Abstract
Operative treatment is an option for fractures when the fracture is unstable or the patient wishes to return early to daily life or social activities. Metal plates such as titanium and stainless steel are often used in fracture surgery, but the metal plate lacks bone-healing activity and is not bioabsorbable, requiring a second surgery to remove it after bone union. Here we show that a magnesium (Mg) plate made from an alloy of yttrium, zinc, and aluminum with magnesium as the main component in a long-period stacking ordered structure promotes bone formation in a rabbit tibia fracture model and is also bioabsorbable. We show that the Mg plate significantly promoted bone and callus formation compared to a titanium plate in the rabbit tibia fracture model. Moreover, the Mg plate was mostly bioabsorbed once bone union was achieved, but rabbits showed no evidence of biotoxic effects, such as weight loss or increased blood magnesium levels. We also demonstrate that treatment with exogenous magnesium significantly enhanced calcium deposition in an in vitro osteoblast culture system. Magnesium is an essential element, and its radiolucency facilitates observation of the fracture site during Mg plate fixation, while its lack of magnetic properties allows its use in patients who require MRI scans. Accordingly, we propose that a use of a Mg plate could be beneficial in treating bone fracture.
Similar content being viewed by others
Introduction
In developed countries, the number of fracture patients among the elderly is increasing due to the current expansion of the elderly population1. In the United States, the number of fracture cases among the elderly is estimated to be 2 million per year, a number expected to continue to increase2,3. The elderly are often at risk for fracture healing disorders4, including development of comorbidities such as osteoporosis5. Because fractures can impair activities of daily living (ADLs) in the elderly, smooth fracture healing is essential to maintain ADLs and independence after fracture healing6. In younger patients, shortening the time to bone healing in fracture treatment is also a challenge.
Fracture treatment can be divided into conservative therapy or operative treatment. Operative treatment is often chosen when it is estimated to have significant patient benefits, such as maintenance of ADLs and early return to society7,8,9. Medical implants, such as metal plates, are often used in operative treatment of fractures. After bone fusion, the patient will often undergo another surgery to remove the metal implant6,10,11,12,13. Avoiding this second surgery would require use of bioabsorbable therapeutic implants, but the development of metal implants that are both sufficiently strong and bioabsorbable is a challenge in fracture treatment.
Among various metal materials, magnesium (Mg) is biocompatible because it is an essential element, and pure Mg implants have been confirmed to be bioabsorbable14,15. Due to this high biocompatibility, Mg is considered a useful material for metal implants15,16. However, pure Mg implants have low mechanical strength and corrosion resistance, and maintaining fixation and fixation force is a concern in terms of using pure Mg implants for fracture treatment14,17,18,19,20,21. Therefore, in this study, we created an alloy of magnesium mixed with other metals to increase Mg implant strength.
Basically, Mg exhibits a hexagonal close-packed (hcp) structure, but a Mg alloy with zinc (Zn) and yttrium (Y) has a specific long stacking cycle called a long-period stacking ordered structure (LPSO structure). Mg-Zn-Y alloy with this structure consists of two phases: α-Mg (hexagonal closed-packed structure) and 18R-LPSO (rhombohedral structure). The LPSO phase is a periodic layered structure composed of a soft layer of Mg and a hard layer of solute-enriched stacking-fault. When the LPSO-type Mg alloy is extruded, both fine dynamic recrystallized grain regions and coarse un-recrystallized grain regions with strong texture are formed in the α-Mg phase. Moreover, kink bands also form in the LPSO phase. Thus, LPSO-type Mg-Zn-Y alloy reportedly exhibits high yield strength and reasonable elongation due to formation of this bimodal structure in the α-Mg phase and kink bands in the LPSO phase22,23,24. In particular, LPSO-type Mg-Zn-Y alloy prepared by rapid solidification exhibits an extremely high yield strength and good corrosion resistance with nanocrystalline and uniform microstructure25. In fact, pure Mg has yield strength and elongation of 125 MPa and 6.3%, respectively, while Mg- 0.56Zn- 1.5Y shows yield strength and elongation of 362 MPa and 18.2%, respectively26. Moreover, adding aluminum (Al) to the LPSO-type Mg-Zn-Y alloy improves corrosion resistance27,28. Recently, a rapidly-solidified (RS) Mg- 0.56Zn- 1.5Y alloy was developed for use in bioabsorbable medical devices26. This alloy has high ductility (14–19%) but maintains a high tensile yield strength of 362–383 MPa due to dilution of Zn and Y. We also found that adding 0.15 atom (at.) % Al to Mg-Zn-Y-alloy improved corrosion resistance29. Thus, RS Mg- 0.56Zn- 1.5Y- 0.15 Al alloy has mechanical properties and corrosion resistance superior to pure Mg and commercial Mg alloys and could be used to make bioabsorbable bone plates. Bone plates of pure Mg or commercial Mg alloys have not been used due to their low mechanical properties. However, RS Mg-Zn-Y alloy has a yield strength 1.9–2.0 times higher than that of commercially available Mg alloys such as WE43, and thus, potentially could be used to make implants.
In this study, we compared bone healing ability of an existing titanium plate (Ti plate) and a plate made from an LPSO-type Mg-Zn-Y-Al alloy of the same geometry (hereafter called a Mg plate) using a rabbit fracture model. Both plates produced bone fusion, but the Mg plate produced significantly greater callus; the peak force at failure after bone fusion was significantly higher for both bones after fixation with Mg plates as compared to contralateral normal bone. In addition, in osteoblast cultures in vitro, treatment with Mg significantly activated osteoblast differentiation and mineralization. In conclusion, the Mg plate is expected to be a new type of bioabsorbable implant that promotes bone healing as bone fracture treatment.
Material and methods
Rabbits
Japanese white rabbits were purchased from Japan SLC Co Ltd (Hamamatsu, Shizuoka, Japan).
-
1.
Approval: All animal experiment procedures were approved by the Animal Studies Committee and the Institutional Animal Care and Use Committee at Kumamoto University, Japan.
-
2.
Accordance: All animal experiments were carried out in accordance with the Institutional Guidelines on Animal Experiment at Kumamoto University. This study is reported in accordance with ARRIVE guidelines.
Mg plate preparation from LPSO-type Mg alloys
The master alloy, Mg- 0.75Zn- 2Y (at.%) alloy, was procured from Fuji Light Metal Co., Ltd., Kumamoto, Japan. It was melted in an Ar atmosphere using a high-frequency induction heating method, and pure Mg (99.99 wt.%) and Al (99.99 wt.%) were added to produce the Mg- 0.56Zn- 1.5Y- 0.15 Al (at.%) cast alloy. RS ribbons of the Mg- 0.56Zn- 1.5Y- 0.15 Al alloy were prepared by a single-roller melt-spinning method at a roll-circumferential velocity of 10 m s−1 and were pre-consolidated into the copper billet with an outer diameter of 29 mm in an Ar atmosphere using a glove box. Degassing was carried out at 573 K for 15 min. Prior to hot extrusion, pre-extrusion heat treatment was performed at 673 K for 24 h. Hot extrusion was performed at an extrusion ratio of 10, an extrusion temperature of 623 K, and a ram speed of 5.0 mm s−1 to obtain the RS Mg- 0.56Zn- 1.5Y- 0.15 Al alloy rod 10 mm in diameter utilized here. Those rods were machined into bone plates of the same shape as the existing Ti plate (VariAx Hand Locking Plate M Straight plate 4 holes, Stryker Japan K.K., Koraku, Tokyo, Japan) using machining center (Fig. 1A).
Metal plates and surgical procedures used in this study. (A) Shown are representative Ti (VariAx Hand Locking Plate M, Straight plate 4 hole) (top) or Mg (bottom) plates used for internal fixation in a right tibial fracture model using six-month-old female Japanese white rabbits (7 per group). (B) A 5-cm incision was made on the medial portion of the lower limb and bone fracture was created in the right proximal tibia using a bone saw, without cutting through to the contralateral cortical bone. (C) Ti or Mg plates were used for each group and internal fixation for the right tibial fracture was performed. In both groups, four threaded 2.3 mm titanium screws were used for plate fixation in each rabbit.
Fracture model
All surgical procedures were performed under general anesthesia. Medetomidine hydrochloride (0.25 mg/kg; Fujita) and midazolam (3 mg/kg; Sandoz) and butorphanol tartrate (0.4 mg/kg; Meiji) were administered subcutaneously in the neck region of 6-month-old female rabbits. Rectal administration of buprenorphine (0.2 mg; Otsuka Pharmaceutical) was performed along with intramuscular administration of the antibiotic enrofloxacin (7 mg/kg; Bayer) into the upper right limb. The surgical area was shaved and disinfected, followed by administration of local anesthesia with lidocaine hydrochloride (Maruishi Pharmaceutical) immediately before making a 5-cm incision on the medial portion of the lower limb. A bone fracture proximal to the middle of the right tibia was then made using a bone saw without cutting through to the contralateral bone cortex. Ti (group T) or Mg (group M) plates were used for each group and internal fixation was performed (Fig. 1, B and C). Four all threaded 2.3 mm titanium screws were used in all surgeries. Dermabond Advanced (Johnson & Johnson) was used to close the wound to complete the surgery.
All rabbits were sacrificed 12 weeks after operation. For sacrifice, rabbits were first sedated by subcutaneous administration of medetomidine hydrochloride (0.1 mg/kg; Fujita), midazolam (1.5 mg/kg; Sandoz) and butorphanol tartrate (0.2 mg/kg; Meiji) in the neck region. Subsequently, ketamine hydrochloride (100 mg/kg; Diichi Sankyo) and xylazine hydrochloride (10 mg/kg; Elanco Japan) were administered intravenously.
Measurements
Body weight was measured before the operation and at 12 weeks afterwards. Blood samples were collected from auricular veins before and at 1 and 12 weeks after the operation, and Mg concentration was analyzed by Fujifilm Vet Systems Co Ltd (Mitaka, Tokyo, Japan).
Radiographic examination
X-ray examination was performed to confirm bone union on the day of sacrifice. Soft tissues, muscles and tendons attached to the bone were removed when imaging. μCT scanning (Scan Xmate-L090H, Comscantecno) was performed to analyze the amount of callus (volumetric amount). Measurement of callus volume was taken from the top edge of the plate to the bottom edge. Filming and image construction was performed by Kureha special laboratory Co Ltd (Iwaki, Fukushima, Japan).
Three-point bending test
Before testing, the plate and screws were removed from the tibia in group T and the screws were removed in group M (as the plate had been biodegraded). The prepared tibia was mounted on a three-point bending test device (Shimadzu, AGS- 5kNX). All bones were loaded with a low strain rate (10 mm/min) until failure, and the ultimate strength (in Newtons) was determined from the load–displacement curve. The bending load was applied to the specimen at the site of the osteotomy and in the sagittal plane.
In vitro osteoblastic differentiation
Human adipose-derived stem cells (ADSCs) were cultured in a culture dish in DMEM containing 10% FBS. After a 5-day incubation, cells were resuspended in osteogenic medium (Osteoblast-Inducer Reagent, Takara Bio Inc.) and seeded in 24-well plates (2.0 × 104 cells per well). Magnesium chloride (MgCl2) solution was added to these culture media and Mg2+ concentration was adjusted to 2.5 or 10 mMOL. Cells growing in MgCl2-free medium served as controls. Culture medium was changed every 4 days. After 13 or 20 days of culture, cells were washed with PBS three times, and fixed in 100% methanol at − 20 °C. After washing with dH2O, cells were stained with Alizarin Red S staining solution (pH6.3). Staining solution was washed away with dH2O, and stained cells were air-dried and observed under a microscope. To quantitate mineralization, Alizarin Red S was extracted in 5% formic acid and assessed for absorbance at 450 nm using an iMark Microplate Absorbance Reader (BIO-RAD). Values were normalized to those seen in untreated samples.
Statistical analysis
All results are reported as the mean ± s.d. Student’s t-test was used to calculate p values. A p value < 0.05 was considered statistically significant (*p < 0.05; **p < 0.01).
Results
The presence of Mg plates significantly increases callus formation
A transverse fracture model was created in the tibial diaphysis of 6-month-old female Japanese white rabbits, and the fracture site was immediately fixed with Mg (group M) or titanium (group T) plates. At 12 weeks postoperatively, rabbit tibiae were harvested and evaluated for gross effects, an analysis that revealed greater callus formation in the M versus the T group (Fig. 2, A and B). The Mg plate was also found to have undergone biodegradation (Fig. 2C).
Fractures fixed by Mg plates exhibit greater callus formation and biodegradability than fractures fixed by titanium plates. Internal fixation was performed on the right tibia of six-month-old female Japanese white rabbits in either the Ti (group T) or Mg (group M) plate groups (7 rabbits each). Twelve weeks later, lower limbs were harvested and observed macroscopically (A and B) and biodegraded Mg plates were removed (C).
Rabbits implanted with Mg plates do not exhibit biotoxicity
The presence or absence of biotoxicity potentially due to Mg plate biodegradation was evaluated by changes in body weight and in blood Mg levels. For this analysis 6-month-old female Japanese white rabbits were modeled with transverse fractures in the tibial diaphysis, fractures were fixed with Mg (group M) or titanium (group T) plates, and body weight was measured before surgery and 12 weeks later. Changes in weight between a preoperative time point and 12 weeks postoperatively were comparable in both groups (Fig. 3A). Blood tests were performed preoperatively, 1 week postoperatively, and 12 weeks postoperatively, and we observed were no significant differences between the two groups in terms of Mg levels at 1 and 12 weeks postoperatively compared to preoperative levels (Fig. 3, B and C).
Rabbits with fractures fixed by Mg plates shown no signs of biotoxicity. Internal fixation was performed on the right tibia of six-month-old female Japanese white rabbits in either the Ti (group T) or Mg (group M) plate groups (7 rabbits each). Body weight of each rabbit was measured preoperatively and 12 weeks later, and changes were monitored (A). Graph shows the mean body weight change ± s.d. at 12 weeks postoperatively relative to preoperative body weight (n = 7, NS, not significant). Peripheral blood was collected preoperatively and at 1 and 12 weeks later, and blood Mg levels were assessed. Graph shows mean changes in blood Mg levels ± s.d. at 1 (B) or 12 (C) weeks postoperatively (PO) relative to preoperative levels (n = 7, NS, not significant).
Use of Mg plates significantly increases callus formation and bone strength
We created the transverse fracture model in the tibial diaphysis of 6-month-old female Japanese white rabbits, and the fracture site was fixed with Mg (M group) or titanium (T group) plates. Bone union was evaluated and confirmed at 12 weeks postoperatively in all animals in both groups by radiographic examination (Fig. 4A). Callus volume (Fig. 4B, highlighted in yellow) was measured by μCT examination at 12 weeks postoperatively. Significantly greater callus formation was observed in the M versus the T group (Fig. 4, B and C). After bone union was confirmed, bone strength at the fracture site was compared at 12 weeks postoperatively. Analysis of the fracture site of the M group indicated significantly increased bone strength relative to contralateral non-fracture bones (Fig. 4D).
Use of a Mg plate enhances callus formation relative to a Ti plate and strengthens bone relative to non-fracture controls. Internal fixation was performed on the right tibia of six-month-old female Japanese white rabbits in either the Ti (group T) or Mg (group M) plate groups (7 rabbits each). Bone union was confirmed 12 weeks later by X-ray analysis of all rabbits (A). Callus formation (B) and volume (C) were analyzed by micro–computed tomography (μCT) 12 weeks after surgery. Callus is highlighted in yellow (B). Graph showing mean callus volume (cm3) ± s.d. in T versus M groups (n = 3, *p < 0.05) (C). Biomechanical strength of bone at fracture union sites of the M group and at contralateral non-fracture sites, as assessed by three-point bending tests at 12 weeks after surgery (D). Graph represents mean peak force at failure (N) ± SD (each n = 4, *p < 0.05) at 12 weeks postoperatively.
Treatment with exogenous Mg promotes osteoblast differentiation in vitro
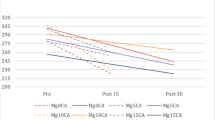
Given that we observed significantly more callus formation in Mg than Ti plates, we conducted Mg addition experiments in an in vitro osteoblast culture system. To do so, we cultured human adipose-derived stem cells (ADSCs) in osteoblast differentiation medium supplemented with different concentrations of Mg and then evaluated calcium deposition in the culture plate by alizarin red staining on days 13 and 20 of culture (Fig. 5A). Alizarin red stain was extracted by formic acid and the amount of calcification was quantitatively based on absorbance. We observed a significant increase in the amount of calcification at Mg concentrations of 2.5 and 10 mMOL on day 13 and at a Mg concentration of 10 mMOL on day 20 compared to controls (Fig. 5, B and C).
Treatment with Mg ions stimulates mineralization of human adipose-derived stem cells (ADSCs). ADSCs were cultured in osteogenic medium in 24-well plates (2.0 × 104 cells per well) in the presence or absence of 2.5 or 10 mMOL Mg2+. Culture medium was changed every 4 days. Alizarin Red S staining was performed on days 13 or 20, and cells were observed microscopically (A). Quantification of Alizarin Red S stain extracted in 5% formic acid in culture wells, based on absorbance at 450 nm using an iMark Microplate Absorbance Reader (BIO-RAD). Values were normalized to those in untreated samples. Data represents mean relative absorbance ± SD at day 13 (B) or 20 (C) (each n = 3, *p < 0.05; **p < 0.01).
Discussion
Treatment of fractures demands strong internal fixation to allow proper repair, accelerate bone union, and maintain fracture stability30. For this reason, for most fractures, titanium metal plates are generally used as fixation materials due to their excellent biocompatibility and high strength17,31,32,33. However, because titanium is not bioabsorbable, a second surgery is generally required to remove the plate after bone union at the fracture site is achieved6,10,11,12,13. This second surgery could be avoided if the metal plate were bioabsorbable. Also, since it is known that the ability to heal fractures decreases in the elderly4, it is desirable to activate callus formation in order to promote bone healing at the fracture site; however, titanium lacks the ability to activate callus formation at a fracture site. Hence, the ideal fixation material for fracture treatment should have the strength to stabilize the fracture and the capacity to activate callus formation but be bioabsorbable, to avoid subsequent surgery. Here, we found that a metal with Mg-based LPSO-type Mg-Zn-Y-Al alloy properties meets these requirements.
In addition to titanium, stainless steel and cobalt chromium are other implant materials used in medical applications. These metals have sufficient strength to stabilize fractures, but are not bioabsorbable and lack callus-forming activity. Mg is bioabsorbable and has osteogenic activity34,35,36,37, but pure Mg is quickly absorbed by the body and is not strong enough to stabilize fracture sites16. Therefore, we created LPSO-type Mg alloys by adding 0.56 at. % Zn, 0.15 at. % Al, and 1.5 at. % Y to pure magnesium and applying the RS process. Kink bands form in the LPSO phase by plastic deformation, dramatically improving mechanical properties. In addition, fine α-Mg and LPSO phases form in RS Mg-Zn-Y-Al alloys. It is likely that kink band formation in the LPSO phase and the fine microstructure formation formed by RS underlie the increased strength shown by RS LPSO-type Mg alloys relative to pure Mg or commercial Mg alloys. It has recently become clear that corrosion resistance of LSPO-type Mg alloys improves as the cooling rate increases during solidification, and optimized Zn addition and inclusion of small amounts of Al further improve strength and corrosion resistance. Indeed, our RS Mg- 0.56Zn- 1.5Y- 0.15 Al alloy exhibited ~ 1.9–2.0 times greater yield strength than does the extruded WE43 alloy commonly used in bioabsorbable medical devices (data not shown), suggesting that our alloy could be used to create implant material to treat long bone fracture in humans, a possibility considered impossible until now. Although the strength of our Mg-Zn-Y-Al alloy is still not as great as that of titanium (data not shown), the bioabsorbable and radiolucent properties of pure Mg are maintained in our Mg-Zn-Y-Al alloy without severe adverse events, such as weight loss or even death. We believe these benefits suggest use of our Mg-Zn-Y-Al alloy rather than pure magnesium. Indeed, the LPSO-type Mg-Zn-Y-Al alloy used here is bioabsorbable but is not absorbed until sufficient bone healing is achieved, and it strongly activates callus formation at fracture sites. We found that bone strength at a fracture site treated using this material was significantly higher than that of the intact contralateral bone without fracture.
There are no reports of harmful effects of using aluminum implants in humans over the complete degradation phase. Absorption by the body of a large amount of aluminum reportedly causes acute toxicity in mammals, but the 50% lethal dose (LD50) after a single administration to animals is 2–4 g/kg body weight38. Implantation of ~ 0.2 g of Mg-Zn-Y-Al alloy does not reach this value (0.05 g/kg body weight in rabbits), and since Mg-Zn-Y-Al alloy degrades gradually, there is almost no possibility of acute toxicity. As for continuous intake of aluminum, there is one report that rabbits administered 1.8 g/day dietary aluminum daily showed some weight loss39. However, aluminum in the alloy used here was only 0.15 at. % of total elements, an extremely small amount. Also, we observed no adverse events such as death or weight loss in rabbits implanted with this Mg alloy. Thus, we believe that toxicity is minimal.
Mg is an essential element, and its deficiency causes tremor, tetany, and convulsions40,41,42. On the other hand, there are no known cases of poisoning due to Mg excess43. The mechanism of Mg-induced activation of callus formation is not fully understood. Bone healing is generally known to be a process of endochondral ossification, in which cartilage is formed and then replaced by bone44. Periosteal cells also migrate to the fracture site to promote bone healing45. In this study, Mg significantly stimulated osteoblast differentiation and calcium deposition in an osteoblast differentiation system composed of mesenchymal stem cells in vitro, suggesting that Mg directly promotes bone formation at fracture sites. As noted in the Introduction section, neither Zn, Y, nor Al was added to improve biocompatibility. Instead, we added those materials to improve strength and corrosion resistance. Indeed, we could not confirm activation of bone formation with either 0.56Zn, 1.5Y or 0.15 Al at.% compared to 97.79 Mg at.% (Supplementary Fig. 1). One experimental limitation, however, is that Y was not in solution.
Generally, two-phase alloys promote galvanic corrosion due to the potential difference between the matrix and the phases. However, the LPSO phase of this RS Mg-Zn-Y-Al alloy is finely dispersed. Therefore, our alloy exhibited good corrosion resistance. We also believe that its necessary mechanical properties will be maintained until treatment completion of the fractures because we did not see any fracture healing failures in our experiments. Here, to evaluate issues relevant to fracture treatment potentially due to differences in plate material, and because we constructed the plate from our magnesium alloy, we used ready-made Ti screws. Therefore, we believe that we were able to evaluate the difference in fracture treatment effect due to the difference in the material of the plate. Moreover, differences in mechanical properties highly influence the healing process in the case of fractures. Indeed, Young’s modulus of our Mg-Zn-Y-Al alloy is equivalent to pure Mg, but lower than titanium (data not shown). Moreover, relative to the titanium value, Young’s modulus of magnesium and its alloys is closer to that of bone (data not shown), a property that likely prevents stress shielding and may promote bone formation.
Mg implants in the body reportedly react with water to produce Mg(OH)2 and gas, making formation of hydrogen gas pockets problematic in some cases. Here, we did not assess potential formation of hydrogen gas pockets because tibiae of rabbits implanted with our magnesium alloy were removed prior to micro-CT evaluation. Therefore, in this study, we assessed hydrogen gas generation by ultrasonography. Compared to titanium plates, we observed no evidence of a hydrogen gas reservoir in Mg-Zn-Y-Al-alloy (Supplementary Fig. 2). Nonetheless, when used as implants, our magnesium alloys may generate hydrogen gas as they undergo degradation in an aqueous environment. We note that Mg-Zn-Y-Al-alloy clearly enhances bone formation; thus, we conclude that generation of small amounts of hydrogen gas in this context is not toxic, at least locally. Future analysis is, however, required to confirm whether this is the case.
Mg is radiolucent, and clinicians may find it is easy to check the fracture site by X-ray examination, even during plate fixation46. The screws used in this study were made of titanium, but it is thought that the fracture site can be more easily confirmed by radiographic examination if the screws are also made of Mg. Mg is also not magnetic, providing an advantage for patients who require MRI scans. Thus, MRI scans to evaluate various comorbidities other than fractures, such as lumbar spinal canal stenosis, would be possible. Overall, based on evidence provided here, LPSO-type Mg-Zn-Y-Al alloys represent a promising metallic material for use in future fracture treatment.
Conclusion
In summary, a plate with a Mg alloy containing zinc, yttrium and aluminum with LPSO structure was developed for fracture treatment. As bone fracture treatment, plates made of this Mg alloy have sufficient strength to fix and stabilize a fracture site. Mg plates also promote osteogenesis at the fracture site. Magnesium significantly also stimulates calcium deposition in an in vitro osteoblast culture system, suggesting that it directly activates osteoblast bone formation. Mg plates are bioabsorbable, and once bone union is achieved, a significant portion is absorbed. Mg plates are also radiolucent, allowing X-ray examination of the fracture site even during fracture fixation. These properties are relevant to clinical concerns of patients with reduced fracture healing capacity, such as the elderly, individuals who want to accelerate bone healing, and patients who wish to avoid a second surgery to remove the plate. This work will provide an innovative paradigm for further research related to various uses of Mg alloy.
Data availability
The data that support the findings of this study are available from the corresponding author, TM, upon reasonable request.
References
Cheung, W. H., Miclau, T., Chow, S. K., Yang, F. F. & Alt, V. Fracture healing in osteoporotic bone. Injury 47(Suppl 2), S21-26 (2016).
Irgebay, Z., Kahan, E. H., Park, K. E., Choi, J. & Zellner, E. G. Characteristics and patterns of facial fractures in the elderly population in the united states based on Trauma quality improvement project data. J. Craniofac. Surg. 33, 1294–1298 (2022).
Burge, R. et al. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J. Bone Miner. Res. 22, 465–475 (2007).
Foulke, B. A., Kendal, A. R., Murray, D. W. & Pandit, H. Fracture healing in the elderly: A review. Maturitas 92, 49–55 (2016).
Dent, E., Daly, R. M., Hoogendijk, E. O. & Scott, D. Exercise to prevent and manage frailty and fragility fractures. Curr. Osteoporos. Rep. 21, 205–215 (2023).
Aspenberg, P. et al. Teriparatide for acceleration of fracture repair in humans: a prospective, randomized, double-blind study of 102 postmenopausal women with distal radial fractures. J. Bone Miner. Res. 25, 404–414 (2010).
Yates, J. et al. Jones fracture of the fifth metatarsal: Is operative intervention justified? A systematic review of the literature and meta-analysis of results. Foot (Edinb). 25, 251–257 (2015).
Fletcher, J. W. A. et al. Intracapsular femoral neck fractures-a surgical management algorithm. Medicina (Kaunas) 57, 791 (2021).
Virtanen, K. J., Malmivaara, A. O., Remes, V. M. & Paavola, M. P. Operative and nonoperative treatment of clavicle fractures in adults. Acta. Orthop. 83, 65–73 (2012).
Tsai, S. W. et al. Risk factors for refracture after plate removal for midshaft clavicle fracture after bone union. J. Orthop. Surg. Res. 14, 457 (2019).
Gyuricza, C. et al. Removal of locked volar plates after distal radius fractures. J. Hand. Surg. Am. 36, 982–985 (2011).
Busam, M. L., Esther, R. J. & Obremskey, W. T. Hardware removal: Indications and expectations. J. Am. Acad. Orthop. Surg. 14, 113–120 (2006).
Park, J. B. & Kim, Y. K. Metallic Biomaterials Biomaterials 1–1–1–22 (CRC press, 2007).
Kamrani, S. & Fleck, C. Biodegradable magnesium alloys as temporary orthopaedic implants: A review. Biometals 32, 185–193 (2019).
Radha, R. & Sreekanth, D. Insight of magnesium alloys and composites for orthopedic implant applications – a review. J. Magnes. Alloy. 5, 286–312 (2017).
Staiger, M. P., Pietak, A. M., Huadmai, J. & Dias, G. Magnesium and its alloys as orthopedic biomaterials: A review. Biomaterials 27, 1728–1734 (2006).
Niinomi, M., Nakai, M. & Hieda, J. Development of new metallic alloys for biomedical applications. Acta. Biomater. 8, 3888–3903 (2012).
González, S., Pellicer, E., Suriñach, S., Baró, M. D. & Sort, J. Biodegradation and Mechanical Integrity of Magnesium and Magnesium Alloys Suitable for Implants. In Biodegradation, Ch. 12 (eds, Rolando, C. & Francisca, R.) (IntechOpen, 2013).
Choudhary, L. & Singh Raman, R. K. Magnesium alloys as body implants: Fracture mechanism under dynamic and static loadings in a physiological environment. Acta. Biomater. 8, 916–923 (2012).
Lambotte, A. L’utilisation du magnesium comme materiel perdu dans l’osteosynthèse. Bull. Mem. Soc. Nat. Chir. 28, 1325–1334 (1932).
Witte, F. et al. In vivo corrosion of four magnesium alloys and the associated bone response. Biomaterials 26, 3557–3563 (2005).
Yoshimoto, S., Yamasaki, M. & Kawamura, Y. Microstructure and mechanical properties of extruded Mg-Zn-Y alloys with 14H Long period ordered structure. Mater. Trans. 47, 959–965 (2006).
Kawamura, Y. & Yoshimoto, S. High strength Mg-Zn-Y alloys with LPSO structure (2005).
Kawamura, Y. & Yamasaki, M. Formation and mechanical properties of Mg97Zn1RE2 alloys with long-period stacking ordered structure. Mater. Trans. 48, 2986–2992 (2007).
Kawamura, Y., Hayashi, K., Inoue, A. & Masumoto, T. Rapidly solidified powder metallurgy Mg97Zn1Y2 alloys with excellent tensile yield strength above 600 MPa. Mater. Trans. 42, 1172–1176 (2001).
Drozdenko, D. et al. Optimization of mechanical properties of dilute Mg-Zn-Y alloys prepared by rapid solidification. Mater. Des. 181, 107984 (2019).
Izumi, S., Yamasaki, M. & Kawamura, Y. Improvement of corrosion resistance of extruded Mg-Zn-Y Mg/LPSO two-phase alloys by fourth element addition. Mater. Sci. Forum. 654–656, 767–770 (2010).
Yamasaki, M., Shi, Z., Atrens, A., Furukawa, A. & Kawamura, Y. Influence of crystallographic orientation and Al alloying on the corrosion behaviour of extruded α-Mg/LPSO two-phase Mg-Zn-Y alloys with multimodal microstructure. Corros. Sci. 200, 110237 (2022).
Yamasaki, M., Izumi, S., Kawamura, Y. & Habazaki, H. Corrosion and passivation behavior of Mg–Zn–Y–Al alloys prepared by cooling rate-controlled solidification. Appl. Surf. Sci. 257, 8258–8267 (2011).
Augat, P. & von Rüden, C. Evolution of fracture treatment with bone plates. Injury 49(Suppl 1), S2-s7 (2018).
Marin, E. & Lanzutti, A. Biomedical applications of titanium alloys: A comprehensive review. Materials (Basel) 17, 114 (2023).
Eriksson, C. et al. Callus formation and remodeling at titanium implants. J. Biomed. Mater. Res. A. 83, 1062–1069 (2007).
Leventhal, G. S. Titanium, a metal for surgery. J. Bone Joint. Surg. Am. 33-a, 473–474 (1951).
He, W., Zhang, H. & Qiu, J. Osteogenic effects of bioabsorbable magnesium implant in rat mandibles and in vitro. J. Periodontol. 92, 1181–1191 (2021).
Yu, Y. et al. Multifunctions of dual Zn/Mg ion co-implanted titanium on osteogenesis, angiogenesis and bacteria inhibition for dental implants. Acta. Biomater. 49, 590–603 (2017).
Choi, S. et al. Biochemical activity of magnesium ions on human osteoblast migration. Biochem. Biophys. Res. Commun. 531, 588–594 (2020).
He, L. Y., Zhang, X. M., Liu, B., Tian, Y. & Ma, W. H. Effect of magnesium ion on human osteoblast activity. Braz. J. Med. Biol. Res. 49, 7 (2016).
Luckey, T. D. & Venugopal, B. Toxicologic significance of the physicochemical properties of metals. In Physiologic and Chemical Basis for Metal Toxicity, (eds, Luckey, T. D. & Venugopal, B.) 103–128 (Springer US, 1977).
Schneider, H. J. et al. Effect of drugs used for the prevention of urinary calculi recurrence on the growth and metabolism of young experimental animals. Z. Urol. Nephrol. 72, 237–247 (1979).
Gröber, U., Schmidt, J. & Kisters, K. Magnesium in prevention and therapy. Nutrients 7, 8199–8226 (2015).
Saris, N.-E.L., Mervaala, E., Karppanen, H., Khawaja, J. A. & Lewenstam, A. Magnesium: An update on physiological, clinical and analytical aspects. Clin. Chim. Acta 294, 1–26 (2000).
Okuma, T. Magnesium and bone strength. Nutrition 17, 679–680 (2001).
Van Laecke, S. Hypomagnesemia and hypermagnesemia. Acta. Clin. Belg. 74, 41–47 (2019).
Kronenberg, H. M. Developmental regulation of the growth plate. Nature 423, 332–336 (2003).
Wang, T., Zhang, X. & Bikle, D. D. Osteogenic differentiation of periosteal cells during fracture healing. J. Cell Physiol. 232, 913–921 (2017).
Herber, V. et al. Can hardware removal be avoided using bioresorbable Mg-Zn-Ca screws after medial malleolar fracture fixation? mid-term results of a first-in-human study. Injury 53, 1283–1288 (2022).
Acknowledgements
No funds, grants, or other support was received.
Author information
Authors and Affiliations
Contributions
KT, MY, YK, TM (Miyamoto) designed research; KT, TM (Miyamoto), SU performed research; KT, MY, TM (Miyamoto) performed the data collection, formal analysis, and visualization.; KT, MY, SK, TK, YU, TM (Masuda), TN, TT, SH, KS, RY, KI, YF, MU TA, JK, KM, NY, HM, YK, ST, MS, YS, MT, ST, HG, MY, YT, SI, RK, RT, XT, FH, TM (Miyamoto) analyzed data.; KT, MY, SI, YK, TM (Miyamoto) wrote the paper. All the authors contributed to the investigation, methodology, validation, and writing – review & editing. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Takata, K., Yugami, M., Karata, S. et al. Plates made from magnesium alloy with a long period stacking ordered structure promote bone formation in a rabbit fracture model. Sci Rep 15, 12210 (2025). https://doi.org/10.1038/s41598-025-96853-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-96853-3