Abstract
Defence personnel need to be agile and responsive in their assessment of strategic and tactical tasks. Sleep and circadian disruptions, however, can compromise personnel’s readiness. Digital health technologies have the potential to provide sleep and circadian health management advice but need to be designed with active involvement from stakeholders and communities. This study explored challenges with shift work in a cohort of defence personnel to identify end-user expectations for a sleep health smartphone application. Eight shift working Air Traffic Control personnel from the Australian Defence Force participated in 60-70-minute semi-structured online interviews. Informal discussions were also held with various defence stakeholders to determine requirements for an app. Defence personnel reported disruptions to their sleep, family, and social life due to environmental and operational circumstances, such as shift work, mental load, and unplanned schedules. They were highly receptive to a digital intervention and emphasised need for personalised support. Gamification, availability of the app via the defence forces, and high data security were recognised as key enablers. These insights should serve as theoretical foundation for further development, co-design, and testing of digital health tools in other shift worker cohorts, and to better examine and address the impacts of operational demands on their health and performance.
Similar content being viewed by others
Introduction
Shift work is a ubiquitous part of the modern, 24/7 world. While critical to the functioning of society, it can lead to chronic disruption of sleep due to misalignment between sleep-wake behaviours and circadian rhythms, resulting in adverse cognitive, health and safety consequences1. Sleep and circadian disruption can exacerbate existing health conditions and increase the risk of developing cardiovascular and metabolic diseases, as well as certain forms of cancer2,3. Compared to the general population, shift workers are at a greater risk of workplace accidents and adverse driving events post shift4,5. Organisational and individual-level approaches are needed to prevent and ameliorate the negative impacts of shift work.
At an organisational level, common sleep and circadian management practices include rostering practices such as forward rotation rosters, i.e., starting with morning and ending with evening or night shifts, strategic napping during the shift, and consideration of light intensity and spectral composition for alertness optimisation1,2,6,7. While useful, these practices are inconsistently adopted and vary considerably across industries. Often, these practices are not tailored to address individual differences in coping with shift work, such as sex, age, diurnal preference, light sensitivity, and habitual sleep practices. Non-pharmacological individual approaches, such as sleep psychoeducation, light interventions, stress reduction, timed caffeine, diet and exercise have been shown to improve sleep and alertness in shift workers, with positive implications for health6,8,9,10,11,12,13,14,15. These strategies can be delivered as lifestyle management support for circadian disruption, demonstrating their potential utility across all types of shift work. However, implementing these individual-level interventions on a large scale can be challenging, due to barriers such as irregular and unplanned work hours that prevent shift workers from accessing standard healthcare16,17. They also require continuous adaptation and personalisation to suit operational and personal contexts, which may be difficult to achieve if the interventions are delivered manually1,10,17,18.
Defence personnel represent a unique population of shift workers who work long hours and experience high levels of psychophysiological stress that comes with hazardous and sensitive military operations19. These unique operational challenges make them particularly susceptible to sleep disturbances and circadian disruption20,21. Sleep disruption is pervasive in military personnel22, and up to 77% of active-duty personnel report getting less than seven hours of sleep23,24,25,26,27. Sleep disturbances are also common across most operational units, including pilots, air traffic controllers, submariners and special forces15,21,28,29. Insufficient or disrupted sleep is associated with poorer health, more lost work days due to sick leave and lower productivity, and higher odds of early discharge from the military22. A number of cognitive functions that are critical for the military’s demanding work environments may also be compromised with restricted sleep19,24. This is why management of sleep-wake schedules is recognised as a key protective factor for optimising cognitive fitness in defence personnel30,31. It is also recognised that addressing sleep and circadian disruption can have a positive impact on the military’s physical fitness and field training32,33. Nuanced, individually tailored approaches that address operational complexities are needed to optimise sleep and circadian function in order to enable defence personnel to sustain operational performance and recovery.
Digital technologies are a highly promising and cost effective option34 for addressing sleep and circadian disruption in shift workers. Unlike one-size-fits-all psychoeducation, digital technologies can expand the scope of existing interventions, drive behaviour change and provide timely, tailored support that addresses variability across job roles, individual circumstances, diurnal preferences, and differences in circadian biology. Recently, a beta version of a smartphone app that was co-designed with shift working healthcare workers found that personalised sleep-wake recommendations significantly improve insomnia, sleep impairments and mental health in shift workers10,15. Targeted redevelopment of an app for use in defence can serve as a scalable, efficacious pathway to maximise defence personnel’s sleep and circadian health, with flow-on impacts on cognitive fitness and job performance. This study utilised a qualitative, exploratory methodology to understand sleep health challenges and identify requirements for a smartphone application for defence personnel undertaking shift work.
Methods
Recruitment
Community engagement
To involve the defence community in all stages of design and implementation of the digital technology, we engaged the Defence, Science, and Technology Group (DSTG, a research institution within the Australian Department of Defence), other Defence stakeholders and a digital health organisation, Curve Tomorrow. Informal group discussions were convened at several stages throughout the project to identify potential participant cohorts for interviews, explore working conditions within their operational environments, seek expert advice and feedback on data collection and documentation, and finalise key requirements for technology development. Groups involved in participatory approaches of this research are highlighted in Fig. 1.
The study was approved by DSTG Low-Risk Ethics Panel (Protocol: LD 13–21), registered with the Monash University Human Research Ethics Committee (Protocol: 31242), and performed in accordance with the Declaration of Helsinki. Participants were recruited from the Royal Australian Air Force (RAAF) through purposive sampling from a specialist squadron that included the RAAF Air Traffic Controller (ATC) personnel - a cohort whose job is characterised by 24/7 mission profiles and shift work rosters that are often non-negotiable. RAAF was selected as the participating group for the consultation in the design and implementation of this digital technology because the ATC job requires exceptional cognitive flexibility, deep expertise in resource management and risk-based decision making under pressure, similar to other military roles. ATC experiences may also align with broader defence lifestyle challenges, including sleep disturbances, shift schedules with periods of high training and demand. Volunteers were invited from the participant pool of approximately 20 personnel; their decision to participate was guaranteed to have no impact on their employment, in accordance with the Australian Defence policy on research ethics. Participants provided informed consent for confidential participation, and for the interviews to be audio recorded and transcribed verbatim. Participants were considered to be on-duty during their participation, and in addition received AUD$100 gift vouchers for their participation and time commitment to the study.
A digital invitation to participate in the study was distributed via the Squadron chain of command, inviting expressions of interest to be sent directly to the research team. A researcher contacted interested individuals via phone or email to explain the study’s objectives. Participants were told that the research would draw on their perspectives to outline the initial requirements of a smartphone application that addresses sleep and circadian disruption in defence personnel. Participants were not informed about the beta version of the healthcare shift work app to ensure that their responses were not influenced by this information.
Data collection
We conducted participatory research35,36 to engage with community stakeholders for identifying the concerns with shift work, developing an interview guide, conducting interviews and finalising user requirements for an app-based product35,37. This was done to ensure that the digital technology was driven by and aligned with the unique needs36,38 of this industry. While it is beyond the scope of this study, upon product development, stakeholders were invited to comment on the product from conceptual stages to final design to ensure that the product met their requirements. Their feedback is currently being used to improve product features, design and delivery.
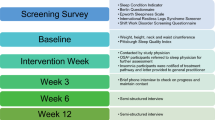
This research adopted reflexive thematic analysis, which is a qualitative research method designed for flexible, reflective, and theory-driven coding or analyses of data39,40. We used this method as it allows researchers to engage deeply with data, and favours an iterative, recursive process where themes are co-constructed with data. Interviews were selected as a mode for data collection to allow users to contribute independent ideas confidentially. A semi-structured interview guide was developed based on guidelines for qualitative research41. The question guide was developed by the research team and the tech(nology) development team based on a co-design question guide that was previously developed for examining sleep in shift workers and identifying potential requirements for app-based products in healthcare workers10. This guide was reviewed by the research team at DSTG and approved by the DSTG ethics committee and the Wing Commander of the participating base. Broad lines of questioning included: (i) the structure of routines and lifestyles around shift work; (ii) the impact of shift work on sleep, family or social life, work and general performance, and health; (iii) current strategies to manage sleep and health (including commercially available smartphone apps or tools); (iv) expectations and requirements for a technology that addresses sleep and circadian management in shift work; and (v) sociotechnical features that would increase end user engagement and long term adoption. A brief, preliminary question guide, and prompts are provided in Table 1.
All interview sessions (approximately 60–70 min) were conducted remotely using Google Meet. There were two interviewers (PV and always one member of the tech development team) that facilitated these interviews. Reflective notes were initially made by PV with the tech development team after these interviews to ensure contextual understanding, document any additional insights or reflect on the interview process itself. The interview guide was refined to include any additional prompts (e.g. if participants had a specific term for “night shift” or phrases that were relevant) for the next participant. All participant information was deidentified, encrypted and stored in a secure database.
Data analyses
Data were analysed using NVivo software (version 1.7.1) to condense meanings based on participant descriptions and researcher interpretation. The six phase process within reflexive thematic analysis was used to identify patterns and themes in the data39 that emphasised the quality of data and depth of narratives by inclusion of a broad range of participants (including different gender, career stages, marital status, family and caregiving responsibilities, and life experiences)42. A constructivist-interpretivist approach was applied, which views knowledge as co-constructed through interaction43. The approach also acknowledges that reality is subjective and shaped by our cultural and social construct. We maintained reflexive notes to document any personal reactions, thoughts and decisions made during the coding process44. Authors PV, LS and TLS have backgrounds in psychology, physiology, and development of shift work specific sleep interventions and treatments. During interviews, author PV and the tech development team adopted a flexible and sensitive approach, built rapport and established trust with participants. PV and interviewers from the tech development team took notes during and just after each interview. In the first phase of analyses, two authors (PV and LS) and two research interns reviewed all interview audio and transcripts independently to identify any inflections, emotional responses, specific content, frequent references and patterns. Following this, PV and LS systematically worked through each transcript, discussed their notes and assigned initial codes. This process was collaborative, and these codes provided a shorthand way of categorising data into segments. As coding progressed, several potential themes were generated, which PV and LS initially reviewed with each other to identify any themes that overlapped and merging those. Themes that were considered too broad or not well supported by the data were removed. A secondary collaborative review of themes, defining and naming them was conducted by PV, LS and TLS. During these discussions, authors shared their reflections on why certain themes stood out. A visual thematic map was developed to depict theme relationships and titles were assigned to each theme. Extracts that best represented the themes were included in the final report. The final phase of reporting findings is presented in this manuscript, with participant codes included after their quotes (e.g. P1). Themes were further reviewed by the research team and stakeholders (see community engagement above) and collated into a list of potential areas for app development (i.e. user requirements for an app). These potential areas for app development were then discussed with senior leadership within the Defence, Science and Technology Group to finalise features for initial tech development.
Results
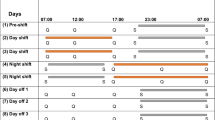
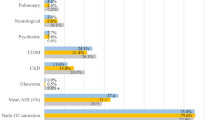
Nine air force personnel from a participant pool of approximately 20 shift working personnel expressed interest in participating in the study and eight were interviewed (three females, aged 21–42 years, 1–12 years’ experience with shift work, ). One person could not participate due to unexpected travel arrangements. All participants worked forward rotation shifts (two morning, two afternoon and one night shift). Participants knew about their schedules for a month in advance, with the expectation that the roster may change during periods of high demand. Specific demographic information collected for each participant, including age, gender, role, number of years of experience and marital status are not included here to ensure confidentiality. Three themes and five subthemes were generated, as summarised in Fig. 2: (i) Challenges with shift work (two subthemes); (ii) Coping strategies; and (iii) Requirements for digital tool strategies (three subthemes).
Challenges with shift work
Personal impacts
Participants reported that operational circumstances impacted their sleep and lifestyle. All participants reported that rotating shift work and daily changes in the shift start, or end times made it difficult for them to fall or stay asleep. Participants highlighted falling asleep as a primary concern, especially following busy shifts. “I have insomnia,” or “I have not slept well,” were the most common sleep complaints. Some participants reported that even when they were not on shift, they were at the workplace to use other facilities, such as for “gym and exercise”, or to “stay here and catch up on other things” which usually reduced opportunities to sleep. They described periods of high workload “very fatiguing” and particularly “difficult to unwind” after work. High workload was also described as a reason for “cumulative fatigue” that further impacted sleep and work performance. In addition, participants remarked that sleeping was difficult in their ___location due to “weather”, “harsh conditions”, or “noisy” environments.
“They (general observation) cannot unwind and get themselves to sleep any time before two o’clock in the morning.” (P4).
“I have seen (referring to someone else) like 2–3 hours of sleep (due to insomnia)… where there is a lot of pressure.” (P7).
“People are getting fatigued… they are not resetting their system.” (P8).
Participants demonstrated awareness of circadian misalignment and the negative impacts of shift work on physical and mental health. They noted that some shifts were particularly challenging if they conflicted with their body clock, which made their sleep worse, especially after a shift. Participants reported that they perceive their functioning to be poor on days after their night shifts. All participants indicated that they have concerns about their risk of developing health conditions in the future due to sleep loss and shift work.
“ I struggle most with morning shifts, (no) matter what I do I can’t sleep before midnight, unless I am sick, I might be able to pass out but that’s where I struggle. I know others struggle with night shift.” (P2).
“I know about my risk of having brain problems long term. And others know about the risks too…” (P3).
“…my personal decision making the day after a night shift is not as good. Things like I won’t do any DIY or anything like that because I’ll make a mess of it.” (P7).
Impacts on family and lifestyle
When discussing their partners or spouses, participants indicated that it was difficult to plan activities or take care of their child(ren) when the partner was working because their shift schedules were modified often, especially during periods of high demand when there is a need to work a shift on short notice. They mentioned that because of their roles, they were expected to minimise events scheduled between shifts and “choose best options” to limit the amount of social or personal commitments to ensure they were always ready for work.
”And it’s (shift work) also draining for my partner a lot …, that’s been a tough adjustment. It was also tough adjusting to the sleep cycle as well.” (P1).
“I definitely feel like I am missing out… I have duty of care and that responsibility to support the roster.” (P1).
“…my (kid) is at home, I will get a couple of hours (of sleep) max, it is very difficult.” (P4).
“If you ask my (partner), it’s not the best day (after night shift) to do anything or—I’m just less personable and not as enjoyable to be around.” (P7).
Coping strategies
All participants reported having a range of personal strategies that they were using to manage shift work. Each participant reported using some form of an app to manage how they cope with the negative impacts of shift work. While none of these apps was shift work oriented, they used it broadly to manage lifestyles or sleep. The most common apps were related to meditation, exercise, wearable technology, and using an external calendar to note their rosters and personal commitments. The most common strategy reported for managing their lifestyle was exercise, to both “keep a routine” and “stay active” for their job demands. Each participant had some form of sleep hygiene strategy for managing their bedroom environment, such as blackout blinds, noise-cancellation headphones, or air conditioning. None of the participants reported the use of sleep medications but said they “had knowledge” about medications available. Natural remedies such as herbal teas, and relaxation strategies such as meditation were regularly used, with the latter helping them relax and unwind after work.
“I really love their (referring to an app) meditations… I need help falling asleep, then I will play one of them.” (P1).
“Meditation definitely helps me calm my mind because for me it feels slack.” (P2).
“Another tool that I sort of use sometimes is like having a nap after a morning shift as well…. to be productive later in afternoons.” (P5).
(When referring to napping) “My old school method is to just get on with it.” (P6).
“There is no like a crash course on how to survive shift work or anything, you sort of just have to feel it out yourself.” (P7).
“Not much, we have some information, (but) you just have to really deal with it. And we’re all adults so you’re expected to manage it.” (P7).
User requirements for a digital shift work tool
Uses a scientific approach
Participants reported that while they had researched ways to support themselves as a shift worker, they needed readily accessible, scientifically validated resources. They acknowledged having previously looked for online information or smartphone apps to help manage shift work but have not seen anything that provides dedicated support for their circumstances. Participants also demonstrated awareness of circadian rhythms and underlined the need for having technologies that used circadian neuroscience for recovery for better performance.
“I did not know that shift work causes insomnia. Knowing shift work impacts on my life is important.” (P2).
“I want a product that does not tell me to have a consistent bedtime, because I really cannot.” (P2).
“I don’t think there is an app for shift workers”. (P4 and 6)
“A lot of what we do is not the same as someone who sleeps at night, it is not that easy.” (P5).
“When my (child) was born, we used an app that told us when a good time for him would be to nap so he could sleep better through the night. That circadian element is what I want.” (P7) “I use sounds to fall asleep, sometimes mindfulness meditation, but I am not sure if the app I use has scientific support. Some evidence-based strategies would help.” (P8).
Personalisation of recommendations
A common comment from personnel was that they needed more information on what broader lifestyle strategies they can use to better prepare themselves for shift work, like a “toolkit approach” to choose information of interest. In addition to general pick and choose strategies, all participants highlighted that having day-to-day, timed recommendations for sleep and light or other behaviours adapted to their rosters, personal commitments, and changing sleep and fatigue levels was a crucial requirement.
“(The app should) give me a greater understanding of practices I can use to feel more in control of my work.” (P2).
“I would like to know when I should do different activities. What if the app can tell me, your bedtime is xx and you should take a shower before bed. That I will follow because it makes it easy for me.” (P5).
“I need to know what to do” (P8).
Given the nature of their work, requiring sustained attention across shifts, participants suggested that the recommendations they receive should also be aimed at reducing fatigue and maximising alertness.
“It should tell me when I should have caffeine on night shifts so I can feel alert but go back to bed after the shift”. (P4)
“What can I do to be more active during the shift?” (P7).
Gamification and adoption
Gamification was identified as a key need for the technology. Participants indicated that existing applications are not useful as they either do not have any metrics that they can track and improve or when they are available, they do not know how to interpret the metrics. That led to “frustrations due to unclear goals,” which was a key barrier to long term engagement.
“I know these apps (referring to non shift work) cannot provide support for shift work, but what am I supposed to do with a score of ‘50’ for my sleep – am I supposed to nap or skip work?” (P7).
“I want to know that if I slept poorly, what can I do? If I can take an extra nap before the shift or if I can sleep early but not wake up early, or if I can go for a walk at a certain time.” (P8).
It was also observed that there is high competitiveness among personnel and individuals are motivated to improve. They use apps with options to connect socially with their peers to compare their performance. Participants noted that adaptiveness of an app and the metrics received on it will help with their compliance and keep them accountable. It was also suggested that having an option to connect with other users will increase accountability with the use of recommendations.
“Scores specific to me will make me feel more in control of my actions, so I can improve more.” (P2).
“We use xx app for seeing distances covered during our runs. Some of that element would keep us accountable for our fatigue.” (P3).
“It (metrics) would add a competitive element to the app – so if I did poorly, I will be motivated to improve”, and “If the app told me I did well, I will be encouraged.” (P8).
There was an emphasis on the need for an app to connect to other technologies as both a way to increase its adoption and improve recommendations. This was identified as a key incentive to adoption, which would link it to their everyday life.
“What I’ve been able to find so far in general, if the information can be gathered automatically, without requiring too much input from the controllers, is generally the best way to go.” (P3)“I use my xx (watch) every day. Having it take all my data, such as heart rate, sleep and using it to provide recommendations.” (P3).
“There is a lot of things we do, so reducing our burden would be helpful. Automatically drawing information from like my xx (watch) or sending it to (the watch).” (P8).
Lastly, participants reported a greater willingness to adopt an app and higher compliance if it was made available via defence. It was noted that while the access to an app should be via their department, an app should be confidential and private. Participants remarked that the technology should be available on multiple platforms, such as iOS and Android to reduce barriers to access.
“If we are told there is a free app available by our supervisors, we will likely volunteer to use it.” (P1).
“I do not want our managers and supervisors to know how we sleep, but some form of support (should be available).” (P6).
The three themes determined as user requirements for an app were utilised to generate a list of potential areas for app development. These areas for app development were identified by the research team, partnering digital health technology company and senior leadership within defence. These are summarised in Fig. 3. The first area for app development, uses a scientific approach, and suggests providing shift workers with specific resources that support management of lifestyles as a shift worker, with scientific reasoning for each recommended strategy. The second area of app development is personalisation of recommendations, which is based on participants’ commenting on their need for specific instructions on activities that they should do, which aligns with their requirements and adapts to their needs around rostering or personal commitments. Lastly, gamification and adoption highlights strategies that may encourage defence personnel to adopt an app, through social connection with peers, use of metrics to document changes in sleep or performance and inclusion of some form of competitive element to promote adherence.
Discussion
Insufficient or poor quality sleep among defence personnel can directly affect the health and readiness of the workforce45. Optimising sleep health and circadian functioning can increase the capacity of defence personnel to deploy neurocognitive resources and support tactical decision making. In this study, we examined some of the key challenges a representative cohort of defence shift workers experience with their sleep and lifestyle when working nonstandard work hours and identified individual needs for digital technology to support sleep health. Consistent with research in other shift work contexts21,46,47, our findings suggest that defence air traffic controllers often experience sleep disruption due to nonstandard work hours, operational and environmental factors. All participants reported that they actively try to manage their sleep to sustain or improve their functioning, expressing interest and willingness to utilise digital technologies that can help improve their sleep and alertness.
This study delivers key priorities for developing a sleep and circadian health app for shift working defence personnel, as illustrated in Fig. 3. These priorities are categorised into three areas: (i) scientific approach; (ii) personalisation of recommendations; and (iii) gamification and adoption. First, an app needs to adopt a scientific approach that is specific to shift work, as existing tools emphasise night-time sleep. Explanation to personnel on why certain strategies may be useful and the scientific basis for recommendations may promote adherence. Second, recommendations need to be personalised. The product should offer tailored strategies that consider the personal, family and lifestyle impacts of shift work. These tailored strategies need to be multifaceted and account for differences in operational circumstances, personal commitments, and unpredictability of schedules. Implementation of biomathematical modelling approaches may address these operational and work-life balance pressures to provide sleep and light recommendations in an automated manner, adaptable to individual differences in lifestyle15,48,49,50,51,52,53.
These findings are based on a specific cohort of RAAF Air Traffic Controllers and in addition to personal and operational circumstances, it is also crucial to acknowledge substantial variability in how individuals from broader defence ecosystem may respond to shift work, including the direction and magnitude of their circadian phase shift, especially after consecutive night shifts54,55. Consistent with previous research48,53,56,57,58, our findings suggest that air traffic controllers in defence may find it difficult to undertake shifts or follow recommendations that conflict with their chronotype, compromising both their job performance and wellbeing. While biomathematical models predict circadian phase, inter-individual variability in circadian timing may need to be accounted for to further personalise these models. However, accurate estimations of circadian timing and subsequent changes across different shift schedules may not be feasible with current measures, in which case, improving phase predictions48,59, or using diurnal preference can be employed as an alternative to help with timing or dosage of other fatigue countermeasures, such as caffeine and exercise, which will offer necessary personalisation in a practical way.
Lastly, for long term adoption of an app, the technology needs to offer confidential support with relatable, clear language and reduced manual input. In agreement with earlier literature60, our study also found that the integration of multiple technologies, such as wearables and mobile health apps is a key facilitator for app uptake in Defence. This is likely because wearable technology can improve the personalisation of sleep-wake management systems, enable goal tracking, and encourage health behaviour change, accelerating engagement and uptake at scale. Integrative technology can also reduce manual input from the user to enable long term adoption, allowing for more seamless integration with personnel’s daily activities.
Related to personalisation, gamification was identified as a promising avenue for improving user engagement61. This included features such as having clear benefits outlined, allowing goal setting, and encouraging value-creating behaviours through metrics that are updated using data collected through wearables. Previous research has shown that these “in-game” elements such as goal setting, rewards and metrics can increase intention, effort, and persistence61,62,63. A recent systematic review has also shown that goal setting, particularly in health-related apps can have positive impact on engagement and health-related behaviour change64. Intra-organisational gamification through competitive elements or connecting with other employees was suggested as a motivation, which is a well-studied strategy for enhancing productivity and motivating employees65.
Sleep education was a frequently requested feature from an app. A recent trial examining the utility of sleep education in service members showed that individuals may be unaware of the number of hours of sleep they may need24, thus demonstrating the usefulness of generating awareness. In addition, existing information related to sleep is mostly geared towards nocturnal sleep, which is not translatable to shift working populations. Scientifically validated content, presented in an interactive format can also increase the uptake and long term adoption of an app. In an active, highly motivated population, such as defence personnel19, there is considerable potential to improve sleep and health through focused goal setting.
Accessibility was a key requirement for the adoption of an app. Digital and telehealth services offer feasible, scalable support for health management, but disparities may exist, with some communities unable to gain access66. Participants noted that an app’s uptake will likely depend on whether it is available across multiple operating systems, and while there should be options to discuss an app’s content and data with one’s workplace stakeholders, the tool should ideally offer confidential support.
This study was conducted as an initial discovery preceding the development of a sleep and circadian management tool for shift workers and was subject to the following limitations. First, it involved a purposive sample of participants from a single military unit which may have caused self-selection bias. More diverse operator communities covering a wider range of operational settings may need to be engaged to provide further input on the design and usability of the technology. First, while Air Traffic Controllers recruited in the study perform risk-taking tasks that require high neurocognitive processing, their needs may be different to other personnel, such as those involved in combat duty or submarine operations. However, it should be noted while the operational challenges and nuances of sleep disruption may vary across roles and branches, the core, fundamental risks of circadian misalignment and fatigue, and the need for tailored sleep management strategies likely remain across the board. Future research should consider expanding these insights to additional defence cohorts to deliver more responsive interventions. Second, the study’s sample size was small as our cohort included only 20 potential participants. We acknowledge that while large sample sizes are not necessary for proof-of-concept or participatory measures, this may restrict generalisability. It is noted that digital technologies require individuals to self-engage in their care and motivation to use such tools can fluctuate34. Retention ranges anywhere from 7 to 42% for web- and app-based programs68, and less than 10% for mental health apps beyond Day 2034. Highly targeted solutions are a good starting point for broader user uptake, with the feedback from the target group serving both as a catalyst for wider interest, and as a testing ground for an app’s validation and iterative improvement.
Community engagement and the use of participatory approaches are key strengths of this research. While sleep is considered critical for optimal health, performance and well-being of defence personnel30,69, there is very little information on how defence personnel perceive sleep management or seek to enhance it24,69. This study addresses a major knowledge gap by aiming to understand the impacts of shift work on defence personnel, practices they use for sleep management, specific barriers and potential facilitators of utilising sleep management tools in this population. Important potential roles for digital technology were identified in this study, particularly using them to deliver personalised strategies, and the need for a toolkit approach where they can select strategies that work best for their contexts. Current sleep interventions, including telehealth or digitally delivered are primarily targeted towards night sleepers70. Without tailored support and resources, these interventions may not be effective in shift work populations1. Future studies should prioritise co-designing any interventions with partnerships between researchers, defence personnel and other stakeholders to ensure genuine collaboration and development of technologies that addresses their needs.
Conclusions
This study advances our understanding of common burdens that defence personnel experience with shift work, its adverse impacts, and the support they need. This project highlights the need for interventions that go beyond one-size-fits-all models to develop multifaceted adaptive tools that offer personalised solutions to the burden of shift work in defence. It provides community derived knowledge for development of digital technologies that can be deployed across defence to promote accessible sleep and circadian health management. A digital intervention targeting sleep and circadian health, developed with the community could serve both immediate operational performance requirements and long term force preservation, career longevity and duty-of-care objectives for defence personnel.
Data availability
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author ([email protected]) upon reasonable request.
References
Crowther, M. E., Ferguson, S. A., Vincent, G. E. & Reynolds, A. C. Non-Pharmacological interventions to improve chronic disease risk factors and sleep in shift workers: A systematic review and Meta-Analysis. Clocks Sleep. 3 (1), 132–178. https://doi.org/10.3390/clockssleep3010009 (2021).
Rajaratnam, S. M. W., Howard, M. E. & Grunstein, R. R. Sleep loss and circadian disruption in shift work: health burden and management. Med. J. Aust. 199 (S8). https://doi.org/10.5694/mja13.10561 (2013).
Sletten, T. L. et al. Health consequences of circadian disruption. Sleep 43 (1), zsz194 (2020).
Folkard, S. & Lombardi, D. A. Modeling the impact of the components of long work hours on injuries and accidents. Am. J. Ind. Med. 49 (11), 953–963. https://doi.org/10.1002/ajim.20307 (2006).
Lee, M. L. et al. High risk of near-crash driving events following night-shift work. Proc. Natl. Acad. Sci. U.S.A. 113 (1), 176–181 (2016).
Sletten, T. L. et al. A Blue-Enriched, increased intensity light intervention to improve alertness and performance in rotating night shift workers in an operational setting. Nat. Sci. Sleep. 13, 647–657. https://doi.org/10.2147/NSS.S287097 (2021).
Vetter, C., Fischer, D., Matera, J. L. & Roenneberg, T. Aligning work and circadian time in shift workers improves sleep and reduces circadian disruption. Curr. Biol. 25 (7), 907–911. https://doi.org/10.1016/j.cub.2015.01.064 (2015).
Booker, L. A. et al. The effectiveness of an individualized sleep and shift work education and coaching program to manage shift work disorder in nurses: a randomized controlled trial. J. Clin. Sleep. Med. Published Online Dec. 7 https://doi.org/10.5664/jcsm.9782 (2021).
Chinoy, E. D., Harris, M. P., Kim, M. J., Wang, W. & Duffy, J. F. Scheduled evening sleep and enhanced lighting improve adaptation to night shift work in older adults. Occup. Environ. Med. Published online August 25, 2016:oemed-2016-103712. https://doi.org/10.1136/oemed-2016-103712
Murray, J. M. et al. Mobile app for personalized sleep–wake management for shift workers: A user testing trial. Digit. Health. 9, 20552076231165972 (2023).
Shriane, A. E., Ferguson, S. A., Jay, S. M. & Vincent, G. E. Sleep hygiene in shift workers: A systematic literature review. Sleep Med. Rev. 53, 101336. https://doi.org/10.1016/j.smrv.2020.101336 (2020).
Sletten, T. L. et al. Health consequences of circadian disruption. Sleep 43 (1), zsz194. https://doi.org/10.1093/sleep/zsz194 (2020).
Vetter, C. Circadian disruption: what do we actually mean? Eur. J. Neurosci. 51 (1), 531–550. https://doi.org/10.1111/ejn.14255 (2020).
Vincent, G. E., Jay, S. M., Vandelanotte, C. & Ferguson, S. A. Breaking up sitting with Light-intensity physical activity: implications for Shift-Workers. Int. J. Environ. Res. Public Health. 14 (10), 1233 (2017).
Varma, P. et al. SleepSync: early testing of a personalised sleep–Wake management smartphone application for improving sleep and cognitive fitness in defence shift workers. Clocks Sleep. 6 (2), 267–280. https://doi.org/10.3390/clockssleep6020019 (2024).
Crowther, M. E., Saunders, W. J., Sletten, T. L., Drummond, S. P. A. & Bei, B. Tailoring cognitive behavioural therapy for insomnia across contexts, conditions, and individuals: what do we know, where do we go? J. Sleep Res. 32 (6), e14023. https://doi.org/10.1111/jsr.14023 (2023).
Reynolds, A. C., Loffler, K. A., Grivell, N., Brown, B. W. J. & Adams, R. J. Diagnosis and management of sleep disorders in shift workers, with patient informed solutions to improve health services research and practice. Sleep Med. 113, 131–141. https://doi.org/10.1016/j.sleep.2023.11.027 (2024).
Rahman, S. A. et al. Dynamic lighting schedules to facilitate circadian adaptation to shifted timing of sleep and wake. J. Pineal Res. 73 (1), e12805. https://doi.org/10.1111/jpi.12805 (2022).
Main, L. C., McLoughlin, L. T., Flanagan, S. D., Canino, M. C. & Banks, S. Monitoring cognitive function in the fatigued warfighter: A rapid review of cognitive biomarkers. J. Sci. Med. Sport Published Online May. 6 https://doi.org/10.1016/j.jsams.2023.04.009 (2023).
Cooper, A. D., Kolaja, C. A., Markwald, R. R., Jacobson, I. G. & Chinoy, E. D. Longitudinal associations of military-related factors on self-reported sleep among U.S. Service members. Sleep 44 (12), zsab168. https://doi.org/10.1093/sleep/zsab168 (2021).
Good, C. H., Brager, A. J., Capaldi, V. F. & Mysliwiec, V. Sleep in the united States military. Neuropsychopharmacol 45 (1), 176–191. https://doi.org/10.1038/s41386-019-0431-7 (2020).
Seelig, A. D. et al. Sleep and health resilience metrics in a large military cohort. Sleep 39 (5), 1111–1120. https://doi.org/10.5665/sleep.5766 (2016).
Adler, A. B., Bliese, P. D., LoPresti, M. L., McDonald, J. L. & Merrill, J. C. Sleep leadership in the army: A group randomized trial. Sleep. Health. 7 (1), 24–30. https://doi.org/10.1016/j.sleh.2020.06.001 (2021).
Harrison, E. M., Schmied, E. A., Hurtado, S. L., Easterling, A. P. & Glickman, G. L. The development, implementation, and feasibility of a circadian, light, and sleep skills program for shipboard military personnel (CLASS-SM). Int. J. Environ. Res. Public Health. 19 (5), 3093 (2022).
McDonald, J. L., Ganulin, M. L., LoPresti, M. L. & Adler, A. B. Sleep knowledge, goals, and habits in soldiers. Sleep. Health. 5 (4), 426–428. https://doi.org/10.1016/j.sleh.2019.04.006 (2019).
Smith, C. D. et al. Sleep restriction and cognitive load affect performance on a simulated marksmanship task. J. Sleep Res. 28 (3), e12637. https://doi.org/10.1111/jsr.12637 (2019).
null null, Watson, N. F. et al. Recommended amount of sleep for a healthy adult: A joint consensus statement of the American academy of sleep medicine and sleep research society. J. Clin. Sleep Med. 11(06):591–592. https://doi.org/10.5664/jcsm.4758
Mantua, J. et al. A review of environmental barriers to obtaining adequate sleep in the military operational context. Mil. Med. 184 (7–8), e259–e266 (2019).
Lopez, N., Previc, F. H., Fischer, J., Heitz, R. P. & Engle, R. W. Effects of sleep deprivation on cognitive performance by united States air force pilots. J. Appl. Res. Memory Cognition. 1 (1), 27–33 (2012).
Aidman, E. Cognitive Fitness Framework: Towards Assessing, Training and Augmenting Individual-Difference Factors Underpinning High-Performance Cognition. Frontiers in Human Neuroscience. ;13. Accessed June 5, 2023. https://www.frontiersin.org/articles/ (2020). https://doi.org/10.3389/fnhum.2019.00466
Albertella, L. et al. Building a transdisciplinary expert consensus on the cognitive drivers of performance under pressure: an international multi-panel Delphi study. Front. Psychol. 13, 1017675 (2023).
Brown, S., Matsangas, P. & Shattuck, N. L. Comparison of a circadian-based and a forward rotating watch schedules on sleep, mood, and psychomotor vigilance performance. In Proceedings of the Human Factors and Ergonomics Society Annual Meeting. Vol 59. SAGE Publications Sage CA: Los Angeles, CA; :1167–1171. (2015).
Sabzevari, R., Hamideh ·, Hosseini, M. & Shirvani, H. Circadian rhythm effect on military physical fitness and field training: a narrative review. Sport Sci. Health. 17, 3. https://doi.org/10.1007/s11332-020-00692-w (2021).
Baumel, A., Muench, F., Edan, S. & Kane, J. M. Objective user engagement with mental health apps: systematic search and Panel-Based usage analysis. J. Med. Internet. Res. 21 (9), e14567. https://doi.org/10.2196/14567 (2019).
Cargo, M. & Mercer, S. L. The value and challenges of participatory research: strengthening its practice. Annu. Rev. Public. Health. 29 (1), 325–350. https://doi.org/10.1146/annurev.publhealth.29.091307.083824 (2008).
Jagosh, J. et al. Uncovering the benefits of participatory research: implications of a realist review for health research and practice. Milbank Q. 90 (2), 311. https://doi.org/10.1111/j.1468-0009.2012.00665.x (2012).
Duea, S. R., Zimmerman, E. B., Vaughn, L. M., Dias, S. & Harris, J. A guide to selecting participatory research methods based on project and partnership goals. J. Participatory Res. Methods. 3 (1). https://doi.org/10.35844/001c.32605 (2022).
Macaulay, A. C. et al. Assessing the benefits of participatory research: a rationale for a realist review. Glob Health Promot. 18 (2), 45–48. https://doi.org/10.1177/1757975910383936 (2011).
Braun, V. & Clarke, V. Using thematic analysis in psychology. Qualitative Res. Psychol. 3 (2), 77–101. https://doi.org/10.1191/1478088706qp063oa (2006).
Braun, V. & Clarke, V. Reflecting on reflexive thematic analysis. Qualitative Res. Sport Exerc. Health. 11 (4), 589–597. https://doi.org/10.1080/2159676X.2019.1628806 (2019).
Brinkmann, S. & Kvale, S. Doing InterviewsVol 2 (Sage, 2018).
Braun, V. & Clarke, V. Thematic Analysis: A Practical Guide (SAGE Publishing Ltd, 2021).
Constructivist Grounded Theory or Interpretive Phenomenology? Methodological Choices Within Specific Study Contexts - Margie Burns, Bally, J., Burles, M., Holtslander, L. & Peacock, S. Accessed October 23, 2024. (2022). https://journals.sagepub.com/doi/10.1177/16094069221077758.
Brown, A. D. et al. Integrating lived experience to develop a tailored sleep intervention for people living with dementia and carepartners. Dement. Published Online September. 9, 14713012241282769. https://doi.org/10.1177/14713012241282769 (2024).
LoPresti, M. L. et al. The impact of insufficient sleep on combat mission performance. Military Behav. Health. 4 (4), 356–363. https://doi.org/10.1080/21635781.2016.1181585 (2016).
Capaldi, V. F., Balkin, T. J. & Mysliwiec, V. Optimizing sleep in the military: challenges and opportunities. Chest 155 (1), 215–226. https://doi.org/10.1016/j.chest.2018.08.1061 (2019).
Martin, K., Périard, J., Rattray, B. & Pyne, D. B. Physiological factors which influence cognitive performance in military personnel. Hum. Factors. 62 (1), 93–123. https://doi.org/10.1177/0018720819841757 (2020).
Knock, S. A. et al. Prediction of shiftworker alertness, sleep, and circadian phase using a model of arousal dynamics constrained by shift schedules and light exposure. Sleep 44 (11), zsab146. https://doi.org/10.1093/sleep/zsab146 (2021).
Postnova, S. Sleep modelling across physiological levels. Clocks Sleep. 1 (1), 166–184. https://doi.org/10.3390/clockssleep1010015 (2019).
Postnova, S., Robinson, P. A. & Postnov, D. D. Adaptation to shift work: physiologically based modeling of the effects of lighting and shifts’ start time. PLOS ONE. 8 (1), e53379. https://doi.org/10.1371/journal.pone.0053379 (2013).
Phillips, A. J. K. & Robinson, P. A. A quantitative model of Sleep-Wake dynamics based on the physiology of the brainstem ascending arousal system. J. Biol. Rhythms. 22 (2), 167–179. https://doi.org/10.1177/0748730406297512 (2007).
Tekieh, T. et al. Modeling melanopsin-mediated effects of light on circadian phase, melatonin suppression, and subjective sleepiness. J. Pineal Res. 69 (3), e12681. https://doi.org/10.1111/jpi.12681 (2020).
Varma, P. et al. Pilot feasibility testing of biomathematical model recommendations for personalising sleep timing in shift workers. J. Sleep Res.. e14026. https://doi.org/10.1111/jsr.14026.
Hansen, J. H., Geving, I. H. & Reinertsen, R. E. Adaptation rate of 6-sulfatoxymelatonin and cognitive performance in offshore fleet shift workers: a field study. Int. Arch. Occup. Environ. Health. 83 (6), 607–615. https://doi.org/10.1007/s00420-010-0547-x (2010).
Stone, J. E. et al. Temporal dynamics of circadian phase shifting response to consecutive night shifts in healthcare workers: role of light–dark exposure. J. Physiol. 596 (12), 2381–2395. https://doi.org/10.1113/JP275589 (2018).
Faulkner, R. et al. Differences in nutritional profile by chronotype among 12-h day shift and night shift nurses. Chronobiology international. Published Online Dec. 13, 1–12. https://doi.org/10.1080/07420528.2023.2294036 (2023).
Reiter, A. M., Roach, G. D. & Sargent, C. The night before night shift: chronotype impacts total sleep and rapid eye movement sleep during a strategically delayed sleep. J. Sleep Res. 32 (2), e13683. https://doi.org/10.1111/jsr.13683 (2023).
Reinke, L., Özbay, Y., Dieperink, W. & Tulleken, J. E. The effect of chronotype on sleepiness, fatigue, and psychomotor vigilance of ICU nurses during the night shift. Intensive Care Med. 41 (4), 657–666. https://doi.org/10.1007/s00134-015-3667-7 (2015).
Stone, J. E. et al. Application of a Limit-Cycle oscillator model for prediction of circadian phase in rotating night shift workers. Sci. Rep. 9 (1), 11032. https://doi.org/10.1038/s41598-019-47290-6 (2019).
Mallis, M., Banks, S., Dorrian, J. & Dinges, D. F. Chapter 12 - Aircrew fatigue, sleep need, and circadian rhythmicity. In: Keebler JR, Lazzara EH, Wilson KA, Blickensderfer EL, eds. Human Factors in Aviation and Aerospace (Third Edition). Academic Press; :309–339. (2023). https://doi.org/10.1016/B978-0-12-420139-2.00011-3
Bitrián, P., Buil, I. & Catalán, S. Enhancing user engagement: the role of gamification in mobile apps. J. Bus. Res. 132, 170–185. https://doi.org/10.1016/j.jbusres.2021.04.028 (2021).
Gutt, D., von Rechenberg, T. & Kundisch, D. Goal achievement, subsequent user effort and the moderating role of goal difficulty. J. Bus. Res. 106, 277–287. https://doi.org/10.1016/j.jbusres.2018.06.019 (2020).
Wünderlich, N. V., Gustafsson, A., Hamari, J., Parvinen, P. & Haff, A. The great game of business: advancing knowledge on gamification in business contexts. J. Bus. Res. 106, 273–276. https://doi.org/10.1016/j.jbusres.2019.10.062 (2020).
Szinay, D., Jones, A., Chadborn, T., Brown, J. & Naughton, F. Influences on the uptake of and engagement with health and Well-Being smartphone apps: systematic review. J. Med. Internet. Res. 22 (5), e17572. https://doi.org/10.2196/17572 (2020).
Mitchell, L. J., Bisdounis, L., Ballesio, A., Omlin, X. & Kyle, S. D. The impact of cognitive behavioural therapy for insomnia on objective sleep parameters: A meta-analysis and systematic review. Sleep Med. Rev. 47, 90–102 (2019).
Czeisler, M. É. A case for permanent adoption of expanded telehealth services and prescribing flexibilities for opioid use disorder: insights from Pandemic-Prompted emergency authorities. JAMA Psychiatry Published Online August. 31 https://doi.org/10.1001/jamapsychiatry.2022.2032 (2022).
Varma, P. & Rahman, S. A. Lighting the path forward: the value of sleep- and circadian-informed lighting interventions in shift work. Sleep. Published Online September. 20, zsae214. https://doi.org/10.1093/sleep/zsae214 (2024).
Fleming, T. et al. Beyond the trial: systematic review of Real-World uptake and engagement with digital Self-Help interventions for depression, low mood, or anxiety. J. Med. Internet. Res. 20 (6), e9275. https://doi.org/10.2196/jmir.9275 (2018).
Abdelwadoud, M. et al. Engaging stakeholders to optimize sleep disorders’ management in the U.S. Military: A qualitative analysis. MILIT. MED. 187 (7/8), e941–e947. https://doi.org/10.1093/milmed/usab341 (2022).
Bullock, B., Learmonth, C., Davis, H. & Al Mahmud, A. Mobile phone sleep self-management applications for early start shift workers: A scoping review of the literature. Front. Public. Health. 10 https://doi.org/10.3389/fpubh.2022.936736 (2022).
Acknowledgements
The authors thank the team at Curve Tomorrow for their partnership and support with data collection for the project, particularly Ms Ivy Xie and Mr George Charalambous who were involved in user interviews. We thank Dr Mark Corbett for his support in identifying participation group(s), Ms Alvita Sam and Ms Yichen Zhong for preliminary data cleaning, and the leadership and participating squadron for their enthusiasm and support with the data collection.
Funding
This work was supported by the Next Generation Technologies Fund from the Defence, Science and Technology Group, Australia awarded to Monash University and Curve Tomorrow.
Author information
Authors and Affiliations
Contributions
Project conceptualisation: PV, SP, MH, SMWR, TLSStudy design: PV, EA, SMWR, TLSData collection: PVData analysis and interpretation: PV, LS, TLSDrafting of the manuscript: PV, LS, TLSCritical feedback and revision: PV, LS, SP, MH, EA, SMWR, TLSAll authors review the manuscript.
Corresponding author
Ethics declarations
Competing interests
Drs Varma, Shen and King, A/Prof Sletten and Prof Aidman have no conflicts of interest to declare in relation to this study. Other authors note following disclosures: Dr Postnova has no conflict of interest to declare. In the interest of full disclosure, she has projects with Qantas Airways Ltd and has an unpaid appointment with the Sleep Health Foundation. A/Prof Howard reports receiving institutional consulting fees from Teva Pharmaceuticals, Biogen, and Sanofi; and equipment to support research from Optalert and Philips Respironics outside the submitted work. Prof Rajaratnam is the current chair of the Sleep Health Foundation and has also been supported on grants from Vanda Pharmaceuticals, Philips Respironics, Cephalon, Rio Tinto, BHP Billiton, and Shell. Prof Rajaratnam also has received other support from Optalert, Compumedics, Teva Pharmaceuticals and Circadian Therapeutics, through his institution. He is a member of the National Sleep Foundation Sleep Timing Variability Consensus Panel, for which he was paid an honorarium through his institution. None of these disclosures are related to the current study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Varma, P., Shen, L., Postnova, S. et al. Understanding sleep health challenges of defence shift workers to design a digital, sleep and circadian management tool. Sci Rep 15, 10483 (2025). https://doi.org/10.1038/s41598-025-93597-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-93597-y