Abstract
To validate the efficacy and safety of thymosin α-1 combined with lenvatinib plus sintilimab in the treatment of unresectable hepatocellular carcinoma. Patients with unresectable hepatocellular carcinoma treated with lenvatinib plus sintilimab at the People’s Hospital of Guangxi Zhuang Autonomous Region from January 2020 to June 2022 were retrospectively analyzed. The patients were divided into an experimental group and a control group based on their therapeutic regimens: thymosin α-1 plus lenvatinib and sintilimab (experimental group), and lenvatinib plus sintilimab (control group). The primary endpoints were overall survival and progression-free survival. Tumor response was evaluated according to mRECIST criteria, and the partial response, complete response, stable disease, progressive disease, object response rate, and disease control rate of the two groups were compared. Adverse events were evaluated using the Common Terminology Criteria for Adverse Events version 5.0. The median overall survival of all patients was 13.0 months (95% CI 10.587–15.413). The experimental group had a longer median overall survival than the control group (16 months vs. 11 months, P = 0.018). The median progression free survival of all patients was 5.0 months (95% CI 3.721–6.279). The experimental group had a longer median progression-free survival than the control group (7 months vs. 4 months, P = 0.006). The objective response rate of the experimental group was 55.8% (24/43), and of the control group’s 34.7% (17/49) (P = 0.042). The disease control rate of the experimental group was 76.7% (33/43), while the control group had a rate of 59.2% (29/49) (P = 0.073). There was no significant difference in the incidence of grade 1–2 adverse events or grade 3–4 adverse events between the two groups (P > 0.05). Thymosin α-1 combined with lenvatinib plus sintilimab is an effective and safe therapeutic regimen in unresectable hepatocellular carcinoma.
Similar content being viewed by others
Introduction
Primary liver cancer is a malignant tumor with a high incidence worldwide. The latest data show that there will be 906,000 new liver cancer cases and 830,000 deaths worldwide in 2020, ranking sixth and third in morbidity and mortality1. Moreover, since 2000, the incidence of primary liver cancer has continued to increas2, so there is still great pressure on the treatment of liver cancer. Due to the insidious onset of liver cancer, most patients are already in the mid-to-late stage when discovered and have lost the chance for radical surger3,4. In recent years, with the development of systemic therapeutic drugs and in-depth clinical research, targeted therapy combined with immunotherapy has become a key transformational treatment method for patients with unresectable liver cancer. Zhang et al.5 found that the conversion therapy regimen of nivolumab combined with cabozantinib in the treatment of intermediate and advanced liver cancer had an objective response rate of 42% and a successful conversion surgery rate of 80%, which greatly improved the prognosis of advanced liver cancer patient. The results of the IMbrave150 study showed that the median overall survival (OS) of the atezolizumab combined with bevacizumab (T + A) regimen in the treatment of unresectable liver cancer reached 19.2 months, and the median progression-free survival (PFS) reached 6.9 months, which was better than that of sorafenib alone6. Other clinical studies, including ORIENT-32 and RESCUE, have also achieved promising results7,8. Although more clinical studies are being carried out and the targeted therapy combined with immunotherapy options are growing steadily, according to current clinical research results, the objective response rate of most systemic treatment options is 20–50%9, which is far from satisfactory. Improving the effectiveness of targeted therapy combined with immunotherapy drugs is a very important research direction.
Thymosin α-1 is a nonspecific immunotherapy drug that enhances the antitumor immunity by promoting the maturation and differentiation of T cells and increasing the secretion of interferons, interleukins and other cytokines. Linye et al.10 showed that the prophylactic use of thymosin α-1 after hepatocellular carcinoma surgery substantially prolonged OS and PFS. Recent research by Wei et al.11 found that thymosin α-1 can promote the transformation of tumor-associated macrophages from the M2 type to the M1 type by participating in the regulation of macrophage efferocytosis, thereby reversing the tumor immunosuppression state and enhancing antitumor effect. Therefore, from the perspective of the mechanism, thymosin α-1 combined with chemotherapy or tumor immunotherapy, such as PD-1/PD-L1 and CD47, may have clinical application value. Danielli et al.12 reviewed the treatment records of melanoma patients in phase II trials and expanded-access programs and calculated the median survival rate of patients who received thymosin α-1 before CTLA-4 inhibitor treatment and those who did not receive thymosin. The survival times were 38.4 months and 8.0 months respectively, confirming that thymosin combined with CTLA-4 inhibitor has a synergistic effect. There are no research reports on whether thymosin has a synergistic effect with targeted therapy combined with immunotherapy for hepatocellular carcinoma. Therefore, our center retrospectively analyzed clinical data of unresectable hepatocellular carcinoma patientis aimed to validate the efficacy and safety of thymosin α-1 combined with lenvatinib plus sintilimab in the treatment of unresectable hepatocellular carcinoma.
Methods
Study design and patients
This is a single center retrospective cohort study that collected the data of patients with unresectable hepatocellular carcinoma who were hospitalized in the People’s Hospital of Guangxi Zhuang Autonomous Region from January 2020 to June 2022 and were treated with lenvatinib combined with sintilimab. Inclusion criteria: (1) histologically confirmed hepatocellular carcinoma; (2) ECOG-PS score 0–1; (3) Child–Pugh liver function classification A or B; (4) Barcelona Clinic liver cancer (BCLC) stage B or C; and (5) no previous systemic or local antitumor treatment and at least one measurable tumor lesion according to mRECIST. The exclusion criteria were as follows: (1) autoimmune diseases or previous systemic or local antitumor treatment; (2) other primary malignant tumors; and (3) follow-up time ≤ 6 months or incomplete follow-up data. All included patients were divided into two groups according to whether they used thymosin α-1 at the same time: the experimental group (lenvatinib + sintilimab + thymosin α-1) and the control group (lenvatinib + sintilimab).
Treatment methods
All patients took lenvatinib 8 mg (body weight ≤ 60 kg) or 12 mg (body weight > 60 kg) orally, once a day, and sintilimab 200 mg intravenously, once every 3 weeks. Patients in experimental group were also injected with thymosin α-1 (1.6 mg) subcutaneously on the first day of treatment, twice a week. Patients received corresponding treatment until unacceptable side effects occurred or death led to loss to follow-up or treatment cessation. If the unequivocal disease progression was absent, indicated by signs and symptoms and there was definite evidence of clinical benefit observed by investigators, patients could continue treatment beyond disease progression.
Follow-up and assessments
From the beginning of drug treatment, reexamination and follow-up should be carried out every four weeks. The review included chest CT, abdominal multiphase enhanced CT or MRI, liver function, kidney function, blood routine, coagulation function, electrolytes, alpha-fetoprotein (AFP) and protein induced by vitamin K absence II (PIVKA-II). Tumor control was assessed under mRECIST criteria. The incidence and severity of adverse events were monitored and assessed using the National Cancer Institute Common Terminology Criteria for Adverse Events 5.0. The primary endpoints were overall survival (OS) and progression free survival (PFS), and the secondary endpoints were object response rate (ORR), disease control rate (DCR) and treatment-related adverse events. When patients experienced disease progression or discontinued treatment, their overall survival is monitored every 30 days until they die, lost contact and the study ended.
Statistical analysis
Efficacy assessments were performed on all treated patients. Measurement data are expressed as the mean ± standard deviation and compared using the independent sample T test (normal distribution) or the Mann–Whitney U test (abnormal distribution), and count data were compared using the chi-square test. PFS and OS were estimated using the Kaplan–Meier method. Prognostic factors were first evaluated using univariate Cox regression analysis. Multivariate Cox regression analysis was used to evaluate the significant factors (p < 0.05) identified in the univariate Cox regression analysis. Descriptive statistics were used to describe the adverse event outcomes. All analyses were performed using Statistical Package for the Social Sciences (SPSS) version 26 (IBM, Armonk, NY, USA).
Results
Baseline characteristics
Between January 2020 and June 2022, a total of 92 patients who met the study criteria were included, with 43 patients in the experimental group (lenvatinib + sintilimab + thymosin α-1) and 49 patients in the control group (lenvatinib + sintilimab). The average age of all patients was 53.3 ± 11.8 years old, and there were 80 male patients. There was no significant difference in general traits such as sex, age, ECOG-PS score, Child–Pugh classification, and BCLC stage between the two groups (Table 1).
Effectiveness
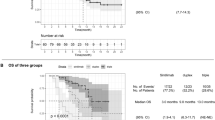
By the end of December 31, 2023, the shortest survival time of all patients was 3.0 months, the longest survival time was 23.0 months, and the median overall survival was 13.0 months (95% CI 10.587–15.413) (Fig. 1A). At the end of follow-up, 44 patients (47.8%) had died. The median overall survival time of the experimental group was 16.0 months (95% CI 13.767–18.233), and that of the control group was 11.0 months (HR = 0.470, 95% CI 0.252–0.879). It was significantly longer than that of the control group (P = 0.018) (Fig. 1B). A total of 68 patients (73.9%) experienced disease progression, and the median progression-free survival time was 5.0 months (95% CI 3.721–6.279) (Fig. 2A). The median progression-free survival time in the experimental group was 7.0 months (95% CI 3.229–10.771), and that of the control group was 4.0 months (HR = 0.482, 95% CI 0.286–0.814) (P = 0.006) (Fig. 2B).
Kaplan–Meier analysis of overall survival. (A) All patients’ Kaplan–Meier analysis of overall survival (OS) are shown, according to modified response evaluation criteria in solid tumors. Median OS is 13.0 months (95% CI 10.587–15.413). (B) Kaplan–Meier estimates of OS among experimental group and control group are shown. P-value calculated is < 0.05.
Kaplan–Meier analysis of progression free survival. (A) All patients’ Kaplan–Meier analysis of progression free survival (PFS) are shown, according to modified response evaluation criteria in solid tumors. Median PFS is 5.0 months (95% CI 3.721–6.279). (B) Kaplan–Meier estimates of PFS among experimental group and control group are shown. P-value calculated is < 0.05.
According to the mRECIST assessment of tumor response, a total of 34 patients had partial response (PR), 7 patients had complete response (CR), 21 patients had stable disease (SD), and 30 patients had disease progression (PD). 20 patients (46.5%) in the experimental group and 14 patients (28.6%) in the control group had PR (P = 0.075). 4 people (9.3%) in the experimental group had CR and 3 people (6.1%) in the control group had CR (P = 0.702). The objective response rate (ORR) of the experimental group was 55.8% (24/43) and that of the control group was 34.7% (17/49) (P = 0.042). The disease control rate of the experimental group was 76.7% (33/43) and that of the control group was 59.2% (29/49) (P = 0.073) (Table 2).
Prognostic factors
We included sex, age, ECOG-PS score, Child–Pugh classification, BCCL stage, therapeutic regimen, drinking history, Concomitant disease, HBsAg, HBV-DNA, degree of differentiation, microvascular invasion, extrahepatic metastasis, esophageal and gastric varices, portal hypertension, large vessel invasion, alanine aminotransferase (ALT), total bilirubin (TB), prothrombin time (PT), international normalized ratio (INR), PIVKA-II, AFP in the univariate analysis of OS and PFS. Univariate analysis showed that BCLC stage (B vs. C), therapeutic regimen (control vs. experimental), tumor differentiation (poorly vs. well and moderately), extrahepatic metastasis (yes vs. no), total bilirubin (≤ 20 µmol/L vs. > 20 µmol/L), PT (≤ 16 s vs. > 16 s), AFP (≤ 200 ng/ml vs. > 200 ng/ml) were significantly associated with OS. Therefore, therapeutic regimen (control vs. experimental), PT (≤ 16 s vs. > 16 s) and AFP (≤ 200 ng/ml vs. > 200 ng/ml) were associated with PFS (Table 3). When these factors above were included into the multivariate analyses of OS and PFS, BCLC stage (B vs. C) (HR = 0.366; 95% CI 0.143–0.934; P = 0.036), total bilirubin (≤ 20 µmol/L vs. > 20 µmol/L) (HR = 0.421; 95% CI 0.210–0.844; P = 0.015), AFP (≤ 200 ng/ml vs. > 200 ng/ml) (HR = 0.479; 95% CI 0.234–0.979; P = 0.043) were independent factors affecting the OS of patients with unresectable hepatocellular carcinoma (Table 4; Fig. 3A), and PT (≤ 16 s vs. > 16 s) ( HR = 0.496; 95% CI 0.303–0.812; P = 0.005), therapeutic regimen (control vs. experimental) (HR = 0.567; 95% CI 0.340–0.945; P = 0.029) were independent factors affecting their PFS (Table 5, Fig. 3B).
Safety
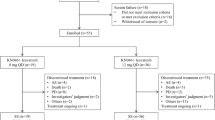
The most common treatment-related adverse events among all patients were alanine transaminase (ALT) elevation in 41 cases (45%), hypertension in 35 cases (38%), thrombocytopenia in 32 cases (35%), fatigue in 32 cases (35%), diarrhea in 31 cases (34%), proteinuria in 29 cases (32%), and anemia in 27 cases (29%). The most common grade 3–4 treatment-related adverse events were hypertension in 6 cases, thrombocytopenia in 5 cases, nausea in 3 cases, fatigue in 3 cases, diarrhea in 2 cases, pruritus in 2 cases, neutropenia in 2 cases, blood bilirubin increase in 2 cases, and proteinuria in 2 cases. There was no significant difference between patients in the experimental group and the control group in the incidence of grade 1–2 treatment-related adverse events, grade 3–4 treatment-related adverse events, or treatment-related adverse events overall. None of the patients included in this study discontinued treatment due to adverse events, which were all controlled through dose adjustment or symptomatic treatment (Table 6).
Discussion
In this retrospective study, we compared the efficacy and safety of lenvatinib plus sintilimab and thymosin α-1 with lenvatinib plus sintilimab in patients with unresectable hepatocellular carcinoma. The results showed that the experimental group was significantly better than the control group in OS, PFS and ORR, and there was no significant difference between the two groups in the incidence of adverse events.
Most patients with liver cancer have lost the opportunity for surgery when they seek treatment. For patients with intermediate and advanced liver cancer who cannot receive radical surgical treatment, only systemic treatment can be attempted. Their 5-year survival rate is only 10–1813. Their is still much room for improvement in the treatment of these patients. Carrying out relevant research on this group of patients and enriching the treatment methods for these patients will be key to improving the overall prognosis of patients with hepatocellular carcinoma.
In recent years, various treatments, such as tyrosine kinase inhibitors (TKI), immune checkpoint inhibitors (ICI), CART immunotherapy, radiotherapy, and interventional therapy (transcatheter arterial chemoembolization and hepatic artery infusion chemotherapy), have brought new hope to patients with intermediate and advanced liver cancer, especially tyrosine kinase inhibitors and immune checkpoint inhibitors. Although targeted therapy combined with immunotherapy is the current mainstream treatment method, the effectiveness of most treatment plans is not high. Lenvatinib plus pembrolizumab is a treatment method with a relatively high ORR, but even this is only 46%14. How to maximize the effectiveness of existing drugs is a clinical issue that requires attention.
Although our study was a single-center retrospective study, its results are encouraging. Our results show that the median OS of the experimental group was 16.0 months (95% CI 13.767–18.233) and that of the control group was 11.0 months (95% CI 7.142–14.858) (P = 0.018). The median PFS in the experimental group was 7.0 months (95% CI 3.229–10.771) and that of the control group was 4.0 month (95% CI 2.766–5.234) (P = 0.006). The median OS of the T + A regimen in the IMbrave15 reached 19.2 months6, and the median OS of lenvatinib plus pembrolizumab in the LEAP-00 reached 21.1 months15. Our OS was shorter, although the comparison of such different studies may not be scientific. First, our study was a retrospective study and may have had some resulting biases. Second, the proportion of our patients who had an ECOG-PS score of 1 point was 65.2% because the indications for the studied medications are relatively broad, and the proportion of patients with Child–Pugh scores of 8–9 was relatively high. These factors may have affected our overall patient OS. Because thymosin α-1 has an anti-hepatitis B virus effect, we also considered whether the significant results in OS and PFS were obtained due to its antiviral effect. Therefore, we conducted a univariate analysis on HBsAg and HBV-DNA, and the results showed that they were not factors affecting OS or PFS. At the same time, all patients included in the study, as long as they are HBsAg positive, received antiviral treatment, and the HBV-DNA of all patients returned to normal within one month after standard antiviral treatment. Therefore, we believe that thymosin α-1 may improve the therapeutic effect in cancer patients by enhancing the antitumor effect of targeted drugs and immunotherapy drugs. Danielli R et al. found that thymosin α-1 enhanced the effect of CTLA-4 inhibitors in the treatment of melanoma. Our results and theirs both show the role of thymosin α-1 in enhancing the antitumor effect of targeted drugs and immunotherapy drugs12.
According to the mRECIST criteria, the experimental group had 20 people (46.5%) reach PR and 4 people (9.3%) reach CR, the control group had 14 people (28.6%) reach PR and 3 people (6.1%) reach CR. Although patients in both groups had no significant difference in PR or CR, the ORR of the experimental group was 55.8% (24/43), and the ORR of the control group was 34.7% (17/49) (P = 0.042). Finn RS reported that the ORR of lenvatinib combined with pembrolizumab was 46%14. This is a relatively high ORR of targeted therapy combined with immunotherapy in a current study. The ORR of our study is 55.8%. A preliminary cross-sectional comparison of ours studies have achieved a relatively high ORR. TKIs can reduce the percentage of immunosuppressive regulatory T cells and myeloid-derived suppressor cells and increase T-cell infiltratio16,17, while ICIs need to work under conditions of T-cell infiltratio18, and the combination of the two treatment methods can produce a synergistic antitumor effect. The tumor immunosuppressive microenvironment is an important reason for PD-1 resistance19, and tumor-associated macrophages are the key to the tumor immune microenvironment, and are divided into the M1 type and M2 type. M2-type macrophages participate in tumor growth, angiogenesis, metastasis and invasion by secreting growth factors and cytokines. They can also inhibit the metabolism and function of T-cells by releasing immunosuppressive cytokines. The above is one of the important mechanisms of the creation of a tumor immunosuppressive microenvironmen20,21. Thymosin α-1 can reverse the polarization of the M2 type of tumor-associated macrophages and promote their transformation to the M1 type. This enhances the body’s antitumor abilit while inhibiting the release of immunosuppressive factors such as IL-10 and improving the immunosuppressive microenvironment11. Therefore, from a mechanistic perspective, thymosin α-1 combined with targeted therapy and immunotherapy can enhance their efficacy, and our results also support this hypothesis at the clinical level. Currently, in clinical work, the more mainstream treatment option for unresectable hepatocellular carcinoma is interventional therapy combined with targeted therapy and immunotherapy. whether thymosin α-1 combined with interventional therapy, radiotherapy or chemotherapy still effective remains unclear. Further research is needed to confirm this hypothesis.
Our univariate analysis showed that BCLC stage (B vs. C), therapeutic regimen (control vs. experimental), tumor differentiation (poorly vs. well and moderately), extrahepatic metastasis (yes vs. no), total bilirubin (≤ 20 µmol/L vs. > 20 µmol/L), PT (≤ 16 s vs. > 16 s), AFP (≤ 200 ng/ml vs. > 200 ng/ml) were associated with OS. Therapeutic regimen (control vs. experimental), PT (≤ 16 s vs. > 16 s) and AFP (≤ 200 ng/ml vs. > 200 ng/ml) were associated with PFS. When these factors were included in the multivariate analyses of OS and PFS, BCLC stage (B vs. C) (HR = 0.366; 95% CI 0.143–0.934; P = 0.036), total bilirubin (≤ 20 µmol/L vs. > 20 µmol/L) (HR = 0.421; 95% CI 0.210–0.844; P = 0.015), AFP (≤ 200 ng/ml vs. > 200 ng/ml) (HR = 0.479; 95% CI 0.234–0.979; P = 0.043) were independent factors affecting the OS of patients with unresectable hepatocellular carcinoma, and PT (≤ 16 s vs. > 16 s) (HR = 0.496; 95% CI 0.303–0.812; P = 0.005), therapeutic regimen (control vs. experimental) (HR = 0.567; 95% CI 0.340–0.945; P = 0.029) were independent factors affecting the PFS of patients with unresectable hepatocellular carcinoma. Multivariate analyses of OS showed no significance of therapeutic regimen. To further explore the reason of no significance in the multivariate analysis of the treatment regimen, we removed the treatment regimen and conducted a multivariate analysis, then compared the results of the two multivariate analyses. We found that the most affected were BCLC stages and AFP, indicating that treatment regimen have multicollinearity with BCLC stages and AFP, and their contribution to the model is not entirely unique. Furthermore, considering small sample size of this study, the statistical power may be insufficient. Therefore, the results of the multivariate analysis (treatment regimen, p = 0.101) should not be considered definitive conclusions. Ding reported that AFP was an independent factor affecting the OS of advanced liver cancer, in line with our results22. However, Dai reported that PT is an independent factor affecting overall survival in advanced liver cancer23, inconsistent with our results. We believe that prothrombin time is an indicator of exogenous coagulation function. Coagulation function is regulated by many factors and does not well reflect the load of tumors and liver. On the other hand, our results show that bilirubin was an independent prognostic factor for OS of advanced hepatocellular carcinoma. We believe that total bilirubin can more intuitively reflect the load of the liver, thereby affecting many subsequent treatment measures.
Although we have added thymosin α-1 to lenvatinib and sintilimab, there was no significant increase in either grade 1–2 or grade 3–4 treatment-related adverse events. The three most common grade 1–2 adverse events in the experimental group were increased ALT, thrombocytopenia, and proteinuria. The three most common grade 3–4 adverse events in the experimental group were proteinuria, thrombocytopenia, and hypertension. The three most common grade 1–2 adverse events in the control group were increased ALT, fatigue, and hypertension. The three most common grade 3–4 adverse events in the control group were hypertension, thrombocytopenia, fatigue, increased bilirubin, and nausea. Notably, there was no significant difference in the occurrence of these adverse events between the two groups. Thymosin is an endogenous peptide known for its immunomodulatory activity. It is believed that thymosin does not increase adverse events in the body. Rengga et al. discovered that thymosin α-1 can effectively prevent immunodeficiency pathology in the intestine by promoting the indoleamine 2,3-dioxygenase (IDO) 1-dependent tolerance immune pathway, ultimately reducing immune enteritis caused by CTLA-4 inhibitors24. However, our study did not demonstrate the advantage of thymosin in reducing adverse events. This may be attributed to the small number of cases and the potential bias inherent to retrospective studies. Further in-depth research is needed to investigate the role of thymosin in reducing adverse events to systemic treatment.
There were several limitations in this study. First, it was a single center retrospective study with a limited sample size and a short follow-up period, which may lead to bias. Nonetheless, our findings show the promise of thymosin α-1 combined with targeted therapy and immunotherapy. In the future, we hope to conduct a larege, multicenter, prospective, randomized controlled study to further evaluate the effect of thymosin α-1 on targeted therapy combined with immunotherapy and even interventional therapy and chemotherapy.
In conclusion, our findings indicate that thymosin α-1 combined with lenvatinib plus sintilimab can significantly improve the ORR and prolong the OS and PFS of unresectable hepatocellular carcinoma patients while maintaining an acceptable safety profile.
Data availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
References
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71(3), 209–249 (2021).
Petrick, J. L. et al. International trends in hepatocellular carcinoma incidence, 1978–2012. Int. J. Cancer 147(2), 317–330 (2020).
Galun, D. et al. Precision medicine for hepatocellular carcinoma: Clinical perspective. J. Pers. Med. 12(2), 149 (2022).
Ahn, J. C., Qureshi, T. A., Singal, A. G., Li, D. & Yang, J. D. Deep learning in hepatocellular carcinoma: Current status and future perspectives. World J. Hepatol. 13(12), 2039–2051 (2021).
Zhang, W. et al. Surgery after conversion therapy with PD-1 inhibitors plus tyrosine kinase inhibitors are effective and safe for advanced hepatocellular carcinoma: A pilot study of ten patients. Front. Oncol. 11, 747950 (2021).
Cheng, A. L. et al. Updated efficacy and safety data from IMbrave150: Atezolizumab plus bevacizumab vs. sorafenib for unresectable hepatocellular carcinoma. J. Hepatol. 76(4), 862–873 (2022).
Ren, Z. et al. Sintilimab plus a bevacizumab biosimilar (IBI305) versus sorafenib in unresectable hepatocellular carcinoma (ORIENT-32): A randomised, open-label, phase 2–3 study. Lancet Oncol. 22(7), 977–990 (2021).
Xu, J. et al. Camrelizumab in combination with apatinib in patients with advanced hepatocellular carcinoma (RESCUE): A nonrandomized, open-label Phase II trail. Clin. Cancer Res. 27(4), 1003–1011 (2021).
Translational Therapy Collaboration Group, Liver Cancer Professional Committee, Chinese Anticancer Association. Chinese expert consensus on conversion therapy for liver cancer (2021 edition). Chin. J. Dig. Surg. 20(06), 600–616 (2021).
Linye, H. et al. Thymosin alpha-1 therapy improves postoperative survival after curative resection for solitary hepatitis B virus-related hepatocellular carcinoma: A propensity score matching analysis. Medicine (Baltimore) 100(20), e25749 (2021).
Wei, Y. T. et al. Thymosin α-1 reverses M2 polarization of tumor-associated macrophages during efferocytosis. Cancer Res. 82(10), 1991–2002 (2022).
Danielli, R. et al. Long-term follow up of metastatic melanoma patients treated with Thymosin alpha-1: Investigating immune checkpoints synergy. Expert Opin. Biol. Ther. 18(sup1), 77–83 (2018).
Dai, L. et al. Therapeutic effectiveness and safety of sintilimab-dominated triple therapy in unresectable hepatocellular carcinoma. Sci. Rep. 11(1), 19711 (2021).
Finn, R. S. et al. Phase Ib study of lenvatinib plus pembrolizumab in patients with unresectable hepatocellular carcinoma. J. Clin. Oncol. 38(26), 2960–2970 (2020).
Wu, C. J. et al. Lenvatinib plus pembrolizumab for systemic therapy-naïve and -experienced unresectable hepatocellular carcinoma. Cancer Immunol. Immunother. 71(11), 2631–2643 (2022).
Kwilas, A. R., Donahue, R. N., Tsang, K. Y. & Hodge, J. W. Immune consequences of tyrosine kinase inhibitors that synergize with cancer immunotherapy. Cancer Cell Microenviron. 2(1), e677 (2015).
Yasuda, S. et al. Simultaneous blockade of programmed death 1 and vascular endothelial growth factor receptor 2 (VEGFR2) induces synergistic anti-tumour effect in vivo. Clin. Exp. Immunol. 172(3), 500–506 (2013).
Reig, M. & Bruix, J. Lenvatinib: Can a non-inferiority trial change clinical practice?. Lancet 391(10126), 1123–1124 (2018).
Pang, K. et al. Research progress of therapeutic effects and drug resistance of immunotherapy based on PD-1/PD-L1 blockade. Drug Resist. Updat. 66, 100907 (2023).
Osipov, A., Saung, M. T., Zheng, L. & Murphy, A. G. Small molecule immunomodulation: The tumor microenvironment and overcoming immune escape. J. Immunother. Cancer 7(1), 224 (2019).
Mantovani, A., Marchesi, F., Malesci, A., Laghi, L. & Allavena, P. Tumour-associated macrophages as treatment targets in oncology. Nat. Rev. Clin. Oncol. 14(7), 399–416 (2017).
Xiong, D., Zhang, K. & Xu, M. Prognostic factors of nivolumab in advanced hepatocellular carcinoma: A systematic review and meta-analysis. Panminerva Med. 65, 506–510 (2021).
Dai, L. et al. Therapeutic effectiveness and safety of sintilimab-dominated triple therapy in unresectable hepatocellular carcinoma. Sci. Rep. 11(1), 19711 (2021).
Renga, G. et al. Thymosin α1 protects from CTLA-4 intestinal immunopathology. Life Sci. Alliance 3(10), e202000662 (2020).
Funding
National Natural Science Foundation of China (82160589). Nanning Qingxiu District Science and Technology Bureau key research and development plan (2020035). The youth funding of The People’s Hospital of Guangxi Zhuang Autonomous Region (QN2018-12). Self-financed Research Program of Health and Family Planning Commission of Guangxi Zhuang Autonomous Region (Z20180722).
Author information
Authors and Affiliations
Contributions
Siyang Yao and Qiangsong Huang: Conceptualization, Writing Original Draft. Yan Zou: Data Curation. Tianqi Liu and Yongyu Yang: Formal analysis and Methodology. Tao Huang and Yuanquan Zhao: Figures and Tables. Xiaofeng Dong: Supervision, Funding acquisition. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and informed consent
This study was approved by the Ethics Committee of The People’s Hospital of Guangxi Zhuang Autonomous Region and conducted in strict accordance with the principles of the Declaration of Helsinki. Due to the retrospective nature of the study, informed consent was waived. All patient-related data used in this study were de-identified and anonymized to protect privacy.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yao, S., Huang, Q., Zou, Y. et al. The efficacy and safety of thymosin alpha-1 combined with lenvatinib plus sintilimab in unresectable hepatocellular carcinoma: a retrospective study. Sci Rep 15, 13960 (2025). https://doi.org/10.1038/s41598-025-97160-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-97160-7