Abstract
Familial cerebral cavernous malformation (FCCM), especially severe cases, impose a heavy physical and psychological burden on patients and their families. To explore the differences in plasma biomarker levels between patients with FCCM and their healthy first-degree relatives (FDRs) and between FCCM patients with and without severe chronic disease aggressiveness (CDA). In a cross - sectional study, magnetic resonance imaging (MRI) scanning and genetic testing were performed in patients with multiple CCMs and their FDRs. Subsequently, sixty-seven plasma biomarkers were tested using a customised multiplex bead immunoassay kit. Univariate and multivariate unconditional logistic regression analyses were conducted to determine the associations between plasma factors and the risk of developing FCCM and severe CDA. Receiver operating characteristic (ROC) curves were generated for each independent risk factor. As a result, plasma factors of 37 patients with FCCM and 37 FDRs were examined. Low CD31 (P < 0.001) and BDNF levels (P = 0.013) were independent risk factors for FCCM. The best model was achieved by combining the results of CD31 and BDNF (AUC = 0.845, sensitivity 0.838, specificity 0.784, cutoff score − 4.295) to distinguish patients with FCCM from healthy FDRs. Low Serpin E1/PAI-1 (P = 0.011) and high ROBO4 levels (P = 0.013) were independent risk factors for severe CDA in patients with FCCM. The best model was achieved by combining the results of Serpin E1/PAI-1 and ROBO4 levels (AUC = 0.913, sensitivity 1.000, specificity 0.760, cutoff score − 0.525) to identify patients with FCCM and severe CDA. In summary, the plasma concentrations of CD31 and BDNF seem to be lower in patients with FCCM than in their healthy FDRs. Low Serpin E1/PAI-1 and high ROBO4 concentrations may be correlated with high lesion burden and risk of recurrent bleeding.
Trial registration: ClinicalTrials.gov Identifier: NCT03467295.
Similar content being viewed by others
Introduction
Cerebral cavernous malformations (CCMs) are abnormally clustered, dilated capillary caverns lined by a single layer of leaky endothelium1. Most CCM cases comprise sporadic CCMs. Hereditary or familial CCM (FCCM) is caused by an autosomal dominant inherited genetic mutation associated with multiple lesions2. Three protein-encoding genes, viz.CCM1/KRIT1,CCM2/malcavernin, and CCM3/PDCD10, are known to cause FCCM3,4. However, the clinical behavior of CCM remains unpredictable. Some patients remain asymptomatic, while others are disabled due to recurrent bleeding or a high lesion burden or a combination of both5. Early detection using biomarkers may improve the outcome of patients with CCM. However, the molecular mechanisms influencing and predictive biomarker for chronic or acute disease severity remain largely unknown.
Based on recent discoveries that implicate angiogenic, immune, and inflammatory mechanisms in CCM, some authors have proposed that serum biomarkers may reflect chronic or acute disease activity6. Girard et al. pioneered the study of the predictive value of a panel of 24 candidate plasma biomarkers, each with a reported role in the physiopathology of CCMs, to predict clinically relevant disease activity7,8. According to their results, the participants who had experienced symptomatic lesional hemorrhagic expansion had low sCD14, IL-6, and VEGF levels and high IL-1 and sROBO4 plasma levels8. The research findings of Seán B. Lyne et al. show that the biomarker combination of sCD14, VEGF, IL − 1β, and sROBO4 can predict the bleeding situation of CCM in the subsequent year9. Recently, Roberto Latini et al. revealed sROBO4, thrombomodulin (TM) and CRP can predict incident adverse clinical events10. However, in the FCCM cohort, particularly the FCCM cases within the Chinese population, only a limited number of studies have investigated the association between the burden of CCMs and biomarker plasma levels and the predictive model of lesional activity. However, familial cases with germline mutations are generally associated with a greater lesion burden and hemorrhagic risk.
Therefore, this study aimed to explore the differences in plasma biomarker levels between patients with FCCM and their healthy first-degree relatives (FDRs) and between FCCM patients with mild and severe chronic disease aggressiveness (CDA) to identify and stratify patients with FCCM using new panels of 67 selected candidate plasma biomarkers.
Methods
Study objects
Patient with multiple CCM and their FDRs were enrolled our studies in the First Affiliated Hospital of Fujian Medical University between October 2020 and August 2021. Patients with multiple CCM were enrolled and FDRs screening procedures were previously described11. The inclusion criteria was as follow: patients with multiple CCMs and their FDRs were recruited after providing written informed consent for brain magnetic resonance imaging (MRI) scanning, blood sample collection and gene testing. According to the currently accepted categorization12,13,14, familial cases were defined as CCM patients with germline loss-of-function mutations in the CCM complex proteins or with a family history of CCM in FDRs. In an FCCM family, FDRs of either the proband or newly identified CCM patients were screened by MRI.
Based on the pedigree investigation, brain MRI scanning, and whole-exome sequencing (WES), the probands and FDRs with CCM were assigned to the CCM group, and healthy FDRs were assigned to the non-CCM group. The exclusion criteria were as follows: patients (1) without brain MRI or SWI sequencing; (2) with suspected CCM; (3) with arteriovenous malformation (AVM); (4) with acute intra or extra hemorrhage (≤ 1 month); or (5) without serum samples.
Our manuscript was structured in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines for cohort studies15.All performed in accordance with the Declaration of Helsinki and approved by the First Affiliated Hospital of Fujian Medical University Institutional Review Board (IRB; approval number: [2018] No. 003).
Screening of participants, collection of clinical information and definition of severe chronic disease aggressiveness
The process of patient screening and inclusion, as well as the collection of information, has been previously described11. The information was electronically stored in a secure database (Real Data EDC system) for subsequent analysis. Patients were classified as mild and severe CDA, and the latter referred to those who meet any of the following criteria: (1) experiencing symptomatic hemorrhage by the age of 18; (2) experiencing more than one symptomatic hemorrhage event; (3) showing more than 25 lesions on SWI, or more than 5 lesions on T2-weighted images (Fig. 1). Adjudication of the classification was performed by the senior author of this study, who was blinded from any information on the biomarker levels.
Assessment of plasma biomarker levels
Candidate biomarkers were selected based on their reported roles in angiogenesis, inflammation, endothelial cell integrity and permeability, cell adhesion, and extracellular matrix remodeling (Supplemental Table 2)8,16,17,18,19. All blood samples were collected using 5ml BD Vacutainer® serum separation tubes. For plasma isolation, 5 ml blood was centrifuged at 3000 rpm for 5 min. The supernatant plasma was aliquoted into cryogenic storage tubes (500 µl) and stored at − 80 °C. Fasting was not required because the clinical visits were conducted at various times of the day. Sixty-seven plasma biomarkers were assessed using a customized multiplex bead immunoassay kit (R&D Systems, Minnesota, USA). According to the technical requirements of the customized kit, 67 factors were customized in 7 kits (Supplemental Table 1). The detection principle of the kit is to utilize Luminex detection technology to detect the expression of various factors in the sample. The detection methods are carried out in accordance with the protocol of the kit. Measurements were performed using a Luminex X-200 liquid suspension chip analysis system (Luminex, Texas, USA). All the plasma samples used in this study were processed and tested in the same batch. The concentration levels of plasma factors below the limit of detection were replaced by the limit of detection divided by the square root of 2.
Statistical analysis
First, normal analysis was performed using the Shapiro-Wilk test on quantitative data, including demographic data, clinical characteristics, and plasma factors. Most of the data showed a skewed distribution, medians and interquartile ranges were used to describe these data. Quantitative data were compared between two groups using the Mann-Whitney U test. Categorical variables were descriptively summarized as numbers (%), and distribution differences between groups were calculated using the chi-square test or Fisher’s test. The correlations between plasma factors were analysed with Spearman’s rank correlation coefficient. Second, logistic regression analyses were performed to determine the associations between plasma factors and the risk of CCM occurrence and severe CDA. Variables with P < 0.05 in the univariate analysis were selected for inclusion in a multivariate logistic model (Backwald: Wald). Third, receiver operating characteristic (ROC) curves were generated, and the area under the curve (AUC) was calculated for each plasma factor and in linear combination (discriminant score). The best model was defined as the one for which the AUC value was greatest, and the optimal cut-off value which provides the best tradeoff between sensitivity and specificity was found using the Youden index method. Finally, generalized linear mixed models (GLMM) were used for sensitivity analysis, defining the individual level as low level 1 and pedigree level as high level 2. Analyses were performed using SPSS (version 26.0; R version 4.1.0) and GraphPad Prism (version 8.0). Two-tailed P-values < 0.05 were considered statistically significant.
Results
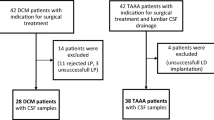
Twenty-one multiple CCM patients and their FDRs were screened to identify FCCM families. Based on the MRI scanning, gene testing, and family history survey, 4 patients with neither germline mutations in the CCM1/KRIT1, CCM2/malcavernin, or CCM3/PDCD10 genes nor a family history of CCM were defined as sporadic CCM cases. The remaining 17 multiple CCM patients were identified as index cases of FCCM families. The initial symptoms noted in the 17 probands were hemorrhage in 5 patients (29.4%), epilepsy in 5 patients (29.4%), headache in 2 patients (11.8%), functional neurological deficit (FND) in 1 patient (5.9%), and fever in 1 patient (5.9%), and incidentally spotted by MRI in 3 patients (17.6%). Among a total of 86 participants from the 17 FCCM families, two without intact MRI images, four with suspected CCMs and two with arteriovenous malformations on MRI, one with acute intracerebral hemorrhage on MRI and three who refused to draw blood were all excluded. Finally, the plasma biomarker candidates were examined in the CCM group consisted of 37 FCCM patients and the non-CCM group consisted of 37 healthy FDRs (Fig. 2).
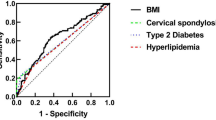
Baseline epidemiological and clinical characteristics of study participants were showed in Supplementary table 3. The differences in baseline characteristics, between patients with FCCM and healthy FDRs were not significant. The details of the comparison of plasma factor levels between patients with FCCM and healthy FDRs are listed in Table 1. Low CD31 (P < 0.001), BDNF (P = 0.002), myeloperoxidase/MPO (P = 0.005), Serpin E1/PAI-1 (P = 0.018), FGF basic/FGF2/bFGF (P = 0.035), and MMP-8 (P = 0.036) levels were associated with the occurrence of FCCM, as assessed from the Mann-Whitney U test (Fig. 3a-f). However, according to the multivariate logistic regression analysis, only low CD31 [OR (95%CI) 0.193(0.0780–0.478); P < 0.001] and BDNF levels [OR (95%CI) 0.441(0.231–0.844); P = 0.013] were independent risk factors for the occurrence of FCCM (Table 1). The accuracies to distinguish patients with FCCM from healthy FDRs were considered as “fair” when using CD31 (AUC = 0.790, sensitivity 0.838, specificity 0.730, cutoff point 15348.50 pg/mL) and BDNF as biomarkers (AUC = 0.714, sensitivity 0.676, specificity 0.811, cutoff point 16960.50 pg/mL) (Fig. 3g-i). Further analysis showed that the best model (Eq. 1) was achieved by combining the results for CD31 and BDNF (AUC = 0.845, sensitivity 0.838, specificity 0.784, cutoff score − 4.295). Equation 1: Discriminant score= [CD31/PECAM1]/ (-6436.353) +[BDNF] / (-8890.952); the discriminant score was calculated based on multivariate regression coefficients. The GLMM results showed that the family aggregation effect (intraclass correlation coefficient [ICC] = 0.042, P = 0.660) was not significant for plasma factors. However, low CD31 [OR (95%CI) 0.187 (0.068–0.514)] and BDNF [OR (95%CI) 0.431(0.212–0.875)] levels were still associated with the occurrence of FCCM when analyzed using the GLMM. The discriminant ability of the discriminant score established using the GLMM (AUC = 0.846, sensitivity = 0.838, specificity = 0.784) agreed with and supported the logistic regression results mentioned above.
(a–f) Lower CD31 (P < 0.001), BDNF (P = 0.002), Myeloperoxidase/MPO (P = 0.005), Serpin E1/PAI-1 (P = 0.018), FGF basic/FGF2/bFGF (P = 0.035) and MMP-8 (P = 0.036) were associated with the occurrence of CCM in FCCM family determined between 37 FCCM patients and 37 healthy FLRs by Mann-Whitney U test. (g–i) The receiver operating characteristic (ROC) curve generated using plasma factors distinguished the CCM patients from non-CCMs FLRs. (g) The ROC curve of BDNF. (h) The ROC curve of CD31/PECAM-1. (i) The ROC curve generated using the combination of plasma levels of BDNF and CD31/PECAM-1 to differentiate CCM patients from non-CCMs FLRs.
According to the criteria of CDA, 12 patients were dichotomized into the severe CDA group and the other 25 into the mild CDA group. The differences in baseline characteristics, including sex (P = 0.893), body mass index (P = 0.897), lifestyle habits (smoking P = 0.328, drinking P = 0.582), underlying diseases (hypertension, P = 0.819; diabetes, P = 0.324; and hyperlipidemia, P = 1.000), and mutation in CCM genes (P = 0.225), between the two groups were not significant. However, the mean age was higher in the severe CDA group than in the mild group (47.50 [38.00, 58.50] vs.34.00 [9.00, 43.00] years, P = 0.008) (Supplemental Table 4). The details of the plasma biomarker comparisons between the severe and mild CDA groups are listed in Table 2. Low Serpin E1/PAI-1 (P = 0.002), myeloperoxidase/MPO (P = 0.007), and BDNF (P = 0.016) but high IL-7 (P = 0.007) and ROBO4 (P = 0.006) levels were associated with severe CDA in FCCM patients, as determined by the Mann-Whitney U test (Fig. 4a-e). However, according to the multivariate logistic regression analysis, only low Serpin E1/PAI-1 [OR (95%CI) 0.026(0.002–0.437); P = 0.011] and high ROBO4 [OR (95%CI) 7.624(1.548–37.558); P = 0.013] were independent risk factors for severe CDA in patients with FCCM (Table 2). The accuracies to distinguish severe CDA FCCM patients were considered as “fair” when using ROBO4 (AUC = 0.780, sensitivity 0.917, specificity 0.680, cutoff point 10.58 pg/mL) and as “good” when using E1/PAI-1 as markers (AUC = 0.813, sensitivity 0.750, specificity 0.840, cutoff point 106706.00 pg/mL) (Fig. 4f-h). Further analysis showed that the best model (Eq. 2) was achieved by combining the results of E1/PAI-1 and ROBO4 (AUC = 0.913, sensitivity = 1.000, specificity = 0.760, cutoff score − 0.525). Equation 2: Discriminant score= [Serpin E1/PAI-1]/(-14508.416)+[ROBO4]/(1.423); the discriminant score was calculated based on multivariate regression coefficients. The GLMM results showed that the family aggregation effect (intraclass correlation coefficient ICC = 0.412, P = 0.592) was not significant for plasma factors. However, low Serpin E1/PAI-1 [OR (95%CI) 0.012 (0.000–0.491)] and high ROBO4 levels [OR (95%CI) 11.797 (1.483–93.844)] were still associated with severe CDA in patients with FCCM when analyzed using the GLMM. The discriminant ability of the discriminant score established using the GLMM (AUC = 0.915, sensitivity = 1.000, specificity = 0.822) agreed with and supported the logistic regression results mentioned above.
(a–e) Lower Serpin E1/PAI-1 (P = 0.002), Myeloperoxidase/MPO (P = 0.007) and BDNF (P = 0.016), but higher IL-7 (P = 0.007) and ROBO4 (P = 0.006) were associated with the severe CDA in FCCM patients determined between 12 FCCM patients with severe CDA and 25 FCCM patients with mild CDA by Mann-Whitney U test. (f–h) The receiver operating characteristic (ROC) curve generated using plasma factors to distinguish patients with the severe or mild chronic disease aggressiveness in CCM patients. (f) The ROC curve of Serpin E1/PAI-1. (g) The ROC curve of ROBO4. (h) The ROC curve generated using the combination of plasma levels of Serpin E1/PAI-1 and ROBO4.
The correlation analysis for 67 serum factors were independent of each other or showed a weak correlation (Supplementary Excel). However, among the candidate factors, strong correlations were found between MPO and MMP8 (r = 0.92, 95% CI: 0.87–0.95) and MPO and CD31 (r = 0.71, 95% CI: 0.57–0.81; Fig. 5).
Discussion
The plasma levels of molecules reflecting proliferative dysangiogenesis, blood-brain barrier hyperpermeability, inflammatory/immune processes, and measures of vascular permeability and iron deposition on magnetic resonance imaging are important biomarkers correlated with CCM occurrence and bleeding6,7,8,20. In 2021, the American NIH/NINDS published the protocol of their study on biomarkers of cerebral cavernous angioma with symptomatic hemorrhage (CASH) to optimize these biomarkers to accurately diagnose CCM with symptomatic hemorrhage (R01NS114552)21. However, there are relatively few literature reports suggesting that biomarkers have shown an association with de novo lesion genesis and symptomatic hemorrhage in FCCM cases. Patients with FCCM with small non-aggressive multiple lesions are usually managed conservatively2. Lazzaroni et al. (2024) in ‘Circulating biomarkers in familial cerebral cavernous malformation’ concluded that the correlations between FLT3L, CXCL9, FGF − 21 and CDCP1, accessed by Spearman’s correlation, confirmed that these four protein biomarkers were correlated (r ≤ 0.36 95% CI: 0.12–0.56 between FLT3L and CDCP1)22. They further stated that the combination of these proteins has a good power in the prediction of new lesion formation. There may be differences in the results due to variations in the study populations, especially in genetic diseases, as well as differences in research designs. Nevertheless, invasive intervention in multifocal FCCM cases, although controversial, can be justifiable when these lesions become symptomatic or develop. Thus, development and validation of a biomarker model to predict the occurrence and clinical activity of FCCMs may play a direct role in selecting patients with FCCM for aggressive therapies and in the stratification of cohorts in future clinical trials. To the best of our knowledge, this study is the first to investigate the differences in plasma biomarker levels between FCCM patients and their healthy FDRs and between FCCM patients with and without severe CDA in a large panel of 67 candidate plasma biomarkers. We found that low CD31and BDNF levels were independent risk factors associated with the occurrence of FCCM; the best model was achieved by combining the results of CD31 and BDNF (AUC = 0.845). Furthermore, Serpin E1/PAI-1 and high ROBO4 levels were independent risk factors associated with severe CDA in patients with FCCM, and the best model was achieved by combining the results of Serpin E1/PAI-1 and ROBO4 (AUC = 0.913).
Patients and healthy FDRs have similar genetic backgrounds and lifestyles. Therefore, the significant differences in plasma concentrations of CD31 and BNDF might be related to the pathogenesis of CCM. The past two decades have witnessed a remarkable enhancement of our understanding of the pathogenesis of this vascular disease. In FCCM, lesion formation is initiated by a somatic mutation in the CCM gene, resulting in biallelic loss of function, and a secondary somatic gain-of-function mutation in PIK3CA (phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha), which fuels lesion growth23,24. As a ligand, BDNF-induced TrkB activation of the PI3-kinase and Akt-mTOR pathway may mediate a reduction in EC–cell contacts and in normal EC apoptosis, leading to the development of FCCMs25,26. BDNF is best characterized for its pro-survival and differentiative effects on neurons; additionally, studies have uncovered the contribution of the cerebral microvasculature to BDNF production in the brain27,28. BDNF deficiency can lead to a reduction in endothelial cell-cell contacts29. However, whether the reduction in plasma BDNF concentration in FCCM patients is due to excessive utilization of BDNF remains unknown and could not be clarified in this study. CD31 is a cell-cell adhesion glycoprotein that belongs to the immunoglobulin superfamily30,31. CD31 is not only an endothelial marker but is also involved in the regulation of endothelial cell-cell interactions and angiogenesis32,33. The observation that the anti-CD31 antibody blocks the initiation of EC-EC contact suggests an important role of CD31 in maintaining the structural integrity of the EC layer34. A previous study showed that murine hemangioendothelioma cells expressed lower levels of CD31 and other components of adherent junctions than wild-type brain endothelial cells (BECs)35. BECs with CD31 deficiency (isolated from CD31-knockout mice) would in part mimic the phenotypes of cultured hemangioendothelioma cells, exhibiting an “overriding” morphology, a higher secondary proliferation rate due to the loss of contact inhibition, and a reduced level of apoptosis35,36. It was demonstrated that in addition to disrupted tight junction integrity, CD31-deficiency resulted in a perturbation of adhesion molecule-mediated signaling, which affected proliferation and suppressed apoptosis35,36, suggesting one of the molecular mechanisms underlying endothelial cell behaviors when vascular anomalies develop in hemangiomas. When the blood-brain barrier (BBB) is disrupted, the local inflammatory response in CCM intensifies. This causes inflammatory cells to secrete more soluble CD31 (sCD31). sCD31 may further damage the BBB via inflammatory pathways such as NF - κB, YAP and so on37,38,39. This could potentially serve as an indicator of disease progression in FCCM. However, sCD31 was not measured in this study. Owing to the popularity of MRI, the use of CD31 and BDNF scores to distinguish patients with FCCM from healthy FDRs has little clinical significance. However, this score may serve as a biomarker for patient screening and a warning for FCCM occurrence at an early stage. Whether CD31 and BDNF are related to the mechanism of FCCM and whether they can serve as targets for medical intervention requires further research.
An early age of lesion onset, multiple hemorrhages, and increased lesion burden have been defined as severe chronic disease severity in various studies6,40. Acute hemorrhage and epileptic seizures have a significant influence on plasma factor concentrations; therefore, they were excluded from this study. The molecular mechanisms influencing chronic disease severity remain incompletely understood, and currently there is a lack of well-validated peripheral blood biomarkers that can reliably reflect or predict disease aggressiveness in the FCCM population. Recently, several plasma factors, including 25-hydroxyvitamin D, non-HDL cholesterol, IL-2, INF-γ, TNF-α, IL-1β, MMP-2, and − 9, intercellular adhesion molecule-1, VEG, and endoglin, have been proposed to monitor disease severity and the course of sporadic CCMs7,41.Furthermore, the weighted linear combination of soluble CD14, IL-1β, VEGF, and soluble ROBO4 can be used to predict symptomatic ICH or lesion expansion8. ROBO4 is an endogenous inhibitor of VEGF signaling expressed by vascular endothelial cells42,43.This protein has been shown to dynamically maintain vascular network stability during pathological angiogenesis and proinflammatory processes44,45. In the FCCM cohort, an increase in plasma ROBO4 levels may reflect pro-inflammatory processes enhancing endothelial permeability, consistent with its prognostic association with CCM bleeding and growth8. Serpin E1/PAI-1 is a fast-acting inhibitor of tissue and urokinase plasminogen activators (tPA and uPA)46. PAI-1 controls the clot lysis triggered by tPA-activated plasminogen. PAI-1 deficiency is characterized by hyperfibrinolysis, which results in frequent bleeding episodes. Patients with this condition form normal blood clots, which are quickly lysed by unopposed tPA-activated plasmin. Spontaneous bleeding is rare in PAI-1 deficient patients, but moderate hemorrhage of the knees, elbows, nose, and gums can be triggered by mild trauma47. In the context of FCCM, lower plasma levels of Serpin E1/PAI-1 maybe associated with more frequent cerebral bleeding and a larger hemorrhage volume after ictus. However, the role of Serpin E1/PAI-1 in CCM lesion development and hemorrhage requires further investigation. In our study, age was higher in the severe CDA group than in the mild CDA group (P = 0.008) in the univariate analysis (Supplemental Table 4). Variables with P < 0.05 in the univariate analysis, including age, Serpin E1/PAI-1, ROBO4, IL-7, and BDNF, were selected for inclusion in a multivariate logistic model. However, age was eliminated from the backward model, and only Serpin E1/PAI-1 and ROBO4 were retained in the final model. In addition, we constructed a new model (age + Serpin E1/PAI-1 + ROBO4) to re-evaluate the effect of age on disease severity. A model algorithm was established based on the results of the multivariate logistic model. Equation: Discriminant score = age × 0.06012+ (Serpin E1/PAI-1)* (-0.00005) +(ROBO4) × 0.78396. The AUC of the new model was 0.940, which was higher than that of the model without age (Serpin E1/PAI-1 + ROBO4 [AUC:0.913]); however, the difference was not statistically significant (Z = − 0.831, P = 0.406). It can be observed that the improvement in age for the model was limited. Overall, we found that the combination of Serpin E1/PAI-1 and ROBO4 was the best model to distinguish FCCM patients with mild and severe CDA; therefore, it may be helpful in the prognostication and stratification of FCCM cases in future clinical trials.
Limitations.
This study is a single - center cross - sectional study, yet it can provide a hint for future multi - center prospective studies. In addition, the correlations herein do not imply a specific causality related to CCM. However, they resulted in a cogent hypotheses about the mechanism of disease occurrence and progression that can be pursued in future laboratory and clinical studies. Finally, the limitations of the assay methodologies and batch effects must be considered in clinical practice. However, in this study, we investigated the differences in plasma biomarker levels between FCCM patients and their FDRs and between FCCM patients with and without CDA in a large panel of 67 plasma biomarkers. These results may play a direct role in selecting FCCM patients for aggressive therapies and may be critical for defining biological targets for medical therapies.
Conclusion
In the FCCM family, plasma concentrations of CD31 and BDNF seems to be lower in FCCM patients; low Serpin E1/PAI-1 and high ROBO4 concentrations may be correlated with high lesion burden and risk of recurrent bleeding. Future multi-site studies with a larger number of cases are needed to confirm our findings.
Data availability
Data is provided within the manuscript or supplementary information files.
References
Carrión-Penagos, J. et al. Subclinical imaging changes in cerebral cavernous angiomas during prospective surveillance. J. Neurosurg. 134(3), 1147–1154. https://doi.org/10.3171/2020.1.Jns193479 (2020).
Zafar, A. et al. Familial cerebral cavernous malformations. Stroke 50(5), 1294–1301. https://doi.org/10.1161/strokeaha.118.022314 (2019).
Morrison, L. & Akers, A. Cerebral Cavernous Malformation, Familial (GeneReviews™, 1993).
Li, X., Fisher, O. & Boggon, T. The cerebral cavernous malformations proteins. Oncotarget 6(32), 32279–32280. https://doi.org/10.18632/oncotarget.5443 (2015).
Al-Shahi Salman, R. et al. Untreated clinical course of cerebral cavernous malformations: a prospective, population-based cohort study. Lancet Neurol. 11(3), 217–224. https://doi.org/10.1016/s1474-4422(12)70004-2 (2012).
Choquet, H. et al. Polymorphisms in inflammatory and immune response genes associated with cerebral cavernous malformation type 1 severity. Cerebrovasc. Dis. 38(6), 433–440. https://doi.org/10.1159/000369200 (2014).
Girard, R. et al. Plasma biomarkers of inflammation reflect seizures and hemorrhagic activity of cerebral cavernous malformations. Translational Stroke Res. 9(1), 34–43. https://doi.org/10.1007/s12975-017-0561-3 (2018).
Girard, R. et al. Plasma biomarkers of inflammation and angiogenesis predict cerebral cavernous malformation symptomatic hemorrhage or lesional growth. Circul. Res. 122(12), 1716–1721. https://doi.org/10.1161/circresaha.118.312680 (2018).
Lyne, S. et al. Biomarkers of cavernous Angioma with symptomatic hemorrhage. JCI Insight. 4(12). https://doi.org/10.1172/jci.insight.128577 (2019).
Lazzaroni, F. et al. Circulating biomarkers in familial cerebral cavernous malformation. EBioMedicine Jan. 99, 104914. https://doi.org/10.1016/j.ebiom.2023.104914 (2024).
Li, C. et al. Prevalence, genetic and clinical characteristics in first-degree relatives of patients with Familial cerebral cavernous malformations in China. Stroke Vasc Neurol. May. 15 https://doi.org/10.1136/svn-2023-003004 (2024).
de Champfleur, N. et al. Magnetic resonance imaging evaluation of cerebral cavernous malformations with susceptibility-weighted imaging. Neurosurgery 68(3), 641–647. https://doi.org/10.1227/NEU.0b013e31820773cf (2011). discussion 647-8.
Campbell, P., Jabbour, P., Yadla, S. & Awad, I. Emerging clinical imaging techniques for cerebral cavernous malformations: a systematic review. NeuroSurg. Focus. 29(3), E6. https://doi.org/10.3171/2010.5.Focus10120 (2010).
de Souza, J. et al. Susceptibility-weighted imaging for the evaluation of patients with familial cerebral cavernous malformations: a comparison with t2-weighted fast spin-echo and gradient-echo sequences. AJNR Am. J. Neuroradiol. 29(1), 154–158. https://doi.org/10.3174/ajnr.A0748 (2008).
Cuschieri SJSjoa. STROBE Guidelines ;13, S31–S34 https://doi.org/10.4103/sja.SJA_543_18 (2019).
Claesson-Welsh, L., Dejana, E. & McDonald, D. Permeability of the endothelial barrier: identifying and reconciling controversies. Trends Mol. Med. 27(4), 314–331. https://doi.org/10.1016/j.molmed.2020.11.006 (2021).
Chai, P. et al. High-throughput transcriptional profiling combined with angiogenesis antibody array analysis in an orbital venous malformation cohort. Exp. Eye Res. 191, 107916. https://doi.org/10.1016/j.exer.2020.107916 (2020).
Retta, S. & Glading, A. Oxidative stress and inflammation in cerebral cavernous malformation disease pathogenesis: two sides of the same coin. Int. J. Biochem. Cell Biol. 81, 254–270. https://doi.org/10.1016/j.biocel.2016.09.011 (2016).
Zhao, M., Peng, C., Li, L., Chen, L. & Zhang, H. Circulating Treg cells from patients with cerebral aneurysms displayed deficiency in ICOS expression and function. Clin. Exp. Pharmacol. Physiol. 47(12), 1923–1931. https://doi.org/10.1111/1440-1681.13388 (2020).
Chohan, M. et al. Emerging pharmacologic targets in cerebral cavernous malformation and potential strategies to alter the natural history of a difficult disease: A review. JAMA Neurol. 76(4), 492–500. https://doi.org/10.1001/jamaneurol.2018.3634 (2019).
Girard, R. et al. A roadmap for developing plasma diagnostic and prognostic biomarkers of cerebral cavernous angioma with symptomatic hemorrhage (CASH). Neurosurgery 88(3), 686–697. https://doi.org/10.1093/neuros/nyaa478 (2021).
Francesca, L. et al. Circulating biomarkers in familial cerebral cavernous malformation. EBioMedicine 99(0). https://doi.org/10.1016/j.ebiom.2023.104914 (2023).
Ren, A. et al. PIK3CA and CCM mutations fuel cavernomas through a cancer-like mechanism. Nature 594(7862), 271–276. https://doi.org/10.1038/s41586-021-03562-8 (2021).
Snellings, D. et al. Cerebral cavernous malformation: from mechanism to therapy. Circul. Res. 129(1), 195–215. https://doi.org/10.1161/circresaha.121.318174 (2021).
Sha’ari, H. et al. Association of BDNF polymorphisms with the risk of epilepsy: a multicenter study. Mol. Neurobiol. 53(5), 2869–2877. https://doi.org/10.1007/s12035-015-9150-1 (2016).
Kermani, P. & Hempstead, B. Brain-derived neurotrophic factor: a newly described mediator of angiogenesis. Trends Cardiovasc. Med. 17(4), 140–143. https://doi.org/10.1016/j.tcm.2007.03.002 (2007).
Guo, S. et al. Neuroprotection via matrix-trophic coupling between cerebral endothelial cells and neurons. Proc. Natl. Acad. Sci. U.S.A. 105(21), 7582–7587. https://doi.org/10.1073/pnas.0801105105 (2008).
Monnier, A. et al. Brain-derived neurotrophic factor of the cerebral microvasculature: a forgotten and nitric oxide-dependent contributor of brain-derived neurotrophic factor in the brain. Acta Physiol. (Oxford, England). 219(4), 790–802. https://doi.org/10.1111/apha.12743 (2017).
Donovan, M. et al. Brain derived neurotrophic factor is an endothelial cell survival factor required for intramyocardial vessel stabilization. Dev. (Cambridge England). 127(21), 4531–4540. https://doi.org/10.1242/dev.127.21.4531 (2000).
DeLisser, H., Newman, P. & Albelda, S. Molecular and functional aspects of PECAM-1/CD31. Immunol. Today. 15(10), 490–495. https://doi.org/10.1016/0167-5699(94)90195-3 (1994).
Watt, S., Gschmeissner, S. & Bates, P. PECAM-1: its expression and function as a cell adhesion molecule on hemopoietic and endothelial cells. Leuk. Lymphoma. 17, 229–244. https://doi.org/10.3109/10428199509056827 (1995).
Albelda, S., Oliver, P., Romer, L. & Buck, C. EndoCAM: a novel endothelial cell-cell adhesion molecule. J. Cell Biol. 110(4), 1227–1237. https://doi.org/10.1083/jcb.110.4.1227 (1990).
Matsumura, T., Wolff, K. & Petzelbauer, P. Endothelial cell tube formation depends on Cadherin 5 and CD31 interactions with filamentous actin. J. Immunol. (Baltimore Md: 1950). 158(7), 3408–3416 (1997).
Albelda, S., Muller, W., Buck, C. & Newman, P. Molecular and cellular properties of PECAM-1 (endoCAM/CD31): a novel vascular cell-cell adhesion molecule. J. Cell Biol. 114(5), 1059–1068. https://doi.org/10.1083/jcb.114.5.1059 (1991).
Tsuneki, M. & Madri, J. Adhesion molecule-mediated Hippo pathway modulates hemangioendothelioma cell behavior. Mol. Cell. Biol. 34(24), 4485–4499. https://doi.org/10.1128/mcb.00671-14 (2014).
Tsuneki, M. & Madri, J. CD44 regulation of endothelial cell proliferation and apoptosis via modulation of CD31 and VE-cadherin expression. J. Biol. Chem. 289(9), 5357–5370. https://doi.org/10.1074/jbc.M113.529313 (2014).
Isabella, W. et al. PECAM-1 stabilizes Blood-Brain barrier integrity and favors paracellular T-Cell diapedesis across the Blood-Brain barrier during neuroinflammation. Front. Immunol. 10(0). https://doi.org/10.3389/fimmu.2019.00711 (2019).
Jonathan, L. et al. Receptor-interacting protein kinase 2 (RIPK2) profoundly contributes to post-stroke neuroinflammation and behavioral deficits with microglia as unique perpetrators. J. Neuroinflammation. 20(1). https://doi.org/10.1186/s12974-023-02907-6 (2023).
Éva, G. et al. BRAF modulates the interplay between cell-cell and cell-extracellular matrix adhesions in PECAM-1-mediated mechanotransduction. Int. J. Mol. Sci. 25(20). https://doi.org/10.3390/ijms252011234 (2024).
Al-Holou, W. et al. Natural history and imaging prevalence of cavernous malformations in children and young adults. J. Neurosurg. Pediatr. 9(2), 198–205. https://doi.org/10.3171/2011.11.Peds11390 (2012).
Girard, R. et al. Peripheral plasma vitamin D and non-HDL cholesterol reflect the severity of cerebral cavernous malformation disease. Biomark. Med. 10(3), 255–264. https://doi.org/10.2217/bmm.15.118 (2016).
Chen, X. et al. Association of six CpG-SNPs in the inflammation-related genes with coronary heart disease. Hum. Genomics. 21. https://doi.org/10.1186/s40246-016-0067-1 (2016).
Becerra, A. et al. Evaluating the prognostic role of elevated preoperative carcinoembryonic antigen levels in colon cancer patients: results from the National Cancer database. Ann. Surg. Oncol. 23(5), 1554–1561. https://doi.org/10.1245/s10434-015-5014-1 (2016).
Gao, Y. et al. Arsenic exposure assists ccm3 genetic polymorphism in elevating blood pressure. Oncotarget 9(4), 4915–4923. https://doi.org/10.18632/oncotarget.23518 (2018).
Shenkar, R. et al. Exceptional aggressiveness of cerebral cavernous malformation disease associated with PDCD10 mutations. Genet. Medicine: Official J. Am. Coll. Med. Genet. 17(3), 188–196. https://doi.org/10.1038/gim.2014.97 (2015).
Vaughan, D. PAI-1 and atherothrombosis. J. Thromb. Haemostasis: JTH. 3(8), 1879–1883. https://doi.org/10.1111/j.1538-7836.2005.01420.x (2005).
Jankun, J. & Skrzypczak-Jankun, E. Plasminogen activator inhibitor with very long half-life (VLHL PAI-1) can reduce bleeding in PAI-1-deficient patients. Cardiovasc. Hematol. Disord. Drug Targets. 13(2), 144–150. https://doi.org/10.2174/1871529x11313020007 (2013).
Funding
This work was supported by grants from Technology Platform Construction Project of Fujian Province (2020Y2003, 2021Y2001). And this work was supported the Fujian Province High level Neuromedical Center Construction Fund (principal investigator: Dezhi Kang), a grant from the Government of Fujian Province (Grant number: HLNCC-FJFY-003).
Author information
Authors and Affiliations
Contributions
Concept and design: F.L., D.K., Y.L.Participants contact and communication: C.L.,Q.L., D.C.Information collection: C.L., L.Z., P.L., Q.L., W.Z.MRI scan, analysis: Y.K., W.H Drafting of the manuscript: C.L., S.H., F.L.Statistical analysis: S.H.Administrative, technical, or material support: F.L., L.Y., D.W.Supervision: K.M., S.H., X.L.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, C., Huang, S., Li, Q. et al. Plasma biomarkers in patients with familial cavernous malformation and their first-degree relatives: a cross-sectional study. Sci Rep 15, 11284 (2025). https://doi.org/10.1038/s41598-025-91141-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-91141-6