Abstract
Brain functional changes and gut microbiota dysbiosis have been observed in perimenopausal syndrome (PMS). We evaluated the effects of a plant-based daily diet enriched with Raphanus sativus L. (RSL, radish seed) on the gut microbiota composition, gastrointestinal symptoms, resting-state local spontaneous brain activity, and neuropsychology in perimenopausal women. For 12 weeks, the participants were instructed to adhere to a controlled, Raphanus sativus L.-rich plant-based diet (a mean RSL intake of 5 g/day). Two test days were organized: before and after the nutritional intervention. The fecal microbiota composition, gastrointestinal symptoms, resting-state brain function, and neuropsychology were assessed twice. A longitudinal single-arm study was conducted on 24 perimenopausal women. The Montreal Cognitive Assessment (MoCA) scores tended to improve in the visuospatial/executive function subitem and in the total score after the diet. The participants presented elevated amplitude of low-frequency fluctuation (ALFF) values in the left middle occipital gyrus, the left precentral gyrus, and the left middle cingulum gyrus. The abundances of the phyla Synergistetes and Verrucomicrobia were positively correlated with the ALFF values of the left middle occipital gyrus, left precentral gyrus, and left middle cingulum gyrus. These data suggest that specific gut microbes may modulate intrinsic brain activity and cognitive function in perimenopausal women. A plant-based RSL-rich diet has beneficial effects on the gut microbial composition and brain function of perimenopausal women.
Similar content being viewed by others
Introduction
Perimenopause is the transitional period before menopause and is accompanied by depletion of ovarian follicles and fluctuating hormone levels in women1. Perimenopausal syndrome (PMS) is a series of symptoms caused by fluctuations in estrogen levels around the time of menopause, which lead to both physical and psychological disorders in women (hot flashes, night sweats, sleep disturbances, depressive symptoms, vasomotor dysfunction, mood disorders, etc.)2. Hormonal disorders and cytokine dysregulation are the main causes of PMS1,2,3,4. Perimenopausal symptoms not only impair quality of life but also may be associated with diabetes5, cardiovascular diseases6,7, cancer8, and neurodegenerative diseases9. Menopausal women have been reported to suffer from cognitive dysfunction, learning disabilities, and memory decline10,11. In addition, the menopausal transition increases the risk of Alzheimer’s disease (AD)-related brain changes and is considered a period of neurological transition9,12. PMS poses a serious threat to the physical and mental health of middle-aged and older women; therefore, more attention should be given to the prevention and treatment of PMS.
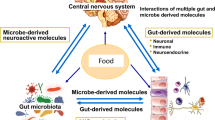
The gut microbiota is a population of microorganisms found in the gastrointestinal tract and is closely associated with health and disease13. It has been suggested that the gut microbiota composition is influenced by the estrogen level and that the gut microbiome also significantly affects the estrogen level14,15. Gut microbiota dysbiosis can occur in PMS16. In estrogen-sufficient women, the intestinal microbiota is diverse, with a predominance of beneficial bacteria17. In pregnant women with PMS, the relative abundance of beneficial bacteria such as Aggregatibacter, Lactobacillus, and Bifidobacteria significantly decreased, whereas those of harmful bacteria such as Enterobacter increased16,18,19. In addition, the gut microbiota may undergo specific compositional changes during perimenopause19,20. Therefore, maintaining the gut microbial balance is crucial to the health of perimenopausal women. There is a bidirectional relationship between the gut microbiota and the brain, referred to as the microbiota-gut-brain-axis21. Preliminary evidence suggests that the gut microbiota is an important environmental factor that closely correlates with brain function (including cognition, mood, and social behavior) and is potentially linked to neurodegenerative diseases, such as AD22,23,24,25,26.
Interactions between the gut and the brain form a complex network involving neuronal, endocrine and immune pathways24,27,28. Because it is difficult to describe the human brain cellular network precisely, few studies have established a direct link between the gut microbiota and brain function in vivo19,29. In patients with amnestic mild cognitive impairment, there is a specific pattern of interaction between the gut microbiota and intrinsic brain activity or mental function. the relative abundances of Bacteroides, Ruminococcaceae, Clostridiaceae, Blautia, and Veillonellaceae are correlated with the inherent activity of different brain areas. Members of Clostridium (Lachnospiraceae and Blautia), as well as Veillonellaceae, are associated with cognition29. Four weeks of probiotic intake from fermented dairy products in healthy women led to significant changes in the intrinsic activities of the resting brain30. They grouped healthy women into Bacteroides-abundant and Prevotella-abundant groups according to genus‐based clusters. The Prevotella group presented decreased hippocampal activity when negative valence images were taken31. To the best of our knowledge, no studies to date have detailed the interactions between the gut microbiota and brain function in women with PMS. However, abnormal spontaneous activities in multiple brain regions (frontal, temporal, and hippocampal areas) have been detected in perimenopausal women during resting states32,33,34,35,36,37. These changes may be related to emotional and cognitive impairments and potentially represent the neural mechanisms of cognitive dysfunction in perimenopausal women.
Analysis of intrinsic brain activity is crucial for understanding the pathogenesis of PMS and its early detection32,38. Resting-state functional MRI (rs-fMRI) detects brain activity when a subject is awake but not performing a specific task or responding to external stimuli39. It reflects the spontaneous activity of the central nervous system in the basal state40. Common measures of rs-fMRI include regional homogeneity (ReHo), which assesses the consistency of activity between adjacent voxel regions39, and the amplitude of low-frequency fluctuation amplitude (ALFF) and fractional ALFF (fALFF), which measures the intensity of regional spontaneous brain activity41,42. The rs-fMRI technique has also been used to evaluate brain function in perimenopausal women33,34,43. Fluctuating estrogen levels during perimenopause exacerbate PMS-related cognitive decline through multiple mechanisms: (1) Reduced estrogen directly inhibits BDNF-dependent synaptic plasticity in the hippocampus, impairing memory encoding efficiency44,45; (2) Estrogen receptor β-mediated disruption of gut barrier integrity promotes translocation of microbiota-derived LPS into circulation, triggering neuroinflammation15,46; and (3) Luteal-phase allopregnanolone metabolic dysregulation causes GABAergic signaling dysfunction, amplifying anxiety-induced executive function impairment47. These interconnected pathways form a vicious "estrogen-gut-brain axis" cycle, which may be interrupted by a Raphanus sativus L.-rich diet through modulation of gut microbiota metabolism (e.g., increased SCFAs) and activation of the Nrf2 antioxidant pathway48.
Diet is one of the most important factors regulating behavioral and mental health throughout life49. Moreover, diet is one of the key determinants of the composition of the gut microbiota50,50. One review reviewed the beneficial effects of diet on brain health51. Raphanus sativus L. (RSL) belongs to the cruciferous family and is edible and used as a traditional medicine. It has over 1000 years of history for treating food stagnation, constipation, abdominal pain, and bloating52.RSL and its major chemical constituent, sulforaphene (SFE) promote gastrointestinal motility through multitarget and multichannel activities52. Therefore, it is presumed that RSL acts on specific microbes in the intestine. While murine models suggest sulforaphene may modulate tau pathology via PI3K/Akt pathway53, human translational evidence remains to be established. In addition, some population studies have shown that eating more cruciferous vegetables can prevent age-related cognitive decline in healthy older adults52,54,55. Few studies have investigated the relationship between diet and functional connectivity in brain networks in the resting state, which may underlie cognitive function36,56. A healthy diet may support cognitive ability despite differences in large-scale network connectivity in the resting state57. The diet also has regulatory effects on multiple pathways that connect the gut microbiota to the brain58,59. Animal studies have demonstrated the potential benefits of a healthy diet in mediating microbiota–brain interactions60,61. However, to our knowledge, no clinical studies have shown the role of dietary interventions in the interactions between the gut microbiota and brain function. In this study, we aimed to evaluate the effects of a plant-based RSL-rich dietary intervention on brain function and the gut microbiota in perimenopausal women and the correlations of the gut microbiota profile with intrinsic cerebral activity (as evaluated by ALFF with rs-fMRI) and cognitive function.
We selected Raphanus sativus L. seeds as the core dietary intervention based on their unique phytochemical composition and clinical advantages. As a traditional medicinal food documented in the Chinese Pharmacopoeia (2020 edition), RSL is particularly rich in sulforaphene and other bioactive isothiocyanates, which have demonstrated both neuroprotective effects62 and gut microbiota-modulating properties63. Compared to other cruciferous vegetables like broccoli, RSL offers superior clinical applicability, containing 2.3-fold higher glucosinolate precursors48 while maintaining excellent storage stability, making them particularly suitable for long-term intervention studies at the 5 g/day dosage, which has shown no reported adverse effects48. The mechanisms linking cognitive changes to the gut microbiota-brain axis in perimenopausal women remain poorly understood, with limited evidence for dietary interventions in this population. Through a longitudinal intervention design, this study systematically evaluates the effects of a Raphanus sativus L. (RSL)-enriched plant-based diet on gut microbiota composition, intrinsic brain activity, and cognitive function in perimenopausal women. The findings may provide novel insights into gut-brain interactions and lay the groundwork for developing safe, accessible dietary strategies to support mental health during menopausal transition.
Results
Baseline characteristics of the study participants
Of the 24 subjects who met the eligibility criteria, 14 dropped out or were excluded, and 10 completed the study. Recruitment took place from December 2021 to May 2022, and the dietary intervention was carried out from August to October 2022, with a follow-up visit one month after the end of the intervention to determine whether the subjects experienced any discomfort. This study was designed as a single-arm longitudinal exploratory investigation. A total of 10 participants were ultimately included (attrition rate: 58.3%). Based on post-hoc power analysis using G*Power 3.1 (paired t-test, two-tailed α = 0.05, effect size d = 0.6), the current sample size achieved a statistical power of 0.42, indicating that only large effects (d ≥ 1.0) could be detected with this study design. The baseline characteristics of the participants were collected on the first day of the intervention study (Table 1). The flowchart of the study (adapted from CONSORT 2010) is presented in Fig. 1.
Flowchart of the study (adapted from CONSORT 2010 Flow Diagram). The study was approved by the Ethics Committee of the Affiliated Hospital of Guizhou Medical University (2021 Ethics No. (675)). The clinical registration number is ChiCTR2400084007. Written informed consent was obtained from all participants before inclusion in this study. All experiments and procedures were carried out in accordance with ethical and biosafety protocols approved by the Institutional guidelines.
Neuropsychological assessments
The results of the seven sub‐items of the MoCA are shown in Table 2. There was a trend toward increased visuospatial/executive function and total score at T1 (at the end of dietary intervention) compared with those at T0 (P = 0.051, P = 0.089). The scores of the other sub‐items of the MoCA did not significantly differ between T0 and T1.
Gastrointestinal symptoms
To assess the effect of probiotics on intestinal health, the participants completed a general health questionnaire comprising items on bowel habit improvement at weeks 0, 4, 8, and 12. There was a significant increase in burping rates at week 12 compared with week 0 (P < 0.05) (Fig. 2a), whereas bloating, abdominal pain, early satiety, acid reflux, abdominal burning sensation, poor appetite, stomach heaviness after eating, indigestion, nausea, poor bowel motility, and dissatisfaction with digestive function were unaffected (Table 3). We observed no effects of the dietary intervention on stool time or consistency (assessed by the Bristol stool scale) (Fig. 2). Stool frequency significantly improved (P < 0.05) (Fig. 2b). Figure 2c shows the results of the Bristol Stool Scale assessment during the dietary intervention.
Gastrointestinal symptoms. (a) Scores of burping measured at each visit (n = 10). (b) Frequency of defecation (n = 10). (c) Percentage of subjects in each category of stool type assessed by the Bristol stool scale (n = 10). Type1: Separate hard lumps, like nuts (hard to pass); Type2: Sausage-shaped but lumpy; Type3: Like a sausage but with cracks on its surface; Type4: Like a sausage or snake, smooth and soft; Type5: Soft blobs with clear-cut edges (passed easily); Type6: Fluffy pieces with ragged edges, a mushy stool; Type7: Watery, no solid pieces, Type 1–2 are considered hard; 3–5 are normal; 4 is the ideal state; 6–7 are soft. Data were analyzed by a Friedman test followed by Dunn’s post hoc tests.
Microbial diversity and gut microbial composition
The analysis of the alpha diversity of the gut microbiome revealed that the Good’s coverage index, which represents coverage, increased significantly, whereas no significant changes were found in the other indices (Fig. 3a). There was no notable difference in terms of beta diversity (Fig. 3b). Next, we analyzed changes in the gut microbial composition at the phylum and genus levels after 12 weeks of dietary intervention and detected differences in the phylum and genus abundances between T0 and T1. We listed the top 10 most abundant phyla and genera at T0 and T1, respectively (Fig. 3c, d). At the phylum level, the phyla Firmicutes and Bacteroidetes decreased significantly during dietary intervention, while the abundances of Proteobacteria, Actinobacteria, Verrucomicrobia and TM7 decreased. Linear discriminative analysis (LDA) effect size (Lefse) revealed that the abundances of the genera Pseudomonas and the family Oxalobacteraceae were relatively high, whereas those of the phyla Actinobacteria and genera Shigella, Subdoligranulum, Aeromonas and Actinomyces, the order Aeromonadales, and the family Actinomycetaceae were relatively low during dietary intervention (Fig. 3e, f). Three KEGG pathways (P < 0.05) enriched at T1 were not apparent at T0, including the lysosome, metabolism of xenobiotics by cytochrome P450 and cyanoamino acid metabolism (Fig. 3g).
Changes in microbial composition after 12-week dietary intervention. (a): Alpha-diversity indices. The “Chao1” and “Observed species” indices represent the richness, the “Shannon” and “Simpson” indicate diversity, the “Faiths_pd” index represents evolutionary diversity, the “Pielou_e” evenness index represents evenness, and the “Goods_coverage” index represents coverage. (b): Beta-diversity indexes. Principal coordinates analysis (PCoA) of the beta–diversity index Weighted UniFrac (b). (c-d): Gut microbiome composition at the level of major phylum (c) and genus (d) in T0 and T1. (e-f): Linear discriminant analysis (LDA) effect size (Lefse) plot and cladogram representing the unique bacterial signatures identified at T0 and T1. (f), family; (g), genus. (g): KEGG metabolic pathway analysis. A positive value of logFC on the horizontal axis represents an upward adjustment (log2(fold change)) of T1 relative to T0. Data are mean ± SEM and were analyzed by the Kruskal-Wallis test followed by Dunn’s post-test: *P < 0.05. T1 vs T0.
Brain function
Compared with the baseline values, the participants demonstrated significantly elevated ALFF values in the left middle occipital gyrus, the left precentral gyrus, and the left middle cingulum gyrus after the dietary intervention (P < 0.05, FDR corrected) (Fig. 4). The detailed data from the ALFF analysis are summarized in Table 4.
Associations between the cognitive test score, brain activity, and gut microbiome abundance
Finally, we analyzed the correlations between the relative abundance of the gut microbiome, intrinsic brain activities (i.e., ALFF values), and cognitive function via Pearson’s correlation analysis. The results revealed that the correlations between the gut microbiota abundance and internal brain activity differed before and after the dietary intervention (Fig. 5). At baseline (T0), there were positive correlations between the relative abundance of the phylum Tenericutes and the ALFF value of the left middle occipital gyrus (Occipital_Mid_L), as well as between the relative abundance of the genus Roseburia and the ALFF values of Occipital_Mid_L, the left precentral gyrus (Precuneus_L), and the left middle cingulum gyrus (Cingulum_Mid_L). Moreover, after 12 weeks of the plant-based RSL-rich diet (T1), the abundances of the phyla Synergistetes and Verrucomicrobia were positively correlated with Occipital_Mid_L, Precuneus_L, and Cingulum_Mid_L. The abundance of the phylum Tenericutes was positively correlated with Occipital_Mid_L and Cingulum_Mid_L.
Next, we assessed the associations between the relative abundances of the altered gut microbiome and the cognitive test scores (Fig. 6). Before dietary intervention (T0), the relative abundance of the phylum Synergistetes was positively correlated with visuospatial/executive function test scores. The phylum Proteobacteria and genus Weissella were negatively correlated with the naming score. The phylum Bacteroidetes, as well as the genera Bacteroides and Coprococcus, were negatively correlated with the Language score. The genera Bifidobacterium and Roseburia were negatively correlated with the abstraction score. After 12 weeks of the plant-based RSL-rich diet, we observed a positive correlation between the genus Faecalibacterium and the language score. The relative abundance of the genus Roseburia was negatively correlated with the delayed recall score. The genus Ruminococcus was negatively correlated with attention test scores.
Discussion
Perimenopause is not only a period of physiological transition (menstrual disorders, osteoporosis, cardiovascular disease, diabetes, tumors and other pathological changes)64 but also a period of neurological transition (depression, mood disorders, insomnia, cognitive decline, increased risk of neurodegenerative diseases, etc.)65, and a significant proportion of women suffer from problems associated with perimenopause, which seriously affects their quality of life66. In addition, the intestinal microbiota can become dysregulated in perimenopausal women. Healthy dietary patterns not only positively regulate the gut microbiota but also have a positive effect on brain health67. Dietary patterns such as the Mediterranean diet and calorie-restricted diets are beneficial to cognition and brain function, reducing the risk of neurodegenerative diseases such as AD66,68. Regulation of the gut microbiome may positively affect neural pathways and contribute to the regulation of several neurochemical and neurometabolic pathways through complex gut–brain interactions, thereby slowing the process of cognitive decline69,70. Therefore, we first explored the effects of a plant-based RSL-rich diet on the gut microbiota and brain function in perimenopausal women. We detected changes in the gut microbial composition, cognitive function and intrinsic brain activity following dietary intervention, followed by further analysis of the associations between these parameters. In this study, we observed a decrease in the relative abundance of several harmful gut bacteria and increased brain activity in the resting state in several brain regions associated with cognition in perimenopausal women after dietary intervention, and the associations between the relative abundance of specific bacterial taxa and intrinsic brain activity paralleled the changes in cognitive domains. Though this was initially designed as a pilot study, the achieved power supports the reliability of our findings regarding the primary outcomes. The limited statistical power (0.42) suggests our findings should be interpreted as preliminary evidence, consistent with the exploratory nature of this pilot study. Future randomized controlled trials with larger samples are needed to confirm these observations.
The Montreal Cognitive Assessment (MoCA) domains exhibit specific neuroanatomical substrates with direct clinical implications: visuospatial/executive performance relies on dorsolateral prefrontal-parietal circuits (2.1 ± 0.4-point deficit post-DLPFC lesions, p < 0.01)71, naming accuracy reflects anterior temporal lobe integrity (r = 0.52 with ATL atrophy, p = 0.003)71, language function depends on arcuate fasciculus white matter microstructure (FA β = 0.34, p = 0.02), while delayed recall strongly predicts hippocampal volume loss72. These region-___domain mappings enhance the interpretability of cognitive declines in perimenopausal women, particularly when correlating MoCA subscores with our observed ALFF changes in corresponding brain regions. Given the small sample size, as expected, we did not observe large clinical effects. As perimenopause may lead to subcognitive abilities, we performed a MoCA assessment before and after the dietary intervention. We reported that visuospatial/executive function tended to increase from a baseline total score of 25.4 ± 1.78 to 26.6 ± 1.96 at the end of the dietary intervention. Although there was no significant difference, this finding suggests that our dietary intervention may have contributed to the overall cognitive profile. Because of the low internal reliability of the scales and the small sample size, these results must be treated with caution. Many dietary patterns, such as the most studied Mediterranean diet73 and the Norwegian and Japanese diets74, have shown protective effects on slowing cognitive decline. These diets have also been associated with a reduced risk of diseases such as depression and AD75. Notably, the neuroprotective effects of our RSL-rich dietary intervention align with established benefits of the Mediterranean diet – a pattern repeatedly associated with reduced cognitive decline in longitudinal studies76. While Mediterranean diets exert protection through polyphenol-rich olive oil and fish-derived ω-3 fatty acids, our plant-based RSL regimen operates via distinct yet complementary mechanisms: (1) sulforaphene-mediated Nrf2 activation (vs. hydroxytyrosol in olive oil), and (2) gut microbiota modulation favoring SCFA-producing taxa (similar to Mediterranean-induced increases in RSL). This convergence of health effects through divergent pathways underscores the versatility of dietary approaches in perimenopausal neuroprotection.
Based on the characteristics of the dietary regimen (consumption of RSL at 5 g/day), we analyzed whether a 12-week nutritional intervention would affect gastrointestinal symptoms. The results showed that our dietary regimen did not have adverse effects on overall intestinal health, except for the reported increased frequency of burping, which could be attributed to the daily consumption of RSL. RSL is a dual-use food, and its beneficial effects on the gastrointestinal tract such as eliminating food stagnation and bloating, promoting intestinal motility, and ameliorating constipation77,78. During the dietary intervention, we observed a significant increase in the frequency of bowel movements, which the consumption of RSL also be explained. However, as this study employed a whole-diet intervention, these effects may also be the result of interactions between various dietary components. In the future, we will conduct a randomized controlled trial to compare the impact of the whole diet with and without the addition of RSL. These results must be treated with caution due to the low internal reliability of the scales and the small sample size.
There is often individual variation in the gut microbiome, even when patients consume the same foods. Our microbiome data are of some benefit because each patient is under their own control79. Although there was no significant difference in β diversity after 12 weeks of the plant-based RSL-rich diet, we detected a trend toward increased α diversity and a substantial difference in the Good’s coverage index. Additionally, several gut bacterial phyla, families, and genera were altered between T0 and T1. For example, the phyla Firmicutes and Bacteroidetes decreased at T1, and the Firmicutes: Bacteroidetes ratio (F/B) decreased. The F/B ratio is greater in postmenopausal women19, and a lower F/B ratio is considered to offer health benefits80. Indeed, the abundances of Oxalobacteraceae and Pseudomonas increased, whereas those of Actinobacteria and Aeromonas decreased after dietary intervention. Several studies have reported the beneficial health effects of Oxalobacter formigenes, which can degrade oxalate and thus reduce the risk of kidney stone formation81. Decreases in Actinobacteria, Aeromonas and Shigell suggest an improvement in dysbiosis82. Aeromonas and Shigella are enteric pathogens that cause diarrhea83,84. Here, we found that RSL improved intestinal health, most likely by lowering Aeromonas and Shigella. More targeted research is needed to validate these findings. Pseudomonas is pathogenic, with its cell walls being rich in inflammatory components, such as LPS, which is known to induce low-level systemic inflammation85. Whether this increased level of pathogenic bacteria is due to dietary intervention or to the patients themselves cannot be concluded owing to the lack of references to relevant studies. At this stage, in our overall knowledge of dietary intervention and the microbiome of perimenopausal women, there is no specific marker to define an improvement in dysbiosis. Therefore, more studies are needed to explore the possible markers in perimenopausal women and the effects of dietary interventions on specific markers.
This study revealed increases in resting‐state activity in the left middle occipital gyrus, the left precuneus, and the left medial cingulum gyrus in perimenopausal women after 12 weeks of dietary intervention. Abnormal spontaneous activities in multiple brain regions during the resting state have been reported to be altered in perimenopausal women. ALFF was significantly elevated in the left rectus gyrus of perimenopausal women compared with premenopausal women. The regions with reduced ALFF during perimenopause include the left superior temporal gyrus, the left inferior frontal gyrus, and the left insula43. Although the results of our study did not correspond to those of Liu et al., the left middle occipital gyrus found in this study is involved in visuospatial perception and the visual network. Kawagoe et al. reported reduced occipital blood perfusion in patients with mild cognitive impairment86. Studies in patients with early mild cognitive impairment have revealed that the decline in working memory tends to occur first in the visual field rather than the verbal field. This may indicate an early compensatory response to neurodegenerative changes in response to neural injury87,88. This result corresponds to the results of our MoCA test. Therefore, our dietary intervention may prevent cognitive impairment at an early stage by affecting the middle occipital gyrus. The functional roles of the precuneus are unclear. Yeager et al. proposed associations of the precuneus with body awareness, complex cognition, and visual processing and that the precuneus had functional connections to other cortical areas associated with executive function, including the dorsolateral prefrontal cortex and the inferior parietal lobe89. Therefore, our dietary intervention may increase cognitive control and executive function in perimenopausal women by increasing the ALFF value of the left precentral gyrus. Abnormal dynamic functional connectivity of the left middle cingulum gyrus and hippocampus in patients with mild cognitive impairment90. Patients with temporal lobe epilepsy have language and cognitive deficits as well as lower right–left middle cingulum gyrus activity than healthy participants91. Therefore, the elevated ALFF in the left middle cingulum gyrus may be associated with cognitive improvement. Our dietary intervention may prevent cognitive decline in perimenopausal women through early improvements in visuospatial perception and visual network function.
In this study, we also observed changes in the pattern of association between intrinsic brain activity and the gut microbiome in perimenopausal women after dietary intervention. At baseline, there was a significant positive association between the genus Roseburia and brain activity in all three brain regions in perimenopausal women. Roseburia intestinalis has been shown to be a beneficial intestinal bacterium that helps prevent intestinal inflammation and maintain energy homeostasis92. These findings suggest that Roseburia intestinalis may have a positive regulatory effect on brain function in perimenopausal women, as previously reported93. However, as studies on the microbiota‒gut‒brain axis in PMS are rare, further investigations into the mechanisms of brain-active bacteria and intrinsic brain function in PMS are needed. Compared with the baseline values, after 12 weeks of dietary intervention, significant positive correlations were found for the phyla Synergistetes, Verrucomicrobia and Tenericutes with all three brain regions. In this study, we also found a positive correlation between the phylum Synergistetes and visuospatial/executive function scores on the MoCA at baseline. In humans, the phylum Synergistetes is more frequently seen and isolated in the oral cavity and may contribute to periodontal diseases. Synergistetes represents a poorly characterized phylotype94. There are fewer types isolated from feces, and little is known about the role of the phylum Synergistetes in other diseases95. Owing to the small sample size in our study, further investigations are needed to demonstrate the causal relationship between the phylum Synergistetes and health improvement as well as brain health. The phylum Verrucomicrobia is associated with longevity96, and our results suggest that this phylum may play a beneficial role by positively modulating brain function to improve cognitive function in perimenopausal women. Finally, our correlation analysis of the gut microbiome and the MoCA cognitive test revealed a greater number of gut bacterial species that were negatively correlated with each score in the MoCA test in perimenopausal women before the dietary intervention than in those after the intervention. These findings suggest that our 12-week healthy diet intervention may have increased the diversity and abundance of the gut microbiota (although not reflected in the diversity analysis) and that these increases in the gut microbiome are beneficial to the understanding of perimenopausal women. In the future, cross-sectional and longitudinal studies with larger sample sizes are needed to verify these findings. Perimenopausal women lack safe, effective non-pharmacological interventions for cognitive decline and abnormal brain activity. This study provides the first longitudinal evidence that a Raphanus sativus L. (RSL)-enriched plant-based diet may modulate spontaneous neural activity (ALFF) through specific gut microbiota (e.g., Synergistetes and Verrucomicrobia), while enhancing visuospatial/executive function. These findings advance our understanding of microbiome-gut-brain axis regulation in perimenopausal syndrome and establish a practical foundation for dietary cognitive protection strategies.
There are several limitations to our study. (1) Due to the small sample size, larger clinical effects and low internal reliability were not observed. (2) Because of the small number of cases recruited, all participants were included in the experimental group to obtain as many significant results as possible. A single-arm study was conducted, and a strictly randomized controlled study was not performed. This may have also had an impact on the experimental results, which need to be further optimized in subsequent studies. (3) Daily consumption of RSL was a major feature of this study. We have high expectations for the therapeutic effects of RSL in this trial. However, since a whole-diet intervention was used, these effects may also be the result of the interaction of various dietary components. In the future, we will conduct a randomized controlled trial to compare the effects of adding and not adding RSL to the whole diet. (4) At this stage, our overall understanding of dietary interventions and the microbiome of perimenopausal women does not yet have specific markers to define improvements in dysbiosis. Therefore, additional studies are needed to explore possible markers in perimenopausal women and the effects of dietary interventions on specific markers. (5) Studies on the microbiota‒gut‒brain axis in premenstrual syndrome patients are uncommon because our results may not be adequately understood. Therefore, more studies are needed in the future to investigate the mechanisms of brain-active bacteria and intrinsic brain function in perimenopausal syndromes.
We conducted a longitudinal single-arm study. After a 12-week plant-based dietary intervention enriched with Raphanus sativus L., perimenopausal women tended toward improvements in the visuospatial/executive function subscale and total scores and changes in the gut microbial composition. The participants presented elevated ALFF values in the left middle occipital gyrus, left precentral gyrus and left middle cingulum gyrus. These brain regions are associated with cognitive performance. The abundances of the phyla Synergistetes and Verrucomicrobia were positively correlated with the ALFF values of the left middle occipital gyrus, left precentral gyrus, and left middle cingulum gyrus, and the abundance of the phylum Tenericutes was positively correlated with the left middle occipital gyrus and left middle cingulum gyrus. These findings suggest that specific gut microbes may modulate intrinsic brain activity and cognitive function. In conclusion, our study suggests the beneficial effects of a plant-based diet on the gut microbial composition and brain function of perimenopausal women. These findings provide supportive evidence for studies of dietary interventions that modulate the gut microbiota and brain function. This study demonstrates the feasibility and guidance of dietary interventions (plant-rich dietary interventions and increased seed intake) to promote health and improve quality of life in perimenopausal women. Innovative demonstration of the role of dietary interventions in the interaction between the gut microbiota and brain function.
Materials and methods
Study participants
Healthy perimenopausal women were recruited consecutively from the Menopause Clinic, Affiliated Hospital of Guizhou Medical University, from February 2021 to May 2022. All participants were recruited from the outpatient clinic after a comprehensive assessment by an obstetrician-gynecologist, met the criteria for perimenopause, which is defined as the transitional stage from 1 year before the onset of obvious menstrual disorders to the complete disappearance of menstruation, and received the domestic modified Kupperman index (KI) test (Supplementary Table 1) at the hospital. The inclusion criteria were as follows: aged 45–55 years; clinical symptoms, signs, and a diagnosis of perimenopausal syndrome; and no previous hormone supplementation therapy. The exclusion criteria were as follows: consumption of antibiotics, probiotics, prebiotics, or synbiotics within 2 months before fecal sample collection; severe malnutrition; infection; drug or alcohol addictions; irritable bowel syndrome; and inflammatory bowel disease; combined severe liver, kidney, lung, heart, brain, and hematopoietic system diseases; other serious primary diseases; schizophrenia; schizoaffective disorders; or primary affective disorders; and MR incompatibility; and severe auditory, visual, or motor deficits hampering cognitive testing. Here, we used the CONSORT Reporting Guidelines97. Fifty-six candidates were enrolled, and 24 were eligible for this study after screening. The flow of participant employment is provided in Fig. 1. The study was approved by the Ethics Committee of the Affiliated Hospital of Guizhou Medical University (2021 Ethics No. (675)). Trial registration: Chinese Clinical Trial Registry (ChiCTR), ChiCTR2400084007. Registered 09 May 2024—Retrospectively registered, https://www.chictr.org.cn/showproj.html?proj=197060. All included subjects signed an informed consent form.
Study design
In this longitudinal single-arm study, all participants underwent a 12-week dietary intervention. They underwent neuroimaging, as well as MMSE and MoCA testing, before and at the end of the dietary intervention. Stool samples were also collected at the two time points. In addition, the participants completed a general health questionnaire comprising items on bowel habit improvement at weeks 0, 4, 8, and 12 (Fig. 7).
Experimental protocol. Subjects included in this study received 12 weeks of dietary intervention. During the two weeks of nutritional intervention, they completed a general health questionnaire and Bristol stool scale to report their intestinal tolerance, appetite feelings, stool frequency, and consistency to this particular diet. at baseline before intervention (T0, Week 0), 4 weeks (Week 4) and 8 weeks (Week 8) after the start of the nutritional intervention, and 12 weeks at the end of the nutritional intervention (T2, Week 12).
The MMSE is used as a global measurement of cognitive status, and a total score of ≥ 27 indicates normal cognition98. The Beijing version of the MoCA is the most widely used version in mainland China and exhibits good internal consistency and general criterion‐related validity99. It includes seven cognitive domains (i.e., visuospatial/executive function, naming, attention, abstraction, language, delayed memory, and orientation), with a total score of ≥ 26 indicating normal function. The MoCA adds 1 point for individuals who have ≤ 12 years of education for education adjustment. The general health questionnaire comprises items measuring gastrointestinal symptoms (bloating, abdominal pain, early satiety, acid reflux, abdominal burning sensation, burping, poor appetite, stomach heaviness after eating, indigestion, nausea, poor bowel motility, and dissatisfaction with digestive function). Each item had a 4-point scale ranging from 1 (“not at all”) to 4 (“very much”) for both symptom severity and frequency; thus, the total score was 8. Lower scores indicate improvement. In addition, the subjects completed a questionnaire on 24-h stool frequency and consistency (Bristol stool scale)100.
Dietary intervention
The diet was developed by a registered nutritionist. The participants were asked to adhere to their daily diet for 12 weeks (see supplementary information for sample menus). Regular online interviews were performed with participants to inform them of meal planning and evaluate their adherence. The participants supplied their own food on the basis of a daily meal plan, food list, and other provided material. To investigate the effect of RSL consumption on perimenopausal women, we formulated a plant-based RSL-rich (5 g/d) diet. RSL belongs to the cruciferous family, and to avoid the intake of other cruciferous vegetables, no other cruciferous vegetables were added to the diet except for RSL. Overall, our dietary intervention provided a controlled, nutrient-dense regimen (≈1300 kcal/day) with optimized macronutrient distribution (protein ≈65 g/day, carbs < 100 g/day, fiber ≈40 g/day), emphasizing RSL (5 g/day) alongside neuroprotective ingredients (e.g., ginkgo, salmon, flaxseed). Throughout the study, the participants received daily multivitamin supplements (B-complex vitamins, vitamin D [400–1000 IU/day], and vitamin C [100–300 mg/d]) and restricted the use of supplements with antioxidant or ketone-inducing effects (i.e., fish oil, coconut oil, and medium-chain triglyceride supplements). In addition, all participants, the experimenter, and the nutritionist had a communication group where they could contact the dietitian during the intervention with any questions they had. Patients were encouraged to post pictures of their daily diets to the communication group, and if they forgot, our lab staff visited them in a private chat to ensure their adherence. During the intervention, we ask about and record any adverse events for participants, and they can also choose to withdraw at any time if they wish. At the end of the intervention, we will maintain the communication group for one month for follow-up.
Analysis of the gut microbiota composition in the stool samples
Each participant was asked to collect a fresh fecal sample. Fecal samples were self-collected by each participant and preserved at − 80 °C until analysis. Genomic DNA was extracted from 500 mg of each stool sample via an Omega M5636-02 kit (Omega, CT, USA), and the DNA was quantified via Nanodrop (Thermo Scientific, Waltham, MA). The quality of the extracted DNA was assessed via 1.2% agarose gel electrophoresis. The DNA samples were subjected to PCR amplification via the primer pair 338F: 5’-ACTCCTACGGGAGGCAGCA -3’ and 806R: 5’-GGACTACHVGGGTWTCTAAT-3’ to amplify the V3-V4 region of the bacterial 16S rRNA gene. The PCR products were purified and sequenced via the Illumina® MiSeq platform. Initial screening of raw downstream data from high-throughput sequencing on the basis of sequence quality. Sequence denoising or OTU clustering was performed according to the QIIME2 dada2 analysis process. The alpha diversity level of each sample was assessed on the basis of the distribution of ASVs/OTUs in different samples and the appropriateness of sequencing depth reflected by sparse curves. The beta diversity of the microbiome was analyzed via principal coordinate analysis (PCoA) with unweighted and weighted UniFrac distances. LEfSE (linear discriminant analysis [LDA] effect size) was used to identify significantly different bacterial taxa after the dietary intervention compared with those at baseline101. The open-source bioinformatics tool PICRUSt (Phylogenetic Study of Communities by Reconstruction of Unobserved States) was used to explore the metabolic and other functional activities of the intestinal bacterial community102. On the basis of the 16S rRNA gene sequencing results, we predicted the metabolic function of the sample’s flora, identified differential pathways, and obtained the species compositions of specific pathways. The inferred gene families were annotated according to KEGG (Kyoto Encyclopedia of Genes and Genomes) Orthology (KOs) and then folded into KEGG pathways to generate functional pathways103.
Neuroimaging acquisition and analysis
MRI data acquisition
All participants underwent brain MRI examination on a 3.0 T MR scanner (Discovery MR 750w, GE Healthcare, Milwaukee, WI) with a 24-channel head/neck coil at Guizhou People’s Hospital. They were asked to remain awake and keep their eyes closed during the scan.
High-resolution whole-brain 3D T1-weighted brain anatomical images were collected via volumetric three-dimensional magnetization via a rapid-acquisition gradient-echo sequence with the following parameters: TR/TE = 8.5/3.2 ms, TI = 450 ms, FA = 15°, FOV = 256 mm × 256 mm, matrix = 256 × 256, thickness = 1 mm, resolution = 1 mm × 1 mm × 1 mm, 176 axial slices, scan time = 273 s, accelerated by ARC parallel acquisition technology with acceleration factor R = 2. The rs-fMRI images were obtained via an echo-planar imaging sequence (repetition time = 2000 ms, echo time = 30 ms, flip angle = 70°, field of view = 216 mm × 216 mm, matrix = 72 × 72, thickness = 3.5 mm, slice gap = 0.5 mm, slices = 34, voxel size = 3 mm × 3 mm × 4 mm, volume = 250). The participants with obvious motion artifacts and metal artifacts were excluded from the analysis. In addition, plain brain MR scans (axial T2, sagittal T2, and axial T2 FLAIR) were performed to exclude organic lesions in the brain.
Data preprocessing
Data preprocessing was performed via SPM12 (http://www.fil.ion.ucl.ac.uk/spm) and the Data Processing Assistant for Resting-State fMRI (DPARSF; http://www.restfmri.net) 104,105 in the MATLAB 2018a (Mathworks, Natick, MA) platform. (1) The functional images of the first 10 time points were removed to ensure that the subjects had adapted to the scanning environment. (2) The remaining 240 images were corrected for time differences and small movements, and the signals collected at different times were modified for time point matching. (3) Subjects with head maximum movement > 2.0 mm in the x-, y-, or z-axis or with angular rotation > 2.0° were excluded. (4) The generated images were normalized to the Montreal Neurological Institute (MNI) standard space. The T1 images were first coregistered to the mean functional images after motion correction and then resampled to a 3 × 3 × 3 mm isotropic voxel size. (5) Linear detrending was performed to remove noise from long-term physiological shifts, residual movement-related artifacts after realignment, and instrumental instabilities. (6) The white matter signal, cerebrospinal signal, and head motion parameters (Friston 24 parameters) were regressed out except for the global signal. (7) Low-frequency filtering (0.01–0.1 Hz) was applied to eliminate high-frequency physiological noise.
ALFF analysis
The ALFF was computed via the DPARSF toolbox. The ALFF is defined as the mean amplitude of the rs-fMRI signal within the frequency band of 0.01–0.1 Hz for each voxel and was used to measure the level of basal neural activity in the brain. This approach can reflect the spontaneous neural activity of each voxel in the resting state. The specific calculation procedures are as follows: (1) The time series of each voxel was transformed into the frequency ___domain via the Fourier transform to obtain the power spectrum. (2) The square root of the power spectrum at each frequency point was computed. (3) The mean square root across all frequency points was deemed the ALFF value, indicating the intensity of spontaneous activity. (4) The ALFF of each voxel was normalized to the global mean ALFF within the brain mask. The normalized ALFF value for each voxel should be approximately 1. (5) The normalized ALFF maps of each subject were spatially smoothed using a 6 × 6 × 6 mm3 full width at the half-maximum Gaussian kernel. In addition, the brain regions that exhibited between-group differences were identified as regions of interest (ROIs). The ALFF values of all the ROIs were calculated for each subject via the REST plus toolbox104-106.
Statistical analyses
A priori power analysis using G*Power 3.1 software to determine the appropriate sample size. Statistical analysis was performed via SPSS version 26.0 (SPSS Inc., Chicago, IL) and GraphPad Prism 8 (GraphPad Software, Inc.). The results are presented as percentages, means ± standard deviations, or medians with interquartile ranges (IQRs). The data were analyzed with paired samples t tests with Tukey post hoc tests if they were parametric and with Friedman tests with Dunn post hoc tests if they were nonparametric. Normality was assessed by the Shapiro‒Wilk test. Statistically significant differences between the gut microbiome groups were calculated via the Kruskal‒Wallis test followed by Dunn post hoc analysis. Correlations between the relative abundance of the fecal gut microbiota, cognitive levels, and ALFF values in active brain regions were performed via Pearson’s correlation analysis. The Pearson correlation coefficient R and the P values were calculated via Python in Excel. All the statistical tests were two-sided, and P < 0.05 was considered statistically significant.
Data availability
The data that support the findings of this study are available from the corresponding author, Yi Zhu, upon reasonable request. Raw data have been deposited to National Center for Biotechnology Information (NCBI) under the BioProject number PRJNA1248708.
Abbreviations
- AD:
-
Alzheimer’s Disease
- ALFF:
-
Amplitude of Low-Frequency Fluctuation
- AAL:
-
Anatomical Automatic Labeling
- IQR:
-
Interquartile Range
- FALFF:
-
Fractional Amplitude of Low-Frequency Fluctuation
- Lefse:
-
Linear Discriminant Analysis Effect Size
- LDA:
-
Linear Discriminant Analysis
- KI:
-
Kupperman Index
- KEGG:
-
Kyoto Encyclopedia of Genes and Genomes
- MoCA:
-
Montreal Cognitive Assessment
- MRI:
-
Magnetic Resonance Imaging
- MMSE:
-
Minimum Mental State Examination
- MNI:
-
Montreal Neurological Institute
- OUT:
-
Operational Taxonomic Unit
- PMS:
-
Perimenopausal Syndrome
- PCR:
-
Polymerase Chain Reaction
- PCoA:
-
Principal Coordinate Analysis
- PICRUSt:
-
Phylogenetic Study of Communities By Reconstruction Of Unobserved States
- RSL:
-
Raphanus Sativus L
- rs-fMRI:
-
Resting-State Functional Magnetic Resonance Imaging
- ReHo:
-
Regional Homogeneity
- ROI:
-
Regions of Interest
- SFE:
-
Sulforaphene
References
Gava, G. et al. Cognition mood and sleep in menopausal transition: The role of menopause hormone therapy. Medicina (Kaunas) 55, 668 (2019).
Sussman, M. et al. Prevalence of menopausal symptoms among mid-life women: Findings from electronic medical records. BMC Women Health 15, 58 (2015).
Sassarini, D. J. Depression in midlife women. Maturitas 94, 149–154 (2016).
Santoro, N., Epperson, C. N. & Mathews, S. B. Menopausal symptoms and their management. Endocrinol. Metab. Clin. North Am. 44, 497–515 (2015).
Herber-Gast, G.-C.M. & Mishra, G. D. Early severe vasomotor menopausal symptoms are associated with diabetes. Menopause 21, 855–860 (2014).
Thurston, R. C. Vasomotor symptoms: Natural history, physiology, and links with cardiovascular health. Climacteric 21, 96–100 (2018).
Miller, V. M. et al. What’s in a name: Are menopausal ‘hot flashes’ a symptom of menopause or a manifestation of neurovascular dysregulation?. Menopause 25, 700–703 (2018).
Dunneram, Y., Greenwood, D. C. & Cade, J. E. Diet, menopause and the risk of ovarian, endometrial and breast cancer. Proc. Nutr. Soc. 78, 438–448 (2019).
Brinton, R. D., Yao, J., Yin, F., Mack, W. J. & Cadenas, E. Perimenopause as a neurological transition state. Nat. Rev. Endocrinol. 11, 393–405 (2015).
Morgan, K. N., Derby, C. A. & Gleason, C. E. Cognitive changes with reproductive aging, perimenopause, and menopause. Obstet. Gynecol. Clin. North Am. 45, 751–763 (2018).
Devi, G. Menopause-Related Cognitive Impairment. Obstet Gynecol 132, 1325–1327 (2018).
Mosconi, L. et al. Increased Alzheimer’s risk during the menopause transition: A 3-year longitudinal brain imaging study. PLoS ONE 13, e0207885 (2018).
Guarner, F. & Malagelada, J.-R. Gut flora in health and disease. Lancet 361, 512–519 (2003).
Chen, K. L. & Madak-Erdogan, Z. Estrogen and microbiota crosstalk: Should we pay attention?. Trend. Endocrinol. Metab. 27, 752–755 (2016).
Flores, R. et al. Fecal microbial determinants of fecal and systemic estrogens and estrogen metabolites: A cross-sectional study. J. Transl. Med. 10, 253. https://doi.org/10.1186/1479-5876-10-253 (2012).
Liu, Y. et al. The relationship between menopausal syndrome and gut microbes. BMC Women Health 22, 437 (2022).
Baker, J. M., Al-Nakkash, L. & Herbst-Kralovetz, M. M. Estrogen-gut microbiome axis: Physiological and clinical implications. Maturitas 103, 45–53 (2017).
Vieira, A. T., Castelo, P. M., Ribeiro, D. A. & Ferreira, C. M. Influence of oral and gut microbiota in the health of menopausal women. Front. Microbiol. 8, 1884 (2017).
Santos-Marcos, J. A. et al. Influence of gender and menopausal status on gut microbiota. Maturitas 116, 43–53 (2018).
Meng, Q. et al. The gut microbiota during the progression of atherosclerosis in the perimenopausal period shows specific compositional changes and significant correlations with circulating lipid metabolites. Gut. Microb. 13(1), 27 (2021).
Cryan, J. F. et al. The Microbiota-gut-brain axis. Physiol. Rev. 99, 1877–2013 (2019).
Jiang, C., Li, G., Huang, P., Liu, Z. & Zhao, B. The gut microbiota and Alzheimer’s Disease. J. Alzheimer. Dis. 58, 1–15 (2017).
Sharon, G., Sampson, T. R., Geschwind, D. H. & Mazmanian, S. K. The central nervous system and the gut microbiome. Cell 167, 915–932 (2016).
Sandhu, K. V. et al. Feeding the microbiota-gut-brain axis: Diet, microbiome, and neuropsychiatry. Transl. Res. 179, 223–244 (2017).
Foster, J. A. & McVey Neufeld, K.-A. Gut-brain axis: How the microbiome influences anxiety and depression. Trend. Neuro. sci. 36(305), 312 (2013).
Seo, D.-O. & Holtzman, D. M. Gut Microbiota: From the forgotten organ to a potential key player in the pathology of Alzheimer’s disease. J. Gerontol. A. Biol. Sci. Med. Sci. 75, 1232–1241 (2020).
C, M., A, S., Ma, M. & C, S. The gut-brain axis: Interactions between enteric microbiota, central and enteric nervous systems. Ann. Gastroenterol. 28, 203 (2015).
Y, S. et al. The gut microbiome as a therapeutic target for cognitive impairment. J. gerontol. Series A, Biol. Sci. Med. Sci. 75, 1242 (2020).
Liu, P. et al. Gut microbiota interacts with intrinsic brain activity of patients with amnestic mild cognitive impairment. CNS Neurosci. Ther. 27, 163–173 (2020).
TILLISCH, K. et al. Consumption of fermented milk product with probiotic modulates brain activity. Gastroenterology https://doi.org/10.1053/j.gastro.2013.02.043 (2013).
Tillisch, K. et al. Brain structure and response to emotional stimuli as related to gut microbial profiles in healthy women. Psychosom. Med. 79, 905–913 (2017).
Lu, W., Sun, Y., Gao, H. & Qiu, J. A review of multi-modal magnetic resonance imaging studies on perimenopausal brain: A hint towards neural heterogeneity. Eur. Radiol. https://doi.org/10.1007/s00330-023-09549-5 (2023).
Liu, M. et al. Changes in the regional homogeneity of resting-state magnetic resonance imaging in perimenopausal women. BMC Women. Health 21, 39 (2021).
Zhang, Y., Fu, W. Q., Liu, N. N. & Liu, H. J. Alterations of regional homogeneity in perimenopause: A resting-state functional MRI study. Climacteric 25, 460–466 (2022).
He, L., Guo, W., Qiu, J., An, X. & Lu, W. Altered spontaneous brain activity in women during menopause transition and its association with cognitive function and serum estradiol level. Front. Endocrinol. (Lausanne) 12, 652512 (2021).
Lu, W., Guo, W., Cui, D., Dong, K. & Qiu, J. Effect of sex hormones on brain connectivity related to sexual function in perimenopausal women: A resting-state fmri functional connectivity study. J. Sex. Med. 16, 711–720 (2019).
Tran, K. H. et al. Decreased GABA+ Levels in the medial prefrontal cortex of perimenopausal women: A 3T 1H-MRS study. Int. J. Neuropsychopharmacol. 26, 32–41 (2022).
Sheline, Y. I. & Raichle, M. E. Resting state functional connectivity in preclinical Alzheimer’s disease. Biol. Psychiatry 74, 340–347 (2013).
Zang, Y., Jiang, T., Lu, Y., He, Y. & Tian, L. Regional homogeneity approach to fMRI data analysis. Neuroimage 22, 394–400 (2004).
Peltier, S. J. & Noll, D. C. T(2)(*) dependence of low frequency functional connectivity. Neuroimage 16, 985–992 (2002).
Zou, Q.-H. et al. An improved approach to detection of amplitude of low-frequency fluctuation (ALFF) for resting-state fMRI: fractional ALFF. J Neurosci Methods 172, 137–141 (2008).
Zang, Y.-F. et al. Altered baseline brain activity in children with ADHD revealed by resting-state functional MRI. Brain Dev 29, 83–91 (2007).
Liu, N., Zhang, Y., Liu, S., Zhang, X. & Liu, H. Brain functional changes in perimenopausal women: An amplitude of low-frequency fluctuation study. Menopause 28, 384–390 (2021).
Brinton, R. D., Yao, J., Yin, F., Mack, W. J. & Cadenas, E. Perimenopause as a neurological transition state. Nat. Rev. Endocrinol. 11(7), 393–405. https://doi.org/10.1038/nrendo.2015.82 (2015).
Mosconi, L. et al. Perimenopause and emergence of an Alzheimer’s bioenergetic phenotype in brain and periphery. PLoS ONE 12(10), e0185926. https://doi.org/10.1371/journal.pone.0185926 (2017).
Chen, K. L. & Madak-Erdogan, Z. Estrogen and Microbiota Crosstalk: Should We Pay Attention?. Trend. Endocrinol. Metab. 27(11), 752–755. https://doi.org/10.1016/j.tem.2016.08.001 (2016).
Santoro, N., Roeca, C., Peters, B. A. & Neal-Perry, G. The Menopause Transition: Signs, Symptoms, and Management Options. J. Clin. Endocrinol. Metab. 106(1), 1–15 (2021).
Gao, L. et al. Traditional uses, phytochemistry, transformation of ingredients and pharmacology of the dried seeds of Raphanus sativus L. (Raphani Semen) A comprehensive review. J. Ethnopharmacol. 294, 115387. https://doi.org/10.1016/j.jep.2022.115387 (2022).
Moore, K., Hughes, C. F., Ward, M., Hoey, L. & McNulty, H. Diet, nutrition and the ageing brain: Current evidence and new directions. Proc. Nutr. Soc. 77, 152–163 (2018).
Moles, L. & Otaegui, D. The impact of diet on microbiota evolution and human health. Is diet an adequate tool for microbiota modulation?. Nutrients 12, 1654 (2020).
Scarmeas, N., Anastasiou, C. A. & Yannakoulia, M. Nutrition and prevention of cognitive impairment. Lancet. Neurol. 17, 1006–1015 (2018).
Nurk, E. et al. Cognitive performance among the elderly in relation to the intake of plant foods. Hordaland Health Study. Br. J. Nutr. 104, 1190–1201 (2010).
Yang, W., Liu, Y., Xu, Q.-Q., Xian, Y.-F. & Lin, Z.-X. Sulforaphene ameliorates neuroinflammation and hyperphosphorylated tau protein via regulating the PI3K/Akt/GSK-3β pathway in experimental models of alzheimer’s disease. Oxid. Med. Cell Longev 2020, 4754195 (2020).
Shiina, A. et al. An open study of sulforaphane-rich broccoli sprout extract in patients with schizophrenia. Clin. Psychopharmacol. Neurosci. 13, 62–67 (2015).
Nouchi, R. et al. Brain training and sulforaphane intake interventions separately improve cognitive performance in healthy older adults, whereas a combination of these interventions does not have more beneficial effects: Evidence from a randomized controlled trial. Nutrient 13, 352 (2021).
Varangis, E., Razlighi, Q., Habeck, C. G., Fisher, Z. & Stern, Y. Between-network functional connectivity is modified by age and cognitive task ___domain. J. Cogn. Neurosci. 31, 607–622 (2019).
Gaynor, A. M. et al. Diet moderates the effect of resting state functional connectivity on cognitive function. Sci. Rep. 12, 16080 (2022).
Berding, K. et al. Diet and the microbiota–Gut–Brain axis: Sowing the seeds of good mental health. Adv. Nutr. 12, 1239–1285 (2021).
Armet, A. M. et al. Rethinking healthy eating in light of the gut microbiome. Cell Host Microb. 30, 764–785 (2022).
Liu, Z. et al. Gut microbiota mediates intermittent-fasting alleviation of diabetes-induced cognitive impairment. Nat. Commun. 11, 855 (2020).
Shi, H. et al. β-glucan attenuates cognitive impairment via the gut-brain axis in diet-induced obese mice. Microbiome 8, 143 (2020).
Kakarla, R. et al. Current understanding and future directions of cruciferous vegetables and their phytochemicals to combat neurological diseases. Phytother. Res. 38(3), 1381–1399. https://doi.org/10.1002/ptr.8122 (2024).
Wang, R. et al. Sulforaphane-driven reprogramming of gut microbiome and metabolome ameliorates the progression of hyperuricemia. J. Adv. Res. 52, 19–28. https://doi.org/10.1016/j.jare.2022.11.003 (2023).
Bacon, J. L. The Menopausal Transition. Obstet. Gynecol. Clin. North Am. 44, 285–296 (2017).
Mosconi, L. et al. Perimenopause and emergence of an Alzheimer’s bioenergetic phenotype in brain and periphery. PLoS ONE 12, e0185926 (2017).
McGrattan, A. M. et al. Diet and inflammation in cognitive ageing and Alzheimer’s Disease. Curr. Nutr. Rep. 8, 53–65 (2019).
Dinan, T. G. et al. Feeding melancholic microbes: MyNewGut recommendations on diet and mood. Clin. Nutr. 38, 1995–2001 (2019).
Prehn, K. et al. Caloric restriction in older adults-differential effects of weight loss and reduced weight on brain structure and function. Cereb. Cortex. 27, 1765–1778 (2017).
Burokas, A., Moloney, R. D., Dinan, T. G. & Cryan, J. F. Microbiota regulation of the Mammalian gut-brain axis. Adv. Appl. Microbiol. 91, 1–62 (2015).
Junges, V. M., Closs, V. E., Nogueira, G. M. & Gottlieb, M. G. V. Crosstalk between gut microbiota and central nervous system: A focus on Alzheimer’s disease. Curr. Alzheimer Res. 15, 1179–1190 (2018).
Whitehouse, P. J. & George, D. R. Dignity for all: How the challenges of Alzheimer’s disease need rethinking and revaluing. JAD. 90(4), 1831–1833. https://doi.org/10.3233/JAD-221066 (2022).
Thanapornsangsuth, P. et al. Prospective evaluation of plasma phosphorylated tau in a real-life memory clinic in Thailand. Alzheimer’s & dementia. 19(6), 2745–2749. https://doi.org/10.1002/alz.13022 (2023).
Psaltopoulou, T. et al. Mediterranean diet, stroke, cognitive impairment, and depression: A meta-analysis. Ann. Neurol. 74, 580–591 (2013).
Opie, R. S. et al. Dietary recommendations for the prevention of depression. Nutr. Neurosci. 20, 161–171 (2017).
Nanri, A. et al. Dietary patterns and depressive symptoms among Japanese men and women. Eur. J. Clin. Nutr. 64, 832–839 (2010).
Scarmeas, N., Anastasiou, C. A. & Yannakoulia, M. Nutrition and prevention of cognitive impairment. Lancet Neurol. 17(11), 1006–1015. https://doi.org/10.1016/S1474-4422(18)30338-7 (2018).
李运伦, 赵婧 & 霍青. 莱菔子的现代研究及临床应用. 长春中医药大学学报 0, (2011).
Gao, L. et al. Traditional uses, phytochemistry, transformation of ingredients and pharmacology of the dried seeds of Raphanus sativus L. (Raphani Semen), A comprehensive review. J. Ethnopharmacol. 294, 115387 (2022).
Johnson, A. J. et al. Daily sampling reveals personalized diet-microbiome associations in humans. Cell Host Microbe 25, 789-802.e5 (2019).
Magne, F. et al. The Firmicutes/Bacteroidetes ratio: A Relevant marker of gut dysbiosis in obese patients?. Nutrient. 12, 1474 (2020).
Stewart, C. S., Duncan, S. H. & Cave, D. R. Oxalobacter formigenes and its role in oxalate metabolism in the human gut. FEMS Microbiol. Lett. 230, 1–7 (2004).
Nishida, A. et al. Gut microbiota in the pathogenesis of inflammatory bowel disease. Clin. J. Gastroenterol. 11, 1–10 (2018).
Baker, S. & The, H. C. Recent insights into Shigella. Curr. Opin. Infect. Dis. 31, 449–454 (2018).
von Graevenitz, A. The role of Aeromonas in diarrhea: A review. Infection 35, 59–64 (2007).
Kitazawa, M., Oddo, S., Yamasaki, T. R., Green, K. N. & LaFerla, F. M. Lipopolysaccharide-induced inflammation exacerbates tau pathology by a cyclin-dependent kinase 5-mediated pathway in a transgenic model of Alzheimer’s disease. J. Neurosci. 25, 8843–8853 (2005).
Kawagoe, T., Onoda, K. & Yamaguchi, S. Subjective memory complaints are associated with altered resting-state functional connectivity but not structural atrophy. Neuroimage Clin. 21, 101675 (2019).
Jung, J. et al. Impact of lingual gyrus volume on antidepressant response and neurocognitive functions in major depressive disorder: A voxel-based morphometry study. J. Affect. Disord. 169, 179–187 (2014).
Kumar, N. & Priyadarshi, B. Differential effect of aging on verbal and visuo-spatial working memory. Aging Dis. 4, 170–177 (2013).
Yeager, B. E. et al. Central precuneus lesions are associated with impaired executive function. Brain Struct. Funct. 227, 3099–3108 (2022).
Wang, J. et al. Hippocampus-based dynamic functional connectivity mapping in the early stages of Alzheimer’s disease. J. Alzheimer’s Dis. 85, 1795–1806 (2022).
Pang, L. et al. Disruption of cerebellar-cerebral functional connectivity in temporal lobe epilepsy and the connection to language and cognitive functions. Front. Neurosci. 16, 871128 (2022).
Nie, K. et al. Roseburia intestinalis: A beneficial gut organism from the discoveries in genus and species. Front. Cell Infect. Microbiol. 11, 757718 (2021).
Eicher, T. P. & Mohajeri, M. H. Overlapping mechanisms of action of brain-active bacteria and bacterial metabolites in the pathogenesis of common brain diseases. Nutrient. 14, 2661 (2022).
McCracken, B. A. & Nathalia Garcia, M. Phylum Synergistetes in the oral cavity: A possible contributor to periodontal disease. Anaerobe 68, 102250 (2021).
Horz, H.-P., Citron, D. M., Warren, Y. A., Goldstein, E. J. C. & Conrads, G. Synergistes group organisms of human origin. J. Clin. Microbiol. 44, 2914–2920 (2006).
Palmas, V. et al. Gut microbiota markers and dietary habits associated with extreme longevity in healthy sardinian centenarians. Nutrient. 14, 2436 (2022).
Schulz, K. F., Altman, D. G. & Moher, D. Consort 2010 statement: Updated guidelines for reporting parallel group randomised trials. J. Pharmacol. Pharmacother. 1, 100–107 (2010).
Folstein, M. F., Folstein, S. E. & McHugh, P. R. ‘Mini-mental state’. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 12, 189–198 (1975).
Yu, J., Li, J. & Huang, X. The beijing version of the montreal cognitive assessment as a brief screening tool for mild cognitive impairment: A community-based study. BMC Psychiatry 12, 156 (2012).
Blake, M. R., Raker, J. M. & Whelan, K. Validity and reliability of the bristol stool form scale in healthy adults and patients with diarrhoea-predominant irritable bowel syndrome. Aliment. Pharmacol. Ther. 44, 693–703 (2016).
Segata, N. et al. Metagenomic biomarker discovery and explanation. Genome. Biol. 12, R60 (2011).
Douglas, G. M. et al. PICRUSt2: An improved and extensible approach for metagenome inference. 672295 Preprint at https://doi.org/10.1101/672295 (2019).
Langille, M. G. I. et al. Predictive functional profiling of microbial communities using 16S rRNA marker gene sequences. Nat. Biotechnol. 31, 814–821 (2013).
Jia, X.-Z. et al. RESTplus: an improved toolkit for resting-state functional magnetic resonance imaging data processing. Sci. Bull. 64, 953–954 (2019).
Yan. DPARSF: a MATLAB toolbox for “pipeline” data analysis of resting-state fMRI. Front. Syst. Neurosci. (2010) https://doi.org/10.3389/fnsys.2010.00013.
Yan, C.-G., Wang, X.-D., Zuo, X.-N. & Zang, Y.-F. DPABI: Data processing & analysis for (Resting-State) brain imaging. Neuroinform 14, 339–351 (2016).
Acknowledgements
The authors gratefully acknowledge all the study participants and staff for their help and cooperation.
Funding
Guizhou Provincial Science and Technology Projects,qkhjc-ZK[2023]yb351,qkhjc-ZK[2023]yb351,qkhjc-ZK[2023]yb351
Author information
Authors and Affiliations
Contributions
Caihui Guo (First Author): Conceptualization, Methodology, Validation, Formal analysis, Investigation, Writing—original draft, Writing—review & editing; Zhenliang Xiong: Formal analysis, Writing—original draft; Lin Yang: Investigation, Resources, Project administration, Funding acquisition; Mingxian Bai: Investigation; Xianchun Zeng (Corresponding Author): Resources, Writing—Review & Editing, Supervision, Project Administration; Yi Zhu (Corresponding Author): Conceptualization, Resources, Writing—Review & Editing, Supervision, Project Administration.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was approved by the Ethics Committee of the Affiliated Hospital of Guizhou Medical University (2021 Ethics No. (675)). The clinical registration ID: ChiCTR2400084007, URL: https://www.chictr.org.cn/showproj.html?proj=197060 (Retrospectively registered).
Consent for publication
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Guo, C., Xiong, Z., Yang, L. et al. Effects of a healthy diet based on seed-rich vegetables on the gut microbiota and intrinsic brain activity in perimenopausal women: A pilot study on cognitive improvement. Sci Rep 15, 17444 (2025). https://doi.org/10.1038/s41598-025-99406-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-99406-w