Abstract
Ischemic stroke is a prominent contributor to cognitive dysfunction and disability. Gaining a comprehensive understanding of the neuronal activity and longitudinal changes underlying stroke is crucial for designing effective rehabilitative strategies. However, the neural mechanisms responsible for the longitudinal reorganization of neuronal activity following stroke remain unclear. The objective of this study was to comprehensively investigate potential abnormalities in brain activity among stroke patients before and after one month of intervention (antiplatelet therapy, as well as intravenous citicoline). To achieve this goal, we combined static and dynamic functional imaging indicators for the comprehensive analysis. Twenty ischemic stroke patients at the subacute stage and seventeen age-matched healthy controls were included in the final analysis of this study from one center. Additionally, resting-state functional magnetic imaging scans were conducted on all patients twice with a one-month interval between scans. Four static intrinsic brain activity indicators (static amplitude of low-frequency fluctuation (sALFF), static fractional amplitude of low-frequency fluctuation (sfALFF), static regional homogeneity (sReHo), and static degree centrality (sDC)), along with their corresponding dynamic indicators, were calculated to detect longitudinal alterations in brain activity following stroke onset. Correlation analyses were also performed between these indicators within areas exhibiting group differences as well as clinical scale scores and disease duration. Significant variations in these static and dynamic image indicators were observed among patients with ischemic stroke. There was substantial overlap among the abnormal brain regions detected, primarily including decreased sALFF/sfALFF/dALFF in the bilateral central precuneus, increased sfALFF/sReHo/sDC/dReHo in the left superior precuneus, increased sALFF/sReHo/dfALFF in the left inferior temporal gyrus, decreased sReHo/sDC in the anterior cingulate cortex, increased sReHo/dfALFF in the right inferior parietal lobe, increased sfALFF/sDC in the right fusiform gyrus, as well as decreased sALFF/dALFF and increased sReHo/sDC in the right angular gyrus. Furthermore, these disrupted image indicators in some regions exhibited only partial recovery at the second time point. The percentage changes of these image indicators (sfALFF in the bilateral central precuneus, sDC in the left fusiform and dALFF in the right central precuneus) between the two time points were positively correlated with the percentage changes of clinical scores (FMA and MBI). In combination, this study demonstrates that a comprehensive understanding of abnormal activity and its longitudinal changes in ischemic stroke can be achieved by integrating static and dynamic imaging methods. Regions showing significant overlap among different brain activity indicators and exhibiting consistent image-behavior relationships may have some potential values for predicting clinical outcomes.
Similar content being viewed by others
Introduction
Stroke is the leading cause of long-term disability in adults worldwide1. Ischemic stroke, being the most prevalent type, often presents with cognitive impairment, particularly affecting language, attention, and motor function. Given the significant morbidity, severe cognitive impairment, and diminished quality of life associated with this condition, it is crucial to fully comprehend the neuropathological mechanisms involved in post-stroke plasticity and reorganization for facilitating clinical work. Additionally, revealing the neural mechanism underlying stroke-induced brain changes is vital for understanding the precise diagnosis and adopting effective treatment. In this regard, functional neuroimaging has made substantial contributions towards unraveling the neural mechanisms underlying post-stroke plasticity and reorganization2,3,4,5,6,7.
Ischemic stroke occurs when there is a lack of blood supply to cerebral tissue due to embolic occlusion of a cerebral artery8. Previous studies have consistently shown that ischemic stroke patients exhibit functional and structural reorganization in perilesional and remote brain regions5,8,9. A consistent finding in stroke is the reduction of interhemispheric connectivity between the primary sensorimotor cortices10,11,12,13. Previous studies on structural and functional connectivity in stroke have confirmed that focal lesions can lead to changes in corresponding sub-networks and affect the efficiency of whole-brain activity14. Changes in patterns of connectivity within and across the hemispheres may be related to cognitive dysfunction and behavioral recovery following stroke. In addition to alterations in brain connectivity, numerous neuroimaging studies have demonstrated abnormal changes in stroke patients, including decreased gray matter volume15, alterations in cerebral activity16,17, changes in static degree centrality (sDC)18, as well as voxel-mirrored homotopic connectivity abnormalities11. These neuroimaging changes may underlie impaired cognitive function and contribute to both the generation of poststroke deficits and recovery processes. However, these previous studies11,15,18 have predominantly focused on a priori selection of specific brain regions or single imaging indices, thereby limiting our understanding of the comprehensive whole-brain and longitudinal changes in stroke, particularly in relation to resting-state functional magnetic resonance imaging (fMRI) investigations. Currently, one of the important trends in stroke research is to study the longitudinal alterations in brain activity and their potential for predicting cognitive performance during the recovery process among ischemic stroke patients19,20.This study also conducted related research on the changes of brain imaging after stroke in this direction.
Considerable advancements in fMRI technology and analysis have significantly enhanced our capacity to evaluate post-stroke brain image alterations more comprehensively. Resting-state fMRI is an emerging functional brain neuroimaging technique that investigates the functional alterations of neural networks without requiring for subjects to perform a demanding task based on blood oxygenation level-dependent signals. This technology has been extensively employed in clinical research due to its potential advantages in capturing pathological changes within the brain21. However, previous studies predominantly relied on measuring inter-regional connectivity (functional connectivity) or intrinsic brain activity (such as static amplitude of low-frequency fluctuation (sALFF), static fractional ALFF (sfALFF), static regional homogeneity (sReHo), sDC). These analyses were all based on the assumption that the functional interactions remained constant during the entire scan duration. Nevertheless, it is well-known that the human brain operates as a dynamic system with millisecond-scale fluctuations22. Therefore, it is plausible to consider the human brain as a self-organizing dynamic entity characterized by co-evolving local activity and functional connectivity. Although these static connectivity and intrinsic activity approaches are simple and convenient, and have successfully identified stroke-related cerebral abnormalities, they overlook temporal properties which reflect the inherent dynamic nature of the brain.
In the last decade, there has been a growing field of study focused on dynamics, which aims to investigate the temporal variability in spontaneous activity and connectivity23,24. A key motivation for the dynamic analyses is that this method can capture uncontrolled but recurring patterns of brain networks and intrinsic activity that cannot be detected by traditional static methods25,26,27,28. For example, Wei et al.28 employed both static and dynamic functional connectivity analyses on acute pontine infarction data, revealing disparities in cerebellar-cerebral connectivity features between patients and normal controls. Decreased temporal variability was observed within a network that remained undetected through static analyses. Similarly, Huang et al.26 reported significant reduction in dynamic functional connectivity during weakly connected states of the salience network, which were not discernible using static approaches. In an extensive literature search encompassing dynamic indicators related to stroke research, most studies have primarily focused on investigating dynamic functional connectivity. Apart from this aspect, researchers are gradually turning their attention towards exploring the dynamic characteristics of local brain activity, such as dynamic ALFF (dALFF), dynamic fALFF (dfALFF), dynamic ReHo (dReHo), and dynamic DC (dDC) in stroke cases25,29,30,31. These local dynamical approaches facilitate exploration into variations in oscillation amplitudes and regional synchronization of spontaneous brain activity, thereby enabling a comprehensive understanding of local activity changes in stroke. However, the above previous studies employing these local indicators were mainly focused on one or two specific measures. To address this issue, integrating various indicators in a single study can provide a more comprehensive understanding of the local activity changes in stroke. Furthermore, considering the effectiveness and complementarity of static and dynamic methods, combining both approaches has emerged as a major trend in stroke research26,28,29, which could reveal more accurate abnormal neuronal activity patterns and shed light on the recovery process after stroke.
As we known, the time after a stroke is often divided into phases. Recovery-related processed post-stroke are time-dependent. The most significant improvements occur in the first few weeks post-stroke2. Improvements of some stroke-induced deficits with medical intervention or training can even be achieved in the chronic phase32. Observing the brain imaging changes before and after treatment would help us understand the alterations of function deficits after stroke. Therefore, the objective of this study was to comprehensively investigate potential abnormalities in whole-brain activity among chronic subcortical stroke patients before and after a one-month medicine intervention. To achieve this goal, we combined static and temporal dynamic characteristics of intrinsic brain activity using multiple indicators including ALFF and fALFF for assessing local activity, ReHo for evaluating local synchronization, and DC for examining whole-brain connectivity. Notably, no prior work has investigated static and dynamic activity changes simultaneously using multiple indicators in the context of stroke research. Additionally, we explored correlations between abnormal activity changes and clinical performance measures as well as disease duration. Leveraging the complementary nature of both static and dynamic methods allowed us to estimate that: (1) patients with stroke exhibit longitudinal variability in regional brain activity; (2) a combination of similar and distinct alterations can be observed among abnormal brain regions identified using various static and dynamic indicators; (3) changes in intrinsic brain activity features are closely associated with clinical impairment during the recovery process.
Materials and methods
Subjects
Twenty-one adults with subcortical stroke were recruited from the Department of Neurology of the First Affiliated Hospital of Chengdu University of Traditional Chinese Medicine in China. Disease duration was defined as the time from the initial onset of stroke to the fMRI scan. Data for one patient were discarded because of head movement during the MRI scan, resulting in 20 patients with stroke (9 females and 11 males, mean age: 65.25 ± 12.31 years) were included for the final analysis. Concurrently, 17 age- and sex-matched healthy controls (HC, 10 females and 7 males, mean age: 64.00 ± 10.64 years) were recruited in the present study. This study was approved by the Ethics Committee of Chengdu University of Traditional Chinese Medicine (no. 2011KL-002), and the research was carried out in accordance with the Declaration of Helsinki. All participants signed informed consent forms prior to the study.
All enrolled participants exhibited unimanual motor deficits resulting from subcortical ischemic lesions. Inclusion criteria for patient selection encompassed: (1) right-handedness before infarction onset, (2) presence exclusively within subcortical regions without concurrent white matter pathology confirmed via structural MRI, (3) a minimum three-week interval between stroke onset and enrollment, (4) absence of comorbid psychiatric or neurological disorders, (5) absence of significant coexisting medical conditions, (6) absence of subsequent cerebral ischemia events post-stroke, and (7) non-participation in any previous experimental therapies prior to enrolling in this investigation. Resting-state fMRI data were collected from all patients at two time points: before and one month after the medicine intervention. Clinical scores were assessed for these patients at both time points. The inclusion criteria for HCs were as follows: (1) right-handedness; (2) age-matched with the stroke patients; (3) no history of neuropsychiatric diseases. All HCs underwent a single scan on the day they were recruited. Detailed information regarding both groups is provided in Table 1 and Supplementary Table 1.
Intervention and clinical assessments
All stroke patients received antiplatelet therapy (75 mg clopidogrel orally once daily and 10 mg Erigeron breviscapus injection), as well as intravenous citicoline (0.5 g daily) to improve clinical outcomes following ischemic stroke. Antiplatelet therapy is the mainstay for the prevention of primary stroke in patients with risk factors and for the prevention of recurrent stroke after transient ischemic attack32. Citicoline is a drug approved for the treatment of acute ischemic stroke. It has been studied for its potential neuroprotective and neuroregenerative effects in the treatment of ischemic stroke33. Each patient underwent drug therapy for one month, during which their neurological function, motor function, and daily living ability were assessed using the nervous functional deficiency scale (NDS), Fugl-Meyer Assessment (FMA), and modified Barthel index (MBI). The NDS assesses consciousness, muscle strength of the upper and lower limbs, and ambulation with scores ranging from 0 to 45; a lower score indicates milder neurological impairments. The FMA evaluates upper and lower limb motor functions after stroke with a maximum score of 100 points; a higher score indicates milder impairments of motor function. The MBI is used to evaluate daily living ability through ten areas of ability evaluation, including feeding, grooming, bathing, and dressing with a maximum score of 85 points; a higher score indicates better daily living ability. A paired t-test was conducted to determine whether there were significant changes in clinical scores between the two time points (p < 0.05, two tailed t-test). The disease durations were also recorded, which were defined as the time between the stroke onset and the first MRI scan.
Image acquisition
The resting-state functional MRI data for the study were acquired using a 3T MR scanner (MAGNETOM Trio Tim, Siemens, Germany) with a standard eight-channel head coil at the West China Hospital MRI Center, Chengdu, China. During the scanning process, participants were instructed to lie quietly with their eyes closed, avoiding sleep, specific thoughts, and any head movement. To avoid the subjects’ falling asleep, a relatively short scan was performed in this study. We also asked about their condition after the scan: such as whether they fell asleep during the scan and whether they felt uncomfortable during the scan. Foam cushions and earplugs were used to minimize head movements and scanner noise. Resting-state fMRI was acquired using echo-planar imaging sequence with the following parameters: repetition time = 2 s; echo time = 30 ms; slice number = 30 interleaved axial slices; slice thickness = 5 mm; flip angle = 90°; field-of-view (FOV) = 240 mm × 240 mm; matrix = 64 × 64; and 180 volumes; The total time for the fMRI acquisition was 6 min. Here, the flip angle of 90° may not be the best parameter. It is recommended to set this parameter as the Ernst angle in future parameter setting. The anatomical three-dimensional T1-weighted structural MRI was recorded by spin-echo planar imaging sequence with the following parameters: repetition time = 1,900 ms; echo time = 2.26 ms; flip angle = 9°; slices number = 176; FOV = 256 mm × 256 mm; in-plane matrix resolution = 256 × 256; and voxel size = 1 × 1 × 1 mm3.
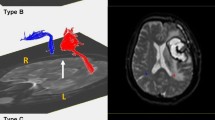
Lesion mapping
The lesion ___location on the T1-weighted MRI images for each patient was determined by an experienced neuroradiologist. We manually delineated the lesion profiles slice by slice using MRIcron software, generating a lesion mask for each patient. The lesion ___location of each subject is listed in supplementary Fig. 1. Subsequently, the lesion masks were normalized to the Montreal Neurological Institute (MNI) space and combined to construct a group lesion map encompassing all patients (refer to Fig. 1). This composite lesion map facilitated visualization of the distribution of lesions across all patients. This group lesion map was used as an exclusion mask to eliminate the brain areas affected by lesions during the following data process of all subjects. To ensure hemispheric consistency, imaging data from two patients with right hemisphere lesions were mirrored along the midsagittal line (flipped from right to left). As a result, the lesions of the patients were mainly located in the left basal ganglia. The image data of two controls were processed in the same manner.
Imaging preprocessing and analysis
The resting-state fMRI data were preprocessed using the Data Processing Assistant for Resting-state fMRI Analysis Toolkit (DPABI, V5.2)34. To minimize the effects of machine instability and participant adaptation to the environment, the first 10 images of each dataset were discarded. The remaining 170 consecutive images underwent slice-timing correction to account for time delays between slices. Subsequently, realignment correction was performed and mean framewise displacement (FD) was calculated to assess head motion. Excessive motion was defined as translation greater than 3 mm or rotation exceeding 3° in any direction. Participants with a mean FD exceeding 0.5 mm or more than 20% of all time points having FD values above this threshold were excluded from analysis. Only one patient was excluded due to excessive motion, while no participants were excluded based on excessive FD criteria. Each participant’s T1-weighted structural image was co-registered with their mean functional image and subsequently segmented. The functional images were then normalized to standard MNI space using T1 image unified segmentation before being resampled at a resolution of 3 mm and detrended linearly in terms of their time series data. Several confounding factors, including head motion parameters, cerebrospinal fluid signals, and white matter signals were regressed out as spurious variances during further analysis steps. Subsequently, functional images were temporally bandpass filtered between 0.01 and 0.1 Hz to reduce the impact of low-frequency drift and high-frequency noise. Lastly, the images were smoothed using a 6 mm full-width half maximum (FWHM) Gaussian kernel for sALFF and sfALFF calculation.
Calculation of sALFF, SfALFF, sReHo, and sDC
The sALFF, sfALFF, sReHo, and sDC were calculated using the Data Processing and Analysis of Brain Imaging (DPABI, V6.0_210501) toolbox35. All of these metrics were calculated based on a brain mask where all the lesioned voxels were excluded. The calculation of sALFF was based on the unfiltered and smoothed preprocessed images. Each time series underwent a fast Fourier transformation to convert it into the frequency ___domain. The square root of the power spectrum was computed in each subject. The average square root across the frequency range of 0.01–0.1 Hz was used to get the sALFF value36. Then, we calculated static sfALFF by obtaining the ratio of the power spectrum in the low frequency range (0.01–0.1 Hz) to that of the entire frequency range (0–0.25 Hz)37. The filtered and unsmoothed preprocessed images were used to calculate the sReHo and sDC. The calculation of static ReHo was based on the Kendall’s coefficient of concordance using the DPABI software. This serves as a measure of the similarity between the time series of a given voxel and its nearest 26 voxels38. The sReHo images were spatially smoothed with a 6 mm FWHM for the statistical analyses. State DC was defined as the weighted sum of voxels whose correlation coefficient with all the other voxels in the whole brain was above the selected threshold (r > 0.25 in the present study). The sDC images were spatially smoothed with 6 mm FWHM for the statistical analyses.
Calculation of dALFF, DfALFF, dReHo, and dDC
The dynamic metrics (dALFF, dfALFF, dReHo, and dDC) were carried out utilizing DPABI-based Temporal Dynamic Toolkits39. In the present study, an approach based on a sliding window was used to calculate the dynamic metrics. Previous studies have proven that this method was sensitive in detecting time-dependent variations and assessing the variability of metrics across the brain31,40. The window length used in resting-state dynamic analyses is a key factor. This parameter should be small enough to monitor potentially transient signals and large enough to analyze the lowest fluctuation of interest in the signals. Currently, window length is an open area of research in detecting the changes of temporal dynamic characteristics. In this study, we used a rectangular sliding window with a size of 60s (30 TRs) across the whole scan with a step of 1 TR, resulting in 141 overlapping windows per subject. We also examined the effect with other window lengths, which were included in validation analyses.
The following analysis procedures were used for the calculation of all dynamic metrics. All of these metrics were calculated based on a brain mask where all the lesioned voxels were excluded. We take the dALFF metric as an example to introduce the analysis process in detail. Within each window, we calculated the ALFF for every voxel in the brain. The sliding window was shifted by 1 TR and the corresponding ALFF was computed. This process was performed until the entire data length was covered. The standard deviation (SD) of dALFF values for all voxels across 141 windows of each participant was calculated to assess the variability of ALFF. Later, dALFF maps were spatially smoothed using a 6 mm FWHM Gaussian kernel. Other dynamic metrics (dfALFF, dReHo, and dDC) were obtained through the same process as above.
Statistical analysis
Demographic and clinical variables between the stroke and HC groups were analyzed using SPSS 19.0 software (SPSS, Inc., Chicago, IL, United States). Group differences in sex and age between the stroke and control group were explored using two-sample t-tests and chi-square tests. Paired t-tests were conducted to assess the therapeutic effect after intervention on behavioral performance within the stroke group. Statistical significance was set at p < 0.05.
For static and dynamic image metrics, a general linear model in SPM 12 was employed to compare differences between groups (the Ppre and the controls). Two-sample t-tests, with age, sex, and mean FD controlled as confounding covariates, were used to compare image values and detect differences between stroke patients at the initial time point and the normal controls. We set the statistical threshold to p < 0.05, corrected with the Gaussian random field approach (the voxel level was p < 0.01). All significant results were displayed using the xjView toolbox and the locations of the significant clusters were based on the AAL atlas. After conducting the two-sample t-test, we regarded areas with significant differences in each metric as regions of interest (ROI). Mean values of static and dynamic metrics from the ROIs were extracted for all participants. Treatment effects on image metrics of these ROIs were calculated among different groups: paired t-tests between the two time points, and two-sample t-tests between the stroke patients at the second time point and the normal controls. Statistical significance was set at p < 0.05. Considering that several comparison analyses were conducted, a multiple comparison correction is required to account for the difference between groups.
Correlation between the neuroimaging index and clinical scores
We further investigated whether changes in brain imaging following a stroke have correlations with the recovery of clinical performance. This analysis specifically focused on regions that exhibited significant differences between the groups in two or more image metrics. Correlation analyses were conducted to examine the relationship between changes in these image metrics and alterations in each clinical score over time among stroke patients. The changes of these image metrics and the clinical scores were calculated in the formula: (Post-Pre)/Pre. Additionally, the correlations were performed to assess the association between changes in these image metrics and disease duration. A significance threshold of p < 0.05 was applied, while controlling for age and sex during the correlation process using SPSS statistical software. Considering that several correlation analyses were conducted, a multiple comparison correction is required to account for correlations. The setting of the statistical threshold mainly depends on how many brain regions we select for correlation analysis and how many image metrics were used.
Validation analyses
We carried out additional analyses to validate our findings of the dynamic indices. We examined the differences using other window sizes (50TRs) to validate our results.
Results
Behavioral data
The demographic and clinical data are presented in Table 1. No significant differences were observed in terms of sex (χ2 = 0.703, p = 0.402) and age (t = 0.327, p = 0.745) between the patient group and the normal control group. Within the patient group, there was a significant increase in FMA scores (paired t-test: t = -9.49, p < 0.001), from an initial score of 83.75 ± 4.56 to a subsequent score of 91.45 ± 3 0.97.The MBI scores also showed a significant improvement within the patient group (paired t-test: t = -7 0.68, p < 0 0.001), increasing from an initial score of 32 0.43 ± 10 0.47 to a subsequent score of 41 0.56 ± 9 0.88. The severity of the neurological functional deficit after stroke was assessed by the NDS and showed a significant decrease (paired t-test: t = 12.87, p < 0.001) from 23.70 ± 4.60 (first time point) to 14.35 ± 5.07 (second time point).
Group differences of static image indices: sALFF, SfALFF, sReHo, sDC
Compared to the normal controls, stroke patients at the initial time point exhibited a significant increase in sALFF in the left medial superior frontal gyrus (SFG), left opercular inferior frontal gyrus (IFG), left inferior temporal gyrus (ITG), and left cerebellum. Following one month of intervention, the abnormally elevated sALFF values in these regions were suppressed and approached levels observed in the normal group except for the left medial SFG. Additionally, stroke patients at the initial time point demonstrated a significant decrease in sALFF within certain regions, including bilateral precuneus, left middle frontal gyrus (MFG), right triangularis IFG, right angular gyrus, and right supplementary motor area (SMA). At the second timepoint, these abnormally decreased sALFF values were changed but the trend was not significant (Ppost vs. Ppre, no significant differences). The detail results of the comparison analyses can be found in the Table 2. The specific locations of these regions can be found in Fig. 2A; Table 3.
Brain regions with significant intergroup differences in static image activity indictors between the stroke patients and the normal controls: (A) sALFF, (B) sfALFF, (C) sReHo, (D) sDC. The statistical threshold was set to p < 0.05 corrected with the Gaussian random field approach (the voxel level was p < 0.01). Data are mean ± SD. The color bar indicates the t-values. Ppre, stroke patients’ results at the first time point; Ppost, stroke patients’ results at the second time point; HC, healthy control; sALFF, static amplitude of low-frequency fluctuation; sfALFF, static fractional ALFF; sReHo, static regional homogeneity; sDC, static degree centrality.
Compared to the normal controls, stroke patients at the initial time point exhibited a significant increase in sfALFF in the left medial frontal gyrus and left superior precuneus. Following one month of intervention, the abnormally elevated sfALFF values in the left medial frontal gyrus and left superior precuneus were suppressed to some degree. Additionally, stroke patients at the initial time point demonstrated a significant decrease in sfALFF in several regions, including bilateral central precuneus, left SFG, right fusiform, and left middle temporal gyrus (MTG). After one month of intervention, these regions showed an increase in their sfALFF values in some degree. Notably, there was a significant increase in the decreased sfALFF values specifically within the bilateral central precuneus after one month of intervention. The detail results of the comparison analyses can be found in the Table 2. The specific locations of these regions can be found in Fig. 2B; Table 3.
For the stroke patients at the initial time point, increased sReHo values were observed in the right angular gyrus, right postcentral gyrus, right MTG, left ITG, and left superior precuneus compared to HCs. Conversely, decreased ReHo values were found in the right anterior cingulate cortex (ACC) and bilateral insula. Following one month of intervention, these aberrant sReHo values in some regions exhibited a tendency towards the normal levels. The detail results of the comparison analyses can be found in the Table 2. The specific locations of these regions can be seen in Fig. 2C; Table 3.
Increased sDC values were detected in the bilateral angular gyri, bilateral SFG, left superior precuneus, right ITG, and left medial SFG among stroke patients at the initial time point compared to HCs. However, decreased sDC values were observed in the bilateral fusiform gyri, right AC, right MFG, right SFG, and cerebellum on the right side. After one month of intervention, these significant increased sDC values were reduced, notably for regions such as the right ITG, right angular gyrus and left medial SFG. Similarly, these significant decreased sDC values were enhanced to some degree, notably for regions such as right ACC and right cerebellum. The detail results of the comparison analyses can be found in the Table 2. The specific locations of these regions can be seen in Fig. 2D; Table 3.
Group differences of dynamic image indices: dALFF, DfALFF, dReHo, dDC
For dynamic ALFF, stroke patients at the initial time point exhibited significantly increased dALFF variability in the bilateral central precuneus, left cuneus, right angular gyrus, and right superior temporal gyrus (STG) compared to that of HCs. No significant decrease in dALFF variability was observed in stroke patients at the initial time point. Following one month of intervention, the abnormally elevated dALFF variability in these regions decreased, particularly in the right central precuneus. The detail results of the comparison analyses can be found in the Table 2. The specific locations of these regions can be found in Fig. 3A; Table 4.
Brain regions with significant intergroup differences in dynamic image activity indicators with window sizes of 30TRs between the stroke patients and the normal controls: (A) dALFF, (B) dALFF, (C) dReHo, (D) dDC. The statistical threshold was set to p < 0.05 corrected with the Gaussian random field approach (the voxel level was p < 0.01). Data are mean ± SD. The color bar indicates the t-values. Ppre, stroke patients’ results at the first time point; Ppost, stroke patients’ results at the second time point; HC, healthy control; dALFF, dynamic amplitude of low-frequency fluctuation; dfALFF, dynamic fractional ALFF; dReHo, dynamic regional homogeneity; dDC, dynamic degree centrality.
Compared to the HCs group, stroke patients at the initial time point exhibited significantly increased variability in dfALFF in the left ITG, left lingual, right MFG and right inferior parietal lobule (IPL). No significant decrease in dfALFF variability was observed. Following one month of intervention, the elevated dfALFF variability in these regions decreased, particularly in the left ITG and right IPL. The detail results of the comparison analyses can be found in the Table 2. The specific locations of these regions can be seen in Fig. 3B; Table 4.
In terms of dynamic ReHo, stroke patients at the initial time point exhibited significantly increased dReHo variability in the left superior precuneus and left superior parietal lobule (SPL) compared to HCs. No significant decrease in dReHo variability was observed in stroke patients at the initial time point. Following one month of intervention, the abnormally elevated dReHo variability in these two regions showed a significant reduction. The detail results of the comparison analyses can be found in the Table 2. The specific locations of these regions can be found in Fig. 3C; Table 4.
The stroke patients exhibited increased dDC variability in several regions, including the bilateral precentral, right orbital SFG, left MFG, left central precuneus, left cerebellum, right thalamus, right amygdala and left paracentral lobule at the initial time point compared to the HCs. Following one month of intervention, these abnormally elevated dDC variabilities in these regions showed some changes but these changes were not significant (Ppost vs. Ppre, no significant differences). The detail results of the comparison analyses can be found in the Table 2. Please refer to Fig. 3D; Table 4 for detailed locations of these regions.
Correlation analysis
The percentage changes of static fALFF and dynamic fALFF in the right central precuneus exhibited positive correlations with the percentage changes of FMA, as well as MBI (as shown in Fig. 4A; Table 5). Considering that several correlation analyses were conducted, a multiple comparison correction is required to account for correlations. None of these correlation analysis results could withstand the multiple comparison correction. In the left central precuneus, significant associations were observed between the percentage changes of static fALFF and behavioral scales (FMA and MBI) (as depicted in Fig. 4B; Table 5). In addition, significant correlations were found between the percentage changes of static fALFF in the left superior precuneus and the FMA scores (as illustrated in Fig. 4C; Table 5). However, this result could not withstand the multiple comparison correction.
Scatter diagrams show the significantly correlations between the percentage changes of image indicators and the percentage changes of scale scores in stroke patients with one-month follow-up. (A) The percentage changes of static fALFF and dynamic ALFF in the right precuneus were positively correlated with the percentage changes of FMA and MBI. (B) The percentage changes of static fALFF in the left precuneus were positively correlated with the percentage changes of FMA and MBI. (C) The percentage changes of dynamic fALFF in the left superior precuneus were positively correlated with the percentage changes of FMA. (D-G) Scatter diagrams show the significantly correlations between the percentage changes of image indicators and the disease duration in stroke patients with one-month follow-up. A significance threshold of p < 0.05 was applied.
The percentage changes of image metrics exhibited significant correlations with the disease duration (see in Fig. 4D-G). These image metrics encompassed the static fALFF in the right fusiform and left superior precuneus, dynamic fALFF variability in the left cuneus, and static DC in the right angular and ACC. Specifically, there were positive associations between the percentage changes of static fALFF in the right fusiform and both FMA scores and MBI scores, as depicted in Table 5. However, the results of these correlation analyses could not withstand correction except for the result between static DC in the left fusiform and MBI.
Validation results
The analyses conducted using varying sliding-window lengths provided further support for our observations of dynamic image metric differences. Notably, the significant cluster between the groups remained consistent even when employing a window length of 50 TRs (as seen in Supplementary Fig. 1). Moreover, both analyses exhibited similar patterns and directions of change.
Discussion
In the present study, we employed a combination of static and dynamic methods to investigate potential abnormalities and changes in intrinsic brain activity among subacute stroke patients before and after one-month medicine intervention. Multiple metrics were calculated to identify specific alterations in activity. We identified a significant overlap among the abnormal brain regions detected using various indicators in patients diagnosed with subcortical ischemic stroke. Furthermore, at the second time point, the level of the disrupted image indicator in some regions showed a tendency toward the direction of the HC group. These longitudinal image alterations were found to be associated with changes in behavioral performance and disease duration in stroke patients. Overall, our study provides consistent and comprehensive evidence for understanding post-stroke changes in brain activity. The image indicators identified within regions showing significant image-behavior relationships may have potential value for predicting clinical outcomes.
Specific disruptions of static and dynamic intrinsic brain activity in stroke
Compared to the normal controls, stroke patients exhibited significant alterations in their intrinsic brain activity. Differences in various static and dynamic indicators of brain activity were observed between the stroke group and HC group in multiple regions including the bilateral central precuneus, bilateral fusiform, bilateral SFG, bilateral MFG, bilateral precentral gyrus, right angular, left ITG, right ACC, right SMA, right IPL, left SPL, right amygdala, right thalamus, and left cuneus. These findings highlight the diverse and widespread nature of abnormal activity changes within the whole brain among patients with subcortical ischemic stroke. Our results are consistent with previous studies that have reported significant alterations in functional connectivity or regional metrics across various brain regions in stroke patients11,17,41,42. Moreover, these results further support the notion that ischemic stroke leads to reorganization of both perilesional and remote brain regions8,43,44.
Furthermore, the brain regions exhibiting significant alterations in resting-state activity are associated with the default mode network (DMN), frontoparietal network (FPN), and somatomotor network (SMN). These widespread changes in activity patterns within cognitive impairment-related regions of stroke patients encompass executive control, self-referential processes, and motor functions. We observed a decrease in sALFF in the right SMA and an increased in dDC in bilateral precentral gyrus in stroke patients. The SMA is known to be involved in motor supplementary functions, while the precentral gyrus plays a crucial role in executive and body motor functions by processing motor information. The decreased sALFF in the right SMA aligns with previous studies45,46 and suggested that intrinsic activity disruption in SMA contribute to motor deficits in stroke patients18. However, caution should be exercised when interpreting the increased dDC results observed in the bilateral precentral gyrus. DC serves as an analytical method for characterizing local properties of resting-state fMRI signals and describes the importance of local brain regions within the whole-brain network. A prior study demonstrated reduced temporal variability of functional connectivity within the precentral gyrus during acute stages compared to subacute stages among ischemic stroke patients47. Long-term motor recovery has been associated with changes in temporal variability within this region. Conversely, another study found significantly decreased DC values specifically within the right precentral gyrus among patients with acute basal ganglia ischemic stroke18. The discrepancy between our findings and these previous studies may stem from differences in the stage-specific subjects included across investigations. Notably, our study primarily focused on non-acute phase stroke patients (1 to 2 months post-stroke onset), which suggests that significant changes occur within local brain properties of activity at different stages of stroke. Additionally, in the present study, the elevated dDC values were suppressed at the second time point, and there was a positive correlation between the percentage changes of dDC and NDS. The temporal variability of DC in the bilateral precentral gyrus decreased during the recovery process. The increased DC observed at the first time point in the bilateral precentral gyrus may be attributed to the compensatory expression of impaired brain function following stroke. This explanation is also applicable to elucidate the abnormal changes in DMN (central precuneus, ACC) and FPN (parietal, frontal cortex) observed in this study since simultaneous increases and decreases in spontaneous activity occur within these regions, which have been previously reported to undergo significant alterations after stroke5,48,49,50,51.
Overlapped disruptions of static and dynamic intrinsic brain activity in stroke
In the present study, we employed a combination of static and dynamic methods to investigate disruptions in brain activity following stroke using resting-state fMRI data. One key finding from our analysis is the substantial overlap observed among abnormal brain regions identified by various indicators in stroke patients. Notably, significant overlap was found in the bilateral central precuneus with decreased sALFF/sfALFF/dALFF, the left superior precuneus with increased sfALFF/sReHo/sDC/dReHo, the left ITG with increased sALFF/sReHo/dfALFF, the ACC with decreased sReHo/sDC, the right IPL with increased sReHo/dfALFF, the right fusiform with increased sfALFF/sDC, and the right angular gyrus with decreased sALFF/dALFF and increased sReHo/sDC. To comprehend these changes in brain activity patterns, it is crucial to consider the fundamental properties of these imaging indicators. Specifically, alterations in ALFF reflect regional spontaneous brain activity intensity through MRI signals. The utilization of sfALFF enhances sensitivity and specificity for detecting spontaneous brain activities by representing the ratio of low-frequency power spectrum to that of the entire frequency range. Consequently, dALFF and dfALFF can capture temporal variability in intrinsic brain activity fluctuations. On the other hand, sReHo measures local neural activity similarity among adjacent regions as an indicator for assessing regional low-frequency spontaneous activity; while dReHo represents temporal variability within this regional low-frequency spontaneous activity.
We observed significant changes in brain activity within the central precuneus, ACC, and angular gyrus, which are components of the DMN. The DMN is a crucial resting-state functional network involved in sustaining attention, emotional control, and self-consciousness16,52. Evidence has shown that stroke patients commonly exhibit dysfunction in DMN’s functional connectivity and brain activity11,53,54. Abnormal alterations in intrinsic brain activity within the DMN can disrupt cognitive processes associated with this network. As a vital component of the DMN, the precuneus plays a pivotal role in memory consolidation, self-reflection, and consciousness55. Recent advancements in resting-state fMRI analyses have provided comprehensive insights into its function by examining its associations with large-scale brain networks56. Our study further demonstrates decreased sALFF/sfALFF/dALFF bilaterally within the central precuneus among stroke patients. These findings align with previous studies reporting reduced functional homotopy within bilateral central precuneus regions among ischemic stroke patients11,57. The decreased measures mentioned above indicate suppressed normal amplitude and temporal variability of intrinsic brain activity within the central precuneus among stroke patients. Additionally, we observed a significant decrease in sReHo/sDC within the ACC (another key region of the DMN) among stroke patients. Previous research has demonstrated a significant reduction in functional connectivity between these two key areas of the DMN (precuneus and ACC) among stroke patients with cognitive impairment16. Based on this, we speculated that a consistent decline in activity of the bilateral central precuneus and ACC may reflect functional disruption associated with cognitive impairment. The angular gyrus has long been regarded as a pivotal node of the DMN58. Positioned at the junction between the temporal, parietal, and occipital lobes, this region is also considered a cross-modal hub where converging multisensory information is integrated59. Due to its unique ___location in the brain, this region plays a critical role in various cognitive functions. In our study, changes in the right angular gyrus varied across indicators: decreased sALFF/dALFF and increased sReHo/sDC. The decrease in sALFF and dALFF values within the angular gyrus may indicate reduced or inhibited brain activity. Conversely, ReHo and DC values exhibited an increase in the right angular gyrus. This finding suggests strengthened connectivity between the right angular gyrus and other associated regions. Our inference is based on both anatomical considerations regarding the ___location of the angular gyrus within the brain and compensatory mechanisms for suppressing spontaneous activity within this region.
In the present study, we observed a significant increase in sfALFF/sReHo/sDC/dReHo in the left superior precuneus. To gain a better understanding of this result, it is important to consider the bilateral precuneus findings (decreased sALFF/sfALFF/dALFF in both hemispheres). Previous neuroimaging studies conducted on macaque monkeys and humans have demonstrated that the precuneus exhibits anatomical heterogeneity60, characterized by three distinct patterns of functional connectivity: anterior, central, and posterior precuneus. The anterior precuneus is functionally connected to the superior parietal cortex, paracentral lobule, and motor cortex; while the central precuneus shows functional connectivity with dorsolateral/dorsomedial prefrontal and multimodal lateral parietal cortex regions. The posterior precuneus demonstrates functional connectivity with adjacent visual cortical regions. By comparing our results with Margulies’ findings, we determined that the superior precuneus in our study corresponds to their anterior precuneus region. Furthermore, our study revealed opposite tendencies in activity between the superior and central precuneus regions, confirming their heterogeneous nature. In addition to increased activity indicators observed in the left superior precuneus (sfALFF/sReHo/sDC/dReHo), we also found significant increases in brain activity indicators within the bilateral precentral cortex (dDC) and the left SPL (dReHo) following stroke onset. Notably, these changes were consistent with previous findings indicating functional connectivity between the anterior precuneus and the superior parietal cortex as well as paracentral lobule60. The heterogeneity of functional connectivity within the precuneus can also explain the decreased sALFF/sfALFF/dALFF in the bilateral central precuneus observed in this study. Functional connectivity patterns from the central precuneus primarily involve the superior frontal lobe, angular gyrus and ACC. Most of the activity indicators in these regions exhibited significant decreases following stroke. The consistent changes observed among the central precuneus, frontal lobe, ACC, and angular gyrus in stroke patients suggest an interaction between these regions. This current research highlights the importance of intrinsic brain activity in stroke. Furthermore, our findings indicate that a combined application of static and dynamic intrinsic brain activity indicators can comprehensively reveal real abnormal neuronal activity and facilitate understanding of recovery processes following stroke.
The alterations of the disrupted activity from the pre- to the post-intervention in stroke
Stroke is a prominent cause of disability, necessitating an understanding of its impact on brain architecture and changes in brain activity during recovery. In this study, we investigated alterations in intrinsic brain activity among ischemic stroke patients before and after one month of intervention. The findings revealed that the disrupted imaging indicators of some regions exhibited partial recovery at the second time point, aligning with our expectations and previous stroke research results. For instance, a prior study demonstrated a trend toward pronounced pre-to-post normalization of hypo-connections in subacute stroke patients following sensorimotor therapy. Notably, improvements in motor function associated with sensorimotor therapy were linked to alterations in functional connectivity approaching normative levels61. Previous studies have also indicated that rehabilitation interventions can modulate intrinsic functional connectivity and cortical activation patterns in stroke patients, wherein plasticity within these networks correlates with motor improvement62,63. These previous studies suggest that the restored pattern observed post-intervention implies the establishment of balanced sensorimotor cortex regions across bilateral hemispheres to expedite motor recovery. In our study, both increases and decreases in activity changes were detected among patients at the initial time point; however, after one month of medication, the abnormal intrinsic brain activity in certain regions showed a tendency toward the direction of the HC group. This restoration not only encompassed motor-related regions but also extended to other cognitive-related areas involved in the recovery process such as the SMN, DMN and FPN. The longitudinal changes in our clinical assessment performance also demonstrated significant improvements in patients’ motor function, daily living ability, and nervous function at the second time point.
After one month of intervention, although there was a tendency for abnormal intrinsic brain activity in these regions, which was observed at the first time point to approach normal levels, not all of the changes were statistically significant. The differences in these regions were mainly determined through statistical analysis comparing patients before and after treatment. It is noteworthy that significant alterations were primarily concentrated within the central precuneus, superior precuneus, ACC, angular gyrus, IPL and frontal cortex. It is also noteworthy that these significant alterations were mainly in the DMN and FPN. Furthermore, it should be noted that different directions of change were observed among these regions. For instance, from the first to the second time point, image indicator values significantly increased in the central precuneus and ACC while a significant decrease was detected in the superior precuneus, IPL, angular gyrus and frontal cortex. Previous studies have indicated that stroke patients exhibit increased activation within FPN as a compensatory mechanism for motor function recovery5. Additionally, stroke patients demonstrate decreased spontaneous activity within DMN and reduced resting-state functional connectivity between the posterior cingulate cortex and the anterior cingulate cortex16. These impaired spontaneous activities and functional connectivity might underlie cognitive decline following stroke onset. Our findings are consistent with these reports as we observe suppression of abnormalities within these regions after an effective intervention period towards the direction of the normal levels.
Another explanation for the brain imaging changes observed before and after treatment lies in the potential effectiveness of the intervention program. In the present study, all ischemic stroke patients, as indicated by their disease duration in the supplemental materials, were in the subacute stage. During this stage, the focus shifts from immediate life-saving interventions to stabilization, rehabilitation, and secondary prevention of another stroke. Our treatment regimen included a combination of antiplatelet therapy and intravenous citicoline. Antiplatelet therapy is a cornerstone in the management and prevention of ischemic strokes32, and it is crucial to initiate this therapy promptly after the onset of stroke symptoms to maximize its benefits. Citicoline, a drug widely used for neuroprotection and neurorepair, particularly in cases of brain injury or disease64, is typically administered immediately following a stroke via intravenous injection at high doses to rapidly exert its neuroprotective effects33. Some studies mention the use of citicoline over a longer period after a stroke, which imply that citicoline may have certain therapeutic effects in the subacute phase64,65. Both drugs likely contribute to improving neurological dysfunction, which aligns with the significant reduction in NDS scores observed between the two time points in our clinical assessments. Additionally, the improvement in imaging indicators of the ROIs from the first to the second time point further supports the notion of neurological function repair in patients.
Although the factor of intervention could account for the longitudinal changes in brain spontaneous activity, we acknowledge that spontaneous recovery after stroke may also influence our findings. Spontaneous recovery following a stroke occurs when survivors exhibit a sudden improvement in symptoms and regain lost functions, which results from the brain’s natural repair of some of the damage incurred by the stroke. This phenomenon typically manifests within the first six months post-stroke and is contingent upon intrinsic repair mechanisms. Previous neuroimaging studies have primarily focused on cerebral reorganization following spontaneous recovery after stroke and have demonstrated that neural reorganization is the key driver of functional recovery post-stroke2,66,67. It is commonly observed that some degree of spontaneous behavioral recovery occurs in the weeks following stroke onset. Brain imaging studies have also shown that behavioral outcomes are associated with a return towards normal brain functional organization66,68. In this study, we employed both static and dynamic intrinsic brain activity methods to investigate longitudinal changes in brain functional patterns after a stroke. As expected, the disrupted imaging indicators of some regions showed partial recovery from the first to the second time point in the patient group. During this period, stroke patients received a combine intervention of antiplatelet therapy and intravenous citicoline. The disruptions in brain function among stroke patients were alleviated at the second time point. Both the combined intervention and spontaneous recovery may contribute to this improvement. However, it should be noted that our study only included one patient group receiving the combined intervention. Therefore, we cannot exclude the potential impact of spontaneous recovery on our results. To address this issue and rule out any confounding effects of spontaneous recovery, future experiments should include a patient group without any therapy intervention as well. Thus, based on our current findings alone, it can be suggested that disrupted intrinsic brain activity tends to recover towards normative levels over time post-stroke. Future research endeavors should aim to refine experimental designs in order to elucidate which factors underlie these observations.
Specific correlations between the alterations of image indicators and behavioral performances
Finally, we investigated whether changes in brain activity observed in these images were correlated with clinical recovery performance. We leveraged the longitudinal changes of resting-state fMRI to assess the recovery processes and combined them with clinical assessments. Previous studies have suggested that most deficits can be restored within three months69. Another study demonstrated that brain oscillatory activity during rehabilitative intervention could serve as a biomarker for motor recovery in chronic stroke patients70. It is well-established in stroke research that plasticity of intrinsic brain connectivity and cortical activation patterns are associated with cognitive improvement62,63,71,72. Therefore, these correlations between imaging findings and behavioral outcomes may indicate that neurological recovery primarily drives longitudinal improvements in clinical scores. Our correlation analysis revealed significant associations between percentage changes in imaging indicators and percentage changes in clinical performances across the two time points. These results align with our expectations and previous stroke studies.
Upon examining the specific correlation results, we observed significant image-behavior correlations in several regions, including bilateral central precuneus, left superior precuneus, bilateral fusiform, right angular gyrus and right ACC. Notably, these regions were predominantly localized within the DMN and FPN. The DMN is commonly associated with internally directed cognition and emotional processing16, while the FPN is recognized as a high cognitive control network involved in cognitive control, goal-directed behavior, and visual attention5. In relation to the longitudinal alterations of brain activity discussed earlier in this study regarding stroke patients’ possible mechanisms of activity changes within the DMN and FPN networks; we speculate that such longitudinal changes may reflect improvements in cognitive function among stroke patients. One study focused on the comprehensive treatment recovery mechanism of acute ischemic stroke and found a significant association between changes in clinical scale scores over time and improvements in the functional connectivity of the cuneus and precuneus73. This study highlighted the critical role of the cuneus and precuneus in stroke recovery. Another study reported a significant positive correlation between the dynamic characteristics of local brain activity and FMA scores in the right precuneus30. Our correlation findings are consistent with these previous studies and further support the aforementioned hypothesis.
Limitations
There were several potential limitations of this study. Firstly, the sample size was small, which could limit the statistical power to detect longitudinal changes in brain spontaneous activity. The distribution of disease duration was not concentrated within the patient group. Future studies should involve larger sample sizes and stratify groups according to disease stages to confirm our findings. Secondly, although the experimental design was longitudinal, we cannot clearly demonstrate whether the significant recovery was induced by treatment or spontaneous recovery alone. Therefore, improvements are needed in the experimental design. Thirdly, multiple activity indicators were analyzed in this study and yielded diverse results. While most of the main findings have been discussed, certain significant results, such as differences in the fusiform and the insula regions, require further explanation. These regions play crucial roles in higher cognitive tasks like face perception, object recognition, and emotional subjective awareness; however, they have rarely been reported in subcortical ischemic stroke studies before. Henceforth, these results need to be validated and reasonably elucidated through future investigations. Fourth, the observed alterations in brain function might originate from post-stroke cerebrovascular changes. However, the current experimental design is inadequate to attribute the imaging changes solely to cerebrovascular modifications. Future research should integrate cerebral vascular imaging data with fMRI data to provide a more comprehensive understanding of the brain function changes following a stroke. And also, when we considered both the ROI numbers and the indicator numbers for multiple comparison correction, the statistical results can’t stand up the correction. Although we found that certain brain regions showed significant changes across different measures, these differences did not withstand multiple comparison adjustments. This limitation indicate that we should take a caution in the interpreting of the current results. Lastly, we utilized a rectangular window in dynamic functional activity analysis, which may not be the most suitable window type for dynamic analysis. Alternative window types, such as tapered windows, should be considered in future investigations.
Conclusions
By employing a combination of static and dynamic indicators, we comprehensively assessed the specific differences in intrinsic brain activity between patients with subcortical ischemic stroke and HC. Additionally, we calculated the longitudinal changes in activity disruption and their correlations with clinical performance. Significant variations were observed in multiple regions, including the SMN, DMN and FPN, using these static and dynamic image indicators in patients with ischemic stroke. Furthermore, there was considerable overlap among the abnormal brain regions identified by different indicators in stroke. At the second time point, a recovery trend of these disrupted imaging indicators was observed in certain regions. Correlation analyses revealed that clinical improvement was associated with the recovery of brain activity. Overall, our findings demonstrate that combining static and dynamic imaging methods can comprehensively elucidate abnormal activity patterns and their longitudinal changes in ischemic stroke. Moreover, identifying regions exhibiting significant overlap across different brain activity indicators as well as establishing image-behavior relationships can provide more comprehensive insights into the neurobiological mechanisms underlying stroke while facilitating the development of therapeutic strategies for this disease.
Data availability
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request.
References
Pu, L. et al. Projected global trends in ischemic stroke incidence, deaths and Disability-Adjusted life years from 2020 to 2030. Stroke 54, 1330–1339. https://doi.org/10.1161/STROKEAHA.122.040073 (2023).
Grefkes, C. & Fink, G. R. Recovery from stroke: current concepts and future perspectives. Neurol. Res. Pract. 2 https://doi.org/10.1186/s42466-020-00060-6 (2020).
Latifi, S. & Carmichael, S. T. The emergence of multiscale connectomics-based approaches in stroke recovery. Trends Neurosci. 47, 303–318. https://doi.org/10.1016/j.tins.2024.01.003 (2024).
Liu, J. et al. Cortical structural changes after subcortical stroke: patterns and correlates. Hum. Brain. Mapp. 44, 727–743. https://doi.org/10.1002/hbm.26095 (2023).
Olafson, E. et al. Frontoparietal network activation is associated with motor recovery in ischemic stroke patients. Commun. Biology. 5, 993. https://doi.org/10.1038/s42003-022-03950-4 (2022).
Ovadia-Caro, S., Margulies, D. S. & Villringer, A. The value of resting-state functional magnetic resonance imaging in stroke. Stroke 45, 2818–2824. https://doi.org/10.1161/STROKEAHA.114.003689 (2014).
Yu, P. et al. Neuroimaging of motor recovery after ischemic stroke - functional reorganization of motor network. NeuroImage Clin. 43, 103636. https://doi.org/10.1016/j.nicl.2024.103636 (2024).
Rehme, A. K. & Grefkes, C. Cerebral network disorders after stroke: evidence from imaging-based connectivity analyses of active and resting brain States in humans. J. Physiol. 591, 17–31. https://doi.org/10.1113/jphysiol.2012.243469 (2013).
Wang, Y. Y. et al. Abnormal functional connectivities patterns of multidomain cognitive impairments in Pontine stroke patients. Hum. Brain. Mapp. 43, 4676–4688. https://doi.org/10.1002/hbm.25982 (2022).
Li, Y., Wu, P., Liang, F. & Huang, W. The microstructural status of the corpus callosum is associated with the degree of motor function and neurological deficit in stroke patients. PloS One. 10, e0122615 (2015).
Li, Y. X., Yu, Z. Y., Zhou, X., Wu, P. & Chen, J. X. Aberrant interhemispheric functional reciprocities of the default mode network and motor network in subcortical ischemic stroke patients with motor impairment: A longitudinal study. Front. Neurol. 13 996621. https://doi.org/10.3389/fneur.2022.996621 (2022).
Park, C. H. et al. Longitudinal changes of resting-state functional connectivity during motor recovery after stroke. Stroke 42, 1357–1362. https://doi.org/10.1161/STROKEAHA.110.596155 (2011).
Volz, L. J. et al. Shaping early reorganization of neural networks promotes motor function after stroke. Cereb. Cortex. 26, 2882–2894. https://doi.org/10.1093/cercor/bhw034 (2016).
Wang, X., Casadio, M., Weber Ii, K. A., Mussa-Ivaldi, F. A. & Parrish, T. B. White matter microstructure changes induced by motor skill learning utilizing a body machine interface. Neuroimage 88, 32–40. https://doi.org/10.1016/j.neuroimage.2013.10.066 (2014).
Wei, Y. et al. Progressive Gray matter atrophy and abnormal structural covariance network in ischemic Pontine stroke. Neuroscience 448, 255–265. https://doi.org/10.1016/j.neuroscience.2020.08.033 (2020).
Liu, J. et al. Altered spontaneous activity in the default-mode network and cognitive decline in chronic subcortical stroke. J. Neurol. Sci. 347, 193–198. https://doi.org/10.1016/j.jns.2014.08.049 (2014).
Wu, P. et al. Changes of resting cerebral activities in subacute ischemic stroke patients. Neural Regeneration Res. 10, 760 (2015).
Chen, H. et al. Frequency specific alterations of the degree centrality in patients with acute basal ganglia ischemic stroke: a resting-state fMRI study. Brain Imaging Behav. 18, 19–33. https://doi.org/10.1007/s11682-023-00806-1 (2024).
Aamodt, E. B. et al. Longitudinal brain changes after stroke and the association with cognitive decline. Front. Neurol. 13 https://doi.org/10.3389/fneur.2022.856919 (2022).
Fan, L. et al. The longitudinal neural dynamics changes of whole brain connectome during natural recovery from poststroke aphasia. NeuroImage: Clin. 36, 103190. https://doi.org/10.1016/j.nicl.2022.103190 (2022).
Mirzaei, G. & Adeli, H. Resting state functional magnetic resonance imaging processing techniques in stroke studies. Rev. Neurosci. 27, 871–885. https://doi.org/10.1515/revneuro-2016-0052 (2016).
Van Den Heuvel, M. P. & Hulshoff Pol, H. E. Exploring the brain network: a review on resting-state fMRI functional connectivity. Eur. Neuropsychopharmacol. 20, 519–534 (2010).
Allen, E. A. et al. Tracking whole-brain connectivity dynamics in the resting state. Cereb. Cortex. 24, 663–676. https://doi.org/10.1093/cercor/bhs352 (2014).
Chang, C. & Glover, G. H. Time-frequency dynamics of resting-state brain connectivity measured with fMRI. Neuroimage 50, 81–98. https://doi.org/10.1016/j.neuroimage.2009.12.011 (2010).
Chen, J. et al. Dynamic alterations in spontaneous neural activity in multiple brain networks in subacute stroke patients: A Resting-State fMRI study. Front. NeuroSci. 12 https://doi.org/10.3389/fnins.2018.00994 (2019).
Huang, J., Cheng, R., Liu, X., Chen, L. & Luo, T. Abnormal static and dynamic functional connectivity of networks related to cognition in patients with subcortical ischemic vascular disease. Neuroradiology 64, 1201–1211. https://doi.org/10.1007/s00234-022-02895-z (2022).
Li, Y., Ran, Y., Yao, M. & Chen, Q. Altered static and dynamic functional connectivity of the default mode network across epilepsy subtypes in children: A resting-state fMRI study. Neurobiol. Dis. 192, 106425. https://doi.org/10.1016/j.nbd.2024.106425 (2024).
Wei, Y. et al. Altered static and dynamic cerebellar-cerebral functional connectivity in acute Pontine infarction. Cereb. Cortex. 34 ARTN bhae18210.1093/cercor/bhae182 (2024).
Chen, J. et al. Altered static and dynamic voxel-mirrored homotopic connectivity in subacute stroke patients: a resting-state fMRI study. Brain Imaging Behav. 15, 389–400. https://doi.org/10.1007/s11682-020-00266-x (2021).
Tian, N. et al. More than just statics: altered complexity of dynamic amplitude of low-frequency fluctuations in the resting brain after stroke. J. Neural Eng. 19 036036. https://doi.org/10.1088/1741-2552/ac71ce (2022).
Wang, X. et al. Altered static and dynamic spontaneous neural activity in patients with ischemic Pontine stroke. Front. NeuroSci. 17 https://doi.org/10.3389/fnins.2023.1131062 (2023).
Kleindorfer, D. O. et al. Guideline for the Prevention of Stroke in Patients With Stroke and Transient Ischemic Attack: A Guideline From the American Heart Association/American Stroke Association. Stroke 52, e364-e467, (2021). https://doi.org/10.1161/STR.0000000000000375 (2021).
Dávalos, A. et al. Citicoline in the treatment of acute ischaemic stroke: an international, randomised, multicentre, placebo-controlled study (ICTUS trial). Lancet 380, 349–357. https://doi.org/10.1016/S0140-6736(12)60813-7 (2012).
Yan, C. & Zang, Y. DPARSF: a MATLAB toolbox for pipeline data analysis of resting-state fMRI. Front. Syst. Neurosci. 4, 13. https://doi.org/10.3389/fnsys.2010.00013 (2010).
Yan, C. G., Wang, X. D., Zuo, X. N. & Zang, Y. F. DPABI: data processing & analysis for (Resting-State) brain imaging. Neuroinformatics 14, 339–351. https://doi.org/10.1007/s12021-016-9299-4 (2016).
Yu-Feng, Z. et al. Altered baseline brain activity in children with ADHD revealed by resting-state functional MRI. Brain Develop. 29, 83–91. https://doi.org/10.1016/j.braindev.2006.07.002 (2007).
Zou, Q. H. et al. An improved approach to detection of amplitude of low-frequency fluctuation (ALFF) for resting-state fMRI: fractional ALFF. J. Neurosci. Methods. 172, 137–141. https://doi.org/10.1016/j.jneumeth.2008.04.012 (2008).
Zang, Y., Jiang, T., Lu, Y., He, Y. & Tian, L. Regional homogeneity approach to fMRI data analysis. Neuroimage 22, 394–400. https://doi.org/10.1016/j.neuroimage.2003.12.030 (2004).
Yan, C. G., Yang, Z., Colcombe, S. J., Zuo, X. N. & Milham, M. P. Concordance among indices of intrinsic brain function: insights from inter-individual variation and Temporal dynamics. Sci. Bull. 62, 1572–1584. https://doi.org/10.1016/j.scib.2017.09.015 (2017).
Li, Y., Qin, B., Chen, Q. & Chen, J. Altered dynamic functional network connectivity within default mode network of epileptic children with generalized tonic-clonic seizures. Epilepsy Res. 184, 106969. https://doi.org/10.1016/j.eplepsyres.2022.106969 (2022).
Wang, S. R. et al. Using fractional amplitude of Low-Frequency fluctuations and functional connectivity in patients with Post-stroke cognitive impairment for a simulated stimulation program. Front. Aging Neurosci. 13, 724267. https://doi.org/10.3389/Fnagi.2021.724267 (2021).
Zhao, Z. et al. Frequency-specific alterations of regional homogeneity in subcortical stroke patients with different outcomes in hand function. Hum. Brain. Mapp. 39, 4373–4384. https://doi.org/10.1002/hbm.24277 (2018).
Olafson, E. R. et al. Functional connectome reorganization relates to post-stroke motor recovery and structural and functional Disconnection. NeuroImage 245, 118642. https://doi.org/10.1016/j.neuroimage.2021.118642 (2021).
Wang, S. R. et al. The resting-state topological organization damage of language-related brain regions in post-stroke cognitive impairment. Brain Imaging Behav. 16, 2608–2617. https://doi.org/10.1007/s11682-022-00716-8 (2022).
Astrakas, L. G., Li, S., Elbach, S. & Tzika, A. A. The severity of sensorimotor tracts degeneration May predict motor performance in chronic stroke patients, while brain structural network dysfunction May not. Front. Neurol. 13, 813763. https://doi.org/10.3389/fneur.2022.813763 (2022).
Quandt, F. et al. The functional role of beta-oscillations in the supplementary motor area during reaching and grasping after stroke: A question of structural damage to the corticospinal tract. Hum. Brain. Mapp. 40, 3091–3101. https://doi.org/10.1002/hbm.24582 (2019).
Hu, J. et al. Dynamic Network Analysis Reveals Altered Temporal Variability in Brain Regions after Stroke: A Longitudinal Resting-State fMRI Study. Neural plasticity 2018, 1–10, (2018). https://doi.org/10.1155/2018/9394156
Stewart, J. C., Dewanjee, P., Shariff, U. & Cramer, S. C. Dorsal premotor activity and connectivity relate to action selection performance after stroke. Hum. Brain. Mapp. 37, 1816–1830. https://doi.org/10.1002/hbm.23138 (2016).
Wang, C. et al. Altered functional organization within and between resting-state networks in chronic subcortical infarction. J. Cereb. Blood Flow. Metabolism: Official J. Int. Soc. Cereb. Blood Flow. Metabolism. 34, 597–605. https://doi.org/10.1038/jcbfm.2013.238 (2014).
Wang, J. et al. Functional connectome hierarchy of thalamus impacts fatigue in acute stroke patients. Cereb. Cortex. 34, bhad534 (2024).
Zhu, T. et al. Altered functional connectivity within default mode network in patients with transient ischemic attack: A Resting-State functional magnetic resonance imaging study. Cerebrovasc. Dis. 48, 61–69. https://doi.org/10.1159/000502884 (2019).
Tuladhar, A. M. et al. Default mode network connectivity in stroke patients. PLoS One. 8, e66556. https://doi.org/10.1371/journal.pone.0066556 (2013).
Dacosta-Aguayo, R. et al. Impairment of functional integration of the default mode network correlates with cognitive outcome at three months after stroke. Hum. Brain. Mapp. 36, 577–590. https://doi.org/10.1002/hbm.22648 (2015).
Wu, C. W. W. et al. Synchrony between Default-Mode and sensorimotor networks facilitates motor function in stroke rehabilitation: A pilot fMRI study. Front. NeuroSci. 14, 54810 (2020).
Fransson, P. & Marrelec, G. The precuneus/posterior cingulate cortex plays a pivotal role in the default mode network: evidence from a partial correlation network analysis. Neuroimage 42, 1178–1184 (2008).
Dadario, N. B. & Sughrue, M. E. The functional role of the precuneus. Brain 146, 3598–3607. https://doi.org/10.1093/brain/awad181 (2023).
Yao, G. et al. Alterations of functional connectivity in stroke patients with basal ganglia damage and cognitive impairment. Front. Neurol. 11, 980. https://doi.org/10.3389/fneur.2020.00980 (2020).
Vatansever, D., Manktelow, A. E., Sahakian, B. J., Menon, D. K. & Stamatakis, E. A. Angular default mode network connectivity across working memory load. Hum. Brain. Mapp. 38, 41–52. https://doi.org/10.1002/hbm.23341 (2017).
Song, Y. et al. Functional hierarchy of the angular gyrus and its underlying genetic architecture. Hum. Brain. Mapp. 44, 2815–2828. https://doi.org/10.1002/hbm.26247 (2023).
Margulies, D. S. et al. Precuneus shares intrinsic functional architecture in humans and monkeys. Proc. Natl. Acad. Sci. U.S.A. 106, 20069–20074. https://doi.org/10.1073/pnas.0905314106 (2009).
De Bruyn, N. et al. Brain connectivity alterations after additional sensorimotor or motor therapy for the upper limb in the early-phase post stroke: a randomized controlled trial. Brain Commun. 3 https://doi.org/10.1093/braincomms/fcab074 (2021).
Ma, Z. Z. et al. Motor imagery-based brain–computer interface rehabilitation programs enhance upper extremity performance and cortical activation in stroke patients. J. Neuroeng. Rehabil. 21, 91. https://doi.org/10.1186/s12984-024-01387-w (2024).
Zheng, X. et al. The plasticity of intrinsic functional connectivity patterns associated with rehabilitation intervention in chronic stroke patients. Neuroradiology 58, 417–427 (2016).
Overgaard, K. The effects of citicoline on acute ischemic stroke: A review. J. Stroke Cerebrovasc. Dis. 23, 1764–1769. https://doi.org/10.1016/j.jstrokecerebrovasdis.2014.01.020 (2014).
Secades, J. J. et al. Citicoline for acute ischemic stroke: A systematic review and formal Meta-analysis of randomized, Double-Blind, and Placebo-Controlled trials. J. Stroke Cerebrovasc. Diseases: Official J. Natl. Stroke Association. 25, 1984–1996. https://doi.org/10.1016/j.jstrokecerebrovasdis.2016.04.010 (2016).
Cramer, S. C. Repairing the human brain after stroke: I. Mechanisms of spontaneous recovery. Ann. Neurol. 63, 272–287. https://doi.org/10.1002/ana.21393 (2008).
Pinter, D. et al. Early progressive changes in white matter integrity are associated with stroke recovery. Transl Stroke Res. 11, 1264–1272. https://doi.org/10.1007/s12975-020-00797-x (2020).
Arun, K. M., Smitha, K. A., Sylaja, P. N. & Kesavadas, C. Identifying Resting-State functional connectivity changes in the motor cortex using fNIRS during recovery from stroke. Brain Topogr. 33, 710–719. https://doi.org/10.1007/s10548-020-00785-2 (2020).
Ramsey, L. E. et al. Behavioural clusters and predictors of performance during recovery from stroke. Nat. Hum. Behav. 1, 0038. https://doi.org/10.1038/s41562-016-0038 (2017).
Ray, A. M., Figueiredo, T. D. C., Lopez-Larraz, E., Birbaumer, N. & Ramos-Murguialday, A. Brain oscillatory activity as a biomarker of motor recovery in chronic stroke. Hum. Brain. Mapp. 41, 1296–1308. https://doi.org/10.1002/hbm.24876 (2020).
Li, Y., Yu, Z., Wu, P. & Chen, J. The disrupted topological properties of structural networks showed recovery in ischemic stroke patients: a longitudinal design study. BMC Neurosci. 22, 47. https://doi.org/10.1186/s12868-021-00652-1 (2021).
Li, Y., Yu, Z., Wu, P. & Chen, J. Ability of an altered functional coupling between resting-state networks to predict behavioral outcomes in subcortical ischemic stroke: A longitudinal study. Front. Aging Neurosci. 14, 933567. https://doi.org/10.3389/fnagi.2022.933567 (2022).
Zhu, D. et al. Dynamic changes of resting state functional network following acute ischemic stroke. J. Chem. Neuroanat. 130, 102272. https://doi.org/10.1016/j.jchemneu.2023.102272 (2023).
Acknowledgements
The authors are grateful to the patients who participated in the study.
Funding
This research received funding from the Guangdong Basic and Applied Basic Research Foundation (No. 2023A1515010772, No. 2025A1515011720). This research was also support by the Medical Science and Technology Research Foundation of Guangdong Province (A2024120).
Author information
Authors and Affiliations
Contributions
Yongxin Li and Jianping Wang design the experiment, analyze the data and draft the paper for the work. Yun Ran help to acquire the clinical and fMRI data. Mao Yao helps to revise the paper critically for important intellectual content. Yongxin Li did the financial support, review and final approval of the paper to be published. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare that there is no conflict of interest.
Ethical approval
The current study was approved by the Research Ethics Committee of the Chengdu University of Traditional Chinese Medicine.
Consent to participate
All participants provided written informed consent before undergoing MR imaging.
Consent to publish
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, Y., Wang, J., Yao, M. et al. Alterations of static and dynamic changes in intrinsic brain activity and its relation to behavioral outcomes in subcortical ischemic stroke after one-month intervention. Sci Rep 15, 11961 (2025). https://doi.org/10.1038/s41598-025-96163-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-96163-8