Abstract
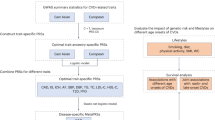
The genetic risk for hypertensive disorders of pregnancy is linked with the development of atherosclerotic cardiovascular disease. However, the effects of lifestyle and metabolic syndrome on atherosclerotic cardiovascular disease have not been evaluated. Here, we assess the long-term association between these factors and atherosclerotic cardiovascular disease in women with genetic risk for hypertensive disorders of pregnancy. We evaluate the genetic risk for hypertensive disorders of pregnancy using a genome-wide polygenic risk score derived from a large-scale GWAS. The incidence of atherosclerotic cardiovascular disease is evaluated according to genetic risk, lifestyle, and metabolic syndrome. Individuals with a very high genetic risk for hypertensive disorders of pregnancy have a 53.0% higher chance of developing atherosclerotic cardiovascular disease than those with a low genetic risk. However, the risk of developing atherosclerotic cardiovascular disease is reduced by up to 64.6% through the maintenance of an ideal metabolic syndrome status and a healthy lifestyle in the high genetic risk group (top 20%), and by up to 65.4% in the low genetic risk group (bottom 20%). These findings emphasize that maintaining a healthy lifestyle in women is equally effective at reducing the risk of atherosclerotic cardiovascular disease independent of genetic risk for hypertensive disorders of pregnancy.
Similar content being viewed by others
Introduction
Hypertensive disorders of pregnancy (HDP) is a serious complication that poses significant health risks for both mothers and newborns1,2,3,4,5. HDP affects not only immediate maternal complications but also long-term maternal health risks later in life6. Notably, there has been a consistent correlation between HDP and the elevated risk of developing atherosclerotic cardiovascular disease (ASCVD) beyond the pregnancy period. A systematic review of cohort studies revealed that women who have experienced HDP are at a higher risk of developing hypertension, ischemic heart disease, stroke, and overall mortality than those who have not7. Furthermore, meta-analyses and large prospective cohort studies have shown that these women have a doubled risk of developing cardiovascular disease (CVD)8,9,10,11. In addition, the Nurses’ Health Study II, with an average follow-up of more than 50 years, reported that chronic hypertension, hypercholesterolemia, type 2 diabetes, and changes in body mass index (BMI) mediated the association between HDP and CVD12. Consequently, the 2011 American Heart Association (AHA) guidelines recommend HDP as a crucial sex-specific risk factor for ASCVD13,14. However, the exact mechanisms linking HDP to ASVCD remain unclear. Shared risk factors, such as high blood pressure (BP), diabetes, and obesity, are speculated to contribute to this association15.
A recent meta-analysis of genome-wide association studies (GWAS) has identified genetic variants associated with HDP16,17. Studies are underway to develop a polygenic risk score (PRS) for HDP based on these genetic variants to predict the risk of HDP18. Notably, genetic predisposition has been revealed as a potential contributor to the development of ASCVD post-HDP18. Individuals with a genetic predisposition to HDP are more likely to develop ASCVD, regardless of whether they have physically manifested HDP. These findings suggest that identifying high-risk individuals based on their genetic factors may lead to different treatment strategies to lower their risk of ASCVD.
Although genetic factors may play an important role, modifiable risk factors such as lifestyle or metabolic health have gained attention regarding preventive modalities to reduce cardiovascular (CV) risk19,20,21. Previous studies have indicated that clinical factors such as metabolic syndrome (MetS) and lifestyle factors are effective in risk reduction in the middle-aged population22,23. However, it remains unclear whether these factors are equally beneficial for general and high-risk populations. In addition, the evaluation of the association between genetic risk and modifiable factors can be an important issue, because understanding the relationship between these factors could guide clinicians to more effective preventive measures.
Given that HDP is a significant female-specific risk factor, we investigated whether modifiable clinical factors can be used to develop effective prevention strategies in high-risk women, especially those with a high genetic predisposition for HDP18,24,25,26. In spite of the established impact of HDP on CV outcomes, there is a paucity of information regarding how modifiable factors can reduce the genetic risk of HDP in terms of long-term CV outcomes.
Overall, this study aimed to investigate the long-term relationship between HDP, genetic risk, MetS, and lifestyle factors and ASCVD development.
Results
Population characteristics
A total of 164,500 parous women of European descent from the UK Biobank (UKBB) were included after excluding those with no history of live birth or a lack of information concerning parity. The mean age of participants was 57.2 years (standard deviation [SD], 7.7 years). Table 1 compares the baseline clinical features and prevalent diseases in the study population according to genetic risk for HDP. Supplementary Table 1 shows the baseline characteristics of the study population based on the presence or absence of HDP. Women with higher genetic risk for HDP had higher BMI, current smoking, and BP and were more likely to use medications (aspirin, antihypertensive medication, and cholesterol medication) than those with lower genetic risk for HDP.
In the replication set, we included 2001 parous women from the Penn Medicine Biobank (PMBB) cohort, comprising 982 of European descent and 1019 of African American descent (Supplementary Table 2). The mean age of participants was 32.7 years (SD, 6.9 years). The study flowcharts are shown in Supplementary Figs. 1 and 2.
Association of the PRS with HDP and validation in the PMBB cohort
Among all the participants in the present study, 2427 (1.5%) had a history of HDP. Using publicly available large-scale GWAS data, we calculated the PRS for HDP and found a strong association with prevalent HDP in the UKBB (odds ratio [OR] 1.23 per 1 SD increase; 95% confidence interval (CI), 1.18–1.28; P < 2.20E-16). Supplementary Table 3 presents the OR for the association of HDP with the PRS-risk groups. In the fully adjusted model, individuals with very high PRS had a 2.24-fold higher risk of developing HDP (95% CI, 1.61–3.12; P = 1.65E-06) than the low-PRS group.
We then replicated the PRS for HDP analysis in a cohort from the PMBB. We observed a significant association between the PRS and prevalent HDP across different ancestries in the overall PMBB cohort (OR 1.17 per 1 SD increase; 95% CI, 1.06–1.30; P = 0.002). Individuals in the high-PRS group demonstrated an increased risk of HDP compared to those in the low-PRS group (P for trend = 8.92E-04). In subpopulation analysis within the PMBB, the PRS for HDP consistently emerged as a significant predictor of prevalent HDP risk across both populations (Supplementary Table 4).
Association of HDP-PRS with incident ASCVD and its subtypes
Among the study participants, 7598 (4.6%) were diagnosed with incident ASCVD during the follow-up period (4.09 occurrences per 1000 women years). Utilizing a multivariable Cox regression model, we established a significant association between the HDP-PRS and incident ASCVD in the UKBB (hazard ratio [HR] 1.09 per 1 SD increase; 95% CI, 1.07–1.12; P = 3.01E-14) (Table 2). In the fully adjusted model, this association remained significant—individuals with very high PRS had a 1.47-fold increased risk of ASCVD compared to those in the low-PRS group (95% CI, 1.18–1.83; P = 5.82E-04). To statistically assess the performance change when incorporating HDP-PRS into conventional risk factors, we conducted analyses using the C-index and net reclassification index (NRI). As a result, in all four additive models presented in Table 2, the addition of PRS information significantly increased the continuous NRI by 7.82% to 11.05% (Supplementary Table 5).
In addition, a significant association was observed between HDP-PRS and various ASCVD subtypes. The adjusted HRs per 1 SD increase were 1.10 (95% CI, 1.08–1.13; P = 1.07E-15) for coronary artery disease, 1.16 (95% CI, 1.10–1.22; P = 5.57E-09) for myocardial infarction, 1.09 (95% CI, 1.03–1.16; P = 0.002) for peripheral artery disease, 1.04 (95% CI, 1.01–1.09; P = 0.040) for ischemic stroke, and 1.02 (95% CI, 0.92–1.13; P = 0.669) for aortic aneurysms (Supplementary Table 6 and Supplementary Fig. 3).
Association of lifestyle and MetS status with incident ASCVD
In the fully adjusted analysis, both lifestyle and MetS status were associated with an increased risk of developing ASCVD. Specifically, an unfavorable lifestyle was associated with a high risk of incident ASCVD (HR, 1.71; 95% CI, 1.59–1.84; P < 2.20E-16) when compared to a favorable lifestyle (Supplementary Table 7). Poor MetS status was associated with a higher risk of incident ASCVD (HR, 1.40; 95% CI, 1.30–1.50; P < 2.20E-16) than was an ideal MetS status (Supplementary Tables 8 and 9).
Joint associations of HDP-PRS, lifestyle, and MetS status with incident ASCVD
To explore the effects of lifestyle and MetS status on incident ASCVD risk according to genetic risk, we stratified lifestyle and MetS factors by the PRS category. We observed a joint association between increasing PRS for HDP, MetS components, and unfavorable lifestyle, and an increased risk of developing incident ASCVD. Individuals with low PRS (< 20%) who had favorable lifestyles had the lowest risk for incident ASCVD (HR, 0.36; 95% CI, 0.32–0.41; P < 2.20E-16) (Fig. 1a), followed by those with low PRS who had ideal MetS status (HR, 0.46; 95% CI, 0.40–0.54; P < 2.20E-16) (Fig. 1b). In both analyses, the P for trends was significant, but no significant interactions were observed. As each component of MetS includes numerous risk factors, we also compared the risk of incident ASCVD between high and low genetic risk groups according to deciles of each component of MetS (Supplementary Fig. 4). Individuals with low PRS had a lower risk for incident ASCVD than those with high PRS in every decile of each component of MetS. The HDP-PRS was significantly associated with incident ASCVD across all MetS subgroups and consistently across lifestyle groups, though marginally significant in the unfavorable lifestyle group (P = 0.079) (Supplementary Tables 10 and 11).
a Risk of incident atherosclerotic cardiovascular disease (ASCVD) according to genetic risk and lifestyle. b Risk of incident ASCVD according to genetic risk and metabolic syndrome. For (a, b), the polygenic risk score for hypertensive disorders of pregnancy (HDP) has been derived from the FinnGen Consortium. The high genetic risk group was defined as individuals in the top 20% of the polygenic risk score distribution, while the low genetic risk group was defined as those in the bottom 20%. No. Events indicate the number of ASCVD incidents that occurred in the UK Biobank. Boxes represent the adjusted hazard ratio, with horizontal lines around the boxes indicating 95% confidence intervals. The hazard ratios were estimated using Cox proportional hazards models, adjusted for history of HDP, age, genotype array, and first ten principal components of ancestry. P-values were determined using a Wald test. P-values for interaction were derived from the multiplicative interaction analysis between genetic risk and each group (lifestyle or metabolic syndrome). All P-values were derived from two-sided tests. Exact statistical values are provided as a Source Data file. HDP hypertensive disorders of pregnancy, ASCVD atherosclerotic cardiovascular disease, HR hazard ratio, CI confidence interval, MetS metabolic syndrome.
In addition, we evaluated whether a favorable lifestyle reduced the risk of ASCVD in women according to their history of HDP. In women with a history of HDP, a combination of low genetic risk (bottom 20%) and favorable lifestyle reduced the risk of ASCVD by 88% compared to those with high genetic risk (top 20%) and unfavorable lifestyle (Supplementary Figs. 5 and 6). Similarly, in women without a history of HDP, a combination of low genetic risk (bottom 20%) and a favorable lifestyle reduced the risk of ASCVD by 63% compared to those with high genetic risk (top 20%) and an unfavorable lifestyle.
We evaluated whether a favorable lifestyle reduced the risk of ASCVD in women based on their BP or glucose status at enrollment. As a result, a combination of low genetic risk (bottom 20%) and a favorable lifestyle reduced the risk of ASCVD compared to those with high genetic risk (top 20%) and an unfavorable lifestyle, both in women with normal and high glucose levels, and both in women with normal and high BPs (Fig. 2).
a Risk of incident atherosclerotic cardiovascular disease (ASCVD) of parous women with normal blood pressure. b Risk of incident ASCVD of parous women with elevated blood pressure. c Risk of incident ASCVD of parous women with normal glucose levels. d Risk of incident ASCVD of parous women with high glucose levels. The normal blood pressure group was defined as systolic blood pressure (sBP) of < 120 mmHg and diastolic blood pressure (dBP) of < 80 mmHg, while the elevated blood pressure group was defined as an sBP ≥ 120 mmHg or a dBP ≥ 80 mmHg. The normal glucose level was < 100 mg/dL (5.6 mmol/L) and the high glucose level was defined as ≥ 100 mg/dL (5.6 mmol/L). For (a–d), the polygenic risk score for hypertensive disorders of pregnancy (HDP) has been derived from the FinnGen Consortium. The high genetic risk group was defined as individuals in the top 20% of the polygenic risk score distribution, while the low genetic risk group was defined as those in the bottom 20%. No. Events indicate the number of ASCVD incidents that occurred in the UK Biobank. In the bar charts, bars represent ASCVD incidence rates per 1000 women-year, with vertical lines indicating 95% confidence intervals (CIs). In the forest plots, boxes represent the adjusted hazard ratio, with horizontal lines around the boxes indicating 95% CIs. The hazard ratios were estimated using Cox proportional hazards models, adjusted for history of HDP, age, genotype array, and first ten principal components of ancestry. P-values were determined using a Wald test. P-values for interaction were derived from the multiplicative interaction analysis between genetic risk and lifestyle groups. All P-values were derived from two-sided tests. Exact statistical values are provided as a Source Data file. HDP hypertensive disorders of pregnancy, PRS polygenic risk score, ASCVD atherosclerotic cardiovascular disease, HR hazard ratio, CI confidence interval, sBP systolic blood pressure, dBP diastolic blood pressure.
Impact of HDP-PRS, lifestyle, and MetS on incident ASCVD
Participants with the highest expected risk having high (top 20%) PRS for HDP, unfavorable lifestyles, and poor metabolic health (MetS ≥ 4) exhibited substantially increased risk of developing ASCVD—3.60 times higher than that of participants having the lowest expected risk (P for trend < 2.20E-16) (Supplementary Table 12).
Overall, maintaining a favorable lifestyle was associated with a 58% reduction in the risk of incident ASCVD (Supplementary Table 7). Subgroup analyses indicated that this risk reduction was consistent across different genetic risk groups. Specifically, a combination of metabolic health and favorable lifestyle reduced the subsequent risk of ASCVD by 64.6% (HR, 0.354; 95% CI, 0.288–0.434; P < 2.20E-16) among those in the high-genetic risk category (top 20%) and by 65.4% (HR, 0.346; 95% CI, 0.269–0.445; P < 2.20E-16) among those in the low genetic risk group (bottom 20%) (Fig. 3 and Supplementary Fig. 7). Notably, in participants within the highest 20th percentile of the genetic risk for HDP who also had four or more components of MetS, adherence to a favorable lifestyle significantly lowered the ASCVD risk by 40% (Fig. 3). The analysis results for each ASCVD subtype are shown in Supplementary Figs. 8–10.
The polygenic risk score for hypertensive disorders of pregnancy (HDP) has been derived from the FinnGen Consortium. The high genetic risk group was defined as individuals in the top 20% of the polygenic risk score distribution, while the low genetic risk group was defined as those in the bottom 20%. No. Events indicate the number of ASCVD incidents that occurred in the UK Biobank. In the bar charts, bars represent ASCVD incidence rates per 1000 women-year, with vertical lines indicating 95% confidence intervals (CIs) (top panel). In the forest plots, boxes represent the adjusted hazard ratio, with horizontal lines around the boxes indicating 95% CIs (bottom panel). The hazard ratios were estimated using Cox proportional hazards models, adjusted for history of HDP, age, genotype array, and first ten principal components of ancestry. P-values were determined using a Wald test. P-values for interaction were derived from the multiplicative interaction analysis between genetic risk and lifestyle groups. All P-values were derived from two-sided tests. Exact statistical values are provided as a Source Data file. HDP hypertensive disorders of pregnancy, PRS polygenic risk score, ASCVD atherosclerotic cardiovascular disease, HR hazard ratio, CI confidence interval, MetS metabolic syndrome.
Replication analysis for incident hypertension in the PMBB cohort
We investigated the association between incident hypertension and HDP-PRS in a replication analysis conducted within the PMBB cohort. Due to the less average age of parous women in the PMBB cohort (mean age 32.7 years, SD 6.9 years) than that in the UKBB cohort (57.2 years, SD, 7.7 years), it was challenging to gather a sufficient number of ASCVD cases for replication. Therefore, our analysis focused on incident hypertension rather than on ASCVD.
In the PMBB replication cohort, 476 (23.8%) were diagnosed with incident hypertension during the follow-up period (33.12 occurrences per 1000 women years of follow-up). Using a multivariable Cox regression model and after adjusting for age at first live birth, history of HDP, and the first ten PCs of ancestry, we observed a significant association between the HDP-PRS and incident hypertension (HR 1.12 per 1 SD increase; 95% CI, 1.01–1.23; P = 0.028) (Supplementary Table 13).
Furthermore, we replicated the analysis to assess the impact of maintaining a favorable lifestyle on incident hypertension, regardless of the HDP genetic risk. Our findings showed that adherence to a favorable lifestyle significantly reduced the risk of incident hypertension (P for trend = 1.06E-09) across all the genetic risk groups, but no significant interactions were observed (Fig. 4 and Supplementary Fig. 11). Specifically, a favorable lifestyle led to a reduction in the risk of hypertension among those with high genetic risk (top 20%) (P for trend = 7.60E-04) and low genetic risk (bottom 20%) (P for trend = 1.03E-05) (Supplementary Fig. 12).
The polygenic risk score for hypertensive disorders of pregnancy (HDP) has been derived from the FinnGen Consortium. Lifestyle was defined by combining smoking status and obesity (body mass index ≥ 30 kg/m2), with each variable coded as 0/1 based on presence or absence, and summed to categorize individuals into three groups: 0 (Favorable), 1 (Intermediate), and 2 (Unfavorable). No. Events indicate the number of incidents of hypertension that occurred in the Penn Medicine Biobank. In the bar charts, bars represent hypertension incidence rates per 1000 women-year, with vertical lines indicating 95% confidence intervals (CIs) (top panel). In the forest plots, boxes represent the adjusted hazard ratio, with horizontal lines around the boxes indicating 95% CIs (bottom panel). The hazard ratios were estimated using Cox proportional hazards models, adjusted for history of HDP, age, ethnicity, and first ten principal components of ancestry. P-values were determined using a Wald test. The P-value for the trend was calculated using the Cochran-Armitage trend test. All P-values were derived from two-sided tests. Exact statistical values are provided as a Source Data file. BMI body mass index, HDP hypertensive disorders of pregnancy, PRS polygenic risk score, HTN hypertension, HR hazard ratio, CI confidence interval.
In subpopulation analysis within the PMBB, the impact of maintaining a favorable lifestyle consistently emerged as a significant factor in reducing the risk of incident hypertension across both groups (Supplementary Figs. 11 and 12).
Discussion
In this study, we aimed to assess the long-term association between HDP genetic risk, MetS, and lifestyle factors and ASCVD development in women with genetic risk for HDP. We observed a significant association between HDP-PRS and an increased risk of developing ASCVD in the UKBB cohort. Adherence to a favorable lifestyle or an ideal MetS status significantly reduced the risk of ASCVD, even in women with high genetic risk for HDP. Replication analysis of the PMBB cohort showed that a high PRS was associated with an increased likelihood of developing hypertension. This risk was exacerbated by a poor lifestyle but mitigated by a favorable lifestyle.
In middle-aged women, several factors, such as early menopause, hysterectomy, and adverse pregnancy outcomes have been recognized as specific risk factors for adverse CV outcomes27,28. With advancements in genetic research, women with a history of preeclampsia can be further stratified to high risk for ASCVD18. Individuals with high HDP-PRS scores were found to be more likely to develop ASCVD, a risk that remained significant even after adjustment for HDP. This highlights the importance of considering genetic factors when stratifying women for adverse CV health after delivery.
Indeed, there can be several underlying mechanisms behind the relationship between high PRS for HDP and later ASCVD. First, individuals with a genetic predisposition to HDP (high HDP-PRS) are more likely to develop ASCVD, regardless of whether they experienced HDP. Second, HDP itself may result in maternal endothelial damage, increasing vulnerability to later ASCVD. Third, shared risk factors such as high BP, diabetes, and obesity may contribute to this association. In a previous study, we reported that both HDP itself and genetic risk for HDP increase the risk of ASCVD18.
In the current study, we additionally showed that a healthy lifestyle can attenuate this risk. Our findings indicate that modifiable factors, such as MetS and lifestyle, play a crucial role in reducing the risk of ASCVD, particularly in women with high genetic risk for HDP. This study showed that the risk of developing ASCVD in women with high genetic risk could be reduced by 40% with a favorable lifestyle and ideal MetS status. In contrast, the risk of ASCVD development in women with low genetic risk was increased by approximately 3-fold in those following an unfavorable lifestyle and having poor metabolic health.
The findings of the current study are consistent with those of previous studies, suggesting several effective preventive measures against ASCVD8,9,10,11. Several studies have highlighted the critical role of lifestyle modification interventions, including diet, exercise, and smoking cessation, in preventing the onset and progression of ASCVD in high-risk populations such as those with morbid obesity or MetS29,30. The findings of the current study highlight the importance of comprehensive approaches that address both genetic predisposition and modifiable risk factors to effectively reduce the risk of developing ASCVD.
We also found that the comprehensive approach of genetic risk, lifestyle choices, and MetS status better predicted the risk of developing ASCVD. Individuals with very high HDP-PRS, who also exhibited unfavorable lifestyle habits or poor MetS status, had the highest risk of developing ASCVD. Nevertheless, even individuals with a low genetic risk for HDP also benefit from a healthy lifestyle, which substantially reduces this risk. The risk of developing ASCVD was reduced by up to 64.6% through the maintenance of an ideal MetS status and a healthy lifestyle in the high genetic risk group (top 20%), which was similar to the 65.4% reduction effect in low genetic risk group (bottom 20%). This underscores the importance of active lifestyle modifications both in high and low genetic risk groups in public health initiatives and individual efforts.
In the current study, we stratified patients according to the genetic risk for HDP, based on our previous work18. In our previous work, we generated PRS for HDP summary statistics from FinnGen from a study population of 4677 cases and 71,711 controls and showed that the PRS for HDP increased the risk of both HDP and subsequent ASCVD. In the current study, we generated new version of PRS for HDP using summary statistics from the recent FinnGen Consortium (Data Freeze R8v4) (13,071 cases and 177,808 controls) and also confirmed that the PRS for HDP increased the risk of both HDP and subsequent ASCVD. We believe that the effectiveness of PRS for HDP should be further validated in other ethnic study populations by other researchers.
Unfortunately, this study did not consider specific types of HDP, as distinguishing between gestational hypertension, preeclampsia, or eclampsia was not possible in the self-report system in the UKBB. In the study by Nurkkala et al., the polygenic risk for BP in preeclampsia showed a differential effect on the development of gestational hypertension and preeclampsia, which in turn may be differently associated with ASCVD risk31. We believe that further studies on the association between gestational hypertension, preeclampsia, and subsequent ASCVD risk will enhance our understanding of ASCVD pathophysiology and preventive strategies.
In addition, we evaluated whether a healthy lifestyle and favorable MetS status can modify the risk of ASCVD in individuals with high genetic risk for HDP. However, other PRS, such as those for BP or ASCVD, may be also used in predicting ASCVD risk. In the previous study, systolic BP-PRS was associated with a higher risk of incident CVD (adjusted HR, 1.07 [95% CI, 1.04–1.10])32. In our current study, HDP-PRS was similarly associated with incident ASCVD, with an adjusted HR of 1.09. In the fully adjusted model, this association remained significant—individuals with very high PRS had a 1.47-fold increased risk of ASCVD compared to those in the low-PRS group (95% CI, 1.18–1.83; P = 5.83E-04). The association between HDP-PRS and future ASCVD might be influenced by genetic factors by BP traits. However, previous studies reported that women with a history of HDP were more likely to develop ASCVD, and this risk is independent of future hypertension after pregnancy. In our study, we further demonstrated that the genetic predisposition to HDP (HDP-PRS) is significantly associated with ASCVD later in life, and this association remained significant even after adjusting for both hypertension and HDP itself. The next step involves adopting multiple PRS, as this has become a recent topic of interest in PRS research.
This study has some limitations. First, we evaluated the risk of ASCVD in the UKBB and PMBB cohorts, which are representative of only European and African-American populations. In addition, we focused on incident hypertension rather than on ASCVD in the PMBB cohort due to the relatively shorter follow-up period after delivery and the small number of cases with incident ASCVD. Because of these limitations, we could not assess the risk of ASCVD in the PMBB cohort. In addition, the relatively small sample size of the PMBB cohort is another limitation in interpreting the results. Therefore, more similar research is needed in Asian populations and other ethnicities.
To our knowledge, the current study is the first to evaluate the importance of lifestyle and MetS in preventing ASCVD in patients with high genetic risk for HDP using a large-scale prospective cohort. The findings from the UKBB can be further demonstrated using an external independent cohort in the United States. Replication analysis in an independent cohort further strengthens our findings, demonstrating that adherence to a favorable lifestyle consistently reduces the risk of hypertension, regardless of genetic risk. This provides additional evidence that lifestyle modifications have a broad preventive effect on CVD.
Methods
Ethics approval
This study complies with all relevant ethical regulations for research involving human participants and was conducted in accordance with the criteria set by the Declaration of Helsinki. The UKBB study was approved by the National Research Ethics Committee (June 17, 2011 [RES Reference11 /NW/0382] and was extended on May 10, 2016 [RES Reference16 /NW/0274]). The collection, storage, and analyses of biospecimens, genetic data, and data derived from electronic health records as part of the PMBB study is approved under the University of Pennsylvania IRB protocol #813913. Participants from the UKBB and PMBB cohorts provided written informed consent allowing for the use of their samples and data for medical research purposes. The use of de-identified data from these biobanks for this specific research was covered under the existing approvals. All data was handled in accordance with relevant data protection and privacy regulations. No additional ethical approval was required for this specific analysis of existing approved datasets. This study adhered to the requirements of the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement.
Study population
The UKBB is a large prospective observational cohort study that recruited over 500,000 adults from 22 centers across the United Kingdom between 2006 and 2010. Participants aged 40–69 years were enrolled and have been followed for subsequent health events. The UKBB collected extensive baseline data, including demographics, lifestyle factors, and physical measurements, alongside biological samples for genotyping and biomarker analysis. For the present study, we included women of European descent who had at least one live birth and available genetic data. The full protocol of the UKBB study is publicly available for reference33.
The PMBB study (i.e., a large-scale academic medical biobank) non-selectively recruited participants from outpatient settings. These participants provided access to their electronic health record data and generated genomic and biomarker data34. All International Classification of Diseases (ICD)-9 and ICD-10 diagnostic codes, clinical imaging, and laboratory measurements up to July 2020 were extracted from the electronic health records. The workflows underlying this study are illustrated in Supplementary Figs. 1 and 2.
Hypertensive disorders of pregnancy and comorbidities
In the UKBB study, female participants provided details about their reproductive history, including parity, during a baseline survey. HDP was defined as gestational hypertension, preeclampsia, eclampsia, or superimposed preeclampsia. This identification was based on self-reports at enrollment or the corresponding ICD codes obtained from primary care or hospital records (Supplementary Table 14). Similarly, in the PMBB study, HDP was defined using relevant ICD codes.
To evaluate HDP risk according to the HDP-PRS, age at first pregnancy and the presence of a disease conferring high risk for HDP before pregnancy were selected as covariates, consistent with the clinical guidelines for high-risk factors for HDP35,36. According to these guidelines, high HDP-risk diseases include hypertension, diabetes mellitus, and dyslipidemia. The presence of a high-risk HDP disease before pregnancy was determined by either self-reporting or diagnosis with relevant ICD codes for each disease (Supplementary Table 15) that occurred before the first live birth.
Cardiovascular outcomes
To analyze incident ASCVD and its association with HDP-PRS, participants with congenital heart disease were excluded to eliminate the possible association between congenital heart disease and CV outcomes (Supplementary Methods contains the relevant diagnosis codes). Prevalent metabolic comorbidities, including hypertension, diabetes mellitus, and dyslipidemia, were used as adjusting covariates and were ascertained either by self-reporting at enrollment or by ICD codes, as described in Supplementary Methods.
Incident ASCVD was defined as a diagnosis of coronary artery disease, myocardial infarction, ischemic stroke, peripheral artery disease, or aortic aneurysm after enrollment of participants without preexisting CVD. In addition, myocardial infarction was algorithmically defined using the UKBB data. For each new-onset ASCVD considered, participants with a preexisting disease at enrollment were excluded from the analysis. For example, participants with preexisting coronary artery disease at enrollment were excluded from the analysis of new-onset coronary artery disease, which ensured that recurrent coronary artery disease was not erroneously counted as new-onset coronary artery disease.
Variables
During the enrollment process in the UKBB study, participants provided information about their sociodemographic characteristics, health/medical history, and lifestyle/environmental factors through a self-administered touchscreen questionnaire and in-person baseline interviews.
According to the AHA, four factors primarily define lifestyle behaviors; these include current smoking status, obesity, physical activity, and eating habits37,38. Smoking status was classified as current smoker or non-smoker. Obesity was defined as a BMI ≥ 30 kg/m2 according to the World Health Organization international classification. With respect to physical activity, participants were classified as having a healthy lifestyle if they reported more than five days per week of moderate or vigorous activity. Eating habits were defined following the recommendations on dietary priorities for CV health, which categorized common dietary components as fruits, vegetables, whole grains, fish, dairy, refined grains, processed meats, and unprocessed meats. Eating habits were considered healthy if participants adhered to at least half of the dietary recommendations for CV health, as assessed using a food frequency questionnaire39. Collectively, lifestyle behaviors were categorized into three groups—unfavorable (0–1 healthy lifestyle factor)40, intermediate (2 healthy lifestyle factors), and favorable ( ≥ 3 healthy lifestyle factors). More detailed descriptions and definitions of the variables considered in lifestyle behaviors can be found in Supplementary Methods.
Metabolic health status was identified according to the presence of the five components of MetS based on criteria from the IDF consensus report41. Metabolic health status was categorized into three groups—ideal (0–1 MetS factor), intermediate (2–3 MetS factors), and poor (≥ 4 MetS factors). Detailed descriptions and definitions of the variables considered in MetS can be found in Supplementary Table 16 and Supplementary Methods.
In the PMBB cohort, smoking status and obesity (BMI ≥ 30) were restrictively used as variables for the replication analysis.
Genotype data quality control and imputation
Genotyping and quality control (QC) procedures and imputation followed standard practices and were performed using a cohort genotyping platform pair. Further details are provided in Supplementary Methods.
UK Biobank
UKBB samples (version 3; March 2018) were genotyped for more than 800,000 SNPs using either the Affymetrix UK BiLEVE Axiom array or the Affymetrix UKBB Axiom array. After QC and imputation, 164,500 European (White British) female participants were found to be eligible for validation genetic analyses.
Penn Medicine Biobank
The PMBB data consisted of 43,623 samples that were genotyped using a GSA genotyping array. After exclusion, 982 parous women participants with European (non-Hispanic White) ancestry and 1019 parous women participants with African American (non-Hispanic Black) ancestry were considered eligible for the replication analysis.
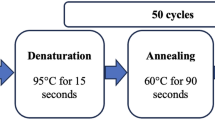
Polygenic risk score
The HDP-PRS was generated using summary statistics of a large-scale HDP GWAS (13,071 cases and 177,808 controls) from the FinnGen Consortium (Data Freeze R8v4)42. The PRS was calculated using the Bayesian polygenic prediction method PRS-CS43. Individual PRSs were determined by applying PLINK version 1.90 using the --score command and were computed from beta coefficients as the weighted sum of the risk alleles44. The details of PRS analysis are described in Supplementary Methods.
Statistical analysis
Demographic and clinical characteristics are presented as mean ± SD or number (percentage). Continuous variables were compared using Student’s t test, one-way ANOVA, or the Mann-Whitney U test, as appropriate. Categorical variables were compared using the chi-squared test or Fisher’s exact test, as appropriate.
To evaluate the risk of HDP according to the HDP-PRS, we used a multivariate logistic regression model to evaluate the association between HDP-PRS and HDP. We calculated the OR and 95% CI after adjusting for age at first live birth, BMI, smoking status, first ten PCs of ancestry, and genotyping array type in the multivariate logistic regression model.
In the primary analysis, the association between HDP-PRS and new-onset CV outcomes was examined using the multivariate Cox regression analysis. Adjustments were made for a history of HDP, age at first live birth, BMI, smoking status, first ten PCs of ancestry, and genotype array to calculate the HR and 95% CIs. The ORs and HRs of the PRSs for HDP were used as quantitative variables reported per SD, and the categorical variables were defined as follows: low (< 20%), intermediate (20–80%), high (80–99%), and very high (>99%). Subsequently, we conducted joint association analyses to investigate the interplay between genetic risk, lifestyle, and MetS status. In addition, we performed sensitivity analyses based on the ASCVD subtypes.
For the replication analysis, the impact of maintaining a favorable lifestyle across different genetic risk groups was studied using the chi-square test and Cox regression analysis in an independent PMBB cohort. Among 2001 parous women in the PMBB cohort, cases with new-onset ASCVD were few, but conditional Cox regression analysis was feasible for incident hypertension, considering smoking status and obesity (BMI ≥ 30) as lifestyle variables.
All statistical tests were two-sided, and statistical significance was set at P < 0.05. All statistical analyses were conducted using the R Statistical Software (version 4.1.0; R Foundation for Statistical Computing, Vienna, Austria) and PLINK version 1.9044. The details of statistical analyses are described in Supplementary Methods.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The UK Biobank data utilized in this study include clinical, genetic, and biomarker datasets (https://www.ukbiobank.ac.uk/enable-your-research/about-our-data/). The UK Biobank data are available to researchers with research inquiries following IRB and UK Biobank approval (https://www.ukbiobank.ac.uk/enable-your-research/apply-for-access). This research was conducted using the UK Biobank Resource under Application Number 68416. The genotype and phenotype data utilized in this study from the Penn Medicine Biobank are available under restricted access for authorized researchers, as they represent sensitive patient data. Access can be obtained by applying through the following link: https://pmbb.med.upenn.edu/investigators.php. The LD reference panels built with 1000 Genomes Project phase 3 samples are available at https://github.com/getian107/PRScs. The GWAS used for HDP-PRS construction in this study is available in part of release 8 of FinnGen (https://r8.finngen.fi/pheno/O15_HYPTENSPREG). Source data are provided in this paper.
Code availability
The HDP-PRS model developed and described in this study is publicly available for download from the GitHub repository https://github.com/dokyoonkimlab/hdp-prs-finngen-r8, and the Zenodo repository https://doi.org/10.5281/zenodo.14211027.
References
Wu, P., Green, M. & Myers, J. E. Hypertensive disorders of pregnancy. BMJ 381, e071653 (2023).
Tita, A. T. et al. Treatment for mild chronic hypertension during pregnancy. N. Engl. J. Med. 386, 1781–1792 (2022).
Barry, M. J. et al. Screening for hypertensive disorders of pregnancy: US Preventive Services Task Force final recommendation statement. JAMA 330, 1074–1082 (2023).
Rolnik, D. L., Nicolaides, K. H. & Poon, L. C. Prevention of preeclampsia with aspirin. Am. J. Obstet. Gynecol. 226, S1108–S1119 (2022).
Ahn, T. G. & Hwang, J. Y. Preeclampsia and aspirin. Obstet. Gynecol. Sci. 66, 120–132 (2023).
Lee, K. H. et al. Long-term renal outcome after hypertensive disease during pregnancy: a nationwide population-based study. Obstet. Gynecol. Sci. 66, 190–197 (2023).
Bellamy, L., Casas, J.-P., Hingorani, A. D. & Williams, D. J. Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ 335, 974 (2007).
Haug, E. B. et al. Association of conventional cardiovascular risk factors with cardiovascular disease after hypertensive disorders of pregnancy: analysis of the Nord-Trøndelag Health Study. JAMA Cardiol. 4, 628–635 (2019).
Grandi, S. M. et al. Cardiovascular disease-related morbidity and mortality in women with a history of pregnancy complications: systematic review and meta-analysis. Circulation 139, 1069–1079 (2019).
Makkonen, N., Harju, M. & Kirkinen, P. Postpartum recovery after severe pre-eclampsia and HELLP syndrome. J. Perinat. Med. 24, 641–649 (1996).
Ruschitzka, F., Schulz, E., Kling, H., Schrader, J. & Rath, W. Longitudinal study of 24-hour blood pressure behavior in pregnancy and puerperium in patients with normal pregnancy, pre-eclampsia, and HELLP syndrome. Z. Geburtshilfe Neonatol. 200, 100–103 (1996).
Stuart, J. J. et al. Cardiovascular risk factors mediate the long-term maternal risk associated with hypertensive disorders of pregnancy. J. Am. Coll. Cardiol. 79, 1901–1913 (2022).
Khosla, K. et al. Long-term cardiovascular disease risk in women after hypertensive disorders of pregnancy: recent advances in hypertension. Hypertension 78, 927–935 (2021).
Mosca, L. et al. Effectiveness-based guidelines for the prevention of cardiovascular disease in women—2011 update: a guideline from the American Heart Association. Circulation 123, 1243–1262 (2011).
Honigberg, M. C. et al. Long-term cardiovascular risk in women with hypertension during pregnancy. J. Am. Coll. Cardiol. 74, 2743–2754 (2019).
Honigberg, M. C. et al. Polygenic prediction of preeclampsia and gestational hypertension. Nat. Med. 29, 1540–1549 (2023).
Qu, K. et al. Hypertensive disorders of pregnancy and stroke: a univariate and multivariate Mendelian randomization study. Front. Endocrinol. 15, 1366023 (2024).
Lee, S. M. et al. Genome-wide polygenic risk scores for hypertensive disorders of pregnancy can also predict the risk for long-term cardiovascular disease. Am. J. Obstet. Gynecol. 229, 298 (2023).
Global Cardiovascular Risk Consortium. Global effect of modifiable risk factors on cardiovascular disease and mortality. N. Engl. J. Med. 389, 1273–1285 (2023).
Yusuf, S. et al. Modifiable risk factors, cardiovascular disease, and mortality in 155,722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet 395, 795–808 (2020).
Kim, H. L. et al. Lifestyle modification in the management of metabolic syndrome: statement from Korean Society of CardioMetabolic Syndrome (KSCMS). Korean Circ. J. 52, 93–109 (2022).
Yamaoka, K. & Tango, T. Effects of lifestyle modification on metabolic syndrome: a systematic review and meta-analysis. BMC Med. 10, 1–10 (2012).
Watanabe, M. et al. Effects of a lifestyle modification programme to reduce the number of risk factors for metabolic syndrome: a randomised controlled trial. Public Health Nutr. 20, 142–153 (2017).
Wu, P., Park, K. & Gulati, M. The fourth trimester: pregnancy as a predictor of cardiovascular disease. Eur. Cardiol. Rev. 16, e31 (2021).
Grundy, S. M. Drug therapy of the metabolic syndrome: minimizing the emerging crisis in polypharmacy. Nat. Rev. Drug Discov. 5, 295–309 (2006).
astro-Barquero, S., Ruiz-León, A. M., Sierra-Pérez, M., Estruch, R. & Casas, R. Dietary strategies for metabolic syndrome: a comprehensive review. Nutrients 12, 2983 (2020).
O’Kelly, A. C. et al. Pregnancy and reproductive risk factors for cardiovascular disease in women. Circ. Res. 130, 652–672 (2022).
Freaney, P. M., Khan, S. S., Lloyd-Jones, D. M. & Stone, N. J. The role of sex-specific risk factors in the risk assessment of atherosclerotic cardiovascular disease for primary prevention in women. Curr. Atheroscler. Rep. 22, 1–11 (2020).
Sperling, L. S. et al. The cardiometabolic health alliance: working toward a new care model for the metabolic syndrome. J. Am. Coll. Cardiol. 66, 1050–1067 (2015).
Grundy, S. M. Metabolic syndrome update. Trends Cardiovasc. Med. 26, 364–373 (2016).
Nurkkala, J. et al. Associations of polygenic risk scores for preeclampsia and blood pressure with hypertensive disorders of pregnancy. J. Hypertens. 41, 380–387 (2023).
Parcha, V. et al. Association of a multiancestry genome-wide blood pressure polygenic risk score with adverse cardiovascular events. Circ. Genom. Precis. Med. 15, e003946 (2022).
Bycroft, C. et al. The UK Biobank resource with deep phenotyping and genomic data. Nature 562, 203–209 (2018).
Verma, A. et al. The Penn Medicine BioBank: Towards a genomics-enabled learning healthcare system to accelerate precision medicine in a diverse population. J. Pers. Med. 12, 1974 (2022).
LeFevre, M. L. & Preventive Services Task Force, U. S. Low-dose aspirin use for the prevention of morbidity and mortality from preeclampsia: US Preventive Services Task Force recommendation statement. Ann. Intern. Med. 161, 819–826 (2014).
Hod, M. et al. The international federation of gynecology and obstetrics (FIGO) initiative on gestational diabetes mellitus: a pragmatic guide for diagnosis, management, and care. Int. J. Gynecol. Obstet. 131, S173–S211 (2015).
Lloyd-Jones, D. M. et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation 121, 586–613 (2010).
Khera, A. V. et al. Genetic risk, adherence to a healthy lifestyle, and coronary disease. N. Engl. J. Med. 375, 2349–2358 (2016).
Mozaffarian, D. Dietary and policy priorities for cardiovascular disease, diabetes, and obesity: a comprehensive review. Circulation 133, 187–225 (2016).
Collaborators, G. R. F. Global, regional, and national comparative risk assessment of 84 behavioural, environmental, and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392, 1923–1994 (2018).
Alberti, K. G. et al. Harmonizing the metabolic syndrome: a joint interim statement of the international diabetes federation task force on epidemiology and prevention; national heart, lung, and blood institute; American heart association; world heart federation; international atherosclerosis society; and international association for the study of obesity. Circulation 120, 1640–1645 (2009).
Kurki, M. I. et al. FinnGen provides genetic insights from a well-phenotyped isolated population. Nature 613, 508–518 (2023).
Ge, T., Chen, C.-Y., Ni, Y., Feng, Y.-C. A. & Smoller, J. W. Polygenic prediction via Bayesian regression and continuous shrinkage priors. Nat. Commun. 10, 1776 (2019).
Chang, C. C. et al. Second-generation PLINK: rising to the challenge of larger and richer datasets. Gigascience 4, https://doi.org/10.1186/s13742-015-0047-8 (2015).
Acknowledgements
This work was supported by the National Institute of Health (R01 GM138597 and R01 HL169458, awarded to DK). This research was also supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. NRF-2021R1F1A1046707, awarded to S.L.) and Seoul National University Hospital research fund (0420240280, awarded to S.L.). This research has been conducted using the UK Biobank Resource under Application Number 68416. We thank the participants who contributed their data in the UK Biobank study. We want to acknowledge the participants and investigators of the FinnGen study. We also acknowledge the Penn Medicine Biobank for providing data and thank the patient-participants of Penn Medicine who consented to participate in this research program. We would like to thank the Penn Medicine Biobank team and Regeneron Genetics Center for providing genetic variant data for analysis.
Author information
Authors and Affiliations
Contributions
S.-H.J., H.K., D.K., and S.L. conceived and designed the study. S.-H.J. performed the genetic data analyses. S.-H.J. and H.K. conducted statistical analyses and drafted the manuscript. Y.J., M.S., and B.X. curated and organized the data. J.K., B.J., and J.-S.Y. performed data pre-processing, including quality control and formatting. S.-H.J. interpreted the data. H.-H.W., C.-W.P., J.P., and J.J. critically reviewed and revised the manuscript for intellectual content. All authors read and approved the final manuscript. S.-H.J. and H.K. contributed equally to this work. D.K. and S.L. jointly supervised this work.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interest.
Peer review
Peer review information
Nature Communications thanks Seung-Pyo Lee, David Williams, and the other anonymous reviewer for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jung, S., Kim, H., Jung, Y.M. et al. Healthy lifestyle reduces cardiovascular risk in women with genetic predisposition to hypertensive disorders of pregnancy. Nat Commun 16, 1463 (2025). https://doi.org/10.1038/s41467-025-56107-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-025-56107-2