Abstract
This retrospective cohort study investigates axial elongation in myopic children and adolescents wearing single vision spectacles, before and after the availability of proven myopia control spectacles. Electronic clinical records of patients aged 3–17 years who were prescribed single vision spectacle lenses between July 2012 and August 2013 (2012_13 cohort) and between July 2018 and August 2019 (2018_19 cohort) were analyzed. Follow-up duration ranged from 12 to 51 months, and axial elongation was normalized to a 12-month change. There were 330 and 165 patients in the 2012_13 and 2018_19 cohorts, respectively. The annualized axial elongation, expressed as mean (standard error), was 0.27 (0.01) mm for the 2012_13 cohort and 0.26 (0.01) mm for the 2018_19 cohort. In both cohorts, median annual axial growth was ≥ 0.40 mm at ages 3–5, ≥ 0.30 mm at ages 6–8, ≥ 0.20 mm at ages 9–10, ≥ 0.10 mm at ages 11–13, and < 0.10 mm at ages 14–17. Younger age was closely associated with faster annualized axial elongation, with each year of increase in baseline age results in a decrease in annualized axial growth by 0.04 mm. These findings serve as a useful reference for future myopia control trials to assess treatment efficacy.
Similar content being viewed by others
Introduction
The global prevalence of myopia has been increasing for years, presenting considerable challenges to public health, and imposing a substantial economic burden on society1. Projections indicate that by 2050, approximately half of the world’s population will be affected by myopia2. Its prevalence is particularly alarming in East and Southeast Asia, surpassing 90% of schoolchildren living in specific urban areas3. While other parts of the world exhibit lower prevalence rates of 20–50%, they remain higher than those in past generations4,5,6.
Myopia is commonly characterized by abnormal axial elongation, in which axial length (AL) growth exceeds the reduction in refractive power of the cornea and lens7,8. Recently, researchers have shown a growing interest in AL owing to its rapid and non-invasive measurement and the dispensability of cycloplegia, particularly among young children and orthokeratology lens wearers9. Previous studies have also suggested a stronger correlation of visual impairment with AL rather than refractive error10, with excessive AL growth increasing the risk of retinal detachment, myopic macular degeneration, cataracts, and glaucoma11. Therefore, the fundamental goal in controlling myopia is to inhibit axial elongation, thereby reducing the risk of axial growth-related myopic complications9,12.
A recent meta-analysis reported an annual axial elongation of approximately 0.50 mm in Asians and 0.30 mm in Caucasians aged 8 years, decreasing to 0.30 mm and 0.20 mm, respectively, at 11 years13. Defining the expected range of axial growth rates at different ages allows clinicians to identify children at risk of excessive axial elongation and determine whether the treatment efficacy for a specific myopia control intervention is adequate. However, these axial elongation data were primarily obtained from untreated control groups in randomized controlled trials (RCTs), where, despite randomization, participants were often selected based on stringent eligibility criteria that could limit their external validity14. As a result, the reported axial elongation trends may not fully reflect those observed in clinical practice.
Therefore, this study aimed to investigate the axial elongation patterns among Hong Kong myopic children and adolescents wearing single vision (SV) spectacles in a clinical setting, considering factors such as age at initial presentation and sex. Given the increasing availability of myopia control interventions over the past decade, it is believed that axial growth rate among children and adolescents who wear SV spectacles nowadays may be lower compared to those who wore SV spectacles in the past, when limited myopia control options were available. Thus, this study also compares annual axial growth rates before and after the introduction of defocus incorporated multiple segments (DIMS) spectacle lenses into clinical practice, as DIMS is the first spectacle lens design proven to effectively slow down myopia progression and axial elongation15. The findings of this study may provide valuable insights for future clinical trials aimed at assessing the efficacy of myopia control interventions in slowing axial elongation, particularly in light of the growing ethical concerns regarding the inclusion of untreated control groups.
Results
Of the 1418 and 1624 patient records reviewed for the 2012_13 and 2018_19 cohorts, 1088 and 1425 patients were excluded from the respective cohorts, most commonly because of loss to follow-up after the baseline visit, SER > − 0.50D and a follow-up period of less than 12 months (Fig. 1).
In total, 330 patients were included in the 2012_13 cohort and 165 patients in the 2018_19 cohort. Table 1 demonstrates the baseline characteristics of SV spectacles wearers in the 2012_13 and 2018_19 cohorts. At baseline, the 2012_13 cohort was significantly more myopic (median [IQR]: − 2.25 [–4.00, − 1.34] vs. − 1.63 [–3.06, − 1.00] D, P < .001), and had a longer AL (median [IQR]: 24.38 [23.64, 25.25] vs. 24.19 [23.35, 25.00] mm, P = .032) than the 2018_19 cohort. Cycloplegic refraction was conducted in 30% (2012_13 cohort) and 40% (2018_19 cohort) of patients. There were no significant differences in the percentage of male and female participants between the two cohorts (P = .405).
The unadjusted median annualized axial elongation and myopia progression were comparable between the 2012_13 and 2018_19 cohorts (change in AL: P = .198; change in SER: P = .774; Table 2). After adjusting for covariates, the GEE model also revealed similar annualized axial elongation (P = .486) and myopia progression (P = .109) in the two cohorts. The adjusted AL changes reported as mean (SE) were 0.27 (0.01) and 0.26 (0.01) mm/year in the 2012_13 and 2018_19 cohorts, respectively. In the GEE model, age and follow-up duration (both P < .001) were closely associated with the annualized AL change (Table 3). When the baseline age and follow-up period increased, annualized axial elongation decreased. Similarly, annualized myopia progression was slower when the baseline age and follow-up period (both P < .001) increased. In contrast, less myopic SER at baseline was associated with faster annualized myopia progression (P = .013).
Figure 2; Table 4 demonstrate the age-specific annual axial elongation for the SV 2012_13 and 2018_19 cohorts across different percentiles. Overall, axial growth decreases with increasing age in both cohorts. The 25th, 50th, and 75th percentile curves are slightly steeper in the 2012_13 cohort, whereas the 5th and 95th percentile curves are steeper in the 2018_19 cohort, suggesting that the slowest- and fastest-growing eyes in the 2018_19 cohort exhibited greater changes in axial elongation over time (Fig. 2). At the 50th percentile, the 2018_19 cohort tends to show slightly lower axial elongation in younger children (ages 3–7) but slightly greater axial growth in older children and adolescents (ages 10–17) compared to the 2012_13 cohort–a trend similarly observed at the 25th and 75th percentiles. In both cohorts, median (50th percentile) annual axial growth was ≥ 0.40 mm at ages 3–5, ≥ 0.30 mm at ages 6–8, ≥ 0.20 mm at ages 9–10, ≥ 0.10 mm at ages 11–13, and < 0.10 mm at ages 14–17 (Table 4).
The baseline characteristics of the two cohorts stratified by age group are presented in Supplementary eTable 2. Patients aged 8–12 years in the 2012_13 cohort were significantly more myopic and had significantly longer AL and follow-up duration than those with similar age range in the 2018_19 cohort (all P < .05). The 2012_13 cohort also had a significantly more myopic SER in the 3–7 age group (P = .007).
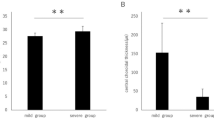
Annualized axial elongation and myopia progression according to age group and sex are shown in Table 5; Fig. 3. Within each cohort, annualized axial growth was significantly different among the three age groups (Kruskal–Wallis test, P < .001). Patients aged 3–7 years had the fastest AL change (median [IQR]: 0.42 [0.30, 0.55] and 0.41 [0.30, 0.55] mm/year), followed by age groups 8–12 years (median [IQR]: 0.20 [0.11, 0.30] and 0.19 [0.11, 0.31] mm/year) and 13–17 years (median [IQR]: 0.08 [0.03, 0.14] and 0.10 [0.05, 0.13] mm/year) for the respective cohorts (Table 5).
In the 2012_13 cohort, the model-adjusted axial elongation was 0.45 (0.03) mm/year in the 3–7 age group, 0.22 (0.01) mm/year in the 8–12 age group, and 0.09 (0.01) mm/year in the 13–17 age group. Similarly, in the 2018_19 cohort, it was 0.43 (0.02), 0.21 (0.01), and 0.12 (0.02) mm/year, respectively (Table 5). Power analysis indicated that the achieved power for age subgroup comparisons exceeded 95% in the 2012_13 cohort and 90% in the 2018_19 cohort. The GEE model showed no significant group × age group interaction effect (P = .480), indicating that annualized axial elongation did not differ significantly between cohorts across age groups. A similar trend in axial growth was observed in both sexes, with no significant group × age group × gender interaction effect (P = .792), suggesting that annualized axial elongation was comparable between male and female participants across all age groups in both cohorts (Fig. 3).
In the 2018_19 cohort, 34 patients switched to DIMS spectacles after wearing SV spectacles for at least 12 months because of fast myopia progression and axial elongation. Due to the small sample size, their results are presented in the Supplementary Information (eTables 3–5, eMethods, eResults, and eDiscussion).
Discussion
This retrospective study is among the first to present axial elongation patterns in myopic children and adolescents in Hong Kong, based on data from a clinical setting. An annual axial growth of 0.27 mm and 0.26 mm was found in the 2012_13 and 2018_19 cohorts, respectively, comprising individuals aged 3–17 years who wore SV spectacles. This aligns closely with recent studies showing a consistent annual elongation of 0.29 mm in Hong Kong children before the COVID-19 pandemic16,17. Additionally, our axial elongation rate was comparable to that of 0.25 mm/year observed in Chinese children with non-progressive myopia18. By contrast, a European study found in individuals with accelerated eye growth an annual axial elongation of 0.30 mm but in those with more consistent eye growth an elongation of 0.13 mm19. Hence, our finding of 0.26–0.27 mm/year axial elongation may be classified as non-progressive compared to the Chinese study but as progressive compared to the European study. This suggests a distinct eye growth pattern between Asians and Caucasians, potentially attributable to the higher prevalence of myopia in Asia (60%) than in Europe (40%)20.
The estimated annual axial elongation in the 2012_13 cohort was 0.45 mm for ages 3–7, 0.22 mm for ages 8–12, and 0.09 mm for ages 13–17. In the 2018_19 cohort, the corresponding values were 0.43, 0.21 and 0.12 mm, respectively. Compared with other studies, Chen et al.21 reported a mean axial elongation of 0.80 mm over three years (0.27 mm/year) in Singaporean children aged 3–6 years. Truckenbrod et al.22 documented a 0.30 mm annual axial growth in 3-year-old German children. The notably higher axial elongation found in our younger age group might be attributed to a greater proportion of progressive myopes in our sample. Using predictive models from the Orinda Longitudinal Study of Myopia (OLSM)23 in the United States and the Singapore Cohort Study of the Risk Factors for Myopia (SCORM)24, Chamberlain et al.12 estimated age-specific axial elongation in myopes. Their virtual cohorts aged 8–12 years exhibited annual axial elongation of 0.25 mm (OLSM) and 0.26 mm (SCORM), slightly higher than our findings for the same age group. This discrepancy may be attributed to the preference of university clinic optometrists in prescribing myopia control interventions to children in this age group, thus leaving those with relatively slower or stable myopia progression to wear SV spectacles. Consistent with our findings, previous studies reported an annual axial growth of approximately 0.10 mm in teenagers aged 13 years and older22,25,26.
Age at baseline was the most significant factor influencing axial elongation, regardless of sex. Both our raw data and model-based estimations consistently show that younger children experience the fastest axial growth, which progressively slows with age. Each year of increase in baseline age results in a decrease in annualized AL change by 0.04 mm (Table 3), a trend also reflected in our quantile regression model-estimated age-specific annual axial growth across different percentiles (Table 4). At the 50th percentile, the estimated annual axial elongation was 0.50 mm at age 3, gradually decreasing to − 0.07 mm at age 17 in the 2012_13 cohort, and 0.47 mm at age 3, decreasing to − 0.02 mm at age 17 in the 2018_19 cohort. A recent retrospective analysis of eight longitudinal studies in China reported that each additional year of baseline age was associated with a decrease in annualised axial elongation by approximately 0.05 to 0.06 mm. Their estimated axial growth rates for myopes range from 0.58 mm/year at age 6 to 0.36 mm/year at age 10, and further reduce to 0.09 mm/year at age 1627. However, these estimates were notably higher than ours, possibly due to the inclusion of six RCTs among the eight studies, in which the authors themselves reported a difference of 0.02 mm in axial growth estimates when study design (RCT vs. population-based study) was factored into their GEE model. These differences suggest that, despite all our study samples being of Chinese ethnicity, population or regional variations may also contribute to differences in axial growth rates among myopic children and adolescents. This underscores the importance of our study in capturing the axial growth patterns in Hong Kong.
In recent years, axial elongation data from control groups in myopia control trials have emerged as a potential source of reference growth data28. When comparing our findings with those of age-matched control groups wearing SV spectacles in RCTs15,29,30,31,32,33,34, the annualized axial elongation of these control groups was generally greater than ours by at least 30%. Similarly, a meta-analysis incorporating data from control groups across more than 40 RCTs estimated that the annual axial elongation among Asian children aged 8–12 years ranged from approximately 0.50–0.25 mm and decreased to approximately 0.22–0.11 mm at 13–17 years13. These values are also much higher than those estimated in our study, which may be attributed to the potential bias inherent in clinical trials, where participants are often recruited based on specific and stringent criteria. RCTs are an established method to accurately assess the true effect of an intervention35. However, given the increasing availability of proven myopia control interventions, the inclusion of untreated control groups in future myopia studies may raise ethical concerns36. A high dropout rate may also occur when participants are not assigned to a treatment37 One solution proposed by Bullimore et al.37 is to adopt a virtual control group. In the three-year DIMS follow-up study, Lam et al.38 incorporated a group of historical SV spectacle lens wearers to serve as a comparison for their treatment group. Nonetheless, the sample size for their historical control group was limited. Hence, our findings may serve as reference data for virtual control groups in future myopia control trials.
Our study found no significant differences in the axial elongation between sexes. This finding aligns with that of a previous study on emmetropes, concluding that sex is not a predictive factor for AL changes during normal eye development39. The Correction of Myopia Evaluation Trial (COMET)26 study and Li et al.40 also documented a similar axial growth rate between boys and girls. Additionally, there is evidence that no gender differences were found in axial elongation and myopia progression in Hong Kong children41. By contrast, several studies suggested that annual axial elongation is notably faster in girls27,42,43. Chen et al.18 reported that axial elongation is not influenced by sex in non-progressive myopes but is significantly faster in female progressive myopes. Therefore, the effect of sex on axial elongation remains controversial. Future research with larger sample sizes and more comprehensive data, including puberty-related factors such as height and weight, may provide further insights into this issue.
The estimated myopia increase in our two cohorts was − 0.47 and − 0.41 D/year. Donovan et al.44 compiled myopia progression data from 20 RCTs using cycloplegic autorefraction and found that Asian children exhibited a myopia progression of − 0.82 D/year. The large difference from our findings may be attributed to recruitment bias in myopia control trials. Moore et al.28 reported myopia progression rates of − 0.67 and − 0.18 D/year at ages 7 and 17 years in a clinical setting in Ireland. This deviation from our results might be due to the lack of cycloplegic refraction data in younger participants. In our study, approximately 35% of all patients underwent cycloplegic refraction during their first visit, primarily younger children. Noncycloplegic refraction tends to overestimate myopia and underestimate hyperopia compared with cycloplegic refraction, with more pronounced differences in younger children45. However, given the retrospective nature of our study conducted in a clinical setting, cycloplegic refraction data were not available for all participants at all follow-up visits. Consequently, this study focused on axial elongation rather than myopia progression. In a survey of UK-based optometrists, 34% agreed with performing cycloplegic refractions in children aged 2–4 years on their first visit but only 25% agreed with it in children aged 5–7 years. For this age group, 9.6% of optometrists supported cycloplegic refractions at each subsequent visit46.
Despite the proven efficacy of myopia control spectacles lenses and contact lenses in reducing myopic axial elongation throughout childhood47, eye care practitioners across the globe still frequently prescribe SV spectacles to young myopes48. This discrepancy in practice may be attributed to the varying levels of awareness regarding available myopia control options among practitioners and parents across countries and regions48. Overall, our 2012_13 and 2018_19 cohorts demonstrated similar rates of annualized axial elongation and myopia progression, indicating that the patterns of axial growth and myopia progression among myopic children and adolescents wearing SV spectacles did not significantly change before and after the introduction of DIMS spectacles into clinical practice. This could be due to the high level of awareness and education among university clinic optometrists in managing myopia progression, even when limited myopia control interventions were available. The stable and consistent axial growth patterns observed over the past 10 years suggest that our cohorts could serve as a valuable reference for future clinical trials.
Given the rapid axial elongation observed in younger children in our cohort, practitioners must exercise greater caution when prescribing SV spectacles to young children. More frequent follow-up visits (at least every 6 months) should be scheduled for children wearing SV spectacles49, and myopia control strategies should be promptly implemented upon detecting a rapid or abnormal increase in axial elongation. Educating parents about the importance of increasing outdoor time50, while reducing screen time and near work51 for their children, is also crucial.
The strength of our study lies in the use of axial elongation data derived from electronic clinical records in an optometry practice, offering a better representation of axial elongation patterns in routine clinical settings. Based on reported axial elongation rates of 0.37 ± 0.16 mm before 201252 and 0.29 ± 0.18 mm after 201917 for Hong Kong children, we sought to achieve 90% power to detect a 0.08 mm difference in axial elongation (SD = 0.17 mm) between two cohorts at a significance level of 0.05 (two-tailed). Using G*Power analysis, the final achieved power in our study was up to 98%, given the inclusion of 330 participants in the 2012_13 cohort and 165 participants in the 2018_19 cohort. This indicates that our sample size was more than adequate to draw robust conclusions regarding the comparison of axial elongation trends between the two cohorts. Our study also provided comprehensive estimates of axial elongation across different age groups, serving as a useful reference for future myopia control trials assessing treatment efficacy.
Nevertheless, this study has several limitations. First, the study sample was obtained solely from an optometry clinic on a university campus, which may not fully reflect the general population of Hong Kong. Additionally, the axial elongation rate may have been underestimated due to university clinic optometrists’ preference for prescribing myopia control treatments rather than SV spectacles to children, potentially introducing selection bias. Future research should include a more diverse sample from various clinical settings in Hong Kong to improve the generalizability of the findings. Second, we only included individuals who presented to the clinic for new prescriptions of SV spectacles, whereas those without correction or those who did not renew their prescriptions during the study period were excluded from analyses. Individuals with stable or no myopia progression were less likely to renew their prescriptions53. Third, due to the retrospective nature of this study, we were unable to assess the participants’ compliance with wearing the SV spectacles. Fourth, the retrospective design raises concerns about the lack of measurement standardization, the lack of consistent cycloplegic refraction data across all patients, and lack of information on parental myopia, age of myopia onset and time spent on near work and outdoor activities, all of which may be significant factors influencing axial growth and myopia progression patterns54. While future prospective studies with stricter control over these factors would provide a more robust benchmark, conducting such studies has become increasingly challenging, as more children are now managed with myopia control interventions rather than wearing SV spectacles alone. This is particularly difficult in East Asia, where myopia prevalence is high and myopia control measures are widely adopted. Fifth, the inclusion of two study cohorts separated by several years may introduce variability due to changes in lifestyle or environmental factors over time, such as increased screen time and changes in educational demands. Additionally, our 2018_19 cohort was affected by the COVID-19 pandemic, in which their annual follow-up visits were reduced or postponed, thus potentially introducing variability into our estimates of axial elongation17,55. Lastly, this study provides axial elongation data only for myopic children and adolescents, with a significant number of non-myopic patients (baseline SER > − 0.50D) excluded from both cohorts. Comparing axial elongation patterns between myopic and non-myopic children and adolescents could be an important avenue for future research.
Conclusions
The use of SV spectacle lenses, as prescribed by optometrists in a clinical setting, resulted in an average axial elongation of 0.26–0.27 mm/year in children and adolescents. Our findings may serve as a reference for future myopia control trials to evaluate treatment efficacy. Regular follow-up visits with young children wearing SV spectacles are essential to identify rapid axial elongation, thereby facilitating the timely implementation of myopia control management.
Methods
Study design and population
In this retrospective study, data were collected from a clinical setting where patients typically visited for routine eye examinations. Electronic clinical records of patients prescribed SV spectacles between July 1, 2012, and August 31, 2013 (the 2012_13 cohort) and July 1, 2018, and August 31, 2019 (the 2018_19 cohort) at the Optometry Clinic of The Hong Kong Polytechnic University were reviewed. These two cohorts were included to facilitate a comparison of axial elongation before and after the availability of a proven myopia control spectacle lens. Specifically, the 2018_19 cohort covered the period after defocus incorporated multiple segments (DIMS) spectacle lenses were proven effective to reduce myopia progression in a two-year RCT15, whereas the 2012_13 cohort was a randomly chosen earlier cohort to match the total number of clinical records in the 2018_19 cohort. The last follow-up date was September 30, 2016, for the 2012_13 cohort and September 30, 2022, for the 2018_19 cohort, with a maximum follow-up period of 51 months. This duration covered summer breaks over four consecutive years, during which schoolchildren and teenagers usually have their spectacles updated before starting a new academic year. All participants had previously provided informed consent during their routine visits to the university optometry clinic, where they were informed that their clinical data might be used for teaching and research purposes. This study conformed to the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board of The Hong Kong Polytechnic University (HSEARS20210612001).
Data including age, sex, visit dates, spectacles prescription dates, refractive error (sphere, cylinder, and axis), and AL were extracted from clinical records (all data were extracted between October 2022 and September 2023). Refractive errors were assessed by multiple registered optometrists using subjective refraction, with or without cycloplegia. The endpoint of subjective refractive was determined using the Maximum Plus to Maximum Visual Acuity (MPMVA) principle56. Based on the subjective refraction data, spectacle correction was prescribed to all participants. According to the general practice of the Optometry Clinic, cycloplegic refraction was performed at the discretion of the optometrists, though it is generally encouraged for children presenting to the clinic for the first time. AL was measured using either the IOLMaster (Carl Zeiss Meditec AG) or ALScan (Nidek Co., Ltd.). The first visit of the study period during which SV spectacle lenses were prescribed was regarded as the baseline visit.
The inclusion criteria were Chinese individuals aged 3–17 years with a minimum of two visits separated by at least 12 months. The exclusion criteria were as follows: (1) missing required data, (2) baseline spherical equivalent refractive error, (SER; sphere plus one half of cylinder power) >–0.50 D, (3) anisometropia > 2.00D at baseline, (4) presence of any ocular diseases that might affect refractive development, (5) presence of tropia or decompensated phoria, (6) history of ocular trauma or ocular surgery, and (7) previous or current use of any myopia control interventions.
Statistical analysis
The primary outcome was axial elongation. Axial elongation was defined as the difference in AL between baseline and final visits, normalized for the follow-up duration, and expressed as the annualized AL change for each patient. Myopia progression, the secondary outcome, was calculated as the SER difference between baseline and final visits. It was similarly normalized and expressed as the annualized SER change.
Data was assessed for normality using the Kolmogorov–Smirnov test. Unless otherwise specified, data are presented as the median and interquartile range (IQR). Baseline characteristics of the right and left eyes are provided in Supplementary eTable 1. The correlation between right and left eyes was examined using Pearson correlation for AL and Spearman’s rank correlation for SER. AL and SER were highly correlated between both eyes at baseline in the 2012_13 cohort (AL: r = .966, P < .001; SER: rs = 0.888, P < .001) and the 2018_19 cohort (AL: r = .964, P < .001; SER: rs = 0.809, P < .001). Therefore, only data from the right eyes were analyzed and presented.
To compare the baseline characteristics of SV spectacle wearers between the two cohorts, the Mann–Whitney U test or unpaired t-test was used for continuous variables, whereas Pearson’s χ2 test was used for categorical variables. The annualized AL and SER changes were compared between the two cohorts using the Mann–Whitney U test.
To account for the effects of age and emmetropization on axial growth and refractive error development, particularly in children57, quantile regression models were adopted to predict age-specific annualized axial elongation and myopia progression at different percentiles (5th, 25th, 50th, 75th, and 95th ). For better comparability with myopia control treatment groups in RCTs, patients were also categorized into three age groups of 5-year intervals (3–7, 8–12, and 13–17 years). The annualized axial elongation and myopia progression across these age groups were analyzed using the Kruskal–Wallis test with Bonferroni post-hoc correction.
A generalized estimating equations (GEE) model with robust standard error (SE) was used to estimate the annualized AL and SER changes while adjusting for covariates. These covariates included demographic and baseline characteristics such as age, sex, SER, AL and follow-up duration. The significance level was set at P < .05. Statistical analyses were conducted using SPSS (version 29.0, IBM).
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonablerequest.
References
Agyekum, S. et al. Cost-Effectiveness analysis of myopia progression interventions in children. JAMA Netw. Open. 6(11), e2340986–e2340986 (2023).
Holden, B. A. et al. Global prevalence of myopia and high myopia and Temporal trends from 2000 through 2050. Ophthalmology 123(5), 1036–1042 (2016).
Ding, B. Y. et al. Myopia among schoolchildren in East Asia and Singapore. Surv. Ophthalmol. 62(5), 677–697 (2017).
Sankaridurg, P. et al. IMI impact of myopia. Investig. Ophthalmol. Vis. Sci. 62(5), 2–2 (2021).
Vitale, S., Sperduto, R. D. & Ferris, F. L. Increased prevalence of myopia in the United States between 1971–1972 and 1999–2004. Arch. Ophthalmol. 127(12), 632-9 (2009).
Williams, K. M. et al. Increasing prevalence of myopia in Europe and the impact of education. Ophthalmology 122(7), 1489–1497 (2015).
Flitcroft, D. I. et al. IMI—defining and classifying myopia: A proposed set of standards for clinical and epidemiologic studies. Investig. Ophthalmol. Vis. Sci. 60(3), M20–M30 (2019).
Iribarren, R. Crystalline lens and refractive development. Prog Retin Eye Res. 47, 86–106 (2015).
Wolffsohn, J. S. et al. IMI—clinical myopia control trials and instrumentation report. Investig. Ophthalmol. Vis. Sci. 60(3), M132–M160 (2019).
Tideman, J. W. et al. Association of axial length with risk of uncorrectable visual impairment for Europeans with myopia. JAMA Ophthalmol. 134(12), 1355–1363 (2016).
Haarman, A. E. G. et al. The complications of myopia: A review and meta-analysis. Investig. Ophthalmol. Vis. Sci. 61(4), 49–49 (2020).
Chamberlain, P. et al. Axial length targets for myopia control. Ophthalmic Physiol. Opt. 41(3), 523–531 (2021).
Shamp, W. et al. Influence of age and race on axial elongation in myopic children. Investig. Ophthalmol. Vis. Sci. 63(7), 257 (2022).
Kostis, J. B. & Dobrzynski, J. M. Limitations of randomized clinical trials. Am. J. Cardiol. 129, 109–115 (2020).
Lam, C. S. Y. et al. Defocus incorporated multiple segments (DIMS) spectacle lenses slow myopia progression: A 2-year randomised clinical trial. Br. J. Ophthalmol. 104(3), 363–368 (2020).
Zhang, X. et al. Myopia incidence and lifestyle changes among school children during the COVID-19 pandemic: A population-based prospective study. Br. J. Ophthalmol. 106(12), 1772–1778 (2022).
Choi, K. Y. et al. Evaluation of an optical defocus treatment for myopia progression among schoolchildren during the COVID-19 pandemic. JAMA Netw. Open. 5(1), e2143781 (2022).
Chen, J. et al. Axial length changes in progressive and non-progressive myopic children in China. Graefes Arch. Clin. Exp. Ophthalmol. 261(5), 1493–1501 (2023).
McCullough, S. et al. Axial growth and refractive change in white European children and young adults: predictive factors for myopia. Sci. Rep. 10(1), 15189 (2020).
Grzybowski, A. et al. A review on the epidemiology of myopia in school children worldwide. BMC Ophthalmol. 20(1), 27 (2020).
Chen, D. Z. et al. Axial length elongation profiles from 3 to 6 years in an Asian paediatric population: the growing up in Singapore towards healthy outcomes birth cohort study (GUSTO). Br. J. Ophthalmol. (2023).
Truckenbrod, C. et al. Longitudinal analysis of axial length growth in a German cohort of healthy children and adolescents. Ophthalmic Physiol. Opt. 41(3), 532–540 (2021).
Jones, L. A. et al. Comparison of ocular component growth curves among refractive error groups in children. Investig. Ophthalmol. Vis. Sci. 46(7), 2317–2327 (2005).
Wong, H. B. et al. Ocular component growth curves among Singaporean children with different refractive error status. Investig. Ophthalmol. Vis. Sci. 51(3), 1341–1347 (2010).
Birte, G. et al. Age-matched analysis of axial length growth in myopic children wearing defocus incorporated multiple segments spectacle lenses. Br. J. Ophthalmol. bjo-2023-324508 (2023).
Hou, W. et al. Axial elongation in myopic children and its association with myopia progression in the correction of myopia evaluation trial. Eye Contact Lens 44(4), 248–259 (2018).
Naduvilath, T. et al. Normative data for axial elongation in Asian children. Ophthalmic Physiol. Opt. 43(5), 1160–1168 (2023).
Moore, M. et al. Myopia progression patterns among paediatric patients in a clinical setting. Ophthalmic Physiol. Opt. 44(2), 258–269 (2024).
Bao, J. et al. Spectacle lenses with aspherical lenslets for myopia control vs Single-Vision spectacle lenses: A randomized clinical trial. JAMA Ophthalmol. 140(5), 472–478 (2022).
Chen, H. et al. Low-intensity red-light therapy in slowing myopic progression and the rebound effect after its cessation in Chinese children: A randomized controlled trial. Graefes Arch. Clin. Exp. Ophthalmol. 261(2), 575–584 (2023).
Kanda, H. et al. Effect of spectacle lenses designed to reduce relative peripheral hyperopia on myopia progression in Japanese children: a 2-year multicenter randomized controlled trial. Jpn J. Ophthalmol. 62 (5), 537–543 (2018).
Liu, X. et al. One-year myopia control efficacy of cylindrical annular refractive element spectacle lenses. Acta Ophthalmol. 101(6), 651–657 (2023).
Rappon, J. et al. Control of myopia using diffusion optics spectacle lenses: 12-month results of a randomised controlled, efficacy and safety study (CYPRESS). Br. J. Ophthalmol. (2022).
Xiong, R. et al. Sustained and rebound effect of repeated low-level red-light therapy on myopia control: A 2-year post-trial follow-up study. Clin. Exp. Ophthalmol. 50(9), 1013–1024 (2022).
Bothwell, L. E. & Podolsky, S. H. The emergence of the randomized, controlled trial. N Engl. J. Med. 375(6), 501–504 (2016).
Jong, M. et al. IMI 2021 yearly digest. Investig. Ophthalmol. Vis. Sci. 62(5), 7–7 (2021).
Bullimore, M. A., Brennan, N. A. & Flitcroft, D. I. The future of clinical trials of myopia control. Ophthalmic Physiol. Opt. 43(3), 525–533 (2023).
Lam, C. S. et al. Myopia control effect of defocus incorporated multiple segments (DIMS) spectacle lens in Chinese children: Results of a 3-year follow-up study. Br. J. Ophthalmol. 106(8), 1110–1114 (2022).
Fledelius, H. C., Christensen, A. S. & Fledelius, C. Juvenile eye growth, when completed? An evaluation based on IOL-Master axial length data, cross-sectional and longitudinal. Acta Ophthalmol. 92(3), 259–264 (2014).
Li, T., Jiang, B. & Zhou, X. Axial length elongation in primary school-age children: A 3-year cohort study in Shanghai. BMJ Open. 9(10), e029896 (2019).
Lam, C. S. et al. A 2-year longitudinal study of myopia progression and optical component changes among Hong Kong schoolchildren. Optom. Vis. Sci. 76(6), 370–380 (1999).
Du, R. et al. Continued increase of axial length and its risk factors in adults with high myopia. JAMA Ophthalmol. 139(10), 1096–1103 (2021).
Saw, S. M. et al. Eye growth changes in myopic children in Singapore. Br. J. Ophthalmol. 89(11), 1489–1494 (2005).
Donovan, L. et al. Myopia progression rates in urban children wearing single-vision spectacles. Optom. Vis. Sci. 89(1), 27–32 (2012).
Zhu, D. et al. Pre- and postcycloplegic refractions in children and adolescents. PLOS ONE. 11(12), e0167628 (2016).
Doyle, L. A., McCullough, S. J. & Saunders, K. J. Cycloplegia and spectacle prescribing in children: attitudes of UK optometrists. Ophthalmic Physiol. Opt. 39(3), 148–161 (2019).
Sarkar, S., Khuu, S. & Kang, P. A systematic review and meta-analysis of the efficacy of different optical interventions on the control of myopia in children. Acta Ophthalmol. 102(3), e229–e244 (2024).
Wolffsohn, J. S. et al. IMI—global trends in myopia management attitudes and strategies in clinical practice—2022 update. Investig. Ophthalmol. Vis. Sci. 64(6), 6–6 (2023).
Verkicharla, P. K. et al. The IMPACT myopia management guidelines. Indian J. Ophthalmol. 71(7), 2882–2884 (2023).
He, X. et al. Time outdoors in reducing myopia: A School-Based cluster randomized trial with objective monitoring of outdoor time and light intensity. Ophthalmology 129(11), 1245–1254 (2022).
Enthoven, C. A. et al. The impact of computer use on myopia development in childhood: the generation R study. Prev. Med. 132, 105988 (2020).
Cho, P. & Cheung, S. W. Retardation of myopia in orthokeratology (ROMIO) study: A 2-year randomized clinical trial. Investig. Ophthalmol. Vis. Sci. 53(11), 7077–7085 (2012).
Alexandre, D. et al. Progression of myopia in teenagers and adults: A nationwide longitudinal study of a prevalent cohort. Br. J. Ophthalmol. 107(5), 644 (2023).
Jones, L. A. et al. Parental history of myopia, sports and outdoor activities, and future myopia. Invest. Ophthalmol. Vis. Sci. 48(8), 3524–3532 (2007).
Wang, J. et al. Evaluation and Follow-up of myopia prevalence among School-Aged children subsequent to the COVID-19 home confinement in Feicheng, China. JAMA Ophthalmol. 141(4), 333–340 (2023).
Kurtz, D. & Carlson, N. B. Refraction. in Clinical Procedures for Ocular Examination 111–205 (McGraw Hill-Education, New York, 2003).
Wojciechowski, R. Nature and nurture: The complex genetics of myopia and refractive error. Clin. Genet. 79(4), 301–320 (2011).
Acknowledgements
The authors would like to thank the Belt and Road Scholarship under the HKSAR Government Scholarship Fund to support the postgraduate study of K.W.
Funding
PolyU Internal grant (1-BD90), Health and Medical Research Fund (10211476), and RCSV (1-BBC0).
Author information
Authors and Affiliations
Contributions
K.W., R.C. and A.L. conceptualized and designed the project. K.W. and A.L. collected, analyzed and interpreted the data. K.W. drafted the manuscript. K.W., R.C. and A.L. reviewed and edited the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wong, K.Y.Q., Chun, R.K.M. & Lam, A.K.C. Axial elongation among Hong Kong myopic children and adolescents wearing single vision spectacles from a clinical setting. Sci Rep 15, 15478 (2025). https://doi.org/10.1038/s41598-025-99954-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-99954-1