Abstract
Women undergoing in vitro fertilization-embryo transfer (IVF-ET) can suffer from anxiety and depression at various levels during the process. This study aimed to assess the anxiety and depression statuses (primary outcome) and influencing factors (secondary outcome) among patients undergoing IVF-ET. A 2019–2020 survey at Northwest Women’s and Children’s Hospital studied IVF-ET patients, evaluating anxiety and depression with GAD-7 and PHQ-9 alongside demographic data, using logistic regression for influencing factors. Among the 2465 women who undergoing IVF-ET, 27.18% had depression, and 18.46% had anxiety. Bachelors’ degree (OR = 0.659, 95%CI: 0.503–0.864), male factor infertility (OR = 0.745, 95%CI: 0.558–0.995), and assessment on the day of starting gonadotropin stimulation (OR = 0.781, 95%CI: 0.626–0.974) were negatively independently associated with depression, while comorbidities (OR = 1.541, 95%CI: 1.281–1.854) and an extended ART strategy (OR = 1.394, 95%CI: 1.162–1.672) were independently associated with depression. High school/technical school education (OR = 0.669, 95%CI: 0.490–0.915) and bachelor’s degree (OR = 0.640, 95%CI: 0.472–0.868) were negatively independently associated with anxiety, while an extended ART strategy (OR = 1.476, 95%CI: 1.197–1.820) was independently associated with anxiety. In conclusion, the prevalence of depression and anxiety was high in women undergoing IVF-ET. The study identified factors independently associated with depression and anxiety that could be used to guide the psychological management of women undergoing IVF-ET.
Similar content being viewed by others
Introduction
Assisted reproduction technology (ART) refers to all treatments or procedures that include the handling of human oocytes or embryos to help achieve pregnancy. In vitro fertilization (IVF) involves the extraction of oocytes, fertilization in the laboratory, and transfer of embryos into the uterus through the cervix. A full cycle of IVF typically includes one episode of controlled ovarian stimulation followed by oocyte retrieval. Oocyte retrieval involves the aspiration of any resultant oocytes just before follicular rupture under ultrasound guidance. The aspirated oocytes are then fertilized and cultivated in vitro, and one or two of the resultant embryos may be immediately transferred to the uterus for a fresh IVF cycle. Any remaining or all the embryos may be frozen for transfer later, referred to as a frozen IVF cycle1,2. Several ovarian stimulations, oocyte retrieval, and embryo transfer (ET) strategies are available; they all involve taking pills and/or receiving injections, culminating with oocyte retrieval (transvaginally or transabdominally), and terminating with embryo transfer. Still, despite all procedures, the success rates of IVF-ET are highly variable and depend on the cause of infertility, the woman’s age, comorbidities, and the selected strategy, among others3,4,5.
Therefore, IVF-ET can be a psychologically difficult period. The prevalence of depression and anxiety during IVF can be high, at 9%-17% for depression and 14%-23% for anxiety, and reaching disabling extents in 15%6,7,8. Indeed, women can already be affected by negative emotions due to infertility9,10. On top of that, IVF-ET involves hormonal manipulations, invasive procedures, a strict timetable without compromise, and uncertain pregnancy and birth outcomes that can be distressful to women11,12. Furthermore, previous studies showed that anxiety was associated with age, education level, and annual family income and that the incidence of depression was related to age and infertility period11,13,14,15,16.
Considering the various steps during an IVF cycle and the dynamic changes in hormones during the process, anxiety, and depression can vary in time during IVF-ET procedures. Indeed, Liu et al.11 showed that the incidence of anxiety peaked on the human chorionic gonadotropin (hCG) trigger day, while the depression scores peaked on the day the women started their treatments. Huang et al.17 also reported that depression scores were higher when starting treatments but subsequently decreased. Wu et al.18 reported different dominant negative emotions at different stages of IVF-ET. The previous studies examined the anxiety and depression scores on the day of treatment start, on hCG trigger day, and 4 days after ET. Additional time points and determining the factors associated with anxiety and depression during stimulation could help optimize the psychological support during IVF-ET.
Therefore, this study aimed to assess the anxiety and depression statuses and influencing factors among patients undergoing IVF-ET. Anxiety and depression were assessed at the start of ovarian stimulation, at the start of gonadotropin (Gn) stimulation, and on hCG trigger day.
Methods
Study design and participants
This cross-sectional survey study was conducted between September 2019 and May 2020 at the Reproductive Medicine Center of Northwest Women’s and Children’s Hospital and enrolled patients undergoing IVF-ET. This study was approved by the Ethics Committee of the Reproductive Medicine Center of Northwest Women’s and Children’s Hospital. Written informed consent was obtained from all participants.
The inclusion criteria were 1) patients undergoing IVF-ET and 2) able to understand and independently complete the clinical symptom questionnaires and the General Anxiety Disorder (GAD)-7 and Patient Health Questionnaire (PHQ)-9 scales. The exclusion criteria were 1) severe auditory or visual impairment, 2) concurrent malignancies, severe endocrine or reproductive organ diseases, or severe mental illnesses, or 3) significant psychological trauma in the past 2 years.
Outcomes
The primary outcome was the prevalence of anxiety and depression at different time points during IVF-ET. The secondary outcome was the factors influencing anxiety and depression.
Questionnaire design
Before the study, the investigators compiled and formulated the questionnaire survey through literature review, expert consultation, pre-experimentation, etc. The final survey tool included the basic and clinical information questionnaire and the GAD-7 and PHQ-9 self-assessment scales.
The basic and clinical information questionnaire was completed by the patients to collect personal information. It included sections on basic information, lifestyle and habits, medical history, female physiological and reproductive history, infertility status, menstrual and vaginal discharge conditions, general health status, and other relevant content.
The GAD-7 scale, due to its good internal consistency and convergent validity (Cronbach’s α = 0.917), is commonly used to measure general anxiety symptoms in various environments and populations19,20, including in patients undergoing IVF-ET21,22. It is simple, economical, and practical and is one of the most used diagnostic self-report scales for screening, diagnosing, and assessing the severity of anxiety disorders. The seven items are based on the Diagnostic and Statistical Manual of Mental Disorders (4th edition). Each item is scored as follows: 3 points = nearly every day, 2 points = more than half the days, 1 point = several days, 0 points = not at all. The total score is the sum of all items. The final score was categorized as 0–5 points indicating no anxiety, 6–9 points indicating mild anxiety, 10–14 points indicating moderate anxiety, and 15–21 points indicating severe anxiety19,20. The participants rated their symptoms over the past 2 weeks for each item.
The PHQ-9 is a self-reported questionnaire with nine items used for diagnosing depression and assessing its severity, with high validity (Cronbach’s α = 0.886)23, including patients with infertility and undergoing IVF-ET18,24. A systematic review comparing the specificity and sensitivity of 20 tools for diagnosing and grading depression found that the PHQ-9 has higher sensitivity and lower specificity for diagnosing depression compared to other psychological testing tools25. The brevity, self-administration, positive wording, and ease of scoring of PHQ-9 enhance its practicality and suitability in large-sample survey research and clinical settings, making it the most widely used instrument for measuring depressive symptoms in sample studies and clinical settings. The Chinese version of the PHQ-9 has reliable applicability in screening depression26,27. Maroufizadeh et al.28 studied the reliability and validity of the PHQ-9 in patients with infertility and found that the overall internal consistency and convergent validity of the sample were good, making it a reliable and effective tool for measuring depressive symptoms in patients with infertility and suitable for routine use in patients with infertility. The scale consists of nine items, and the severity of each depressive symptom is based on the Diagnostic and Statistical Manual of Mental Disorders (4th edition). Each item is scored as follows: 3 points = nearly every day, 2 points = more than half the days, 1 point = several days, 0 points = not at all. The total score is the sum of all items and is classified according to 0–4 points indicating no depression, 5–9 points indicating mild depression, 10–14 points indicating moderate depression, 15–19 points indicating moderately severe depression, and 20–27 points indicating severe depression23. The participants rated their symptoms over the past 2 weeks for each item.
Data collection
The patients scheduled to start IVF-ET and meeting the eligibility criteria were approached to ask whether they were interested in participating in the study. They were assured of the confidentiality of the collected data and that completing the questionnaires would take only a few minutes of their time during their visit to the hospital. Patients willing to participate provided written informed consent after the study personnel explained the study and answered any questions.
IVF-ET is the use of artificial methods to fertilize oocytes with sperm outside the body, undergo early embryonic development, and then transfer them into the uterine cavity of the mother. IVF-ET is a form of ART that develops into a fetus by implantation. The downregulation start date refers to the date on which the downregulation drugs were started. The Gonadotropin (Gn) start date was the date on which ovulation induction therapy with Gn was started. The hCG trigger day was the date when hCG was used to trigger the final maturation and ovulation.
Controlled ovarian stimulation is an important step in ART. In the process, it is necessary to go through three key steps: downregulation, superovulation, and hCG trigger. This study takes the starting point of these three key steps as the investigation time points. The purpose was to observe the degree of depression and anxiety endured by the patients at different time points of ART and related influencing factors to provide targeted guidance for the psychological management of women receiving IVF. At the same time, at these three time points, the types of drugs used and the mechanism of action change, resulting in fluctuations in hormone levels in the patients, and the impact on anxiety, depression, and other emotions is also more obvious. The investigators conducted separate questionnaire surveys on the participants at three time points: the start of ovarian stimulation, the start of Gn stimulation, and the hCG trigger day. These time points were selected because they were at the start of a new phase of IVF-ET and because they concluded the preceding phase. The start of a new IVF-ET phase is the moment when there are the most uncertainties for the patients and when the likelihood of anxiety or depression is the highest11,17,18. The participants completed the questionnaires at only one time point, selected randomly for each participant. The GAD-7 and PHQ-9 scales were self-administered during a waiting time during the hospital visit. For patients with lower levels of education, the investigators could read each statement of the scale to ensure that all items in the scale were correctly understood by the participants and that the participants made their judgments.
Quality control
This study is based on the National Major Difficult and Rare Diseases Collaborative Clinical Pilot Project for Infertility in Traditional Chinese and Western Medicine. In August 2019, a preliminary investigation was conducted at the Reproductive Center of Northwest Women’s and Children’s Hospital for 1 month. Over 500 survey forms were collected. Relevant gynecological experts and statisticians analyzed and modified the content of the questionnaire survey to determine the final questionnaire. Standardized training was conducted for the survey personnel before the formal survey, including training on the research protocol, diagnostic interviews, and filling out the forms to improve the homogeneity of the survey personnel and ensure the accuracy and reliability of the survey data. Before the survey, the principle of informed consent from the research subjects was followed, and informed consent forms were signed. Trained traditional Chinese medicine practitioners (investigators) filled out the information collection forms. The survey was conducted in independent consultation rooms to ensure a bright, comfortable, and quiet environment. Each investigator was responsible for one survey unit and asked the participants about each item in the survey form, ensuring that each participant understood the questions consistently. The participants were allowed to complete the entire questionnaire without interference, typically taking about 10 min.
Statistical analysis
In this study, the depression and anxiety status of each time point were investigated, and the TCM syndromes of the participants were also collected. The sample size of the depression and anxiety survey was referred to using the TCM syndrome survey sample size calculation. That is, there are 31 TCM syndrome items in total. The sample size is then the number of diagnostic indicators of syndrome × 5–10 times, indicating that the minimal sample size would be 155 patients. Therefore, the number of patients with depression or anxiety at each time point should be ≥ 155. The actual three time points included 836, 806, and 823 patients, respectively.
A database was established using EpiData 3.0 (www.EpiData.dk), and double data entry was conducted using the double-entry method for questionnaire input and consistency checks. Statistical analysis was performed using SPSS 25.0 (IBM, Armonk, NY, USA). Missing data were not imputed. The categorical data were expressed as n (%) and compared using the chi-squared test. Multivariable logistic regression was used to analyze the factors independently associated with anxiety and depression, using no anxiety/depression vs. with anxiety/depression and then using the severity of anxiety/depression among those with anxiety/depression. Variables with P < 0.05 and without multicollinearity (Table S1) to each other in the univariable analysis were included into the multivariable logistic regression model. Two-sided P-values < 0.05 were considered statistically significant.
Results
Characteristics of the participants
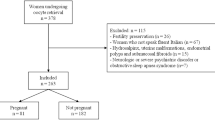
This study enrolled 2465 women undergoing IVF-ET. Among them, 54.28% were 21–27, 37.08% were 28–34, and 8.64% were ≥ 35. Most women had a junior college education or above (57.08%), an income of 2000–4999 RMB/month (46.29%), and comorbidities (51.32%). The cause of infertility was female factors in 52.37%, male factors in 21.62%, and female and male factors in 6.49%; idiopathic infertility was observed in 19.51%. The duration of infertility was ≥ 3 years in 59.83% of the women. About half of the patients underwent the standard and extended strategies. About one-third of the participants were assessed for anxiety and depression at each of the three time points. Furthermore, the depression status varied with comorbidities (P < 0.001), the cause of infertility (P = 0.008), the duration of infertility (P = 0.021), the ART strategy (P < 0.001), and the time of assessment (P = 0.006). The anxiety status varied with educational level (P = 0.015), comorbidities (P < 0.001), cause of infertility (P = 0.008), duration of infertility (P = 0.021), and ART strategy (P < 0.001) (Table 1).
Occurrence rate of anxiety and depression
Among the 2465 participants, 20.93% (95%CI: 19.33%-22.54%) had mild depression, 4.71% (95%CI: 3.87%-5.54%) had moderate depression, 1.22% (95%CI: 0.78%-1.65%) had severe depression, and 0.32% (95%CI: 0.10%-0.55%) had very severe depression. Regarding anxiety, 13.75% (95%CI: 12.39%-15.11%) had mild anxiety, 3.98% (95%CI: 3.20–4.75) had moderate anxiety, and 0.73% (95%CI: 0.39–1.07) had severe anxiety (Table 2).
Multivariable analyses
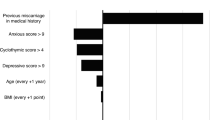
Bachelors’ degree (OR = 0.659, 95%CI: 0.503–0.864, P = 0.002), male factor infertility (OR = 0.745, 95%CI: 0.558–0.995, P = 0.046), and assessment on the start of Gn (OR = 0.781, 95%CI: 0.626–0.974, P = 0.028) were negatively (i.e., protective) independently associated with depression. On the other hand, comorbidities (OR = 1.541, 95%CI: 1.281–1.854, P < 0.001) and an extended ART strategy (OR = 1.394, 95%CI: 1.162–1.672, P < 0.001) were independently associated with depression (Table 3). In addition, high school/technical school education (OR = 0.669, 95%CI: 0.490–0.915, P = 0.012) and bachelor’s degree (OR = 0.640, 95%CI: 0.472–0.868, P = 0.004) were negatively (i.e., protective) independently associated with anxiety; an extended ART strategy (OR = 1.476, 95%CI: 1.197–1.820, P < 0.001) was independently associated with anxiety (Table 4).
Moreover, infertility for 3–5 years (OR = 0.651, 95%CI: 0.425–0.997, P = 0.048) was independently associated with the severity of depression (Table 5). No factor was observed exhibiting association with the severity of anxiety (all P > 0.05) (Table 6).
Discussion
Women undergoing IVF-ET can suffer from anxiety and depression at various levels during the process. This study assessed the anxiety, depression status, and influencing factors among patients undergoing IVF-ET at three different time points. The results suggested that the prevalence of depression and anxiety was high in women undergoing IVF-ET. Bachelor’s degree, male factor infertility, and assessment on the day of starting Gn were negatively (i.e., protective) independently associated with depression, while comorbidities and an extended ART strategy were independently associated with depression. High school/technical school education and a bachelor’s degree were negatively (i.e., protective) independently associated with anxiety, while an extended ART strategy was independently associated with anxiety.
In China, infertile couples are under pressure from families and society to attain traditional family ideals, leading to negative emotions22,29. In the present study, the prevalence of depression was 27.18%, and the prevalence of anxiety was 18.46%. Those figures are the reverse of previous studies that showed a prevalence of depression of 15.8%-30.0% and a prevalence of anxiety of 30.0%-42.9% among women undergoing IVF-ET11,17. The discrepancy could be due to the different tools used: GAD-7 and PHQ-9 in the present study, Beck depression and anxiety scales in Huang et al.17, and Zung Self-Rating Depression/Anxiety Scales in Liu et al.11. Other local factors could also be involved, such as psychological support offered by the different hospitals during IVF-ET, as well as local traditional ideals and peer pressure.
The present study showed that a bachelor’s degree, male factor infertility, and assessment on the day of starting Gn were protective factors against depression, while comorbidities and an extended ART strategy were associated with depression. Similarly, high school/technical school education and a bachelor’s degree were protective against anxiety, while an extended ART strategy was associated with anxiety. Those factors are globally supported by Liu et al.11, who showed that age, education level, and annual family income were associated with anxiety and that age and infertility period were associated with depression. Xu et al.13 also reported that a lower educational background was associated with anxiety and depression. Other studies reported similar associations14,15,16. The prevalence of infertility is higher in women than in men15,30,31. Women will experience more anxiety and depression when the cause of infertility is female factors only32, supporting male-factor infertility as a protective factor against depression in infertile couple women and highlighting the need for proper psychological support for infertile women33. A longer ART strategy will expose the women to longer procedures, which can ultimately lead to higher depression when starting IVF-ET due to the expected longer exposure to hormonal manipulations.
The first time point of downregulation indicates the formal initiation of treatment. At this time point, although the patient is fully prepared psychologically, the various unknowns in the subsequent treatment make them stressful. The second time point, the Gn start day, is the core link of controlled ovarian stimulation, and the initiation dose should be determined according to the patient’s previous treatment history, BMI, AMH, and antral follicle number. After the use of moderating drugs, the effect of the drug is observed on the patient and whether it will cause the emergence or severity of depression and anxiety in the patients. The third time point is the hCG trigger day, i.e., when the controlled ovarian stimulation treatment is completed, and the oocyte retrieval process is about to enter. The quantity and quality of oocytes obtained are the issues and common concerns of physicians and patients. At this time, with the obvious changes in hormone levels in the body, the body and the mind have synchronized changes, and it is necessary to compare and understand the changes and progress of the anxiety and depression state of patients.
Hence, the psychological status of infertile women can change during the IVF process. When entering the IVF-ET process, they know that the success rate is not 100%, but they still feel pressure due to their history of infertility and peer and societal pressure34,35. On hCG trigger day, they can feel more confident because they feel the effects of ovarian stimulation, and they have higher success expectations34. After the cycle, the women can worry about whether the time, money, and effort spent will be rewarded34. Liu et al.11 and Huang et al.17 reported that depression peaked when entering the cycle, while anxiety peaked on hCG trigger day. Awtani et al.34 reported that anxiety peaked after the cycle. The present study showed that the prevalence of depression was lower on the day of starting Gn, which could be related to the positive feelings and confidence of the women, as supported by a previous study34, but no influence was seen for anxiety. The discrepancies among studies could be due to the different time points selected and the different assessment tools. Still, depression was observed during the whole cycle, suggesting that the women would need psychological support during the entire process. Nevertheless, identifying the moments during IVF-ET when the patients are more susceptible to developing anxiety and/or depression would allow for a more optimal screening for negative emotions, which could be managed in time for optimal outcomes. In addition, identifying the factors contributing to anxiety and depression during IVF-Et could allow for a more personalized approach.
This study had strengths and limitations. This study enrolled many participants, but they were all from the same geographical area and hospital, decreasing the generalizability of the results. Indeed, the course of IVF-ET and associated depression and anxiety could be related to local practices and cultural characteristics. The cross-sectional nature of the study prevents the analysis of causality and mechanisms. Furthermore, the present study covered only the IVF-ET period, and anxiety and depression were not assessed after IVF-ET. It can be hypothesized that anxiety and depression will be different according to the pregnancy outcomes. Correlations with the IVF-ET outcomes were not performed since the outcomes were not collected. Future studies could include such time points. Furthermore, the enrolled patients were assessed at only one of the three time points. The three time points were relatively close in time, and assessing the same patients three times within a short time window would increase the risk of a carryover bias, i.e., the participants remembering what they responded to the last time. No measures were taken to account for seasonal variations. Finally, part of the study was performed during the beginning of the COVID-19 pandemic, which added a psychological burden to the general population and the patients undergoing ART, which might have influenced the results36. Although the COVID-19 pandemic was officially called by the WHO in March 202037, the first cases were reported in China in December 201938, and public anxiety was already increasing39. China started to take measures to control the spread of the virus before the WHO declared the pandemic status39. Therefore, most of the patient enrollment occurred during the COVID-19 period. ART involves frequent visits to the hospital, bringing fear of COVID-19 infection because sick people were visiting the hospitals and were being hospitalized when they tested positive for COVID-19. Visiting the hospital could also involve public transportation, adding to fear. With the COVID-19 measures being firmly followed in China, the lockdown also brought challenges for patients who had to visit the hospital frequently. Considering the precise timing of IVF-ET procedures, such factors, combined with the anxiety directly related to COVID-1940, could have contributed to anxiety and depression. Of course, now that the COVID-19 pandemic has officially ended, the results should be externally validated to confirm whether they are still observed.
The prevalence of depression and anxiety was high in women undergoing IVF-ET. The study identified factors independently associated with depression and anxiety that could be used to guide the psychological management of women undergoing IVF-ET. The depression status changed during the IVF cycle.
Data availability
All data generated or analysed during this study are included in this published article.
References
Child, T. Optimising the management of patients with infertility. Practitioner. 257(19–22), 12–13 (2013).
Lindsay, T. J. & Vitrikas, K. R. Evaluation and treatment of infertility. Am. Fam. Physician. 91, 308–314 (2015).
Zargar, M., Dehdashti, S., Najafian, M. & Choghakabodi, P. M. Pregnancy outcomes following in vitro fertilization using fresh or frozen embryo transfer. JBRA Assist. Reprod. 25, 570–574 (2021).
Mizrachi, Y. & McQueen, D. B. Embryo transfer success: It is in our hands. Fertil. Steril. 118, 815–819 (2022).
Muhaidat, N. et al. Factors Affecting the Outcomes of First in vitro Fertilization and Embryo Transfer: A Retrospective Investigation. Int. J. Womens Health. 15, 1537–1545 (2023).
Chen, T. H., Chang, S. P., Tsai, C. F. & Juang, K. D. Prevalence of depressive and anxiety disorders in an assisted reproductive technique clinic. Hum. Reprod. 19, 2313–2318 (2004).
Li, G. et al. Trajectories and predictors of anxiety and depression amongst infertile women during their first IVF/ICSI treatment cycle. J. Psychosom. Res. 142, 110357 (2021).
Zhang, L. et al. Prevalence and associated risk factors for anxiety and depression in infertile couples of ART treatment: a cross-sectional study. BMC Psychiatry. 22, 616 (2022).
Fallahzadeh, H., Zareei Mahmood Abadi, H., Momayyezi, M., Malaki, M. H. & Keyghobadi, N. The comparison of depression and anxiety between fertile and infertile couples: A meta-analysis study. Int. J. Reprod. Biomed. 17, 153–162 (2019).
Braverman, A. M., Davoudian, T., Levin, I. K., Bocage, A. & Wodoslawsky, S. Depression, anxiety, quality of life, and infertility: a global lens on the last decade of research. Fertil. Steril. 121, 379–383 (2024).
Liu, Y. F., Fu, Z., Chen, S. W., He, X. P. & Fan, L. Y. The analysis of anxiety and depression in different stages of in vitro fertilization-embryo transfer in couples in China. Neuropsychiatr. Dis. Treat. 17, 649–657 (2021).
Zhou, Y., Sun, Z. & Song, J. Research progress on the impact of anxiety and depression on embryo transfer outcomes of in vitro fertilization. Zhejiang Da Xue Xue Bao Yi Xue Ban. 52, 61–67 (2023).
Xu, H. et al. The effects of anxiety and depression on in vitro fertilisation outcomes of infertile Chinese women. Psychol. Health Med. 22, 37–43 (2017).
Chiaffarino, F. et al. Prevalence and incidence of depressive and anxious symptoms in couples undergoing assisted reproductive treatment in an Italian infertility department. Eur. J. Obstet. Gynecol. Reprod. Biol. 158, 235–241 (2011).
Karimzadeh, M. et al. Psychological disorders among Iranian Infertile couples undergoing assisted reproductive technology (ART). Iran J. Public Health. 46, 333–341 (2017).
Crawford, N. M., Hoff, H. S. & Mersereau, J. E. Infertile women who screen positive for depression are less likely to initiate fertility treatments. Hum. Reprod. 32, 582–587 (2017).
Huang, L. H., Kuo, C. P., Lu, Y. C., Lee, M. S. & Lee, S. H. Association of emotional distress and quality of sleep among women receiving in-vitro fertilization treatment. Taiwan J. Obstet Gynecol. 58, 168–172 (2019).
Wu, L. et al. Psychological distress among women undergoing in vitro fertilization-embryo transfer: A cross-sectional and longitudinal network analysis. Front. Psychol. 13, 1095365 (2022).
Spitzer, R. L., Kroenke, K., Williams, J. B. & Lowe, B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 166, 1092–1097 (2006).
Johnson, S. U., Ulvenes, P. G., Oktedalen, T. & Hoffart, A. Psychometric properties of the general anxiety disorder 7-item (GAD-7) scale in a heterogeneous psychiatric sample. Front Psychol. 10, 1713 (2019).
Omani-Samani, R., Maroufizadeh, S., Ghaheri, A. & Navid, B. Generalized Anxiety Disorder-7 (GAD-7) in people with infertility: A reliability and validity study. Middle East Fertil. Soc. J. 23, 446–449 (2018).
Omani-Samani, R., Ghaheri, A., Navid, B., Sepidarkish, M. & Maroufizadeh, S. Prevalence of generalized anxiety disorder and its related factors among infertile patients in Iran: a cross-sectional study. Health Qual. Life Outcomes. 16, 129 (2018).
Kroenke, K., Spitzer, R. L. & Williams, J. B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 16, 606–613 (2001).
Wan, L. & He, S. Association between depression and infertility based on the PHQ-9 score: Analyses of NHANES 2013–2018. PLoS One. 19, e0305176 (2024).
Negeri, Z. F. et al. Accuracy of the Patient Health Questionnaire-9 for screening to detect major depression: updated systematic review and individual participant data meta-analysis. BMJ. 375, n2183 (2021).
Ye, X. et al. Reliability and validity of the Chinese version of the patient health questionnaire-9 (C-PHQ-9) in patients with psoriasis: a cross-sectional study. BMJ Open. 10, e033211 (2020).
Wang, W. et al. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen. Hosp. Psychiatry. 36, 539–544 (2014).
Maroufizadeh, S., Omani-Samani, R., Almasi-Hashiani, A., Amini, P. & Sepidarkish, M. The reliability and validity of the Patient Health Questionnaire-9 (PHQ-9) and PHQ-2 in patients with infertility. Reprod. Health. 16, 137 (2019).
Omani-Samani, R., Maroufizadeh, S., Almasi-Hashiani, A. & Amini, P. Prevalence of depression and its determinant factors among infertile patients in Iran based on the PHQ-9. Middle East Fertil. Soc. J. 23, 460–463 (2018).
Maroufizadeh, S., Hosseini, M., Rahimi, F. A., Omani-Samani, R. & Amini, P. The effect of depression on quality of life in infertile couples: an actor-partner interdependence model approach. Health Qual. Life Outcomes. 16, 73 (2018).
Maroufizadeh, S., Hosseini, M., Rahimi, F. A., Omani-Samani, R. & Amini, P. Application of the dyadic data analysis in behavioral medicine research: marital satisfaction and anxiety in infertile couples. BMC Med. Res. Methodol. 18, 117 (2018).
Massarotti, C. et al. Impact of infertility and infertility treatments on quality of life and levels of anxiety and depression in women undergoing in vitro fertilization. Gynecol. Endocrinol. 35, 485–489 (2019).
Lim, G. S., Kayanoth, R. K., Broekman, B. F. & Chee, C. Y. Perception of a single-session pre-in vitro fertilisation counselling service and attitudes towards support group: a survey of patients in Singapore. Singapore Med. J. 59, 316–321 (2018).
Awtani, M. et al. Anxiety and stress at different stages of treatment in women undergoing in vitro fertilization-intracytoplasmic sperm injection. J. Hum. Reprod. Sci. 12, 47–52 (2019).
Ishihara, O. et al. International committee for monitoring assisted reproductive technologies: world report on assisted reproductive technologies, 2007. Fertil. Steril. 103(402–413), e411 (2015).
Cao, J. X. et al. Anxiety and depression among pregnant women undergoing IVF-ET and WeChat group peer support during the COVID-19 pandemic: Study protocol for a randomized controlled trial. Medicine (Baltimore). 101, e32515 (2022).
Cucinotta, D. & Vanelli, M. WHO declares COVID-19 a pandemic. Acta. Biomed. 91, 157–160 (2020).
Sadeghmoghadam, L., Daneshfar, M., Sharifi, F. & Alizad, V. How the first cases of COVID-19 in 10 countries become infected? a case series. Respir. Med. Case Rep. 46, 101219 (2020).
Zhao, H. et al. COVID-19 infection outbreak increases anxiety level of general public in China: involved mechanisms and influencing factors. J. Affect. Disord. 276, 446–452 (2020).
Delpino, F. M. et al. Prevalence of anxiety during the COVID-19 pandemic: A systematic review and meta-analysis of over 2 million people. J. Affect. Disord. 318, 272–282 (2022).
Funding
This work was supported by the National Major Difficult Diseases Infertility Clinical Collaboration project of Traditional Chinese and Western Medicine ([2018] No. 3), the Research project of the Traditional Chinese Medicine Administration of Shaanxi Province (SZY-KJCYC-2023–030), National Famous Old Chinese Medicine Experts Inheritance Studio Construction Project ([2022] 36), Xianyang City Science and Technology Bureau key research and development plan project (L2023-ZDYF-SF-039), and Traditional Chinese Medicine Technology Innovation and Capacity Expansion Plan Project (TZKN-CXRC-11).
Author information
Authors and Affiliations
Contributions
Data curation: Hongli Zhu, Jiaojiao Dong, Mimi Luo, Han Zhang, Di Xu Conceptualization, Methodology: Mei Chen, Fengjie He, Juanzi Shi Formal analysis, Visualization, Investigation, Writing—original draft preparation: Nan Li, Jun Bai, Lijun Wang Writing—review and editing: Nan Li, Jun Bai, Lijun Wang, Mei Chen, Hongli Zhu, Jiaojiao Dong, Mimi Luo, Han Zhang, Di Xu, Fengjie He, Juanzi Shi.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This work has been carried out in accordance with the Declaration of Helsinki (2000) of the World Medical Association. This study was approved by the Ethics Committee of the Reproductive Medicine Center of Northwest Women’s and Children’s Hospital (2019003). Written informed consent was obtained from all participants.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, N., Bai, J., Wang, L. et al. Factors influencing the anxiety and depression status in patients undergoing in vitro fertilization-embryo transfer assisted pregnancy. Sci Rep 15, 16303 (2025). https://doi.org/10.1038/s41598-025-94247-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-94247-z