior vaginal wall incision was made and periurethral fascia was fully dissociated (Fig. 2c.). Contrary to traditional practice, for the complex UD that was difficult to dissociate, we did not blindly pursue the complete liberation of the diverticulum, but directly open the wall of the diverticulum and visually find the ostium of the diverticulum. If the ostium was not obvious, a guide wire or urethral water injection test could be assisted (Fig. 2d and Supplementary Video S1 online). The diverticulum ostium and part of the urethral wall were removed in a circular shape like removing the fistula and closed by suture in the parallel urethral direction. The diverticulum wall was stripped as much as possible under the premise of preserving the urethral sphincter mechanism. The remaining wall was cauterized by electrotome (Fig. 3a.). Then, two-layer malposition suture was used to prevent the occurrence of urethrovaginal fistula, and figure-of-eight suture (Fig. 3b. and Supplementary Video S2 online) that effectively approximate the sphincter muscle and the vagina was used to prevent urinary incontinence20. Finally, n-shaped vaginal flap covered the wound and was sutured tightly.
An F12/14 catheter was placed postoperatively and antibiotics were administered for 3 days. Surgery time, estimated blood loss, hospital stay time, duration of catheter retention, PVR after catheter removal was recorded respectively. According to Clavien–Dindo classification system21, postoperative complications were graded.
Follow-up
All the 21 patients were followed postoperatively at 1 week, 3 weeks, 3 months, 6 months, and yearly thereafter. PVR after catheter removal, de novo SUI rate, persistent SUI rate and occurrence of complications were evaluated respectively. “Symptom cure rate” was defined the proportion of patients with symptomatic UD that became asymptomatic post-operation. Additionally, patients were assessed with Urogenital Distress Inventory questionnaire (UDI-6) and Quality of Life (QoL) questionnaires before surgery and at the latest follow-up after surgery22. During the follow-up, patients with complications were treated promptly and followed up continuously.
Statistical methods
SPSS version 25.0 was used for statistical analyses. Normality and homogeneity of variance were assessed before data analysis. Continuous variables were presented as median ± standard deviation (SD) and interquartile range (IQR). Categorical variables were reported as frequencies (%) and percentages. The Wilcoxon test was used to compare the differences between pre- and post-operative questionnaire scores. P < 0.05 was considered statistically significant.
Data availability
All data supporting the results of our study are available from the corresponding author on reasonable request.
References
Greiman, A. K., Rolef, J. & Rovner, E. S. Urethral diverticulum: A systematic review. Arab. J. Urol. vol. 17, 49–57 Preprint at https://doi.org/10.1080/2090598X.2019.1589748 (2019).
Vaidya, R. V., Olson, K., Wolter, C. & Khan, A. Characterization of urethral diverticula in women. Female Pelvic Med Reconstr Surg 28, 54–56 (2022).
Warde, N. Imaging: MRI in the diagnosis of urethral diverticulum: Discrepancies between imaging and surgical findings. Nat Rev Urol 7, 366 (2010).
Xie, J., Liu, B., Li, J. & Luo, Z. ‘Sandwich’ mesh reconstruction of female giant urethral diverticulum: A case report. BMC Urol. 20 (2020).
Barratt, R. et al. The incidence and outcomes of urodynamic stress urinary incontinence in female patients with urethral diverticulum. Neurourol Urodyn 38, 1889–1900 (2019).
Kim, H. W., Lee, J. Z. & Shin, D. G. Pathophysiology and management of long-term complications after transvaginal urethral diverticulectomy. Int. Neurourol. J. 25 202–209. Preprint at https://doi.org/10.5213/INJ.2142006.003 (2021).
Serrell, E. C. & McAchran, S. E. Urethral masses. Obstet Gynecol Clin North Am 48, 599–616 (2021).
Chavez, J. A. et al. Stress urinary incontinence after urethral diverticulum repair without concomitant anti-incontinence procedure. Urology 154, 103–108 (2021).
Greenwell, T. J. & Spilotros, M. Urethral diverticula in women. Nature Rev. Urol. 12, 671–680. Preprint at https://doi.org/10.1038/nrurol.2015.230 (2015).
Jacox, N., Yao, H. H. I., Baverstock, R., Trpkov, K. & Carlson, K. Periurethral and anterior vaginal wall masses: Etiology, presentation, and treatment outcomes. Obstet. Gynecol. 140, 778–783 (2022).
Shafat Heller, L., Feiner, B., Sharabi, H., Brodner, Y. & Shrim, A. Transvaginal ultrasound imaging of female urethral diverticulum before and after voiding. Ultrasound Obstet. Gynecol. 58, 640–641. https://doi.org/10.1002/uog.23766 (2021).
Maetzold, E. & Takacs, E. B. Urethral pathology in women. Curr. Urol. Rep. 23, 225–234. https://doi.org/10.1007/s11934-022-01109-6 (2022).
Seth, J. H. et al. Correlation of MRI features of urethral diverticulum and pre- and post-operative stress urinary incontinence. Neurourol Urodyn 38, 180–186 (2019).
Przydacz, M. & Goldman, H. B. Videourodynamics—role, benefits and optimal practice. Nature Rev. Urol. https://doi.org/10.1038/s41585-024-00923-6 (2024).
Mehta, S., Suh, C. & Harmanli, O. Circumferential urethral diverticulum: A surgical conundrum. Int Urogynecol J 31, 2683–2685 (2020).
Spence, H. M. & Duckett, J. W. J. Motion picture: Simple operation for cure of diverticula of female urethra. Trans Am Assoc Genitourin Surg 61, 78–79 (1969).
Spence, H. M. & Duckett, J. W. Diverticulum of the female urethra: Clinical aspects and presentation of a simple operative technique for cure. J. Urol. 104, 432 (1970).
Stein, R. Campbell walsh wein urology. Aktuelle Urol 52, 25 (2021).
Leach, G. E., Sirls, L. T., Ganabathi, K. & Zimmern, P. E. LNS C3: A proposed classification system for female urethral diverticula. Neurourol Urodyn 12, 523–531 (1993).
Osman, N. I. et al. The modified prone Jack-knife position for the excision of female urethral diverticula. Eur Urol 79, 290–297 (2021).
Clavien, P. A. et al. The Clavien–Dindo classification of surgical complications: Five-year experience. Ann. Surg. 250, 187–196. https://doi.org/10.1097/SLA.0b013e3181b13ca2 (2009).
Skorupska, K., Grzybowska, M. E., Kubik-Komar, A., Rechberger, T. & Miotla, P. Identification of the urogenital distress inventory-6 and the incontinence impact questionnaire-7 cutoff scores in urinary incontinent women. Health Qual. Life. Outcomes 19 (2021).
Funding
This work was supported by Horizontal project of Soochow University (P112201624).
Author information
Authors and Affiliations
Contributions
Xin Chen, Xiaojie Ang and Xiaojian Xu contributed equally as first authors of this manuscript. Jiawei You was responsible for informed consent and perioperative patient management. Weiguo Chen, Yuhua Huang and Miao Li were responsible for performing the operation. Xiaojie Ang and Xiaojian Xu contributed to patients’ follow up and data acquisition of this study. Xin Chen and Miao Li performed statistical analysis and completed the first draft of this manuscript. Jianquan Hou provided critical revision of this manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, X., Ang, X., Xu, X. et al. Experience in conversion of symptomatic urethral diverticulum to asymptomatic status through surgery. Sci Rep 15, 7533 (2025). https://doi.org/10.1038/s41598-025-90748-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-90748-z