Abstract
Aplastic anemia (AA) is a life-threatening bone marrow (BM) failure syndrome characterized by pancytopenia. Recent studies revealed that dysfunctional endothelial progenitor cells (EPCs), critical components of the BM microenvironment, are involved in hematopoietic-dysfunction-related diseases, including AA. However, the mechanism underlying EPC damage in AA remains unknown. Here we find that transforming growth factor-β (TGF-β) signaling is hyperactive in dysfunctional AA EPCs with impaired hematopoietic support and immune regulatory ability, and TGF-β inhibition promotes hematopoiesis and immune rebalance by repairing dysfunctional EPCs. Through impaired EPC and AA murine models, we validated that TGF-β inhibition restores EPC dysfunction to improve hematopoiesis and immune status in vitro and in vivo. RNA sequencing and real-time quantitative polymerase chain reaction provided further validation. These results indicate that dysfunctional BM EPCs with hyperactive TGF-β signaling are involved in AA. TGF-β inhibition promotes multilineage hematopoiesis recovery and immune balance by repairing dysfunctional EPCs, providing a potential therapeutic strategy for AA.

Similar content being viewed by others
Introduction
Aplastic anemia (AA) is a rare but life-threatening disease characterized by peripheral pancytopenia due to multilineage hematopoietic deficiency1,2. Accumulating evidences suggest that the pathogenesis of AA is manifold and involves T-cell-mediated immune destruction3,4, intrinsic defects in hematopoietic stem cells (HSCs)5 and that an impaired bone marrow (BM) microenvironment contributes to diminished hematopoietic capacity6. Effective treatments for severe AA are immunosuppressive therapies but with variable responsiveness7 or allogenic HSC transplantation (allo-HSCT) but with age restrictions8. As a complement, in-depth exploration of BM microenvironment may be a potential direction for AA amelioration.
Endothelial progenitor cells (EPCs) are crucial components of the BM microenvironment and regulate HSC fate and immune balance under physiological conditions or after myeloablation9,10,11,12,13. Conditional deletion of EPC-specific receptor (vascular endothelial growth factor receptor 2, VEGFR2) prevented EPC regeneration and hematopoiesis reconstitution in irradiated mice14, whereas infusion of EPCs can improve HSC and immune reconstitution in vivo12,15,16, which indicates that BM EPCs are essential to support hematopoiesis. EPCs also fulfill immunoregulation as a T cell mobilizer by production of chemokines17 or as novel innate immune cells with antigen presentation18. Moreover, dysregulated expansion of T helper 1 (TH1), T helper 2 (TH2) and T helper 17 (TH17) cells, whereas reduced or dysfunctional regulatory T cells (Treg) are consistent features of severe AA4. Expansion of B cells was also reported in patients with AA19. Mutually, anti-inflammatory angiogenic factors produced by EPCs can weaken T cell proliferation and alter T cell activation20,21. Recently, we reported that reactive oxygen species (ROS)-induced dysfunctional BM EPCs interfere with the self-renewal and differentiation of HSCs in multiple hematopoietic-dysfunction-related diseases, including corticosteroid-resistant immune thrombocytopenia, AA, myelodysplastic neoplasms (MDS) and poor hematopoietic reconstitution after allo-HSCT in vitro and in vivo6,22,23,24,25,26,27. Clinically, we conducted an open-label, randomized, phase III trial reinforced that hematopoietic reconstitution can be improved by repairing dysfunctional BM EPCs with N-acetyl-L-cysteine (a ROS scavenger) after allo-HSCT28. In addition, ROS-induced damage to the BM EPCs of mice and pateints with AA disabled not only their hematopoietic support function but also their immunoregulatory function6. However, how dysfunctional EPCs affect hematopoiesis and immunoregulation during the development of AA is not completely understood.
Transforming growth factor-β (TGF-β), an inflammatory cytokine produced primarily by HSC-adjacent niche cells such as Schwann cells and megakaryocytes attached around vessels, is an important component of the BM microenvironment29,30,31. Initially, TGF-β was considered a cardinal regulator that provides a quiescence signal to HSCs during homeostatic conditions32,33,34. However, accumulating evidences suggest that the effects of TGF-β on HSCs are more complex than previously thought. Different hematopoietic stem and progenitor cells (HSPC) respond differently to TGF-β1 in a stage-specific and dose-dependent manner35,36,37. High-dose TGF-β1 can arrest megakaryoblast maturation and erythroblast proliferation but augment lymphopoiesis29,38,39. Uniformly, the Smad2/3 circuitry downstream of TGF-β pathway is constitutively increased in erythroid progenitors of patients or disease models with ineffective erythropoiesis, such as MDS40,41 and β-thalassemia42,43. The clinical benefit of TGF-β superfamily ligand trap (luspatercept) for ineffective erythropoiesis is promising44,45,46,47,48. Moreover, recent research has confirmed that hyperactive TGF-β signaling in HSPCs contributes to BM failure in Fanconi anemia49 and Shwachman–Diamond syndrome50. Existing studies have primarily focused on the direct effects of TGF-β on hematopoietic cells, where it plays a crucial role in regulating HSCs by inducing quiescence and maintaining genomic stability49,50,51,52,53,54. However, its impact on EPC-mediated hematopoiesis has not been investigated in patients with BM disorders. Even though reports implicated that TGF-β induces apoptosis and prevents the proliferation of endothelial cells (ECs)55,56. Moreover, the role of TGF-β signaling in ECs is heterogeneous and pleiotropic57,58,59. TGF-β signaling either stimulates vascular formation or hampers biological function of vascular ECs, especially in their abilities of proliferation, migration and vessel maturation59,60. Thus, it raised our interest in whether activation of TGF-β signaling pathway in BM EPCs would perturb their regulation of hematopoietic support and immune balance in patients with AA.
In this study, we found that Smad2/3 signaling occurred in response to increased levels of TGF-β1 binding with type I TGFβ receptor (TGF-βRI) in BM EPCs from patients with AA compared with those from normal controls (NCs), which not only impeded erythropoiesis, megakaryopoiesis and myelopoiesis but also disrupted T cell differentiation. Furthermore, the hematopoiesis-supporting ability and immune-modulation function of BM EPCs were restored after TGF-β inhibition in vitro and in vivo. Together, these data suggest that TGF-β inhibition might be a promising approach for improving the prognosis of patients with AA.
Materials and methods
Patients and controls
Patients with AA (N = 15, aged 21–61 years with a median age of 54 years) and age-matched NCs (N = 15, aged 24–64 years with a median age of 53 years) were enrolled in this prospective case‒control study. There were no significant differences between the ages of patients with AA and NCs (Supplementary Table 1).
The Ethics Committee of Peking University People’s Hospital approved the study (2022PHB037-001), and all the subjects signed written informed consent in accordance with the Declaration of Helsinki.
Isolation, cultivation and characterization of human primary BM EPCs
As previously reported6,22,23,24,25,26,27, BM mononuclear cells (BMMNCs) were separated with lymphocyte separation medium (GE Healthcare) and cultivated for 7 days. The identification of BM EPCs was performed with mouse anti-human CD45 (BD Biosciences), CD34 (BioLegend), VEGFR2 (CD309) (BD Biosciences) and CD133 (Miltenyi Biotec) monoclonal antibodies through flow cytometry via BD LSRFortessa (Becton Dickinson).
Measurement of the levels of TGF-β1, TGF-βRI and p-Smad2/3 and the apoptosis ratio in BM EPCs and T cell subsets
After isolation from BMMNCs, the protein levels of TGF-β1 (BD Biosciences), TGF-βRI (Abcam) and phospho-Smad 2/3 (p-Smad2/3) (BD Biosciences) in BM EPCs were evaluated via flow cytometry. The cultivated BM EPCs were incubated with Annexin-V (BioLegend) and 7-amino-actinomycin D (7-AAD; BD Biosciences) to assess the apoptosis ratio of BM EPCs, which was measured via flow cytometry. As previously reported22,24,61,62, the apoptosis ratio includes the total percentage of early apoptosis cells(AnnexinV+7-AAD−) and late apoptosis cells (AnnexinV+7-AAD+), while live cells were defined as AnnexinV−7-AAD−. After 3 days of coculture, CD3+ T cells were collected and stimulated with a cocktail (eBioscience). The frequencies of different types of T cell were evaluated as previously reported6,25.
Tube formation, migration and double-positive staining assays
The functions of EPCs were evaluated through tube formation, migration and double-positive staining assays following the published protocol6,22,23,24,25,26,27,34. After 7 days of cultivation, 4 × 104 BM EPCs were seeded in Matrigel-coated (Corning) plates for 24 h. As previously reported6,22,23,24,26,27,34,63,64,65,66,67, tube formation was observed using a phase contrast microscope (Olympus). Three random fields were photographed in each group. The capillary tube length was calculated by drawing a line along each tube and measuring the length of the line in pixels using the ImageJ software. A total of 1 × 105 BM EPCs were placed in the upper chambers (Corning) for 24 h to evaluate the number of migrated cells. A total of 1 × 105 BM EPCs were stained with both diI-acetylated low-density lipoprotein (DiI-Ac-LDL) (Life Technologies) and fluorescein isothiocyanate-labeled UEA-1 (FITC-UEA-1) (Sigma) to evaluate the number of double-positive BM EPCs. All the cells were counted in three random fields.
Coculture assays of EPC–HSC and EPC–T cell
The BM CD34+ cells were isolated from NC BMMNCs with CD34+ MicroBead kits (Miltenyi Biotec)6,22,23,24,25,26,27,68. The isolated HSCs derived from NCs (1 × 105 per well) were cocultured with precultivated BM EPCs in StemSpan Serum-Free Expansion Medium (Stem Cell Technologies) for 5 days (Supplementary Fig. 1a). In addition, the BM CD3+ cells sorted from NC BMMNCs via CD3+ MicroBead kitsc (Miltenyi Biotec) were cocultured directly with precultivated BM EPCs in RPMI 1640 medium (Gibco) supplemented with 10% fetal bovine serum (Gibco) for 3 days6,25.
EdU assay
After the coculture experiment of HSCs with BM EPCs, the HSCs were separately incubated with 50 μM 5-ethynyl-20-deoxyuridine (EdU) (RiboBio) for 24 h. The nuclear fluorescence intensity of the HSCs was evaluated via flow cytometry to investigate their proliferation ability of HSCs25,69.
CFU assays
The hematopoiesis-supporting ability of EPCs was assessed via colony-forming unit (CFU) assays. A total of 1 × 105 BM CD34+ cells from NCs were sorted via CD34+ microbead kits (Miltenyi Biotec) and then were performed direct-coculture assay with primary EPCs from patients with AA or NCs. After 5 days, the HSCs were collected and seeded in a 24-well plate (Corning) using MethoCult H4434 Classic (Stem Cell Technologies) for 14 days. The CFU erythroid (CFU-E), burst-forming unit erythroid (BFU-E), CFU granulocyte–macrophage (CFU-GM) and CFU granulocyte, erythroid, macrophage and megakaryocyte (CFU-GEMM) were scored as previously described6,22,23,24,26,27.
Establishment of a BM EPC damage model in vitro
To establish the BM EPC damage model, the primary BM EPCs derived from NCs were treated with TGF-β1 (4 nM ml−1, PeproTech) in vitro for 24 h (ref. 70). To further determine the effect of TGF-β pathway inhibition on damaged EPC function, the EPCs were treated with TGF-β1 plus the TGF-βRI inhibitor galunisertib (LY2157299, LY, 75 nM ml−1, Selleck)71.
Establishment of a classical AA murine model
The classical AA murine model was established as previously reported3,6,72,73. Hybrid (BALB/cBy × C57BL/6(B6)) F1 (CByB6F1) mice were treated with 5 Gy total-body irradiation (TBI) and then intravenously injected with allogeneic lymph nodes (5 × 106 per mouse) from B6 mice 4‒6 h later on day 0. The B6 and CByB6F1 mice between 8 and 10 weeks of age were purchased from Beijing Vitalstar Biotechnology and bred there. The animal studies were approved by the Ethics Committee of Peking University People’s Hospital (2022PHE008).
Treatment of AA mice with a TGF-βRI inhibitor
The TBI group and TBI and lymph nodes infusion group were orally administered LY (100 mg kg−1 per day) on days 1, 3, 5, 7, 9, 11 and 12. An equal volume of dimethyl sulfoxide (Sigma-Aldrich) was given to the untreated group at the same time.
On day 13, retroorbital blood was collected from the mice and used to analyze the number of blood cells with an automated hematology analyzer (Sysmex Corporation). The mice were euthanized to collect BM cells and femur tissues on day 14. The femur tissues were fixed in 4% paraformaldehyde and then separately stained with hematoxylin‒eosin and the EC marker endomucin (Santa Cruz Biotechnology) for immunohistochemistry to assess the percentages of different types of BM vessel and BM hematopoietic volume. In addition, the BM cells were collected to determine the cell counts of hematopoietic cells per million cells in BM, frequencies of myeloid cells (CD45+Gr-1+), B cells (CD45+CD3−B220+) and T cells (CD45+CD3+B220−)(Supplementary Fig. 1f) and the percentages of different types of T cell in the murine BM through flow cytometry26,27.
Bulk RNA sequencing and data analysis
The BM EPCs derived from patients with AA (N = 4) and NCs (N = 4) were subjected to RNA sequencing (RNA-seq) analysis. Next-generation RNA-seq libraries were generated with the NEBNext Ultra II RNA Library Prep Kit (NEB, E7770S). The paired-end sequencing was performed on a NovaSeq 6000 (Illumina), which produced between 28 and 35 million 150-bp paired-end reads per sample. The raw FASTQ files were processed according to a previously described method and with modifications68,74,75,76. After removing low-quality reads and adapter sequences, the remaining reads were quantified against the SAF genome index (GRCh38 reference) at the transcript level using Salmon software in mapping-based mode and aggregated at the gene level using the R package tximport. The count values were calculated for differentially expressed genes (DEGs) with the R packages DESeq2 and IHW. The DEGs with weighted P values <0.05 and the absolute of a fold change(log2) >0.5 were used for Kyoto Encyclopedia of Genes and Genomes (KEGG) enrichment analysis using R package clusterProfiler.
qRT‒PCR
The mRNA levels of FLT3LG, KIT, FLT3 and IL11RA were detected with a SYBR-Green real-time quantitative polymerase chain reaction (qRT‒PCR) kit (Thermo Fisher Scientific). The 18S rRNA gene expression levels were used for normalization. All sequences of the primers used in this study are listed in Supplementary Table 2.
Statistical analysis
The study data were analyzed with GraphPad Prism 8.0 (GraphPad). For the matched statistical data, the Wilcoxon matched-pairs signed rank test was used. For continuous data, the Mann‒Whitney U test and unpaired Student’s t-test were used. The results are presented as the means ± standard error of the mean (s.e.m.), and a P < 0.05 was considered statistically significant.
Results
TGF-β signaling pathway is hyperactive in impaired BM EPCs from patients with AA
To investigate whether TGF-β signaling pathway is activated in BM EPCs in patients with AA, the expression levels of TGF-β1 and TGF-βRI in BM EPCs were compared through a prospective case‒control study involving AA patients and their age-matched NCs. The percentage of AA EPCs was significantly lower than that of NC EPCs (0.03 ± 0.004 versus 0.10 ± 0.007, P < 0.0001) (Fig. 1a,b). The expressions of TGF-β1 (2,762.00 ± 275.20 versus 1,186.00 ± 119.90, P < 0.0001) (Fig. 1c), TGF-βRI (2,742.00 ± 277.60 versus 1,067.00 ± 133.70, P < 0.0001) (Fig. 1d) and p-Smad2/3 (5,972.00 ± 200.80 versus 3,501.00 ± 315.40, P < 0.0001) (Fig. 1e and Supplementary Fig. 1b) in AA EPCs were significantly higher than those in NC EPCs. The primary EPCs from patients with AA or NCs were treated with or without TGF-βRI kinase inhibitor (galunisertib(LY2157299, hereafter referred to as LY)) for 24 h. Compared with NC EPCs, AA EPCs demonstrated functional damage characterized by an increased apoptosis ratio (18.48 ± 0.99 versus 9.68 ± 0.75, P < 0.0001) (Fig. 1f and Supplementary Fig. 1c), reduced tube formation (1.00 ± 0.15-fold versus 2.25 ± 0.29-fold, P = 0.009) (Fig. 1g,h) and cell migration (1.00 ± 0.25-fold versus 1.90 ± 0.22-fold, P = 0.04) (Fig. 1i,j) and decreased numbers of double-positive cells stained with DiI-Ac-LDL and FITC-UEA-1 (typical EPC markers; 1.00 ± 0.21-fold versus 2.36 ± 0.26-fold, P = 0.004) (Fig. 1k,l). Taken together, these results indicate that hyperactivation of TGF-β signaling pathway with downstream Smad2/3 phosphorylation is involved in numerically and functionally impaired BM EPCs in patients with AA, with high apoptosis and decreased abilities of angiogenesis and migration.
a,b, Representative images (a) and the frequency (b) of BM EPCs (CD34+CD309+CD133+) among BMMNCs in AA EPCs and NC EPCs. c, A representative image showing the mean fluorescence intensity (MFI) of the TGF-β1 level and the expression level of TGF-β1 in AA EPCs and NC EPCs. d, A representative image of the TGFβ-RI level (MFI) and the expression level of TGFβ-RI in AA EPCs and NC EPCs. e, The expression level of p-Smad2/3 (MFI) in AA EPCs and NC EPCs. f, The apoptosis of AA EPCs and NC EPCs with or without TGF-β inhibition. g,h, Representative images (g) and quantification (h) of tube formation (pixels of tubes per field of view) by BM EPCs. Scale bars, 50 μm; original magnification, 10×. i,j Representative images (i) and quantification (j) of the transwell migration assay of cultivated BM EPCs. Scale bars, 50 μm; original magnification, 10×. k,l, Representative images (k) and quantification (l) of double-positive staining (merged in yellow) with DiI-Ac-LDL (red) and FITC-UEA-1 (green). Scale bars, 50 μm; original magnification, 10×. The data are presented as the mean ± s.e.m. (*P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001).
The TGF-β inhibitor restores the dysfunction of AA EPCs in vitro
To determine whether hyperactive TGF-β signaling pathway is involved in the dysfunction of AA EPCs, we next examined whether the dysfunction of AA EPCs could be reversed by TGF-β inhibition. Compared with AA EPCs, LY treatment significantly reduced the degree of apoptosis (12.35 ± 1.59 versus 18.48 ± 0.99, P = 0.005) (Fig. 1f and Supplementary Fig. 1c), improved tube formation (1.77 ± 0.11-fold versus 1.00 ± 0.15-fold, P = 0.007) (Fig. 1g,h) and migration (1.46 ± 0.27-fold versus 1.00 ± 0.25-fold, P = 0.03) (Fig. 1i,j) and increased the number of double-positive stained cells (1.79 ± 0.35-fold versus 1.00 ± 0.21-fold, P = 0.02) (Fig. 1k,l). LY treatment had no significant effect on NC EPCs. These results suggest that TGF-β inhibition repairs the dysfunction of AA EPCs, resulting in reduced apoptosis and increased angiogenesis and migration in vitro.
The TGF-β inhibitor ameliorates the hematopoiesis-supporting ability of AA EPCs in vitro
To evaluate whether inhibition of TGF-β signaling pathway could improve the hematopoiesis-supporting ability of dysfunctional EPCs, direct-contact coculture experiments of HSCs with AA EPCs or NC EPCs were performed to evaluate the proliferation and functions of HSCs after coculture. Compared with the group cocultured with NC EPCs, the AA group demonstrated worse hematopoiesis-supporting ability, characterized by a decreased ratio of EdU-positive HSCs (45.27 ± 2.60% versus 63.88 ± 6.01%, P = 0.02) (Fig. 2a) and worse CFU efficiencies, including CFU-E (1.00 ± 0.34-fold versus 3.08 ± 0.77-fold, P = 0.02) (Fig. 2b), BFU-E (1.00 ± 0.21-fold versus 2.48 ± 0.30-fold, P = 0.004) (Fig. 2b), CFU-GM (1.00 ± 0.58-fold versus 4.08 ± 0.28-fold, P = 0.0007) (Fig. 2b) and CFU-GEMM (1.00 ± 0.15-fold versus 1.79 ± 0.26-fold, P = 0.02) (Fig. 2b).
a,b, The HSC EdU-positive ratio (a) and the CFU plating efficiency (b) of BM CD34+ cells from NCs after 5 days of coculture with cultivated AA EPCs or NC EPCs. c, Representative gating strategies of TH1 (CD3+CD8-IFN-γ+), TH2(CD3+CD8-IL-4+), and TH17 (CD3+CD8-IL-17+) cells among CD4+ T cells, as well as TC cells 1(CD3+CD8+IFN-γ+), TC2 (CD3+CD8+IL-4+), and TC17 (CD3+CD8+IL-17+) cells among CD8+ T cells via flow cytometry, after 3 days of coculture with AA EPCs or NC EPCs with or without TGF-βRI kinase inhibitor. d–j, The frequencies of BM TH1 cells among CD4+ T cells (d), TC1 cells among CD8+ T cells (e), TH2 cells among CD4+ T cells (f), TC2 cells among CD8+ T cells (g), TH17 cells among CD4+ T cells (h), TC17 cells among CD8+ T cells (i) and Treg (CD3+CD8−CD25+Foxp3+) among CD4+ T cells (j).
LY treatment improved the proliferation and function of HSCs in AA group, as shown by the increased ratio of EdU-positive HSCs (55.08 ± 3.57 versus 45.27 ± 2.60, P = 0.02) (Fig. 2a) and increased CFU efficiencies, including improved CFU-E (2.06 ± 0.56-fold versus 1.00 ± 0.34-fold, P = 0.008) (Fig. 2b), BFU-E (1.83 ± 0.39-fold versus 1.00 ± 0.21-fold, P = 0.01) (Fig. 2b), CFU-GM (2.92 ± 0.84-fold versus 1.00 ± 0.58-fold, P = 0.02) (Fig. 2b) and CFU-GEMM (1.66 ± 0.34-fold versus 1.00 ± 0.15-fold, P = 0.03) (Fig. 2b), whereas LY had no effect on the HSC-supporting ability of NC EPCs. These results indicate that the impaired hematopoiesis-supporting ability of AA EPCs could be restored by TGF-β inhibition.
The TGF-β inhibitor rebalances the abnormal T cell differentiation-supporting ability of AA EPCs in vitro
TGF-β is a regulatory cytokine with a pleiotropic function in immune homeostasis and with context-dependent nature, including target cell type and cytokine milieu. As previously reported, the effects of TGF-β inhibition on T cells varied depending on downstream signals, resulting in either immune overactivation through uncontrolled activation of T cells and TH1 differentiation77 or immunosuppression through the reduction of TH17 differentiation and the enhancement of Treg generation78,79. To explore the effect of TGF-βRI inhibition on the ability of BM EPCs modulating T cell differentiation, direct-contact coculture experiments of CD3+ T cells from NCs with AA EPCs or NC EPCs were performed. Representative flow cytometry gating strategies of T cell subsets after coculture are shown in Fig. 2c. Compared with the NC group, the AA group presented increased frequencies of TH1 (7.11 ± 0.43 versus 4.18 ± 0.53, P = 0.002) (Fig. 2d) and cytotoxic T type 1 (TC1) cells (12.22 ± 1.83 versus 6.78 ± 1.19, P = 0.03) (Fig. 2e), increased percentages of TH2 (9.82 ± 1.01 versus 3.36 ± 0.35, P = 0.002) (Fig. 2f) and cytotoxic T type 2 (TC2) cells (12.52 ± 1.02 versus 5.74 ± 0.67, P = 0.002) (Fig. 2g) and increased frequencies of TH17 (6.76 ± 0.31 versus 3.56 ± 0.38, P = 0.002) (Fig. 2h) and cytotoxic T type 17 (TC17) cells (8.41 ± 0.74 versus 3.82 ± 0.71, P = 0.002) (Fig. 2i) but a decreased frequency of Treg (2.25 ± 0.35 versus 5.01 ± 0.63, P = 0.004) (Fig. 2j).
After LY treatment, AA EPCs were altered in their abilities to modulate T cell subset differentiation. LY treatment reduced the abnormal activation of three major immune types in AA EPC group, including the frequencies of TH1 (3.73 ± 1.11 versus 7.11 ± 0.43, P = 0.006) (Fig. 2d) and TC1 (6.71 ± 1.57 versus 12.22 ± 1.83, P = 0.002) (Fig. 2e) involved in type 1 immunity, the frequencies of TH2 (6.22 ± 1.44 versus 9.82 ± 1.01, P = 0.02) (Fig. 2f) and TC2 (6.38 ± 1.98 versus 12.52 ± 1.02, P = 0.02) (Fig. 2g) involved in type 2 immunity and the frequencies of TH17 (3.98 ± 0.45 versus 6.76 ± 0.31, P = 0.003) (Fig. 2h) and TC17 (5.51 ± 1.34 versus 8.41 ± 0.74, P = 0.01) (Fig. 2i) involved in type 3 immunity. Inversely, the frequency of Treg increased after LY treatment in AA EPC group (3.64 ± 0.55 versus 2.25 ± 0.35, P = 0.008) (Fig. 2j). No significant differences were detected in the T cell differentiation-supporting ability of NC EPCs with or without LY.
In summary, we validated the abnormal expansion of the three major Th cells and reduction of Treg in patients with AA in line with previous reports4. These data indicate that TGF-βRI inhibition on AA EPCs could attenuate the abnormal immune activation and restore Treg-mediated immune tolerance.
Hyperactive TGF-β signaling pathway leads to BM EPC dysfunction, especially in terms of hematopoiesis and immunoregulation
To further validate our hypothesis that hyperactive TGF-β signaling pathway may lead to BM EPC dysfunction, an in vitro model of TGF-β1-triggered BM EPC damage was established. BM EPC function significantly deteriorated after exogenous TGF-β1 exposure, as demonstrated by decreased tube formation (0.48 ± 0.10-fold versus 1.00 ± 0.16-fold, P = 0.03) (Fig. 3a,b) and migration abilities (0.63 ± 0.15-fold versus 1.00 ± 0.18-fold, P = 0.003) (Fig. 3c,d), as well as a reduced number of double-positive stained cells (0.33 ± 0.04-fold versus 1.00 ± 0.21-fold, P = 0.01) (Fig. 3e,f) but increased the apoptosis rate of BM EPCs (13.45 ± 0.95 versus 9.72 ± 0.66, P = 0.03) (Fig. 3g).
a,b, Representative images (a) and quantification (b) of tube formation (pixels of tubes per field of view) of BM EPCs derived from NCs. Scale bars, 50 μm; original magnification, 10×. c,d, Representative images (c) and quantification (d) of the transwell migration assay for cultivated BM EPCs. Scale bars, 50 μm; original magnification, 10×. e,f, Representative images (e) and quantification (f) of the double-positive-stained cell assay for cultivated BM EPCs. g, The apoptotic ratio of cultivated BM EPCs. h,i, The EdU-positive ratio (h) and CFU plating efficiency (i) of BM CD34+ cells from NCs after 5 days of coculture with cultivated NC EPCs. j–m, The frequencies of TH1 cells among CD4+ T cells (j), and TC1 cells among CD8+ T cells (k), TH17 cells among CD4+ T cells (l) and TH2 cells among CD4+ T cells (m), after 3 days of coculture of BM CD3+ cells with NC EPCs. The data are presented as the mean ± s.e.m. (*P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001).
TGF-β1 treatment contributed to a decreased hematopoiesis-supporting ability of BM EPCs, including a lower EdU ratio of cocultured HSCs (48.72 ± 5.48 versus 63.88 ± 6.01, P = 0.01) (Fig. 3h) and decreased counts of CFU-E (0.40 ± 0.12-fold versus 1.00 ± 0.21-fold, P = 0.002) (Fig. 3i), BFU-E (0.25 ± 0.06-fold versus 1.00 ± 0.12-fold, P = 0.0003) (Fig. 3i), CFU-GM (0.55 ± 0.10-fold versus 1.00 ± 0.13-fold, P = 0.02) (Fig. 3i) and CFU-GEMM (0.11 ± 0.03-fold versus 1.00 ± 0.11-fold, P = 0.0003) (Fig. 3i), compared with those in NC group alone.
In terms of immunoregulation, the frequencies of T cell subsets were detected via flow cytometry after coculture with EPCs (Supplementary Fig. 1d). Type 1 T cells, including TH1 (7.21 ± 1.04 versus 4.44 ± 0.48, P = 0.03) (Fig. 3j) and TC1 cells (15.40 ± 2.05 versus 7.21 ± 1.79, P = 0.03) (Fig. 3k), were significantly increased in TGF-β1 group. These findings indicate that hyperactive TGF-β pathway contributes to dysfunctional BM EPCs with increased apoptosis, decreased angiogenesis, impaired hematopoiesis-supporting ability and impaired immunoregulation ability.
The TGF-β inhibitor restores the impaired BM EPCs induced by TGF-β1 in vitro
Although hyperactive TGF-β1 led to BM EPC dysfunction, LY treatment improved tube formation (0.91 ± 0.12-fold versus 0.48 ± 0.10-fold, P = 0.02) (Fig. 3a,b) and migration (0.88 ± 0.14-fold versus 0.63 ± 0.15-fold, P = 0.006) (Fig. 3c,d), increased the number of double-positive stained EPCs (0.81 ± 0.14-fold versus 0.33 ± 0.04-fold, P = 0.007) (Fig. 3e,f) and reduced the apoptosis ratio of BM EPCs (9.93 ± 1.68 versus 13.45 ± 0.95, P = 0.03) (Fig. 3g).
LY treatment reversed the deteriorated hematopoiesis-supporting ability of BM EPCs caused by TGF-β1, as indicated by the increased EdU ratio of cocultured HSCs (69.85 ± 4.74 versus 48.72 ± 5.48, P = 0.004) (Fig. 3h) and improved CFU efficiencies, including CFU-E (0.93 ± 0.22-fold versus 0.40 ± 0.12-fold, P = 0.009) (Fig. 3i), BFU-E (0.86 ± 0.14-fold versus 0.25 ± 0.06-fold, P = 0.001) (Fig. 3i), CFU-GM (0.93 ± 0.08-fold versus 0.55 ± 0.10-fold, P = 0.03) (Fig. 3i) and CFU-GEMM (0.80 ± 0.15-fold versus 0.11 ± 0.03-fold, P = 0.005) (Fig. 3i). Compared with in coculture with TGF-β1-exposed EPCs, the differentiation potential of T cells was rebalanced when in coculture with TGF-β1-exposed EPCs and LY treatment, as indicated by decreased ratios of TH1 (4.02 ± 0.84 versus 7.21 ± 1.04, P = 0.03) (Figs. 3j), TH17 (3.06 ± 1.26 versus 5.99 ± 1.18, P = 0.03) (Fig. 3l) and TH2 cells (2.71 ± 0.66 versus 5.90 ± 1.39, P = 0.03) (Fig. 3m).
Consistent with the results of AA EPCs, the TGF-β1-exposed EPCs and LY treatment model also validated that the TGF-β inhibitor could repair dysfunctional BM EPCs, resulting in decreasing apoptosis, increasing angiogenesis and migration, and improving hematopoietic support and immunoregulation ability.
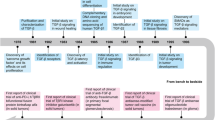
AA mice exhibit decreased BM ECs and hyperactive TGF-β signaling pathway
A classical AA murine model was established to further investigate whether TGF-β signaling is activated in impaired BM ECs in vivo (Fig. 4a). Compared with TBI mice, AA mice presented significantly fewer BM ECs (CD45−Ter119−CD31+VE-Cadherin+; 0.04 ± 0.01 versus 0.18 ± 0.07, P = 0.03) (Fig. 4b) but hyperactive expression of TGF-βRI (2,406.00 ± 264.30 versus 1,665.00 ± 78.71, P = 0.02) (Fig. 4c) and p-Smad2/3 in BM ECs (5,848.00 ± 408.30 versus 954.50 ± 37.42, P < 0.0001) (Fig. 4d). We next performed hematoxylin‒eosin staining and immunohistochemistry with anti-endomucin to evaluate the structure of BM vessels in the different groups (Fig. 4e). AA mice consistently presented a significantly disrupted BM vessel structure (normal: 1.33 ± 0.33 versus 18.33 ± 6.01, P = 0.05, dilated: 73.33 ± 6.67 versus 31.67 ± 7.27; P = 0.01) (Fig. 4f) compared with that of TBI mice. Therefore, these results further confirm our previous findings and indicate decreased and damaged BM ECs with hyperactive TGF-β pathway in AA mice.
a, The establishment of classical AA mice with preirradiation and lymph node (LN) injection and schematic diagram of the different groups and treatments of the mice. b–d, The percentages of ECs (b) and the expression levels of TGFβ-RI (MFI) (c) and p-Smad2/3 (MFI) (d) in murine BM ECs. e, Representative images of BM vessels stained with an anti-endomucin antibody (scale bars, 10 μm) and BM sections stained with hematoxylin‒eosin (scale bars, 10 μm) in murine femurs. The green arrows represent normal vessels, the red arrows represent dilated vessels and the blue arrows represent discontinuous vessels in the murine femur. f, The percentages of normal and dilated as well as discontinuous BM vessels among the total vessels in the different murine groups. The data are presented as the mean ± s.e.m. (*P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001).
TGF-β pathway inhibition enhances the regeneration of BM ECs and vessels in AA mice
To further investigate the effect of TGF-βRI inhibitor on BM ECs in vivo, the classical AA murine model was treated with LY. After oral administration of LY for 13 days in AA mice (AA + LY mice), the ratio of BM ECs in AA + LY mice was markedly higher (0.15 ± 0.01 versus 0.04 ± 0.01, P < 0.0001) (Fig. 4b) than that in AA mice. The expression levels of TGF-βRI (1,869.00 ± 204.10 versus 2,406.00 ± 264.30) (Fig. 4c) and p-Smad2/3 (2,007.00 ± 206.10 versus 5,848.00 ± 408.30, P < 0.0001) (Fig. 4d) in BM ECs decreased in AA + LY mice than those in AA mice. In addition, higher percentages of normal BM vessels were detected in AA + LY mice (10.00 ± 5.00 versus 1.33 ± 0.33) (Fig. 4f) than in AA mice. Therefore, inhibition of TGF-β pathway promotes the repair of BM vessels and BM EC function.
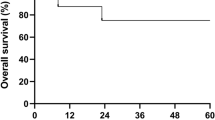
TGF-β pathway inhibition might promote hematopoietic recovery by repairing EC damage in AA mice
To further validate whether inhibition of TGF-β pathway modulates hematopoietic recovery in vivo, peripheral blood cells and BM HSPCs were analyzed in AA mice. AA + LY mice presented better peripheral blood cell performance, including improved hemoglobin (66.67 ± 1.87 g l−1 versus 33 ± 1.90 g l−1, P < 0.0001) (Fig. 5a), red blood cell ((4.87 ± 0.14) × 1012 l−1 versus (2.30 ± 0.13) × 1012 l−1, P < 0.0001) (Fig. 5b), platelet ((17.83 ± 1.58) × 109 l−1 versus (9.33 ± 0.33) × 109 l−1, P = 0.0004) (Fig. 5c) and white blood cell ((0.13 ± 0.02) × 109 l−1 versus (0.10 ± 0.00) × 109 l−1) (Fig. 5d) counts.
a–d, Counts of hemoglobin (a), red blood cells (RBCs) (b), platelets (c) and white blood cells (WBCs) (d) in all the mouse groups. e–h, The counts of myeloid progenitor cells (MPCs) (lineage−cKIT+SCA1−) (e), KLS (cKIT+lineage−SCA1+) cells (f), HSCs (g) and multipotent progenitors (MPPs) (lineage−SCA1+cKIT+CD150−CD48−) (h) per million cells within murine BM. i, The hematopoietic volume in murine BM. j, The frequencies of myeloid cells (CD45+Gr-1+), B cells (CD45+CD3−B220+) and T cells (CD45+CD3+B220−) among CD45+ cells in murine BM. The data are presented as the mean ± s.e.m. (*P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001).
The gating strategy for hematopietic cells is displayed in Supplementary Fig. 1e. Higher cell counts per million cells in BM of myeloid progenitor cells (lineage−cKIT+SCA1−; 1,145.00 ± 117.60 versus 233.40 ± 50.96, P < 0.0001) (Fig. 5e), KLS (cKIT+lineage−SCA1+) cells (1,953.00 ± 416.80 versus 512.30 ± 106.40, P = 0.007) (Fig. 5f), HSCs (lineage−cKIT+SCA1+CD150+CD48−; 195.10 ± 48.17 versus 28.93 ± 5.71, P = 0.007) (Fig. 5g) and multipotent progenitors (lineage−SCA1+cKIT+CD150−CD48−; 407.10 ± 61.51 versus 53.94 ± 11.97, P = 0.0002) (Fig. 5h) were found in AA + LY mice than in AA mice. In addition, a greater hematopoietic volume in BM was observed in AA + LY mice (36.67 ± 1.67 versus 20.00 ± 2.89, P = 0.008) (Fig. 5i) than in AA mice, which demonstrated that TGF-β pathway inhibition improved hematopoietic regeneration in AA mice.
The gating strategies for myeloid cells, B cells and T cells in murine BM are displayed in Supplementary Fig. 1f. AA + LY mice displayed improved hematopoietic lineage and myeloid cells (5.61 ± 0.48 versus 1.73 ± 0.29, P = 0.002) (Fig. 5j), whereas lower frequencies of B cells (6.49 ± 0.66 versus 11.82 ± 0.78, P = 0.002) (Fig. 5j) and T cells (3.59 ± 0.60 versus 5.18 ± 0.65) (Fig. 5j) in BM. Taken together, these findings indicate that inhibition of the hyperactive TGF-β pathway could improve multilineage hematopoiesis recovery and rebalance the immune homeostasis, which might be achieved by repairing BM EC damage in AA mice.
TGF-β pathway inhibition regulates T cell differentiation in AA mice
Since the in vitro findings suggested that TGF-β pathway inhibition in EPCs could regulate T cell differentiation in AA group, we investigated the effect of TGF-β inhibition in AA mice. The gating strategies for TH1, TH2, TH17, TC1, TC2 and TC17 cells and Treg in BM are shown in Fig. 6a. The frequencies of TH1 (10.61 ± 1.68 versus 21.85 ± 1.57, P = 0.0006) (Fig. 6b), TH2 (6.63 ± 1.52 versus 17.08 ± 2.00, P = 0.002) (Fig. 6c), TH17 (4.54 ± 0.87 versus 14.62 ± 0.95, P < 0.0001) (Fig. 6d), TC1 (3.71 ± 0.56 versus 18.85 ± 1.20, P < 0.0001) (Fig. 6e), TC2 (4.23 ± 0.94 versus 17.94 ± 2.38, P = 0.0003) (Fig. 6f) and TC17 cells (3.02 ± 0.51 versus 14.88 ± 0.97, P < 0.0001) (Fig. 6g) were significantly decreased, but the frequency of Treg was increased (21.21 ± 3.82 versus 7.90 ± 1.15, P = 0.008) (Fig. 6h) in AA mice administered with LY compared with untreated AA mice. The results from in vivo and in vitro coculture models uniformly demonstrated that TGF-β pathway inhibition could decrease aberrant immune activation and recover Treg-mediated immune tolerance by repairing BM ECs in AA mice.
a, Representative flow cytometry gating strategies for murine BM TH1, TH2, TH17, TC1, TC2 and TC17 cells and Treg. b–d, The percentages of BM TH1 cells (b), TH2 cells (c) and TH17 cells (d) among BM CD4+ T cells in all the mouse groups. e–g, The percentages of BM TC1 cells (e), TC2 cells (f) and TC17 cells (g) among BM CD8+ T cells in all the mouse groups. h, The percentage of Treg among BM CD4+ T cells in all the mouse groups. The data are presented as the mean ± s.e.m. (*P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001).
RNA-seq analysis validates that TGF-β signaling pathway is related to BM EPC dysfunction
To investigate the potential mechanism of BM EPC dysfunction in patients with AA, RNA-seq was performed on BM EPCs from four pairs of patients with AA and their age-matched NCs (Fig. 7a). A principal component analysis demonstrated that the expression patterns of EPCs in patients with AA and NCs were completely different (Fig. 7b). The expression levels of TGF-β1, TGF-β2 and type II TGF-β receptor were significantly higher in AA EPCs than in NC EPCs (Fig. 7c). The KEGG pathway gene set enrichment analysis showed that TGF-β signaling pathway were significantly upregulated in AA EPCs compared with NC EPCs (Fig. 7d). Besides, the pathways involved with the hematopoietic cell lineage commitment and differentiation and immune regulation were significantly downregulated in AA EPCs compared with NC EPCs (Fig. 7e), which verified the important role of EPCs in supporting hematopoiesis and regulating immunology at the genetic level.
a, A schematic diagram of the study design for RNA-seq analysis of AA EPCs and NC EPCs. b, A principal component analysis (PCA) of AA EPCs and NC EPCs. c, A heat map of upregulated and downregulated genes in AA EPCs and NC EPCs. d, A KEGG pathway analysis showing that TGF-β pathway was upregulated in AA EPCs. e, A KEGG analysis of enriched pathways in NC EPCs. f,g, The mRNA levels of hematopoietic-related genes in impaired EPC models (f) and in AA EPCs (g). h, A schematic illustration indicating that hyperactive TGF-β signaling pathway with downstream Smad2/3 phosphorylation contributes to dysfunctional BM EPCs in AA, whereas TGF-β inhibition repairs dysfunctional BM EPCs, decreasing apoptosis, increasing angiogenesis and migration, and improving multilineage hematopoiesis and immune balance in vitro and in vivo, providing a potential therapeutic strategy for patients with AA. The data are presented as the mean ± s.e.m. (*P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001).
The mRNA levels of hematopoiesis-related genes, including FLT3LG (0.24 ± 0.07 versus 1.00 ± 0.00, P = 0.0001) (Fig. 7f) and IL11RA (0.50 ± 0.11 versus 1.00 ± 0.00, P = 0.001) (Fig. 7f), were decreased in the impaired BM EPC model induced by TGF-β1, as detected via qRT‒PCR. After inhibition of TGF-β in the impaired EPC model, the expressions of genes, including FLT3LG (0.71 ± 0.23 versus 0.24 ± 0.07, P = 0.04) (Fig. 7f) and IL11RA (0.94 ± 0.20 versus 0.50 ± 0.11, P = 0.03) (Fig. 7g), were restored. After inhibition of TGF-β, a similar improvement in the mRNA levels of hematopoiesis-related genes, such as FLT3 (3.38 ± 1.64 versus 1.00 ± 0.00, P = 0.03) (Fig. 7g) and IL11RA (1.81 ± 0.87 versus 1.00 ± 0.00) (Fig. 7g) was detected in BM EPCs from patients with AA, suggesting that these genes may be potential targets of TGF-β pathway that regulate hematopoiesis.
Discussion
Although the involvement of dysfunctional EPCs in the development of AA was demonstrated in our previous work6, there is currently no tangible explanation for the underlying molecular mechanism involved. Here, we reverified that BM EPCs from patients with AA were numerically and functionally impaired and further revealed that overactivation of canonical TGF-β pathway, with downstream Smad2/3 phosphorylation contributing to increased apoptosis, decreased angiogenesis, impaired hematopoiesis support and imbalanced immunoregulation abilities in BM EPCs from patients with AA. TGF-β inhibition could restore the multilineage hematopoietic support and T cell immune rebalancing capacity of BM EPCs in vitro or in AA mice (Fig. 7h).
Hyperactive TGF-β signaling has been implicated in the pathogenesis of several anemia-associated diseases, such as MDS47,48,80, β-thalassemia81,82,83 and primary myelofibrosis84 and the prognosis of these diseases benefits from luspatercept, a TGF-β superfamily ligand trap that improves anemia by promoting late-stage erythropoiesis82,85. However, there are no reports of luspatercept in the treatment of AA. Intriguingly, patients with MDS were enrolled in the COMMANDS trial (NCT03682536), a phase III study that compared the efficacy and safety of luspatercept with those of epoetin alfa and achieved hematologic improvements in erythrocytes, neutrophils and platelets after receiving luspatercept47,86. Indeed, a recent study suggested that RAP-536, an analog of luspatercept, has no direct effect on HSPCs80. These findings indicate the potential role of luspatercept in the BM microenvironment.
In the current study, we demonstrate that TGF-β signaling is overactivated by autocrine secretion of TGF-β1 in BM EPCs of patients with AA and in classical AA mice, resulting in peripheral pancytopenia. In line with the multilineage hematopoietic restoration effects of luspatercept in patients with MDS45,86, we found that galunisertib (LY2157299 monohydrate), a TGF-βRI kinase inhibitor that downregulates the phosphorylation of Smad2/3, improved multilineage hematopoiesis in an AA mouse model. In addition, previous studies have shown that EPC or EC infusion can augment BM HSC reconstitution and the production of mature blood cells15,87. TGF-β inhibition not only repaired dysfunctional BM EPCs but also expanded the number of ECs endogenously, which could eliminate access restrictions associated with BM EPC or EC infusion.
With respect to the mechanism underlying TGF-β signaling-induced hematopoiesis damage, qRT‒PCR analysis revealed that TGF-β1 inhibited hematopoiesis gene expression in BM EPCs via FLT3LG and IL11RA, which could be reversed by LY. As previously reported, FLT3 is essential hematopoietic factor with prominent effects on the development of hematopoietic multilineages88, and IL11RA is the receptor for interleukin-11 (IL-11) which promotes HSC engraftment in AA mice via promoting megakaryopoiesis89. These results are consistent with our findings in vitro and in vivo, indicating the pivotal role of TGF-β signaling in regulating the hematopoiesis-supporting capacity of BM EPCs.
In addition to the indirect suppression of hematopoiesis by TGF-β-activated BM EPCs, direct regulation of TGF-β signaling on HSPCs cannot be excluded in the development of AA. During homeostasis, TGF-β was reported to directly maintain HSC hibernation through up-regulating p57 cyclin-dependent kinase inhibitor51. Beyond physiological effects, TGF-β directly causes HSPC growth arrest in mice and patients with Fanconi anemia49. However, maintenance of HSC quiescence is dependent on BM microenvironment, such as megakaryocyte-derived TGF-β rather than an autocrine TGF-β signaling loop in HSCs32,51. Although further validation in a BM EC-specific TGF-βRI-overexpressing murine model is needed, the present study is the first to demonstrate that LY2157299 monohydrate inhibits TGF-βRI kinase in impaired BM EPCs and restores hematopoiesis and immune homeostasis, identifying a potential mechanism in AA.
Different from other BM failure disease, AA has been well characterized as an immune-mediated BM disorder1,2,3,4. In our study, abnormal expansion of TH1, TH2, and TH17 cells and reduction of Treg cells were observed in cocultures with AA EPCs, and the differentiation potential of T cells was rebalanced after LY treatment, confirming that TGF-β1-activated EPCs are defective in modulating immune homeostasis in AA. In addition to the abnormal number of T cell subsets, functional abnormalities of Treg cells were also reported in AA4,6,90. However, we are aware that the function of rebalanced T cells in cocultures with AA EPCs needs to be further explored in the future.
Our findings show that dysfunctional BM EPCs with hyperactive TGF-β signaling are involved in AA, whereas the inhibition of TGF-β pathway could promote multilineage hematopoiesis recovery and immune balance in AA via the repair of dysfunctional BM EPCs. Our preliminary data indicate that the use of TGF-β signaling inhibitors (such as luspatercept) might be a potential therapeutic strategy for patients with AA, which provides a rationale for further clinical trials in patients with AA to validate our preliminary findings in the future.
References
Young, N. S., Calado, R. T. & Scheinberg, P. Current concepts in the pathophysiology and treatment of aplastic anemia. Blood 108, 2509–2519 (2006).
Young, N. S. Aplastic anemia. N. Engl. J. Med. 379, 1643–1656 (2018).
Sun, W. et al. Macrophage TNF-α licenses donor T cells in murine bone marrow failure and can be implicated in human aplastic anemia. Blood 132, 2730–2743 (2018).
Kordasti, S. et al. Functional characterization of CD4+ T cells in aplastic anemia. Blood 119, 2033–2043 (2012).
Zhu, C. et al. Single-cell transcriptomics dissects hematopoietic cell destruction and T-cell engagement in aplastic anemia. Blood 138, 23–33 (2021).
Tang, S. Q. et al. Repair of dysfunctional bone marrow endothelial cells alleviates aplastic anemia. Sci. China Life Sci. 66, 2553–2570 (2023).
Peffault de Latour, R. et al. Eltrombopag added to immunosuppression in severe aplastic anemia. N. Engl. J. Med. 386, 11–23 (2022).
Montoro, J. et al. Alternative donor transplantation for severe aplastic anemia: a comparative study of the SAAWP EBMT. Blood 144, 323–333 (2024).
Calvanese, V. et al. Mapping human haematopoietic stem cells from haemogenic endothelium to birth. Nature 604, 534–540 (2022).
Ding, L., Saunders, T. L., Enikolopov, G. & Morrison, S. J. Endothelial and perivascular cells maintain haematopoietic stem cells. Nature 481, 457–462 (2012).
Sugiyama, T., Kohara, H., Noda, M. & Nagasawa, T. Maintenance of the hematopoietic stem cell pool by CXCL12–CXCR4 chemokine signaling in bone marrow stromal cell niches. Immunity 25, 977–988 (2006).
Salter, A. B. et al. Endothelial progenitor cell infusion induces hematopoietic stem cell reconstitution in vivo. Blood 113, 2104–2107 (2009).
Butler, J. M. et al. Endothelial cells are essential for the self-renewal and repopulation of Notch-dependent hematopoietic stem cells. Cell Stem Cell 6, 251–264 (2010).
Hooper, A. T. et al. Engraftment and reconstitution of hematopoiesis is dependent on VEGFR2-mediated regeneration of sinusoidal endothelial cells. Cell Stem Cell 4, 263–274 (2009).
Chute, J. P. et al. Transplantation of vascular endothelial cells mediates the hematopoietic recovery and survival of lethally irradiated mice. Blood 109, 2365–2372 (2007).
Zeng, L. et al. Infusion of endothelial progenitor cells accelerates hematopoietic and immune reconstitution, and ameliorates the graft-versus-host disease after hematopoietic stem cell transplantation. Cell Biochem Biophys. 64, 213–222 (2012).
Mai, J. et al. An evolving new paradigm: endothelial cells-conditional innate immune cells. J. Hematol. Oncol. 6, 61 (2013).
Shao, Y. et al. Vascular endothelial cells and innate immunity. Arterioscler Thromb. Vasc. Biol. 40, e138–e152 (2020).
Fang, J. et al. Regulatory T cells and CD20+ B cells in pediatric very severe aplastic anemia: possible clinical markers for evaluating the therapeutic efficacy and prognosis. Hematology 23, 823–827 (2018).
Hassanpour, M., Salybkov, A. A., Kobayashi, S. & Asahara, T. Anti-inflammatory prowess of endothelial progenitor cells in the realm of biology and medicine. NPJ Regen. Med. 9, 27 (2024).
Chen, P. M. et al. Induction of immunomodulatory monocytes by human mesenchymal stem cell-derived hepatocyte growth factor through ERK1/2. J. Leukoc. Biol. 96, 295–303 (2014).
Shi, M. M. et al. Atorvastatin enhances endothelial cell function in posttransplant poor graft function. Blood 128, 2988–2999 (2016).
Kong, Y. et al. N-acetyl-l-cysteine improves bone marrow endothelial progenitor cells in prolonged isolated thrombocytopenia patients post allogeneic hematopoietic stem cell transplantation. Am. J. Hematol. 93, 931–942 (2018).
Kong, Y. et al. Atorvastatin enhances bone marrow endothelial cell function in corticosteroid-resistant immune thrombocytopenia patients. Blood 131, 1219–1233 (2018).
Xing, T. et al. Dysfunctional bone marrow endothelial progenitor cells are involved in patients with myelodysplastic syndromes. J. Transl. Med. 20, 144 (2022).
Lyu, Z. S. et al. The glycolytic enzyme PFKFB3 determines bone marrow endothelial progenitor cell damage after chemotherapy and irradiation. Haematologica 107, 2365–2380 (2022).
Liang, M. et al. Activation of PPARδ in bone marrow endothelial progenitor cells improves their hematopoiesis-supporting ability after myelosuppressive injury. Cancer Lett. 592, 216937 (2024).
Wang, Y. et al. Prophylactic NAC promoted hematopoietic reconstitution by improving endothelial cells after haploidentical HSCT: a phase 3, open-label randomized trial. BMC Med. 20, 140 (2022).
Sakamaki, S. et al. Transforming growth factor-beta1 (TGF-beta1) induces thrombopoietin from bone marrow stromal cells, which stimulates the expression of TGF-beta receptor on megakaryocytes and, in turn, renders them susceptible to suppression by TGF-beta itself with high specificity. Blood 94, 1961–1970 (1999).
Yamazaki, S. et al. Nonmyelinating Schwann cells maintain hematopoietic stem cell hibernation in the bone marrow niche. Cell 147, 1146–1158 (2011).
Blank, U. & Karlsson, S. TGF-β signaling in the control of hematopoietic stem cells. Blood 125, 3542–3550 (2015).
Zhao, M. et al. Megakaryocytes maintain homeostatic quiescence and promote post-injury regeneration of hematopoietic stem cells. Nat. Med. 20, 1321–1326 (2014).
Jiang, L. et al. SHP-1 regulates hematopoietic stem cell quiescence by coordinating TGF-β signaling. J. Exp. Med 215, 1337–1347 (2018).
Wang, Z. K. et al. Inhibition of TGF-β signaling in bone marrow endothelial cells promotes hematopoietic recovery in acute myeloid leukemia patients. Cancer Lett. 605, 217290 (2024).
Hayashi, S. et al. Differential effects of TGF-beta 1 on lymphohemopoiesis in long-term bone marrow cultures. Blood 74, 1711–1717 (1989).
Challen, G. A., Boles, N. C., Chambers, S. M. & Goodell, M. A. Distinct hematopoietic stem cell subtypes are differentially regulated by TGF-beta1. Cell Stem Cell 6, 265–278 (2010).
Quéré, R. et al. Tif1γ regulates the TGF-β1 receptor and promotes physiological aging of hematopoietic stem cells. Proc. Natl Acad. Sci. USA 111, 10592–10597 (2014).
Carlino, J. A. et al. Transforming growth factor beta 1 systemically modulates granuloid, erythroid, lymphoid, and thrombocytic cells in mice. Exp. Hematol. 20, 943–950 (1992).
Zermati, Y. et al. Transforming growth factor inhibits erythropoiesis by blocking proliferation and accelerating differentiation of erythroid progenitors. Exp. Hematol. 28, 885–894 (2000).
Suragani, R. N. et al. Transforming growth factor-β superfamily ligand trap ACE-536 corrects anemia by promoting late-stage erythropoiesis. Nat. Med. 20, 408–414 (2014).
Zhou, L. et al. Inhibition of the TGF-beta receptor I kinase promotes hematopoiesis in MDS. Blood 112, 3434–3443 (2008).
Dussiot, M. et al. An activin receptor IIA ligand trap corrects ineffective erythropoiesis in β-thalassemia. Nat. Med. 20, 398–407 (2014).
Suragani, R. N. et al. Modified activin receptor IIB ligand trap mitigates ineffective erythropoiesis and disease complications in murine β-thalassemia. Blood 123, 3864–3872 (2014).
Piga, A. et al. Luspatercept improves hemoglobin levels and blood transfusion requirements in a study of patients with β-thalassemia. Blood 133, 1279–1289 (2019).
Garcia-Manero, G. et al. Neutrophil and platelet increases with luspatercept in lower-risk MDS: secondary endpoints from the MEDALIST trial. Blood 139, 624–629 (2022).
Taher, A. T. et al. Luspatercept for the treatment of anaemia in non-transfusion-dependent β-thalassaemia (BEYOND): a phase 2, randomised, double-blind, multicentre, placebo-controlled trial. Lancet Haematol. 9, e733–e744 (2022).
Platzbecker, U. et al. Efficacy and safety of luspatercept versus epoetin alfa in erythropoiesis-stimulating agent-naive, transfusion-dependent, lower-risk myelodysplastic syndromes (COMMANDS): interim analysis of a phase 3, open-label, randomised controlled trial. Lancet 402, 373–385 (2023).
Porta, M. G. D. et al. Luspatercept versus epoetin alfa in erythropoiesis-stimulating agent-naive, transfusion-dependent, lower-risk myelodysplastic syndromes (COMMANDS): primary analysis of a phase 3, open-label, randomised, controlled trial. Lancet Haematol. 11, e646–e658 (2024).
Zhang, H. et al. TGF-β inhibition rescues hematopoietic stem cell defects and bone marrow failure in fanconi anemia. Cell Stem Cell 18, 668–681 (2016).
Joyce, C. E. et al. TGFβ signaling underlies hematopoietic dysfunction and bone marrow failure in Shwachman–Diamond syndrome. J. Clin. Invest 129, 3821–3826 (2019).
Yamazaki, S. et al. TGF-β as a candidate bone marrow niche signal to induce hematopoietic stem cell hibernation. Blood 113, 1250–1256 (2009).
Bataller, A., Montalban-Bravo, G., Soltysiak, K. A. & Garcia-Manero, G. The role of TGFβ in hematopoiesis and myeloid disorders. Leukemia 33, 1076–1089 (2019).
Batard, P. et al. TGF-β1 maintains hematopoietic immaturity by a reversible negative control of cell cycle and induces CD34 antigen up-modulation. J. Cell Sci. 113, 383–390 (2000).
Hatzfeld, J. et al. Release of early human hematopoietic progenitors from quiescence by antisense transforming growth factor beta 1 or Rb oligonucleotides. J. Exp. Med. 174, 925–929 (1991).
Takehara, K., LeRoy, E. C. & Grotendorst, G. R. TGF-beta inhibition of endothelial cell proliferation: alteration of EGF binding and EGF-induced growth-regulatory (competence) gene expression. Cell 49, 415–422 (1987).
Ferrari, G. et al. VEGF, a prosurvival factor, acts in concert with TGF-beta1 to induce endothelial cell apoptosis. Proc. Natl Acad. Sci. USA 103, 17260–17265 (2006).
Goumans, M. J., Liu, Z. & ten Dijke, P. TGF-beta signaling in vascular biology and dysfunction. Cell Res. 19, 116–127 (2009).
Goumans, M. J. et al. Activin receptor-like kinase (ALK)1 is an antagonistic mediator of lateral TGFbeta/ALK5 signaling. Mol. Cell 12, 817–828 (2003).
Goumans, M. J. et al. Balancing the activation state of the endothelium via two distinct TGF-beta type I receptors. Embo J. 21, 1743–1753 (2002).
Goumans, M. J. & Ten Dijke, P. TGF-β signaling in control of cardiovascular function. Cold Spring Harb. Perspect. Biol. 10, a022210 (2018).
Dubiella, C. et al. Sulfopin is a covalent inhibitor of Pin1 that blocks Myc-driven tumors in vivo. Nat. Chem. Biol. 17, 954–963 (2021).
Delangre, E. et al. Underlying mechanisms of glucocorticoid-induced β-cell death and dysfunction: a new role for glycogen synthase kinase 3. Cell Death Dis. 12, 1136 (2021).
Lyu, Z. S. et al. Autophagy in endothelial cells regulates their haematopoiesis-supporting ability. EBioMedicine 53, 102677 (2020).
Deng, F. et al. Tumor-secreted dickkopf2 accelerates aerobic glycolysis and promotes angiogenesis in colorectal cancer. Theranostics 9, 1001–1014 (2019).
Gray, W. D. et al. Identification of therapeutic covariant microRNA clusters in hypoxia-treated cardiac progenitor cell exosomes using systems biology. Circ. Res 116, 255–263 (2015).
Wang, S. et al. Exosomes released by hepatocarcinoma cells endow adipocytes with tumor-promoting properties. J. Hematol. Oncol. 11, 82 (2018).
Xu, W. et al. Endothelial FAM3A positively regulates post-ischaemic angiogenesis. EBioMedicine 43, 32–42 (2019).
Zhao, H. Y. et al. M2 macrophages, but not M1 macrophages, support megakaryopoiesis by upregulating PI3K–AKT pathway activity. Signal Transduct. Target Ther. 6, 234 (2021).
Xing, T. et al. Bone marrow macrophages are involved in the ineffective hematopoiesis of myelodysplastic syndromes. J. Cell Physiol. 239, e31129 (2024).
Wang, D. et al. GARP-mediated active TGF-β1 induces bone marrow NK cell dysfunction in AML patients with early relapse post-allo-HSCT. Blood 140, 2788–2804 (2022).
Lin, S. et al. TGFβ signalling pathway regulates angiogenesis by endothelial cells, in an adipose-derived stromal cell/endothelial cell co-culture 3D gel model. Cell Prolif. 48, 729–737 (2015).
Bloom, M. L. et al. A mouse model of lymphocyte infusion-induced bone marrow failure. Exp. Hematol. 32, 1163–1172 (2004).
Feng, X. et al. Rapamycin is highly effective in murine models of immune-mediated bone marrow failure. Haematologica 102, 1691–1703 (2017).
Guo, L. et al. Characteristics, dynamic changes, and prognostic significance of TCR repertoire profiling in patients with renal cell carcinoma. J. Pathol. 251, 26–37 (2020).
Zhu, J. et al. Delineating the dynamic evolution from preneoplasia to invasive lung adenocarcinoma by integrating single-cell RNA sequencing and spatial transcriptomics. Exp. Mol. Med. 54, 2060–2076 (2022).
Xiong, L. L. et al. Single-cell RNA sequencing reveals B cell-related molecular biomarkers for Alzheimer’s disease. Exp. Mol. Med. 53, 1888–1901 (2021).
Marie, J. C., Liggitt, D. & Rudensky, A. Y. Cellular mechanisms of fatal early-onset autoimmunity in mice with the T cell-specific targeting of transforming growth factor-beta receptor. Immunity 25, 441–454 (2006).
Aarts, J. et al. Local inhibition of TGF-β1 signaling improves Th17/Treg balance but not joint pathology during experimental arthritis. Sci. Rep. 12, 3182 (2022).
Li, M. O., Wan, Y. Y. & Flavell, R. A. T cell-produced transforming growth factor-β1 controls T cell tolerance and regulates Th1- and Th17-cell differentiation. Immunity 26, 579–591 (2007).
Wobus, M. et al. Luspatercept restores SDF-1-mediated hematopoietic support by MDS-derived mesenchymal stromal cells. Leukemia 35, 2936–2947 (2021).
Cappellini, M. D. et al. A Phase 3 trial of luspatercept in patients with transfusion-dependent β-thalassemia. N. Engl. J. Med. 382, 1219–1231 (2020).
Garbowski, M. W. et al. Luspatercept stimulates erythropoiesis, increases iron utilization, and redistributes body iron in transfusion-dependent thalassemia. Am. J. Hematol. 99, 182–192 (2024).
Martinez, P. A. et al. Smad2/3-pathway ligand trap luspatercept enhances erythroid differentiation in murine β-thalassaemia by increasing GATA-1 availability. J. Cell Mol. Med. 24, 6162–6177 (2020).
Lecomte, S. et al. Therapeutic activity of GARP:TGF-β1 blockade in murine primary myelofibrosis. Blood 141, 490–502 (2023).
Fenaux, P., Kiladjian, J. J. & Platzbecker, U. Luspatercept for the treatment of anemia in myelodysplastic syndromes and primary myelofibrosis. Blood 133, 790–794 (2019).
Garcia-Manero G. et al. Multilineage and Safety Results From the COMMANDS Trial in Transfusion-Dependent, Erythropoiesis-Stimulating Agent-Naive Patients With Very Low-, Low-, or Intermediate-Risk Myelodysplastic Syndromes. EHA. P780 (2024).
Qiao, J. et al. Endothelial progenitor cells improve the quality of transplanted hematopoietic stem cells and maintain longer term effects in mice. Ann. Hematol. 96, 107–114 (2017).
Momenilandi, M. et al. FLT3L governs the development of partially overlapping hematopoietic lineages in humans and mice. Cell 187, 2817–2837.e2831 (2024).
Wang, Y. et al. IL-11 promotes the treatment efficacy of hematopoietic stem cell transplant therapy in aplastic anemia model mice through a NF-κB/microRNA-204/thrombopoietin regulatory axis. Exp. Mol. Med. 49, e410 (2017).
Solomou, E. E. et al. Deficient CD4+ CD25+ FOXP3+ T regulatory cells in acquired aplastic anemia. Blood 110, 1603–1606 (2007).
Acknowledgements
We thank all the core facilities at the Peking University Institute of Hematology for patients care and sample collection. This work was supported by the National Key R&D Program of China (grant nos. 2021YFA1100900 and 2022YFA1103300), the National Natural Science Foundation of China (grant nos. 82270229, 82070188 and 82200240), Major Program of the National Natural Science Foundation of China (grant no. 82293630), Beijing Natural Science Foundation (grant no. 7232181), Peking University People’s Hospital Scientific Research Development Funds (grant no. RDGS2022-04). American Journal Experts (www.journalexperts.com) provided editorial assistance to the authors during the preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Y.K. and X.J.H. conceived and designed the study and supervised the manuscript preparation. X.Y.Z. and L.P.G. performed the experiments and data analysis. X.Y.Z., L.P.G. and Z.W.Z. wrote the manuscript. L.P.G. performed the bioinformatic analysis. All other authors participate in the collection of patients data. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhang, XY., Guo, LP., Wang, YZ. et al. TGF-β inhibition restores hematopoiesis and immune balance via bone marrow EPCs in aplastic anemia. Exp Mol Med (2025). https://doi.org/10.1038/s12276-025-01483-4
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s12276-025-01483-4