Abstract
Few epidemiological studies have explored the longitudinal relationship between atherosclerosis and periodontitis. The aim of this study was to investigate the longitudinal relationship between atherosclerosis and the progression of periodontitis in community-dwelling individuals in Japan. Progression of periodontitis was defined as the presence of the teeth demonstrating a longitudinal loss of proximal attachment ≥ 3 mm during the study period. Oral examinations and subclinical atherosclerosis assessments were performed. The surrogate markers of early-stage atherosclerosis were increased carotid intima-media thickness (cIMT), low ankle-brachial index (ABI), and cardio-ankle vascular index (CAVI). The study included 222 Japanese adults. While CAVI increased significantly in both groups, the prevalence of CAVI ≥ 8 was significantly increased in only the progression group during the study period. Logistic regression analysis indicated that the progression of periodontitis was significantly associated with cIMT. Additionally, CAVI positively correlated with changes in probing pocket depth, while ABI negatively correlated with changes in clinical attachment loss. These results suggest that participants with high cIMT, high CAVI and low ABI had a high risk of periodontitis progression after adjusting for risk factors. In conclusion, subclinical markers of early-stage atherosclerosis are significantly associated with a greater risk of periodontitis progression in community-dwelling Japanese participants.
Similar content being viewed by others
Introduction
The prevalence of non-communicable diseases (NCDs) is increasing globally, accounting for 41 million deaths each year or 71% of all global deaths1. Periodontitis is an NCD with one of the highest prevalence of 45–50% worldwide and is characterized by gingival bleeding, periodontal pocket formation, and destruction of the connective tissue attachment surrounding the teeth in response to subgingival infection with various periodontal pathogens2. Pathogens in the microbial biofilm in the subgingiva stimulate the host immune system, resulting in the destruction of the supporting tissues of the teeth, and finally, tooth loss. Periodontitis is now considered the main cause of tooth loss in people older than 40 years, with a higher prevalence compared to that of caries3.
Initially, it was assumed that periodontitis mainly led to tooth loss that required prosthetic rehabilitation. However, links between periodontitis and other systemic diseases have only been established since the early 2000s. Research on the systemic implications of periodontitis has exponentially increased over the past few years. Epidemiological studies indicate that 57 systemic conditions are linked to periodontitis4. There is now significant evidence to support the independent association between severe periodontitis and several NCDs including cardiovascular diseases (CVD)5.
Atherosclerosis is a major cause of vascular disease, characterized by the thickening of the arterial wall due to chronic inflammation and lipid and metabolic alterations in the vessel walls. Multiple meta-analyses have linked atherosclerosis to periodontitis, both of which are chronic inflammatory diseases6,7. A recent study also suggested that a chronic low-grade inflammatory process in periodontitis contributes to the pathogenesis of atherosclerosis subsequently leading to ischemic heart disease and stroke8. These studies have presented associations between periodontitis and surrogate markers of atherosclerosis, including subclinical morphological changes such as increased carotid intima-media thickness (cIMT) and low ankle-brachial index (ABI). Abnormally increased cIMT and low ABI indicate subclinical atherosclerosis and peripheral arterial disease, respectively9. We have also reported cross-sectional evidence that the cardio-ankle vascular index (CAVI) is related to periodontal status10. CAVI was developed to overcome the dependency of pulse-wave velocity measurements on blood pressure and has recently been used as a new tool to assess arterial stiffness of the aorta, femoral artery, and tibial artery11 and to appropriately screen for subclinical atherosclerosis12.
In 2014, Nagasaki University launched a population-based prospective open cohort study in remote islands, called the Nagasaki Islands Study (NaIS)13. This study aimed to identify the influence of aging on health conditions; elucidate the risk factors of cardiovascular diseases, rheumatic and autoimmune diseases, dental diseases, frailty, sarcopenia, osteoporosis, and fracture; and contribute to preventive medicine. In this cohort study, we hypothesized that atherosclerosis affects the progression of periodontitis. However, most previous studies, including our previous study have investigated the association between atherosclerosis and periodontitis using a cross-sectional design10. A longitudinal study is needed to elucidate the temporal associations. Therefore, we designed a longitudinal study to investigate these associations over a 3-year follow-up.
The aims of the present study, therefore, were to analyze the longitudinal relationship between three subclinical markers of early-stage atherosclerosis and the progression of periodontitis, defined by the change in clinical attachment loss (CAL), in community-dwelling people in Goto City, Japan.
Methods
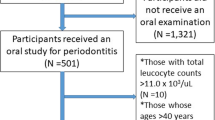
Study population
The present investigation was designed as a 3-year cohort study. In the surveys of our open-cohort, 597 subjects at baseline, aged ≥ 40 years attended a specific health check-up that included an oral assessment conducted in Goto City, Nagasaki Prefecture, Japan. Of these, a total of 238 subjects who attended both the baseline and follow-up health checkups after 3 years, including assessments of subclinical atherosclerosis, potential confounders, and oral examinations were enrolled13. Additionally, 16 subjects were excluded from the present analysis due to fewer than 10 remaining teeth or missing data. Ultimately, all of 222 patients, included in the study were attend all assessments both baseline and 3-year follow-up.
All participants provided signed informed consent before participating in the study. This study was approved by the Ethics Committee of Nagasaki University Graduate School of Biomedical Sciences (No. 090528160 and No. 14051404) and was performed in accordance with the Declaration of Helsinki.
Oral examination
Periodontal examination was performed using a modified version of the Third National Health and Nutrition Examination Survey by one of the four calibrated dentists under sufficient illumination, as described previously14. The probing pocket depth (PPD) and CAL, which indicate the distance from the cementoenamel junction to the bottom of the pocket, were measured using a periodontal probe for all teeth, excluding the third molar15. Before starting this study, all examiners and volunteers at Nagasaki University Hospital were trained and calibrated using a dental chart for periodontal models. If caries or deep periodontal pocket were detected, the participants were instructed to visit dental clinic.
Assessment of subclinical atherosclerosis
The surrogate markers of early-stage atherosclerosis used in this study were cIMT, CAVI, and ABI. The cIMT of the left and right common carotid arteries were evaluated using ultrasonography, as previously described10. The maximum values of the right and left cIMTs were used for analysis, and values exceeding the normal range by ≥ 1 mm were defined as the higher group, based on a previous study16. CAVI was recorded using a Vasera VS-1500 vascular screening system (Fukuda Denshi Ltd., Tokyo, Japan) with the participant resting in the supine position, as described in a previous report10. The averages of the right and left CAVI were used in the analysis. A CAVI exceeding the normal range by ≥ 8 was defined as a higher CAVI, which was reported to be the optimal cutoff point for arteriosclerosis17. Blood pressure in the upper and lower extremities was measured, and the ABI was calculated separately by dividing the higher of the two systolic pressures in the ankle by the higher of the two systolic pressures in the arm18. The threshold value for the ABI was 1.0, based on a previous study18.
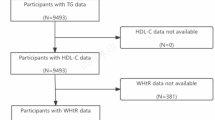
Assessment of potential confounders
Information on each participant, including current medication use, smoking, and habitual alcohol consumption status, as well as medical history, including hypertension, diabetes mellitus, and dyslipidemia, were collected using standardized questionnaires by trained physicians and research assistants. The height and weight of each participant were measured using calibrated scales, and the body mass index (BMI) was calculated. Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were recorded at rest. Blood samples were obtained from the antecubital vein after overnight fasting and separated serum samples were used to measure biochemical parameters. Triglyceride, high- and low-density lipoprotein (HDL and LDL) cholesterol, and hemoglobin A1c (HbA1c) levels were measured. The estimated glomerular filtration rate (eGFR) was calculated using the abbreviated Modification of Diet in Renal Disease Study equation, with a Japanese coefficient of 0.88119.
Statistical analysis
Paired t-tests for continuous variables and chi-squared tests for categorical variables were used to compare the variables at baseline and 3-year follow-up. We divided the subjects into those with progression or non-progression of periodontitis at baseline as follows: Subjects diagnosed with disease progression (progression group) were defined based on the presence of ≥ 2 teeth demonstrating a longitudinal loss of proximal attachment of ≥ 3 mm during the 3-year period20. The remaining participants were assigned to the non-progression group. Student’s t-test and chi-square test were used to compare the baseline variables between the progression and non-progression groups.
Odds ratios (ORs) and 95% confidence intervals (CI) for periodontitis progression were calculated using logistic regression models. Factors that showed significant associations with the risk of periodontitis progression in univariate analysis were subsequently included in the multivariate model to assess the effect of subclinical atherosclerosis on periodontitis progression. Multiple linear regression analyses for all participants at baseline were also performed to evaluate the relationship between changes in CAL and PPD.
All analyses were performed using JMP software (version 12; SAS Institute, Cary, NC, USA). Statistical significance was set at p < 0.05.
Results
The characteristics of the study population at baseline and 3-year follow-up are shown in (Table 1). The mean age of the participants at baseline was 64.5 ± 10.3 years, and 39.2% were men. There were significant differences between baseline and 3-year follow-ups in the number of teeth present, periodontal parameters, BMI, HDL-cholesterol, SBP, HbA1c, and CAVI. During the study period, cIMT and ABI did not change significantly. Moreover, Supplementary Table 1 indicated the characteristics of 3-year follow-up and baseline only participants at baseline. There were no significant differences between groups with respect to all factors.
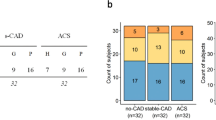
Comparisons of participants with non-progression and progression of periodontitis at baseline are shown in (Table 2). In total, 26.1% of the study participants (58/222) had progression of periodontitis. Statistical analyses indicated that gender, age, number of teeth present, PPD, CAL, smoking status, hypertension, cIMT, prevalence of cIMT > 1 mm, and CAVI differed significantly between the two groups. Although the prevalence of diabetes mellitus and dyslipidemia was higher in participants with periodontitis progression, the difference was not statistically significant. While CAVI increased significantly in both groups, the prevalence of CAVI value of ≥ 8 was significantly increased in only the progression group during this study period (Table 3). cIMT and ABI did not significantly change in either group during the 3-years.
Factors related to the progression of periodontitis were calculated using a logistic regression model with a significance level of p < 0.1. Age, gender, smoking status, and hypertension were significantly associated with the progression of periodontitis (Table 4). These factors were used to adjust for the confounding caused by the progression of periodontitis.
Table 5 shows the results of the multiple logistic regression models for the three markers of subclinical atherosclerosis, as reported by the ORs and 95% CIs. After applying age and gender (Model 2), the high cIMT group was associated with a significantly higher OR for periodontitis progression (OR 2.35; 95% CI 1.18–4.70). This association remained significant after adjusting for additional covariates, including smoking status and hypertension (Model 3). The multivariable-adjusted OR for periodontitis progression was 2.23 (95% CI 1.09–4.57) with high cIMT. However, there were no statistically significant associations between progression of periodontitis and CAVI (≥ 8) or ABI (< 1).
The results of the multiple linear regression analyses are shown in (Tables 6 and 7). The results adjusted with age and gender (Model 2) indicated that CAVI was positively correlated with the change of CAL (β = 0.046; 95% CI 0.008–0.083), and ABI was negatively correlated with the change of PPD (β=−0.667; 95% CI −1.237 and −0.097). These associations remained significant after adjusting for all covariates (Model 3). CAVI was significantly correlated with the change in CAL, but not with the change in PPD (β = 0.027; 95% CI −0.017–0.072). Similarly, ABI was significantly correlated with the change in PPD (β=−0.655; 95% CI −1.236 and −0.084), but not with the change in CAL. However, no significant relations were observed between cIMT and changes in CAL or PPD.
Discussion
In the present study, we assess the longitudinal association between three subclinical markers of atherosclerosis and periodontitis progression, and suggest that atherosclerosis is significantly associated with the progression of periodontitis in community-dwelling participants in Japan. Further, multiple logistic regression analyses revealed that participants with cIMT > 1 mm had a high risk of periodontitis progression after adjusting for risk factors. Moreover, multiple linear regression models showed that CAVI was positively correlated with changes in CAL and that ABI was negatively correlated with changes in PPD. Considering these results, our findings suggest that subclinical markers of early-stage atherosclerosis are associated with a greater risk of periodontitis progression. This finding supports the findings of previous cross-sectional studies showing an association between atherosclerosis and periodontitis.
Our study has several strengths. First, we used a longitudinal epidemiological design and analyzed the associations between the three subclinical markers of atherosclerosis and the progression of periodontitis or changes in periodontal parameters. Second, the participants of this study were selected from a community-dwelling general population, as opposed to patients in a hospital, which reduces the chance of selection bias and enhances the generalizability of our results. Third, we used three subclinical early-stage markers of atherosclerosis: cIMT, CAVI, and ABI. This corroborated the results with a higher level of evidence.
Since 1989, the association between periodontitis and CVD has been continually investigated, and a meta-analysis indicated that periodontitis is a risk factor for CVD21. Atherosclerosis, an inflammatory disorder of the arteries, is a well-known leading cause of CVD. Because periodontitis is a chronic inflammatory disease, inflammation occurring in periodontitis may play a role in atherosclerosis. A large cohort study of 60,174 participants in the Netherlands showed that periodontitis was independently associated with atherosclerosis after adjusting for confounders22. However, these factors have only been investigated in cross-sectional epidemiological studies. Currently, there is limited scientific evidence suggesting that CVD or atherosclerosis are risk factors for the onset or progression of periodontitis23. Additionally, interventional studies mainly focusing on the effects of periodontitis have increased in recent years, and the available evidence remains insufficient to establish a relationship between periodontitis and atherosclerosis. Although most of these studies have focused on the effects of periodontitis on atherosclerosis, we hypothesized that atherosclerosis may affect the progression of periodontitis.
Several mechanisms have been proposed for the association between atherosclerosis and periodontitis. A recent study suggested that periodontal pathogenic bacteria and their components can reach the coronary artery. For example, Porphyromonas gingivalis, Prevotella intermedia, and Tennerella forsythensis, known to be putative periodontal pathogenic bacteria, have been identified in atherosclerotic plaques24, as well as in the human aortic and coronary endothelium25. Animal studies have shown that periodontal pathogens promote atheroma formation. P. gingivalis has been shown to accelerate atherosclerosis in murine models by inducing fatty streaks in the aorta of rabbits, and coronary lesions after bacteremia in normocholesterolaemic pigs26. Additionally, there is evidence that periodontal pathogens can enter cells in vitro27. The importance of the fimbriae of P. gingivalis is also investigated, and they were observed to enter host cells and promote atherothrombotic lesions in experimental animal models28.
Evidence suggests that the production and/or levels of inflammatory mediators associated with the pathophysiology of atherosclerosis are increased in patients with periodontitis. C-reactive protein (CRP) levels are higher in patients with CVD and periodontitis than in healthy controls with periodontitis. The effects of periodontal therapy were also investigated, and the results revealed associations with a significant decrease in CRP levels along with improvements in the surrogate conditions of cardiovascular health29. Because peripheral neutrophils of patients with periodontitis release excess inflammatory cytokines when stimulated by periodontal pathogens, the serum levels of these cytokines are elevated. These inflammatory mediators are important cardiovascular risk factors that may affect the development of CVD as a complication30. Nonetheless, periodontal therapy only partially reduces cytokine hyperreactivity, with some evidence of a constitutively elevated response23.
Our previous cross-sectional study observed linear and dose-dependent associations between the markers of subclinical atherosclerosis and periodontal parameters10. Periodontal status was potentially associated with alterations in both arterial wall thickness (cIMT) and stiffness of the aorta (CAVI) during the initial stages of atherosclerosis. Particularly, CAVI has been developed as a new tool to assess the arterial stiffness of the aorta, femoral artery, and tibial artery, and is appropriate as a screening tool for atherosclerosis with higher reproducibility. The CAVI adjusts for blood pressure based on the stiffness parameter β and is minimally influenced by blood pressure at the time of measurement9. Recently, CAVI showed a linear relationship with increased tooth loss in the Nagahama study in Japan31. Tooth loss is frequently caused by the progression of periodontitis and is a marker of the current and long-term cumulative influence of periodontitis; however, periodontal parameters have not been directly evaluated. Our study is the first to demonstrate that CAVI is associated with periodontitis progression. We found that periodontitis progression was associated with higher cIMT, a marker of subclinical atherosclerosis. A previous study indicated that periodontitis with elevated bacterial exposure is associated with early atheroma plaque formation and significantly increased cIMT32. These findings suggest that the level of systemic bacterial exposure in periodontitis is biologically related to subclinical atherosclerosis. Moreover, an improvement in the periodontal and microbiological status was associated with atherosclerosis, as assessed by cIMT, over an average period of 3 years33. These findings may support a mechanistic explanation for the association between cIMT and the progression of periodontitis. Based on an epidemiological survey, it is difficult to define why CAVI or ABI is related to changes in the periodontal index. However, there is a positive relationship between periodontitis based on CAL and low ABI, as described previously34. The prevalence of P. gingivalis and the serum CRP levels were also higher in the low ABI group. Possible associations between the ABI and both bacterial and inflammatory components of periodontitis were considered. These factors may affect the progression of both atherosclerosis and periodontitis.
Periodontal treatment, especially full-mouth subgingival instrumentation could reduce periodontal parameters, periodontal pathogens and critical inflammatory mediators35,36. Moreover, our previous study indicated that periodontal treatment reduced systemic oxidative stress, and may be beneficial in preventing systemic disease37. Additionally, oxidized LDL is known to have proatherogenic and proinflammatory properties, and decreased by periodontal treatment38. Though periodontal treatment would be useful for maintaining cardiovascular health by decreasing plasma levels of oxidative stress and oxidized LDL, our study did not collect the information about dental history and dental treatment during the study period. These indicators could affect oral and atherosclerosis status. In the future, randomized clinical study will be required to investigate that periodontal treatment could reduce the risk of atherosclerosis.
Although the present study provides new epidemiological findings on longitudinal associations between atherosclerosis and periodontitis in Japan, it has several limitations. First, not all participants underwent follow-up health checkups, and we could not obtain data on the reasons for their non-participation in dental examinations. However, there were no significant differences between participants who did and did not undergo follow-up checkups in terms of all factors, including those related to periodontal disease and atherosclerosis. Furthermore, participants living in nursing homes were excluded from this study. Therefore, the sample used in this study may be healthier than the general Japanese population. Second, information regarding health status was self-reported, as these were collected using a questionnaire; however, we measured HbA1c, blood pressure, and biochemical parameters. Third, although our analyses were adjusted for various potentially confounding variables, information related to socio-economic statuses was not collected. Additionally, other possible confounders, such as household income, education level, and nutritional intake are also widely accepted to affect oral conditions, and might have played an important role in this study. Although previous studies have described the influence of socio-economic differences on disease risk factors, the Japanese population may not reflect the same patterns of relationships observed in other developed countries39. Finally, our study did not indicate the biological mechanisms. However, plausible mechanisms between atherosclerosis and periodontal diseases, including microbiological or inflammatory mechanism, and molecular mimicry are proposed40. To further solidify the apparent link, it would be important to conduct intervention studies focusing on the effects of periodontal treatment are also essential. Despite these limitations, the results of this study are sufficiently reliable to test the hypothesis that subclinical markers of atherosclerosis are associated with the progression of periodontitis.
In conclusion, our findings indicate that atherosclerosis is significantly associated with the progression of periodontitis in community-dwelling participants in Japan, and support the hypothesis that atherosclerosis affects the progression of periodontitis. This study, conducted over a relatively short period, strengthens that atherosclerosis explains previous reports linking periodontitis. The prevention of subclinical atherosclerosis could therefore improve periodontal conditions. These findings provide further evidence that implementing strategies to prevent atherosclerosis may prevent the progression of periodontitis, with important public health as well as clinical implications. Encouraging participants to prevent subclinical atherosclerosis is expected to benefit their systemic health as well as their oral health.
Data availability
The data that support the findings of this study are available from the Nagasaki Island Study (NaIS); however, restrictions apply to the availability of these data, which were used under license for the current study and are not publicly available. However, the data are available from the corresponding authors upon reasonable request and with permission from the NaIS.
References
Forouzanfar, M. H. et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: A systematic analysis for the global burden of disease study 2015. Lancet 388, 1659–1724 (2016).
Demmer, R. T. & Papapanou, P. N. Epidemiologic patterns of chronic and aggressive periodontitis. Periodontol. 2000 53, 28–44 (2010).
Frencken, J. E. et al. Global epidemiology of dental caries and severe periodontitis—A comprehensive review. J. Clin. Periodontol. 44 (18), S94–S105 (2017).
Monsarrat, P. et al. Clinical research activity in periodontal medicine: A systematic mapping of trial registers. J. Clin. Periodontol. 43, 390–400 (2016).
Tonetti, M. S. & Van Dyke, T. E. Working group 1 of the joint, EFP/AAP workshop Periodontitis and atherosclerotic cardiovascular disease: Consensus report of the joint EFP/AAP workshop on periodontitis and systemic diseases. J. Clin. Periodontol. 40 (14), 24–29 (2013).
Zeng, X. T. et al. Periodontal disease and carotid atherosclerosis: A meta-analysis of 17,330 participants. Int. J. Cardiol. 203, 1044–1051 (2016).
Arbildo-Vega, H. I. et al. Periodontal disease and cardiovascular disease: Umbrella review. BMC Oral Health 24, 1308. https://doi.org/10.1186/s12903-024-04907-1 (2024).
Lockhart, P. B. et al. Periodontal disease and atherosclerotic vascular disease: Does the evidence support an independent association? A scientific statement from the American heart association. Circulation 125, 2520–2544 (2012).
Feinstein, S. B., Voci, P. & Pizzuto, F. Noninvasive surrogate markers of atherosclerosis. Am. J. Cardiol. 89, 31 C–43 C (2002).
Hayashida, H. et al. Association of periodontitis with carotid artery intima-media thickness and arterial stiffness in community-dwelling people in Japan: The Nagasaki Islands study. Atherosclerosis 229, 186–191 (2013).
Takaki, A. et al. Cardio-ankle vascular index is superior to brachial-ankle pulse wave velocity as an index of arterial stiffness. Hypertens. Res. 31, 1347–1355 (2008).
Kadota, K. et al. Availability of cardio-ankle vascular index (CAVI) as a screening tool for atherosclerosis. Circ. J. 72, 304–308 (2008).
Miyata, J. et al. Profile of Nagasaki Islands Study (NaIS): A population-based prospective cohort study on multi-disease. J. Epidemiol. 34, 254–263 (2024).
Tamaki, N. et al. Oxidative stress and antibody levels to periodontal bacteria in adults: The Nagasaki Islands study. Oral Dis. 20, e49–56 (2014).
Tamaki, N. et al. Relationship among salivary antioxidant activity, cytokines, and periodontitis: The Nagasaki Island study. J. Clin. Periodontol. 42, 711–718 (2015).
Zhao, Y. et al. Multisite atherosclerosis in subjects with metabolic syndrome and diabetes and relation to cardiovascular events: The Multi-Ethnic study of atherosclerosis. Atherosclerosis 282, 202–209 (2019).
Hu, H. et al. A cutoff point for arterial stiffness using the cardio-ankle vascular index based on carotid arteriosclerosis. Hypertens. Res. 36, 334–341 (2013).
Ahn, Y. B. et al. Periodontitis is associated with the risk of subclinical atherosclerosis and peripheral arterial disease in Korean adults. Atherosclerosis 251, 311–318 (2016).
Imai, E. et al. Estimation of glomerular filtration rate by the MDRD study equation modified for Japanese patients with chronic kidney disease. Clin. Exp. Nephrol. 11, 41–50 (2007).
Takeuchi, N., Ekuni, D., Yamamoto, T. & Morita, M. Relationship between the prognosis of periodontitis and occlusal force during the maintenance phase—A cohort study. J. Periodont. Res. 45, 612–617 (2010).
Bahekar, A. A., Singh, S., Saha, S., Molnar, J. & Arora, R. The prevalence and incidence of coronary heart disease is significantly increased in periodontitis: A meta-analysis. Am. Heart J. 154, 830–837 (2007).
Beukers, N. G., van der Heijden, G. J., van Wijk, A. J. & Loos, B. G. Periodontitis is an independent risk indicator for atherosclerotic cardiovascular diseases among 60,174 participants in a large dental school in the Netherlands. J. Epidemiol. Commun. Health 71, 37–42 (2017).
Sanz, M. et al. Periodontitis and cardiovascular diseases: Consensus report. J. Clin. Periodontol. 47, 268–288 (2020).
Haraszthy, V. I., Zambon, J. J., Trevisan, M., Zeid, M. & Genco, R. J. Identification of periodontal pathogens in atheromatous plaques. J. Periodontol. 71, 1554–1560 (2000).
Deshpande, R. G., Khan, M. B. & Genco, C. A. Invasion of aortic and heart endothelial cells by Porphyromonas gingivalis. Infect. Immun. 66, 5337–5343 (1998).
Schenkein, H. A. & Loos, B. G. Inflammatory mechanisms linking periodontal diseases to cardiovascular diseases. J. Periodontol. 84, S51–69 (2013).
Reyes, L., Herrera, D., Kozarov, E., Roldan, S. & Progulske-Fox, A. Periodontal bacterial invasion and infection: Contribution to atherosclerotic pathology. J. Clin. Periodontol. 40 (14), S30–S50 (2013).
Yang, J. et al. Porphyromonas gingivalis infection reduces regulatory T cells in infected atherosclerosis patients. PLoS One 9, e86599. https://doi.org/10.1371/journal.pone.0086599 (2014).
Demmer, R. T. et al. The influence of anti-infective periodontal treatment on C-reactive protein: A systematic review and meta-analysis of randomized controlled trials. PLoS One 8, e77441. https://doi.org/10.1371/journal.pone.0077441 (2013).
Mesa, F. et al. Periodontitis and mechanisms of cardiometabolic risk: Novel insights and future perspectives. Biochim. Biophys. Acta Mol. Basis Dis. 1865, 476–484 (2019).
Asai, K. et al. Tooth loss and atherosclerosis: The Nagahama study. J. Dent. Res. 94, 52S–58S (2015).
Mustapha, I. Z., Debrey, S., Oladubu, M. & Ugarte, R. Markers of systemic bacterial exposure in periodontal disease and cardiovascular disease risk: A systematic review and meta-analysis. J. Periodontol. 78, 2289–2302 (2007).
Desvarieux, M. et al. Changes in clinical and Microbiological periodontal profiles relate to progression of carotid intima-media thickness: The oral infections and vascular disease epidemiology study. J. Am. Heart Assoc. 2, e000254. https://doi.org/10.1161/JAHA.113.000254 (2013).
Soto-Barreras, U. et al. Peripheral arterial disease associated with caries and periodontal disease. J. Periodontol. 84, 486–494 (2013).
Isola, G. et al. Effects of minimally invasive non-surgical therapy on C-reactive protein, lipoprotein-associated phospholipase A(2), and clinical outcomes in periodontitis patients: A 1-year randomized, controlled clinical trial. J. Periodontol. 95, 949–962 (2024).
Isola, G. et al. Effect of quadrantwise versus full-mouth subgingival instrumentation on clinical and microbiological parameters in periodontitis patients: A randomized clinical trial. J. Periodont. Res. 59, 647–656 (2024).
Tamaki, N. et al. Short-term effects of non-surgical periodontal treatment on plasma level of reactive oxygen metabolites in patients with chronic periodontitis. J. Periodontol. 80, 901–906 (2009).
Tamaki, N., Tomofuji, T., Ekuni, D., Yamanaka, R. & Morita, M. Periodontal treatment decreases plasma oxidized LDL level and oxidative stress. Clin. Oral Investig. 15, 953–958 (2011).
Kagamimori, S., Gaina, A. & Nasermoaddeli, A. Socioeconomic status and health in the Japanese population. Soc. Sci. Med. 68, 2152–2160 (2009).
Kanpittaya, B. et al. Periodontitis is associated with arterial stiffness as measured by serial cardio-ankle vascular index (CAVI): A 10-Year cohort study. J. Clin. Periocdontol. 52, 363–374 (2025).
Acknowledgements
The authors wish to thank all the members of Nagasaki Island Study for their time and generosity. We thank Dr. Koji Kawasaki and Dr. Hideaki Hayashida for their oral assessment and examinations.
Funding
This work was supported by a Grant-in-Aid for Scientific Research (C) from the Japan Society for the Promotion of Science (JSPS), KAKENHI, Grant Number JP24K13261.
Author information
Authors and Affiliations
Contributions
N.T. contributed to data analysis and interpretation and wrote the manuscript. M.F., M.K., H.F., R.F., H.Y. and J.M. collected and assembled the data. T.S. (Deceased September 14, 2022) and T.M. contributed to the development of the study concept and design. All authors provided their final approval and agreed to be accountable for all aspects of the study.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tamaki, N., Fukui, M., Kitamura, M. et al. Longitudinal relationship between atherosclerosis and progression of periodontitis in community-dwelling people in Nagasaki Islands Study. Sci Rep 15, 13437 (2025). https://doi.org/10.1038/s41598-025-98377-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-98377-2