Abstract
This study uses Mendelian randomization (MR) to investigate the causal roles of CD40 and CD40L in BC.Data from genome-wide association studies (GWAS) on BC (overall, ER-positive, and ER-negative subtypes) and CD40/CD40L levels were obtained from the IEU database. Causal associations were assessed using the inverse-variance weighted (IVW) method, with additional robustness checks performed via MR-Egger, weighted median, and weighted mode methods. Sensitivity analyses, including Cochran’s Q test and MR-PRESSO, were conducted to assess heterogeneity and pleiotropy. Reverse MR analyses were also performed to examine if BC influences CD40/CD40L levels.A borderline significant association was found between CD40 levels and overall BC risk (IVW OR 1.027, 95% CI 1.000–1.054, p = 0.049), with a more robust association observed for ER-positive BC (OR 1.048, 95% CI 1.016–1.082, p = 0.003). No significant associations were found between CD40 levels and ER-negative BC. CD40L did not show any significant associations with BC. Reverse MR analysis indicated no causal effect of BC on CD40/CD40L levels. CD40 is causally associated with a borderline increase in overall BC risk and a more significant increase in ER-positive BC risk. These findings suggest a potential role for CD40 in BC, particularly in ER-positive cases.
Similar content being viewed by others
Introduction
Breast cancer (BC) is a significant global health concern and remains the most commonly diagnosed cancer among women worldwide. In 2022, approximately 2.3 million women were diagnosed with BC, leading to around 670,000 deaths globally1. Despite advancements in early detection and treatment, BC remains a leading cause of cancer-related mortality in women. While several risk factors, including genetic predisposition, lifestyle, and environmental influences, have been identified, a substantial portion of BC cases occur without clear, identifiable risk factors beyond sex and age1,2. This highlights the importance of continuing to investigate potential molecular and genetic contributors to BC risk. CD40, a receptor expressed on various immune and non-immune cells, is primarily known for its role in immune responses, where it functions as a critical regulator of inflammation and immune cell activation. CD40 interacts with its ligand, CD40 ligand (CD40L), which is expressed on activated CD4 + T cells, platelets, and other immune cells3,4,5. The CD40/CD40L axis has been implicated in the pathogenesis of several diseases, including atherosclerosis, autoimmune disorders, and malignancies6,7,8.
In the context of breast cancer (BC), CD40 has shown promise as a prognostic marker. For instance, Slobodova et al. reported that cytoplasmic CD40 expression is associated with more favorable prognostic factors in BC patients9. Experimental studies further suggest that activation of the CD40/CD40L pathway can inhibit the growth of CD40-positive BC cells while having no effect on CD40-negative cells10. These findings highlight the potential role of CD40 in BC progression, particularly through its regulation of immune responses and inflammation. However, while CD40 expression has been linked to better prognosis, the exact causal relationship between CD40/CD40L signaling and the development or progression of BC remains poorly understood, necessitating further investigation.
CD40 is primarily known for its role in immune responses, where it functions as a critical regulator of inflammation and immune cell activation. It interacts with its ligand, CD40L, which is expressed on activated CD4 + T cells, platelets, and other immune cells11. The CD40/CD40L axis has been implicated in the pathogenesis of several diseases, including atherosclerosis, autoimmune disorders, and malignancies. In the context of BC, CD40 expression has been linked to better prognostic factors. Moreover, experimental studies have demonstrated that activation of the CD40/CD40L pathway can inhibit the growth of CD40-positive BC cells, while having no effect on CD40-negative cells10. Despite these findings, the causal relationship between CD40/CD40L signaling and BC development or progression remains poorly understood, necessitating further investigation.
Mendelian randomization (MR) is a powerful approach to investigating causal relationships between genetic variants and disease outcomes12. Although MR is most commonly applied when there is an observed association between an exposure and an outcome, it is also useful for exploring causal hypotheses when there is strong biological plausibility but limited observational evidence. CD40’s established role in immune regulation and its suggested link to BC progression provide a compelling rationale for employing MR to investigate causality in this context. MR uses genetic variants as instrumental variables (IVs) to infer causality between an exposure and an outcome13, relying on certain assumptions: (1) the variant must be associated with the exposure; (2) it should not be associated with confounders that affect the outcome; and (3) it should influence the outcome solely through the exposure.
MR has been widely applied in BC research, leveraging large-scale genome-wide association studies (GWAS) and biobank data to investigate risk factors. For instance, prior MR studies have suggested a causal role for high-density lipoprotein cholesterol (HDL-C) in BC etiology14, as well as type 2 diabetes mellitus in BC-specific survival15. However, the causal relationship between CD40 and CD40L levels and BC risk using MR has yet to be thoroughly explored.
In this study, we applied MR analysis to investigate whether CD40 and its ligand CD40L are causally associated with BC risk. By leveraging large-scale genetic data, we aim to provide insight into the roles of CD40 and CD40L in BC pathogenesis, potentially offering new avenues for targeted prevention and treatment strategies.
Methods
Study design
The MR analysis followed the Strengthening the Reporting of Observational Studies in Epidemiology using Mendelian Randomization (STROBE-MR) guidelines16. No further ethical approval was required because the present study was based on publicly available GWAS data. The analysis adhered to three assumptions of MR studies (Fig. 1)13.
Data source
The BC and subtype GWAS data were obtained from previously published studies17. The overall BC data (including both ER + and ER- subtypes) were sourced from a GWAS study published in Nature18, which included 122,977 BC cases and 105,974 controls, with a total of 10,680,257 SNPs. The ER- positive (ER+) BC data were obtained from a recent GWAS the same study, which analyzed 69,501 ER + BC cases and 105,974 controls, with a total of 10,680,257 SNPs. For ER-negative (ER-) BC, data were similarly extracted from the same GWAS, involving 21,468 ER- BC cases and 105,974 controls, with 10,680,257 SNPs. All data were derived from populations of European ancestry. ER-negative BC data were extracted from the same study18; this GWAS assessed variants associated with the risk of ER-negative BC in 21,468 ER-negative BC cases and 100,594 controls, combined with 18,908 BRCA1 mutation carriers (9,414 with BC), all of European origin.
The exposure data for CD40 and CD40L were obtained from two separate GWAS studies19,20; Data on CD40 were sourced from a study published in Nature Immunology20, which included 14,736 participants and 12,958,023 SNPs. Data on CD40L came from another study published in Nature Metabolism19, which included 21,758 participants and 20,300,000 SNPs. All participants in these studies were of European ancestry.
Instrumental variable (IVs) selection
MR studies used single nucleotide polymorphisms (SNPs) as IVs. The IVs included in this study met the following criteria: (i) SNPs were first screened for genome-wide significant association with BC (P < 5 * 10−8). Due to the insufficient number of IVs for CD40 and CD40L, the threshold for these exposures was relaxed to P < 5 * 10−621; (ii) SNPs with a minimum minor allele frequency (MAF) > 0.01 were screened; (iii) according to the standard of R2 < 0.001 and window size = 10,000 kb, linkage disequilibrium (LD) between SNPs were removed22; (4) when the selected IVs were not present in the summary data of the outcome, we searched for SNPs with high LD (R2 > 0.8) with the IVs as proxy SNPs to replace the existing ones; (5) the F-value for each SNP in the IV was calculated to assess IV strength, excluding potential weak instrument bias between the IV and exposure factors, using the following formula: F = R2 * (N-2) / (1-R2) where R2 represents the proportion of exposure variance explained by the SNP in the IV. The requirement for the F-value was >10.
MR analysis
The inverse variance weighted (IVW) method23 was used to assess the causal association between CD40/CD40L and the BC by calculating the odds ratio (OR) and 95% confidence interval (CI). MR-Egger, weighted median, and weighted mode methods were used to test the robustness of the results24; the MR-Egger method accounts for the presence of intercept and provides accurate causal effect estimates in the presence of pleiotropic bias25; the weighted median method assumes that half of the instrumental variables are valid, analyzing the causal association between exposure and outcome26. All analyses in this study were conducted using the “Two Sample MR” package. Visualizations were performed using scatter plots and sensitivity analysis plots.
Sensitivity analysis
Sensitivity analysis was conducted to detect potential heterogeneity in MR studies. Cochran’s Q test was used to assess heterogeneity among IVs, with P > 0.05 indicating low heterogeneity, meaning the estimates among instrumental variables were randomly distributed and had little impact on IVW results. Considering the potential impact of genetic variation on the estimation of association effects, this study used the MR-Egger regression method to explore the presence of horizontal pleiotropy. When the intercept of MR-Egger regression approaches zero or is not statistically significant, it suggests the absence of pleiotropy. Additionally, the MR pleiotropy residual sum and outlier (MR-PRESSO) method was used to detect potential outliers (i.e., SNPs with P < 0.05) and re-estimate causal associations after their removal to correct for horizontal pleiotropy. Leave-one-out analysis was employed to assess the robustness and consistency of the results.
Reverse MR analysis
To explore whether the BC had any causal effect on CD40/CD40L, we also performed a reverse MR Analysis using BC-associated SNPs as IVs (i.e., BC as exposure and identified CD40/CD40L as outcome).
Results
Causal association between CD40/CD40L and BC
Selection of IVs
In total, 44 SNPs were selected as IVs for the analysis of CD40 and CD40L. Specifically, 28 SNPs were selected as IVs for CD40 measurement, with an average F-statistic of 70.63, ranging from 20.89 to 1275.9. For CD40L measurement, 16 SNPs were selected with an average F-statistic of 22.9, ranging from 20.88 to 32.02. These values indicate that the IVs are sufficiently strong for the MR analysis. One SNP (rs141401004) did not match the summary data for BC and its subtypes (ER-positive and ER-negative), and proxy SNPs (rs2963653 and rs67794450) were used as replacements.
MR analysis
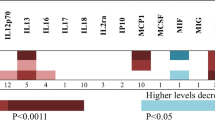
The results of the MR analysis revealed significant associations between CD40 measurement and ER-positive BC (Table 1). Using the IVW method, CD40 measurement was associated with an increased risk of ER-positive BC (Fig. 2), with an OR of 1.048 (95% CI 1.016–1.082, p = 0.003). Furthermore, the weighted median method also indicated a significant association (OR 1.043, 95% CI 1.005–1.081, p = 0.024), and the weighted mode method supported this association as well (OR 1.043, 95% CI 1.006–1.08, p = 0.033). For overall BC (Fig. 3), a borderline significant association was observed between CD40 measurement and increased risk, with the IVW method yielding an OR of 1.027 (95% CI 1.000–1.054, p = 0.049). However, no statistically significant associations were found between CD40 measurement and ER-negative BC across any of the MR methods.
In contrast, no significant associations were found between CD40L and overall BC or its subtypes (ER-positive and ER-negative BC) based on the IVW results. The MR-Egger regression indicated potential pleiotropy for CD40L in relation to overall BC (p = 0.013) and ER-positive BC (p = 0.038), but these findings were not corroborated by the other MR methods, which showed no significant associations.
Sensitivity analysis
The MR-Egger regression results indicated no evidence of horizontal pleiotropy affecting the analysis (Table S1). The heterogeneity test showed no significant heterogeneity for the CD40/CD40L measurement and BC associations (Table S1). Moreover, the MR-PRESSO analysis confirmed the robustness of the results, with no outliers detected in the analyses (Table S2).
Reverse analysis of the causal relationship between BC and CD40/CD40L
Selection of IVs
We reverse-assessed the causal relationship between BC and CD40/CD40L. A total of 287 SNPs were selected as IVs for this analysis. For CD40 measurement, 137 SNPs were selected with an average F-statistic of 92.73 (range: 29.74–1231.66). For CD40L measurement, 139 SNPs were selected with an average F-statistic of 87.9 (range: 29.73–1231.6). Additionally, several proxy SNPs were used in cases where the original SNPs were not present in the summary data. For example, rs490706 was replaced by rs599298 for CD40L levels, while rs10623258 was replaced by rs4983543 for CD40 measurements. Several palindromic SNPs, including rs418053, rs9284657, and rs62116991, were excluded from the analysis due to their weak instrument characteristics.
MR analysis
The results of reverse gene prediction showed no statistically significant association between BC and CD40 traits (Table 2). For CD40 measurement, the IVW method showed no significant association with BC overall (OR 1.027, 95% CI 1.000–1.054, p = 0.049) or its subtypes, including ER-positive and ER-negative BC. Similarly, no significant associations were found between CD40L levels and BC [OR 0.987, 95% CI 0.958–1.018, p = 0.405].
Sensitivity analysis
The MR-Egger regression results indicated no evidence of horizontal pleiotropy affecting the analysis (Table S3). For BC overall, the MR-Egger intercept for CD40 measurement was − 0.002 (p = 0.463), and for CD40L levels, it was − 0.001 (p = 0.642), suggesting that pleiotropy did not bias the results. Heterogeneity tests demonstrated no significant heterogeneity in most analyses. For instance, the Cochran’s Q statistic for CD40 measurement and BC was 148.619 (p = 0.217), and for CD40L and BC, it was 138.196 (p = 0.479). However, some heterogeneity was noted in the CD40 measurement and ER-positive BC analysis (Q = 138.694, p = 0.009). The MR-PRESSO analysis also confirmed that there were no notable outliers affecting the results (Table S4). The global test p-values for BC and CD40/CD40L were all non-significant, further supporting the robustness of the findings. For example, for ER-positive BC and CD40 measurement, the global p-value was 0.01, and for BC and CD40L levels, it was 0.492, without any distortion in the results.
Discussion
In this study, we conducted a comprehensive MR analysis to investigate the potential causal relationships between CD40, CD40L, and BC, including its subtypes, estrogen receptor (ER)-positive and ER-negative BC. We found evidence suggesting a causal association between CD40 and a borderline increase in overall BC risk, with a more significant increase in ER-positive BC risk, while no association was observed for ER-negative BC. However, no significant causal associations between CD40L and any BC subtypes were identified. Additionally, reverse MR analysis indicated no causal relationship between BC and CD40/CD40L levels, supporting the directionality of our findings.
Our results align with previous observational studies that suggest CD40 plays a role in BC progression, particularly in ER-positive cases. CD40, known for its role in immune regulation, has been linked to better prognosis in BC patients, especially those with ER-positive tumors27,28,29. The significant association observed in our study supports the hypothesis that CD40 may contribute to the pathogenesis or progression of ER-positive BC, potentially through immune modulation mechanisms30. The absence of a causal relationship between CD40 and ER-negative BC, however, is notable. ER-negative BC is typically more aggressive and driven by distinct molecular mechanisms, which could render the immune-related pathways mediated by CD40 less relevant in its pathogenesis9. Furthermore, the more immunosuppressive tumor microenvironment observed in ER-negative cancers may limit the effects of CD40 activation, which often promotes anti-tumor immune responses31. Future research should explore the specific pathways by which CD40 influences ER-positive BC and investigate the tumor microenvironment’s role in modulating these effects.
In contrast, no significant associations were found between CD40L and BC overall or its subtypes. CD40L, which primarily functions as a ligand for CD40, regulates immune responses and has been shown to promote anti-tumor immunity by activating immune cells such as macrophages, dendritic cells, and B cells4,32. Despite its biological relevance, the absence of significant findings in our MR analysis may reflect several factors, including insufficient statistical power. The number of instrumental variables (16 SNPs) for CD40L was smaller compared to CD40 (28 SNPs), limiting the ability to detect potential causal effects. Additionally, CD40L has pleiotropic effects, influencing multiple biological pathways beyond cancer progression, which may dilute its specific impact on BC risk33,34. The potential for horizontal pleiotropy was suggested by the MR-Egger regression, highlighting the need for caution in interpreting the null findings for CD40L. Future studies with expanded datasets and more robust genetic instruments are warranted to clarify CD40L’s role in BC.
This study’s reliance on data from populations of European ancestry represents another limitation, as it restricts the generalizability of our findings. BC risk and the role of immune-related pathways, including the CD40/CD40L axis, may differ across ethnic groups. Incorporating data from more diverse populations in future studies is critical to understanding the global relevance of CD40 and CD40L in BC. Furthermore, the modest effect sizes observed in our analysis (e.g., ORs of 1.043–1.048 for CD40 and ER-positive BC) suggest that while CD40 may contribute to BC risk, its clinical impact may be limited. These effect sizes are smaller compared to established BC risk factors, such as BRCA1/2 mutations or hormonal factors, highlighting the need to consider CD40 in conjunction with other risk factors when assessing BC susceptibility.
Reverse MR analysis revealed no causal effect of BC on CD40 or CD40L levels, suggesting that changes in CD40/CD40L levels observed in BC patients are more likely a consequence of immune system activation rather than a direct effect of the tumor itself. However, potential confounding factors, such as lifestyle and environmental exposures, which may influence both CD40/CD40L levels and BC risk, were not accounted for in our analysis. Addressing these factors in future studies could provide a more comprehensive understanding of the observed associations.
Finally, the subtype-specific findings for ER-positive BC emphasize the need to explore the biological mechanisms underlying the observed differences. Variations in the tumor microenvironment, immune response, and molecular drivers between ER-positive and ER-negative cancers likely contribute to the differential associations. Understanding these mechanisms could provide valuable insights into the role of CD40 in BC and inform targeted prevention or treatment strategies.
Conclusion
In this study, our findings suggest that CD40 may have subtype-specific roles in BC, particularly in ER-positive cases, while the involvement of CD40L in BC remains unclear. Addressing the limitations of pleiotropy, statistical power, and population diversity in future research will be essential for validating and expanding upon these results. Additionally, integrating genetic, environmental, and clinical data will help refine our understanding of the CD40/CD40L axis’s role in BC and its potential as a therapeutic target.
Data availability
All data generated or analysed during this study are included in this published article.
References
(2023). Available from: https://www.who.int/news-room/fact-sheets/detail/breast-cancer#:~:text=In%202022%2C%20there%20were%202.3,increasing%20rates%20in%20later%20life
Chien, T. J. A review of the endocrine resistance in hormone-positive breast cancer. Am. J. Cancer Res. 11 (8), 3813–3831 (2021).
Bullock, T. N. J. CD40 stimulation as a molecular adjuvant for cancer vaccines and other immunotherapies. Cell Mol. Immunol. 19 (1), 14–22 (2022).
Yuan, M. et al. CD40LG as a prognostic molecular marker regulates tumor microenvironment through immune process in breast Cancer. Int. J. Gen. Med. 14, 8833–8846 (2021).
Zhou, Y., Richmond, A. & Yan, C. Harnessing the potential of CD40 agonism in cancer therapy. Cytokine Growth Factor Rev. 75, 40–56 (2024).
Yan, J. C. et al. Increased levels of CD40-CD40 ligand system in patients with essential hypertension. Clin. Chim. Acta. 355 (1–2), 191–196 (2005).
Damas, J. K. et al. Soluble CD40 ligand in pulmonary arterial hypertension: Possible pathogenic role of the interaction between platelets and endothelial cells. Circulation 110 (8), 999–1005 (2004).
Daub, S. et al. CD40/CD40L and related signaling pathways in cardiovascular health and Disease-The pros and cons for cardioprotection. Int. J. Mol. Sci. 21(22), 8533 (2020).
Slobodova, Z. et al. Analysis of CD40 expression in breast cancer and its relation to clinicopathological characteristics. Neoplasma 58 (3), 189–197 (2011).
Esteva, F. J. et al. CD40 signaling predicts response to preoperative trastuzumab and concomitant Paclitaxel followed by 5-fluorouracil, epirubicin, and cyclophosphamide in HER-2-overexpressing breast cancer. Breast Cancer Res. 9 (6), R87 (2007).
Aloui, C. et al. The signaling role of CD40 ligand in platelet biology and in platelet component transfusion. Int. J. Mol. Sci. 15 (12), 22342–22364 (2014).
Sanderson, E. et al. Mendelian randomization. Nat. Rev. Methods Primers 2, 6 (2022).
Martens, E. P. et al. Instrumental variables: Application and limitations. Epidemiology 17 (3), 260–267 (2006).
Zhou, M. et al. Mendelian randomization analysis revealed potential metabolic causal factors for breast cancer. Sci. Rep. 13 (1), 14290 (2023).
Escala-Garcia, M. et al. Breast cancer risk factors and their effects on survival: A Mendelian randomisation study. BMC Med. 18 (1), 327 (2020).
Skrivankova, V. W. et al. Strengthening the reporting of observational studies in epidemiology using Mendelian randomisation (STROBE-MR): Explanation and elaboration. BMJ 375, n2233 (2021).
Michailidou, K. et al. Association analysis identifies 65 new breast cancer risk loci. Nature 551 (7678), 92–94 (2017).
Milne, R. L. et al. Identification of ten variants associated with risk of estrogen-receptor-negative breast cancer. Nat. Genet. 49 (12), 1767–1778 (2017).
Folkersen, L. et al. Genomic and drug target evaluation of 90 cardiovascular proteins in 30931 individuals. Nat. Metab. 2 (10), 1135–1148 (2020).
Zhao, J. H. et al. Genetics of Circulating inflammatory proteins identifies drivers of immune-mediated disease risk and therapeutic targets. Nat. Immunol. 24 (9), 1540–1551 (2023).
Chen, H. et al. The association between genetically predicted systemic inflammatory regulators and polycystic ovary syndrome: A Mendelian randomization study. Front. Endocrinol. (Lausanne). 12, 731569 (2021).
Wang, R. Mendelian randomization study updates the effect of 25-hydroxyvitamin D levels on the risk of multiple sclerosis. J. Transl. Med. 20 (1), 3 (2022).
Bowden, J. et al. Consistent Estimation in Mendelian randomization with some invalid instruments using a weighted median estimator. Genet. Epidemiol. 40 (4), 304–314 (2016).
Minelli, C. et al. The use of two-sample methods for Mendelian randomization analyses on single large datasets. Int. J. Epidemiol. 50 (5), 1651–1659 (2021).
Burgess, S. & Thompson, S. G. Interpreting findings from Mendelian randomization using the MR-Egger method. Eur. J. Epidemiol. 32 (5), 377–389 (2017).
Burgess, S. et al. A robust and efficient method for Mendelian randomization with hundreds of genetic variants. Nat. Commun. 11 (1), 376 (2020).
Cui, X. et al. Causal associations between CD40/CD40L and aortic diseases: A Mendelian randomization study. Front. Genet. 13, 998525 (2022).
Kim, H. et al. Direct interaction of CD40 on tumor cells with CD40L on T cells increases the proliferation of tumor cells by enhancing TGF-beta production and Th17 differentiation. PLoS ONE. 10 (5), e0125742 (2015).
Wingett, D. G. et al. CD40 is functionally expressed on human breast carcinomas: Variable inducibility by cytokines and enhancement of Fas-mediated apoptosis. Breast Cancer Res. Treat. 50 (1), 27–36 (1998).
Unver, N. et al. Transcriptional splice variants of CD40 and its prognostic value in breast cancer. Turk. J. Biol. 44 (2), 73–81 (2020).
Rodriguez-Perdigon, M. et al. Dual CSF1R Inhibition and CD40 activation demonstrates anti-tumor activity in a 3D macrophage- HER2(+) breast cancer spheroid model. Front. Bioeng. Biotechnol. 11, 1159819 (2023).
Rakhmilevich, A. L., Alderson, K. L. & Sondel, P. M. T-cell-independent antitumor effects of CD40 ligation. Int. Rev. Immunol. 31 (4), 267–278 (2012).
Yedjou, C. G. et al. Assessing the racial and ethnic disparities in breast Cancer mortality in the United States. Int. J. Environ. Res. Public. Health 14(5), 486 (2017).
Hirko, K. A. et al. The impact of race and ethnicity in breast cancer-disparities and implications for precision oncology. BMC Med. 20 (1), 72 (2022).
Acknowledgements
Not applicable.
Funding
This work was supported by the National Natural Science Foundation of China (Nos. 81902816, 82303815) and the Natural Science Funding of Shandong Province (ZR2023MH060). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Junyu Yi, Qingfeng Chen and Xiaoyi Liu carried out the studies, participated in collecting data, and drafted the manuscript. Junyu Yi and Yan Mao performed the statistical analysis and participated in its design. Yongmei Wang and Meng Lv participated in acquisition, analysis, or interpretation of data and draft the manuscript. Yuanyuan Wang and Haibo Wang were responsible for the conception and design of the project and performed revising manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
No further ethical approval was required because the present study was based on publicly available GWAS data. All methods were performed in accordance with the relevant guidelines.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yi, J., Chen, Q., Liu, X. et al. Genetic evidence from Mendelian randomization links CD40 levels to increased risk of estrogen receptor-positive breast cancer. Sci Rep 15, 14892 (2025). https://doi.org/10.1038/s41598-025-99410-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-99410-0