Abstract
Spontaneous blinking is a rapid and unconscious type of blinking that has been linked to several cognitive processes. Blink rate has been established as a reliable measure of cognitive processing and a predictor of dopamine-related cognitive function. Patients with Parkinson’s disease (PD) have a reduced spontaneous blink rate. In this study, we propose an additional measure of blink characteristic, namely blink duration, and evaluate its alteration in a large cohort of 107 patients with PD. We also investigate the relationship between blink rate and blink duration and disease characteristics such as severity and dopaminergic neuronal loss. The results show that the blink rate is reduced, and blink duration is increased in patients compared to healthy controls. Blink rate is related to motor deficit severity and significantly correlated with dopamine depletion (dopamine transporter striatal binding ratio). Conversely, blink duration is related to non-motor aspects such as sleepiness. These findings highlight the potential of blink as a distinguishing feature of Parkinson’s disease, underscoring the importance of incorporating blink assessments into standardized oculomotor testing protocols for PD.
Similar content being viewed by others
Introduction
Blinking, the brief and simultaneous closing of both eyes, can serve as a valuable cognitive marker in various contexts1,2,3,4,5,6,7,8. The blinking act can be categorized into three types: spontaneous blink, which occurs independently of any stimulus; reflex blink, triggered by external stimulation, such as an air puff; and voluntary blink, performed intentionally. Spontaneous blinking can be quantitatively analyzed using blink rate (BR) and blink duration (BD). Blink rate refers to the frequency of blinking without external triggers and blink duration is the length of time for which the eyelids remain closed. Blinking is modulated by changes in cognitive load across various tasks9,10,11,12. Engaging in cognitively demanding processes such as speaking, reading, watching a video, or exercising has been shown to alter spontaneous blink rate in healthy individuals13,14,15. While it reduced with reading and while watching video, the blink rate increased during conversation and speech. Blink rate has also been found to be related to working memory16,17,18 and attentional demand in several studies19,20,21. Task manipulating attentional load using the Mackworth Clock Test showed an inverse relationship between blink rate and task difficulty19, where the high attentional load was accompanied by decreased blink rates. Tasks demanding regulation of working memory have shown an increase in blink rates and an association between working memory performance and blink rates16,17,18. In summary, increased demand for visual attention lowers the spontaneous eye blink rates while engagement of working memory is reflected as increased blinking. These findings indicate that blink rate serves as a well-studied marker of cognitive processes22,23,24. Research on blink duration has been less extensive compared to blink rate. Blink duration has been suggested to be influenced by cognitive control mechanisms involving attention and sensory information processing22,25,26,27,28. Some studies showed that blink duration decreases with increased workload, for example, during driving and to be more sensitive to visual cognitive demands29. Thus, it may be an alternative measure for assessing spontaneous blinking.
Several studies have suggested that spontaneous blinking is linked to dopamine activity in humans and non-human primates, although the exact physiology is not fully elucidated. In Parkinson’s disease (PD), alterations in spontaneous blinking have been observed. A study of spontaneous blink rate in non-human primate models with neurotoxin MPTP (1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine)-induced parkinsonism found a negative correlation between the severity of parkinsonism and blink rate30. Many studies have also reported reduced blink rates in PD patients compared to healthy individuals31,32,33 with more severe patients exhibiting lower blink rate34. In contrast, another case–control study of 20 PD patients reported a weak and non-significant correlation between reduced blink rate and PD duration as well as no correlation between blink rate and disease severity (Hoehn and Yahr score)35. Thus, there is a need for further research, to clarify these inconsistencies. Although blink rate has been studied in PD, blink duration has not yet been investigated as a marker of the disease despite its potential as a proxy for cognitive abilities such as attention in healthy subjects29,36. The relationships between PD motor and non-motor features, blink rate, and blink duration also remain to be explored.
Finally, in most studies investigating blinking in clinical conditions like PD, the blink rate has been manually assessed by counting patients’ blinks, either in real time or from video recordings. However, it is possible to automate blink rate assessment using electromyography, electrooculogram, or eye/eyelid trackers37,38,39,40,41. There is a lack of objective and quantitative approaches to studying blinks in PD. Our study aims to quantify eye-tracking data collected during an oculomotor test in a large cohort of early PD patients to determine the significance of an automated blink analysis in the clinical assessment of the disease. We have quantified blink rate and duration in PD patients, compared them with those of age-matched healthy controls, and tested their relation to disease severity, dopaminergic denervation (DaTscan), and non-motor symptoms. We hypothesize that blink rate and blink duration may reflect different aspects of brain dysfunctions and may be used as diagnostic or prognostic markers for disease severity.
Methods
Participants
All participants in this study were recruited in a monocentric prospective longitudinal research cohort (ICEBERG study ClinicalTrials.gov Identifier: NCT02305147) at the Paris Brain Institute. For further details on this cohort relevant to the present study, please refer to Biondetti et al.42. The local ethics committee approved the study (CPP Paris VI, RCB: 2014-A00725-42). All subjects gave written informed consent, and the research was performed in accordance with the Declaration of Helsinki. Inclusion criteria involved a PD clinical diagnosis (UK Brain Bank criteria) by sleep neurologists or movement disorder specialists, age between 18 and 75, no or subtle cognitive impairment (Mini-Mental State Examination score > 26/30), and a time-from-diagnosis ≤ 4 years.
Clinical assessment
PD patients underwent a standardized clinical assessment involving the Movement Disorder Society Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) with part III in the ON condition and the OFF condition (which evaluates motor disability 12 h after withdrawing dopaminergic treatment); the Mattis Dementia Rating Scale (MDRS), the Montreal Cognitive Assessment score (MoCA) (which evaluate cognitive impairment) and the Epworth scale (ESS) (to evaluate daytime sleepiness). Oculomotor tests were performed at each visit in dopamine-ON condition. Age-matched healthy control individuals (HC, referred to as Controls in figures) had no neurological or psychiatric disease history. They also underwent clinical examination, oculomotor testing, and MRI examination. The PD patients were also recruited for a follow-up visit (V1) ~ 25 months after their first visit (V0) and this data was used for a longitudinal analysis.
Oculomotor test setup
During the experiment, the participants were seated in a dark room with their eyes open facing a 26-inch LCD screen (ProLite, Iiyama model PL 2600, visual angle 56° × 35°) positioned at 60 cm. The display presented the stimulus during the experiment at a resolution of 1920 pixels × 1080 pixels and a refresh rate of 144 Hz. Data were collected using a remote video-based eye tracker (Mobile EBT©, eyeBRAIN, France, sampling rate 500 Hz). A standard 9-point calibration was carried out before the start of the task in which the participant had to fixate on a 0.5° red target for 250 ms each. The eye tracker gives a very high accuracy of 0.25° to 0.5° with noise in recording calculated from the baseline data being less than 0.5°. The task control was done using MeyeParadigm software, and the collected data were then extracted using MeyeAnalysis 1.20.1 software.
Oculomotor task design
Participants were asked to perform a reflexive saccade task which is a standard paradigm used to study oculomotor control43. The paradigm started with a central green fixation point (FP) (size: 15 × 15 pixels; luminance: 120 cd/m2) displayed at the center of the screen on a black background for a fixation period (jittered in the range 2500–3500 ms). After the FP disappeared, a red target (the same size as the FP) appeared after 200 ms at an eccentricity of 25° to the right or left of the FP along the horizontal axis. The target position (right or left) was randomized uniformly. The target was displayed for 1000 ms and the participants had to immediately respond by making an eye movement to the target. Once the participant’s eye reached the target, the red target disappeared and the central white fixation for the next trial appeared. Each participant completed either two blocks (24 target appearances) or four blocks (12 target appearances) of horizontal saccades, resulting in 48 saccades performed. Participants were unaware of the study of blinking during eye movement recordings and were not instructed anything regarding blinking timing. They were only instructed to make quick eye movements to red targets as soon as they appeared and remain fixated on the central green box at all other times.
Data analysis
Oculomotor data analyses were performed using Matlab (R2023a version, the MathWorks, MA, USA), and statistical analyses were conducted on Matlab and GraphPad Prism version 9.5.0 software (macOS, GraphPad Software, San Diego, California USA, www.graphpad.com).
Eyeblink detection
Blinks were detected using custom algorithms written in Matlab which involved the following steps. The eye tracking camera provided horizontal and vertical eye displacement data that was smoothened and baseline corrected by subtracting the mean of 500 samples (from 500 to 1000 bins) at the start of the block. This data was then used to calculate the angular displacement as \(\theta = \sqrt {x^{2} + y^{2} }\), (with x the horizontal and y the vertical displacements), and then smoothed using a Savitzky Golay filter (order = 3, frame length = 71) as it preserves the essential features of the data, such as peaks and overall trends, while reducing noise. This denoising of the data is important for the next steps of peak detections used for blink detection. Filtered angular displacement data were checked to detect all peaks with a height of at least one-third of the highest peak in the session, above its baseline noise value, to avoid detecting the saccade peaks. Distinct peaks with high prominence and peak width between 160 and 400 ms of duration were considered spontaneous blinks. Blinks occurring within the first 1000 ms of the session start and the last 400 ms were excluded to stabilize performance and avoid unnecessary artifacts. We also specifically only included blinks occurring during fixation. The blinks riding on the saccades were excluded. A quality check of the blink detection was carried out through visual inspection of the eye recording for each session. After visual inspection of all blink detections, those with a high percentage of under or overestimation (~ 18.6%) of a few blinks (due to noisy data) were excluded. This resulted in a 20% data loss from the entire dataset (640 sessions).
Further, the blink parameters of blink rate per minute and blink duration were calculated. The number of blinks in the whole block was counted and divided by the length of the block in minutes to get the blink rate for each block. The mean blink rate for each subject was quantified as the average across the multiple blocks they performed. To calculate the blink duration, we looked at the angular velocity of the data around the time points at which a blink peak was detected (in angular displacement) as described above. This allowed us to avoid mixing saccade peaks with blinks. Before the blink peak and after the blink peak, we defined 400 ms as the blink regions. In each blink region, when the velocity values decreased below the baseline noise (which is defined as the values below 10% of the blink region’s velocity lies), before and after the blink peak, we marked the start and end of the blink respectively. The blink duration was quantified as the difference between the time of the end and the time of the start of the blinks. The blink parameters of blink rate and blink duration were used for all further analysis.
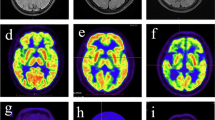
DaTscan analysis
A description of DaT-specific binding ratios (SBRs) calculation has been detailed in Villain et al. (2021 70). Briefly, the DaTscanTM image was first aligned to the corresponding T1-weighted anatomical MRI and corrected for partial volume effect using 3 compartments (high, intermediate, and low dopaminergic density levels). SBR values were obtained by normalizing the DaTscan signal intensity to a reference region of interest (occipital lobe). Basal ganglia regions of interest were identified using the T1-weighted anatomical MR segmentation (nucleus accumbens, putamen, caudate nucleus). The average DaT-SBR for left and right together was then calculated in each striatal region of interest.
Statistical tests
Normality assumptions for the variables blink rate and blink duration were assessed using the Shapiro–Wilk test, revealing non-normal distributions. Hence, we used Spearman’s nonparametric correlation to calculate the correlation coefficient (ρ) and p values (P) (shown in the inset in the Figures). Differences between groups were assessed using the Mann–Whitney U test/Student t-test for non-parametric/parametric cases respectively. The tests used also accounted for the fact that the sample size of healthy controls was less than half of the PD group. In the case of comparisons between dependent observations of V0 and V1, a Wilcoxon signed rank test was used. Statistical analyses were conducted with significance levels set at α = 0.05, using GraphPad Prism. Due to the high interdependence of measures involved in the correlations (correlation coefficients greater than 0.5), standard multiple comparison corrections (e.g., Bonferroni or FDR) are not straightforward or suitable, as these methods assume independence or a low degree of correlation between tests. Hence to avoid the risk of spurious findings, we did a k-leave-out permutation analysis (10,000 permutations, set to k = 10) in the significant correlation analyses and re-confirmed the results. Additionally, the prediction power of blink features to various clinical measures was tested using stepwise linear regression (stepwiselm) and confirmed with robust linear regression (robustfit) along with permutation test (n = 10,000). The figures show significance levels of statistical tests by asterisks, where one asterisk (*) signifies P < 0.05, two asterisks (**) signify P < 0.01, three asterisks (***) signify P < 0.001, and four asterisks (****) denote extremely low P values, typically less than 0.0001, indicating a very high level of statistical significance.
Results
107 PD patients and 48 HC underwent oculomotor testing. Demographic and clinical data are displayed in Table 1 for controls and PD for both V0 and V1 visits. The averages and standard deviations of all scores relevant to this study are presented. None of the confounding variables of age, MMSE, MOCA, MDRS, FAB, or ESS were significantly different between the PD patients and healthy controls (Wilcoxon rank-sum test, all P values greater than Bonferroni corrected P = 0.008).
Baseline comparisons of blink features between PD patients and HC
The blink rate of PD patients (15.28 ± 8.92 blinks per minute) was significantly lower compared to the HC group (19.30 ± 17.06 blinks per minute) (Mann–Whitney test, two-tailed, P < 0.0001, U = 1459) (Fig. 1A). Blink duration was significantly longer in the PD group, 63.25 ± 15.74 ms compared to 55.05 ± 8.10 ms in the HC group (Mann Whitney test, two-tailed, P < 0.001, U = 1567 Fig. 1B). A significant negative correlation between blink rate and duration was only observed in the PD group (Spearman ρ = − 0.21, CI − 0.40 to − 0.01, P = 0.03; Fig. 1C), not in the HC group (Spearman ρ = 0.01, CI − 0.28 to 0.30, P = 0.92; Fig. 1D).
Distributions of blink features between HC and PD patients. (A) Blink rate comparison. The line at the center shows the mean. (B) Blink duration comparison. The x-axis presents two groups, and the y-axis is the blink duration in milliseconds. Each dot is the mean blink duration for each subject over the multiple blocks. The line at the center shows the mean. (C) Blink rate and blink duration correlation in PD. Each dot represents the value for a participant. The red robust regression line (β = − 0.37, P = 0.017) is significant. (D) Blink rate and blink duration correlation in controls. As in (C), each dot is data for an individual participant. The red robust regression line is not significant (β = − 0.02, P = 0.83).
Longitudinal changes of BR and BD over time
To test if these blink features evolved over the progression of the disease, we compared the data from 71 PD patients who made a follow-up visit (V1). At the follow-up visit V1, the blink rate was significantly lower (Mann Whitney test, two-tailed, P < 0.001, U = 904) and blink duration was significantly longer in PD than in HC (Mann Whitney test, two-tailed, P = 0.01, U = 1191). However, neither the blink rate (Wilcoxon signed-rank test, two-tailed, P = 0.32, zval = 0.99, signed rank = 1452) nor the blink duration (Wilcoxon signed-rank test, two-tailed, P = 0.23, zval = − 1.19, signed rank = 1071) showed any significant difference between the visits.
Relationship of blink features to disease severity
We found a negative correlation (Spearman ρ = − 0.25, CI − 0.42 to − 0.05, P = 0.01) within the PD group between blink rate and UPDRS III OFF scores (Fig. 2C, red markers).
Correlations between blink features and disease severity scores. Each point is data for an individual participant. The red is the robust linear regression line (none of them are significant). (A) Blink rate versus UPDRS-I score: The x-axis is the UPDRS-I score, and the y-axis is the blink rate per minute. Each subject’s average blink rate over the blocks is shown using a filled black circular marker. The inset shows the Spearman correlation value (ρ) and P value. (B) Blink rate versus UPDRS-I score: The x-axis is UPDRS-II scores, and the y-axis is blink rate. The other figure conventions are the same as (A). (C) Blink rate versus UPDRS-III score: The x-axis is UPDRS-II scores, and the y-axis is blink rate. Each dot represents the value of a subject. Green markers are for dopamine medication-ON condition, and red markers are for dopamine medication-OFF condition. (D) Blink duration versus UPDRS-I score: The x-axis is UPDRS-I scores, and the y-axis is blink duration in milliseconds. The other figure conventions are the same as (A). (E) Blink duration versus UPDRS-II score: The x-axis is UPDRS-II scores, and the y-axis is blink duration. The other figure conventions are the same as (A). (F) Blink duration versus UPDRS-III score: The x-axis is UPDRS-III scores, and the y-axis is blink duration. Other figure conventions are the same as (C).
On medication, we found no significance but a trend regarding a negative correlation between blink rate and UPDRS III ON score (Spearman ρ = − 0.18, CI − 0.37 to 0.03, P = 0.08, Fig. 2C, green markers). Blink rate was also correlated to UPDRS II (Spearman ρ = − 0.20, CI − 0.38 to 0.006, P = 0.04) (Fig. 2B) but not to UPDRS I score (Spearman ρ = 0.06268, CI − 0.13 to 0.26, P = 0.52) (Fig. 2A). Blink duration was correlated to the UPDRS II score (Spearman ρ = 0.25, CI 0.06–0.43, P = 0.008, Fig. 2E), but not to UPDRS I (Spearman ρ = 0.01, CI − 0.18 to 0.21, P = 0.88, Fig. 2D) scores or UPDRS III scores ON (Spearman ρ = 0.17, CI − 0.037 to 0.37, P = 0.10, Fig. 2F, green markers) or OFF medication (Spearman ρ = 0.12, CI − 0.08 to 0.31, P = 0.21, Fig. 2F, red markers). UPDRS IV scores were zero for all patients but four and were not included in this analysis. We did not find any significant correlation between blink rate and age (Spearman ρ = − 0.02, CI − 0.21 to 0.18, P = 0.86) or disease duration (Spearman ρ = − 0.07, CI − 0.27 to 0.13, P = 0.47) in PD group.
For all UPDRS scores, we ran a stepwise linear regression model to check the predictive power of blink features on these scores. Only for UPDRS II, the regression resulted in a model with BIC = 594.06 when the blink rate was removed, and blink duration remained a significant predictor (P = 0.0016). This result was confirmed by a robust linear regression model. The blink duration and UPDRS II show a small but statistically significant positive correlation (β = 0.067, P = 0.013), while the blink rate did not show any significance (β = − 0.065, P = 0.18). The permutation testing (n = 10,000) confirmed the significance of blink duration to be not spurious (P = 0.011) while BR was confirmed to be not predictive of UPDRS II (P = 0.20). This result aligns with the strong correlations observed between blink duration and UPDRS II scores. The statistical results of the other UPDRS score prediction analysis are presented in the supplementary material (section B. UPDRS scores and blink feature regression models).
There was no significant correlation between blink duration and age (Spearman ρ = − 0.13, CI − 0.32 to 0.07, P = 0.19) or disease duration (Spearman ρ = 0.15, CI − 0.04 to 0.34, P = 0.11) as well in PD. Even with HC, no correlation was observed between blink features and age. The significant correlations were tested using a 10-leave-out permutation test (n = 10,000) and the observed correlations were confirmed not to be an extreme case (permutation P values for all cases were greater than 0.4). The blink features were not dependent on the dopaminergic treatment as neither blink rate nor duration correlated with the Levodopa equivalent dose (LED). Motor dopa-sensitivity, which quantifies the improvement of the UPDRS III score after levodopa intake, was not correlated with blink rate and duration.
Relationship of blink features to dopaminergic denervation
Correlations between blink features (blink rate and duration) and DaTscan SBR were performed in the PD group, across the different striatal regions of interest: the entire putamen, caudate, and nucleus accumbens.
A significant correlation was observed between blink rate and SBR in bilateral putamen (Spearman ρ = 0.27, CI 0.00–0.51, P = 0.04; Fig. 3A) but not in bilateral caudate nucleus or accumbens (Fig. 3B,C). There was no correlation between blink duration and SBR (Fig. 3D–F). Additionally, we also found that neither BR nor BD values were able to predict the SBR values (details presented in supplementary material section B. DaTscan SBR and blink feature regression model). Hence, the significant correlations were again tested using a 10-leave-out permutation test (n = 10,000). The permutation P values for all cases were greater than 0.4, confirming that observed correlations were not an extreme case. These findings suggest that while the variability in blink features limits their predictive power for DaTscan SBR, the observed correlation between blink rate and putamen SBR remains robust, highlighting a consistent association despite the lack of predictive strength.
Correlation of blink features with DaTScan SBR. Each black dot is the value for each participant. The linear regression line is shown in red (none of the regressions were significant). The inset shows the Spearman correlation value (ρ) and P value. The figure conventions are the same for all subplots. (A) Putamen SBR and blink rate. (B) Accumbens SBR and blink rate. (C) Caudate SBR and blink rate. (D) Putamen SBR and blink duration. (E) Accumbens SBR and blink duration. (F) Caudate SBR and blink duration.
Blink features and non-motor features of PD
In the PD group, there was no significant correlation between blink rate or blink duration and cognitive alteration (MDRS). Neither the total score nor the attention, conception, or initiation subtest scores showed any correlation to blink features. We did not find any correlation between MOCA or its sub-scores and blink features.
Blink duration significantly correlated with Epworth Sleepiness Score (ESS) in PD patients (Spearman ρ = − 0.248, CI 0.46–0.43, P = 0.014; Fig. 4A), while blink rate did not (Spearman ρ = − 0.108, CI − 0.30 to 0.09, P = 0.282; Fig. 4B). This correlation was absent for both blink rate and duration in healthy controls. We also tested if blink features have a predictive power on the ESS scores. However, no significance was obtained with robust linear regression with BR: (β = − 0.04, P = 0.43) or BD (β = 0.01, P = 0.64) and permutation test (n = 10,000) with BR (P = 0.43) as well as BD (P = 0.64).
Blink features and ESS. (A) Blink rate and Epworth Score. Each data point represents the data of a participant in black circular markers. The unfilled markers are outliers (values that were outside three standard deviations of the data distribution) and were excluded from correlation calculations. The P value is defined as the values that were outside 3 standard deviations of the blink rate and blink duration distributions and the Spearman correlation is shown in the inset square box on the top right of each subplot. The red line shows a linear regression line on the data (none are significant). (B) Blink duration and Epworth Score. The conventions of the plot remain the same as (A).
Discussions
In this study of early PD, we observed significant changes in blink rate and duration within the 4 years following the clinical diagnosis. PD showcased a significantly lower blink rate and significantly longer blink duration than HC. These results suggest that blink characteristics may be a distinguishing feature indicative of pathology in PD. It was very close to values observed by Biousse et al.32 and Fitzpatrick et al.35 in their studies of 17.1 ± 12.7 blinks/min (n = 30) and 18 blink/min (n = 20) respectively. However, the mean blink rate was very high compared to the values of 5.8 ± 1.4 which is reported in44, which may probably be due to the disease progression differences between the cohorts. Hence, similar to the analysis reported by45 for the OFF state, we classified our ON-state mean blink rates into low blink rate (LBR, < 15 blinks/min) and high blink rate (HBR, > 15 blinks/min). We observed that only 20% of our 107 patients presented LBR. On the other hand, there are no studies that have measured blink durations in PD patients and hence further studies will be needed to benchmark how variable this measure is across cohorts.
Blink features as a biomarker of PD
Both blink features of blink rate and blink duration were also correlated and predictive of UPDRS II, suggesting that they are reflective of the general disease-related loss of functional independence to carry out activities of daily life, which is not specific to the motor or non-motor aspects. Importantly, the blink rate was correlated with UPDRS-III off score but not with cognitive tests, suggesting a specific link between blink rate and motor disability and not cognitive or attentional deficits. Blink rate was also found to be exclusively sensitive to alterations in the PD motor network (putamen) independent of associative or limbic networks. Interestingly, blink duration was correlated with the Epworth Sleepiness Scale. The ESS is used to assess excessive daytime sleepiness and has been linked to lower cognitive function in PD patients46,47. Hence, the positive correlation between blink duration and ESS suggests that blink duration could be a potential marker of non-motor alterations in PD. Additionally, a correlation between blink rate and blink duration was observed only in the PD group. These results put together suggest that blink duration may be reflecting a more generic aspect of the pathology possibly related to non-motor aspects, while blink rate may be explicitly related to motor impairment. Overall, understanding the blink abnormalities may offer valuable markers of disease prognosis and potentially aid in early diagnosis and intervention. However, the lack of predictive power of blink features (taken from a saccade task) towards any of the clinical measures in our study suggests that a standardized blink assessment is incorporated into oculomotor test batteries, and this may be combined with other clinical measures for effective diagnosis of PD.
Purpose of blinks
Blinking serves multiple purposes beyond ocular lubrication and avoiding fatigue of the eyes. These purposes include information processing, attention modulation, and cognitive function. Studies suggest that high blinking may indicate attentional disengagement (the process of shifting attention away from one focus to another) allowing focus on goal-relevant information48. If so, our observation of decreased blink rate and increased blink duration may suggest an alteration in attentional levels in patients. However, we did not find any correlation of the blink features in sub-scores of MOCA that specifically evaluated attention such as digit span and serial subtraction task. It is also interesting to note that blink patterns are suggested to be strategically executed22,23,49,50 and have been associated with various types of workload such as cognitive load which increases when tasks require attention and memory (reciting a sequence of numbers or performing mental arithmetic51), the motor load which increases with tasks involving fine motor skills (blinking while driving52 or speaking53) and visual load which increases with higher visual attention requirements (blinking while tracking moving objects or reading text14). These studies suggest that blinking may be reflecting the information processing in the brain. However, we did not observe any correlation between the blink features with Stroop test scores, which measure cognitive flexibility and processing speed in patients. It will still be interesting to investigate in future studies if blinking may be another additional marker of attention and cognitive processes which is different from MOCA and other tests providing additional insight in cognitive processes with disease progression.
Blink neurophysiology and its relevance
Blink rate is regulated by a neural system that originates in the paramedian pontine reticular formation (PPRF), is facilitated by the substantia nigra and superior colliculus, and inhibited by regions including the cerebellum and occipital cortex54,55, while the role of thalamus remains to be clarified56. Given the possible involvement of several subcortical structures and brainstem regions in blink generation, spontaneous blinking is most likely a multifaceted process involving multiple neurotransmitter systems. Neuropharmacological experiments have suggested dopaminergic, cholinergic, GABAergic, serotonergic, and glutamatergic involvement in blinking23,57,58,59. Dopamine is very closely linked31,60,61. The presence of a correlation between the blink rate and the MDS UPDRS III score OFF- but not on ON-medication confirms that the dopaminergic system is involved in the control of the blink rate. Unlike blink rate, blink duration was not motor-specific and may be driven by other neurotransmitter systems, particularly the cholinergic system involved in inhibitory control. Hence, investigating the role of neurotransmitters in modulating blink features can enhance our understanding of the neurobiological mechanisms underlying disease-related changes.
Several arguments suggest that blink rate are relevant measure of PD pathophysiology and dopamine denervation. First, blink rate was correlated with reduced DaTScan SBR in the putamen which suggests that blink rate may be considered a potential marker of motor network alterations independently of the associative and limbic networks. Interestingly, this result is consistent with our observations that blink rate mostly correlated with clinical motor scores (UPDRS III, II) and not the others. Additionally, regression analysis showed that blink duration could predict UPDRS II scores. Further, blink features did not correlate with age which suggests that they are not age-dependent. Also, previous studies showed that blink rate and duration were not reliable measures of task difficulty (Cho 202071). Thus, put together, although blink features were calculated from a saccade task in this study, they may be still considered a robust measure reflecting PD pathophysiology and not task characteristics.
Behavioral blink features and its measurement
In this study, we presented blink duration, a less explored blink measure, and found that it was a sensitive measure of PD pathology exploring different networks and pathways than those related to blink rate. Blink duration was less variable compared to blink rate across participants (Levene test, P value = 0.026). Apart from blink rate and blink duration, amplitude (range of eyelid movement during a blink), blink velocity (speed of eyelid movement during a blink), and time for opening and closing of eyelids can be quantified. Only a few studies have quantified kinematic measures such as blink magnitude or velocity or eyelid dynamics62,63,64,65,66,67 and establishing the usability of blink kinematics as markers for disease-related changes needs further investigation.
Several factors currently limit progress in the study of blinking. The primary factor is the technical limitations of eye-tracking devices, which are not adapted for accurately capturing blinks. In the past, eyelid position was assessed using devices such as electrooculography or magnetic search coils, it is now more commonly estimated from video recordings of people’s faces. However, in modern video-based eye trackers, blink classification is typically based on the pupil size (PS) signal, where clusters of samples are reported as invalid, or data loss is taken as blinks. It is important to note that the PS signal can have invalid samples for other reasons besides eyelid closure, such as head movements relative to the camera68, looking outside, or toward the edges of the screen69. Moreover, the eyelid position cannot be measured directly from the PS signal, which creates a need for better methods to study different properties of blinks in greater detail. Some eye trackers, such as the Smart Eye Pro, Tobii Pro Spectrum, and Tobii Pro Fusion, output information about the position of the eyelids and/or the distance between the upper and lower eyelids (i.e., the eye openness signal) and some clinical device (Neuroclues) might integrate blink signal measurement itself into the basic system.
Yet another challenge is to develop a generalized algorithm for automatic blink detection, given that there is high intra and inter-subject variability. In our study, we lost about 20% of blink data with our automatic blink detection system. The missing data were due to noise, difficulty for patients to hold their heads steady even with a chin rest, or special scenarios like blinks riding on the starting edge of saccades, which were not picked up. Improving the eye tracking devices with head-mounted trackers, which effectively cancel head movements (Pupil Core eye tracker), is a step forward in overcoming this problem. Establishing standardized blink protocols with different cognitive, motor, and visual loads could also help ensure consistency across studies and facilitate comparison of results.
Further research is needed to validate anatomical substrates and explore underlying mechanisms linking blink features with disease. Studying their progression in relation to the disease and neurotransmitter levels will offer further insights into prognosis and pathophysiology. Standardized blink protocols and novel blink analysis methods that extract kinematic measures will enhance blink assessment sensitivity and specificity and, in the future advanced technology leveraging videographic acquisitions and parametric extractions will make this possible.
Conclusions
In this study, we explored blink features in a large cohort of PD patients. Patients exhibited decreased blink rate and longer blink duration than HC. Our study demonstrates that blink rate and blink duration reflect different aspects of functional deficit in PD. We observed that only blink rate was closely related to motor scores and dopaminergic activity. In contrast, blink duration reflected a generic decline in performance and non-motor aspects such as sleepiness. These findings imply that blinks could be a valuable diagnostic tool in Parkinsonian conditions. Beyond PD, these parameters, observed across various diseases and potential neuropathological conditions, hold promise for studying the progression of diseases and assessing prognosis. Hence, creating and implementing standardized protocols for spontaneous blink assessments in the battery of oculomotor tests for PD may thus be crucial for its management.
Data availability
The data supporting the findings of this study will be shared at the request of the corresponding author.
References
Holland, M. K. Cognitive processes—Role of blinking. J. Learn. Disabil. 9, 290–291 (1976).
Van Bochove, M. E., Van Der Haegen, L., Notebaert, W. & Verguts, T. Blinking predicts enhanced cognitive control. Cogn. Affect. Behav. Neurosci. 13, 346–354 (2013).
Joiner, T. E. et al. Staring down death: Is abnormally slow blink rate a clinically useful indicator of acute suicide risk?. Crisis 37, 212–217 (2016).
Eckstein, M. K., Guerra-Carrillo, B., Miller Singley, A. T. & Bunge, S. A. Beyond eye gaze: What else can eyetracking reveal about cognition and cognitive development?. Dev. Cogn. Neurosci. 25, 69–91 (2017).
Renker, J., Kreutzfeldt, M. & Rinkenauer, G. Eye blinks describing the state of the learner under uncertainty. In Lecture Notes in Computer Science (including Subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics), vol. 11597, 444–454 (LNCS, 2019).
Magliacano, A. et al. Spontaneous eye blinking as a diagnostic marker in prolonged disorders of consciousness. Sci. Rep. 11, 22393 (2021).
Hollander, J. & Huette, S. Extracting blinks from continuous eye-tracking data in a mind wandering paradigm. Conscious. Cogn. 100, 103303 (2022).
Lange, E. B. & Fink, L. K. Eye blinking, musical processing, and subjective states—A methods account. Psychophysiology 60, e14350 (2023).
Boehm-Davis, D. A., Gray, W. D. & Schoelles, M. J. The eye blink as a physiological indicator of cognitive workload. In Proceedings of the XIVth Triennial Congress of the International Ergonomics Association and the 44th Annual Meeting of the Human Factors and Ergonomics Association. Ergonomics New Millenn., vol 44, 116–119 (2000).
Tsai, Y. F., Viirre, E., Strychacz, C., Chase, B. & Jung, T. P. Task performance and eye activity: Predicting behavior relating to cognitive workload. Aviat. Space Environ. Med. 78, B176–B185 (2007).
Magliacano, A., Fiorenza, S., Estraneo, A. & Trojano, L. Eye blink rate increases as a function of cognitive load during an auditory oddball paradigm. Neurosci. Lett. 736, 135293 (2020).
Kuwamizu, R. et al. Spontaneous eye blink rate connects missing link between aerobic fitness and cognition. Med. Sci. Sports Exerc. 53, 1425–1433 (2021).
Karson, C. N. et al. Speaking, thinking, and blinking. Psychiatry Res. 5, 243–246 (1981).
Orchard, L. N. & Stern, J. A. Blinks as an index of cognitive activity during reading. Integr. Physiol. Behav. Sci. 26, 108–116 (1991).
Descroix, E., Świątkowski, W. & Graff, C. blinking while speaking and talking, hearing, and listening: Communication or individual underlying process?. J. Nonverbal Behav. 46, 19–44 (2022).
Rac-Lubashevsky, R., Slagter, H. A. & Kessler, Y. Tracking real-time changes in working memory updating and gating with the event-based eye-blink rate. Sci. Rep. 7, 2547–2547 (2017).
Buitenweg, J. I. V., Murre, J. M. J. & Ridderinkhof, K. R. Spontaneous eye blinks predict executive functioning in seniors. J. Cogn. Enhanc. 5, 468–479 (2021).
Ortega, J., Plaska, C. R., Gomes, B. A. & Ellmore, T. M. Spontaneous eye blink rate during the working memory delay period predicts task accuracy. Front. Psychol. 13, 788231 (2022).
Gavas, R. et al. Blink rate variability: A marker of sustained attention during a visual task. In UbiComp/ISWC 2020 Adjunct—Proceedings of the 2020 ACM International Joint Conference on Pervasive and Ubiquitous Computing and Proceedings of the 2020 ACM International Symposium on Wearable Computers, 450–455 (2020).
Sciaraffa, N. et al. Joint analysis of eye blinks and brain activity to investigate attentional demand during a visual search task. Brain Sci. 11, 562 (2021).
Kim, S. K. et al. The investigation of the relationship between eye blink and visual attention with video clip. J. Biomed. Eng. Res. 35, 99–104 (2014).
Wascher, E., Heppner, H., Möckel, T., Kobald, S. O. & Getzmann, S. Eye-blinks in choice response tasks uncover hidden aspects of information processing. EXCLI J. 14, 1207–1218 (2015).
Paprocki, R. & Lenskiy, A. What do eye-blink rate variability dynamics tell us about cognitive performance?. Front. Hum. Neurosci. 11, 620 (2017).
Vanneste, P. et al. Towards measuring cognitive load through multimodal physiological data. Cogn. Technol. Work 23, 567–585 (2021).
Holland, M. K. & Tarlow, G. Blinking and thinking. Percept. Mot. Skills 41, 503–506 (1975).
Bauer, L. O., Strock, B. D., Goldstein, R., Stern, J. A. & Walrath, L. C. Auditory discrimination and the eyeblink. Psychophysiology 22, 636–641 (1985).
Liu, C. C., Hajra, S. G., Cheung, T. P. L., Song, X. & D’Arcy, R. C. N. Spontaneous blinks activate the precuneus: Characterizing blink-related oscillations using magnetoencephalography. Front. Hum. Neurosci. 11, 489–489 (2017).
Murali, S. & Händel, B. The latency of spontaneous eye blinks marks relevant visual and auditory information processing. J. Vis. 21, 1–12 (2021).
Benedetto, S. et al. Driver workload and eye blink duration. Transp. Res. Part F Traffic Psychol. Behav. 14, 199–208 (2011).
Taylor, J. R. et al. Spontaneous blink rates correlate with dopamine levels in the caudate nucleus of MPTP-treated monkeys. Exp. Neurol. 158, 214–220 (1999).
Karson, C. N. Spontaneous eye-blink rates and dopaminergic systems. Brain 106, 643–653 (1983).
Biousse, V. et al. Ophthalmologic features of Parkinson’s disease. Neurology 62, 177–180 (2004).
Reddy, V. C., Patel, S. V., Hodge, D. O. & Leavitt, J. A. Corneal sensitivity, blink rate, and corneal nerve density in progressive supranuclear palsy and parkinson disease. Cornea 32, 631–635 (2013).
Karson, C. N., Lewitt, P. A., Calne, D. B. & Wyatt, R. J. Blink rates in parkinsonism. Ann. Neurol. 12, 580–583 (1982).
Fitzpatrick, E., Hohl, N., Silburn, P., O’Gorman, C. & Broadley, S. A. Case-control study of blink rate in Parkinson’s disease under different conditions. J. Neurol. 259, 739–744 (2012).
Ahlstrom, U. & Friedman-Berg, F. J. Using eye movement activity as a correlate of cognitive workload. Int. J. Ind. Ergon. 36, 623–636 (2006).
Kaneko, K. & Sakamoto, K. Spontaneous blinks of Parkinson’s disease patients evaluated by EMG and EOG. Electromyogr. Clin. Neurophysiol. 41, 87–95 (2001).
Kimura, N. et al. Measurement of spontaneous blinks in patients with Parkinson’s disease using a new high-speed blink analysis system. J. Neurol. Sci. 380, 200–204 (2017).
Iwaki, H. et al. Using spontaneous eye-blink rates to predict the motor status of patients with parkinson’s disease. Intern. Med. 58, 1417–1421 (2019).
Maremmani, C. et al. Objective assessment of blinking and facial expressions in Parkinson’s disease using a vertical electro-oculogram and facial surface electromyography. Physiol. Meas. 40, 065005 (2019).
Coe, B. C. et al. Automated analysis pipeline for extracting saccade, pupil, and blink parameters using video-based eye tracking. Vision 8, 14 (2024).
Biondetti, E. et al. The spatiotemporal changes in dopamine, neuromelanin and iron characterizing Parkinson’s disease. Brain 144, 3114–3125 (2021).
Leigh, R. J. & Kennard, C. Using saccades as a research tool in the clinical neurosciences. Brain 127, 460–477 (2004).
Deuschl, G. & Goddemeier, C. Spontaneous and reflex activity of facial muscles in dystonia, Parkinson’s disease, and in normal subjects. J. Neurol. Neurosurg. Psychiatry 64, 320–324 (1998).
Hayashi, S. et al. Increased blink rate in advanced Parkinson’s disease: A form of ’off’-period dystonia?. Mov. Disord. 15, 982–985 (2000).
Jester, D. J., Lee, S., Molinari, V. & Volicer, L. Cognitive deficits in Parkinson’s disease with excessive daytime sleepiness: A systematic review. Aging Ment. Heal. 24, 1769–1780 (2020).
Montanaro, E. et al. Association between sleep disorders and cognitive dysfunctions in non-demented patients with advanced Parkinson’s disease. J. Neurol. 269, 1538–1545 (2022).
Nakano, T., Kato, M., Morito, Y., Itoi, S. & Kitazawa, S. Blink-related momentary activation of the default mode network while viewing videos. Proc. Natl. Acad. Sci. U.S.A. 110, 702–706 (2013).
Shultz, S., Klin, A. & Jones, W. Inhibition of eye blinking reveals subjective perceptions of stimulus salience. Proc. Natl. Acad. Sci. U.S.A. 108, 21270–21275 (2011).
Langbehn, E., Steinicke, F., Lappe, M., Welch, G. F., & Bruder, G. (2018). In the blink of an eye: leveraging blink-induced suppression for imperceptible position and orientation redirection in virtual reality. ACM Transactions on Graphics (TOG), 37(4), 1-11.
Tanaka, Y. & Yamaoka, K. Blink activity and task difficulty. Percept. Mot. Skills 77, 55–66 (1993).
Faure, V., Lobjois, R. & Benguigui, N. The effects of driving environment complexity and dual tasking on drivers’ mental workload and eye blink behavior. Transp. Res. Part F Traffic Psychol. Behav. 40, 78–90 (2016).
Brych, M., Murali, S. & Händel, B. How the motor aspect of speaking influences the blink rate. PLoS ONE 16, e0258322 (2021).
Karson, C. N. Physiology of normal and abnormal blinking. Adv. Neurol. 49, 25–37 (1988).
Karson, C. N. Blinking. Bull. Soc. Belge Ophtalmol. 237, 443–457 (1989).
Chia, L. G. Late blink reflex changes in lesions of thalamus and internal capsule. Neurology 49, 874–876 (1997).
Keifer, J. In vitro eye-blink reflex model: role of excitatory amino acids and labeling of network activity with sulforhodamine. Exp. Brain Res. 97, 239–253 (1993).
Colzato, L. S., Van Den Wildenberg, W. P. M., Van Wouwe, N. C., Pannebakker, M. M. & Hommel, B. Dopamine and inhibitory action control: Evidence from spontaneous eye blink rates. Exp. Brain Res. 196, 467–474 (2009).
Naicker, P., Anoopkumar-Dukie, S., Grant, G. D., Neumann, D. L. & Kavanagh, J. J. Central cholinergic pathway involvement in the regulation of pupil diameter, blink rate and cognitive function. Neuroscience 334, 180–190 (2016).
Jongkees, B. J. & Colzato, L. S. Spontaneous eye blink rate as predictor of dopamine-related cognitive function—A review. Neurosci. Biobehav. Rev. 71, 58–82 (2016).
Maffei, A. & Angrilli, A. Spontaneous eye blink rate: An index of dopaminergic component of sustained attention and fatigue. Int. J. Psychophysiol. 123, 58–63 (2018).
VanderWerf, F., Brassinga, P., Reits, D., Aramideh, M. & Ongerboer de Visser, B. Eyelid movements: Behavioral studies of blinking in humans under different stimulus conditions. J. Neurophysiol. 89, 2784–2796 (2003).
Korošec, M., Zidar, I., Reits, D., Evinger, C. & VanderWerf, F. Eyelid movement during blinking in patients with Parkinson’s disease. Mov. Disord. 21, 1248–1251 (2006).
Bologna, M. et al. Voluntary, spontaneous and reflex blinking in patients with clinically probable progressive supranuclear palsy. Brain 132, 502–510 (2009).
Bologna, M. et al. Blinking in patients with clinically probable multiple system atrophy. Mov. Disord. 29, 415–420 (2014).
Kwon, K. A. et al. High-speed camera characterization of voluntary eye blinking kinematics. J. R. Soc. Interface 10, 1–16 (2013).
Nyström, M., Andersson, R., Niehorster, D. C., Hessels, R. S. & Hooge, I. T. C. What is a blink? Classifying and characterizing blinks in eye openness signals. Behav. Res. Methods 56, 3280–3299 (2024).
Wass, S. V. & Smith, T. J. Individual differences in infant oculomotor behavior during the viewing of complex naturalistic scenes. Infancy 19, 352–384 (2014).
Hessels, R. S., Andersson, R., Hooge, I. T. C., Nyström, M. & Kemner, C. Consequences of eye color, positioning, and head movement for eye-tracking data quality in infant research. Infancy 20, 601–633 (2015).
Villain, N., Béra, G., Habert, MO. et al. Dopamine denervation in the functional territories of the striatum: a new MR and atlas-based 123I-FP-CIT SPECT quantification method. J. Neural Transm. 128, 1841–1852 https://doi.org/10.1007/s00702-021-02434-9 (2021).
Cho, P., Sheng, C., Chan, C., Lee, R., & Tam, J. Baseline blink rates and the effect of visual task difficulty and position of gaze. Current Eye Research, 20(1), 64–70. https://doi.org/10.1076/0271-3683(200001)2011-HFT064 (2000).
Funding
This work was supported by grants from ANR Nucleipark, DHOS-Inserm, France Parkinson, Ecole des NeuroSciences de Paris (ENP), Fondation pour la Recherche Médicale (FRM), and the Investissements d’Avenir, IAIHU-06 (Paris Institute of Neurosciences—IHU), ANR-11-INBS-0006, Fondation d’Entreprise EDF, BIOGEN Inc., Fondation Thérèse and René Planiol, JPND Control-PD (ANR-21-JPW2-0005-05), unrestricted support for Research on Parkinson’s disease from Energipole (M. Mallart) and Société Française de Médecine Esthétique (M Legrand). Emma Biondetti has received funding from the European Union’s Horizon Europe research and innovation program under the Marie Skłodowska-Curie grant agreement No 101066055—acronym HERMES. Views and opinions expressed are, however, those of the author(s) only and do not necessarily reflect those of the European Union or the European Research Executive Agency (REA). Neither the European Union nor the granting authority can be held responsible for them.
Author information
Authors and Affiliations
Contributions
VV: Varsha Vasudevan, QS: Quentin Salardaine, SRP: Sophie Rivaud-Péchoux, EB: Emma Biondetti, NV: Nicolas Villain, SL: Stephane Lehericy, MV: Marie Vidailhet, PP: Pierre Pouget. VV, QS, MV, and PP conceptualized the study. SRP, SL, MV, and PP executed the study and collected the data. VV and QS analyzed the data, prepared figures, and wrote the main manuscript text. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Vasudevan, V., Salardaine, Q., Rivaud-Péchoux, S. et al. Revisiting eye blink in Parkinson’s disease. Sci Rep 15, 10751 (2025). https://doi.org/10.1038/s41598-025-95182-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-95182-9