Abstract
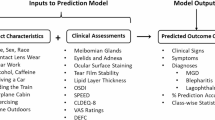
Eye washing is a common over-the-counter, self-administered method for managing hay fever-related ocular symptoms. However, epidemiological data on eyewash users with hay fever and their characteristics are limited. This study aimed to profile eyewash usage and preferences in individuals with hay fever. This digital, cross-sectional cohort study was conducted between February 2018 and May 2020. Individuals in Japan who downloaded the AllerSearch smartphone application were included. Factors associated with eyewash and non-eyewash users among patients with hay fever were assessed using multivariable logistic regression analyses. Of the 11,284 participants, 9,041 had hay fever. Among them, 40.7% were eyewash users (43.9% used eyewash products as needed during symptom flare-ups, 24.8% used them in the morning, and 19.4% in the evening). Factors associated with eyewash use included younger age, previous psychiatric illness, history of contact lens use, current contact lens use, active smoking, higher yogurt intake, lower nasal symptom score, higher non-nasal symptom score, and dry eye symptoms. Non-use of eyewash was linked to older age, sleep duration < 6 h, lower yogurt intake, and dry eye symptoms. This study elucidated characteristics and factors associated with eyewash use among individuals with hay fever, guiding an individualized approach to treatment and public health initiatives.
Similar content being viewed by others
Introduction
Hay fever is a highly prevalent immunoallergic disease, estimated to affect 25% of the global population, with its prevalence expected to increase in the future1,2. Hay fever manifests through various phenotypes, including allergic rhinitis and conjunctivitis, which can significantly impair quality of life, academic performance, sleep hygiene, and work productivity3,4. Current treatment methods for allergic rhinitis and conjunctivitis secondary associated with hay fever involves oral or ophthalmic topical administration of antihistamines, with steroids used in more severe cases5,6. Additionally, active patient involvement in lifelong self-care is crucial for managing the chronic nature of hay fever and preventing symptom exacerbation7. However, symptoms are highly variable and heterogeneous, depending on the affected individual, and a tailored treatment and prevention regimen based on a comprehensive review of associated factors may be needed to maximize efficacy7,8.
Allergic rhinitis and conjunctivitis associated with hay fever result from type I hypersensitivity reactions due to direct contact of the nose or eyes to pollen, which acts as a local allergen9,10. Therefore, preventive measures, such as wearing goggles and masks and physically removing allergens from the affected ocular surface using eyewash, are often recommended as part of hay fever self-management guidelines9,10. These measures are more accessible to the general public and easier to incorporate into daily routines compared with traditional medical treatments. Eyewash, in particular, can help eliminate ocular surface allergens, eosinophils, and allergic mediators from the eyelid margin10. However, frequent use of eyewash may theoretically disrupt the physiological tear film homeostasis, leading to dry eye (DE) disease. Additionally, preservatives such as benzalkonium chloride, often found in commercial eyewash products, may exacerbate allergic symptoms if overused11. A recent report by Yazu et al. suggested that using eyewash products did not worsen DE symptoms11, and was effective in reducing early-phase symptoms of allergic conjunctivitis12. Currently, a knowledge gap exists regarding the epidemiology and characteristics unique to eyewash users within the hay fever population. Filling this gap is crucial for developing well-rounded, evidence-based guidelines for eyewash that can provide tailored self-care practices, enhance preventive measures, improve treatment efficacy, reduce risks, and ensure more targeted use in hay fever management.
AllerSearch, a smartphone application released in 2018 for hay fever research, allows the collection of comprehensive participant data on demographics, medical history, lifestyle, hay fever symptoms, current and past treatments, and preventive measures2,8. We hypothesize that using eye irrigation and eyewash products may be common self-management tools for patients with hay fever and ocular symptoms. A large-scale epidemiological analysis of eyewash users among patients with hay fever could help elucidate the unique features and patterns related to age, sex, and hay fever severity. This may help lay the groundwork for future efforts to promote targeted therapy and prevention tailored to each patient. The wide reach and advantages of AllerSearch, due to its mobile health nature, make it well-suited for conducting epidemiological studies on eyewash users.
In this study, we aimed to identify patterns and features related to hay fever and self-care practices by conducting a comprehensive profiling of eyewash users among patients with hay fever compared to non-eyewash users. This large scale-epidemiological study may have implications for establishing future guidelines for proper and targeted eyewash use, enhancing efficacy and reducing risks in hay fever management.
Results
Application downloads and participants enrollment
A detailed description of the database collected using the AllerSearch smartphone application (AllerSearch) has been described previously2,4,8,13. Briefly, 17,597 individual data points were identified via unique identifier extraction from the database. Of these, 15,749 individuals provided electronic informed consent (eConsent, agreement rate: 89.5%), while 1,848 did not respond. Among those who consented to participate, 15,649 provided basic information, and 11,442 completed the daily hay fever monitoring survey. After excluding 4,207 individuals with incomplete data records, 113 with outlier data, and 45 without geographic data, 11,284 of the 17,597 initial users (64.1%) were included in this study. The flow diagram of participant enrollment in this study is shown in Fig. 1. The geographic distribution of the participants in Japan was as follows: 2,510 users in Tokyo (22.2%), 1,070 in Kanagawa (9.5%), and 957 in Osaka (8.5%).
Among the 11,284 participants, 9,041 presented with hay fever, 1,523 had an unknown diagnosis, and 720 did not have hay fever.
Characteristics of eyewash use in individuals with hay fever
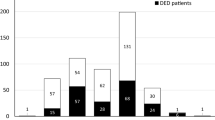
The usage rate of eyewash products was 23.9% (172/720) among individuals without hay fever, 40.7% (3,683/9,041) among those with hay fever, and 26.8% (408/1,523) among individuals with unknown diagnoses (Fig. 2a). Figure 2b shows the eyewash usage rate according to the age of individuals with hay fever. The highest rate of eyewash use (47.6%) was observed in the age group comprising individuals aged < 20 years, followed by the 20–30-year (41.5%) and 40–50-year (40.3%) age groups. Figure 2c shows the timing of eyewash use among individuals with hay fever. The most frequently reported timing of eyewash use was when symptoms worsened (43.9%), followed by morning (24.8%) and nightly (19.4%) use. Figure 2d shows the frequency of eyewash use based on contact lens (CL) status. Individuals who discontinued CL use during the hay fever season had the highest rate of eyewash use (50.9%), followed by current (44.1%) and past (39.3%) CL users.
Comparison of characteristics and hay fever symptoms between eyewash and non-eyewash user groups in individuals with hay fever
The demographics, medical history, residential environment, and lifestyle information of the 9,041 individuals with hay fever are shown in Table 1. The median age of the participants was 34 (range: 23–46) years, and 56.2% were female participants.
Among these participants, 3,683 (40.7%) reported eyewash use, while 5,358 (59.3%) did not. Younger age, higher body mass index (BMI), lower frequency of medicated hypertension, and higher frequency of psychiatric disease, DE diagnosis, and kidney disease were observed in the eyewash user group than in the non-eyewash user group. The eyewash group had a higher frequency of current and past CL use and a lower frequency of discontinuation during the hay fever season than the non-eyewash user group. Active smoking was significantly higher in the eyewash user group than in the non-eyewash user group. Moreover, yogurt intake was reported more frequently in the eyewash user group than in the non-eyewash user group.
Table 2 summarizes the characteristics of hay fever symptoms between eyewash users and non-eyewash users among individuals with hay fever. Eyewash users had significantly higher total nasal symptom scores (TNSS), total non-nasal symptom scores (TNNSS), and total symptom score (TSS) than non-eyewash users (TNSS, 4 (1–6) points vs. 3 (1–6) points; TNNSS, 2 (0–4) points vs. 1 (0–4) points; TSS, 5 (2–11) points vs. 5 (2–10) points; P < 0.001 for all comparisons).
Comparison of DE symptoms between eyewash and non-eyewash users with hay fever
DE symptoms in the eyewash users and non-eyewash users among individuals with hay fever are summarized in Table 3. The Japanese version of the Ocular Surface Disease Index (J-OSDI) total score was significantly higher among eyewash users than among non-eyewash users (Eyewash users: 14.6 (6.3–25) points, non-eyewash users: 12.5 (4.2–22.9) points; P < 0.001).
Factors associated with eyewash user compared to non-eyewash user in individuals with hay fever
The crude and multivariate odds ratios (ORs) with 95% confidence intervals (CI) of each factor for the eyewash user compared to non-eyewash user groups are shown in Table 4. Independent factors associated with eyewash use included younger age, higher BMI, history of psychiatric disease, past CL use, current CL use, shorter sleep duration per day, active smoking, frequent yogurt intake, higher TNSS, higher TNNSS, and higher J-OSDI total scores.
Factors associated with non-eyewash user compared to eyewash user in individuals with eye symptoms related to hay fever
The factors associated with non-eyewash users (vs. eyewash users) among individuals with eye symptoms related to hay fever are shown in Table 5. Older age, lower BMI, shorter sleep duration per day, and moderate-to-severe DE symptoms were independently associated with non-eyewash user compared with that in the user group among individuals with eye symptoms related to hay fever.
Discussion
Hay fever, exacerbated by seasonal allergens, is an allergic disease that requires ongoing and effective patient self-care in addition to topical ophthalmic and oral treatments. In this study, we performed a digital cohort study using AllerSearch for comprehensive profiling of eyewash usage among patients with hay fever to identify patterns of self-care and features related to the disease. Notably, 40.7% of participants with hay fever used eyewash products for symptom management. Patients with more severe ocular symptoms had higher eyewash usage, with a pattern of greater adoption among younger participants. Interestingly, older age and the presence of moderate-to-severe DE were associated with non-eyewash use among patients with hay fever and ocular symptoms. This suggests that older patients and those with hay fever and concomitant DE disease who do not routinely use eyewash—despite evidence of a reduction in early-phase ocular symptoms and its safety profile—may represent vulnerable populations that could benefit from public health initiatives aimed at promoting and raising awareness of better self-care for hay fever.
The strengths of this study lie in its large-scale digital cohort using the AllerSearch app, which facilitated the collection of real-world data from a broad and diverse group of participants2,4,8,13. It provided valuable insights into eyewash usage as a self-management tool for hay fever, particularly highlighting its higher use among younger individuals. This finding could help target specific patient groups for education and personalized treatments, facilitating individualized care in hay fever management. In addition, the use of smartphone-based surveys offers an efficient alternative to traditional paper-based or interview-based studies14,15, allowing for easier participation and direct access to patients in their daily environments16. This enabled the study to gather substantial data, especially from younger populations7,17.
Commercial eyewash solutions, such as over-the-counter cup-type eyewashes, are widely available in Japan and are commonly used as irrigating solutions for ocular surfaces and conjunctival fornices18. However, a gap exists in understanding the current usage of eyewash and irrigation as self-management tools among patients with hay fever. In a digital cohort study using the AllerSearch app, we reported a 40.7% eyewash usage rate among participants with hay fever. In addition, this study identified that younger patients exhibited significantly higher usage of eyewash products than their older counterparts. This likely reflects the higher sensitivity and awareness of new medical information among younger generations, allowing for faster adoption of eye washing as part of their symptom care routine. Previous studies suggest younger generations exhibit higher sensitivity and awareness to new medical information, leading to faster adoption of self-management behaviors for chronic conditions19,20. This underscores the importance of educating older populations about the demonstrated efficacy of available new hay fever management tools, including eye washing. Additionally, specific to this population group, improving ease of use is essential, as patients may have limited mobility and capacity to perform activities of daily living, which can act as a barrier to the frequent use of eyewash products21. Proactive measures and self-management are particularly important for hay fever22,23, and promoting routine eye washing with or without ongoing symptoms to prevent disease onset and exacerbation may benefit patients. Furthermore, healthcare providers should educate patients and encourage eye irrigation alongside commonly prescribed topical ophthalmic drops and oral medications as valid self-management tools for patients with hay fever.
Our study revealed several characteristics of eyewash users with hay fever, including high BMI, history of psychiatric conditions, history of CL use, current CL use, shorter sleep duration, active smoking, frequent yogurt intake, lower TNSS, higher TNNSS, and higher J-OSDI total scores. As inferred from the higher eyewash usage among younger participants, the younger generation appears to be aware of the efficacy of eye washing against hay fever-related ocular symptoms and views it as an easily accessible self-management measure. However, despite experiencing active ocular symptoms, the lower usage of eyewash products among older participants highlights the need to target this population to promote awareness and education regarding their use. A previous report demonstrated an association between high BMI and allergic rhinitis24, with worse symptom severity among participants with higher BMI leading to a higher usage rate of eyewash products. Additionally, high stress and anxiety associated with numerous psychiatric conditions can predispose patients to hypersensitive states regarding physical discomfort25, and eye washing may have been utilized to mitigate ocular symptoms. Past and active CL use has been previously linked to exacerbated allergic conjunctivitis among patients with hay fever. Our results likely reflect the discontinuation of CL use and higher eyewash utilization to address ocular symptoms in CL users who are experiencing more frequent exacerbations26. Seasonal allergic conjunctivitis and allergic rhinitis secondary to hay fever are chronic conditions with long and recurrent disease courses. The resultant chronic ocular discomfort can cause sleep disturbances, which patients may attempt to mitigate through routine eyewash use to maintain good sleep hygiene27. The association between smoking and numerous ocular surface diseases, including DE and allergic eye disease, has been suggested in multiple reports2,28,29,30, and our results reinforce these previous findings. Interestingly, yogurt consumption has been posited to have anti-allergic effects, with efficacy shown in a study on allergic conjunctivitis31. Health-driven and motivated patients with hay fever may consume yogurt and use eyewash products to manage allergic conjunctivitis. However, the clinical relevance of yogurt intake in the context of hay fever management remains an area requiring further investigation. Regarding the association between eyewash use, ocular symptoms of hay fever, and DE severity, eyewash appears to be an intuitive choice for addressing ocular symptoms associated with hay fever among our participants. The unique characteristics associated with eyewash use among patients with hay fever observed in this study may reflect a complex relationship between self-care patterns and lifestyle, as well as physical and psychological factors beyond hay fever symptom severity, thus emphasizing the importance of a multifaceted, comprehensive evaluation when managing patients with hay fever. Furthermore, the identified characteristics of eye wash users should be carefully considered when generalizing the findings since this study included a higher proportion of women, with a greater prevalence of hay fever among participants than those among excluded2.
Our results indicated that eyewash users experienced more severe DE symptoms than their counterparts. Concerns and debates exist among ophthalmologists regarding the safety of frequent eyewash usage stemming from the commonly found preservatives in commercial eyewash products, namely benzalkonium chloride. However, reports have not shown a deleterious effect on DE or corneal epithelial damage before and after moderate eyewash use11,32. Cup-type eyewash products in Japan are often sold as quasi-drugs or pharmaceuticals under the Pharmaceuticals and Medical Devices Act, ensuring their product quality. In addition, most cup-type eyewash products are preservative-free, mitigating concerns related to toxic ocular surface diseases. A more likely explanation for this association is the overlap between DE and allergic conjunctivitis symptoms8,13,16,29,30, which acts as a confounder. Patients with hay fever and more severe ocular symptoms tend to use eyewash products more frequently. Our results also support the hypothesis of increased eyewash use during symptom exacerbation. Additionally, the beneficial effects of eyewash on hay fever-related ocular symptoms have been previously reported by Yazu et al.12. Hence, rather than indicating a causative effect of eyewash on DE, our results likely reflect that patients with more severe ocular symptoms, including both allergic conjunctivitis and DE, use eyewash as an effective self-care measure for both disease processes. However, more severe DE has been observed among eyewash users with ocular symptoms, suggesting concerns about exacerbating DE with frequent eyewash use. Therefore, initiatives to promote public awareness and education on the benefits of allergen removal and the low risk of ocular surface disease with proper eyewash and optimal preservation solution use may be warranted to diversify patient self-management tools and improve outcomes, particularly targeting patients with ocular symptoms.
This study has some limitations as a digital cohort study using a smartphone application, similar to those reported in previous studies29,30,33,34,35. First, this study may have been subject to selection bias based on age, sex, socioeconomic factors, and other user characteristics, thereby limiting its generalizability. Participants who were more interested in hay fever and who had experienced hay fever symptoms may have had increased motivation to complete all surveys and were subsequently included. Older adults lacking access to smart devices or mobile service providers may have been underrepresented, whereas younger people who utilize smart devices more often and those who can socioeconomically afford smartphones may have been overrepresented. mHealth accrued a nationally representative participant pool; however, many participants resided in urban localities, leading to possible geographical bias. Furthermore, the participants were limited to iPhone users in Japan, who might exhibit distinct behavioral and consumer habits. Therefore, a random sampling of controls from the general population may be ideal. Second, this study employed many self-administered surveys, leading to possible recall bias or overreporting. The internal validity of paper-based and smartphone-based questionnaires was demonstrated in our previous study29. However, socioeconomic status, education level, cultural background, and some important unmeasured factors related to hay fever were not investigated. In addition, the complications due to eye washing were not collected in this study. Third, this was a cross-sectional study; therefore, temporal relationships and causality between eye washing and the identified factors, such as BMI and yogurt intake could not be inferred. A longitudinal or interventional follow-up study could explore whether eye washing improves hay fever symptoms for establishing the causality. Additionally, this smartphone-based digital study determined the presence of hay fever based solely on the administered questionnaires and might be prone to false positives due to the lack of a physician-confirmed diagnosis. This study included various scoring systems and demographic questions, which could have contributed to extended completion times. In addition, the AllerSearch app does not automatically optimize illumination to a standard setting. Instead, the lighting adjustments were left to the discretion of users, allowing them to complete the survey under conditions they found most comfortable. They may cause potential issues of visual fatigue in completing the hay fever survey. Although the time to complete the survey was not explicitly measured for each participant, to reduce the risk of visual fatigue and minimize potential biases in responses, the survey was divided into manageable sections, with clear instructions provided throughout. Additionally, rigorous data quality checks were implemented to identify and correct any inconsistencies in the responses, including those potentially caused by fatigue-related errors. These measures were taken to ensure that the collected data remained accurate and reliable throughout the study. Another potential limitation of this study is the risk of rushed or random responses, especially if participants experienced visual fatigue or attempted to complete the survey rapidly. The extended completion times, associated with complex scoring systems and numerous demographic questions, may have contributed to fatigue and led some participants to select arbitrary responses without careful consideration. As retrospective validation of these responses was not possible, this could have led to false positives or inconsistencies in the data. This underscores the importance of managing survey duration and response patterns, particularly in self-administered digital studies, which was considered in our interpretation of the results. Furthermore, the sample size in this study was determined using the events per variable (EPV) approach44, which does not account for the statistical power of each exposure variable. Despite these limitations, AllerSearch, our in-house smartphone application, represents a novel digital tool for conducting research and collecting real-world data across diverse populations. The integration of technology and medical research may become mainstream in future methodologies.
In conclusion, this study identified the characteristics, behavioral patterns, and biological profiles related to eyewash use among individuals with hay fever using AllerSearch. Several unique factors associated with ocular symptoms in eyewash users and non-eyewash users have been identified. Notably, our results highlight the possibility that the older population and patients with more severe DE may not be utilizing eyewash for ocular symptoms of hay fever, which may have implications for guiding future targets for public initiatives on the efficacy, side effects, and safety profiles of commercial eyewash products for hay fever prevention and management.
Methods
AllerSearch smartphone application
The AllerSearch was initially developed using Apple Inc.’s (Cupertino, CA, USA) open-source framework, ResearchKit2,8,36. In Japan, AllerSearch was released on Apple’s App Store on February 1, 2018, and on Google Play (Google LLC, CA, USA) on August 26, 2020, under a consignment contract with Juntendo University Graduate School of Medicine, Tokyo, Japan, and InnoJin, Inc., Tokyo, Japan36. It is freely available on both platforms. AllerSearch includes functionalities for electronic patient-reported data collection, with questionnaires in formats specified by validated scales15,37.
The survey questionnaires in AllerSearch were developed through a consensus process by a scientific committee consisting of allergy specialists, ophthalmologists, otolaryngologists, epidemiologists, and members of Patient and Public Involvement (PPI)7,8.
Study enrollment and participants
This digital cross-sectional observational cohort study with prospective data collection was conducted using the iPhone operating system version of the AllerSearch between February 1, 2018, and May 1, 20202,8. Potential participants were recruited via Apple’s App Store, and the study was announced through online media (https://allergy-search.com) and social networking service platforms (X: https://x.com/allersearch and Facebook: https://www.facebook.com/allersearchapp/). All participants provided eConsent after being informed about the nature of the study and its potential consequences.
This study was approved by the Independent Ethics Committee of Juntendo University Graduate School of Medicine (approval number 17–061) and was conducted in accordance with the principles of the Declaration of Helsinki38. The methodology and results of this survey are reported according to the checklist for reporting results of internet e-surveys39.
The study participants downloaded AllerSearch using their own App Store credentials. Those who consented completed a basic information survey and submitted daily hay fever monitoring surveys. The data collected included demographics, medical history, residential environment, lifestyle information, hay fever status, and preventive behaviors. Supplementary Table 1 lists the specific questions and parameters used for data collection. Subsequently, participants used the “daily tasks” function to receive daily assessments of the conjunctiva and complete questionnaires on hay fever, including the nasal symptom score (NSS), non-nasal symptom score (NNSS)40, daily subjective symptoms, and work productivity.
User data collection
The AllerSearch was used to collect participant data on demographics, medical history, residential environment, lifestyle information, hay fever status, preventive behaviors against hay fever, DE symptoms, hay fever-related quality of life, lower eyelid conjunctival hyperemia (assessed using a smartphone camera), environmental data (temperature, humidity, pollen, and particulate matter 2.5), and ___location data via global positioning system (GPS)2,13.
This study included those who provided eConsent and completed all required components, including the surveys on characteristics, lifestyle factors, hay fever status, and daily hay fever monitoring. Data points identified as outlier data or missing GPS information were excluded. From this refined dataset, individuals diagnosed with hay fever were selected for inclusion in the analysis.
Assessment of hay fever symptoms
Participants were classified into three groups (non-hay fever, hay fever, and unknown) according to their responses to the following question: “Do you have hay fever?” (Supplementary Table 1). Hay fever symptoms were evaluated using composite scores, including the NSS and NNSS (Supplementary Table 2). The NSS comprises items pertaining to rhinorrhea, nasal congestion, nasal itching, sneezing, and interference with daily life. The NNSS consists of items pertaining to itchy eyes, watery eyes, eye redness, itchy ears, and a dry mouth. Each item of the NSS and NNSS was scored on a four-point scale: 0 = no symptoms, 1 = mild symptoms, 2 = moderate symptoms, and 3 = severe symptoms40. The TSS was the sum of the individual scores for the NSS and NNSS (range: 0–36 points). The presence of ocular manifestations related to hay fever was defined as a total score of ≥ 3 points in any of the first three NNSS items.
Assessment of DE symptoms
DE symptoms were assessed using the 12-item J-OSDI questionnaire, which evaluates the severity of DE symptoms based on ocular symptoms, impact on visual functioning, and environmental triggers41,42. The J-OSDI total scores are based on a 100-point scale, with scores of 0–12, 13–22, 23–32, and 33–100 points representing normal healthy eyes, mild DE, moderate DE, and severe DE, respectively43. Symptomatic DE was defined as a J-OSDI total score ≥ 13 points30.
Statistical analysis
Participant characteristics were compared between eyewash users and non-eyewash users. Continuous variables are presented as medians and interquartile ranges for non-normally distributed variables based on the Shapiro–Wilk test, and categorical variables are presented as percentages. The Mann–Whitney U test was performed for non-normally distributed continuous variables, and the chi-square test was used for categorical variables. Differences with P-values < 0.05 were considered statistically significant.
Multivariate logistic regression analyses were performed to identify factors associated with eyewash users (versus non-eyewash users) among individuals with hay fever and eyewash non-eyewash users (versus eyewash users) among individuals with eye manifestations of hay fever, with results presented ORs and 95% CIs. To account for potential confounding factors, variables were selected a priori based on existing literature and clinical considerations through a consensus process by a scientific committee consisting of allergy specialists, ophthalmologists, otolaryngologists, epidemiologists, and members of PPI7,8.
The required minimum sample size was determined based on the requirements for multivariate logistic regression analysis. Following the conventional rule of EPV of 10, a sample size was considered sufficient when the number of individuals in the smallest category exceeded 30044.
All data were analyzed using STATA (version 15.1; Stata Corp, College Station, TX, USA) and GraphPad Prism (version 10.2.0; La Jolla, CA, USA).
PPI
PPI principles were not implemented during the initial planning, execution, and analysis of this project.
Data availability
The data that support the findings of this study are available from the corresponding author, [T.I.], upon reasonable request.
References
Sheikh, A., Singh Panesar, S., Salvilla, S. & Dhami, S. Hay fever in adolescents and adults. BMJ Clin. Evid. 2009, 0509 (2009).
Inomata, T. et al. Individual characteristics and associated factors of hay fever: A large-scale mHealth study using AllerSearch. Allergol Int 71, 325–334. https://doi.org/10.1016/j.alit.2021.12.004 (2022).
Yamada, T., Saito, H. & Fujieda, S. Present state of Japanese cedar pollinosis: the national affliction. J. Allergy Clin. Immunol. 133, 632-639.e635. https://doi.org/10.1016/j.jaci.2013.11.002 (2014).
Inomata, T. et al. Individual multidisciplinary clinical phenotypes of nasal and ocular symptoms in hay fever: Crowdsourced cross-sectional study using AllerSearch. Allergol. Int. 72, 418–427. https://doi.org/10.1016/j.alit.2023.01.001 (2023).
Akasaki, Y. et al. Impact of COVID-19 on care-seeking patterns for hay fever in Japan: A retrospective claims database cohort study. Allergy 79, 1056–1060. https://doi.org/10.1111/all.15947 (2024).
Akasaki, Y. et al. The impact of COVID-19 on hay fever treatment in Japan: A retrospective cohort study based on the Japanese claims database. Clin. Transl. Allergy 14, e12394. https://doi.org/10.1002/clt2.12394 (2024).
Inomata, T. et al. New medical big data for P4 medicine on allergic conjunctivitis. Allergol. Int. 69, 510–518. https://doi.org/10.1016/j.alit.2020.06.001 (2020).
Inomata, T. et al. Symptom-based stratification for hay fever: A crowdsourced study using the smartphone application AllerSearch. Allergy 76, 3820–3824. https://doi.org/10.1111/all.15078 (2021).
Okubo, K. et al. Japanese guidelines for allergic rhinitis 2020. Allergol. Int. 69, 331–345. https://doi.org/10.1016/j.alit.2020.04.001 (2020).
Miyazaki, D. et al. Japanese guidelines for allergic conjunctival diseases 2020. Allergol. Int. 69, 346–355. https://doi.org/10.1016/j.alit.2020.03.005 (2020).
Yazu, H., Kozuki, N., Dogru, M., Shibasaki, A. & Fujishima, H. The effect of long-term use of an eyewash solution on the ocular surface mucin layer. Int. J. Mol. Sci. https://doi.org/10.3390/ijms20205078 (2019).
Yazu, H., Dogru, M., Matsumoto, Y. & Fujishima, H. Efficacy and safety of an eye wash solution in allergic conjunctivitis after conjunctival allergen challenge. Ann. Allergy. Asthma. Immunol. 117, 565–566. https://doi.org/10.1016/j.anai.2016.08.030 (2016).
Inomata, T. et al. Using the allersearch smartphone app to assess the association between dry eye and hay fever: mhealth-based cross-sectional study. J. Med. Internet Res. 25, e38481. https://doi.org/10.2196/38481 (2023).
Nagino, K. et al. Minimal clinically important differences with the outcomes of the app-based japanese allergic conjunctival diseases quality of life questionnaire: cross-sectional observational study. JMIR Form Res 8, e60731. https://doi.org/10.2196/60731 (2024).
Akasaki, Y. et al. Reliability and validity of electronic patient-reported outcomes using the smartphone app allersearch for hay fever: prospective observational study. JMIR Form Res 6, e38475. https://doi.org/10.2196/38475 (2022).
Inomata, T. et al. Smartphone-based digital phenotyping for dry eye toward P4 medicine: a crowdsourced cross-sectional study. NPJ Digit. Med. 4, 171. https://doi.org/10.1038/s41746-021-00540-2 (2021).
Inomata, T. et al. Using medical big data to develop personalized medicine for dry eye disease. Cornea 39(Suppl 1), S39-s46. https://doi.org/10.1097/ico.0000000000002500 (2020).
Mimura, T. et al. Cleaning effects of eyewashes on ocular surface symptoms caused by air pollution in a single-center, two-arm, nonrandomized trial in Indonesia: first report from Jakarta study. Environ. Sci. Pollut. Res. Int. 31, 10967–10975. https://doi.org/10.1007/s11356-024-31982-2 (2024).
Dobson, K. G. & Hall, P. A pilot study examining patient attitudes and intentions to adopt assistive technologies into type 2 diabetes self-management. J. Diabetes Sci. Technol. 9, 309–315. https://doi.org/10.1177/1932296814560395 (2015).
Goonawardene, N., Jiang, J., Tan, S. & Jiang, Z. Online health information seeking and dolescents’ intention towards health self-management. Proceedings - Pacific Asia Conference on Information Systems, PACIS 2013 (2013).
Burns, E. & Mulley, G. P. Practical problems with eye-drops among elderly ophthalmology outpatients. Age Ageing 21, 168–170. https://doi.org/10.1093/ageing/21.3.168 (1992).
Fukushima, A., Miyazaki, D., Kishimoto, H. & Ebihara, N. Efficacy of proactive topical antihistamine use in patients with seasonal allergic conjunctivitis. Adv. Ther. 39, 5568–5581. https://doi.org/10.1007/s12325-022-02324-w (2022).
Tamayama, K., Hoshi, S. L., Kondo, M. & Okubo, I. Cost-effectiveness analysis of pre-seasonal medication for cedar pollinosis in Japan. Yakugaku Zasshi 130, 1725–1736. https://doi.org/10.1248/yakushi.130.1725 (2010).
Harugop, A. S., Walia, A., Havaldar, R. R. & Mudhol, R. S. Correlation between allergic rhinitis and body mass index: an observational study. Indian J Otolaryngol Head Neck Surg 74, 1033–1036. https://doi.org/10.1007/s12070-020-02095-2 (2022).
Lautenbacher, S., Spernal, J., Schreiber, W. & Krieg, J. C. Relationship between clinical pain complaints and pain sensitivity in patients with depression and panic disorder. Psychosom. Med. 61, 822–827. https://doi.org/10.1097/00006842-199911000-00015 (1999).
Fujio, K. et al. Effect of antihistamine-releasing contact lenses on ocular symptoms and treatment behavior in patients with seasonal allergic conjunctivitis: A retrospective study. Heliyon 10, e33385. https://doi.org/10.1016/j.heliyon.2024.e33385 (2024).
Koinis-Mitchell, D., Craig, T., Esteban, C. A. & Klein, R. B. Sleep and allergic disease: a summary of the literature and future directions for research. J. Allergy Clin. Immunol. 130, 1275–1281. https://doi.org/10.1016/j.jaci.2012.06.026 (2012).
Stapleton, F. et al. TFOS lifestyle: Impact of societal challenges on the ocular surface. Ocul. Surf. 28, 165–199. https://doi.org/10.1016/j.jtos.2023.04.006 (2023).
Inomata, T. et al. Risk factors for severe dry eye disease: crowdsourced research using DryEyeRhythm. Ophthalmology 126, 766–768. https://doi.org/10.1016/j.ophtha.2018.12.013 (2019).
Inomata, T. et al. Characteristics and risk factors associated with diagnosed and undiagnosed symptomatic dry eye using a smartphone application. JAMA Ophthalmol. 138, 58–68. https://doi.org/10.1001/jamaophthalmol.2019.4815 (2020).
Hara, Y. et al. Effect of mandarin orange yogurt on allergic conjunctivitis induced by conjunctival allergen challenge. Invest. Ophthalmol. Vis. Sci. 58, 2922–2929. https://doi.org/10.1167/iovs.16-21206 (2017).
Iwashita, M. & Murato, D. Effect of eyewash solution (commercial washing solution) on the corneal epithelium: adverse effects of benzalkonium chloride on the eye surface. J. Clin. Exp. Ophthalmol. https://doi.org/10.4172/2155-9570.1000571 (2016).
Eguchi, A. et al. Heterogeneity of eye drop use among symptomatic dry eye individuals in Japan: large-scale crowdsourced research using DryEyeRhythm application. Jpn. J. Ophthalmol. https://doi.org/10.1007/s10384-020-00798-1 (2021).
Inomata, T. et al. Stratification of individual symptoms of contact lens-associated dry eye using the iphone app DryEyeRhythm: crowdsourced cross-sectional study. J. Med. Internet Res. 22, e18996. https://doi.org/10.2196/18996 (2020).
Inomata, T. et al. Association between dry eye and depressive symptoms: Large-scale crowdsourced research using the DryEyeRhythm iPhone application. Ocul Surf 18, 312–319. https://doi.org/10.1016/j.jtos.2020.02.007 (2020).
Inomata, T. et al. New medical big data for P4 medicine on allergic conjunctivitis. Allergol Int https://doi.org/10.1016/j.alit.2020.06.001 (2020).
Nagino, K. et al. The minimal clinically important difference of app-based electronic patient-reported outcomes for hay fever. Clin Transl Allergy 13, e12244. https://doi.org/10.1002/clt2.12244 (2023).
World Medical Association (AMM). Helsinki declaration. ethical principles for medical research involving human subjects. Assist. Inferm. Ric. 20, 104–107 (2001).
Eysenbach, G. Improving the quality of web surveys: the checklist for reporting results of internet E-surveys (CHERRIES). J. Med. Internet Res. 6, e34. https://doi.org/10.2196/jmir.6.3.e34 (2004).
Kirtsreesakul, V., Somjareonwattana, P. & Ruttanaphol, S. The correlation between nasal symptom and mucociliary clearance in allergic rhinitis. Laryngoscope 119, 1458–1462. https://doi.org/10.1002/lary.20146 (2009).
Schiffman, R. M., Christianson, M. D., Jacobsen, G., Hirsch, J. D. & Reis, B. L. Reliability and validity of the ocular surface disease index. Arch. Ophthalmol. 118, 615–621 (2000).
Midorikawa-Inomata, A. et al. Reliability and validity of the Japanese version of the ocular surface disease index for dry eye disease. BMJ Open 9, e033940. https://doi.org/10.1136/bmjopen-2019-033940 (2019).
Miller, K. L. et al. Minimal clinically important difference for the ocular surface disease index. Arch. Ophthalmol. 128, 94–101. https://doi.org/10.1001/archophthalmol.2009.356 (2010).
Peduzzi, P., Concato, J., Kemper, E., Holford, T. R. & Feinstein, A. R. A simulation study of the number of events per variable in logistic regression analysis. J. Clin. Epidemiol. 49, 1373–1379. https://doi.org/10.1016/s0895-4356(96)00236-3 (1996).
Acknowledgements
We thank the members of our patient panel for their advice, which has improved our research project, and the Medical Logue, Inc. (Tokyo, Japan) for developing and releasing the iOS and Android versions of AllerSearch.
Funding
This work was supported by the Japan Agency for Medical Research and Development [grant numbers JP20ek0410063 (T.I.), 24ek0410090s0503 (T.I.)]; Japan Society for the Promotion of Science, Grants-in-Aid for Scientific Research [grant numbers: 22K16983 (A.E.), 23K16364 (A.M.I), 24K19796 (A.E)]; the Institute for Environmental & Gender-specific Medicine, Juntendo University; and the OTC Self-Medication Promotion Foundation. The funding sources had no role in the study design; collection, analysis, and interpretation of data; writing of the report; and in the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
Takenori Inomata: Conceptualization, Data curation, Formal analysis, Funding acquisition, Methodology, Project administration, Resources, Software, Visualization, Writing- Original draft preparation, Writing- Reviewing and Editing. Jaemyoung Sung: Visualization, Writing- Original draft preparation, Writing- Reviewing and Editing Ken Nagino: Data curation, Formal analysis, Writing- Original draft preparation. Akie Midorikawa-Inomata: Formal analysis, Funding acquisition, Writing- Original draft preparation, Writing- Reviewing and Editing. Atsuko Eguchi: Funding acquisition, Writing- Original draft preparation, Writing- Reviewing and Editing. Takeya Adachi: Project administration, Writing- Original draft preparation, Writing- Reviewing and Editing. Hiroyuki Kobayashi: Supervision, Writing- Original draft preparation, Writing- Reviewing and Editing. Shintaro Nakao: Supervision, Writing- Original draft preparation, Writing- Reviewing and Editing. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
AllerSearch was created using Apple’s ResearchKit (Cupertino, CA, USA). T.I. is the owner of InnoJin, Inc., Tokyo, Japan who developed AllerSearch. T.I. reports non-financial support from Lion Corporation. and Sony Network Communications Inc.; grants from Yuimedi Inc., ROHTO Pharmaceutical Co. Ltd., Kobayashi Pharmaceutical Co. Ltd., and Kandenko Co. Ltd.; and personal fees from Santen Pharmaceutical Co. Ltd., and InnoJin Inc., outside the submitted work. K.N. and A.M.I. reported receiving personal fees from InnoJin, Inc. S.N. reported grants from Kowa Co. Ltd., Mitsubishi Tanabe Pharma Corp., Alcon Japan, Ltd., Santen Pharmaceutical Co. Ltd., Machida Endoscope Co. Ltd., Wakamoto Pharmaceutical Co. Ltd., Bayer Yakuhin Ltd., Senju Pharmaceutical Co. Ltd., Nippon Boehringer Ingelheim Co. Ltd., Chugai Pharmaceutical Co. Ltd., Hoya Corp., and Novartis Pharma KK, outside the submitted work. The remaining authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Inomata, T., Sung, J., Nagino, K. et al. Profiling eyewash usage and preferences in individuals with hay fever using a digital cross-sectional cohort study with AllerSearch. Sci Rep 15, 8275 (2025). https://doi.org/10.1038/s41598-025-93027-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-93027-z