Abstract
The traditional Lamaze breathing technique has limitations. We analyzed the effect of our new warm and calm (WC) breathing pattern on the incidence of fetal intrauterine distress, emergency cesarean delivery, forceps-assisted delivery, episiotomy, third- and fourth-degree perineal tears, and postpartum hemorrhage. Pregnant women who underwent a labor trial at the Second Hospital of West China University of Sichuan University between January 2020 and November 2023 and practiced the WC breathing pattern (n = 28,369) were recruited as the study group and those who underwent routine labor and practiced the Lamaze breathing technique between January 2016 and December 2019 (n = 21,110) constituted the control group. The chi-square test was used to compare differences in the incidence of fetal intrauterine distress, emergency cesarean delivery, forceps-assisted delivery, episiotomy, third- and fourth-degree perineal tears, and postpartum hemorrhage between the two groups. The incidence of the aforementioned events was significantly lower in the study group than in the control group. P-values were all ˂0.05, indicating significant differences. The WC breathing pattern increases the chances of a labor trial for pregnant women; reduces the incidence of fetal intrauterine distress, emergency cesarean delivery, forceps-assisted delivery, episiotomy, third- and fourth-degree perineal tears, and postpartum hemorrhage; and promotes safe delivery.
Similar content being viewed by others
Introduction
The traditional Lamaze breathing technique, developed by French physician Fernand Lamaze in the early 20th century, involves an alternating pattern of deep and shallow breaths to help pregnant women relax their bodies during labor contractions1. It is a breathing technique used to assist women in maintaining deep breathing, relaxation, and focus during childbirth2. However, its clinical use has revealed drawbacks such as complexity, the need for professional guidance, practical difficulties, and time constraints. Learning and mastering the Lamaze breathing technique requires time and patience, which may be challenging for some women, given the limited time available during childbirth. In actual delivery environments, especially in emergencies, women may find it challenging to continue Lamaze breathing practice, as emotions, pain, and physiological changes can affect their ability to correctly apply these techniques. Therefore, in practice, healthcare teams may need to consider providing simpler, easier-to-master breathing methods to meet the needs of a wider range of individuals. Therefore, a multidisciplinary team, including obstetricians, anesthesiologists, traditional Chinese medicine practitioners, and nurses at the Second Hospital of West China, Sichuan University, conducted in-depth research and successfully developed and proposed the new warm and calm (WC) breathing pattern, which incorporates elements of West China, warmth and calmness, and the defecation reflex. By comparing the WC breathing pattern with the Lamaze breathing technique, this study aimed to explore the impact of the WC breathing pattern on the incidence of fetal intrauterine distress, forceps-assisted delivery, postpartum hemorrhage, episiotomy, neonatal asphyxia, third- and fourth-degree perineal tears, and emergency cesarean delivery.
Results
Comparison of general characteristics between the two groups of parturients
No statistically significant differences in age, gestational weeks, gravidity, or newborn birth weight were observed between the two groups of parturients (all P > 0.05) (Table 1). In addition, we conducted a comparative analysis of the data related to forceps-assisted delivery in the two groups. The forceps-assisted delivery rate was 3.0% in the intervention group and 2.7% in the control group; however, the difference was not statistically significant (chi-square value = 3.599, P = 0.058).
Between 2016 and 2023, the total number of deliveries and vaginal deliveries increased yearly, whereas the rates of cesarean deliveries, postpartum hemorrhage, mediolateral episiotomy, severe perineal lacerations, fetal distress, and neonatal asphyxia decreased annually (Fig. 1).
Comparison of delivery complications between the two groups of parturients
The incidence of obstetric complications, such as cesarean delivery, vacuum-assisted delivery, mediolateral episiotomy, and postpartum hemorrhage, was significantly lower in the study group than in the control group (Tables 2 and 3).
Comparison of neonatal outcomes between the two groups of parturients
The incidence of fetal distress was significantly lower in the intervention group than in the control group; however, no statistically significant difference in the incidence of neonatal asphyxia was observed between the two groups (Table 4).
Discussion
The WC breathing method is not a single breathing pattern but an amalgamation of several commonly used methods in practice. It aims to adjust the physiological and psychological responses through conscious breathing techniques, ensuring that pregnant women feel warmer and calmer and providing support for physical and emotional adaptation during childbirth. This method combines the principles of deep abdominal breathing, breath control, and mental focus, simulating various common scenarios in life and combining them with the physiological aspects of defecation to play a positive role in childbirth. In addition, this method focuses on stabilizing the breathing rhythm and prolonging exhalation, activating the vagus nerve through abdominal breathing to adjust the balance of the autonomic nervous system3, thereby inducing a warm and calm physiological state4. In clinical practice, the WC breathing method can be used as an adjunctive technique for pain management during labor, reducing the need for pharmacological interventions. Studies have shown that prolonged exhalation and deep abdominal breathing can reduce the perception of pain during childbirth by promoting relaxation and calming the nervous system. Stable breathing rhythm and prolonged exhalation has the following effects on physiology, especially on the respiratory system and overall physiological health5,6. (1) Slowing down the respiratory rate: this may lead to deeper, more rhythmic breathing, which helps improve respiratory efficiency. (2) Increasing heart rate variability: deep and rhythmic breathing helps increase heart rate variability, which is related to the balance of the autonomic nervous system and may be associated with better cardiovascular health and stress-coping abilities. (3) Stimulating the vagus nerve: prolonged exhalation stimulates the vagus nerve (parasympathetic nervous system), thereby reducing the heart rate, lowering blood pressure, and facilitating a more relaxed state. (4) Improving lung function: deep breathing and prolonged exhalation increase lung capacity, improving ventilation and gas exchange efficiency. This is beneficial for increasing oxygen intake and carbon dioxide excretion. (5) Reducing respiratory muscle tension: a regular breathing pattern reduces discomfort and tension in the respiratory muscles, helping to improve breathing coordination. (6) Adjusting acid-base balance: deep breathing and slow exhalation help adjust acid-base balance by reducing carbon dioxide emissions, helping to maintain blood acid-base balance. (7) Lowering stress levels: regular deep breathing activates the parasympathetic nervous system, reduces the secretion of stress hormones, and helps alleviate physical and psychological tension. (8) Improving attention and cognitive ability: stable breathing and deep breathing helps increase blood oxygen levels, which may be related to improved attention, cognitive ability, and clear thinking7,8. The WC breathing technique helps to relax the body, relieve stress, and provide a positive physiological and psychological experience. It can help alleviate pain, improve oxygen supply, promote parasympathetic activity, maintain a steady heart rate, and improve concentration and attention. Through conscious deep breathing, pregnant women can better focus and stay calm and alert, helping them to better participate in the childbirth process and understand the natural attributes of childbirth. Ultimately, this promotes respect for life from the obstetric staff, pregnant women, and the pregnant woman’s family9. Further research is needed to explore the long-term effects of this technique on postpartum recovery, as it may contribute to faster physical and emotional recovery in the postpartum period.
Through deep breathing and slowing the respiratory rate, the pregnant woman can relax her body, reduce anxiety, and alleviate tension, which may have a positive impact on the delivery process10. Adequate oxygen supply is crucial for the health of the mother and fetus11, which is ensured through respiratory control12. Some breathing techniques may help reduce the perception of pain during delivery, enabling the mother to cope with pain. Respiratory control may be related to the relaxation of the pelvic floor muscles, which may be beneficial for vaginal delivery during childbirth13. Midwives can play a crucial role in offering continuous emotional and physical support by guiding women through the breathing techniques, ensuring that they feel empowered and in control during childbirth. Insights for midwifery practice may include training women in effective breathing techniques during childbirth to help them better manage the physiological and psychological challenges of childbirth. Providing psychological support for pregnant women via teaching techniques, such as respiratory control and deep breathing, to help them relax and reduce anxiety during childbirth is essential13. Considering individual differences, providing personalized breathing guidance to meet pregnant women’s specific needs during childbirth is also vital. Applying breathing techniques to promote natural childbirth reduces the need for medical interventions. Midwives can encourage and guide the use of these techniques during childbirth.
The “controlled breathing” pattern reduces the incidence of fetal distress and neonatal asphyxia because breathing control helps ensure an adequate supply of oxygen to the fetus, which is crucial for their normal growth and development. In this study, we determined the presence of fetal distress based on the medical diagnosis of the mother. In addition, we used a 1-min Apgar score of ˂8 to assess the risk of neonatal asphyxia. Deep and regular breathing helps maintain good oxygen saturation, reducing the risk of intrauterine distress and postnatal asphyxia14. The “controlled breathing” pattern also reduces the occurrence of postpartum hemorrhage, possibly because breathing control helps maintain an adequate oxygen supply. Maintaining an adequate oxygen supply helps maintain normal tissue function, including uterine contractions and blood vessel constriction, thereby reducing the risk of bleeding15. Deep and regular breathing may help maintain the smooth operation of the circulatory system during delivery, ensuring sufficient blood delivery to the uterus and other tissues and reducing the risk of bleeding16. During delivery, tension and anxiety may lead to stress responses in the body, affecting the normal function of the circulatory system and uterus17,18. Controlling breathing helps reduce tension, aiding in maintaining physiological balance. A reduction in severe third- and fourth-degree perineal tears may also be facilitated by conscious breathing, which promotes relaxation and reduces muscle tension. Conscious breathing makes the birth canal softer and more elastic, reducing excessive pressure on the perineal area when the fetus passes through. Conscious breathing practices can make pregnant women more aware of their sensations and needs, helping them better cooperate and comply with guidance from healthcare providers19.
Overall, the control of breathing plays an important role in the childbirth process, with its positive effects encompassing multiple aspects. First, through conscious breathing practices, pregnant women cultivate a deep sense of body awareness, enabling them to better perceive and understand their condition during childbirth. This self-awareness not only helps alleviate tension and anxiety but also prompts them to be more cooperative and better follow the guidance of healthcare professionals. Physiologically, the control of breathing affects oxygen supply and blood circulation. By maintaining an adequate oxygen supply, respiratory adjustments help ensure that both the mother and fetus receive sufficient oxygen to maintain normal physiological functions. Additionally, regular breathing coordinates uterine contractions, promoting a smooth delivery process. For vaginal delivery, this means a greater likelihood of achieving a natural, non-invasive delivery. Furthermore, breathing control may help reduce the perception of pain. Pain is a common experience during childbirth, and by adopting deep and conscious breathing techniques, pregnant women can lower their perception of pain and better cope with the physiological processes of childbirth. Overall, the “controlled breathing” pattern is a comprehensive approach that not only focuses on the physiological effects but also involves emotional and consciousness states on the psychological level. In practical application, during antenatal training and labor, breathing control may serve as a natural and simple tool to provide a more positive childbirth experience for mothers and help reduce some potential health risks. Midwives and healthcare professionals can guide expectant mothers in incorporating breathing techniques into their birth plans, ensuring that they feel well-prepared and confident to manage the physical and emotional demands of childbirth.
The main limitation of this study is that the results were based solely on samples from a single top-tier hospital in China, which may limit the generalizability of the findings. Additionally, over time, obstetric techniques may have improved (such as advancements in pain relief methods). Although we implemented appropriate quality control measures in the study, there may still be some confounding factors that were not fully eliminated. Based on our results, future multi-center and big data studies are needed to further validate and expand our findings.
Methods
Study population
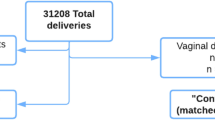
This study has a retrospective cohort design. The research design is detailed in Fig. 2. A total of 28,369 pregnant women who underwent a trial of labor in the delivery room of the Second Hospital of West China University of Sichuan University from January 2020 to November 2023 and practiced the WC breathing pattern were recruited as the study group. Additionally, 21,110 pregnant women who underwent routine labor and practiced the Lamaze breathing technique between January 2016 and December 2019 were recruited as the control group. The differences between the two groups in terms of the incidence of fetal intrauterine distress, emergency cesarean delivery, forceps-assisted delivery, episiotomy, third- and fourth-degree perineal tears, and postpartum hemorrhage (primary outcomes) were compared. In addition, the trends in changes of these indicators (secondary outcomes) were compared. The p-value was set to 0.05. The inclusion criteria included singleton pregnancy, full-term, vertex presentation, absence of fetal abnormalities, pregnancy complications or comorbidities, and a history of uterine surgery. The study was approved by the Medical Research Ethics Committee of West China Second University Hospital, Sichuan University (approval number: 072) and conducted in accordance with relevant regulations and guidelines. The need to obtain the informed consent was waived by the ethical committee.
Grouping criteria
The study group underwent assisted labor using the WC breathing pattern, whereas the control group underwent assisted labor using the Lamaze breathing pattern.
Diagnostic criteria
Postpartum hemorrhage is defined as > 500 mL of vaginal bleeding within 24 h after delivery20. Fetal distress refers to the condition of the fetus in utero being at risk of health and life due to hypoxia and acidosis16. Neonatal asphyxia was diagnosed based on the 1-min Apgar score: 0‒3 points indicate severe asphyxia and 4‒7 points indicate mild asphyxia21. A third-degree perineal tear was defined as damage extending beyond the perineal skin, mucosa, and muscle involving the anal sphincter, and a fourth-degree perineal tear involved injury extending to the rectum22.
Operational method of the WC breathing pattern
The operational method of the WC breathing pattern involved the following steps. (1) A comfortable position was ensured for the pregnant woman, such as sitting or semi-reclining, to reduce abdominal pressure and facilitate deep diaphragmatic breathing. (2) Deep and slow inhalation was encouraged: deep inhalation through the nose to allow air to fully enter the lungs, emphasizing the use of the diaphragm and abdominal muscles. This helps increase lung capacity and stabilizes gas exchange. (3) Prolonged exhalation: slow and controlled exhalation was emphasized by adjusting the duration of the exhalation phase to effectively promote gas expulsion and gas exchange. (4) The breathing rhythm was adjusted by using longer inhalation and exhalation durations to help regulate heart rate, reduce sympathetic nervous system activity, and induce a calm physiological state. (5) Simulated yawning exhalation: a yawning motion was simulated to prolong exhalation by exhaling slowly and completely to emphasize use of the diaphragm and abdominal muscles. (6) Simulated cough or sneeze exhalation: after inhalation, a rapid and forceful exhalation simulating a cough or sneeze motion was practiced. The rapid and coordinated contraction of the abdominal muscles and diaphragm was emphasized to significantly increase the flow rate of the exhalation phase. This process helps clear secretions in the airways and promotes airway clearance. (7) Mental focus and mindfulness: the WC breathing method emphasizes mental focus and mindfulness, directing attention during the breathing process from external stimuli to the sensation of breathing, which helps increase a sense of mental calmness. (8) Regular practice: pregnant women were advised to practice the WC breathing method regularly during pregnancy to increase proficiency in the technique and ensure thy could apply it more effectively during pregnancy and childbirth when needed.
Analysis content
We compared the differences in general conditions, intrauterine fetal distress, forceps-assisted delivery, postpartum hemorrhage, episiotomy, neonatal asphyxia, third- and fourth-degree perineal tears, and cesarean delivery rates between the two groups.
Statistical analysis
Statistical analysis was performed using SPSS 26.0 software. Normally distributed continuous data were presented as means ± standard deviation and compared between groups using the t-test. Categorical data were presented as frequencies and percentages and compared between groups using the chi-square test. Statistical significance was set at P < 0.05.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Wu, C. et al. The combined effects of lamaze breathing training and nursing intervention on the delivery in Primipara: A PRISMA systematic review meta-analysis. Med. (Baltim). 100, e23920 (2021).
Podgurski, M. J. Theorists and techniques: connecting education theories to lamaze teaching techniques. J. Perinat. Educ. 25, 9–17 (2016).
LoMauro, A. & Aliverti, A. Respiratory physiology in pregnancy and assessment of pulmonary function. Best Pract. Res. Clin. Obstet. Gynaecol. 85, 3–16 (2022).
Bates, M. L. Respiratory diseases are whole body diseases: opportunities for growth in respiratory physiology. Am. J. Physiol. Lung Cell. Mol. Physiol. 321, L628–L630 (2021).
Sepúlveda Oviedo, E. H. & Clavijo, B. Méndez Córdoba, L. C. OpenModelica-based virtual simulator for the cardiovascular and respiratory physiology of a neonate. J. Med. Eng. Technol. 46, 179–197 (2022).
Ekström, M. et al. Abnormal exertional breathlessness on cardiopulmonary cycle exercise testing in relation to self-reported and physiological responses in chronic airflow limitation. Chest 166, 81–94 (2024).
Fan, S. & Ma, J. The value of five scoring systems in predicting the prognosis of patients with sepsis-associated acute respiratory failure. Sci. Rep. 14, 4760 (2024).
Siroux, V. et al. Intra-breath changes in respiratory mechanics are sensitive to history of respiratory illness in preschool children: the SEPAGES cohort. Respir Res. 25, 99 (2024).
Pu, C. Y. et al. Effects of preoperative breathing exercise on postoperative outcomes for patients with lung cancer undergoing curative intent lung resection: A meta-analysis. Arch. Phys. Med. Rehabil. 102, 2416–2427e4 (2021).
Issac, A. et al. Effectiveness of breathing exercise on the duration of labour: A systematic review and meta-analysis. J. Glob Health. 13, 04023 (2023).
Zwaag, J., Naaktgeboren, R., van Herwaarden, A. E., Pickkers, P. & Kox, M. The effects of cold exposure training and a breathing exercise on the inflammatory response in humans: A pilot study. Psychosom. Med. 84, 457–467 (2022).
Jahan, I. et al. Effects of alternate nostril breathing exercise on cardiorespiratory functions in healthy young adults. Ann. Afr. Med. 20, 69–77 (2021).
Das, R. R., Sankar, J. & Kabra, S. K. Role of breathing exercises in asthma-yoga and Pranayama. Indian J. Pediatr. 89, 174–180 (2022).
Dunietz, G. L., Sever, O., DeRowe, A. & Tauman, R. Sleep position and breathing in late pregnancy and perinatal outcomes. J. Clin. Sleep. Med. 16, 955–959 (2020).
Felton, M., Hundley, V. A., Grigsby, S. & McConnell, A. K. Effects of slow and deep breathing on reducing obstetric intervention in women with pregnancy-induced hypertension: A feasibility study protocol. Hypertens. Pregnancy. 40, 81–87 (2021).
Zhu, M. & Liu, L. Fetal heart rate extraction based on wavelet transform to prevent fetal distress in utero. J. Healthc. Eng. 7608785 (2021).
Cosmi, E. V., Anceschi, M. M., Cosmi, E., Piazze, J. J. & La Torre, R. Ultrasonographic patterns of fetal breathing movements in normal pregnancy. Int. J. Gynaecol. Obstet. 80, 285–290 (2003).
Fentie, Y., Yetneberk, T. & Gelaw, M. Preoperative anxiety and its associated factors among women undergoing elective caesarean delivery: A cross-sectional study. BMC Pregnancy Childbirth. 22, 648 (2022).
Martherus, T. et al. Supporting breathing of preterm infants at birth: A narrative review. Arch. Dis. Child. Fetal Neonatal Ed. 104, F102–F107 (2019).
Okaforcha, E. I. et al. Intravenous versus intramuscular Oxytocin injection for preventing uterine atonic primary postpartum haemorrhage in third stage of labour: A double-blind randomised controlled trial. Sage Open. Med. 12 (2024).
Russ, J. B., Simmons, R. & Glass, H. C. Neonatal encephalopathy: beyond hypoxic-ischemic encephalopathy. NeoReviews 22, e148–e162 (2021).
Magoga, G. et al. Warm perineal compresses during the second stage of labor for reducing perineal trauma: A meta-analysis. Eur. J. Obstet. Gynecol. Reprod. Biol. 240, 93–98 (2019).
Acknowledgements
We would like to thank Editage (www.editage.cn) for English language editing.
Funding
This research received funding from the project “Clinical Study of Hypnosis Delivery Training Improving Delivery Outcomes (2017) 919 − 26.” The funding agency had no role in study design, collection, analysis, and interpretation of data, writing the report, and the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
All authors contributed to the research and preparation of the manuscript and approved the final submitted version. Each author participated in the conceptualization and design of the study, as well as the data analysis. Jingjing He was responsible for writing the original draft; Yuxin Tang conducted the formal data analysis; Yonghong Wang provided resources; and Huafeng Li reviewed the manuscript. Guoyu Wang, Zhuli Chen, Yan Zuo, and Xiangmin Liu were responsible for data collection and organization. Chaojun Shan supervised further discussions and revisions of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
He, J., Tang, Y., Wang, G. et al. Impact of the warm and calm breathing pattern on delivery outcomes in pregnant Chinese women: a retrospective cohort study. Sci Rep 15, 13200 (2025). https://doi.org/10.1038/s41598-025-97971-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-97971-8