Abstract
We aimed to explore the effectiveness of CTH as a serum inflammation biomarker for HCC. Enzyme-linked immunosorbent assay was used to detect serum levels of CTH, interleukin-6 (IL-6), C-reactive protein (CRP), and IL-10. The Scheuer scoring system was used to assess the liver inflammation grading (significant liver inflammation: ≥ G2 grade). CTH levels in the HCC group were significantly elevated (P < 0.0001). Of 146 patients, 58.22% exhibited significant liver inflammation. CTH levels in patients with significant liver inflammation were significantly higher than those in patients with no or mild liver inflammation (< G 2) (p < 0.0001). The area under the Receiver Operating Characteristic (ROC) curve for CTH in predicting significant hepatitis was 0.77 (sensitivity, 81.2%; specificity,62.3%). There was a significant positive correlation (r = 0.50, p < 0.05) between serum CTH levels and histopathological parameter G. The area under the ROC curve for CTH in predicting hepatocellular carcinoma was 0.83 (sensitivity, 64.6%; specificity, 83.3%). CTH and AFP improved the diagnostic accuracy of HCC. CTH levels significantly decreased 6 months post-operation (p < 0.05). The recurrence of HCC caused significant increases in CTH levels. Thus, CTH can serve as a serum inflammation marker for HCC.
Similar content being viewed by others
Introduction
Hepatocellular carcinoma (HCC) is one of the leading causes of cancer-related deaths worldwide. The Global Cancer Observatory (GLOBOCAN) report published by the WHO International Agency for Research on Cancer reports that1 in 2020, HCC incidence accounted for 4.7% of global cancer cases, and for 8.3% of cancer-related deaths, ranking as the 6th most common cancer in incidence and 3rd in mortality. Hepatitis B virus (HBV) causes HCC. In China, 70% of HCC cases are caused by HBV infection2,3,4. Significant liver inflammation is a prominent factor in HCC. Accurately assessing the grading of liver inflammation and controlling its progression early are crucial for improving the long-term prognosis of patients with chronic HBV infection5,6.
The cystathionine gamma-lyase (CTH) gene is located on the short arm of chromosome 1, with a full length of 28,584 bp, composed of 13 exons and 12 introns7. It encodes a cytosolic enzyme: CTH, responsible for the production of endogenous hydrogen sulfide (H2S)8. H2S/CSE system extensively participates in various cellular functions9. H2S is involved in many physiological and pathological processes, such as neural regulation10, hypertension11, pain perception12, diabetes13, inflammation closely related to tumor occurrence14, and angiogenesis15. CTH can promote the progression of various tumors and is significantly elevated in tumors. One study16 used tissue microarray technology to detect the expression of CTH in 32 cases of benign testicular tissue, 88 of seminoma, 34 of embryonal carcinoma, 4 of mature teratoma, and 16 of yolk sac tumor, and compared it with the expression of CSE in benign testicular tissue. Thus, compared to benign testicular tissue, CSE expression is increased in testicular tumors, but no increase is observed in mature teratomas. CTH expression is highest in embryonal carcinoma, which typically has a relatively aggressive clinical course. H2S produced by CTH can promote the occurrence and development of prostate cancer through the interleukin (IL-1β/NF-κB) signaling pathway17. The abundance and activity of CTH are relatively high in neuroblastoma cells18. However, the potential molecular mechanisms and immunological progress of CTH in hepatocellular carcinoma (HCC) remain unclear. Therefore, in this study, we aimed to determine the expression pattern of CTH at different stages of HBV-related liver disease and to explore whether CTH can serve as a serum inflammatory biomarker reflecting disease progression, prognosis, and recurrence in patients with HCC.
Materials and methods
Research subjects
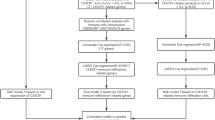
A total of 587 patients with chronic HBV infection were collected from the outpatient departments of the Infectious Disease and Hepatobiliary Surgery Departments at the First Affiliated Hospital of Guangxi Medical University from January 2022 to August 2024. Additionally, 57 healthy volunteers with normal blood routine and biochemical indicators and negative HBV immunological markers were included as a healthy control group.All blood samples in this study were collected and processed equally .The study was conducted with the informed consent of the patients and was approved by the Ethics Committee of the First Affiliated Hospital of Guangxi Medical University (Lot No.: 2024-E726-01).
-
(1)
Inclusion Criteria: (1) Age ≥ 18 years; (2) diagnosis of CHB, LC, and HCC according to the “Guidelines for the Prevention and Treatment of Chronic Hepatitis B (2022 Edition),” “Guidelines for the Diagnosis and Treatment of Cirrhosis” (2019 Edition), and “Guidelines for the Diagnosis and Treatment of Primary Liver Cancer (2024 Edition)”; (3) patients in the liver cancer group, with a blood sample collected prior to undergoing radical surgery, and another blood sample collected six months post-surgery. At the six-month follow-up, follow-up continued for two years if there was no recurrence. Another blood sample was taken in case of recurrence.
-
(2)
Exclusion Criteria: (1) Acute HBV infection; (2) Co-infection with hepatitis C virus (HCV) or human immunodeficiency virus (HIV), and other causes of liver disease (including autoimmune liver disease, alcoholic liver disease, drug-induced liver injury); (3) Co-existing diseases of other major organs such as heart, lung, kidney, or malignant tumors; (4) Pregnant or lactating women; and (5) Patients with a history of acute or chronic inflammation, obesity, diabetes, impaired glucose tolerance (pre-diabetes), or hyperthyroidism in the past three months.
Each patient underwent a medical history assessment and a clinical evaluation. All participants were tested for HBsAg, HCV, and HIV.
Data collection
-
(1)
Observation Indicators (1) General Information: Gender, Age; (2) Serum Biochemical Indicators: AST, ALT, TBIL, AFP; (3) Serum Virological Indicators: HBV DNA, HBsAg; (4) Imaging evaluation of all participants was conducted through abdominal ultrasound.
-
(2)
Research Indicator Detection Methods: The serum levels of CTH, IL-6, CRP, and IL-10 were measured using ELISA kits (double-antibody sandwich enzyme-linked immunosorbent assay) produced by Quanzhou Ruixin Biotechnology Co., Ltd., from the same batch. The enzyme-linked immunosorbent assay kit was used for the quantitative detection of CTH, IL-6, CRP, and IL-10, following the specific procedures outlined in the manual. This kit can be used for the quantitative detection of human CTH, IL-6, CRP, and IL-10 concentrations in samples such as serum, plasma, and cell culture supernatants. Validity period: 6 months; Storage conditions: 2–8°C. The standard curve for each assay must meet r2 ≥ 0.99.
-
(3)
Liver biopsy/Surgical pathological tissue examination: Percutaneous liver biopsy was performed under ultrasound guidance. All biopsy specimens were fixed in formalin, embedded in paraffin, and stained with hematoxylin and eosin. In HCC surgical patients, pathological specimens are prepared and submitted for examination after the excision of the diseased tissue during surgery. The Scheuer scoring system is used to evaluate liver inflammation, with grades G0-1 considered as no or mild inflammation, while grades G2-4 are considered as significant inflammation or moderate to severe inflammation.
Statistical methods
SPSS 26.0 software (SPSS, Inc., Chicago, IL, USA) was used for statistical analysis. Data with a normal distribution are expressed as mean ± standard deviation (X ± S), and analyzed using analysis of variance; Data with a non-normal distribution are expressed as median and interquartile range [M(P25, P75)], and analyzed using the rank-sum test. The comparison of rates between groups was performed using the Chi-square test. Spearman correlation analysis was used to assess the correlation between CTH and histopathological parameters G, and the diagnostic capability of anti-CTH for significant inflammation and hepatocellular carcinoma was evaluated through the Receiver Operating Characteristic (ROC) curve. The cutoff value was determined by the Youden Index, which represents the best combination of sensitivity and specificity. Statistical significance was defined as p < 0.05.
Results
Patient demographics and clinical characteristics
A total of 644 participants were included in this study and divided into four groups. The healthy control group comprised 57 healthy individuals, among which 33 (7.35%) were male, and 24 (12.31%) were female, with an average age of 42.6 ± 13.51 years. The Chronic Hepatitis B group comprised 254 patients, of which 148 (32.96%) were male and 106 (54.36%) were female, with an average age of 41.11 ± 10.71 years. The Cirrhosis group comprised 206 patients with cirrhosis following chronic HBV infection, of which 158 (35.19%) were male and 48 (24.62%) were female, with an average age of 49.24 ± 10.58 years. The Liver cancer group comprised 127 patients with hepatitis B-related hepatocellular carcinoma, of which 110 (24.50%) were male and 17 (8.72%) were female, with an average age of 53.17 ± 11.87 years. There were significant differences among the four study groups in terms of AST, ALT, TBIL, HBV DNA, HBsAg, and AFP levels (P < 0.001). The serum HBsAg level in the Chronic Hepatitis B group was higher than that in the Cirrhosis group and the Liver Cancer group. The serum TBIL level in the Cirrhosis group was significantly higher than that in the Healthy Control group, Chronic Hepatitis B group, and Liver Cancer group. The Liver Cancer group exhibited higher levels of serum AST, ALT, AFP, and HBV DNA load (Table 1).
Expression levels of CTH, IL-6, CRP, and IL-10 in the healthy control group and chronic HBV infection group
We used ELISA kits to measure serum levels of CTH, IL-6, CRP, and IL-10 in the control and the chronic HBV infection group (Fig. 1). Compared to the control group (7.69 ± 1.83 ng/ml), the serum CTH levels were significantly increased in the Chronic Hepatitis B group (9.98 ± 1.9 ng/ml), the Cirrhosis group (11.54 ± 1.79 ng/ml), and the Liver Cancer group (13.52 ± 2.21 ng/ml) (P < 0.0001) (Fig. 1a). In the Liver Cancer group (153.43 ± 36.71 pg/ml), the expression level of IL-6 was significantly higher than that in the LC group (130.87 ± 30.62 pg/ml), the Chronic Hepatitis B group (110.62 ± 31.43 pg/ml), and the Healthy Control group (103.24 ± 36.68 pg/ml) (P < 0.0001). There was no significant difference between the CHB group and the Healthy Control group (P > 0.05) (Fig. 1b). In the liver cancer group, the expression level of CRP (16.6 ± 4.54 ng/ml) was significantly higher than that in the LC (13.33 ± 3.74 ng/ml), CHB (11.60 ± 4.02 ng/ml), and healthy control (9.98 ± 2.41 ng/ml) groups (P < 0.0001) (Fig. 1c). For the cytokine IL-10, there was a significant difference between the healthy control group (309.56 ± 106.22 pg/ml) and the chronic hepatitis B (196.22 ± 103.51 pg/ml) (P < 0.05), cirrhosis (178.8 ± 85.61 pg/ml) (P < 0.001), and liver cancer (109.07 ± 74.68 pg/ml) groups (P < 0.0001). There was no significant difference between the CHB group and the LC group (P > 0.05). As the disease progressed, the expression level of IL-10 gradually decreased (Fig. 1d).
Association between serum levels of CTH, IL-6, CRP, and IL-10 and liver inflammation grading
As shown in Fig. 2, the levels of CTH (13.12 ± 2.4 ng/ml), IL-6 (155.52 ± 40.5 pg/ml), and CRP (16.28 ± 4.97 ng/ml) in patients with significant inflammation (G2-4) were significantly higher than those in patients with no or mild inflammation (G0-1) (10.79 ± 2.17 ng/ml, 127.18 ± 32.2 pg/ml, and 12.26 ± 5.68 ng/ml, respectively; P < 0.0001). The IL-10 level (99.50 ± 85.02 pg/ml) in patients with significant inflammation (G2-4) was significantly lower than that in patients with no or mild inflammation (G0-1) (149.62 ± 89.37 pg/ml), P < 0.0001.
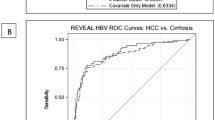
The efficacy of serum CTH, IL-6, CRP, and IL-10 in diagnosing significant inflammation
The diagnostic accuracy of serum CTH, IL-6, CRP, and IL-10 for significant inflammation was assessed using the Receiver Operating Characteristic (ROC) curve (Fig. 3 and Table 2). The area under the curve (AUC) for predicting significant hepatitis using CTH, IL-6, CRP, and IL-10 levels were 0.77, 0.70, 0.73, and 0.69, respectively (95% Confidence Intervals:[0.69–0.85)], [0.62–0.79], [0.64–0.82], and [0.60–0.78), respectively, with sensitivities of 81.2%, 45.9%, 77.6%, and 67.1%, respectively, and specificity is 62.3%, 86.9%, 65.6%, and 68.9% respectively.
Correlation between CTH, IL-6, CRP, and IL-10 and pathological parameter G
In the HBV infection group, CTH (r = 0.50, P < 0.0001), IL-6 (r = 0.33, P < 0.0001), and CRP (r = 0.37, P < 0.0001) showed a significant positive correlation with G, while IL-10 (r = − 0.34, P < 0.0001) showed a significant negative correlation with G (Fig. 4a). In the Chronic Hepatitis B group, CTH (r = 0.41, P = 0.01) showed a significant positive correlation with G, while IL-6 (r = 0.17, P = 0.33), CRP (r = 0.23, P = 0.17), and IL-10 (r = − 0.11, P = 0.53) did not show significant correlations with G (Fig. 4b). In the Cirrhosis group, CTH (r = 0.42, P = 0.04) exhibited a significant positive correlation with G, whereas IL-6 (r = 0.32, P = 0.12), CRP (r = 0.29, P = 16), and IL-10 (r = − 0.32, P = 0.12) did not show significant correlations with pathological G (Fig. 4c). In the Liver cancer group, CTH (r = 0.47, P < 0.0001), IL-6 (r = 0.38, P < 0.0001), and CRP (r = 0.36, P = 0.001) are significantly positively correlated with G, while IL-10 (− 0.35, P = 0.001) shows a significant negative correlation with G (Fig. 4d).
Immunohistochemistry images and correlation analysis of CTH, IL-6, CRP, and IL-10 with pathological parameter G in HBV infection group, CHB, LC, and HCC groups. (a) represents CHB immunohistochemistry; (b) represents LC immunohistochemistry; Figure c represents HCC immunohistochemistry. The bar chart indicates HBsAg( +). AFP alpha-fetoprotein; CHB chronic hepatitis B; CRP C-reactive protein; CTH Cystathionine γ-lyase; HBV Hepatitis B virus; HCC hepatocellular carcinoma; IL interleukin; LC cirrhosis.
Serum CTH, IL-6, CRP, IL-10, AFP, and the combined efficacy of CTH + AFP in HCC diagnosis
The ROC curve shows that the area under the curve (AUC) for diagnosing HCC using CTH, IL-6, CRP, IL-10, and AFP is 0.83, 0.77, 0.78, 0.76, and 0.82, respectively. The combined diagnosis of HCC with AFP + CTH had an AUC of 0.88, which is superior to any single test value mentioned above (95% confidence intervals: [0.79–0.87], [0.72–0.81], [0.73–0.82], [0.72–0.81], [0.77–0.86], and [0.84–0.91]), with sensitivities of 64.6%, 77.2%, 68.5%, 60.6%, 70.9%, and 73.2%, respectively, and specificities of 83.3%, 65.0%, 79.8%, 81.7%, 82.2%, and 85.2%, respectively (Fig. 5 and Table 3).
Association of serum CTH, IL-6, CRP, and IL-10 levels with HCC BCLC staging
In patients with early (BCLC A stage, n = 82 cases), intermediate (BCLC B stage, n = 17 cases), and advanced (BCLC C stage, n = 28 cases) HCC, the expression of CTH in advanced stage (15.33 ± 1.98 ng/ml) HCC patients was higher than in early (12.8 ± 2.02 ng/ml) and intermediate (13.99 ± 1.64 ng/ml) patients (P < 0.0001) (Fig. 6a,b). The expression level of IL-6 in patients with late-stage (164.68 ± 25.47 pg/ml) HCC was significantly higher than that in patients with early-stage (148.53 ± 39.96 pg/ml) HCC (P < 0.05). The expression of CRP in patients with late-stage (18.92 ± 4.81 ng/ml) HCC was higher than that in patients with early-stage (15.92 ± 4.48 ng/ml) and mid-stage (16.06 ± 3.12 ng/ml) HCC (P < 0.05). There was no significant difference in IL-10 expression among patients with early-stage, mid-stage, and late-stage HCC patients.
According to the classifications of BCLC system, the correlations (a) serum CTH concentrations (b) serum IL-6 concentrations (c) serum CRP concentrations (d) serum IL-10 concentrations in different-stage hepatocellular carcinoma patients. *P < 0.05 was defined as statistically significant. CRP C-reactive protein; CTH Cystathionine γ-lyase; IL interleukin.
Expression levels of serum CTH, IL-6, CRP, and IL-10 in the CHB, LC, preoperative HCC, and postoperative 6-month HCC groups
Almost all HBV-related HCC in China develops from LC, therefore, further analysis was conducted on the differences in the expression of CTH, IL-6, CRP, and IL-10 between the CHB group, LC group, preoperative group, and postoperative 6-month group. In the postoperative 6-month group, the CTH expression level (10.57 ± 2.02 ng/ml) was significantly lower than that of the cirrhosis group (11.54 ± 1.79 ng/ml) (P < 0.05), with no significant difference compared to the chronic Hepatitis B group (Fig. 7a). The pro-inflammatory cytokine IL-6 expression level in the postoperative 6-month group (142.64 ± 33.34 pg/ml) was significantly higher than that in the chronic Hepatitis B group (110.62 ± 31.43 pg/ml) and the cirrhosis group (130.87 ± 30.62 pg/ml) (Fig. 7b). The expression level CRP in the postoperative 6-month group (12.77 ± 5.48 ng/ml) showed no significant difference compared to the chronic Hepatitis B group (11.6 ± 4.02 ng/ml) and the cirrhosis group (13.33 ± 3.74 ng/ml) (Fig. 7c). In the postoperative 6-month non-recurrence group (131.47 ± 46.84 pg/ml), the expression level of the anti-inflammatory cytokine IL-10 was significantly lower than that in the chronic Hepatitis B group (196.22 ± 103.51 pg/ml) and the cirrhosis group (178.8 ± 85.61 pg/ml) (Fig. 7d, Table 4).
Expression of CTH, IL-6, CRP, and IL-10 in the CHB group, LC group, pre-operative HCC group, and post-operative 6-month group (*P < 0.05; **P < 0.01; ***P < 0.001; ****P < 0.0001). CHB chronic hepatitis B; CRP C-reactive protein; CTH Cystathionine γ-lyase; HCC hepatocellular carcinoma; IL interleukin; LC cirrhosis.
Expression levels of CTH, IL-6, CRP, and IL-10 in pre-operative, post-operative, and recurrent HCC
There is no significant difference in serum expression levels of CTH, IL-6, CRP, and IL-10 between the pre-operative and recurrent groups. However, compared to the pre-surgery group, the expression level of CTH in the post-surgery group significantly decreased, and as HCC recurred, the CTH level increased again. The level of IL-10 showed the opposite trend, with the post-surgery group having significantly higher IL-10 levels than the pre-surgery group, and the IL-10 level decreased with the recurrence of HCC. There was no significant difference in the levels of IL-6 and CRP between the post-surgery group and the recurrence group (Tables 3, 5, Fig. 8).
Discussion
Chronic inflammation is associated with the occurrence, progression, invasion, and metastasis of tumors19,20,21,22,23,24,25,26,27. HBV-related hepatocellular carcinoma is a typical inflammation-associated malignant tumor28,29,30.
In this study, as the disease progressed, the CTH level gradually increased, with the highest levels observed in the hepatocellular carcinoma group, significantly higher than those in the LC, CHB, and the healthy control groups. During inflammatory stimulation, the immune response triggered by the activation of Toll-like receptors (TLR) stimulates the upregulation of CTH and the concomitant production of H2S, which is a pro-inflammatory mediator produced by the activation of CTH in macrophages31,32, further activating macrophages33. Macrophages play a key role in the inflammatory response. The long-term high expression of CTH in chronic liver inflammation reflects the severity and persistence of inflammation of liver tissue. Persistent upregulation signifies that hepatocytes are constantly undergoing degeneration, necrosis, and regeneration, leading to an imbalance in the overall liver microenvironment, promoting fibrous proliferation, the formation of pseudo-lobules, and the gradual progression of chronic hepatitis to the cirrhosis stage34,35. A study36 introduced the normal hepatocyte line, HL-7702 and two liver cancer cell lines, HepG2 and PLC/PRF/5. CTH was overexpressed in the liver cancer cell lines HepG2 and PLC/PRF/5. Inhibition of the endogenous H2S/CSE pathway significantly reduced the proliferation of HepG2 and PLC/PRF/5 cells, enhanced the generation of reactive oxygen species (ROS), led to mitochondrial disruption, exacerbated DNA damage, and increased apoptosis. These findings are consistent with the results of our experiment, indicating that CTH levels gradually increase with disease progression. Thus, CTH can serve as a novel inflammatory marker for monitoring disease progression. The pathogenesis of HBV is not due to the direct action of HBV on the body, but the activation of the body’s immune system following HBV infection, which leads to an inflammatory response, ultimately causing liver tissue damage37,38,39,40. Clinical manifestations include chronic hepatitis, LC, and HCC40,41,42,43,44. The outcome of HBV infection is influenced by both viral and host characteristics. Innate and adaptive immunity, play a crucial role in initiating and regulating immune responses. IL-6, CRP, and IL-10 are associated with HBV infection and disease onset. IL-6 is one of the most important cytokines in the process of HBV infection. It is produced by macrophages, promoting tumor growth and progression by facilitating chronic inflammation45. In HBV infection, IL-6 can stimulate the immune response through infected hepatocytes to eliminate the virus; or it can induce the occurrence of CHB, LC, and HCC46. Here, the levels of IL-6 in the CHB, LC, and HCC groups were significantly higher than those in the HI group, confirming the results of the aforementioned studies. C-reactive protein (CRP) is a sensitive acute-phase reactant synthesized by the human liver. When the body is in an inflammatory state, serum CRP levels increase. Li et al.47 used a fully automated biochemical analyzer to detect the serum CRP levels in patients with chronic HBV infection and healthy controls. The differences in serum CRP levels among patients with Chronic Hepatitis B (CHB), Cirrhosis (LC), and Hepatocellular Carcinoma (HCC) were compared and analyzed. Serum CRP levels in patients with hepatitis B were significantly elevated (P < 0.05). The CRP levels in patients with LC and HCC were significantly higher than that in those with chronic hepatitis B. This is consistent with the results of our experiment thus, CRP is a protein marker capable of reflecting various acute and chronic inflammation diseases48,49. IL-10 can limit immune cell activation and cytokine production by innate immune cell types50. Here, the expression level of IL-10 in the HI group was significantly higher than that in the CHB, LC, and HCC groups, which, in contrast to the expression levels of pro-inflammatory factors CTH, IL-6, and CRP, also confirmed the other research conclusions.
Current guidelines recommend that accurately assessing the grading of liver inflammation and early controlling the development of inflammation is crucial for improving the long-term prognosis of patients with chronic HBV infection. Wu et al.51 explored whether anti-HBc could serve as a predictive indicator for significant liver inflammation in patients with chronic HBV infection. Overall, 117 patients were included, among whom 50 patients (42.7%) exhibited significant liver inflammation. The serum anti-HBc levels in patients with significant liver inflammation were significantly higher than that in those with no or mild liver inflammation (< G2) (p < 0.001). The area under the ROC curve for serum anti-HBc in predicting significant liver inflammation was 0.769, with an optimal cutoff value of 10.87 S/CO, a sensitivity of 59.2%, and a specificity of 87.9%. We analyzed the severity of liver inflammation in patients with chronic HBV infection and assessed the accuracy of CTH, IL-6, CRP, and IL-10 levels in predicting the presence of significant inflammation. Overall, 58.2% of the patients had significant inflammation. CTH, IL-6, CRP, and IL-10 had high accuracy in predicting significant inflammation.
CTH, IL-6, CRP, and IL-10 were useful biomarkers for reflecting liver inflammation. Moreover, CTH showed a significant positive correlation with pathological parameter G in the CHB group, LC group, and HCC group, indicating that CTH can be used as a novel and reliable biomarker to assess the persistent state of inflammation in high-risk Hepatitis B populations and predict the risk of disease occurrence during the early stages of disease. This provides the feasibility of finding corresponding interventions in the process of chronic inflammation progressing to liver cancer, thereby preventing or to some extent reversing the development towards cirrhosis and liver cancer.
Since the discovery of AFP in the 1970s, remained the only widely used serological marker for HCC. However, its diagnostic capability is debatable. Elevated serum AFP is observed in only 60–70% of HCC patients, and this proportion drops to just 33–65% in HCC patients with tumors smaller than 3 cm in diameter52,53. Moreover, non-specific elevation of serum AFP concentrations occur in patients with non-malignant chronic liver diseases, such as those with CHB (15–58%) and LC (11–47%)54,55,56. Therefore, there is an urgent need to develop more effective alternative diagnostic methods to supplement AFP and improve clinical outcomes. The ROC curve in this study indicates that serum CTH, IL-6, CRP, and IL-10 levels contribute to the diagnosis of hepatitis B-related liver cancer. However, the AUC and specificity of CTH are significantly superior to IL-6, CRP, and IL-10. Moreover, CTH combined with AFP can effectively diagnose the occurrence of hepatitis B-related liver cancer.
In over 90% of cases, hepatocellular carcinoma (HCC) develops following cirrhosis. Here, the immune status of patients in the non-recurrent group 6 months post-operation is similar to that of patients with chronic hepatitis B (CHB) and cirrhosis (LC), mainly reflected in their inflammatory phenotype, as they no longer exhibit the phenotype induced by cancer cells. Therefore, both HCC and cirrhosis significantly affect patient survival rates and simultaneously determine treatment applicability and effectiveness. The Barcelona staging system is a Liver cancer clinical staging system, the introduction of which will help assess the patient’s condition, provide accurate treatment plans, and predict patient prognosis. In this study, among HCC patients, the expression of CTH in advanced HCC patients was higher than that in early and intermediate-stage patients, and the CTH level in intermediate-stage HCC patients was higher than that in early-stage patients. The expression level of IL-6 in advanced HCC patients was significantly higher than that in early-stage HCC patients. CRP expression in advanced-stage HCC patients is higher than in early and intermediate-stage patients. This indicates that the expression levels of serum CTH, IL-6, and CRP are closely related to the malignancy of HBV-related hepatocellular carcinoma. The higher the levels of serum CTH, IL-6, and CRP, the greater the malignancy of hepatocellular carcinoma and the worse the patient’s prognosis.
CTH expressed in the tumor microenvironment supports the formation of glioblastoma without affecting the microvascular density of the tumor. Further, High expression of CTH in human GBM tumors is associated with poorer overall survival. In mouse or human GBM cells, pharmacological inhibition (PAG) or CTH knockdown (siRNA) can reduce the proliferation, migration, and stem cell formation frequency of GBM cells57. In this study, the high preoperative expression of CTH in the HCC group, the significant decrease in CTH levels postoperatively, and the rise in CTH levels upon recurrence suggest that CTH may be secreted by cancer cells. The dynamic changes in CTH levels before and after surgery and upon recurrence indicate that CTH can be used as a biomarker to reflect disease prognosis and recurrence. Chau GY58 and others reported that tumor cells secrete IL-10 which significantly decrease after hepatocellular carcinoma (HCC) resection. Further, serum IL-10 concentration is a factor for poor prognosis and can lead to a significantly shortened median survival period59,60. Contrarily, IL-10 levels measured by Su Z et al. in the liver cancer group were significantly lower than those in the Chronic Hepatitis B (CHB) group61. Here, postoperative IL-10 levels increased and decreased after recurrence, consistent with the findings of Su Z et al.
In conclusion, our study highlight the fluctuation of CTH in the progression of HBV infection-related diseases. Thus, CTH can serve as a biomarker for the progression of HBV-related diseases. Serum CTH is an effective diagnostic marker for HCC, complementing AFP. Compared to individual testing, the combined detection of CTH and AFP improves the diagnostic accuracy for HCC. Serum CTH measurement assess the persistence of inflammation in high-risk Hepatitis B populations the feasibility of predicting liver cancer risk, and is an independent marker for prognosis and recurrence in HCC patients.
Data availability
The datasets generated and analyzed during the present study are available from the corresponding author upon reasonable request.
References
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA. Cancer J. Clin. 71, 209–249. https://doi.org/10.3322/caac.21660 (2021).
de Martel, C., Maucort-Boulch, D., Plummer, M. & Franceschi, S. World-wide relative contribution of hepatitis B and C viruses in hepatocellular carcinoma. Hepatology 62, 1190–1200. https://doi.org/10.1002/hep.27969 (2015).
Liu, J. et al. Seroepidemiology of hepatitis B virus infection in 2 million men aged 21–49 years in rural China: A population-based, cross-sectional study. Lancet Infect. Dis. 16, 80–86. https://doi.org/10.1016/S1473-3099(15)00218-2 (2016).
Huang, J., Qiu, G. & Zeng, Y. Advances in surgical treatment of hepatocellular carcinoma. Surg. Theory Pract. 27, 113–118 (2022).
European Association for the Study of the Liver. EASL 2017 clinical practice guidelines on the management of hepatitis B virus infection. J. Hepatol. 67, 370–398. https://doi.org/10.1016/j.jhep.2017.03.021 (2017).
Terrault, N. A. et al. Update on prevention, diagnosis, and treatment of chronic hepatitis B: AASLD 2018 hepatitis B guidance. Hepatology 67, 1560–1599. https://doi.org/10.1002/hep.29800 (2018).
Jurkowska, H., Kaczor-Kamińska, M., Bronowicka-Adamska, P. & Wróbel, M. Cystathionine γ-lyase. Postepy. Hig. Med. Dosw. 68, 1–9. https://doi.org/10.5604/17322693.1085372 (2014).
Giannakopoulou, E. et al. Association study of the CTH 1364 G>T polymorphism with coronary artery disease in the Greek population. Drug. Metab. Pers. Ther. 34, 20180033. https://doi.org/10.1515/dmpt-2018-0033 (2019).
Yin, P. et al. Sp1 is involved in regulation of cystathionine γ-lyase gene expression and biological function by PI3K/Akt pathway in human hepatocellular carcinoma cell lines. Cell Signal 24, 1229–1240. https://doi.org/10.1016/j.cellsig.2012.02.003 (2012).
Boehning, D. & Snyder, S. H. Novel neural modulators. Annu. Rev. Neurosci. 26, 105–131. https://doi.org/10.1146/annurev.neuro.26.041002.131047 (2003).
Yang, G. et al. H2S as a physiologic vasorelaxant: Hypertension in mice with deletion of cystathionine gamma-lyase. Science 322, 587–590. https://doi.org/10.1126/science.1162667 (2008).
Kawabata, A. et al. Hydrogen sulfide as a novel nociceptive messenger. Pain 132, 74–81. https://doi.org/10.1016/j.pain.2007.01.026 (2007).
Yusuf, M. et al. Streptozotocin-induced diabetes in the rat is associated with enhanced tissue hydrogen sulfide biosynthesis. Biochem. Biophys. Res. Commun. 333, 1146–1152. https://doi.org/10.1016/j.bbrc.2005.06.021 (2005).
Li, L., Bhatia, M. & Moore, P. K. Hydrogen sulphide–a novel mediator of inflammation?. Curr. Opin. Pharmacol. 6, 125–129. https://doi.org/10.1016/j.coph.2005.10.007 (2006).
Cai, W. J. et al. The novel proangiogenic effect of hydrogen sulfide is dependent on Akt phosphorylation. Cardiovasc. Res. 76, 29–40. https://doi.org/10.1016/j.cardiores.2007.05.026 (2007).
Ozluk, E. et al. Cystathionine gamma-lyase is increased in testicular seminomas, embryonal, and yolk sac tumors. Anticancer Res. 41, 4211–4214. https://doi.org/10.21873/anticanres.15225 (2021).
Wang, Y. H. et al. Dysregulation of cystathionine γ-lyase promotes prostate cancer progression and metastasis. EMBO. Rep. 20, e45986. https://doi.org/10.15252/embr.201845986 (2019).
Bronowicka-Adamska, P., Bentke, A. & Wróbel, M. Hydrogen sulfide generation from l-cysteine in the human glioblastoma-astrocytoma U-87 MG and neuroblastoma SHSY5Y cell lines. Acta. Biochim. Pol. 64, 171–176. https://doi.org/10.18388/abp.2016_1394 (2017).
Balkwill, F. & Mantovani, A. Inflammation and cancer: Back to Virchow?. Lancet 357, 539–545. https://doi.org/10.1016/S0140-6736(00)04046-0 (2001).
Okada, F. Inflammation-related carcinogenesis: Current findings in epidemiological trends, causes and mechanisms. Yonago Acta. Med. 57, 65–72 (2014).
Feng, J. F., Huang, Y. & Chen, Q. X. A new inflammation index is useful for patients with esophageal squamous cell carcinoma. Onco. Targets Ther. 7, 1811–1815. https://doi.org/10.2147/OTT.S68084 (2014).
Nishikawa, H. et al. Pre-treatment C-reactive protein as a prognostic factor for recurrence after surgical resection of hepatocellular carcinoma. Anticancer Res. 33, 1181–1188 (2013).
Zhao, X., Luo, J., Li, B., Liu, S. & Li, D. The association between preoperative serum C-reactive protein and hepatocellular carcinoma recurrence in patients with chronic hepatitis B virus (HBV) infection–a retrospective study. PLoS ONE 10, e0116909. https://doi.org/10.1371/journal.pone.0116909 (2015).
He, X., Wang, Y. & Zhang, W. Screening differential expression of serum proteins in AFP-negative HBV-related hepatocellular carcinoma using iTRAQ-MALDI-MS/MS. Neoplasma 61, 17–26 (2014).
Imai, N. et al. Persistent elevated C-reactive protein after treatment is an independent marker of a poor prognosis in patients with hepatocellular carcinoma. Clin. Transl. Oncol. 15, 575–581. https://doi.org/10.1007/s12094-012-0976-y (2013).
Sieghart, W. et al. Single determination of C-reactive protein at the time of diagnosis predicts long-term outcome of patients with hepatocellular carcinoma. Hepatology 57, 2224–2234. https://doi.org/10.1002/hep.26057 (2013).
Liu, C. et al. Interleukin-23A is associated with tumor growth in Helicobacter-pylori-related human gastric cancer. Cancer Cell Int. 14, 104. https://doi.org/10.1186/s12935-014-0104-x (2014).
Szabo, G. & Lippai, D. Molecular hepatic carcinogenesis: impact of inflammation. Dig. Dis. 30, 243–248. https://doi.org/10.1159/000336913 (2012).
Morales-Sánchez, A. & Fuentes-Pananá, E. M. Human viruses and cancer. Viruses 6, 4047–4079. https://doi.org/10.3390/v6104047 (2014).
Chen, Y., Williams, V., Filippova, M., Filippov, V. & Duerksen-Hughes, P. Viral carcinogenesis: Factors inducing DNA damage and virus integration. Cancers (Basel) 6, 2155–2186. https://doi.org/10.3390/cancers6042155 (2014).
Wallace, J. L., Ferraz, J. G. & Muscara, M. N. Hydrogen sulfide: An endogenous mediator of resolution of inflammation and injury. Antioxid. Redox Signal. 17, 58–67. https://doi.org/10.1089/ars.2011.4351 (2012).
Zheng, Y. et al. Lipopolysaccharide regulates biosynthesis of cystathionine γ-lyase and hydrogen sulfide through Toll-like receptor-4/p38 and Toll-like receptor-4/NF-κB pathways in macrophages. In Vitro Cell Dev. Biol. Anim. 49, 679–688. https://doi.org/10.1007/s11626-013-9659-4 (2013).
Badiei, A., Muniraj, N., Chambers, S. & Bhatia, M. Inhibition of hydrogen sulfide production by gene silencing attenuates inflammatory activity by downregulation of NF-κB and MAP kinase activity in LPS-activated RAW 264.7 cells. Biomed. Res. Int. 2014, 848570. https://doi.org/10.1155/2014/848570 (2014).
Ci, L., Yang, X. & Gu, X. Cystathionine γ-lyase deficiency exacerbates CCl(4)-induced acute hepatitis and fibrosis in the mouse liver. Antioxid. Redox Signal. 27, 133–149 (2017).
Yamada, H. et al. Methionine excess in diet induces acute lethal hepatitis in mice lacking cystathionine γ-lyase, an animal model of cystathioninuria. Free Radic. Biol. Med. 52, 1716–1726. https://doi.org/10.1016/j.freeradbiomed.2012.02.033 (2012).
Pan, Y. et al. Hydrogen sulfide (H2S)/cystathionine γ-lyase (CSE) pathway contributes to the proliferation of hepatoma cells. Mutat. Res. 763–764, 10–18. https://doi.org/10.1016/j.mrfmmm.2014.03.002 (2014).
Ferrari, C. HBV and the immune response. Liver Int. 35, 121–128 (2015).
Bertoletti, A. & Gehring, A. J. The immune response during hepatitis B virus infection. J. Gen. Virol. 87, 1439–1449. https://doi.org/10.1099/vir.0.81920-0 (2006).
Huang, C. F., Lin, S. S., Ho, Y. C., Chen, F. L. & Yang, C. The immune response induced by hepatitis B virus principal antigens. Cell Mol. Immunol. 3, 97–106 (2006).
Tan, A. T., Koh, S. & Goh, V. Understanding the immunopathogenesis of chronic hepatitis B virus: An Asian prospective. J. Gastroenterol. Hepatol. 23, 833–843. https://doi.org/10.1111/j.1440-1746.2008.05385.x (2008).
Ganem, D. & Prince, A. M. Hepatitis B virus infection–natural history and clinical consequences. N. Engl. J. Med. 350, 1118–1129. https://doi.org/10.1056/NEJMra031087 (2004).
Yim, H. J. & Lok, A. S. Natural history of chronic hepatitis B virus infection: What we knew in 1981 and what we know in 2005. Hepatology 43, S173-181. https://doi.org/10.1002/hep.20956 (2006).
Tanaka, M. et al. Hepatitis B and C virus infection and hepatocellular carcinoma in China: A review of epidemiology and control measures. J. Epidemiol. 21, 401–416. https://doi.org/10.2188/jea.je20100190 (2011).
Xu, R., Zhang, Z. & Wang, F. S. Liver fibrosis: Mechanisms of immune-mediated liver injury. Cell Mol. Immunol. 9, 296–301. https://doi.org/10.1038/cmi.2011.53 (2012).
Lan, T., Chang, L., Wu, L. & Yuan, Y. F. IL-6 plays a crucial role in HBV infection. J. Clin. Transl. Hepatol. 3, 271–276. https://doi.org/10.14218/JCTH.2015.00024 (2015).
Vinhaes, C. L. et al. Chronic hepatitis B infection is associated with increased molecular degree of inflammatory perturbation in peripheral blood. Viruses 12, 864. https://doi.org/10.3390/v12080864 (2020).
Hao, S., Wang, Y., Gao, G. & Li, Z. Hepatitis B virus upregulates the expression of C-reactive protein both in vivo and in vitro. Ann. Clin. Lab. Sci. 47, 432–435 (2017).
Black, S., Kushner, I. & Samols, D. C-reactive protein. J. Biol. Chem. 279, 48487–48490. https://doi.org/10.1074/jbc.R400025200 (2004).
Agrawal, A. CRP after 2004. Mol. Immunol. 42, 927–930 (2005).
York, A. G. et al. IL-10 constrains sphingolipid metabolism to limit inflammation. Nature 627, 628–635. https://doi.org/10.1038/s41586-024-07098-5 (2024).
Yao, K. et al. Association of anti-HBc and liver inflammation in HBeAg-negative chronic hepatitis B virus-infected patients with normal ALT and detectable HBV DNA. J. Med. Virol. 94, 659–666. https://doi.org/10.1002/jmv.27327 (2022).
Patel, M. et al. Hepatocellular carcinoma: Diagnostics and screening. J. Eval. Clin. Pract. 18, 335–342. https://doi.org/10.1111/j.1365-2753.2010.01599.x (2012).
Shariff, M. I. et al. Hepatocellular carcinoma: Current trends in worldwide epidemiology, risk factors, diagnosis and therapeutics. Expert Rev. Gastroenterol Hepatol. 3, 353–367. https://doi.org/10.1586/egh.09.35 (2009).
Shen, Q. et al. Serum DKK1 as a protein biomarker for the diagnosis of hepatocellular carcinoma: A large-scale, multicentre study. Lancet Oncol. 13, 817–826. https://doi.org/10.1016/S1470-2045(12)70233-4 (2012).
Chen, W. et al. Association between C-reactive protein, incident liver cancer, and chronic liver disease mortality in the Linxian nutrition intervention trials: A nested case-control study. Cancer Epidemiol. Biomark. Prev. 24, 386–392. https://doi.org/10.1158/1055-9965.EPI-14-1038 (2015).
Sherman, M. & Colombo, M. Hepatocellular carcinoma screening and diagnosis. Semin. Liver Dis. 34, 389–397. https://doi.org/10.1055/s-0034-1394139 (2014).
Peleli, M. et al. Cystathionine gamma-lyase (CTH) inhibition attenuates glioblastoma formation. Redox Biol. 64, 102773. https://doi.org/10.1016/j.redox.2023.102773 (2023).
Chau, G. Y. et al. Serum interleukin-10 but not interleukin-6 is related to clinical outcome in patients with resectable hepatocellular carcinoma. Ann. Surg. 231, 552–558. https://doi.org/10.1097/00000658-200004000-00015 (2000).
Hattori, E. et al. Possible contribution of circulating interleukin-10 (IL-10) to anti-tumor immunity and prognosis in patients with unresectable hepatocellular carcinoma. Hepatol. Res. 27, 309–314. https://doi.org/10.1111/j.1478-3231.2004.00882.x (2003).
Chan, S. L. et al. A study of circulating interleukin 10 in prognostication of unresectable hepatocellular carcinoma. Cancer 118, 3984–3992. https://doi.org/10.1002/cncr.26726 (2012).
Su, Z. et al. Circulating IL-1β, IL-17, and IP-10 as potential predictors of hepatitis b virus infection prognosis. J. Immunol. Res. 2022, 5202898. https://doi.org/10.1155/2022/5202898 (2022).
Acknowledgements
We appreciate the experimental support from the First Affiliated Hospital of Guangxi Medical University
Funding
This work was supported by the National Natural Science Foundation of China (Grant Numbers: 82160123, 81960115, 82260124); Key Laboratory of High-Incidence-Tumor Prevention and Treatment (Guangxi Medical University), Ministry of Education (Grant Number: GKE-ZZ202107); and Guangxi Key Laboratory of Early Prevention and Treatment for Regional High Frequency Tumor (Grant Number: GKE-ZZ202218).
Author information
Authors and Affiliations
Contributions
Chao Jin was responsible for conception, paper writing, statistical analysis, chart drawing ; Minghua Su was responsible for reviewing and revising the article, and financial support; Jianning Jiang, Bobin Hu, and Rongming Wang provided writing guidance ; Hongyu Liu was responsible for patient follow-up and data collection.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
All procedures involving human participants were performed in accordance with the ethical standards of the institutional and/or national research committee and the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was conducted in Guangxi Province on October 14, 2024, and approved by the Medical Ethics Committee of the First Affiliated Hospital of Medical University (Lot No.: 2024-E726-01).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jin, C., Hu, B., Liu, H. et al. Cystathionine gamma-lyase as an inflammatory factor and its link with immune inflammation in hepatitis B virus-related liver disease. Sci Rep 15, 17777 (2025). https://doi.org/10.1038/s41598-025-98922-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-98922-z