Abstract
This study utilized a longitudinal survey in Japan to investigate whether higher Central Sensitization Inventory (CSI) scores, serving as a proxy for central sensitization-related symptoms, are associated with an increased risk of developing chronic low back pain (CLBP), focusing on the impact of the coronavirus disease (COVID-19) pandemic on these conditions. Healthy volunteers (n = 227; mean age: 68.5 ± 9.5 years) were surveyed at baseline (July 2019) and at follow-up (October 2020). The participants were categorized into four groups based on their CLBP status: None, De novo, Continued, and Improved. CLBP prevalence increased from 26% at baseline to 32% at follow-up. Higher baseline CSI scores (odds ratio [OR] 1.05, 95% confidence interval [CI] 1.02–1.09; p = 0.005) and older age (OR 1.06, 95% CI 1.02–1.11; p = 0.007) were identified as significant risk factors for developing CLBP. The mean CSI scores exhibited a slight non-significant increase from 16.9 ± 11.4 to 17.1 ± 11.7. Participants who adhered more strictly to the COVID-19 guidelines and engaged in reduced physical activity reported a higher CLBP prevalence. Our findings suggest that early identification and management of central sensitization are crucial for improving clinical outcomes, particularly during periods of external stress, such as the COVID-19 pandemic.
Similar content being viewed by others
Introduction
Chronic low back pain (CLBP) is a prevalent and debilitating condition that affects millions of individuals worldwide1. It is a leading cause of disability and has profound socioeconomic implications, affecting an estimated 23% of the world’s population at any given time2. CLBP is defined as pain localized between the lower end of the 12th rib and the inferior gluteal fold that persists for more than three months. Various mechanical, psychological, and biological factors contribute to the onset and persistence of CLBP. Central sensitization (CS) refers to the increased responsiveness of nociceptive neurons in the central nervous system to normal or subthreshold afferent input3. This phenomenon has been implicated in various chronic pain conditions including CLBP. The Central Sensitization Inventory (CSI) is a widely used tool for assessing self-reported symptoms commonly associated with CS, providing a standardized method to evaluate the severity of these symptoms in patients4,5. The coronavirus disease (COVID-19) pandemic, which was declared in early 2020, substantially impacted public health and daily life globally6,7. Several studies have reported that lockdowns, social distancing protocols, and changes in daily routines significantly reduced physical activity levels while increasing sedentary behaviors, psychological distress, and musculoskeletal pain conditions8,9. Moreover, healthcare access restrictions, including delayed elective procedures and limited rehabilitation services, have been associated with worsening outcomes for patients with chronic musculoskeletal conditions, including chronic low back pain (CLBP)10,11,12. Understanding the relationship between CS and CLBP during a pandemic is essential for developing effective management strategies. Previous studies have revealed a significant association between higher CSI scores—reflecting centrally-driven hypersensitivity—and various chronic pain conditions, including CLBP3,4,5. The CSI has been validated as an effective screening tool for CS4,5, comprising 25 questions that include symptoms such as sleep disturbances, emotional distress, and sensitivity to light and smell. Higher CSI scores are associated with greater pain severity and poorer clinical outcomes in patients with CLBP13. The prevalence of CLBP is well-documented, with studies reporting rates of approximately 20–30% in adult populations14,15. However, the influence of demographic factors and temporal changes, particularly in response to significant events, such as the COVID-19 pandemic, are not well understood. The pandemic introduced unique challenges that may have potentially influenced the prevalence and severity of CLBP through increased sedentary behaviors and stress. The known risk factors for CLBP include age, sex, and psychological factors, while the role of body mass index (BMI) remains controversial, with inconsistent findings reported in the literature16,17,18. Nevertheless, the role of CS as a predictive factor for the onset and persistence of CLBP has not been fully examined in longitudinal studies. Although previous studies identified an association between CLBP and symptoms commonly linked to central sensitization (CS), these symptoms do not affect all individuals with CLBPs19,20,21. The influence of baseline CS levels on the trajectory of CLBP over time, particularly in the context of external factors, such as the COVID-19 pandemic, warrants investigation. Additionally, the effects of pandemic-related changes on CLBP and CS remain unclear. The reduction in physical activity and increased psychological stress during the pandemic may have exacerbated CLBP symptoms. However, empirical data regarding this relationship are lacking. Furthermore, there is insufficient information regarding the CSI score thresholds that predict the development of CLBP. Hence, identifying specific CSI cutoff points that correlate with increased risk can enhance early intervention strategies and potentially improve patient outcomes.
We hypothesized that higher baseline CSI scores would be predictive of the development of CLBP and that pandemic-related factors would influence the prevalence and severity of CLBP. To test this hypothesis, we performed this study with the primary objective of clarifying the relationship between CS and CLBP, using a longitudinal survey conducted in Japan. This study utilized data collected before and after the emergence of the COVID-19 pandemic, thereby providing a unique opportunity to examine the impact of the global health crisis on CLBP and CS. The secondary objectives were to investigate changes in CSI scores and the prevalence of CLBP, and CSI scores over the study period to identify baseline characteristics and risk factors associated with the development and persistence of CLBP. By focusing on a specific population in rural Japan, this study provides insights into the relationship between CS and CLBP in a demographic context that may be underrepresented in existing research. The findings of this study can inform clinical practice and public health policies aimed at mitigating the impact of CLBP, particularly in the context of unprecedented global events such as the COVID-19 pandemic.
Methods
Ethical considerations
This longitudinal study was approved by the Wakayama Medical University Research Ethics Committee (No. G92). All participants provided written informed consent for the inclusion and publication of their data. All procedures were performed in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and the Declaration of Helsinki.
Study design
This is an observational cohort study designed to examine the relationship between CS and CLBP. We utilized data from a large-scale, prospective study focused on screening for arteriosclerosis in a population-based cohort from Japan. This longitudinal survey was conducted during the COVID-19 pandemic, thereby providing a unique context for examining changes in CLBP prevalence and CS levels. The study was conducted in rural areas of Japan. Baseline data were collected in July 2019, prior to the spread of COVID-19, and follow-up data were collected in October 2020, during the pandemic. Data were obtained from a previous study that included comprehensive health information from healthy volunteers residing in rural Japan. The present study focused on a sub-cohort of participants who provided data at baseline and the follow-up evaluation.
Population
The study population comprised community-dwelling adults who participated in both the baseline survey in July 2019 and the follow-up survey in October 2020. Participants included individuals with and without chronic low back pain (CLBP). Those with serious comorbidities or debilitating conditions unrelated to CLBP were excluded from the study. Follow-up invitations were sent to all 771 participants from the baseline survey, and 227 individuals completed the follow-up assessment. Participants who failed to respond to the follow-up survey were excluded from the analysis.
Data collection
The process of data collection included two primary surveys:
-
1.
Baseline Survey (July 2019):
-
Participants provided demographic information and anthropometric measurements (height, weight, and BMI) and completed the CSI, a validated tool for assessing self-reported symptoms associated with CS. Since all participants in this study were native Japanese speakers, we utilized the Japanese version of the CSI, which has been validated and demonstrated strong reliability4. Furthermore, the CSI has demonstrated high validity and reliability in multiple languages, including English22, Spanish23, Dutch24, and Turkish25, supporting its cross-cultural applicability in assessing CS-related symptoms.
-
The presence of CLBP was assessed using a self-reported questionnaire at both baseline and follow-up. Participants were asked: 'Have you experienced low back pain (pain localized between the lower end of the 12th rib and the inferior gluteal fold) that persisted for more than three months?' (Response options: Yes / No). Participants who responded ‘Yes’ were classified as having CLBP.
-
-
2.
Follow-up Survey (October 2020):
-
Participants were reassessed for CLBP using the same criteria as at baseline and completed the CSI again.
-
Additional questions regarding changes in physical activity and behavior due to the COVID-19 pandemic were incorporated.
Physical activity assessment
-
Participants were asked the flowing question:
-
'Has your physical activity level changed compared to before the COVID-19 pandemic?' (Response options: Increased / Decreased / No change).
Physical Activity was defined as any light to moderate activity that may not significantly increase heart rate or breathing, including walking, light jogging, and exercise routines.
Social behavior assessment
-
Participants were asked the flowing question:
-
'Has your physical activity level changed compared to before the COVID-19 pandemic?' (Response options: Increased / Decreased / No change).
Physical Activity was defined as any light to moderate activity that may not significantly increase heart rate or breathing, including walking, light jogging, and exercise routines.
Social Behavior was defined as interactions and activities involving communication or shared experiences with others, including outdoor activities, in-person social interactions, and participation in community events.
These additional questions were employed to analyze potential behavioral factors contributing to the incidence and persistence of CLBP during the study period.
-
Outcome measures
The primary outcome measures were as follows:
-
Central Sensitization Inventory (CSI): The CSI, comprising parts A and B, is a screening tool used to identify the presence of central sensitivity syndrome, and the CSI-J, a Japanese translation of the CSI, is used in clinical practice4,5. Part A of the CSI comprises a scoring system includes 25 self-reported items on symptoms associated with central sensitivity scored from 0 to 100 points, with 0 and 100 representing the best and worst scores, respectively. Part B of the CSI is used to screen for previous diagnoses of CS syndromes that have been associated with CS components, and are included in the CS syndrome family26,27. A CSI score ≥ 30 points was considered indicative of CS, as previously reported4,5,26,27. The total score (0–100) was calculated by summing the scores for each of the 25 questions in Part A and the mean score and distribution of the five categories (0:0–9, 1:10–19, 2:20–29, 3:30–39, 4: ≥ 40) were assessed. The presence or absence of a history of the ten CS syndromes identified in Part B of the CSI-J was also evaluated. The CSI scores were obtained at both the baseline and follow-up assessments.
-
Prevalence of CLBP: CLBP was defined as pain localized between the lower end of the 12th rib and the inferior gluteal fold that persisted for more than three months28,29. The prevalence of CLBP was assessed at the baseline and follow-up evaluations.
-
Changes in Physical Activity and Behavior: Changes in physical activity, social behavior, and adherence to COVID-19 guidelines were assessed at follow-up using self-reported questionnaires. These assessments were conducted based on the specific questions described in the Data Collection section.
Group classification
The participants were categoerized into four groups based on the presence or absence of CLBP at baseline and at follow-up.
-
None Group: No CLBP at both baseline and follow-up.
-
De novo Group: No CLBP at baseline, but CLBP at follow-up.
-
Continued Group: Presence of CLBP at both baseline and follow-up.
-
Improved Group: Presence of CLBP at baseline, but no CLBP at follow-up.
Age groups (< 65 years, 65–74 years, and ≥ 75 years) were defined based on classifications commonly employed in geriatric and musculoskeletal research30. These categories correspond to younger adults (< 65 years), the ‘young-old’ population (65–74 years), and the ‘old-old’ population (≥ 75 years), reflecting differing stages of age-related musculoskeletal and functional changes.
Statistical analysis
All statistical analyses were performed using JMP version 16 software (SAS Inc., Cary, NC, USA). A priori power calculation was not performed due to the retrospective nature of the study and the use of an existing dataset. However, a post hoc power analysis was conducted to evaluate the adequacy of the sample size for detecting associations between CSI scores and CLBP prevalence. Assuming an effect size of 0.3, a significance level of 0.05, and a sample size of 227 participants, the statistical power was calculated to be approximately 80%. Baseline characteristics were compared among the four groups using analysis of variance or Kruskal–Wallis tests for continuous variables, depending on their distribution, and chi-square tests for categorical variables.
The primary outcomes analyzed were changes in the prevalence of chronic low back pain (CLBP) and Central Sensitization Inventory (CSI) scores from baseline to follow-up. Descriptive statistics were calculated for each group, and changes over time were assessed using paired t-tests or Wilcoxon signed-rank tests, as appropriate.
To identify risk factors for the development of CLBP, multiple logistic regression analysis was conducted on a subset of participants (n = 163) without CLBP at baseline. Explanatory variables included baseline age, sex, body mass index (BMI), and CSI scores. Variables with p-values < 0.1 in univariate analyses were included in the multivariate logistic regression model. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated.
Subgroup analyses were conducted to ascertain whether the relationship between CSI scores and CLBP varied across age groups (< 65 years, 65–74 years, and ≥ 75 years), sex, and BMI categories. Further analyses were performed to evaluate the impact of COVID-19-related behavioral changes, such as adherence to guidelines and changes in physical activity levels, on the prevalence of CLBP.
The fit of the logistic regression model was assessed using the Hosmer–Lemeshow test, and its predictive ability was evaluated by calculating the area under the receiver operating characteristic curve. Statistical significance was set at p < 0.05 for all analyses.
Results
Participant characteristics
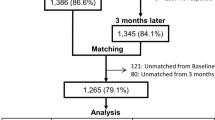
Among the 771 individuals invited to participate in the follow-up survey, 227 (79 men, 148 women; mean age at baseline: 68.5 ± 9.5 years) completed both baseline and follow-up assessments and were included in the analysis (Fig. 1). The demographic and clinical characteristics of the participants at baseline are summarized in Table 1. No significant differences were observed in sex distribution or BMI among the four groups (None, De novo, Continued, Improved). However, significant differences were identified in the baseline age and CSI scores. The post-hoc test results indicated no significant differences between the groups regarding age. Moreover, the post-hoc test results revealed significant differences in the mean baseline CSI score between the None and Continued groups (p = 0.001), with no significant differences observed between the other groups.
Changes in CLBP prevalence and CSI scores
The prevalence of CLBP increased from 26% (59/227) at baseline to 32% (71/227) at the follow-up assessment (Table 2). However, this increase was not statistically significant (p = 0.06). The mean CSI score was 16.9 ± 11.4 at baseline and 17.1 ± 11.7 at follow-up, indicating a slight but non-significant increase over the observation period.
Risk factors for the development of CLBP
In the sub-analysis of the risk factors for new-onset CLBP, the p-values were less than 0.1 for age and CSI score at baseline. We used these two factors as explanatory variables for the multiple logistic regression analysis (Table 3). Multiple logistic regression analysis included 163 participants without CLBP at baseline to identify risk factors for the development of CLBP. The analysis revealed that higher baseline CSI scores (OR 1.05, 95% CI 1.02–1.09; p = 0.005) and older age (OR 1.06, 95% CI 1.02–1.11; p = 0.007) were significant risk factors for the development of CLBP (Table 4).
Subgroup analyses (Table 5)
-
Age: Older participants (≥ 75) exhibited the highest prevalence of CLBP (36%) and the highest mean CSI score (18.1). Participants aged 65–74 years and those below 65 years exhibited prevalences of CLBP and mean CSI scores of 32% and 17.5, and 28% and 16.2, respectively.
-
Sex: Females displayed a slightly higher prevalence of CLBP (33%) than males (30%). The mean CSI score was also slightly higher in females (17.3) than in males (16.8).
-
BMI: Participants with BMI ≥ 25 kg/m2 exhibited a higher prevalence of CLBP (34%) and a higher mean CSI score (17.9) compared to those with BMI < 25 kg/m2 (prevalence: 30%, mean CSI score: 16.5).
Additional analyses (Table 6)
-
Adherence to COVID-19 guidelines: Participants with high adherence to the COVID-19 protocols exhibited a higher prevalence of CLBP (34%) and a higher mean CSI score (17.4) than those with low adherence (prevalence: 30%, mean CSI score: 16.9).
-
Physical activity: Participants who reported decreased physical activity during the pandemic exhibited a higher prevalence of CLBP (33%) and a higher mean CSI score (17.5) than those who reported increased physical activity (prevalence: 28%, mean CSI score: 16.0). However, this difference was not statistically significant (p = 0.27). We conducted a multivariable logistic regression analysis to assess the association between changes in physical activity and the presence of CLBP at follow-up, adjusting for sex, age, BMI, and CSI score. The analysis indicated that participants who reported decreased physical activity during the pandemic exhibited higher odds of CLBP compared to those who maintained or increased their physical activity (adjusted OR: 1.29, CI: 0.62 – 2.69, p = 0.499). However, this association did not achieve statistical significance.
Discussion
In this study, we investigated the relationship between CS and CLBP in a Japanese cohort before and during the COVID-19 pandemic. Our findings indicate that the prevalence of CLBP increased from 26% at baseline to 32% at follow-up. Higher baseline CSI scores and older age were significant risk factors for the development of CLBP. The mean CSI score remained relatively stable, exhibiting only a slight increase from 16.9 at baseline to 17.1 at follow-up. The participants were categorized into four groups based on their CLBP status. Significant differences in baseline CSI scores and ages were observed among these groups, underscoring the importance of considering the CLBP status. This study provided several novel insights. First, it is one of the few longitudinal studies to investigate the direct impact of CS on the development and persistence of CLBP, particularly during the COVID-19 pandemic. The application of CSI provides a standardized and validated tool to assess self-reported symptoms commonly associated with CS, which enhances the reliability of our findings. However, it is important to note that CSI does not directly measure the physiological processes of CS.
Additionally, this study was conducted in rural Japan thereby providing unique demographic insights that are often underrepresented in global research. Although our analysis indicated a trend suggesting that decreased physical activity during the pandemic was associated with a higher prevalence of CLBP, this association was not statistically significant (adjusted OR: 1.29, CI: 0.62 – 2.69, p = 0.499). This finding is consistent with those of previous studies which suggest that reduced physical activity may contribute to deconditioning and increased sedentary behavior, both of which are linked to chronic pain exacerbation8,9,10,11,12. The lack of statistical significance in our study suggests that additional factors may be contributing to the observed differences in CLBP prevalence. Future studies with larger cohorts and more detailed measures of physical activity are warranted to clarify this relationship and further explore the role of behavioral modifications in chronic pain management. A particularly notable finding was the significant impact observed in voluntary activity over the period of one year. Despite the relatively short duration of the study, substantial changes in CLBP prevalence and associated risk factors were evident. Our findings suggest that changes in activity levels and external stressors may be associated with CLBP prevalence; however, given the descriptive nature of several analyses, these trends should be cautiously interpreted. While subgroup comparisons provided useful insights into differences across age, sex, and BMI categories, such comparisons alone do not establish causal relationships. Future studies incorporating longitudinal regression models and additional covariate adjustments are warranted to clarify the statistical associations between these factors and CLBP. This is particularly relevant for clinicians and policymakers, as it suggests that even short-term circumstances can meaningfully impact chronic pain outcomes, reinforcing the necessity for continuous monitoring and adaptive management strategies in response to changing conditions such as those induced by the pandemic.
Our findings align with those of previous research that identified CS as a significant factor in chronic pain31. Studies have consistently demonstrated that higher CSI scores correlate with greater pain severity and poorer clinical outcomes in CLBP patients13,32. The increase in CLBP prevalence observed in this study mirrors global trends, where the pandemic has exacerbated various health conditions due to increased stress and reduced physical activity7,33. However, our study adds to the literature by providing longitudinal data, which is less common in the existing research.
The identification of higher baseline CSI scores and older age as significant risk factors for the development of CLBP has important clinical implications. This suggests that early screening for CS using CSI could help identify individuals at a higher risk of developing CLBP, facilitating timely interventions. The stability of the mean CSI scores despite the pandemic indicates that CS levels may be relatively resistant to short-term external stressors, highlighting the need for the ongoing management of CS in patients with chronic pain. The observed increase in the prevalence of CLBP during the pandemic highlights the potential impact of lifestyle and environmental changes on chronic pain. While psychosocial stressors, including mental health factors, are known to influence chronic pain outcomes, our study did not include direct measures of mental health. Therefore, further research is required to evaluate the role of psychological factors in CLBP progression. Clinicians should consider incorporating strategies to manage CS and promote physical activity, even during periods of restricted movement, to mitigate the effects of external stressors on chronic pain. The significant impact observed over just one year of voluntary activity change highlights the rapid response of CLBP and CS to lifestyle and environmental factors. This finding is particularly relevant for clinicians and policymakers as it suggests that even short-term interventions can have meaningful effects on chronic pain outcomes. This reinforces the need for continuous monitoring and adaptive management strategies in response to changing circumstances such as those induced by pandemics.
This study had several limitations. The most significant limitation is the substantial decline in participant retention, with only approximately one-third of the participants in the initial study participating in the second study. This reduction was primarily due to the COVID-19 pandemic, which introduced several unprecedented challenges that affected our ability to follow up with participants.
One of the major limitations of this study is the low follow-up rate. While 771 individuals were invited to participate in the follow-up survey, only 227 (29.4%) completed both the baseline and follow-up assessments. We did not determine specific reasons for non-participation; however, given that invitations were sent during the second wave of COVID-19 infections in Japan, it is possible that pandemic-related concerns contributed to the low response rate. Other factors, such as scheduling conflicts, relocation, or mortality, may have also played a role. As a result, our study population may represent individuals with relatively higher activity levels or those more willing to engage in follow-up assessments, potentially introducing a selection bias. Future studies should aim to improve follow-up rates and investigate non-participation factors to enhance the generalizability of findings. The self-reported nature of the data, particularly concerning changes in physical activity and adherence to COVID-19 guidelines, introduces potential bias. Additionally, our study did not collect data on mental health status or psychological distress, which have been suggested as potential contributors to chronic pain development. As a result, we were unable to examine the impact of mental health on CLBP incidence and progression. Future studies should incorporate validated mental health assessments, such as depression or anxiety scales, to better understand their role in chronic pain conditions. Furthermore, the study population was limited to healthy volunteers from a specific geographic region of Japan, which may not be representative of the wider population. Additionally, although we conducted subgroup analyses and examined group differences, we acknowledge that these comparisons do not account for potential confounders, such as socioeconomic status, comorbidities, or baseline pain severity. The lack of multivariate modeling for some associations may have led to residual confounding. Future studies should integrate more comprehensive statistical approaches, including propensity score matching or multivariable regression, to better assess causal relationships between central sensitization-related symptoms, activity levels, and CLBP development. The reliance on CSI as the sole measure of CS, although validated, is a limitation as it assesses self-reported symptoms rather than directly measuring the neurophysiological processes underlying CS. Future studies should incorporate objective measures, such as quantitative sensory testing or functional imaging, to provide a more comprehensive evaluation of CS. While these factors present significant challenges, they also provide a unique context for understanding the impact of external stressors on CLBP and CS. Future studies should consider alternative data collection methods such as remote or telehealth approaches to mitigate the impact of similar disruptions and improve participant retention. Despite these limitations, the data collected offer valuable insights into the relationship between CS and CLBP during an unprecedented global health crisis, underscoring the importance of adaptable research methodologies in the face of external challenges.
In conclusion, this study highlights the significant role of CS in the etiology of CLBP. Higher baseline CSI scores and older age are key risk factors for CLBP, suggesting that early identification and management of symptoms associated with CS may potentially improve clinical outcomes. However, further research is required to explore objective methods for directly assessing CS. These findings emphasize the need for integrated approaches to chronic pain management that consider both biological and psychosocial factors. The significant impact observed over just one year of changes in voluntary activity underscores the importance of timely and adaptive interventions. Policymakers and healthcare providers should prioritize maintaining physical activity and addressing psychosocial stressors, particularly during periods of external stress such as those experienced during the COVID-19 pandemic. Future research should focus on larger and more diverse populations, and explore additional methods for measuring CS to validate and extend these findings.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
References
Agnus, T. A., Rajkumar, E., John, R. & Joshua, G. A. Determinants of quality of life in individuals with chronic low back pain: A systematic review. Health Psychol. Behav. Med. 10, 124–144 (2022).
Gouveia, N. et al. Prevalence and social burden of active chronic low back pain in the adult Portuguese population: Results from a national survey. Rheumatol. Int. 36, 183–197 (2016).
Woolf, C. J. Central sensitization: Implications for the diagnosis and treatment of pain. Pain 152, S2–S15 (2011).
Tanaka, K. et al. Validation of the Japanese version of the Central Sensitization Inventory in patients with musculoskeletal disorders. PLOS ONE 12, e0188719 (2017).
Mayer, T. G. et al. The development and psychometric validation of the central sensitization inventory. Pain Pract. 12, 276–285 (2012).
Chow, E. J., Uyeki, T. M. & Chu, H. Y. The effects of the COVID-19 pandemic on community respiratory virus activity. Nat. Rev. Microbiol. 21, 195–210 (2023).
Fallon, N. et al. Adverse effects of COVID-19-related lockdown on pain, physical activity and psychological well-being in people with chronic pain. Br. J. Pain 15, 357–368 (2021).
Stockwell, S. et al. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: A systematic review. BMJ Open Sport Exerc. Med. 7, e000960 (2021).
Meyer, J. et al. Changes in physical activity and sedentary behavior in response to COVID-19 and their associations with mental health in 3052 US adults. Int. J. Environ. Res. Public Health 17, 6469 (2020).
Fatoye, F., Fatoye, C., Lawoe, J., Mbada, C. & Gebrye, T. Does COVID-19 related lockdown restrictions impact people with musculoskeletal disorders? A systematic review. Musculoskelet. Care 22, e1920 (2024).
Gebrye, T., Niyi-Odumosu, F., Lawoe, J., Mbada, C. & Fatoye, F. The impact of COVID-19 related lockdown restrictions on musculoskeletal health: A systematic review. Rheumatol. Int. 43, 2011–2019 (2023).
Moretti, A. et al. Characterization of home working population during COVID-19 emergency: A cross-sectional analysis. Int. J. Environ. Res. Public Health. 17, 6284 (2020).
Miki, T., Nishigami, T., Takebayashi, T. & Yamauchi, T. Association between central sensitivity syndrome and psychological factors in people with presurgical low back pain: A cross-sectional study. J. Orthop. Sci. 26, 337–342 (2021).
Ishimoto, Y. et al. Association of lumbar spondylolisthesis with low back pain and symptomatic lumbar spinal stenosis in a population-based cohort: The Wakayama spine study. Spine 42, E666–E671 (2017).
Angst, F. et al. Epidemiology of back pain in young and middle-aged adults: A longitudinal population cohort survey from age 27–50 years. Psychosomatics 58, 604–613 (2017).
Shiri, R., Karppinen, J., Leino-Arjas, P., Solovieva, S. & Viikari-Juntura, E. The association between obesity and low back pain: A meta-analysis. Am. J. Epidemiol. 171, 135–154 (2010).
Hartvigsen, J. et al. What low back pain is and why we need to pay attention. Lancet 391, 2356–2367 (2018).
Shmagel, A., Foley, R. & Ibrahim, H. Epidemiology of chronic low back pain in US adults: Data from the 2009–2010 National Health and Nutrition Examination Survey. Arthritis Care Res. 68, 1688–1694 (2016).
Neblett, R., Hartzell, M. M., Cohen, H., Mayer, T. G. & Gatchel, R. J. Ability of the central sensitization inventory to identify central sensitivity syndromes in an outpatient chronic pain sample. Clin. J. Pain 31, 323–332 (2015).
Nijs, J. et al. Applying modern pain neuroscience in clinical practice: Criteria for the classification of central sensitization pain. Pain Physician 17, 447–457 (2014).
Roussel, N. A. et al. Central sensitization and altered central pain processing in chronic low back pain: Fact or myth?. Clin. J. Pain 29, 625–638 (2013).
Neblett, R., Hartzell, M. M., Mayer, T. G., Cohen, H. & Gatchel, R. J. Establishing clinically relevant severity levels for the central sensitization inventory. Pain Pract. 17, 166–175 (2017).
Roldán-Jiménez, C. et al. Structural validity and reliability of the Spanish Central Sensitization Inventory in breast cancer survivors. Pain Pract. 21, 740–746 (2021).
Zheng, X., Lamoth, C. J., Timmerman, H., Otten, E. & Reneman, M. F. Establishing central sensitization inventory cut-off values in Dutch-speaking patients with chronic low back pain by unsupervised machine learning. Comput. Biol. Med. 178, 108739 (2024).
Düzce Keleş, E. et al. Validity and reliability of the Turkish version of the central sensitization inventory. Arch. Rheumatol. 36, 518–526 (2021).
Clement, N. D., MacDonald, D., Howie, C. R. & Biant, L. C. The outcome of primary total hip and knee arthroplasty in patients aged 80 years or more. J. Bone Joint Surg. Br. 93, 1265–1270 (2011).
Skyttä, E. T., Jarkko, L., Antti, E., Huhtala, H. & Ville, R. Increasing incidence of hip arthroplasty for primary osteoarthritis in 30- to 59-year-old patients. Acta Orthop. 82, 1–5 (2011).
Maher, C., Underwood, M. & Buchbinder, R. Non-specific low back pain. Lancet 389, 736–747 (2017).
Hooten, W. M. & Cohen, S. P. Evaluation and treatment of low back pain: A clinically focused review for primary care specialists. Mayo Clin. Proc. 90, 1699–1718 (2015).
Fried, L. P., Ferrucci, L., Darer, J., Williamson, J. D. & Anderson, G. Untangling the concepts of disability, frailty, and comorbidity: Implications for improved targeting and care. J. Gerontol. A Biol. Sci. Med. Sci. 59, 255–263 (2004).
Adams, L. M. & Turk, D. C. Psychosocial factors and central sensitivity syndromes. Curr. Rheumatol. Rev. 11, 96–108 (2015).
Yücel, F. N. & Sanal-Toprak, C. Central sensitization-related symptoms and their relationship to disability in prevalent chronic musculoskeletal pain: A cross-sectional study. Musculoskelet. Sci. Pract. 73, 103147 (2024).
Kersebaum, D. et al. The early influence of COVID-19 pandemic-associated restrictions on pain, mood, and everyday life of patients with painful polyneuropathy. Pain Rep. 5, e858 (2020).
Funding
This study was supported by Grant-in-Aid funding from the Ministry of Health, Labour and Welfare 21FA0601 (Director, HY), Scientific Research grants (KAKENHI) 21K18291 (KM), and the Japan Agency for Medical Research and Development (AMED) JP22dk0110047 (KM). This study was supported by Grants-in-Aid for Scientific Research (KAKENHI) (26462249 and 21K09306) (HH), 23K09724 (YN), 21K11703 (NM), and 22K09430 (YE). The funders had no role in the study design, data collection and analysis, decision to publish, or manuscript preparation.
Author information
Authors and Affiliations
Contributions
S.M. and H.H. conceived and designed the study. S.I., S.K., Y.M., T.U., A.M., Y.K., M.S., T.S., H.T., R.T., M.T., Y.E., and Y.N. acquired the data. H.O. and H.H. analyzed and interpreted the data. S.M. drafted the manuscript, while H.H., K.M., N.M., and H.Y. critically revised it. All authors reviewed and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This longitudinal study was approved by the Wakayama Medical University Research Ethics Committee (No. G92). All participants provided written informed consent for the inclusion and publication of their data. All procedures were performed in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and the Declaration of Helsinki.
Consent for publication
All participants provided written informed consent to publish their data.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Murata, S., Hashizume, H., Mure, K. et al. Longitudinal study of central sensitization and chronic low back pain in a Japanese cohort during the COVID-19 pandemic. Sci Rep 15, 8012 (2025). https://doi.org/10.1038/s41598-025-93178-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-93178-z