Abstract
Respiratory syncytial virus (RSV) is the leading cause of infant hospitalization. All current RSV therapeutics, including antibody prophylaxis and adult vaccination, target the RSV fusion glycoprotein (RSV-F). The seven neutralization sites on RSV-F are highly conserved and infrequently mutate. Here, we show that a single amino acid mutation at position 305 in RSV-F significantly alters antigenic recognition of RSV-F binding sites and reduces the susceptibility of RSV to neutralizing antibodies. In an in vitro evolution assay, we show that RSV-F L305I occurs in a majority of RSV quasi-species. Computational modeling predicted that the L305I mutation altered the epitope landscape of RSV-F, resulting in changes to neutralizing antibody sensitivity and affinity towards the RSV-F glycoprotein. Screening of published RSV-F sequences revealed that position 305 in RSV-F was conserved with a leucine and isoleucine in RSV-A and RSV-B subtypes respectively. Our study suggests that select amino acids in RSV-F may act as ‘conformational switches’ for RSV to evade host serum antibodies. This work has important implications in understanding RSV evolution and resistance as it suggests that mutational resistance to neutralizing antibodies can occur at sites distal to antigenic epitopes, significantly altering antibody sensitivity to viral infection. These unique antigenic landscape changes should be considered in the context of vaccine and therapeutic development in order to better understand viral mechanisms of evasion and resistance.
Similar content being viewed by others
Introduction
Respiratory Syncytial Virus (RSV) is the leading cause of infant hospitalization and the second leading cause of infant mortality worldwide1. There are an estimated 33 million cases of RSV-associated acute-lower respiratory tract infections annually, over 100,000 of which lead to death1. Immunocompromised and elderly populations are increasingly being recognized as vulnerable high-risk groups for severe disease2. Despite the enormous disease burden presented by RSV, there are few effective antiviral therapies readily available for the treatment of active infection. Biologics in the form of prophylactic monoclonal antibodies provide a means of passive immunization and are the treatment of choice for RSV infection. Until recently, the prophylactic monoclonal antibody Palivizumab (PZMB) was the only preventative therapeutic available for high-risk infants. PZMB is administered monthly throughout the RSV season to only the highest-risk infants. PZMB is costly, has variable efficacy, and leaves a large population of infants and susceptible adults unprotected3. In 2023, the FDA approved Nirsevimab for use in all infants under 8 months old entering their first RSV season, and Merck has a Phase III biologic - Clesrovimab - in development4. In contrast to PZMB, Nirsevimab and Clesrovimab are more potent, and thus administration is only required once per RSV season. Two new adult vaccines created by Pfizer (Abrysvo) and GSK (Arexvy) were also approved for use in the elderly, and pregnant women respectively5,6.
In light of these promising advancements, it is critical that we better understand how RSV might adapt to evade the selective pressures that are sure to be elicited by novel therapeutics. RSV is under consistent evolutionary pressure while circulating in the human population. While the primary burden of RSV is in infants, it continuously circulates in healthy adults and accounts for approximately 15–35% of all respiratory virus cases in any given season7. The antiviral immune response mounted during the course of RSV infection places selective pressures on the virus that lead to quasi-species displaying an array of polymorphisms. Like other RNA viruses, RSV adapts readily while circulating in the population, particularly in the highly variable gene that encodes the attachment glycoprotein, RSV-G8. Genetically distinct viruses impact viral load and pathology in humans during subsequent RSV seasons, which we have previously correlated with viral replication in tissue culture9.
There are two subtypes of RSV, subtype A (RSV-A) and subtype B (RSV-B). RSV-A and RSV-B are estimated to have diverged from their most recent common ancestor approximately 338 years ago10. In any given season, one subtype typically predominates over the other and alternates annually11. However, some reports show that the two subtypes can co-circulate in the population and even present as co-infections in the same patient12. Overall, RSV-A and RSV-B share about 90% nucleotide sequence identity, with the highest regions of sequence variability occurring in the RSV-M2-2 and RSV-G genes13. RSV-A and RSV-B are primarily differentiated by high amino acid variability between their RSV-G glycoproteins14. Notably, there are also select residues in other viral proteins, including RSV-F, that are conserved within each RSV subtype and distinguish the two. Although it is widely disputed whether these genetic differences alter disease severity, genetic differences between RSV-A and RSV-B can result in varying viral susceptibility to antibodies. The prophylactic monoclonal antibody, Suptavumab by Regeneron Pharmaceuticals, was halted in phase III clinical trials due to two amino acid substitutions in RSV-B that rendered it ineffective15. It is critical that we better understand how mutations and subtype differences in RSV-F affect viral susceptibility to therapeutics in order to predict how RSV will mutate in response to antiviral pressure.
The RSV fusion glycoprotein (RSV-F) is the primary therapeutic target for the majority of biologics and vaccines in development against RSV as it induces highly potent neutralizing antibodies16,17,18,19. RSV-F mediates viral entry by attachment to a primary signaling receptor and fusion protein. We have previously reported that IGF1R is a primary signaling receptor for RSV-F whereby the interaction of the two increases the expression of the fusion receptor, nucleolin, to the cell surface20,21. This interaction results in a dynamic conformational change of RSV-F that fuses the viral envelope and cell membrane22. RSV-F exists in two conformational forms, a prefusion, and a post-fusion form. Prefusion RSV-F is highly antigenic and contains 7 potent neutralization sites: ∅, I, II, III, IV, V, and the newly identified site VI23,24. Of these, sites ∅, I, and V are lost upon fusion25. PZMB, Nirsevimab, and Clesrovimab bind to sites II, ∅, and IV respectively. The majority of RSV-F is highly conserved with the exception of the signal peptide and p27 domains where consistently high levels of sequence variability between RSV isolates are observed26,27,28. Even so, there are positions in RSV-F that appear to be more variable than others, like positions 172 and 173 at site V, and positions 206 and 209 just outside of and within antigenic site ∅29,30. Additionally, polymorphisms at positions 272 and 276 have previously been associated with PZMB resistance31.
Here, we report on a mutation in the RSV-F glycoprotein at position 305. In an evolution assay using lab strain RSV-A2, we found that a leucine (L) to isoleucine (I) mutation in RSV-F at residue 305 occurred at an evolutionary bottleneck in the presence of polyclonal antibody pressure. Importantly, position 305 in RSV-F is one of the key conserved differences between RSV-A and RSV-B subtypes, marked by amino acids L305 and I305 respectively. Computational modeling predicted that this single amino acid difference caused a change in the RSV-F conformational landscape. Subsequently, we showed that introducing an L305I mutation in lab strain RSV-A2 reduced RSV susceptibility to neutralizing serum and monoclonal antibodies that targeted various binding sites on RSV-F. In light of these findings and recent therapeutic advancements, a better understanding of RSV adaptation and evolution is critical for monitoring potential breakthrough viral isolates and future vaccine design.
Results
Lab adapted RSV-A2 develops a leucine to isoleucine mutation at position 305 under polyclonal antibody selective pressure at bottleneck titers
To understand how RSV mutates in response to antibody pressure, we performed an in vitro resistance and evolution assay in the presence of a neutralizing polyclonal anti-RSV antibody, a non-nucleoside polymerase inhibitor that we previously developed32,33, and a DMSO control. The virus was harvested every two days for 20 passages. Viral titer was measured by qRT-PCR and viral genomes were next-generation sequenced (NGS) following significant drops in titer, which we refer to hereafter as bottlenecks (Fig. 1a–c). We were specifically interested in looking at bottlenecks because we sought to determine if mutations arising at these positions lead to viral evasion of neutralizing antibody pressure and subsequently increased viral titer. The first bottleneck we identified under polyclonal anti-RSV antibody selective pressure was at passage 5 (Fig. 1a). Additional bottlenecks at passages 9 and 13 were observed but reliable sequences could not be obtained by NGS past passage 9 and the virus was undetectable past passage 13 by RT-qPCR. Sequencing of the passage 5 viral population revealed the RSV-F L305I mutation as the only non-synonymous mutation occurring in the majority of sequencing reads (Fig. 1b, Supplementary Table 1). Here, 42.03% of reads contained L (CTA) while 57.93% of reads contained the mutated I (ATA) (Fig. 1b, Supplementary Table 1). An increase in the proportion of RSV-F L305I was subsequently associated with a rebound in viral titer (Fig. 1a and b). The next two most frequently occurring non-synonymous mutations were RSV-F N276S and RSV-F V152I, occurring at 36.92% and 31.82% respectively (Supplementary Table 2). Interestingly, the RSV-F N276S has previously been associated with Palivizumab resistance, and modern RSV strains appear to be mutating away from the historic asparagine (N) at position 276 to a serine (S)34. To the best of our knowledge, an RSV-F V152I mutation has not been reported in the context of viral resistance. However, upon analysis of published RSV-F sequences, we determined that 98.7% of sequences contain isoleucine (I) at position 152, suggesting that a valine (V) may be characteristic of the early RSV-A2 genotype and that most modern circulating RSV strains have since mutated away from this. We also observed the RSV-F L305I mutation upon treatment with our synthesized RSV polymerase inhibitor33 (Fig. 1c). At 10 µM and 25 µM, RSV-F L305I occurs at passage 8 (17.25%) and passage 6 (41.53%) respectively but is undetectable by passage 20 at both concentrations (data not shown). The presence of an L305I mutation in RSV-F following treatment by a polymerase inhibitor was interesting and might suggest that this mutation is a general mechanism of RSV evasion, rather than a direct response to RSV-F selective pressures.
a RSV-A2 was passaged 20 times for 40 days in the presence of anti-RSV antibody or 0.25% DMSO (control). Viral titer at each passage was determined via qRT-PCR and whole viral genomes were sequenced by NGS. Mutations are indicated at the passage numbers at which they first arose. b The proportion of RSV-A reads with amino acids Leucine and Isoleucine at position 305 are plotted alongside viral titer at each corresponding passage. c The same evolution experiment as described in Fig. 1a was conducted in Hela cells in the presence of an RSV polymerase inhibitor (compound 5 f, right) at a concentration of 10 µM and 25 µM . d Comparison of sequenced clinical isolates from Alberta and Ohio. The percentage identity is shown within and between each RSV subtype at the whole genome level and at each gene. e Graphical representation of RSV-F amino acid differences in RSV-A (blue) and RSV-B (red). 3747 RSV-F amino acid sequences were obtained from NCIB and aligned. Consensus sequences of subtypes A and B were compared and positions with less than 65% sequence identity are shown. The RSV-F domains are displayed and bindings sites Ø (orange), II (green), and IV (purple) are highlighted.
Published and clinical RSV isolates show that amino acid position 305 is subtype specific
Since RSV-F L305I was the only mutation to emerge in the majority of sequenced reads under anti-RSV selective pressure, we wanted to better understand its potential role in viral evasion. To determine the biological relevance of the RSV-F L305I mutation, we analyzed published RSV-F sequences from the Virus Pathogen Resource (ViPR) database and representative samples from previously sequenced RSV-A and B clinical isolates from hospitalized patients in Alberta, Canada, and Nationwide Children’s Hospital in Columbus, Ohio, during the 2014 to 2016 seasons9. The percent identities between representative clinical isolates were determined (Fig. 1d). We found that RSV-F was one of the most conserved genes among our clinical isolates, in agreement with previous reports26. RSV-F sequences shared greater than 99% identity within each individual subtype and 90.4% identity between RSV-A and RSV-B isolates (Supplementary Table 3). Further analysis of our clinical isolates revealed that all RSV-A and RSV-B sequences had a conserved leucine and isoleucine at position 305, respectively (Supplementary Table 4)9.
To support our modest sample size, we downloaded 3747 complete RSV-F sequences from the ViPR database and analyzed their amino acid composition (Fig. 1e and Supplementary Table 5). As we observed in our clinical isolates, RSV-A and RSV-B subtypes differed in their amino acid composition at position 305, as others have previously noted35. In addition to position 305, there were approximately 50 other residues throughout RSV-F that appeared to be subtype-specific (Fig. 1e). It is worth noting that no other amino acids were found to occupy position 305 in any RSV isolates, providing evidence that the RSV-F L305I mutation is not simply an artifact of our in vitro evolution assay and may serve a biological function.
An L305I mutation in the RSV-A2 fusion glycoprotein alters the conformation of the RSV-F protomer
Constitutional isomers, leucine and isoleucine, inherently share several biochemical properties and differ structurally only in the position of a side chain methyl group (Fig. 2a). We asked whether this structural difference could have a steric effect on nearby amino acids in the RSV-F protein. To investigate this, we introduced the L305I mutation into the cryo-EM structure of the RSV-A2 prefusion F glycoprotein using the Schrödinger Small Molecule Discovery Suite followed by a molecular dynamics simulation of both proteins. Comparison of the wild-type RSV-F L305 and mutant RSV-F I305 models revealed that an L305I mutation induces a subtle protein-wide conformational change (Fig. 2b). Superimposition of wild-type and mutant RSV-F suggests that this structural change extends to various binding sites including antigenic sites ∅, II, and IV (Fig. 2b and c).
a Molecular structures of leucine and isoleucine. b A single RSV-F protomer. Overlay of RSV-A2 prefusion F protein: RSV-F L305 (WT, peach) and RSV-F I305 (L305I, green) showing the change in orientation of amino acids L305 (blue) and I305 (red), and the subsequent effect on the overall shape of the protomer. c Space filling models of RSV-F L305 and RSV-F I305 protomers colored in peach and green, respectively, with binding site II highlighted in teal and orange and residues L305 and I305 in red and blue, respectively. To the right, the protomers are overlaid. d One-step growth curve and e a time course of focal forming unit (FFU) release of rgRSV WT (white) and rgRSV L305I (red) on indicator HeLa cells (n = 3). d Cells were infected with an MOI of 0.25 and particle release was measured by RT-qPCR every 6 h for 96 h. e Cells were infected with an MOI of 0.3. Every 24 h media was used to reinfect new cells and resulting FFUs were determined by colorimetric immunostaining. 2-way ANOVA with multiple comparisons test was used to determine statistical significance (**p < 0.005, ****p < 0.0001).
RSV-F exists on the surface of the RSV virion as a dynamic trimer that has been shown to “breathe”, a phenomenon that can alter the accessibility of specific epitopes on trimerized RSV-F36. We wanted to determine whether L305I affects trimer breathing. To do this we evaluated the dynamics of RSV-F L305 and RSV-F I305 using Molecular Dynamics (MD) simulations (Supplementary Fig. 1). Analysis of the MD trajectories revealed that the Cα of both systems each equilibrated around 200 ns of the simulation time with an average RMSD of 2.3 Å and 2.8 Å for RSV-F L305 and RSV-F I305 respectively, suggesting that the mutation has little effect on trimer breathing (Supplementary Fig. 1a). Next, we investigated the flexibility of the system residues using atomic fluctuations expressed as a function of B-factor of the protein backbone atoms for both systems (Supplementary Fig. 1b). The majority of protein residues were stable during the entire simulation with more flexibility observed in the region 250–284 for RSV-F I305 compared to that of the RSV-F L305 and with increased flexibility in the 420–500 region of RSV-F L305 compared to RSV-F I305 (Supplementary Fig. 1b and Supplementary Movie 1).
The flexibility of the 420–500 region may be attributed to the electrostatic repulsion caused by clustered negatively charged residues, particularly at positions 486 and 487, within the heptad repeat B (HRB) ___domain (residues 476–516). This charge repulsion destabilizes the prefusion conformation which may have contributed to the increased atomic fluctuations we observed in our MD simulations. Previous studies have attempted to reduce this repulsion using charge-neutralizing mutations, such as D486N, D486S, E487Q, and D489S, as part of efforts to develop a stable prefusion RSV-F vaccine37,38,39. However, the reason for the increased flexibility of this region in RSV-F L305 compared to RSV-F I305 remains unclear. One possible explanation is that the L305I mutation stabilizes the trimeric structure in a way that propagates through the protein, reducing the dynamic fluctuations in the 420–500 region. This suggests that changes at position 305 may have a distal effect on the overall conformational dynamics and stability of the RSV F trimer. Overall, we predicted that there are flexibility differences between RSV-F L305 and RSV-F I305 proteins in certain regions that may explain the observed structural alterations between the two proteins.
To further validate the significance of the RSV-F L305I mutation, we compared the structure of the RSV-A2 prefusion F protein containing an asparagine (N) or serine (S) at position 228. We chose this position because analysis of published RSV isolates highlighted it as another subtype-specific residue in RSV-F - asparagine in RSV-A and serine in RSV-B - and is found distal to binding site ∅ (Fig. 1e). Clustering of the MD trajectories suggested that the RSV-F S228 mutant did not show a noticeable conformational shift from the wild-type RSV-F N228. Atomic alignment of the RSV-F S228 and RSV-F N228 structures had an RMSD of 2.4 Å. The RMSD of both systems showed a stable structure during the entire simulation with an average RMSD of 2.9 Å and 2.7 Å for the RSV-F N228 and RSV-F S228, respectively (Supplementary Fig. 1c). We also analyzed the atomic fluctuation to understand the regional flexibility of the structures. Our results indicate a similar trend in region flexibility between RSV-F N228 and RSV-F S228 suggesting that this mutation causes little to no conformational change to the protein (Supplementary Fig. 1d). Additionally, flexibility in the 420–500 region was higher in RSV-F N228 compared to RSV-F N228S, mirroring the trend observed in the L305I comparison, though to a lesser extent.
Taken together, our computational modeling predicts that introducing the conservative RSV-F L305I mutation into RSV-A2 might alter the structural conformation of the entire RSV-F glycoprotein and that this observed difference is likely not due to alterations in trimer breathing.
A conservative leucine to isoleucine mutation at position 305 in an RSV reverse genetics model alters infectivity of viral particles and susceptibility to human sera
Given that our models predict a structural difference in RSV-A2 fusion proteins containing either an L or an I at position 305, we wondered whether this single mutation would have a functional impact on RSV in vitro. To test this, we used a recombinant reverse genetics model of RSV-A2 based on the RW30 backbone (rgRSV)40,41. We added in an L305I mutation via Gibson assembly and the resulting plasmid was sequenced to confirm the presence of RSV-F I305. First, we looked at whether there were any changes in growth characteristics between the wild-type rgRSV-A2 L305 and mutant rgRSV-A2 I305, which we will hereafter refer to as RSV WT and RSV L305I respectively. Since RSV-B isolates have been found to grow slower than RSV-A isolates in tissue culture, we wondered if RSV L305I might also grow slower than RSV WT42,43. To test this, we created a one-step growth curve of RSV WT and RSV L305I in which HeLa cells were infected with equivalent MOIs, and the media was collected every 6 h over 96 h (Fig. 2d). Subsequent viral particle release was measured by RT-qPCR. We found no significant difference in the number of viral transcripts released between RSV WT and RSV L305I (Fig. 2d). However, when we measured foci of infection across 72 h, we found that RSV L305I resulted in significantly fewer foci than RSV WT (Fig. 2e and Supplementary Fig. 2). This suggests that although similar amounts of transcripts are produced by the two viruses, the virions produced by RSV L305I are significantly less infectious (Fig. 2e).
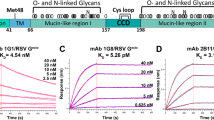
Taking into account our modeling data, we wondered whether the sensitivity of RSV to human sera may be altered by the L305I mutation. We took polyclonal sera from otherwise healthy full-term infants that had confirmed infections with RSV-A or RSV-B. We decided to use infant sera to reduce confounding results from older patients which may be complicated by immune memory to previous RSV infections. However, our sera samples were obtained from infants ranging in age from 2 weeks - 13.3 months. Although maternal RSV antibodies have been previously reported to be mostly absent by 3 months of age, we cannot rule out whether these infants had received passive RSV antibodies from their mothers, particularly in sera samples from infants less than 3 months of age44. Due to the limited amount of human sera we had available, we were unable to conduct complete EC50 curves for all sera samples. Instead, we evaluated the difference in percent neutralization between RSV WT and L305I at a single dilution for each sera sample, and conducted two representative EC50 curves for one RSV-A (A50) and one RSV-B (B18) sera samples (Fig. 3). HeLa cells were infected at an MOI of 0.3 with RSV WT or RSV L305I that had been incubated with human sera for 1 h, and percentage of infected cells was determined by flow cytometry (Fig. 3). The IgG antibody concentration of each serum sample was determined and either 15 µg/mL, 75 µg/mL, or 150 µg/mL of serum IgG was incubated with virus. We used varying dilutions of IgG antibodies based on the potency of the sera samples in order to observe between 20–80% inhibition of the virus. As was expected, different sera samples had varying levels of neutralization against RSV WT and RSV L305I even with varying levels of IgG antibodies (Fig. 3a). However, we found that overall RSV L305I was significantly more resistant to human sera than RSV WT (p < 0.0001) (Fig. 3b). This is in line with what we observed in our in vitro evolution experiment, wherein the introduction of the L305I mutation led to a temporary rebound in viral titer (Fig. 1a). To compliment these results, we also conducted two complete EC50 curves for representative RSV-A and RSV-B serum samples, based on sera availability (Fig. 3c and d). With both serum samples, we observed a significant reduction in neutralization of RSV L305I compared to RSV WT. This is particularly interesting with RSV-A50, where we observe a small difference in neutralization at a single dilution (Fig. 3a and b) but a statistically significant reduction with a complete EC50 curve (Fig. 3c). Overall, RSV L305I appears to be significantly more resistant to neutralization by human sera.
a, b RSV WT (blue) and RSV L305I (red) neutralization susceptibility to human sera were compared using sera collected from RSV-A or RSV-B infected infants. RSV WT and RSV L305I viruses at an MOI of 0.3 were incubated for 1 h with infant serum diluted to 15 μg/mL, 75 μg/mL, or 150 μg/mL of IgG antibody followed by infection of HeLa cells. Infectious virus was determined by GFP expression using flow cytometry (n = 2). a, percent inhibition was determined for 15 sera samples by comparison to a virus untreated control. b total percent inhibition for all sera samples. Statistical significance was determined using a paired two-tailed t-test (****p < 0.0001). c, d complete EC50 curves were conducted for two representative sera samples (n = 2) c, RSV-A50 and d, RSV-B18. Sera was diluted down 5-fold from a starting dilution of 0.07 and incubated with RSV WT and RSV L305I viruses at an MOI of 0.3 prior to infecting HeLa cells. Percent inhibition was determined by GFP expression by flow cytometry relative to a virus alone control. EC50 values for RSV WT and RSV L305I are indicated at the top left of each graph. Data were fit using a non-linear regression curve and EC50 values were compared using the extra sum-of-squares F test.
Computational modeling of the RSV-F L305I mutation shows a structural shift in RSV-F antigenic site II
Currently, prophylactic monoclonal antibodies are the therapeutic of choice to prevent RSV infection in infants. PZMB and Nirsevimab have been FDA-approved for use in infants and Clesrovimab is in late-phase clinical trials4. These antibodies target antigenic sites II, ∅, and IV respectively, on RSV-F (Fig. 4a). We sought to investigate the impact that the L305I mutation may have in the context of these prophylactic treatments. Our in silico structural modeling shows that position 305 is located in antigenic site III, which is typically considered a weak antigenic site (Fig. 2b). However, we also observed that position 305 is located directly behind PZMB binding site II in RSV-F (Figs. 2a and 4b)25. Using molecular dynamics simulations at over 500 ns, we found that the L305I mutation led to a conformational change in antigenic site II (Fig. 4b). Superimposition of site II RSV-F L305 and RSV-F I305 revealed not only a movement in the PZMB binding site but also a change in the orientation of several residues. The L305I mutation forced residue N254 to change orientation outwards by 137.4˚ (Fig. 4c). In addition, Q279 has a bond angle change of 137.2˚ from the wildtype RSV-F L305 to the mutant RSV-F I305 (Fig. 4c). Moreover, trajectory analysis revealed local structural rearrangements within the PMZB binding site. Specifically, reorientations of residues T267, D269, K272, and L273 were observed in RSV-F I305 compared to RSV-F L305. These changes may reduce the accessibility of PMZB to key residues within RSV-F antigenic site II, which are critical for effective neutralization of the virus (Supplementary Fig. 3). Notably, mutations at residue K272 have been previously associated with escape variants resistant to PMZB neutralization45. In summary, it appears that the steric effects caused by the L305I mutation extend to and affect the structural conformation and rearrangement of critical residues in antigenic site II.
a Space filling structural model of the RSV-F trimer with antigenic sites Ø (orange), II (green), and IV (purple) highlighted. b Superimposition of the residues at position 305 in RSV-F L305 (green) and RSV-F I305 (peach). The ___location of the leucine and isoleucine residues at position 305 are indicated in blue and red respectively. c Computational model of the changes in the PZMB binding site (site II) with the L305I mutation. Conformational changes in select amino acid residues surrounding position 305 are indicated. d EC50 curves of PZMB neutralization of RSV WT (blue) and RSV L305I (red) determined by flow cytometry (n = 3). EC50 values are indicated in parentheses. Data were fit using a non-linear regression curve and EC50 values were compared using the extra sum-of-squares F test. e Total protein and anti-histidine-stained gels of purified DS-Cav1L305 and DS-Cav1I305 constructs. f, g SPR binding curves of PZMB to DS-Cav1L305 and DS-Cav1I305 are indicated in blue and red respectively (n = 2). Fitted curves were determined using a 1:1 binding model and are indicated in black. Observed KD values are indicated for each curve.
The structural change elicited by RSV-F L305I alters antibody binding affinity to site II and viral susceptibility to palivizumab
To determine whether the predicted change in structure of binding site II affects PZMB neutralization, we conducted an in vitro neutralization assay with RSV WT and RSV L305I. We found that RSV WT was more susceptible to palivizumab (EC50 = 80.24 ng/mL) than RSV L305I (EC50 = 207.2 ng/mL) (Fig. 4d). Even at a maximum concentration of 105 ng/mL, PZMB was unable to fully neutralize RSV L305I, whereas RSV WT appeared to be almost fully neutralized by 103 ng/mL of PZMB (Fig. 4d). To further validate the change in PZMB sensitivity to neutralization, we directly assessed the binding affinity of PZMB to RSV-F using surface plasmon resonance (SPR). To do this we used a recombinant prefusion stabilized RSV-F protein trimer called DS-Cav118. Wildtype (DS-Cav1 L305) and mutant (DS-Cav1 I305) constructs were used to measure the kinetics of bivalent IgG PZMB binding to protein, where KD is inversely proportional to binding affinity (Fig. 4e). All of the KD values reported here were determined using bivalent IgG antibody binding. As such, it is important to note that these values are the observed relative values between DS-Cav1 L305 and I305 constructs rather than absolute KD values, which are typically determined using Fab fragment binding. We observed a slight, but not significant, decrease in the KD value, for the mutant DS-Cav1 I305 (KD = 0.10 nM) as compared with the WT DS-Cav1 L305 (KD = 0.29 nM) (Fig. 4f and g, Supplementary Table 6). This suggests that there is no observable change in PZMB binding affinity to prefusion stabilized DS-Cav1 induced by the L305I mutation.
RSV-F L305I alters the structure of RSV-F antigenic sites Ø and IV, and subsequent binding affinity of monoclonal antibodies
Following our characterization of the effect of L305I on binding site II, we asked whether the same mutation could similarly affect more distant antigenic sites. Several therapeutic monoclonal antibodies that target various RSV-F antigenic sites are of particular interest to us, including the recently approved Nirsevimab and the phase III clinical trial antibody Clesrovimab, which target binding sites Ø and IV respectively4,46. To study these binding sites, we used monoclonal antibodies D25 and 101 F. D25 is the parental antibody to Nirsevimab47 while 101 F and Clesrovimab both target binding site IV, specifically the epitopes spanning residues 427-438 and 426-447 respectively48,49. Analysis of MD trajectories revealed that antigenic site Ø, at the apex of the RSV-F I305 monomer and trimer, was shifted by 9.1 Å for α1 and 10 Å for α5 helices when compared to RSV-F L305 (Fig. 5a), while site IV shifted by about 8 Å (Fig. 5b). Interestingly, these results suggest that the L305I mutation, which is located in antigenic site III, also affects the structural conformation of antigenic sites Ø and IV in RSV-F.
Representative structures from the MD simulation of RSV-F antigenic sites a Ø and b IV with RSV-F L305 and RSV-F I305 indicated in green and gold, respectively. Neutralization curves for c D25 and d, 101 F monoclonal antibodies against RSV WT (blue) and RSV L305I (red) determined by flow cytometry (n = 3). EC50 values are indicated in parentheses beside each virus. Data were fit using a non-linear regression curve and EC50 values were compared using the extra sum-of-squares F test. SPR sensorgram plots for e D25 and f 101 F monoclonal antibodies against DS-Cav1L305 recombinant proteins in blue and g, h DS-Cav1I305 recombinant proteins in red. e, f are representative plots of n = 3 and n = 2 replicates, respectively. Fitted curves are determined using a 1:1 binding model (black). Observed KD values are indicated for each curve.
To confirm whether these structural changes have biological relevance, we evaluated the neutralizing potential of D25 and 101 F to RSV WT and RSV L305I. We saw similar trends with monoclonal antibodies D25 and 101 F as we did with PZMB. The EC50 value for D25 was higher for RSV L305I (12.29 ng/mL) than RSV WT (5.69 ng/mL) suggesting that the L305I mutation acts like a resistance mutation (Fig. 5c). Similar to our PZMB results, RSV L305I could not be fully neutralized even at a maximum antibody concentration of 104 ng/mL whereas RSV WT was fully neutralized by 102 ng/mL of antibody (Fig. 5c). We observed that the EC50 value of 101 F was also higher for RSV L305I (50.19 ng/mL) compared to RSV WT (24.30 ng/mL), suggesting that the L305I mutation makes RSV less susceptible to 101 F (Fig. 5d). To validate these findings, we again compared the binding kinetics of D25 and 101 F to DS-Cav1 L305 and DS-Cav1 I305 RSV-F proteins using SPR. Consistent with our D25 neutralizations, we report an increased KD for DS-Cav1 I305 (4.40 nM) compared to DS-Cav1 L305 (0.84 nM), suggesting that the binding affinity of D25 is higher to the wildtype RSV-F than the mutant (Fig. 5e and g). SPR with 101 F revealed similar results to PZMB, wherein the observed KD value for DS-Cav1 L305 (0.52 nM) and DS-Cav1 I305 (0.31 nM) were similar, suggesting that the L305I mutation does not affect the binding affinity of 101 F (Fig. 5f and h).
This data suggests that the increased resistance to D25 can be at least partially attributed to a change in binding affinity towards RSV-F, where D25 binds weaker to RSV-F L305I (Fig. 5e and g). However, it is not clear what the source of the increased resistance to PZMB and 101 F is if the L305I mutation does not alter the binding affinity of these antibodies to prefusion RSV-F (Fig. 4 and Fig. 5). Given that antigenic sites II and IV are retained during the conversion of prefusion to post-fusion RSV-F, whereas site Ø is not, it is possible that the L305I mutation also has an effect on antibody binding to post-fusion RSV-F in these cases. One potential explanation for the observed shift in antigenic site Ø, promoted by the L305I mutation, is that this mutation induces a conformational change that alters local dynamics or the accessibility of D25 to RSV F. This aligns with our previous findings that antigenic site Ø exists as an ensemble of conformations, with individual antibodies recognizing distinct structural states29. Such conformational flexibility may modulate the binding affinity of site Ø-targeting antibodies, including D25.
In contrast, the difference in neutralization observed between site Ø and site IV could be attributed to the adaptability of monoclonal antibodies such as 101 F. Unlike D25, 101 F can bind multiple conformations of RSV F at site IV, allowing it to accommodate structural changes induced by the L305I mutation. This is consistent with previous reports demonstrating that 101 F retains binding across different conformations of RSV F19.
To evaluate whether the shifts in antigenic sites Ø and IV induced by the L305I mutation in RSV-A F can also be observed in RSV-B F, we conducted structural alignment and analysis between WT RSV-A L305, RSV-A L305I, and RSV-B F (PDB accession: 5UDE) (Supplementary Fig. 4). Superimposition of RSV-A L305 and RSV-B F structures revealed a significant deviation, with an average RMSD of 3.25 Å (across 575 residue Cα atoms) (Supplementary Fig. 4a). In contrast, the alignment of RSV-A L305I and RSV-B F showed a reduced average RMSD of 1.82 Å (Supplementary Fig. 4b), suggesting that the L305I mutation induces structural rearrangements that make RSV-A L305I more structurally similar to RSV-B F. Interestingly, while both site Ø and site IV undergo shifts when comparing RSV WT to RSV L305I (Fig. 5b), site IV appears to be more conserved between RSV-B F and RSV-A L305I, exhibiting minimal additional deviation. In contrast, site Ø shifts by approximately 14 Å (Supplementary Fig. 4c), indicating that the L305I mutation may selectively drive further changes in site Ø when aligned with RSV-B F, while site IV adopts a conformation closer to RSV-B F. This observation aligns with the hypothesis that conformational changes induced by L305I could influence antibody accessibility and binding. However, rather than acting as a strictly site-specific mutation, L305I appears to induce broader structural rearrangements that impact multiple antigenic sites, including those distal to its ___location.
Despite structural differences between RSV-A and RSV-B F proteins, the similar neutralizing antibody titers reported for these subtypes suggest that compensatory mechanisms or conserved epitopes may help mitigate the impact of the L305I mutation on neutralization44. Additionally, the predicted shift observed in site Ø raises the possibility that some neutralizing antibodies targeting this region might exhibit differential efficacy against RSV-A and RSV-B. Overall, our results suggest that the L305I mutation can elicit significant changes across at least RSV-F antigenic sites Ø, II, and IV, and subsequently impact the effectiveness of monoclonal antibodies that target these regions.
Discussion
To the best of our knowledge, this is the first in vitro analysis of longitudinal RSV-F adaptation in response to antibody pressure. Here we describe a new L305I mutation that changes the structural landscape of the RSV-F trimer and alters viral susceptibility to monoclonal antibodies, despite being located outside of the target antigenic sites. We found that the L305I mutation was the first to arise at a viral bottleneck under anti-RSV polyclonal antibody pressure and is a conserved difference between RSV-A and RSV-B subtypes. We suspect that the L305I mutation developed in a majority of the viral population due to the subtle differences in antibody susceptibility between the viruses so that when the RSV WT load was suppressed, RSV L305I was able to grow. This would suggest that L305I could arise normally but is outcompeted in the presence of RSV-F L305 containing RSV-A viruses. We surmise that, since the emergence of RSV-F I305 in RSV-B strains, compensatory mutations may have resulted in some RSV-B isolates growing to levels that are equivalent to RSV-A isolates allowing the two subtypes to co-circulate.
Using computational modeling we showed that L305I, located in the antigenic site III, was able to alter the conformation of the entire RSV-F trimer. Subsequently, this mutation led to a decrease in viral susceptibility to monoclonal antibodies PZMB, D25, and 101 F, at the cost of viral replicative fitness in tissue culture. Interestingly, this reduced propensity for growth is analogous to growth differences reported between RSV-A and RSV-B subtypes9,42,43. Our neutralization assays revealed that the L305I mutation also altered viral susceptibility to serum neutralization. A previous paper reported high levels of RSV-G diversity in the presence of immune pressure50. It is interesting to consider that L305I, or similar mutations, may have evolved in response to immune pressures in order to evade neutralizing serum antibodies at the expense of viral fitness.
We found that overall, only D25 had a significantly different binding affinity between DS-Cav1 L305 and DS-Cav1 I305, while PZMB and 101 F had a similar binding affinity for both proteins. This suggests that the resistance to D25 observed with RSV L305I can, in part, be explained by a decrease in binding affinity to RSV-F I305. It is interesting to consider what else could cause the increased resistance of RSV-L305I to PZMB and 101 F. For instance, since sites II and IV exist on both prefusion and post-fusion RSV-F, it is possible that the L305I mutation increases antibody binding affinity to post-fusion RSV-F site II and IV. In this case, a higher proportion of circulating antibodies might preferentially bind post-fusion rather than prefusion RSV-F and decrease neutralization potential. Additionally, the L305I mutation may play a role in receptor binding and subsequent entry and fusion dynamics. It is also important to note that measuring EC50 in tissue culture introduces additional factors compared to the highly controlled environment used to measure KD. For example, the observed KD was measured using the stabilized DS-Cav1 protein which is a more rigid form of RSV-F compared to its highly dynamic native state on the viral membrane. This difference in flexibility between the two proteins may also factor into the discrepancy observed between these results.
With the introduction of novel RSV prophylaxis in the form of both vaccines and monoclonal antibodies, it is critical that we carefully monitor circulating RSV strains for escape mutants. Special attention should be paid to mutations located throughout RSV-F and not just in targeted antigenic sites, particularly if treatments cause a significant bottleneck and non-sterilizing reductions in viral titer in recipients. Wilkins et al. recently reported that although the Nirsevimab binding site is relatively conserved, amino acid variability is high outside of the binding site47. It is important to note that they also reported subtle, but not significant, changes in PZMB susceptibility with mutations at the Nirsevimab binding site. Interestingly, they have also reported that the RSV-A and RSV-B RSV-F proteins have less genetic diversity than other class I viral fusion proteins of influenza and beta coronaviruses47. However, we do not know whether this is because the RSV-F protein is structurally constrained or if it is more structurally plastic with fewer mutations compared to other viruses. Other groups have also shown significant functional changes in proteins with conserved mutations. Wu et al. demonstrated that a mutation from isoleucine to leucine, in the KlenTaq1 DNA polymerase, significantly affected its temperature sensitivity51. Despite the mutation being located 20 Å away from the active site, this mutation had a substantial impact on the enzyme’s temperature sensitivity. This suggests that even conservative alterations in the amino acid sequence, such as those in RSV-F, may be critical for maintaining the protein functionality required for viral entry.
The work described herein has novel significance with respect to antiviral and vaccine resistance and highlights the value of in silico modeling combined with functional studies and rigorous viral surveillance. This study highlights the importance of elucidating the full potential of therapeutic breakthroughs by viruses. In light of recent therapeutic advancements, RSV will be under increasing amounts of selective pressure, particularly in the case of widespread distribution of Nirsevimab. We propose that, in addition to surveying for escape mutants in the RSV-F binding site, distal mutations should also be closely monitored, as these adaptations may lead to the emergence of viral resistance. Furthermore, it is crucial to understand that RSV persists and evolves due to imperfect immunity within the population. As highlighted by Grenfell et al., pathogens exposed to incomplete immune responses face selective pressures that drive rapid evolutionary changes52. This concept of imperfect immunity is particularly relevant for RSV, as it creates an environment where the virus can continuously adapt and evade neutralization. We must be vigilant in understanding the mechanisms underlying RSV evolution and adaptation to preserve current prophylactics and ensure the future development of better ones.
Materials and methods
Cell culture
Henrietta Lack’s (HeLa) cells from American Type Culture Collection (ATCC, CCL2) were grown in Dulbecco’s modified Eagle’s medium (DMEM) containing L-glutamine, glucose, and sodium pyruvate with 10% heat-inactivated fetal bovine serum (FBS). Human airway epithelial (1HAEo-) cells (a gift from D.Gruenert, University of California, San Francisco, CA, USA) were grown in minimum essential medium (MEM) supplemented with 10% heat-inactivated FBS. Both immortalized cell lines were grown at 37 °C with 5% CO2.
Reagents, antibodies, antisera, and DNA aptamers
The following reagents were used to stain virally infected cells via our colorimetric immunostaining assay: 0.5 mg/ml X-Gal (5-Bromo-4-chloro-3-indolyl-β-D-galactopyranoside) (Fisher BioReagents™, Cat # BP1615-100) and Yellow Substrate (PBS containing 3 mM potassium ferricyanide III, 3 mM potassium ferrocyanide trihydrate, and 1 mM magnesium chloride hexahydrate). The following commercial antibodies were used: Anti-F (RSV) D25 (human Fc) Antibody (Cambridge Bio, Cat # 01-07-0120), Anti-F (RSV) 101 F (human Fc) Antibody (Cambridge Bio, Cat # 01-07-0140), Goat Anti-RSV Polyclonal Antibody (Meridian Life Science, Cat # B65860G), Rabbit Anti-Goat IgG H&L (β-galactosidase) (Abcam, Cat # ab136712), and Palivizumab (SynagisⓇ). Palivizumab was provided by the Stollery Children’s Hospital neonatal intensive care unit in Edmonton, Alberta, Canada. Infant Anti-RSVA and Anti-RSVB sera, and infant RSV-positive nasopharyngeal samples were kindly provided by Dr. Asuncion Mejias and Dr. Octavio Ramilo from the Nationwide Children’s Hospital in Columbus, Ohio, USA. Pre-fusion stabilized DS-Cav1 WT and L305I proteins and plasmids were kindly provided by Dr. Jason S. McLellan and Dr. Kaci Erwin and generated as previously described22. A new batch of the RSV non-nucleoside polymerase inhibitor was synthesized according to the previously published procedure32,33.
DS-Cav1 protein expression and purification
High-efficiency NEB10-beta competent E.coli cells (New England Biolabs, Cat # C3019H) were transformed according to the NEB protocol using DS-Cav1 WT and L305I DS-Cav1 plasmids, provided by Dr. Jason McLellan. LB+Amp was used for all plates and cultures and all incubations were conducted at 37 °C unless otherwise specified. Single colonies were picked for starter cultures which were then used to inoculate 300 mL for maxi prep recommended protocol using NucleoBond Xtra Maxi EF (Macherey Nagel, Cat # 740424). Endotoxin-free plasmid DNA was sent to Dr. Joanne Lemieux’s lab at the University of Alberta, Edmonton, Canada and her group kindly expressed the protein using the EXPi293 system (Thermo Fisher Scientific) as recommended. Briefly, EXPi293F cells were transfected as per protocol and grown for 5 days before pelleting cells and freezing down the secreted protein found in the media. We confirmed the presence of the DS-Cav1 protein via western blot. The protein was purified on an AKTAstart (Cytiva Life Science, Cat # 29022094) using a HisPur Ni-NTA chromatography cartridge (Thermo Fisher Scientific, Cat # 90099) and an isocratic elution. We concentrated the protein and exchanged the buffer using Amicon Ultra-15, 10 k MWCO (MilliporeSigma, Cat # UFC901024). The final concentration was determined with the Qubit Protein Assay Kit (Invitrogen, Cat # Q33212) and stored at -80 °C in 2 mM Tris, 200 mM NaCl, 0.02% sodium azide.
Virus isolation, propagation, and purification
Clinical samples were tested with a NxTAGⓇ Respiratory Virus Panel (RVP, Luminex, Austin, TX, USA) and samples positive for RSVA or RSVB were subject to further analysis. Clinical strains of RSV were isolated from patient nasopharyngeal samples as previously described9. Briefly, NP samples diluted in 1 mL DMEM + 10% FBS + 1X Penicillin/Streptomycin were added to sub-confluent HeLa cells and incubated at 37 °C with 5% CO2. After 4 h, fresh media was added to the cells and the virus was left to propagate for 96 h. Virus media was harvested and stored in liquid nitrogen. Recombinant lab-adapted strain RSV type-A2 expressing green fluorescent protein (GFP) (rgRSV RW30) was a gift from M.E. Peeples (Children’s Research Institute, Columbus, OH, USA). Lab strain A2 and the RSV L305 mutant were purified by sucrose density gradient purification as described previously9,53. Briefly, the virus was precipitated from conditioned media by stirring with 10% Polyethylene glycol (PEG)-6000 on ice for 90 min. The virus was pelleted by centrifugation at 4300 x g at 4 °C for 30 min, the pellets resuspended in NT buffer (0.15 M NaCl, 0.05 M tris, pH 7.5) and overlaid on a discontinuous sucrose gradient (35%, 45%, 60% sucrose in NT buffer) as previously described. The sucrose-purified RSV band was spun for 4 h at 217,290 × g at 4 °C, harvested, then aliquoted and stored in liquid nitrogen.
Construction of the RSV L305I Mutant
The rgRSV-L305I mutant was constructed by inserting a CTA to ATA mutation at amino acid position 305 into the rgRSV RW30 vector via Gibson Assembly and Cloning54. To clone the RSV-L305I mutant, 6 primers were designed using SnapGene Software, a forward and reverse primer for each of the 3 complementary PCR fragments that were created, with one of the primers containing the CTA to ATA mutation. The online ThermoFisher Multiple Primer Analyzer was used for primer analysis. Each PCR fragment was created separately using the Q5Ⓡ High-Fidelity DNA polymerase protocol. Briefly, dNTPs (NEB, N0446S), template plasmid RSV RW30 DNA, forward and reverse primers, Q5Ⓡ Reaction Buffer (NEB, B9027S) and Q5Ⓡ High-Fidelity DNA polymerase (NEB, M0491S) were combined on ice. PCR reactions were carried out in a thermocycler (Biorad T100) under the following settings: 98 °C for 30 s, [98 °C for 10 s, 55°C for 30 s, 72 °C for 21 s] for 35 cycles, 72 °C for 5 min, and set to hold at 10 °C once the reaction was complete. The sizes of PCR products were confirmed using a 1% agarose gel stained with SYBRⓇ Safe DNA gel stain (ThermoFisher, #S33102). DNA was extracted according to the Qiaex II Gel Extraction Kit (Qiagen, #20051) and purified using the QIAquick PCR purification kit (Qiagen, #28104). The purified products were annealed together using the NEBuilder HiFi DNA Assembly Master Mix and accompanying protocol (NEB, #E2621L) by combining the Master Mix with the purified PCR fragments and incubating them at 50 °C for 15 min in the thermocycler. Annealed viral plasmid DNA was used to transform competent NEB10-beta E.coli (NEB, #C3019) according to the High Efficiency Transformation Protocol (NEB). Briefly, assembled plasmid and competent cells were incubated on ice for 30 min and heat shocked at 42 °C for 30 s, SOC media was added and incubated on a shaker for 1 h at room temperature. Bacteria were plated on YT + 10 µg/mL tetracycline selection plates, incubated overnight at 37 °C, and the following day individual colonies were selected and grown in YT broth overnight at 37 °C. Bacteria were pelleted by centrifugation at 500 x g for 10 mins and plasmid DNA was isolated using the QIAprepⓇ Spin Miniprep Kit (Qiagen, #27106). Extracted plasmid DNA size was confirmed on a 1% agarose gel as described above and plasmids were sent for sequencing to the Molecular Biology Service Unit (MBSU, University of Alberta, Edmonton, AB, Canada) to confirm the presence of the L305I mutation.
RSV reverse genetics
Full length rgRSV RW30 and mutant L305I RW30 cDNA were rescued into infectious virions in HeLa cells. Briefly, full length rgRSV RW30 or RSV-L305I, support plasmids (RSV N, P, L, and M2-1), and T7 RNA polymerase (a gift from Benhur Lee, Addgene plasmid #65974) were transfected into sub-confluent HeLa cells using TransIT-HeLa MONSTER (Mirus Bio, MIR 2900). After rescue, RSV was propagated in HeLa cells in T75 flasks and harvested as cell-free (clarified) RSV-conditioned DMEM with 10% FBS. RSV-conditioned media was aliquoted and stored in liquid nitrogen. The RSV-L305I mutant was used as media-virus and the rgRSV RW30 was further sucrose purified before use in experiments.
Infectious RSV quantification
RSV-infected cells were detected using a colorimetric immunostaining assay as previously described53. Briefly, RSV-infected monolayers were fixed and permeabilized with methanol: acetone (1:1 volume) and incubated for 10 min at RT. Cells were blocked with PBS + 10% FBS and incubated for 30 min at RT. Subsequently, cells were stained with primary goat anti-RSV (diluted 1:1000) and incubated overnight at 4 °C. The following day cells were treated with a secondary rabbit anti-goat antibody conjugated to β-galactosidase (diluted 1:2000) and in the absence of light for 1 h at RT. Cells were then stained blue with 1:1000 X-gal diluted in PBS containing 3 mM potassium ferricyanide III, 3 mM potassium ferrocyanide trihydrate, and 1 mM magnesium chloride hexahydrate and incubated away from light at 37 °C with 5% CO2 for 2–4 h until blue spots were fully developed. Foci of infection stained blue and were counted under the EVOS® Fl Auto Imaging System (ThermoFisher, AMAFD1000). Viral titer was estimated in focus-forming units (FFU/mL). Note that all antibodies were diluted to appropriate concentrations in PBS + 1% FBS and that cells were washed three times with PBS following all blocking and staining treatments unless otherwise specified.
Percent inhibition and EC50 values of human sera and EC50 values for monoclonal antibodies were determined via GFP fluorescence detected by flow cytometry. IgG concentration of all human sera was determined using the Easy-TitreTM IgG (H + L) Assay (Thermo ScientificTM, 23310) and different concentrations of IgG were used in order to achieve a percent inhibition between 20–80%. A4, A50, B18, and B36 sera was used at 15 µg/mL, A5, A13, A164, A29, and B27 sera was diluted to 75 µg/mL, and A7, A10, B22, B24, B28, and B45 was used at 150 µg/mL of IgG antibody. For EC50 curves, A50 and B18 sera were diluted to a starting concentration of 0.07 of the original sample, and subsequently serially diluted 5-fold 7 times. PZMB and 101 F were used at starting concentrations of 1,000,000 ng/mL and D25 started at 100,000 ng/mL due to its increased potency. Monoclonal antibodies were 10-fold serially diluted 8 times. Antibodies and sera were incubated with RSV WT or RSV L305I at an MOI of 0.25 (for monoclonal antibodies) or 0.3 (for human sera) for 1 h. Sub-confluent HeLa cells grown in DMEM + 10% FBS + 1X P/S were infected with the virus antibody dilutions in 12-well (monoclonals) or 48-well (human sera) plates. 4 h post infection fresh media was added to cells. 24 h post-infection cells were prepared for flow cytometry by treatment with a 1:1000 dilution of Ghost DyeTM Violet 450 (Cytek, 13-0863) for 30 min. Viral infection was indicated by GFP fluorescence and percent inhibition was determined by comparison to an antibody-free control group in each experiment. Flow cytometry was conducted using the BD LSRFortessa X-20 (BD Biosciences). B530 and V450 lasers were used to detect GFP and live-dead stains respectively. Flow analysis was completed using FLOWJO software (BD Biosciences) and final EC50 values, curves, and statistics were evaluated using GraphPad Prism.
Growth curves and infectivity assay
To conduct the one step growth curve RSV-WT or RSV-L305I were used to infect HeLa cells at an MOI of 0.25. Every 6 h for 96 h media was collected from the infected cells and replaced with fresh DMEM + 10% FBS +1x P/S. Viral transcripts released in the collected media were determined by RT-qPCR using primers targeting the RSV-N gene. To test infectivity differences between RSV-WT vs RSV-L305I we conducted a progeny assay. Subconfluent HeLa cells were infected at an MOI of 0.3 and every 24 h media was collected from infected cells and subsequently replaced with fresh media. The collected media was serially diluted and placed on new indicator HeLa cells. Infection was allowed to proceed for 24 h and infected cells were subsequently stained using our colorimetric immunostaining assay. Focal forming units were determined and back calculated to determine the number of viral particles released. To visually observe viral spread, HeLa cells were infected with 100ffus of RSV-WT or RSV-L305I and observed over 96 h. Every 24 h cells were fixed and stained using our colorimetric immunostaining assay and imaged with the EVOS M7000 (Thermo ScientificTM, AMF7000HCA). Each section of the 48 well was imaged at 10X and all frames were stitched together to produce the final images.
RSV evolution experiment
Evolution experiments were done as previously described in ref. 33. Briefly, sub-confluent HeLa cells were infected at an MOI of 0.5 with lab strain rgRSV-A2 and incubated with commercial anti-RSV polyclonal goat sera at a 1:1000 dilution, RSV polymerase inhibitor (compound 5 f) at 10 µM and 25 µM diluted in DMSO, or 0.25% DMSO. 4 h post-infection, fresh media containing the same antibody or drug, was added to the cells and the infection was allowed to proceed at 37 °C and 5% CO2. After 48 h, virus-conditioned media was clarified, and a portion was used to infect a new HeLa cell monolayer in the presence of an antibody or drug again to repeat the process. Virus was passaged every two days for 40 days for a total of 20 passages. RNA was harvested from every passage and viral growth was measured by qRT-PCR and a foci counting assay to test infectivity.
Whole genome sequencing
Whole genome sequencing was done as described9. Briefly, viral RNA from each passage of the evolution experiment was extracted using the QIAamp® Viral RNA Mini Kit (Qiagen, 52906). Viral mRNA was isolated by poly-A pulldown with oligo d(T) 25 beads using binding the NEBNext® Poly(A) mRNA Magnetic Isolation Module (NEB, E7490L). The first strand of cDNA was prepared using the High-Capacity cDNA RT Kit (ThermoFisher, 4368814), and the second strand was synthesized with the large Klenow fragment of DNA polymerase 1 (NEB, M0210L). cDNA was purified with the MinEluteTM PCR Purification Kit (Qiagen, 28004). Tagmentation and creation of the library were done using the Nextera XT DNA Library Preparation Protocol (Illumina, FC-131-1096). Index adapters used for sample identification were created by MBSU (Molecular Biology Service Unit, University of Alberta, Edmonton, AB, Canada) and libraries were cleaned up using the MagJET NGS Cleanup Kit (ThermoFisher, K2821). Sample concentration was checked using the NanoDrop TM 8000 Spectrophotometer (ThermoFisher, ND-8000-GL) and sample purity analyzed by the Agilent 2100 Bioanalyzer G2938C (Marshall Scientific, AG-2100C) at the MBSU. Equal amounts of DNA were combined and sent for sequencing to the MBSU for Next Generation Sequencing on the MiSeq® System (Illumina, SY-410–1003).
Surface plasmon resonance
Experiments were performed using the Biacore T200 Surface Plasmon Resonance System (Cytiva, 28975001). Monoclonal antibody binding affinity was determined using His-tag coupling. The kinetics protocol is as follows: NTA chip was Ni2+ activated according to the Series S NTA Sensor Chip protocol (Cytiva, BR100532). Prefusion-stabilized RSV-F DS-Cav1L305 and DS-Cav1I305 proteins (diluted to 0.1 μg/mL were injected onto the chip at 5 μL/min for 60 s. Antibody dilutions were run at 30 μL/min for 180 s, and dissociation was measured over 800 s. HBS-P (pH 7.4) supplemented with 50 µM EDTA was used as a running buffer and each antibody concentration was run in at least duplicate. 350 mM EDTA was used for chip regeneration at 10 µL/min for 60 s three times. Bivalent IgG monoclonal antibodies were 3-fold serially diluted 8 times in the running buffer from a starting concentration of 100 nM. An empty inactivated flow lane was used for double reference subtraction and curves were fit to a 1:1 binding model in Biacore Insight Evaluation Software (Cytiva). Final curves were created in GraphPad Prism.
Determining the % identity and similarity of RSV isolates
Amino acid identity and similarity between RSVA and B were determined using Geneious software, Biomatters, New Zealand.
Aligning multiple clinical isolates of RSV and determining aa differences in RSV-F protein
5141 RSV-F protein sequences were downloaded from the NIAID Virus Pathogen Database and Analysis Resource (ViPR)55 through the web site at http://www.viprbrc.org/. SeqKit56 was then used to filter the RSV-F sequences to include only sequences that are the correct length (574 amino acids), and are identified as RSV type-A or RSV type-B. After this filtering, 3747 sequences remained – 2313 RSV type-A (61.7%) and 1434 RSV type-B (38.3%). The RSV type-A sequences and type-B sequences were aligned separately and together using Clustal Omega57 with default settings and analyzed using Jalview 2.11.1.458. Amino acids with at least 65% greater conservation for both RSV type-A and type-B compared to the combined alignment were marked as being conserved by RSV type.
Protein preparation from molecular dynamics simulations
Starting coordinates for the RSV-F protein were obtained from the Protein Data Bank for both the monomer (PDB accession: 4MMU) and the protomer (PDB accession: 5UDC). The X-ray structure of the protomer was solved with bound MEDI8897, which was removed to obtain the free protomer. Mutation at residue 305 was performed using the Schrödinger Small Molecule Discovery Suite. The Protein Preparation Wizard module in Schrödinger was used to add hydrogen atoms, minimize energy, fill missing loops, and create the appropriate protonation states of amino acid side chains. The protein structure was then subjected to three stages of energy minimization, all of which utilized the OPLS3 force field59.
Molecular dynamics simulations of the RSV-F
The structures of RSV-F protein were solvated in a cuboidal box of TIP3P water molecules using AMBER’s tLEaP tool60. The ff14SB parameters were assigned for the protein. The complexes were then neutralized and solvated in a NaCl salt concentration of 0.15 M with tLEaP using the same process described above. The simulations were performed using PMEMD in AMBER1861. An initial minimization step was performed in order to relax the water and ionic positions. The whole system was then minimized and heated gradually up to 300 K in 100 ps using Langevin dynamics. During the heating process, we restrained the backbone of the protein, and a time step of 0.5 fs and periodic volume conditions were employed during this phase. The time step has been set to 2 fs, and periodic pressure conditions (1 atm) have been imposed and the restraints have been gradually released in four phases of 50 ps each. The production phase of the simulations at the NPT conditions was performed in triplicates for 100, 270, and 500 ns using GPU accelerated version of PMEMD (pmemd. cuda) implemented in AMBER 1860.
Structural analysis of molecular dynamics simulations
The CPPTRAJ software in AMBER18 was used to compute the root mean squared deviation (RMSD) of the protein coordinates with respect to the reference X-ray structure along the MD trajectories. The coordinates of the models were also clustered using CPPTRAJ with the average-linkage clustering algorithm62.
Statistical analysis
Statistical analysis was done using GraphPad Prism 9 software. Unless otherwise indicated, results are expressed as mean±s.d. Group means were compared by either two-tailed Student’s t-tests or one-way analysis of variance (ANOVA) with Tukey’s post hoc analysis, comparing each group with the appropriate control. All tests are two-tailed unless otherwise indicated. We considered a P value ≤ 0.05 to be statistically significant.
Data availability
The sequences generated in this study were submitted to the GenBank database (accession numbers PV460586-PV460601). The modeling data and other data generated during this study are included in this manuscript and its supplementary information files.
References
Li, Y. et al. Global, regional, and national disease burden estimates of acute lower respiratory infections due to respiratory syncytial virus in children younger than 5 years in 2019: a systematic analysis. Lancet 399, 2047–2064 (2022).
Busack, B. & Shorr, A. F. Going Viral-RSV as the Neglected Adult Respiratory Virus. Pathogens 11 https://doi.org/10.3390/pathogens11111324 (2022).
Caserta, M. T., O’Leary, S. T., Munoz, F. M., Ralston, S. L. & Committee On Infectious, D. Palivizumab Prophylaxis in Infants and Young Children at Increased Risk of Hospitalization for Respiratory Syncytial Virus Infection. Pediatrics 152 https://doi.org/10.1542/peds.2023-061803 (2023).
Phuah, J. Y. et al. Quantification of clesrovimab, an investigational, half-life extended, anti-respiratory syncytial virus protein F human monoclonal antibody in the nasal epithelial lining fluid of healthy adults. Biomed. Pharmacother. 169, 115851 (2023).
Kampmann, B., Radley, D. & Munjal, I. Bivalent Prefusion F Vaccine in Pregnancy to Prevent RSV Illness in Infants. Reply. N. Engl. J. Med 389, 1053–1055 (2023).
Melgar, M. et al. Use of Respiratory Syncytial Virus Vaccines in Older Adults: Recommendations of the Advisory Committee on Immunization Practices - United States, 2023. Am. J. Transpl. 23, 1631–1640 (2023).
Griffiths, C., Drews, S. J. & Marchant, D. J. Respiratory Syncytial Virus: Infection, Detection, and New Options for Prevention and Treatment. Clin. Microbiol Rev. 30, 277–319 (2017).
Zlateva, K. T., Lemey, P., Moes, E., Vandamme, A. M. & Van Ranst, M. Genetic variability and molecular evolution of the human respiratory syncytial virus subgroup B attachment G protein. J. Virol. 79, 9157–9167 (2005).
Elawar, F. et al. A Virological and Phylogenetic Analysis of the Emergence of New Clades of Respiratory Syncytial Virus. Sci. Rep. 7, 12232 (2017).
Yu, J. M., Fu, Y. H., Peng, X. L., Zheng, Y. P. & He, J. S. Genetic diversity and molecular evolution of human respiratory syncytial virus A and B. Sci. Rep. 11, 12941 (2021).
Elawar, F. et al. Pharmacological targets and emerging treatments for respiratory syncytial virus bronchiolitis. Pharm. Ther. 220, 107712 (2021).
Utokaparch, S. et al. The relationship between respiratory viral loads and diagnosis in children presenting to a pediatric hospital emergency department. Pediatr. Infect. Dis. J. 30, e18–e23 (2011).
Rebuffo-Scheer, C. et al. Whole genome sequencing and evolutionary analysis of human respiratory syncytial virus A and B from Milwaukee, WI 1998-2010. PLoS One 6, e25468 (2011).
Johnson, P. R., Spriggs, M. K., Olmsted, R. A. & Collins, P. L. The G glycoprotein of human respiratory syncytial viruses of subgroups A and B: extensive sequence divergence between antigenically related proteins. Proc. Natl. Acad. Sci. USA 84, 5625–5629 (1987).
Simoes, E. A. F. et al. Suptavumab for the Prevention of Medically Attended Respiratory Syncytial Virus Infection in Preterm Infants. Clin. Infect. Dis. 73, e4400–e4408 (2021).
McLellan, J. S. Neutralizing epitopes on the respiratory syncytial virus fusion glycoprotein. Curr. Opin. Virol. 11, 70–75 (2015).
McLellan, J. S. et al. Structure-based design of a fusion glycoprotein vaccine for respiratory syncytial virus. Science 342, 592–598 (2013).
McLellan, J. S. et al. Structure of RSV fusion glycoprotein trimer bound to a prefusion-specific neutralizing antibody. Science 340, 1113–1117 (2013).
McLellan, J. S., Yang, Y., Graham, B. S. & Kwong, P. D. Structure of respiratory syncytial virus fusion glycoprotein in the postfusion conformation reveals preservation of neutralizing epitopes. J. Virol. 85, 7788–7796 (2011).
Griffiths, C. D. et al. IGF1R is an entry receptor for respiratory syncytial virus. Nature 583, 615–619 (2020).
Hayes, R. S., Oraby, A. K., Camargo, C., Marchant, D. J. & Sagan, S. M. Mapping respiratory syncytial virus fusion protein interactions with the receptor IGF1R and the impact of alanine-scanning mutagenesis on viral infection. J. Gen. Virol. 105 https://doi.org/10.1099/jgv.0.001951 (2024).
McLellan, J. S., Ray, W. C. & Peeples, M. E. Structure and function of respiratory syncytial virus surface glycoproteins. Curr. Top. Microbiol. Immunol. 372, 83–104 (2013).
Bin, L. et al. Emergence of new antigenic epitopes in the glycoproteins of human respiratory syncytial virus collected from a US surveillance study, 2015-17. Sci. Rep. 9, 3898 (2019).
McCool, R. S. et al. Vaccination with prefusion-stabilized respiratory syncytial virus fusion protein elicits antibodies targeting a membrane-proximal epitope. J. Virol. 97, e0092923 (2023).
Beeler, J. A. & van Wyke Coelingh, K. Neutralization epitopes of the F glycoprotein of respiratory syncytial virus: effect of mutation upon fusion function. J. Virol. 63, 2941–2950 (1989).
Mas, V., Nair, H., Campbell, H., Melero, J. A. & Williams, T. C. Antigenic and sequence variability of the human respiratory syncytial virus F glycoprotein compared to related viruses in a comprehensive dataset. Vaccine 36, 6660–6673 (2018).
Rezende, W., Neal, H. E., Dutch, R. E. & Piedra, P. A. The RSV F p27 peptide: current knowledge, important questions. Front. Microbiol. 14, 1219846 (2023).
Rezende, W. et al. The Efficiency of p27 Cleavage during In Vitro Respiratory Syncytial Virus (RSV) Infection Is Cell Line and RSV Subtype Dependent. J. Virol. 97, e0025423 (2023).
Jones, H. G. et al. Alternative conformations of a major antigenic site on RSV F. PLoS Pathog. 15, e1007944 (2019).
Mukhamedova, M. et al. Vaccination with prefusion-stabilized respiratory syncytial virus fusion protein induces genetically and antigenically diverse antibody responses. Immunity 54, 769–780 e766 (2021).
Zhao, X., Chen, F. P. & Sullender, W. M. Respiratory syncytial virus escape mutant derived in vitro resists palivizumab prophylaxis in cotton rats. Virology 318, 608–612 (2004).
Atienza, B. J. P. et al. Dual Catalytic Synthesis of Antiviral Compounds Based on Metallocarbene-Azide Cascade Chemistry. J. Org. Chem. 83, 6829–6842 (2018).
Oraby, A. K., Bilawchuk, L., West, F. G. & Marchant, D. J. Structure-Based Discovery of Allosteric Inhibitors Targeting a New Druggable Site in the Respiratory Syncytial Virus Polymerase. ACS Omega 9, 22213–22229 (2024).
Hashimoto, K. & Hosoya, M. Neutralizing epitopes of RSV and palivizumab resistance in Japan. Fukushima J. Med. Sci. 63, 127–134 (2017).
Hause, A. M. et al. Sequence variability of the respiratory syncytial virus (RSV) fusion gene among contemporary and historical genotypes of RSV/A and RSV/B. PLoS One 12, e0175792 (2017).
Gilman, M. S. A. et al. Transient opening of trimeric prefusion RSV F proteins. Nat. Commun. 10, 2105 (2019).
Krarup, A. et al. A highly stable prefusion RSV F vaccine derived from structural analysis of the fusion mechanism. Nat. Commun. 6, 8143 (2015).
Che, Y. et al. Rational design of a highly immunogenic prefusion-stabilized F glycoprotein antigen for a respiratory syncytial virus vaccine. Sci. Transl. Med. 15, eade6422 (2023).
Lee, Y. Z. et al. Rational design of uncleaved prefusion-closed trimer vaccines for human respiratory syncytial virus and metapneumovirus. Nat. Commun. 15, 9939 (2024).
Techaarpornkul, S., Barretto, N. & Peeples, M. E. Functional analysis of recombinant respiratory syncytial virus deletion mutants lacking the small hydrophobic and/or attachment glycoprotein gene. J. Virol. 75, 6825–6834 (2001).
Techaarpornkul, S., Collins, P. L. & Peeples, M. E. Respiratory syncytial virus with the fusion protein as its only viral glycoprotein is less dependent on cellular glycosaminoglycans for attachment than complete virus. Virology 294, 296–304 (2002).
Kim, Y. I. et al. Relating plaque morphology to respiratory syncytial virus subgroup, viral load, and disease severity in children. Pediatr. Res. 78, 380–388 (2015).
Rijsbergen, L. C. et al. Human Respiratory Syncytial Virus Subgroup A and B Infections in Nasal, Bronchial, Small-Airway, and Organoid-Derived Respiratory Cultures. mSphere 6 https://doi.org/10.1128/mSphere.00237-21 (2021).
Capella, C. et al. Prefusion F, Postfusion F, G Antibodies, and Disease Severity in Infants and Young Children With Acute Respiratory Syncytial Virus Infection. J. Infect. Dis. 216, 1398–1406 (2017).
Zhao, X., Chen, F. P., Megaw, A. G. & Sullender, W. M. Variable resistance to palivizumab in cotton rats by respiratory syncytial virus mutants. J. Infect. Dis. 190, 1941–1946 (2004).
Zhu, Q. et al. A highly potent extended half-life antibody as a potential RSV vaccine surrogate for all infants. Sci. Transl. Med. 9 https://doi.org/10.1126/scitranslmed.aaj1928 (2017).
Wilkins, D. et al. Nirsevimab binding-site conservation in respiratory syncytial virus fusion glycoprotein worldwide between 1956 and 2021: an analysis of observational study sequencing data. Lancet Infect. Dis. 23, 856–866 (2023).
McLellan, J. S. et al. Structure of a major antigenic site on the respiratory syncytial virus fusion glycoprotein in complex with neutralizing antibody 101F. J. Virol. 84, 12236–12244 (2010).
Tang, A. et al. A potent broadly neutralizing human RSV antibody targets conserved site IV of the fusion glycoprotein. Nat. Commun. 10, 4153 (2019).
Grad, Y. H. et al. Within-host whole-genome deep sequencing and diversity analysis of human respiratory syncytial virus infection reveals dynamics of genomic diversity in the absence and presence of immune pressure. J. Virol. 88, 7286–7293 (2014).
Wu, E. Y. et al. A conservative isoleucine to leucine mutation causes major rearrangements and cold sensitivity in KlenTaq1 DNA polymerase. Biochemistry 54, 881–889 (2015).
Grenfell, B. T. et al. Unifying the epidemiological and evolutionary dynamics of pathogens. Science 303, 327–332 (2004).
Bilawchuk, L. M., Griffiths, C. D., Jensen, L. D., Elawar, F. & Marchant, D. J. The Susceptibilities of Respiratory Syncytial Virus to Nucleolin Receptor Blocking and Antibody Neutralization are Dependent upon the Method of Virus Purification. Viruses 9 (2017). https://doi.org/10.3390/v9080207
Gibson, D. G. et al. Enzymatic assembly of DNA molecules up to several hundred kilobases. Nat. Methods 6, 343–345 (2009).
Pickett, B. E. et al. ViPR: an open bioinformatics database and analysis resource for virology research. Nucleic Acids Res.40, D593–D598 (2012).
Shen, W., Le, S., Li, Y. & Hu, F. SeqKit: A Cross-Platform and Ultrafast Toolkit for FASTA/Q File Manipulation. PLoS One 11, e0163962 (2016).
Madeira, F. et al. The EMBL-EBI search and sequence analysis tools APIs in 2019. Nucleic Acids Res. 47, W636–W641 (2019).
Waterhouse, A. M., Procter, J. B., Martin, D. M., Clamp, M. & Barton, G. J. Jalview Version 2-a multiple sequence alignment editor and analysis workbench. Bioinformatics 25, 1189–1191 (2009).
Harder, E. et al. OPLS3: A Force Field Providing Broad Coverage of Drug-like Small Molecules and Proteins. J. Chem. Theory Comput 12, 281–296 (2016).
Case, D. A. et al. AmberTools. J. Chem. Inf. Model 63, 6183–6191 (2023).
Case, D. A. et al. The Amber biomolecular simulation programs. J. Comput. Chem. 26, 1668–1688 (2005).
Roe, D. R. & Cheatham, T. E. PTRAJ and CPPTRAJ: Software for Processing and Analysis of Molecular Dynamics Trajectory Data. J. Chem. Theory Comput. 9, 3084–3095 (2013).
Acknowledgements
We would like to thank the University of Alberta Faculty of Medicine and Dentistry Flow Cytometry Facility (RRID:SCR_019195) which receives financial support from the Faculty of Medicine & Dentistry and the Canada Foundation for Innovation (CFI) awards to contributing investigators. We would also like to thank Bart Hazes (University of Alberta) for his bioinformatics expertise with evolution experiments and helpful discussions. The Digital Research Alliance of Canada (alliancecan.ca) is thanked for the computational resources. This study was supported in part by the Alberta Ministry of Technology and Innovation through SPP-ARC (Striving for Pandemic Preparedness - The Alberta Research Consortium). A.S. and M.G. are supported by CIHR Canada Graduate Scholarships - Doctoral Program award (A.S. FRN: 514839) (M.G. FRN: 193297). This research was also funded by Stollery Children’s Hospital Foundation through the Women and Children’s Health Research Institute.
Author information
Authors and Affiliations
Contributions
A.K.O., A.S., F.E. and D.J.M. conceived the study. AKO; wrote manuscript and designed and performed the computational study, A.S.; wrote manuscript and performed most experiments, F.E.; performed experiments and initiated the study, L.M.B.; did experiments and helped write manuscript, RDM; analyzed experiments and helped to write manuscript, K.E.; made the L305I DS-CAV1 and expressed the protein, M.J.G.; helped to write manuscript and analyzed experiments, C.D.G. ;analyzed data and helped to write manuscript, J.D.F.; helped to write manuscript and analyzed data, E.A.;designed and conducted experiments, MJL; analyzed data and helped to write manuscript, F.G.W.; helped to write manuscript and design experiments, O.R.; provided human samples and designed experiments and analyzed data, A.M.; provided human samples and designed experiments and analyzed data, J.S.M.; designed experiments and analyzed data and helped to write the manuscript, D.M.; supervised the study, designed experiments and wrote the manuscript. All authors reviewed and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Oraby, A.K., Stojic, A., Elawar, F. et al. A single amino acid mutation alters multiple neutralization epitopes in the respiratory syncytial virus fusion glycoprotein. npj Viruses 3, 33 (2025). https://doi.org/10.1038/s44298-025-00119-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s44298-025-00119-8