Abstract
We aim to explore the contributing factors to intrinsic capacity (IC) in middle-aged and older patients after percutaneous coronary intervention (PCI). Intrinsic capacity comprises six core domains: cognition, locomotion, vitality, psychology, vision, and hearing. Each ___domain was assessed in detail using different scales, based on which the composite IC score was calculated. The study employed latent class analysis (LCA) to identify the various IC subtypes. Logistic regression analyses were used to determine the effect variables of IC subtypes. 318 middle-aged and older post-PCI patients filled out the assessments. Three distinct IC subtypes were found: 47.8% poor audition-vision group (class 1), 38% high cognition-psychology group (class 2), and 14.2% low locomotion-vitality group (class 3). The IC subtype classification may be impacted by factors such as cTnI, NT proBNP, cardiac function, exercise frequency, and comorbidities. Examining IC subtypes may be helpful for focused intervention, and further empirical research is still needed to determine their drivers.
Similar content being viewed by others
Introduction
Coronary heart disease (CHD) is the primary cause of death in cardiovascular disease (CVD), which has been a priority disease for prevention and control globally. The overall death rate from CHD among Chinese citizens, both urban and rural, was 283.27/100,000, according to the most recent China Health Statistics Yearbook. This rate rose sharply with age, with almost 74.3% of the population over 45. Percutaneous coronary intervention (PCI) is currently one of the primary treatments for CHD, and the statistics indicate that its growth rate is 26.4%. More attention must be given to the patient’s general health after PCI in these cases.
Patients in the senior age group (≥ 75) are more likely to get cautious or inadequate treatment, and becoming older is a proven indicator of a poor result following PCI1,2. Patients in this group who need to undergo PCI will again face the challenge of choosing the surgical methods and frequency3. The comorbidity, multiple medications, the number and severity of vascular lesions, and the number of stent implants may all affect the prognosis of patients undergoing PCI. Currently, the short-term functional recovery and long-term prognostic effects of drugs on patients after PCI are still unclear4. This prompts us to consider comprehensively from the perspectives of treatment, organization, and economy, while also paying attention to factors related to PCI and those that may affect the functional recovery of patients after PCI.
According to the most recent healthy ageing framework proposed by WHO, intrinsic capacity (IC) is considered the core of functional ability, which is defined as the sum of an individual’s physiological and psychological abilities at any given time5. IC represents the amount of resources available to an individual’s lifetime and requires a variety of health characteristics to fully reflect his or her overall state. The six interrelated domains of locomotion, cognition, vitality, psychology, vision, and hearing comprise the WHO’s conceptualization of IC6,7. Intrinsic capacity declines since mid-adulthood. Studies have shown that 39.9–93.4% of middle-aged and older adults experience IC decline5,8,9,10,11,12,13, with individual characteristics (including biological indicators), lifestyles, treatments, and environments as the main influences on IC heterogeneity14,15,16,17,18.
Consistent with the WHO concept of interactions between IC and environments, studies have shown that 75% of the diversity in IC is driven by the cumulative effects of individual behavior and environmental exposures, which are controllable, while hereditary variables determine 25% of the diversity in IC. A recent review reached similar conclusions that social determinants (including socioeconomic status, lifestyles, psychosocial factors, material circumstances, and healthcare systems) significantly impact IC19. Understanding the socio-environmental factors influencing IC of reasonably robust individuals prior to significant losses may facilitate the identification of interventions early in the life course. Instead of exploring a comparatively single source of socio-environmental support like earlier research (most support was from family and friends, or society)20,21, chronic disease resource utilization is based on a social-ecological model of resources, viewing the environment as a multi-level overall structure. This concept seems to fit in better with the way that the environment is interpreted in the WHO’s framework for healthy ageing. Therefore, we assessed chronic disease resource utilization, partly as a reflection of socio-environmental factors that may influence the IC. In addition, taking into account the trade-off between improved intervention efficiency and precision, our study also aims to identify the heterogeneous IC subtypes in middle-aged and older patients after PCI and explore the impacts of subtypes. Specifically, we test the hypothesis that preoperative cardiac biomarkers such as NT proBNP, CK, and CK MB, will explain at least some of the association between multiple measures of environment and intrinsic capacity.
Methods
Design and participants
We conducted a cross-sectional study, and patients after PCI were chosen from a tertiary hospital in Zhejiang province through convenience sampling. The inclusion criteria were as follows: (1) age ≥ 45 years old; (2) emergency or elective PCI patients; (3) conscious, can communicate normally and cooperate in completing the assessments; (4) signed the informed consent, willing to accept the follow-up assessments. Patients with severe physical or mental illnesses, end-stage patients, pregnant women, and disabled individuals were excluded. Sociodemographic and clinical characteristics, individual behavior, environmental factors, and IC were collected through in-person interviews.
Before the study began and throughout its duration, all patients were made aware of its goal. Before the patient’s evaluation, informed consent was acquired. The hospital’s ethical committee approved the study (No. 20240459) on April 16, 2024, and it was carried out in compliance with the Declaration of Helsinki.
Measures
Intrinsic capacity
According to previous literature and WHO’s ICOPE guidelines, the measurement tools used to evaluate IC in this study are as follows: The mini-mental state examination (MMSE) was used to assess cognition and a score of ≤ 17 (illiteracy), 20 (primary school), 22 (middle school), or 23 (college) indicates cognitive impairment22,23. The short physical performance battery test (SPPB) was used to assess locomotion, with a score of ≤ 9 indicating a decline in physical function24. The patient health questionnaire-9 (PHQ-9) was used to assess psychology, and a score of ≥ 10 indicates depression25. Vitality was assessed using the mini-nutritional assessment short form (MNA-SF), with a score of ≤ 11 indicating nutritional deficiency26. Simple questions were used for the visual and auditory assessments. A decline in any IC ___domain was scored as a zero. The total IC score is 0–6 points, the higher the score, the better the IC one’s own.
Other variables
Some variables were assessed through interviews, such as age, sex, religion, ethnicity, education, marital status, occupation, family income, living areas, medical insurance, smoking, drinking, daily dietary and exercise habits, chronic disease resource utilization (through Chronic Illness Resource Survey, CIRS27, higher scores on this scale represent the better, with a mean score ≥ 3 considered high). The Charlson comorbidity index28 (CCI, reflecting the severity of comorbidities), the number of medications, cardiac function (NYHA GEADE), and the number of stent implantations were collected from the hospital’s medical record system. We obtained information on multiple coronary artery lesions through medical imaging reports. During hospitalization, N-terminal pro-B-type (NT proBNP), cardiac troponin I (cTnI), creatine kinase (CK), creatine kinase isoenzymes (CK-MB), and hypersensitive C-reactive protein (hs-CRP) were documented for several times. We selected the records tested on patients’ admission for analysis. We also referred to the hospital system’s definition of the normal range for blood indicators.
Data analysis
Descriptive statistics were used for the assessed variables. Latent Class Analysis (LCA) was performed using Mplus 8.3 to explore the heterogeneous IC subtypes of middle-aged and older patients after PCI. For the present study, four latent class models were fitted to determine the optimal number of latent classes. The optimal number of classes was chosen based on a series of model fit statistics and the interpretability of the clusters. The model fit statistics included the Akaike information criterion (AIC), Schwarz’s Bayesian information criterion (BIC), the sample-size-adjusted BIC (aBIC), and the lower information criterion indicating a better model fit. Lo–Mendell–Rubin likelihood ratio test (LMR), bootstrap likelihood ratio test (BLRT), and entropy were also selected as model fit statistics. Significant LMR and BLRT could help evaluate whether a k-class model is better than a k-1 class model. The entropy presents classification accuracy, and an entropy value closer to 1 indicates better accuracy. After identifying the best-fitting profile solution, each participant was assigned to a most likely heterogeneous subtype based on their posterior class probability (no less than 5% of the total number of individuals in each class). Factors assessed were compared between groups using Chi-square tests or nonparametric tests using SPSS version 25.0. Significant variables (P < 0.1) were included in multinomial logistic regression to explore the influencing factors of IC subtypes.
Results
Decline in IC and its domains
The total sample size collected was 318, and the rate of IC decline was 80.2% (composite IC ≤ 5). The mean composite IC score in middle-aged and older post-PCI patients was 4.22 (1.39), while the proportion of the decline in each IC ___domain varies, with 5% of the patients having cognitive impairment, 27.7% having physical function decline, 41.5% having nutritional deficiency, 14.5% having depression, 43.7% having decreased vision, and 45.3% having decreased hearing (Table 1).
Latent class analysis
To identify the heterogenous subtypes of IC among 318 patients after PCI, an LCA was performed on the entire sample using six indicator variables (locomotion, cognition, psychology, vitality, vision, and hearing). The results of LCA (Table 2) indicated that BLRT was significant for the two- to four-class solutions. However, LMR suggested that the 2-class and the 3-class were better than the 4-class and 5-class, respectively. Models with 3-class showed lower AIC, BIC, and aBIC than models with 2-class. Moreover, entropy values in 3-class solutions were much higher than in 2-class solutions. Therefore, the 3-class solutions were chosen to be the best fit to the data based on a series of model fit statistics.
Figure 1 shows the mean scores of six domains of IC (locomotion, cognition, psychology, vitality, vision, and hearing). The y-axis represents the probability of domains, while the x-axis represents IC domains used for the latent class analysis. The three lines showed different IC patterns for the three subtypes (Fig. 1). The first class (47.8%) was labeled as the “low audition-vision group” representing individuals with impairments predominantly in two IC domains (vision and hearing). The second class (38.0%) was labeled as the “high cognition-psychology group” representing individuals with almost no decline in two IC domains (cognition and psychology). The third class (14.2%) was labeled as the “low locomotion-vitality group” representing individuals with impairments mainly in two domains of IC (locomotion and vitality).
Influencing factors on IC subtypes
Univariate analysis results showed age, sex, occupation, education, drinking, exercise frequency, exercise duration, CCI, number of medications, heart function (NYHA GRADE), multiple coronary artery lesions (≥ 2 large vessels and ≥ 50% stenosis), number of stent implants, NT proBNP, and cTnI were significantly different across the three IC subtypes.
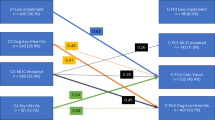
The assignment of variables can be found in Table 3 (highest assigned value as reference). The results of multinomial logistic regression analysis showed that when comparing class 1 and class 3 (class 3 as reference), NYHA GRADE III–IV (OR = 4.31, 95% CI [1.49–12.5]) and abnormal NT proBNP (OR = 2.79, 95% CI [1.17–6.62]) were more likely to be categorized into class 3 (low locomotion-vitality group). When comparing class 2 and class 3 (class 3 as reference), exercise frequency ≥ 5 times per week (OR = 3.12, 95% CI [1.08–8.98]), lower CCI points (OR = 0.34, 95% CI [0.13–0.89]) were more likely to be categorized into class 2 (high cognition-psychology group). NYHA GRADE III–IV (OR = 7.81, 95% CI [1.45–41.67]), abnormal cTnI (OR = 4.90, 95% CI [1.81–13.33]) were more likely to be categorized into class 3 (low locomotion-vitality group) (Tables 4, 5).
Discussion
“Old age” has its own physiological definition, with 60 or 65 years of age often used as the threshold for entering old age in demographics. Most of the existing studies on IC have focused on community-dwelling older adults14,29,30, while only few studies included middle-aged adults or situated the context in a hospitalized setting. Middle-aged people, as a group entering old age, are more likely to be more resistant and resilient and have a higher marginal value for maintaining IC than patients already in old age. To our knowledge, this is the first study to explore the heterogeneous IC subtypes as well as investigate the influence factors of IC subtypes among both middle-aged and older patients after PCI. Although the widespread use of PCI in recent decades has greatly improved the prognosis of patients with CHD, patients still face major burdens from PCI-related unfavorable outcomes, and functional recovery of patients after discharge requires comprehensive attention. We found that the prevalence of IC decline in this population was 80.2%, which was higher than previous studies analyzing the IC decline of patients with CVD (64.1–68.3%)31,32,33. Possible reasons are the differences in regions, populations, and disease severity, or different tools have been used for assessing each ___domain of IC, despite the recommendations in ICOPE guidelines proposed by WHO. Future research could compare the features of the IC ___domain decline in post-PCI patients across different age groups and offer a detailed examination of the dose-response relationship between environmental or individual factors and the IC decline using standardized IC scoring.
In the context of precision medicine’s ongoing development, better information is required to comprehend how different IC subtypes react to specific interventions. Stratifying middle-aged and older post-PCI patients by IC subtypes offers a workable path for identifying populations for whom interventions are most effective and may be more appropriate than categorizing them by age or comorbidity index. Our results revealed three distinct IC subtypes. Comorbidities, cardiac function, exercise frequency, NT proBNP, and cTnI were potential categorization-influencing factors. Highly specific and sensitive inflammatory indicators for identifying IC decline remain elusive. Tumor necrosis factor-alpha, C-reactive protein, and interleukin-6 may all be indicators of IC decline34, however, their outcomes with composite IC or each IC ___domain are not always consistent. A recent study found that soluble suppression of tumorigenicity 2 (sST2) was associated with microvascular occlusion after PCI in ST-segment elevation myocardial infarction (STEMI) patients35. Changes in sST2 may also affect IC in patients after PCI. Taking individual variability or the illness features of a comparable group into account, investigating the use of various analytes rather than depending on a single marker may be more advantageous and informative for tracking IC decline. Future studies can also explore the impact of more new markers on the prognosis of patients undergoing PCI.
The latent category analysis can initially reveal the characteristics of impaired capacities belonging to specific IC subtypes. However, we found that there is no difference in chronic disease resource utilization between the three IC subtypes, which may be due to monocentric environmental sampling bias or explained by the fact that IC has a certain degree of group similarity in a similar context. The feasibility of the classification of IC subtypes suggests that the cognitive, locomotor, psychological, visual, and auditory subdomains can be considered overt manifestations of capacity. On the other hand, this also reveals that the effect of severe impairment of a particular capacity on the composite IC may be covered in the short term, which would hinder the early identification of IC decline.
Limitations
This study has inherent bias because it is a single-center investigation. We anticipate further optimization techniques in the future to enhance this research. First, the IC subtypes we created for middle-aged and older adults after PCI may not be applicable to other populations or situations due to the degree of generalization, and the IC characteristics and correlations of other populations have not yet been studied. Second, the results’ generalizability might be constrained by the small sample size. In the future, multicenter research comparing differences in IC characteristics across different populations and their causes may be undertaken. Furthermore, the more microscopic perspective enables early detection of IC deterioration and precise intervention. Future studies could look more closely at the characteristics of impaired capacities under a certain IC subtype, including which capacities are commonly affected at the same time and whether restoring the bridge capacity improves the others. Finally, to further clarify the link between IC and the environment, dynamic monitoring to analyze longitudinal associations from a prospective standpoint is a problem worth exploring for future research.
Conclusion
Our findings reflect two main conclusions: From a macro viewpoint, the possible connection between a characteristic group’s health and the multi-level environment, in its broadest sense, offers a helpful guide for enhancing the effectiveness of interventions. From a micro perspective, a quick decline in an individual’s functioning might result from changes in one ___domain of IC, which can be easily disregarded in terms of their impact on composite IC. This highlights the significance of focusing on individual heterogeneity and monitoring dynamics.
Data availability
Data is provided within the supplementary information files.
References
Bainey, K. R. et al. Pharmaco-Invasive strategy with Half-Dose tenecteplase in patients with STEMI: prespecified pooled analysis of patients aged ≥ 75 years in STREAM-1 and 2. Circ. Cardiovasc. Interv 17(12), e014251 (2024).
Riehle, L. et al. Implementation of the ESC STEMI guidelines in female and elderly patients over a 20-year period in a large German registry. Clin. Res. Cardiol. 112(9), 1240–1251 (2023).
Biscaglia, S. et al. Complete or Culprit-Only PCI in older patients with myocardial infarction. N Engl. J. Med. 389(10), 889–898 (2023).
Watanabe, H., Ozasa, N., Morimoto, T. & Shiomi, H. Long-term use of carvedilol in patients with ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention (2024).
Beard, J. R., Officer, A. M. & Cassels, A. K. The world report on ageing and health. Gerontologist 56(Suppl 2), S163–166 (2016).
Cesari, M. et al. Evidence for the domains supporting the construct of intrinsic capacity. J. Gerontol. Ser. A. 73(12), 1653–1660 (2018).
Integrated Care for Older People: Guidelines on Community-Level Interventions to Manage Declines in Intrinsic Capacity.; (2017).
Ma, L. et al. Plasma N-Terminal Pro-B-Type natriuretic peptide is associated with intrinsic capacity decline in an older population. J. Nutr. Health Aging. 25(2), 271–277 (2021).
Ma, L. et al. Cross-sectional study examining the status of intrinsic capacity decline in community-dwelling older adults in China: prevalence, associated factors and implications for clinical care. BMJ Open. 11(1), e043062 (2021).
Zhao, J. et al. Intrinsic capacity vs. multimorbidity: a function-centered construct predicts disability better than a disease-Based approach in a community-dwelling older population cohort. Front. Med. 8, 753295 (2021).
Gutiérrez-Robledo, L. M., García-Chanes, R. E. & Pérez-Zepeda, M. U. Screening intrinsic capacity and its epidemiological characterization: a secondary analysis of the Mexican health and aging study. Rev. Panam. Salud Publica Pan Am. J. Public. Health 45, e121 (2021).
Ma, L. et al. Integrated care for older people screening tool for measuring intrinsic capacity: preliminary findings from ICOPE pilot in China. Front. Med. 7, 576079 (2020).
Zhang, J. et al. Relationship between decline of intrinsic capacity and activity of daily living of elderly patients. Chin. J. Mod. Nurs. 26(32), 4466–4469 (2020).
Merchant, R. A., Chan, Y. H., Anbarasan, D. & Vellas, B. Association of intrinsic capacity with functional ability, sarcopenia and systemic inflammation in pre-frail older adults. Front. Med. 11, 1374197 (2024).
Zhang, S. et al. Comparative analysis of intrinsic capacity impairments, determinants, and clinical consequences in older Community-Dwellers in Japan and Taiwan: longitudinal studies showing shared traits and distinct presentations. J. Nutr. Health Aging. 27(11), 1038–1046 (2023).
Lu, W. H. et al. Plasma inflammation-related biomarkers are associated with intrinsic capacity in community-dwelling older adults. J. Cachexia Sarcopenia Muscle 14(2), 930–939 (2023).
Lu, W. H. et al. Association between aging-related biomarkers and longitudinal trajectories of intrinsic capacity in older adults. GeroScience 45(6), 3409–3418 (2023).
Wei, X. et al. Factors associated with the intrinsic capacity in older adults: a scoping review. J. Clin. Nurs. 33(5), 1739–1750 (2024).
Huang, Z. T., Lai, E. T. C., Luo, Y. & Woo, J. Social determinants of intrinsic capacity: a systematic review of observational studies. Ageing Res. Rev. 95, 102239 (2024).
Yu, J. et al. How does social support interact with intrinsic capacity to affect the trajectory of functional ability among older adults? Findings of a population-based longitudinal study. Maturitas 171, 33–39 (2023).
Su, H., Xu, L., Yu, H., Zhou, Y. & Li, Y. Social isolation and intrinsic capacity among left-behind older adults in rural China: the chain mediating effect of perceived stress and health-promoting behavior. Front. Public. Health (2024).
Folstein, M. F., Folstein, S. E. & McHugh, P. R. Mini-Mental State Examination: MMSE-2 (2010).
Zhou, X. A Preliminary Study on the Reliability and Validity of the Chinese Version of the Simple Intelligent Mental State Examination Scale in Stroke Patients (Fujian University of Chinese Medicine, 2015).
Guralnik, J. M. et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J. Gerontol. 49(2), M85–94 (1994).
Spitzer, R. L., Kroenke, K. & Williams, J. B. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary care evaluation of mental disorders. Patient Health Questionnaire JAMA. 282(18), 1737–1744 (1999).
Rubenstein, L. Z., Harker, J. O., Salvà, A., Guigoz, Y. & Vellas, B. Screening for undernutrition in geriatric practice: developing the short-form mini-nutritional assessment (MNA-SF). J. Gerontol. Biol. Sci. Med. Sci. 56(6), M366–372 (2001).
Glasgow, R. E., Strycker, L. A., Toobert, D. J. & Eakin, E. A social-ecologic approach to assessing support for disease self-management: the chronic illness resources survey. J. Behav. Med. 23(6), 559–583 (2000).
Charlson, M. E., Pompei, P., Ales, K. L. & MacKenzie, C. R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J. Chronic Dis. 40(5), 373–383 (1987).
Rico, C. L. V. et al. Factors associated with the deterioration of intrinsic capacity in older people in Mexico and Colombia. Ann. Geriatr. Med. Res. (2024).
Hernandes, E. C. R., Aliberti, M. J. R., Guerra, R. O., Ferriolli, E. & Perracini, M. R. Intrinsic capacity and hospitalization among older adults: a nationally representative cross-sectional study. Eur. Geriatr. Med. (2024).
Ramírez-Vélez, R. et al. Association of intrinsic capacity with incidence and mortality of cardiovascular disease: prospective study in UK biobank. J. Cachexia Sarcopenia Muscle (2023).
Meng, T. & Ren, Y. Psychological heart disease management and maintenance of intrinsic competence in the elderly. J. Chronic Dis. 23(09), 1290–1292 (2022).
Li, M., Lin, Y. & Xing, K. Relationship between intrinsic ability and prognosis in elderly patients with acute coronary syndrome. J. Navy Med. 42(5), 583–587 (2021).
Li, X. & Ma, L. From biological aging to functional decline: insights into chronic inflammation and intrinsic capacity. Ageing Res. Rev. 93, 102175 (2024).
Du, X. et al. Soluble suppression of tumorigenicity 2 associated with microvascular obstruction in patients with ST-segment elevation myocardial infarction. BMC Cardiovasc. Disord. 24(1), 691 (2024).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. Projects Support: (1) A social network study of Health information-seeking and communication behavior in patients with coronary heart disease (Zhejiang medical and Health Science and Technology program Medical Science and Technology Project of Zhejiang Province, project number: 2022KY838); (2) Research on the application of acupoint patch combined with gain-framed message in patients with kinesiophobia after PCI with liver-qi stagnation (Zhejiang Province Traditional Chinese Medicine Science and Technology Project of Zhejiang Provincial Health Commission, project number: 2024ZL584).
Author information
Authors and Affiliations
Contributions
(1) Yuan Zhao: Conceptualization (Lead), Data curation (Lead), Formal analysis (Lead), Investigation (Lead), Methodology (Lead), Software (Lead), Visualization (Lead), Writing-original draft (Lead); (2) Yueying Jiang: Conceptualization (Supporting), Data curation (Supporting), Investigation (Supporting), Methodology (Supporting), Resources (Supporting), Software (Supporting), Visualization (Supporting); (3) Qunyan Xu: Conceptualization (Supporting), Data curation (Supporting), Methodology (Supporting); (4) Dandan Chen: Conceptualization (Supporting), Formal analysis (Supporting), Software (Supporting); (5) Panpan Tang: Formal analysis (Supporting), Validation (Supporting); (6) Xueqing Wang: Methodology (Supporting), Software (Supporting); (7) Yunyu Guo: Methodology (Supporting), Software (Supporting); (8) Chang Liu: Methodology (Supporting), Software (Supporting); (9) Xiuqin Feng*: Formal analysis (Supporting), Resources (Lead), Supervision (Equal), Supervision (Equal), Validation (Supporting), Writing-review & editing (Equal); (10) Leiwen Tang*: Conceptualization (Supporting), Methodology (Supporting), Project administration (Lead), Supervision (Equal), Validation (Supporting), Writing-review & editing (Equal);
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhao, Y., Jiang, Y., Xu, Q. et al. Implications of intrinsic capacity subtypes for post-PCI patients older than 45. Sci Rep 15, 11728 (2025). https://doi.org/10.1038/s41598-025-94485-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-94485-1