Abstract
Language features may reflect underlying cognitive and emotional processes following a traumatic event that portend clinical outcomes. The authors sought to determine whether language features from usual smartphone use were markers associated with concurrent posttraumatic symptoms and worsening or improving posttraumatic symptoms over time following a traumatic exposure. This investigation was a secondary analysis of the Advancing Understanding of RecOvery afteR traumA study, a longitudinal study of traumatic outcomes among survivors recruited from 33 emergency departments across the United States. Adverse posttraumatic sequelae were assessed over the six months following the initial traumatic exposure. Language features were extracted from usual smartphone use in a specialized app. Bivariate linear mixed models were used to identify and validate language features that are markers associated with posttraumatic symptoms. Participants were 1744 trauma survivors, with a mean age of 39 [SD = 13] years old, and 56% were female. Fourteen language features were associated with severity level of posttraumatic symptoms at specific timepoints (cross-sectional markers) and five features were associated with change in severity level of posttraumatic symptoms (longitudinal markers). References to the body and health or illness were predictive of worsening pain, somatic, and thinking/concentration/fatigue symptom severity over time. An increase in references to others was associated with improvement in somatic symptom severity over time and increases in expressions of causation or cognitive processes were associated with improvement in pain symptom severity over time. Language features derived from usual smartphone use can convey important information about health, functioning, and recovery following a traumatic event. Clinicians might utilize such information to determine who may experience a high symptom burden or risk of worsening posttraumatic symptoms.
Lay Summary
Via usual smartphone use following trauma exposure, this study identified language markers associated with patient-reported severity and change in severity for multiple symptoms. Using language markers as a proxy for the status of and changes in specific symptoms supports efficient remote health status monitoring and can provide clinicians with valuable real-time insights into health, functioning, and recovery. These insights can be leveraged to guide targeted interventions tailored to individual trauma survivors.
Similar content being viewed by others
Introduction
Nearly 90% of US adults report exposure to at least one traumatic event during their lifetime [1], with many presenting to an emergency department (ED) for treatment after the experience. Although most are not hospitalized, they are at risk of developing adverse posttraumatic neuropsychiatric sequelae (APNS), including pain and other somatic symptoms, thinking/concentration/fatigue, depression, avoidance, re-experiencing, anxiety, hyperarousal, sleep disruption, and nightmares [2]. These posttraumatic symptoms are highly comorbid [3,4,5] and contribute to negative outcomes such as distress, functional impairment [6, 7], and reduced quality of life [8, 9]. However, physicians lack tools to determine which people are at risk for severe symptoms or might experience longer-lasting symptom burden, particularly as follow-up after an ED visit is often limited.
Computational linguistics has gained attention as an approach for understanding psychological aspects of human language. Combining techniques from linguistics, cognitive science, and artificial intelligence, computational linguistics facilitates automated processing and analysis of human language and is increasingly used to detect mental illness from text [10, 11]. To generate language features, word data are processed using validated models that estimate levels of psychological traits including personality [12], loneliness [13], politeness [14], depression [15], stress [16], emotion categories [17], and sentiment [18,19,20]. These language features may reflect underlying cognitive and emotional processes following a traumatic event that are important for clinical outcomes.
Prior work on language features after a traumatic experience centers on data gathered from either written and transcribed trauma narratives or other sources including non-trauma narratives or memories and social media posts. Previous research in the context of trauma narratives suggests that people diagnosed with posttraumatic stress disorder (PTSD) use higher rates of first-person singular pronouns [21], sensory words (e.g., sight, sound, taste) [22], and emotion words (e.g., anxiety, sadness) [23, 24]. Studies examining symptom severity related to trauma narratives find that lower rates of words expressing cognitive processes (e.g., thoughts, insights) [22, 25], words concerned with death and dying [26], and shorter narrative length [27, 28] predict poorer outcomes. However, a risk of participant distress is inherent in using trauma narratives as data [29].
Text generated through non-trauma narratives and memories or shared on social media offers a more naturalistic dataset than restricting text to trauma narratives. Prior research has shown that the results from studies with trauma narrative text are largely replicated in studies with social media text [30]. Fewer positive and more negative emotion words were associated with more severe avoidance and numbing symptoms [31, 32]. A PTSD diagnosis was associated with higher use of first-person singular pronouns and lower use of first-person plural pronouns [33, 34]. Findings on cognitive processing words are inconsistent [30]. Studies using non-trauma narratives and memories are less naturalistic but usually include well-characterized participants. Although more naturalistic, difficulties verifying diagnoses, symptoms, and demographics for social media users are a consideration in evaluating the outcomes of these studies. This study avoids the shortcomings of other data sources by using the words from usual smartphone use. Our approach avoids the potential distress associated with trauma narratives, provides more naturalistic text than non-trauma narratives, and ensures better characterized participants than social media text.
The vast majority of studies only include the umbrella PTSD diagnosis [21,22,23,24,25,26,27,28, 33, 34] or only a small number of more specific APNS symptom domains [31, 32]. As demonstrated in other examinations of language and co-occurring conditions [35], investigating PTSD without considering individual APNS symptoms domains misses the opportunity to disambiguate language features that are common to more than one APNS or specific to only one. This disambiguation allows better classification and informs transdiagnostic treatments as well as symptom-specific interventions. To understand links between smartphone language features and specific APNS symptom domains, this study examines associations between language features and scores for ten symptom domains.
Leveraging the near ubiquity of smartphones to advance current knowledge of the relationship between usual language and posttraumatic symptoms, we generated language features from smartphone word data and analyzed them against self-reported APNS symptoms from a diverse population of adults (n = 1744) presenting to an ED after traumatic stress exposure. We identified and internally validated language features as both cross-sectional, between-subjects markers (i.e., language characteristics that indicate high concurrent symptoms) and longitudinal, within-subjects markers (e.g., language characteristics that predict worsening or improving symptoms over time). Markers with cross-sectional between-subjects associations can help differentiate severity levels of APNS symptoms at a point in time. Those with longitudinal within-subjects associations can help differentiate worsening or improving APNS symptoms over time.
Materials and methods
Study overview and sample characteristics
This investigation was a secondary analysis of the AURORA (Advancing Understanding of RecOvery afteR traumA) study [2]. AURORA collected prospective genomic, neuroimaging, psychophysical, physiological, neurocognitive, digital phenotype, and self-report data from a diverse sample of trauma survivors who visited one of 33 EDs within 72 h of their trauma. The full methodology of the AURORA study is described in detail by McLean et al. [2] and was ethically approved by the Institutional Review Board (IRB #17-0703) at UNC Chapel Hill. Beginning in September 2017 AURORA recruited participants who were aged 18–65 years old, able to speak and read English, able to follow the protocol at the time of enrollment, physically able to use a smartphone, expected that they would have access to a smartphone for at least one year following study enrollment, and had possessed a smartphone for at least one year prior to study enrollment. We excluded patients if they had a solid organ injury Grade > I according to the American Association for the Surgery of Trauma Injury Scoring Scales [36], significant hemorrhage, needed a chest tube or surgery with anesthesia, or were likely be admitted for > 72 h. Qualifying traumatic events included motor vehicle collision, physical assault, sexual assault, falls > 10 feet, or mass casualty incidents. Although the aim of the AURORA study was to record data from 5000 individuals over five years, data are being analyzed periodically to report early results to the scientific community. This work analyzes data through July 2020 from 1744 participants who used Android smartphones. We did not include participants with Apple phones due to Apple’s privacy restrictions. All participants provided written informed consent after receiving a complete description of the study. By excluding trauma survivors with long bone fractures, laceration with significant hemorrhage, and solid organ injury, the AURORA study was designed to disentangle the potential influence of physiological effects related to general anesthesia, hemorrhage and medication on these APNS symptom development.
Survey data collection and APNS symptom score generation
The Mindstrong Discovery™ app was installed onto the participants’ Android smartphone during enrollment to prompt participants to complete brief “flash” surveys assessing APNS domains at 10 or 11 timepoints. This investigation used flash survey and word data collected in the first six months following enrollment and focuses on ten self-reported measures of psychological and physical symptoms associated with APNS: pain [37, 38], depression [39,40,41,42], sleep continuity [43], nightmares [44,45,46], somatic symptoms [37, 47], thinking/concentration/fatigue [48,49,50,51], avoidance, re-experiencing, anxiety [52, 53], and hyperarousal [54,55,56,57]. For each of the ten APNS symptom domains, flash survey items were selected by ___domain experts as indicator variables to develop joint measurement models across all timepoints based on confirmatory factor analysis. Flash survey items used to define the 10 symptoms and the days on which each was administered are provided in Appendix 1. The joint measurement model pooled data across all timepoints to estimate a consistent set of latent factors (symptom domains) where all flash survey items relevant to the APNS symptom ___domain were included as indicator variables. Factor scores for each symptom were computed for each participant for each timepoint as measures to define these 10 APNS symptom domains. These factor scores were then used to identify and validate language markers that are associated with specific APNS symptom domains either at a point in time (cross-sectional between-subjects trait markers) or over time (longitudinal within-subjects state markers).
Word data collection and language feature generation
The Mindstrong Discovery™ app continuously and passively collected all words entered on the smartphone via the native keyboard or a Mindstrong keyboard and recorded an unordered list of unique words and their frequencies each day. Reconstructing individual text messages, emails, or other text-based interactions from this list is impossible, ensuring participant privacy. These word data were de-identified and encrypted to further ensure confidentiality. As in other studies of language in the context of mental health [35], we then generated language-based estimates of psychological traits and lexicon-based characteristics of text. Validated language models of emotion calculated estimated levels of psychological traits such as personality [12], loneliness [13], politeness [14], depression [15], stress [16], emotion categories [17], and sentiment [18,19,20]. Language Inquiry and Word Count (LIWC) software [58] calculated lexical characteristics such as frequency of parts of speech, references to other people, and word count (see all characteristics in Appendix 3). All language features were normalized to introduce a common scale and ensure that higher scores indicate a higher level of the modeled attribute, and lower scores indicate a lower level of the attribute.
Language feature preprocessing, identification, internal validation, and evaluation
We preprocessed the normalized language features generated in the prior step by checking for extreme and abnormal values, missing and zero percentage of each language feature, as well as the correlation between each pair of features. Next, we identified subsets of language features that were highly correlated (Spearman correlations > 0.85) to reduce redundancy. For each subset, we retained the feature that showed the strongest univariate association with APNS symptom scores or was deemed conceptually most interpretable based on prior research. To minimize the inclusion of features with limited variability, we excluded language features with a zero percentage larger than 90%, set word counts larger than 10,000 to missing, and removed participants who switched smartphone operating system (ex. Android to Apple iOS) within the first six months. Word counts greater than 10,000 were set to missing to address potential outliers that could skew the results. Such extreme values likely reflect data collection artifacts or atypical user behavior, and their exclusion is intended to enhance the robustness of the analysis.
Because missing data is common for large-scale, longitudinal, naturalistic studies, it is critical to examine the missing mechanism of these missing values. We calculated the correlations of the APNS symptom scores with the completion rate of the four main study activities–survey, flash survey, neurocognitive tests, and watch wearing–to evaluate whether missing values were associated with symptom severity. Identifying these associations helps determine whether missingness in the data may be systematically related to participants’ clinical characteristics, which is critical for interpreting results and addressing potential biases in the analysis. All the correlations are weak (<0.1, Appendix 2), suggesting that missing data did not bias the main outcome associations. As a result, we considered these missing data as missing at random, and these missing values were handled by the bivariate linear mixed model using full information maximum likelihood estimation method.
For each flash survey timepoint for each participant, the mean of the language features from the day prior to and the day of APNS symptom data collection were merged with each of the 10 APNS symptom scores and used as candidate language markers for corresponding APNS symptom domains. We randomly divided the aggregated data into two equal parts and used one half for marker identification and the other half for internal validation. The internal validation step was applied to ensure that the markers were consistently associated with the symptoms. To identify and validate markers, we estimate and test the correlation between language features and each of the 10 symptom domains with repeated measures from each participant. To account for the correlation structure of the repeated measures, we used a bivariate linear mixed model approach [59, 60] to simultaneously model the cross-sectional and longitudinal associations of each language feature within each symptom ___domain. Using the first half of the data, language feature variables are identified as potential language markers if their associations (either cross-sectional or longitudinal) with any of the 10 APNS symptom domains are statistically significant (adjusted p-value < 0.05) after False Discovery Rate (FDR) multiple tests correction. These potential markers are then further validated using the same bivariate linear mixed model on the remaining 50% of the data, where markers retaining statistically significant associations (adjusted p-value < 0.05) after Bonferroni multiple tests correction are confirmed as markers for corresponding APNS symptom domains. For those longitudinal language markers passing both identification and validation steps, we evaluated for their accuracy in predicting change in the corresponding APNS symptom scores (e.g., worsening versus improvement). A simple cut-off was used to define worsening and improvement, such that worsening of symptom severity is defined as (severity score at six months minus severity score at one week) > 0, and improvement in symptom severity is defined as (severity score at six months minus severity score at one week) < 0. The predicted symptom score change was generated by applying the same cut-offs to the change of longitudinal markers over the same time window. The sensitivity, specificity, and positive and negative predictive value (PPV, NPV) of the change in marker value associated with the change in symptom score were then assessed. High PPV for worsening or high NPV for improvement would suggest that language markers derived from smartphone use may have utility as initial screening measures for adverse posttraumatic outcomes among trauma survivors.
Results
Sample sociodemographic, trauma exposure, and clinical characteristics
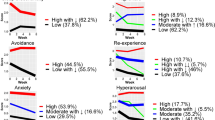
Demographic characteristics of the participants are presented in Table 1. Most of the participants were female (55.5%) with a mean age of 39.0 years old (SD 13.0). More than half were non-Hispanic Black (53.6%), followed by non-Hispanic White (31.7%), and Hispanic (10.9%). The majority did not have a college degree (84.4%). The traumatic exposure that conferred eligibility for the study was a motor vehicle collision for almost three-quarters of the sample (71.0%). Median symptom scores over the first 6 months after trauma exposure indicate that moderate symptoms (e.g., pain > = 4 on a scale of 0–10) were observed for much of the sample and symptom burden tended to improve over time (Fig. 1).
Language feature characteristics
All participants used Android smartphones for the duration of the study and typed a mean of 387.13 (SD = 1137.43) and a median of 143 words per day. Summary statistics for the language features are in Appendix 3, including examples of words associated with each language feature.
Cross-sectional language markers
We first identified and internally validated cross-sectional language markers that differentiated individuals experiencing different severities of specific APNS symptoms at any point in time. Fourteen language markers met internal validation criteria for seven APNS symptom domains with some markers associated with more than one symptom ___domain. The significant cross-sectional, between-subjects correlations between symptom severity scores and language markers are reported in Table 2. We internally validated four significant cross-sectional language markers for the severity of pain, nine for somatic symptoms, one for avoidance, three for hyperarousal, two for nightmares, two for depression, and one for anxiety. Higher levels of pain and somatic symptoms were associated with more frequent references to people (family, other people, males). Higher levels of pain were associated with less frequent expressions of tentativeness and more frequent expressions of happiness. Higher levels of somatic symptoms and hyperarousal were associated with more frequent expressions of loneliness and less frequent use of articles. Higher levels of somatic symptoms, nightmares, and avoidance were associated with more frequent use of first-person singular pronouns and higher levels of somatic symptoms and nightmares were associated with less frequent use of longer words (>6 letters). Higher levels of hyperarousal, depression, and anxiety were associated with more frequent expressions of negative emotion. Lastly, higher levels of somatic symptoms were associated with more frequent use of all personal pronouns and informal speech.
Longitudinal language markers
We next identified and internally validated longitudinal language markers whose changes are associated with changes in severity score (either worsening or improvement) of specific APNS symptom domains. Five language markers met internal validation criteria for three APNS symptom domains with some markers associated with more than one symptom ___domain. The statistically significant longitudinal, within-subjects correlations between change in APNS symptom scores and change in language markers are reported in Table 3. We internally validated four significant language longitudinal markers for change in severity of pain, two for somatic symptoms, and one for thinking/concentration/fatigue. Increases in pain, somatic symptoms, and problems with thinking/concentration/fatigue were associated with an increase in references to health or illness, while an increase in pain was also associated with an increase in references to the body. A decrease in pain was associated with an increase in references to causation and cognitive processes. Finally, a decrease in somatic symptoms was associated with an increase in references to other people.
Utility of predicting worsening and improvement using longitudinal language markers
We evaluated the potential utility of the longitudinal language markers for predicting worsening and improvement of symptoms from one week to six months post-trauma. Worsening pain severity was experienced by 24% of participants, worsening somatic symptom severity was experienced by 22% of participants, and worsening thinking/concentration/fatigue severity was experienced by 28% of participants. PPV was between 0.76 and 0.82 for all markers (see Table 4). Improvement in pain severity was experienced by 76% of participants, improvement in somatic symptom severity was experienced by 78% of participants, and improvement in thinking/concentration/fatigue severity was experienced by 72% of participants. In general, the prediction of improvement in severity was slightly less accurate for each marker than the prediction of worsening severity. NPV was between 0.68 and 0.78 for all markers (see Supplementary Table 1). Relatively high PPV for symptom worsening and High NPV for symptom improvement indicate that these longitudinal markers can predict symptom worsening better than improvement, based on this simple prediction model. However, no single marker achieved both high PPV and NPV in predicting the change of APNS symptom scores.
Discussion
Using language data collected from usual smartphone use, we derived and internally validated 14 cross-sectional and five longitudinal relationships between language features and APNS symptom severity during the first six months following a traumatic event – a high-risk period during which trauma survivors might experience either symptom recovery or persistence [2]. To our knowledge, this is the first study to examine such associations using word data from usual smartphone use. Of interest, pain and somatic symptoms exhibited several cross-sectional and longitudinal associations, suggesting that APNS symptom domains not traditionally considered part of a PTSD diagnosis may be uniquely associated with language features.
In particular, higher frequency of references to others (i.e., family, other people, males) was associated in the cross-sectional analysis with higher pain and somatic symptom scores and an increase in frequency in references to others was associated in the longitudinal analysis with a decrease in somatic symptom scores. The paradox of both higher frequency of references to others being associated with higher somatic symptom severity and increased frequency of references to others being associated with decreased symptom severity should be further investigated. In addition, higher frequency of expressions of loneliness was associated with higher hyperarousal scores. These results concerning references to others and expressions of loneliness support a link between social processes and health outcomes, as suggested by prior work [61], and the role of language should be investigated further. Also, in accordance with previous research, higher scores in the somatic, avoidance, and nightmare domains were associated with higher frequency of use of first-person singular pronouns [21, 22, 62]. This finding may suggest an understandable focus on the self in response to posttraumatic symptoms and may constitute a useful health status marker.
Similar to previous research findings [22, 26, 63,64,65], more frequent use of indicators of language complexity such as words containing over six letters, articles, and expressions of tentativeness were associated with lower cross-sectional scores for pain, somatic, hyperarousal, and nightmare symptom domains. More frequents expressions of sadness, anger, and negative emotions were associated only with higher scores in the affective domains of hyperarousal and depression, and were consistent with prior research suggesting that those with PTSD tend to express more sadness and less happiness [66]. However, in our sample, more frequent expressions of happiness were associated with higher scores in the pain symptoms ___domain, supporting the notion that APNS symptom domains may have unique or overlapping language marker profiles and necessitating further investigation.
We found that worsening pain, somatic, and thinking/concentration/fatigue APNS symptom ___domain scores were associated with more frequent references to the body and health or illness. As with the use of first-person singular pronouns, this usage increase may indicate an understandable increase in focus on concerning APNS symptoms, but prior research has not evaluated language use associations with these specific domains so further work is needed.
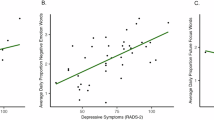
The stronger correlations observed in Table 2 (cross-sectional associations) compared to Table 3 (longitudinal associations) likely reflect the immediate relationship between smartphone usage metrics and contemporaneous survey responses. This suggests that smartphone behavior may be more tightly linked to psychological states or experiences at the moment rather than longitudinally over time.
Smartphones are a near ubiquitous vehicle for communication and internet access. The words we use during interactions mediated by smartphones can convey information about our health, including symptoms occurring after a traumatic experience. In the future, language markers may help clinicians identify individuals who are experiencing a high level of symptom burden or who are at risk for worsening symptoms and merit further evaluation for adverse outcomes. These same language markers might also be useful for monitoring response to treatments or therapeutic interventions.
Limitations
Several limitations are relevant when considering the results of this investigation. Our participants were enrolled in the ED, thus generalizability of findings to trauma survivors who do not present to the ED is not known. The majority of participants were survivors of motor vehicle collisions and the generalizability of results to other types of trauma is also not known. Although missing data were not correlated with the study outcome measures, other missingness patterns could not be accounted for in the analysis. We also used data only from Android phone users and their use patterns may vary from users of other smartphones. We acknowledge that administering flash surveys may have inadvertently primed participants, influencing their word usage or psychological responses. For example, completing a survey in the morning could subtly shape participants’ smartphone interactions later in the day. Furthermore, the daily administration of flash surveys, sometimes on consecutive days, could introduce overlap or carryover effects in word usage or psychological states. For instance, language metrics tied to one construct might inadvertently capture signals from related constructs measured on adjacent days. Future studies are needed to disentangle potential priming effect from natural variation in language usage and psychological symptoms and to adjust for temporal dependencies.
We also remind readers that this investigation is exploratory rather than being a confirmatory study testing theoretical hypotheses. Additionally, study assessments were limited to the six months following a traumatic event and only used language data. Future studies might investigate generalizability and should examine associations between APNS symptom domains and language features in conjunction with other passive data, such as keystroke and activity data, collected over longer durations and including sex-related differences. While our primary analyses did not specifically examine sex-related differences in smartphone word use, this is an important and relevant area for further analyses to assess whether sex might moderate the relationship between language usage and APNS symptoms after trauma exposure. Future studies could leverage symptom trajectory data to investigate whether patterns of smartphone language use vary based on longitudinal symptom trajectories. Finally, we want to note that when demonstrating the potential utility of predicting symptom changes (both worsening and improvement) using longitudinal language markers, we employed a very simple prediction model based solely on individual markers. Consequently, the overall prediction accuracy was not high. We anticipate that much better prediction accuracy can be achieved by using more advanced statistical and machine learning techniques, which would combine all the longitudinal markers along with baseline characteristics. We also recognize that the small degree of change defined by the cutoff of zero may not represent clinically meaningful shifts. This decision was made partly due to a lack of widely accepted cutoffs for these symptoms. However, these improvements are beyond the scope of the current study.
Conclusion
This investigation sought to establish the relationship between language features derived from usual smartphone use and the severity and change in posttraumatic symptoms. The use of smartphone interactions as the data source after a traumatic experience rather than trauma narratives is unique and avoids additional patient burden and possible distress. We identified fourteen language markers for cross-sectional severity of seven APNS symptom domains and five language markers for longitudinal changes in severity for three APNS symptom domains. These findings confirm that language markers derived from usual smartphone use convey important information about health, functioning, and recovery following a traumatic event. Patterns of language use could contribute to remote symptom monitoring during the post trauma period and clinicians might use such information to identify those at risk for high symptom burden or worsening posttraumatic symptoms. Future research includes investigating sex differences and novel associations.
Data used in this manuscript is available through the National Institute of Mental Health (NIMH) Data Archive (NDA). The NDA Collection for the AURORA Project can be found here: https://nda.nih.gov/edit_collection.html?id=2526.
References
Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, Friedman MJ. National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. J Trauma Stress. 2013;26:537–47. https://doi.org/10.1002/jts.21848.
McLean SA, Ressler K, Koenen KC, Neylan T, Germine L, Jovanovic T, et al. The AURORA Study: a longitudinal, multimodal library of brain biology and function after traumatic stress exposure. Mol Psychiatry. 2020;25:283–96. https://doi.org/10.1038/s41380-019-0581-3.
Kilpatrick DG, Ruggiero KJ, Acierno R, Saunders BE, Resnick HS, Best CL. Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: results from the national survey of adolescents. J Consult Clin Psychol. 2003;71:692–700. https://doi.org/10.1037/0022-006x.71.4.692.
Beck JG, Clapp JD. A different kind of co-morbidity: understanding posttraumatic stress disorder and chronic pain. Psychol Trauma. 2011;3:101–8. https://doi.org/10.1037/a0021263.
Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: a literature review. Arch Intern Med. 2003;163:2433–45. https://doi.org/10.1001/archinte.163.20.2433.
Momartin S, Silove D, Manicavasagar V, Steel Z. Comorbidity of PTSD and depression: associations with trauma exposure, symptom severity and functional impairment in Bosnian refugees resettled in Australia. J Affect Disord. 2004;80:231–8. https://doi.org/10.1016/S0165-0327(03)00131-9.
Dobie DJ, Kivlahan DR, Maynard C, Bush KR, Davis TM, Bradley KA. Posttraumatic stress disorder in female veterans: association with self-reported health problems and functional impairment. Arch Intern Med. 2004;164:394–400. https://doi.org/10.1001/archinte.164.4.394.
Clapp JD, Beck GJ, Palyo SA, Grant DM. An examination of the synergy of pain and PTSD on quality of life: additive or multiplicative effects? Pain. 2008;138:301–9. https://doi.org/10.1016/j.pain.2008.01.001.
Gormsen L, Rosenberg R, Bach FW, Jensen TS. Depression, anxiety, health-related quality of life and pain in patients with chronic fibromyalgia and neuropathic pain. Eur J Pain. 2010;14:127.e1–8. https://doi.org/10.1016/j.ejpain.2009.03.010.
Kern ML, Park G, Eichstaedt JC, Schwartz HA, Sap M, Smith LK, et al. Gaining insights from social media language: methodologies and challenges. Psychol Methods. 2016;21:507–25. https://doi.org/10.1037/met0000091.
Guntuku SC, Yaden DB, Kern ML, Ungar LH, Eichstaedt JC. Detecting depression and mental illness on social media: an integrative review. Curr Opin Behav Sci. 2017;18:43–49. https://doi.org/10.1016/j.cobeha.2017.07.005.
Park G, Schwartz HA, Eichstaedt JC, Kern ML, Kosinski M, Stillwell DJ, et al. Automatic personality assessment through social media language. J Pers Soc Psychol. 2015;108:934–52. https://doi.org/10.1037/pspp0000020.
Guntuku SC, Schneider R, Pelullo A, Young J, Wong V, Ungar L, et al. Studying expressions of loneliness in individuals using twitter: an observational study. BMJ Open. 2019;9:e030355. https://doi.org/10.1136/bmjopen-2019-030355.
Li M, Hickman L, Tay L, Ungar L, Guntuku SC. Studying politeness across cultures using english twitter and mandarin weibo. Proc ACM Hum-Comput Interact. 2020;4:119:1–119:15. https://doi.org/10.1145/3415190.
Schwartz HA, Eichstaedt J, Kern ML, Park G, Sap M, Stillwell D, et al. Towards assessing changes in degree of depression through facebook. In: 2014. https://doi.org/10.3115/v1/W14-3214.
Guntuku SC, Buffone A, Jaidka K, Eichstaedt JC, Ungar LH. Understanding and measuring psychological stress using social media. Proc Int AAAI Conf Weblogs Soc Media. 2019;13:214–25.
Mohammad SM, Kiritchenko S. Using hashtags to capture fine emotion categories from tweets. Comput Intell. 2015;31:301–26. https://doi.org/10.1111/coin.12024.
Dodds PS, Harris KD, Kloumann IM, Bliss CA, Danforth CM. Temporal patterns of happiness and information in a global social network: hedonometrics and twitter. PLoS ONE. 2011;6:e26752. https://doi.org/10.1371/journal.pone.0026752.
Mohammad SM, Turney PD. Crowdsourcing a word–emotion association lexicon. Comput Intell. 2013;29:436–65. https://doi.org/10.1111/j.1467-8640.2012.00460.x.
Preoţiuc-Pietro D, Schwartz HA, Park G, Eichstaedt J, Kern M, Ungar L, et al. Modelling valence and arousal in facebook posts. In: Proceedings of the 7th workshop on computational approaches to subjectivity, sentiment and social media analysis. Association for Computational Linguistics; 2016. 9–15. https://doi.org/10.18653/v1/W16-0404.
Kleim B, Horn AB, Kraehenmann R, Mehl MR, Ehlers A. Early linguistic markers of trauma-specific processing predict post-trauma adjustment. Front Psychiatry. 2018;9:645. https://doi.org/10.3389/fpsyt.2018.00645.
D’Andrea W, Chiu PH, Casas BR, Deldin P. Linguistic predictors of post-traumatic stress disorder symptoms following 11 september 2001. Appl Cogn Psychol. 2012;26:316–23. https://doi.org/10.1002/acp.1830.
Crespo M, Fernández-Lansac V. Memory and narrative of traumatic events: a literature review. Psychol Trauma. 2016;8:149–56. https://doi.org/10.1037/tra0000041.
Jaeger J, Lindblom KM, Parker-Guilbert K, Zoellner LA. Trauma narratives: it’s what you say, not how you say it. Psychol Trauma. 2014;6:473–81. https://doi.org/10.1037/a0035239.
Booker JA, Graci ME, Hudak LA, Jovanovic T, Rothbaum BO, Ressler KJ, et al. Narratives in the immediate aftermath of traumatic injury: markers of ongoing depressive and posttraumatic stress disorder symptoms. J Trauma Stress. 2018;31:273–85. https://doi.org/10.1002/jts.22271.
Alvarez‐Conrad J, Zoellner LA, Foa EB. Linguistic predictors of trauma pathology and physical health. Appl Cogn Psychol. 2001;15:S159–S170. https://doi.org/10.1002/acp.839.
Desrochers AB, Beaulieu-Prévost D, Desautels J, Békés V, Belleville G, Guay S, et al. Gender and changes in trauma narrative following CBT for PTSD. J Aggression Maltreat Trauma. 2016;25:974–90. https://doi.org/10.1080/10926771.2016.1231147.
Gray MJ, Lombardo TW. Complexity of trauma narratives as an index of fragmented memory in PTSD: A critical analysis. Appl Cogn Psychol. 2001;15:S171–S186. https://doi.org/10.1002/acp.840.
Legerski JP, Bunnell SL. The risks, benefits, and ethics of trauma-focused research participation. Ethics Behav. 2010;20:429–44. https://doi.org/10.1080/10508422.2010.521443.
Knoff AA, Vasterling JJ, Verfaellie M. Beyond trauma: a review of content and linguistic characteristics of nontrauma narratives in posttraumatic stress disorder. Eur J Psychotraumatol. 2024;15:2407733. https://doi.org/10.1080/20008066.2024.2407733.
Manne S. Language use and post-traumatic stress symptomatology in parents of pediatric cancer survivors. J Appl Soc Psychol. 2002;32:608–29. https://doi.org/10.1111/j.1559-1816.2002.tb00233.x.
Eid J, Johnsen BH, Saus ER. Trauma narratives and emotional processing. Scand J Psychol. 2005;46:503–10. https://doi.org/10.1111/j.1467-9450.2005.00482.x.
Todorov G, Mayilvahanan K, Cain C, Cunha C. Context- and subgroup-specific language changes in individuals who develop PTSD after trauma. Front Psychol. 2020;11:989. https://doi.org/10.3389/fpsyg.2020.00989.
Preotiuc-Pietro D, Eichstaedt J, Park GJ, Sap M, Smith LK, Tobolsky V, et al. The role of personality, age, and gender in tweeting about mental illness. In: Proceedings of the 2nd workshop on computational linguistics and clinical psychology: from linguistic signal to clinical reality. Association for Computational Linguistics; 2015. 21–30. https://doi.org/10.3115/v1/W15-1203.
Stade EC, Ungar L, Eichstaedt JC, Sherman G, Ruscio AM. Depression and anxiety have distinct and overlapping language patterns: Results from a clinical interview. J Psychopathol Clin Sci. 2023;132:972–83. https://doi.org/10.1037/abn0000850.
Injury Scoring Scale. The American association for the surgery of trauma. 2024. https://www.aast.org/resources-detail/injury-scoring-scale.
Moldofsky H, Rothman L, Kleinman R, Rhind SG, Richardson JD. Disturbed EEG sleep, paranoid cognition and somatic symptoms identify veterans with post-traumatic stress disorder. BJPsych Open. 2016;2:359–65. https://doi.org/10.1192/bjpo.bp.116.003483.
Ulirsch JC, Weaver MA, Bortsov AV, Soward AC, Swor RA, Peak DA, et al. No man is an Island: living in a disadvantaged neighborhood influences chronic pain development after motor vehicle collision, and this effect is moderated by common genetic variation influencing HPA axis function. Pain. 2014;155:2116–23. https://doi.org/10.1016/j.pain.2014.07.025.
Gold PW, Chrousos GP. Organization of the stress system and its dysregulation in melancholic and atypical depression: high vs low CRH/NE states. Mol Psychiatry. 2002;7:254–75. https://doi.org/10.1038/sj.mp.4001032.
Doerig N, Krieger T, Altenstein D, Schlumpf Y, Spinelli S, Späti J, et al. Amygdala response to self-critical stimuli and symptom improvement in psychotherapy for depression. Br J Psychiatry. 2016;208:175–81. https://doi.org/10.1192/bjp.bp.114.149971.
Gollan JK, Buchanan A, Connolly M, Hoxha D, Sankin L, Csernansky JG, et al. Differences in the neural correlates of affective responses in depressed and healthy women. Psychiatry Res. 2015;234:336–45. https://doi.org/10.1016/j.pscychresns.2015.10.006.
Liu CH, Ma X, Song LP, Fan J, Wang WD, Lv XY, et al. Abnormal spontaneous neural activity in the anterior insular and anterior cingulate cortices in anxious depression. Behav Brain Res. 2015;281:339–47. https://doi.org/10.1016/j.bbr.2014.11.047.
Koren D, Arnon I, Lavie P, Klein E. Sleep complaints as early predictors of posttraumatic stress disorder: a 1-year prospective study of injured survivors of motor vehicle accidents. Am J Psychiatry. 2002;159:855–7. https://doi.org/10.1176/appi.ajp.159.5.855.
Kobayashi I, Sledjeski EM, Spoonster E, Fallon WF, Delahanty DL. Effects of early nightmares on the development of sleep disturbances in motor vehicle accident victims. J Trauma Stress. 2008;21:548–55. https://doi.org/10.1002/jts.20368.
Bryant RA, Creamer M, O’Donnell M, Silove D, McFarlane AC. Sleep disturbance immediately prior to trauma predicts subsequent psychiatric disorder. Sleep. 2010;33:69–74. https://doi.org/10.1093/sleep/33.1.69.
van Liempt S, van Zuiden M, Westenberg H, Super A, Vermetten E. Impact of impaired sleep on the development of PTSD symptoms in combat veterans: a prospective longitudinal cohort study. Depress Anxiety. 2013;30:469–74. https://doi.org/10.1002/da.22054.
McAndrew LM, Lu SE, Phillips LA, Maestro K, Quigley KS. Mutual maintenance of PTSD and physical symptoms for Veterans returning from deployment. Eur J Psychotraumatol. 2019;10:1608717. https://doi.org/10.1080/20008198.2019.1608717.
Scott JC, Matt GE, Wrocklage KM, Crnich C, Jordan J, Southwick SM, et al. A quantitative meta-analysis of neurocognitive functioning in posttraumatic stress disorder. Psychol Bull. 2015;141:105–40. https://doi.org/10.1037/a0038039.
Christensen H, Griffiths K, Mackinnon A, Jacomb P. A quantitative review of cognitive deficits in depression and Alzheimer-type dementia. J Int Neuropsychol Soc. 1997;3:631–51.
Zakzanis KK, Leach L, Kaplan E. On the nature and pattern of neurocognitive function in major depressive disorder. Neuropsychiatry Neuropsychol Behav Neurol. 1998;11:111–9.
Henry J, Crawford JR. A meta-analytic review of verbal fluency deficits in depression. J Clin Exp Neuropsychol. 2005;27:78–101. https://doi.org/10.1080/138033990513654.
Boffa JW, Norr AM, Raines AM, Albanese BJ, Short NA, Schmidt NB. Anxiety sensitivity prospectively predicts posttraumatic stress symptoms following a campus shooting. Behav Ther. 2016;47:367–76. https://doi.org/10.1016/j.beth.2016.02.006.
Olatunji BO, Fan Q. Anxiety sensitivity and post-traumatic stress reactions: evidence for intrusions and physiological arousal as mediating and moderating mechanisms. J Anxiety Disord. 2015;34:76–85. https://doi.org/10.1016/j.janxdis.2015.06.002.
Pole N. The psychophysiology of posttraumatic stress disorder: a meta-analysis. Psychol Bull. 2007;133:725–46. https://doi.org/10.1037/0033-2909.133.5.725.
Jovanovic T, Sakoman AJ, Kozarić-Kovačić D, Meštrović AH, Duncan EJ, Davis M, et al. Acute stress disorder versus chronic posttraumatic stress disorder: inhibition of fear as a function of time since trauma. Depress Anxiety. 2013;30:217–24. https://doi.org/10.1002/da.21991.
Orr SP, Metzger LJ, Lasko NB, Macklin ML, Hu FB, Shalev AY, et al. Physiologic responses to sudden, loud tones in monozygotic twins discordant for combat exposure: association with posttraumatic stress disorder. Arch Gen Psychiatry. 2003;60:283–8. https://doi.org/10.1001/archpsyc.60.3.283.
Shalev AY, Peri T, Brandes D, Freedman S, Orr SP, Pitman RK. Auditory startle response in trauma survivors with posttraumatic stress disorder: a prospective study. Am J Psychiatry. 2000;157:255–61. https://doi.org/10.1176/appi.ajp.157.2.255.
Pennebaker J, Boyd R, Jordan K., Blackburn K. The development and psychometric properties of LIWC2015. Austin, TX: University of Texas at Austin; 2015.
Huang Q. PROC MIXED: calculate correlation coefficients in the presence of repeated measurements. In; 2019. https://www.semanticscholar.org/paper/PROC-MIXED-%3A-Calculate-Correlation-Coefficients-in-Huang/a0caa84c95e152ade51f398cb6b6555424989544.
Roy A. Estimating correlation coefficient between two variables with repeated observations using mixed effects model. Biom J. 2006;48:286–301. https://doi.org/10.1002/bimj.200510192.
Cohen S. Social relationships and health. Am Psychol. 2004;59:676–84. https://doi.org/10.1037/0003-066X.59.8.676.
Jennings AN, Soder HE, Wardle MC, Schmitz JM, Vujanovic AA. Objective analysis of language use in cognitive-behavioral therapy: associations with symptom change in adults with co-occurring substance use disorders and posttraumatic stress. Cogn Behav Ther. 2021;50:89–103. https://doi.org/10.1080/16506073.2020.1819865.
Jelinek L, Stockbauer C, Randjbar S, Kellner M, Ehring T, Moritz S. Characteristics and organization of the worst moment of trauma memories in posttraumatic stress disorder. Behav Res Ther. 2010;48:680–5. https://doi.org/10.1016/j.brat.2010.03.014.
Jones C, Harvey AG, Brewin CR. The organisation and content of trauma memories in survivors of road traffic accidents. Behav Res Ther. 2007;45:151–62. https://doi.org/10.1016/j.brat.2006.02.004.
Ayers S, Radoš SN, Balouch S. Narratives of traumatic birth: quality and changes over time. Psychol Trauma. 2015;7:234–42. https://doi.org/10.1037/a0039044.
Reece AG, Reagan AJ, Lix KLM, Dodds PS, Danforth CM, Langer EJ. Forecasting the onset and course of mental illness with Twitter data. Sci Rep. 2017;7:13006. https://doi.org/10.1038/s41598-017-12961-9.
Acknowledgements
The investigators wish to thank the trauma survivors participating in the AURORA Study. Their time and effort during a challenging period of their lives make our efforts to improve recovery for future trauma survivors possible. Verily Life Sciences and Mindstrong Health provided some of the hardware and software used to perform study assessments. The Many Brains Project provided software for neurocognitive assessments. Data and/or research tools used in the preparation of this manuscript were obtained from the National Institute of Mental Health (NIMH) Data Archive (NDA). NDA is a collaborative informatics system created by the National Institutes of Health to provide a national resource to support and accelerate research in mental health. Dataset identifier(s): [NIMH Data Archive Collection ID(s) or NIMH Data Archive Digital Object Identifier (DOI)]. This manuscript reflects the views of the authors and may not reflect the opinions or views of the NIH or of the Submitters submitting original data to NDA.
Funding
This project was supported by NIMH under U01MH110925, the US Army MRMC, One Mind, and The Mayday Fund. The content is solely responsibility of the authors and does not necessarily represent the official views of any of the funders.
Author information
Authors and Affiliations
Contributions
Conceptualization: Ideas, formulation or evolution of overarching research goals and aims: Samuel A. McLean, Ronald C. Kessler, Lisa Vizer, Xinming An. Methodology: Development or design of methodology, creation of models: Samuel A. McLean, Ronald C. Kessler, Lisa Vizer, Xinming An, Donglin Zeng, Lyle Ungar, Salvatore Giorgi. Software: Programming, software development, designing computer programs, implementation of the computer code and supporting algorithms, testing of existing code components: Lyle Ungar, Salvatore Giorgi. Validation: Verification, whether as a part of the activity or separate, of the overall replication/ reproducibility of results/experiments and other research outputs: Yinyao Ji, Lisa Vizer, Xinming An. Formal analysis: Application of statistical, mathematical, computational, or other formal techniques to analyze or synthesize study data: Yinyao Ji, Mochuan Liu, Zhaopeng Xing, Lisa Vizer, Xinming An. Investigation: Conducting a research and investigation process, specifically performing the experiments, or data/evidence collection: Stacey L. House, Francesca L. Beaudoin, Xinming An, Jennifer S. Stevens, Thomas C. Neylan, Gari D. Clifford, Tanja Jovanovic, Sarah D. Linnstaedt, Laura T. Germine, Kenneth A. Bollen, Scott L. Rauch, John P. Haran, Alan B. Storrow, Christopher Lewandowski, Paul I. Musey Jr., Phyllis L. Hendry, Sophia Sheikh, Christopher W. Jones, Brittany E. Punches, Lauren A. Hudak, Jose L. Pascual, Mark J. Seamon, Elizabeth M. Datner, Claire Pearson, David A. Peak, Roland C. Merchant, Robert M. Domeier, Brian J. O'Neil, Paulina Sergot, Leon D. Sanchez, Steven E. Bruce, Samuel A. McLean, Ronald C. Kessler, Karestan C. Koenen. Resources: Provision of study materials, reagents, materials, patients, laboratory samples, animals, instrumentation, computing resources, or other analysis tools: Xinming An, Stacey L. House, Francesca L. Beaudoin, Jennifer S. Stevens, Thomas C. Neylan, Gari D. Clifford, Tanja Jovanovic, Sarah D. Linnstaedt, Laura T. Germine, Kenneth A. Bollen, Scott L. Rauch, John P. Haran, Alan B. Storrow, Christopher Lewandowski, Paul I. Musey Jr., Phyllis L. Hendry, Sophia Sheikh, Christopher W. Jones, Brittany E. Punches, Lauren A. Hudak, Jose L. Pascual, Mark J. Seamon, Elizabeth M. Datner, Claire Pearson, David A. Peak, Roland C. Merchant, Robert M. Domeier, Brian J. O'Neil, Paulina Sergot, Leon D. Sanchez, Steven E. Bruce, Samuel A. McLean, Ronald C. Kessler, Karestan C. Koenen, Lyle Ungar, Salvatore Giorgi. Data Curation: Management activities to annotate (produce metadata), scrub data and maintain research data (including software code, where it is necessary for interpreting the data itself) for initial use and later reuse: Xinming An, Stacey L. House, Francesca L. Beaudoin, Jennifer S. Stevens, Thomas C. Neylan, Gari D. Clifford, Tanja Jovanovic, Sarah D. Linnstaedt, Laura T. Germine, Kenneth A. Bollen, Scott L. Rauch, Samuel A. McLean, Ronald C. Kessler, Karestan C. Koenen, Lisa Vizer. Writing - Original Draft: Preparation, creation and/or presentation of the published work, specifically writing the initial draft (including substantive translation): Lisa Vizer, Xinming An, Jennifer Pierce, Yinyao Ji, Meredith Bucher, Zhaopeng Xing. Writing - Review & Editing: Preparation, creation and/or presentation of the published work by those from the original research group, specifically critical review, commentary or revision – including pre-or postpublication stages: Lisa Vizer, Xinming An, Jennifer Pierce, Yinyao Ji, Meredith Bucher, Lyle Ungar, Salvatore Giorgi, Zhaopeng Xing, Stacey L. House, Francesca L. Beaudoin, Jennifer Stevens, Thomas C. Neylan, Gari D. Clifford, Tanja Jovanovic, Sarah D. Linnstaedt, Laura T. Germine, Kenneth A. Bollen, Scott L. Rauch, John P. Haran, Alan B. Storrow, Christopher Lewandowski, Paul I. Musey Jr., Phyllis L. Hendry, Sophia Sheikh, Christopher W. Jones, Brittany E. Punches, Lauren A. Hudak, Jose L. Pascual, Mark J. Seamon, Erica Harris, Claire Pearson, David A. Peak, Roland C. Merchant, Robert M. Domeier, Brian J. O'Neil, Paulina Sergot, Leon D. Sanchez, Steven E. Bruce, Steven E. Harte, Ronald C. Kessler, Karestan C. Koenen, Samuel McLean. Visualization: Preparation, creation and/or presentation of the published work, specifically visualization/ data presentation: Lisa Vizer, Xinming An, Jennifer Pierce, Yinyao Ji, Meredith Bucher, Zhaopeng Xing. Supervision: Oversight and leadership responsibility for the research activity planning and execution, including mentorship external to the core team: Samuel A. McLean, Ronald C. Kessler, Karestan C. Koenen, Lisa Vizer, Xinming An. Project administration: Management and coordination responsibility for the research activity planning and execution: Stacey L. House, Francesca L. Beaudoin, John P. Haran, Alan B. Storrow, Christopher Lewandowski, Paul I. Musey Jr., Phyllis L. Hendry, Sophia Sheikh, Christopher W. Jones, Brittany E. Punches, Lauren A. Hudak, Jose L. Pascual, Mark J. Seamon, Claire Pearson, David A. Peak, Roland C. Merchant, Robert M. Domeier, Brian J. O’Neil, Paulina Sergot, Leon D. Sanchez, Steven E. Bruce, Samuel A. McLean, Ronald C. Kessler, Karestan C. Koenen. Funding acquisition: Acquisition of the financial support for the project leading to this publication. Samuel A. McLean, Ronald C. Kessler, Karestan C. Koenen.
Corresponding author
Ethics declarations
Competing interests
Dr. Vizer reports no financial relationships with commercial interests. Dr. Pierce receives support from the National Institute of Mental Health, K01 MH126079. Ms. Ji reports no financial relationships with commercial interests. Dr. Bucher reports no financial relationships with commercial interests. Dr. Liu reports no financial relationships with commercial interests. Dr. Ungar reports no financial relationships with commercial interests. Dr. Giorgi reports no financial relationships with commercial interests. Dr. Xing reports no financial relationships with commercial interests. Dr. House reports no financial relationships with commercial interests. Dr. Beaudoin reports no financial relationships with commercial interests. Dr. Stevens reports no financial relationships with commercial interests. Dr. Neylan has received research support from NIH, VA, and Rainwater Charitable Foundation, and consulting income from Jazz Pharmaceuticals. In the last three years Dr Clifford has received research funding from the NSF, NIH and LifeBell AI, and unrestricted donations from AliveCor Inc, Amazon Research, the Center for Discovery, the Gates Foundation, Google, the Gordon and Betty Moore Foundation, MathWorks, Microsoft Research, Nextsense Inc, One Mind Foundation, and the Rett Research Foundation. Dr Clifford has financial interest in AliveCor Inc and Nextsense Inc. He also is the CTO of MindChild Medical with significant stock. These relationships are unconnected to the current work. Dr. Jovanovic receives support from the National Institute of Mental Health, R01 MH129495. Dr. Linnstaedt reports no financial relationships with commercial interests. Dr. Germine receives funding from the National Institute of Mental Health (R01 MH121617) and is on the board of the Many Brains Project. Her family also has equity in Intelerad Medical Systems, Inc. Dr. Bollen reports no financial relationships with commercial interests. Dr. Rauch reported serving as secretary of the Society of Biological Psychiatry; serving as a board member of Community Psychiatry and Mindpath Health; serving as a board member of National Association of Behavioral Healthcare; serving as secretary and a board member for the Anxiety and Depression Association of America; serving as a board member of the National Network of Depression Centers; receiving royalties from Oxford University Press, American Psychiatric Publishing Inc, and Springer Publishing; and receiving personal fees from the Society of Biological Psychiatry, Community Psychiatry and Mindpath Health, and National Association of Behavioral Healthcare outside the submitted work. Dr. Haran reports no financial relationships with commercial interests. Dr. Storrow reports no financial relationships with commercial interests. Dr. Lewandowski reports no financial relationships with commercial interests. Dr. Musey reports no financial relationships with commercial interests. Dr. Hendry reports no financial relationships with commercial interests. Dr. Sheikh reports no financial relationships with commercial interests. Dr. Jones has no competing interests related to this work, though he has been an investigator on studies funded by AstraZeneca, Vapotherm, Abbott, and Ophirex. Dr. Punches reports no financial relationships with commercial interests. Dr. Hudak reports no financial relationships with commercial interests. Dr. Pascual reports no financial relationships with commercial interests. Dr. Seamon reports no financial relationships with commercial interests. Dr. Harris reports no financial relationships with commercial interests. Dr. Pearson reports no financial relationships with commercial interests. Dr. Peak reports no financial relationships with commercial interests. Dr. Merchant reports no financial relationships with commercial interests. Dr. Domeier reports no financial relationships with commercial interests. Dr. O’Neil reports no financial relationships with commercial interests. Dr. Sergot reports no financial relationships with commercial interests. Dr. Sanchez reports no financial relationships with commercial interests. Dr. Bruce reports no financial relationships with commercial interests. Dr. Harte has no competing interest related to this work, though in the last three years he has received research funding from NIH, Aptinyx, and Arbor Medical Innovations, and consulting payments from Memorial Sloan Kettering Cancer Center, Wayne State University, Indiana University Indianapolis, The Ohio State University, Dana Farber Cancer Institute, and Stanford University. In the past 3 years, Dr. Kessler was a consultant for Cambridge Health Alliance, Canandaigua VA Medical Center, Holmusk, Partners Healthcare, Inc., RallyPoint Networks, Inc., and Sage Therapeutics. He has stock options in Cerebral Inc., Mirah, PYM, and Roga Sciences. Dr. Koenen has been a paid scientific consultant for the US Department of Justice and Covington Burling, LLP over the last three years. She receives royalties from Guilford Press and Oxford University Press. Dr. McLean has served as a consultant for Walter Reed Army Institute for Research, Arbor Medical Innovations, and BioXcel Therapeutics, Inc. Dr. An reports no financial relationships with commercial interests. The remaining authors have nothing to disclose.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vizer, L., Pierce, J., Ji, Y. et al. Smartphone language features may help identify adverse post-traumatic neuropsychiatric sequelae and their trajectories. NPP—Digit Psychiatry Neurosci 3, 8 (2025). https://doi.org/10.1038/s44277-025-00028-x
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s44277-025-00028-x