Abstract
Increasing evidence suggested the multifactorial nature of nocturia, but the true pathogenesis of this condition still remains to be elucidated. Contemporary clinical medications are mostly symptom based, aimed at either reducing nocturnal urine volume or targeting autonomic receptors within the bladder to facilitate urine storage. The day–night switch of the micturition pattern is controlled by circadian clocks located both in the central nervous system and in the peripheral organs. Arousal threshold and secretion of melatonin and vasopressin increase at night-time to achieve high-quality sleep and minimize nocturnal urine production. In response to the increased vasopressin, the kidney reduces the glomerular filtration rate and facilitates the reabsorption of water. Synchronously, in the bladder, circadian oscillation of crucial molecules occurs to reduce afferent sensory input and maintain sufficient bladder capacity during the night sleep period. Thus, nocturia might occur as a result of desynchronization in one or more of these circadian regulatory mechanisms. Disrupted rhythmicity of the central nervous system, kidney and bladder (known as the brain–kidney–bladder circadian axis) contributes to the pathogenesis of nocturia. Novel insights into the chronobiological nature of nocturia will be crucial to promote a revolutionary shift towards effective therapeutics targeting the realignment of the circadian rhythm.
Key points
-
Growing evidence has shown that disrupted rhythmicity of the central nervous system, kidney and bladder (the brain–kidney–bladder circadian axis) contributes to the pathogenesis of nocturia.
-
The daily rhythm of human behaviour and physiology is regulated by the transcription–translation feedback loop, which exists both in the brain and in peripheral metabolic tissues, consisting of opposite transcriptional activators (CLOCK and BMAL1) and repressors (PER and CRY).
-
Disruption of the central clock in the suprachiasmatic nucleus and neuroendocrine system leads to nocturia through impaired sleep quality and misaligned release of hormones such as melatonin and arginine vasopressin.
-
Most physiological renal processes, such as urine secretion and water reabsorption, follow a circadian pattern of activity; disruptions of this pattern can cause nocturia.
-
The circadian expression of peripheral clock genes in the bladder leads to time-dependent variations of bladder sensation and excitability, which can be disorganized under pathophysiological conditions contributing to nocturia onset.
-
Expanding knowledge of the molecular basis of circadian regulation and dysregulation within the brain–kidney–bladder circadian axis will help to develop strategies for the prevention, management and treatment of nocturia based on chronobiology.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
27,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
209,00 € per year
only 17,42 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Hashim, H. et al. International Continence Society (ICS) report on the terminology for nocturia and nocturnal lower urinary tract function. Neurourol. Urodyn. 38, 499–508 (2019).
Dani, H., Esdaille, A. & Weiss, J. P. Nocturia: aetiology and treatment in adults. Nat. Rev. Urol. 13, 573–583 (2016).
Hashim, H. & Drake, M. J. Basic concepts in nocturia, based on International Continence Society standards in nocturnal lower urinary tract function. Neurourol. Urodyn. 37, S20–S24 (2018).
Nakagawa, H. et al. Impact of nocturia on bone fracture and mortality in older individuals: a Japanese Longitudinal Cohort Study. J. Urol. 184, 1413–1418 (2010).
Obayashi, K., Saeki, K., Negoro, H. & Kurumatani, N. Nocturia increases the incidence of depressive symptoms: a longitudinal study of the HEIJO-KYO cohort. BJU Int. 120, 280–285 (2017).
Funada, S. et al. Impact of nocturia on mortality: the Nagahama Study. J. Urol. 204, 996–1002 (2020).
Bliwise, D. L., Wagg, A. & Sand, P. K. Nocturia: a highly prevalent disorder with multifaceted consequences. Urology 133S, 3–13 (2019).
Azuero, J. et al. Potential associations of adult nocturia. Results from a national prevalence study. Neurourol. Urodyn. 40, 819–828 (2021).
Lazar, J. M. et al. Nocturia is associated with high atherosclerotic cardiovascular disease risk in women: results from the National Health and Nutrition Examination Survey. J. Community Health 46, 854–860 (2021).
Bosch, J. L. H. R. & Weiss, J. P. The prevalence and causes of nocturia. J. Urol. 189, S86–S92 (2013).
Malde, S. et al. Incidence of nocturia in men with lower urinary tract symptoms associated with benign prostatic enlargement and outcomes after medical treatment: results from the Evolution European Association of Urology Research Foundation Prospective Multinational Registry. Eur. Urol. Focus. 7, 178–185 (2021).
Song, Q. X. et al. The characteristics and risk factors of healthcare-seeking men with lower urinary tract symptoms in China: initial report from the POInT group. Neurourol. Urodyn. 40, 1740–1753 (2021).
Daugherty, M., Ginzburg, N. & Byler, T. Prevalence of nocturia in United States women: results from National Health and Nutrition Examination Survey. Female Pelvic Med. Reconstr. Surg. 27, e52–e58 (2021).
Dutoglu, E. et al. Nocturia and its clinical implications in older women. Arch. Gerontol. Geriatr. 85, 103917 (2019).
Bower, W. F. et al. The association between nocturia, hormonal symptoms and bladder parameters in women: an observational study. BJOG 129, 812–819 (2022).
Song, Q., Abrams, P. & Sun, Y. Beyond prostate, beyond surgery and beyond urology: The “3Bs” of managing non-neurogenic male lower urinary tract symptoms. Asian J. Urol. 6, 169–173 (2019).
Chapple, C. R. et al. Lower urinary tract symptoms revisited: a broader clinical perspective. Eur. Urol. 54, 563–569 (2008).
Abrams, P. New words for old: lower urinary tract symptoms for “prostatism”. BMJ 308, 929–930 (1994).
Haga, N. et al. Postoperative urinary incontinence exacerbates nocturia-specific quality of life after robot-assisted radical prostatectomy. Int. J. Urol. 23, 873–878 (2016).
Seki, N., Yuki, K., Takei, M., Yamaguchi, A. & Naito, S. Analysis of the prognostic factors for overactive bladder symptoms following surgical treatment in patients with benign prostatic obstruction. Neurourol. Urodyn. 28, 197–201 (2009).
Smith, A. L. & Wein, A. J. Outcomes of pharmacological management of nocturia with non-antidiuretic agents: does statistically significant equal clinically significant? BJU Int. 107, 1550–1554 (2011).
Araujo, A. B. et al. Sleep related problems and urological symptoms: testing the hypothesis of bidirectionality in a longitudinal, population based study. J. Urol. 191, 100–106 (2014).
Negoro, H. et al. Risk analyses of nocturia on incident poor sleep and vice versa: the Nagahama study. Sci. Rep. 13, 9495 (2023).
Djavan, B., Milani, S., Davies, J. & Bolodeoku, J. The impact of tamsulosin oral controlled absorption system (OCAS) on nocturia and the quality of sleep: preliminary results of a pilot study. Eur. Urol. Suppl. 4, 61–68 (2005).
Schneider, T. & Stanley, N. Impact of nocturia on sleep and energy. Eur. Urol. Suppl. 6, 585–593 (2007).
Hirshkowitz, M. Normal human sleep: an overview. Med. Clin. N. Am. 88, 551–565 (2004).
Stanley, N. The physiology of sleep and the impact of ageing. Eur. Urol. Suppl. 3, 17–23 (2005).
Papworth, E. et al. Association of sleep disorders with nocturia: a systematic review and nominal group technique consensus on primary care assessment and treatment. Eur. Urol. Focus. 8, 42–51 (2022).
Umlauf, M. G. & Chasens, E. R. Sleep disordered breathing and nocturnal polyuria: nocturia and enuresis. Sleep. Med. Rev. 7, 403–411 (2003).
Umlauf, M. G. et al. Obstructive sleep apnea, nocturia and polyuria in older adults. Sleep 27, 139–144 (2004).
Doyle-McClam, M., Shahid, M. H., Sethi, J. M. & Koo, P. Nocturia in women with obstructive sleep apnea. Am. J. Lifestyle Med. 15, 260–268 (2021).
McInnis, R. P., Dodds, E. B., Johnsen, J., Auerbach, S. & Pyatkevich, Y. CPAP treats enuresis in adults with obstructive sleep apnea. J. Clin. Sleep. Med. 13, 1209–1212 (2017).
Weiss, J. P. & Everaert, K. Management of nocturia and nocturnal polyuria. Urology 133S, 24–33 (2019).
Tyagi, S. & Chancellor, M. B. Nocturnal polyuria and nocturia. Int. Urol. Nephrol. 55, 1395–1401 (2023).
van Kerrebroeck, P. et al. The standardisation of terminology in nocturia: report from the standardisation sub-committee of the International Continence Society. Neurourol. Urodyn. 21, 179–183 (2002).
Weiss, J. P., van Kerrebroeck, P. E., Klein, B. M. & Norgaard, J. P. Excessive nocturnal urine production is a major contributing factor to the etiology of nocturia. J. Urol. 186, 1358–1363 (2011).
Goessaert, A. S., Krott, L., Hoebeke, P., Vande Walle, J. & Everaert, K. Diagnosing the pathophysiologic mechanisms of nocturnal polyuria. Eur. Urol. 67, 283–288 (2015).
Hervé, F. et al. Is our current understanding and management of nocturia allowing improved care? International Consultation on Incontinence‐Research Society 2018. Neurourol. Urodyn. 38, S127–S133 (2019).
Emeruwa, C. J., Epstein, M. R., Michelson, K. P., Monaghan, T. F. & Weiss, J. P. Prevalence of the nocturnal polyuria syndrome in men. Neurourol. Urodyn. 39, 1732–1736 (2020).
Drangsholt, S. et al. Diagnosis and management of nocturia in current clinical practice: who are nocturia patients, and how do we treat them? World J. Urol. 37, 1389–1394 (2019).
Gulur, D. M., Mevcha, A. M. & Drake, M. J. Nocturia as a manifestation of systemic disease. BJU Int. 107, 702–713 (2011).
Ohishi, M., Kubozono, T., Higuchi, K. & Akasaki, Y. Hypertension, cardiovascular disease, and nocturia: a systematic review of the pathophysiological mechanisms. Hypertens. Res. 44, 733–739 (2021).
Everaert, K. et al. International Continence Society consensus on the diagnosis and treatment of nocturia. Neurourol. Urodyn. 38, 478–498 (2019).
Fine, N. D., Weiss, J. P. & Wein, A. J. Nocturia: consequences, classification, and management. F1000Res. 6, 1627–1627 (2017).
Drangsholt, S. et al. Diagnosis and management of nocturia in current clinical practice: who are nocturia patients, and how do we treat them? World J. Urol., 37, 1389–1394 (2019).
Gordon, D. J., Emeruwa, C. J. & Weiss, J. P. Management strategies for nocturia. Curr. Urol. Rep. 20, 75 (2019).
Yap, T. L., Brown, C., Cromwell, D. A., van der Meulen, J. & Emberton, M. The impact of self-management of lower urinary tract symptoms on frequency-volume chart measures. BJU Int. 104, 1104–1108 (2009).
Robinson, D., Giarenis, I. & Cardozo, L. You are what you eat: the impact of diet on overactive bladder and lower urinary tract symptoms. Maturitas 79, 8–13 (2014).
Robinson, D., Hanna-Mitchell, A., Rantell, A., Thiagamoorthy, G. & Cardozo, L. Are we justified in suggesting change to caffeine, alcohol, and carbonated drink intake in lower urinary tract disease? Report from the ICI-RS 2015. Neurourol. Urodyn. 36, 876–881 (2017).
Majumdar, A., Hassan, I., Saleh, S. & Toozs-Hobson, P. Inpatient bladder retraining: is it beneficial on its own? Int. Urogynecol. J. 21, 657–663 (2010).
Kaga, K. et al. The efficacy of compression stockings on patients with nocturia: a single-arm pilot study. Cureus 14, e28603 (2022).
Miyazato, M. et al. Effect of continuous positive airway pressure on nocturnal urine production in patients with obstructive sleep apnea syndrome. Neurourol. Urodyn. 36, 376–379 (2017).
Sakalis, V. I. et al. Medical treatment of nocturia in men with lower urinary tract symptoms: systematic review by the European Association of Urology Guidelines Panel for Male Lower Urinary Tract Symptoms. Eur. Urol. 72, 757–769 (2017).
Garrison, S. R. et al. Tolerability of bedtime diuretics: a prospective cohort analysis. BMJ Open 13, e068188 (2023).
Hillier, P., Knapp, M. S. & Cove-Smith, R. Circadian variations in urine excretion in chronic renal failure. Q. J. Med. 49, 461–478 (1980).
Singh, R. K., Bansal, A., Bansal, S. K. & Rai, S. P. Circadian rhythms of common laboratory profiles in serum and urine of healthy Indians. Prog. Clin. Biol. Res. 341B, 559–566 (1990).
Asplund, R. & Aberg, H. E. Micturition habits of older people. Voiding frequency and urine volumes. Scand. J. Urol. Nephrol. 26, 345–349 (1992).
Duffy, J. F., Scheuermaier, K. & Loughlin, K. R. Age-related sleep disruption and reduction in the circadian rhythm of urine output: contribution to nocturia? Curr. Aging Sci. 9, 34–43 (2016).
Smolensky, M. H., Hermida, R. C., Reinberg, A., Sackett-Lundeen, L. & Portaluppi, F. Circadian disruption: new clinical perspective of disease pathology and basis for chronotherapeutic intervention. Chronobiol. Int. 33, 1101–1119 (2016).
Patke, A., Young, M. W. & Axelrod, S. Molecular mechanisms and physiological importance of circadian rhythms. Nat. Rev. Mol. Cell Biol. 21, 67–84 (2020).
Greco, C. M. & Sassone-Corsi, P. Circadian blueprint of metabolic pathways in the brain. Nat. Rev. Neurosci. 20, 71–82 (2019).
Lu, Q. & Kim, J. Y. Mammalian circadian networks mediated by the suprachiasmatic nucleus. FEBS J. 289, 6589–6604 (2022).
Panda, S. Circadian physiology of metabolism. Science 354, 1008–1015 (2016).
Bass, J. Circadian topology of metabolism. Nature 491, 348–356 (2012).
Bass, J. & Takahashi, J. S. Circadian integration of metabolism and energetics. Science 330, 1349–1354 (2010).
Dibner, C., Schibler, U. & Albrecht, U. The mammalian circadian timing system: organization and coordination of central and peripheral clocks. Annu. Rev. Physiol. 72, 517–549 (2010).
Asher, G. & Schibler, U. Crosstalk between components of circadian and metabolic cycles in mammals. Cell Metab. 13, 125–137 (2011).
Gumz, M. L. et al. Toward precision medicine: circadian rhythm of blood pressure and chronotherapy for hypertension — 2021 NHLBI Workshop Report. Hypertension 80, 503–522 (2023).
Stenvers, D. J., Scheer, F., Schrauwen, P., la Fleur, S. E. & Kalsbeek, A. Circadian clocks and insulin resistance. Nat. Rev. Endocrinol. 15, 75–89 (2019).
Lekkas, D. & Paschos, G. K. The circadian clock control of adipose tissue physiology and metabolism. Auton. Neurosci. 219, 66–70 (2019).
McCauley, J. P. et al. Circadian modulation of neurons and astrocytes controls synaptic plasticity in hippocampal area CA1. Cell Rep. 33, 108255 (2020).
Gerstner, J. R. & Yin, J. C. Circadian rhythms and memory formation. Nat. Rev. Neurosci. 11, 577–588 (2010).
Shiju, S. & Sriram, K. Multi-scale modeling of the circadian modulation of learning and memory. PLoS ONE 14, e0219915 (2019).
Crock, L. W. et al. Metabotropic glutamate receptor 5 (mGluR5) regulates bladder nociception. Mol. Pain. 8, 20 (2012).
Ochodnicky, P. et al. Bradykinin modulates spontaneous nerve growth factor production and stretch-induced ATP release in human urothelium. Pharmacol. Res. 70, 147–154 (2013).
Uy, J. et al. Glutamatergic mechanisms involved in bladder overactivity and pudendal neuromodulation in cats. J. Pharmacol. Exp. Ther. 362, 53–58 (2017).
Yokoyama, O., Yoshiyama, M., Namiki, M. & de Groat, W. C. Role of the forebrain in bladder overactivity following cerebral infarction in the rat. Exp. Neurol. 163, 469–476 (2000).
Xie, Z. et al. A review of sleep disorders and melatonin. Neurol. Res. 39, 559–565 (2017).
Yanar, K., Simsek, B. & Cakatay, U. Integration of melatonin related redox homeostasis, aging, and circadian rhythm. Rejuvenation Res. 22, 409–419 (2019).
Rutter, J., Reick, M. & McKnight, S. L. Metabolism and the control of circadian rhythms. Annu. Rev. Biochem. 71, 307–331 (2002).
Huang, W., Ramsey, K. M., Marcheva, B. & Bass, J. Circadian rhythms, sleep, and metabolism. J. Clin. Invest. 121, 2133–2141 (2011).
Boivin, D. B. & Boudreau, P. Impacts of shift work on sleep and circadian rhythms. Pathol. Biol. 62, 292–301 (2014).
Gabriel, B. M. & Zierath, J. R. Circadian rhythms and exercise — re-setting the clock in metabolic disease. Nat. Rev. Endocrinol. 15, 197–206 (2019).
Boivin, D. B., Boudreau, P. & Kosmadopoulos, A. Disturbance of the circadian system in shift work and its health impact. J. Biol. Rhythm. 37, 3–28 (2022).
Bolsius, Y. G. et al. The role of clock genes in sleep, stress and memory. Biochem. Pharmacol. 191, 114493 (2021).
Huang, Y., Wang, H., Li, Y., Tao, X. & Sun, J. Poor sleep quality is associated with dawn phenomenon and impaired circadian clock gene expression in subjects with type 2 diabetes mellitus. Int. J. Endocrinol. 2017, 4578973 (2017).
Matsumoto, T. et al. Nocturia and increase in nocturnal blood pressure: the Nagahama study. J. Hypertens. 36, 2185–2192 (2018).
Furukawa, S. et al. Nocturia and prevalence of depressive symptoms in Japanese adult patients with type 2 diabetes mellitus: the Dogo study. Can. J. Diabetes 42, 51–55 (2018).
Juul, K. V., Jessen, N., Bliwise, D. L., van der Meulen, E. & Norgaard, J. P. Delaying time to first nocturnal void may have beneficial effects on reducing blood glucose levels. Endocrine 53, 722–729 (2016).
Kim, J. W. Effect of shift work on nocturia. Urology 87, 153–160 (2016).
Leng, Y., Musiek, E. S., Hu, K., Cappuccio, F. P. & Yaffe, K. Association between circadian rhythms and neurodegenerative diseases. Lancet Neurol. 18, 307–318 (2019).
Videnovic, A., Lazar, A. S., Barker, R. A. & Overeem, S. ‘The clocks that time us’ — circadian rhythms in neurodegenerative disorders. Nat. Rev. Neurol. 10, 683–693 (2014).
Leng, Y. et al. Excessive daytime sleepiness, objective napping and 11-year risk of Parkinson’s disease in older men. Int. J. Epidemiol. 47, 1679–1686 (2018).
Walsh, C. M. et al. Weaker circadian activity rhythms are associated with poorer executive function in older women. Sleep 37, 2009–2016 (2014).
Rogers-Soeder, T. S. et al. Rest-activity rhythms and cognitive decline in older men: the osteoporotic fractures in men sleep study. J. Am. Geriatr. Soc. 66, 2136–2143 (2018).
Bokenberger, K. et al. Association between sleep characteristics and incident dementia accounting for baseline cognitive status: a prospective population-based study. J. Gerontol. A Biol. Sci. Med. Sci. 72, 134–139 (2017).
Cronin, P. et al. Circadian alterations during early stages of Alzheimer’s disease are associated with aberrant cycles of DNA methylation in BMAL1. Alzheimers Dement. 13, 689–700 (2017).
Musiek, E. S. & Holtzman, D. M. Mechanisms linking circadian clocks, sleep, and neurodegeneration. Science 354, 1004–1008 (2016).
Verma, A. K., Singh, S. & Rizvi, S. I. Aging, circadian disruption and neurodegeneration: Interesting interplay. Exp. Gerontol. 172, 112076 (2023).
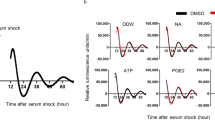
Sengiku, A. et al. Circadian coordination of ATP release in the urothelium via connexin43 hemichannels. Sci. Rep. 8, 1996 (2018).
Negoro, H. et al. Involvement of urinary bladder Connexin43 and the circadian clock in coordination of diurnal micturition rhythm. Nat. Commun. 3, 809 (2012).
Ihara, T. et al. The Clock mutant mouse is a novel experimental model for nocturia and nocturnal polyuria. Neurourol. Urodyn. 36, 1034–1038 (2016).
Noh, J. Y. et al. Circadian rhythms in urinary functions: possible roles of circadian clocks? Int. Neurourol. J. 15, 64–73 (2011).
Goldman, R. Studies in diurnal variation of water and electrolyte excretion; nocturnal diuresis of water and sodium in congestive cardiac failure and cirrhosis of the liver. J. Clin. Invest. 30, 1191–1199 (1951).
Weiss, J. P. & Blaivas, J. G. Nocturia. J. Urol. 163, 5–12 (2000).
Sakakibara, R. et al. Nocturnal polyuria with abnormal circadian rhythm of plasma arginine vasopressin in post-stroke patients. Intern. Med. 44, 281–284 (2005).
Adler, D. et al. Clinical presentation and comorbidities of obstructive sleep apnea-COPD overlap syndrome. PLoS ONE 15, e0235331 (2020).
Asplund, R. & Aberg, H. Diurnal variation in the levels of antidiuretic hormone in the elderly. J. Intern. Med. 229, 131–134 (1991).
Hoshiyama, F. et al. The impact of obstructive sleep apnea syndrome on nocturnal urine production in older men with nocturia. Urology 84, 892–896 (2014).
Forsling, M. L., Montgomery, H., Halpin, D., Windle, R. J. & Treacher, D. F. Daily patterns of secretion of neurohypophysial hormones in man: effect of age. Exp. Physiol. 83, 409–418 (1998).
Potter, G. D. et al. Circadian rhythm and sleep disruption: causes, metabolic consequences, and countermeasures. Endocr. Rev. 37, 584–608 (2016).
Zisapel, N. New perspectives on the role of melatonin in human sleep, circadian rhythms and their regulation. Br. J. Pharmacol. 175, 3190–3199 (2018).
Brzezinski, A., Rai, S., Purohit, A. & Pandi-Perumal, S. R. Melatonin, clock genes, and mammalian reproduction: what is the link? Int. J. Mol. Sci. 22, 13240 (2021).
Bian, J., Wang, Z., Dong, Y., Cao, J. & Chen, Y. Role of BMAL1 and CLOCK in regulating the secretion of melatonin in chick retina under monochromatic green light. Chronobiol. Int. 37, 1677–1692 (2020).
Burke, C. A., Nitti, V. W. & Stothers, L. Melatonin and melatonin receptor agonists in the treatment of nocturia: a systematic review. Neurourol. Urodyn. 43, 826–839 (2024).
Liu, J. et al. MT1 and MT2 melatonin receptors: a therapeutic perspective. Annu. Rev. Pharmacol. Toxicol. 56, 361–383 (2016).
Matsuta, Y. et al. Melatonin increases bladder capacity via GABAergic system and decreases urine volume in rats. J. Urol. 184, 386–391 (2010).
Obayashi, K., Saeki, K. & Kurumatani, N. Association between melatonin secretion and nocturia in elderly individuals: a cross-sectional study of the HEIJO-KYO cohort. J. Urol. 191, 1816–1821 (2014).
Leerasiri, P., Pariyaeksut, P., Hengrasmee, P. & Asumpinwong, C. Effectiveness of melatonin for the treatment of nocturia: a randomized controlled trial. Int. Urogynecol. J. 34, 485–492 (2022).
Batla, A. et al. Exploratory pilot study of exogenous sustained-release melatonin on nocturia in Parkinson’s disease. Eur. J. Neurol. 28, 1884–1892 (2021).
Drake, M. J. et al. Results of a randomized, double blind, placebo controlled, crossover trial of melatonin for treatment of nocturia in adults with multiple sclerosis (MeNiMS). BMC Neurol. 18, 107 (2018).
Leng, G., Brown, C. H. & Russell, J. A. Physiological pathways regulating the activity of magnocellular neurosecretory cells. Prog. Neurobiol. 57, 625–655 (1999).
Nielsen, S. et al. Aquaporins in the kidney: from molecules to medicine. Physiol. Rev. 82, 205–244 (2002).
George, C. P. et al. Diurnal variation of plasma vasopressin in man. J. Clin. Endocrinol. Metab. 41, 332–338 (1975).
Ono, D., Honma, K. I. & Honma, S. Roles of neuropeptides, VIP and AVP, in the mammalian central circadian clock. Front. Neurosci. 15, 650154 (2021).
Ingram, C. D. et al. Vasopressin neurotransmission and the control of circadian rhythms in the suprachiasmatic nucleus. Prog. Brain Res. 119, 351–364 (1998).
Tousson, E. & Meissl, H. Suprachiasmatic nuclei grafts restore the circadian rhythm in the paraventricular nucleus of the hypothalamus. J. Neurosci. 24, 2983–2988 (2004).
Gizowski, C., Trudel, E. & Bourque, C. W. Central and peripheral roles of vasopressin in the circadian defense of body hydration. Best. Pract. Res. Clin. Endocrinol. Metab. 31, 535–546 (2017).
Buijs, R. M. & Kalsbeek, A. Hypothalamic integration of central and peripheral clocks. Nat. Rev. Neurosci. 2, 521–526 (2001).
Nakata, M. et al. Circadian clock component BMAL1 in the paraventricular nucleus regulates glucose metabolism. Nutrients 13, 4487 (2021).
Bing, M. H. et al. Prevalence and bother of nocturia, and causes of sleep interruption in a Danish population of men and women aged 60–80 years. BJU Int. 98, 599–604 (2006).
Obayashi, K., Saeki, K. & Kurumatani, N. Quantitative association between nocturnal voiding frequency and objective sleep quality in the general elderly population: the HEIJO-KYO cohort. Sleep. Med. 16, 577–582 (2015).
Kim, S. J. et al. Influence of circadian disruption associated with artificial light at night on micturition patterns in shift workers. Int. Neurourol. J. 23, 258–264 (2019).
Cosimo DE, N. et al. Night shift workers refer higher urinary symptoms with an impairment quality of life: a single cohort study. Minerva Urol. Nephrol. 73, 831–835 (2021).
Kamperis, K., Hagstroem, S., Radvanska, E., Rittig, S. & Djurhuus, J. C. Excess diuresis and natriuresis during acute sleep deprivation in healthy adults. Am. J. Physiol. Renal Physiol. 299, F404–F411 (2010).
Udo, Y. et al. Sleep duration is an independent factor in nocturia: analysis of bladder diaries. BJU Int. 104, 75–79 (2009).
Kalmbach, D. A., Anderson, J. R. & Drake, C. L. The impact of stress on sleep: pathogenic sleep reactivity as a vulnerability to insomnia and circadian disorders. J. Sleep. Res. 27, e12710 (2018).
Madhu, C. et al. Nocturia: risk factors and associated comorbidities; findings from the EpiLUTS study. Int. J. Clin. Pract. 69, 1508–1516 (2015).
Deger, M. et al. Risk factors associated with nocturia in patients with obstructive sleep apnea syndrome. Int. J. Clin. Pract. 75, e13724 (2021).
Niimi, A. et al. Sleep apnea and circadian extracellular fluid change as independent factors for nocturnal polyuria. J. Urol. 196, 1183–1189 (2016).
Corrado, C. & Fontana, S. Hypoxia and HIF signaling: one axis with divergent effects. Int. J. Mol. Sci. 21, 5611 (2020).
Gabryelska, A. et al. Disruption of circadian rhythm genes in obstructive sleep apnea patients-possible mechanisms involved and clinical implication. Int. J. Mol. Sci. 23, 709 (2022).
Manella, G. et al. Hypoxia induces a time- and tissue-specific response that elicits intertissue circadian clock misalignment. Proc. Natl Acad. Sci. USA 117, 779–786 (2020).
Ghorbel, M. T., Coulson, J. M. & Murphy, D. Cross-talk between hypoxic and circadian pathways: cooperative roles for hypoxia-inducible factor 1α and CLOCK in transcriptional activation of the vasopressin gene. Mol. Cell Neurosci. 22, 396–404 (2003).
Wuerzner, G., Firsov, D. & Bonny, O. Circadian glomerular function: from physiology to molecular and therapeutical aspects. Nephrol. Dial. Transplant. 29, 1475–1480 (2014).
Johnston, J. G. & Pollock, D. M. Circadian regulation of renal function. Free Radic. Biol. Med. 119, 93–107 (2018).
Pollak, M. R., Quaggin, S. E., Hoenig, M. P. & Dworkin, L. D. The glomerulus: the sphere of influence. Clin. J. Am. Soc. Nephrol. 9, 1461–1469 (2014).
Mills, J. N. Human circadian rhythms. Physiol. Rev. 46, 128–171 (1966).
Rossier, B. C., Baker, M. E. & Studer, R. A. Epithelial sodium transport and its control by aldosterone: the story of our internal environment revisited. Physiol. Rev. 95, 297–340 (2015).
Hurwitz, S., Cohen, R. J. & Williams, G. H. Diurnal variation of aldosterone and plasma renin activity: timing relation to melatonin and cortisol and consistency after prolonged bed rest. J. Appl. Physiol. 96, 1406–1414 (2004).
Firsov, D. & Bonny, O. Circadian regulation of renal function. Kidney Int. 78, 640–645 (2010).
Mills, J. N. & Stanbury, S. W. Persistent 24-hour renal excretory rhythm on a 12-hour cycle of activity. J. Physiol. 117, 22–37 (1952).
Mills, J. N. Diurnal rhythm in urine flow. J. Physiol. 113, 528–536 (1951).
Mills, J. N. & Stanbury, S. W. Intrinsic diurnal rhythm in urinary electrolyte output. J. Physiol. 115, 18p–19p (1951).
Ede, M. C., Faulkner, M. H. & Tredre, B. E. An intrinsic rhythm of urinary calcium excretion and the specific effect of bedrest on the excretory pattern. Clin. Sci. 42, 433–445 (1972).
Moore-Ede, M. C. & Herd, J. A. Renal electrolyte circadian rhythms: independence from feeding and activity patterns. Am. J. Physiol. 232, F128–F135 (1977).
Firsov, D. & Bonny, O. Circadian rhythms and the kidney. Nat. Rev. Nephrol. 14, 626–635 (2018).
Stow, L. R. & Gumz, M. L. The circadian clock in the kidney. J. Am. Soc. Nephrol. 22, 598–604 (2011).
Zuber, A. M. et al. Molecular clock is involved in predictive circadian adjustment of renal function. Proc. Natl Acad. Sci. USA 106, 16523–16528 (2009).
Solocinski, K. & Gumz, M. L. The circadian clock in the regulation of renal rhythms. J. Biol. Rhythm. 30, 470–486 (2015).
Doi, M. et al. Salt-sensitive hypertension in circadian clock-deficient Cry-null mice involves dysregulated adrenal Hsd3b6. Nat. Med. 16, 67–74 (2010).
Nikolaeva, S. et al. The circadian clock modulates renal sodium handling. J. Am. Soc. Nephrol. 23, 1019–1026 (2012).
Ge, Y. et al. Endogenously produced 20-HETE modulates myogenic and TGF response in microperfused afferent arterioles. Prostaglandins Other Lipid Mediat. 102–103, 42–48 (2013).
Tokonami, N. et al. Local renal circadian clocks control fluid-electrolyte homeostasis and BP. J. Am. Soc. Nephrol. 25, 1430–1439 (2014).
Ansermet, C. et al. The intrinsic circadian clock in podocytes controls glomerular filtration rate. Sci. Rep. 9, 16089 (2019).
Nikolaeva, S. et al. Nephron-specific deletion of circadian clock gene Bmal1 alters the plasma and renal metabolome and impairs drug disposition. J. Am. Soc. Nephrol. 27, 2997–3004 (2016).
Soundararajan, R., Pearce, D. & Ziera, T. The role of the ENaC-regulatory complex in aldosterone-mediated sodium transport. Mol. Cell Endocrinol. 350, 242–247 (2012).
Gumz, M. L. Molecular basis of circadian rhythmicity in renal physiology and pathophysiology. Exp. Physiol. 101, 1025–1029 (2016).
Gumz, M. L. et al. The circadian clock protein Period 1 regulates expression of the renal epithelial sodium channel in mice. J. Clin. Invest. 119, 2423–2434 (2009).
Richards, J. et al. A role for the circadian clock protein Per1 in the regulation of the NaCl co-transporter (NCC) and the with-no-lysine kinase (WNK) cascade in mouse distal convoluted tubule cells. J. Biol. Chem. 289, 11791–11806 (2014).
Solocinski, K. et al. Transcriptional regulation of NHE3 and SGLT1 by the circadian clock protein Per1 in proximal tubule cells. Am. J. Physiol. Renal Physiol. 309, F933–F942 (2015).
Stow, L. R. et al. The circadian protein period 1 contributes to blood pressure control and coordinately regulates renal sodium transport genes. Hypertension 59, 1151–1156 (2012).
Richards, J. et al. Tissue-specific and time-dependent regulation of the endothelin axis by the circadian clock protein Per1. Life Sci. 118, 255–262 (2014).
Kohan, D. E., Inscho, E. W., Wesson, D. & Pollock, D. M. Physiology of endothelin and the kidney. Compr. Physiol. 1, 883–919 (2011).
Douma, L. G. et al. Kidney-specific KO of the circadian clock protein PER1 alters renal Na+ handling, aldosterone levels, and kidney/adrenal gene expression. Am. J. Physiol. Renal Physiol. 322, F449–F459 (2022).
Miller, M. Nocturnal polyuria in older people: pathophysiology and clinical implications. J. Am. Geriatr. Soc. 48, 1321–1329 (2000).
Schmitt, E. E., Johnson, E. C., Yusifova, M. & Bruns, D. R. The renal molecular clock: broken by aging and restored by exercise. Am. J. Physiol. Renal Physiol. 317, F1087–F1093 (2019).
Cugini, P. et al. Effect of aging on circadian rhythm of atrial natriuretic peptide, plasma renin activity, and plasma aldosterone. J. Gerontol. 47, B214–B219 (1992).
Kirkland, J. L., Lye, M., Levy, D. W. & Banerjee, A. K. Patterns of urine flow and electrolyte excretion in healthy elderly people. Br. Med. J. 287, 1665–1667 (1983).
Wolff, C. A. et al. Defining the age-dependent and tissue-specific circadian transcriptome in male mice. Cell Rep. 42, 111982 (2023).
Moon, D. G. et al. Antidiuretic hormone in elderly male patients with severe nocturia: a circadian study. BJU Int. 94, 571–575 (2004).
Asplund, R. Diuresis pattern, plasma vasopressin and blood pressure in healthy elderly persons with nocturia and nocturnal polyuria. Neth. J. Med. 60, 276–280 (2002).
Tamma, G., Goswami, N., Reichmuth, J., De Santo, N. G. & Valenti, G. Aquaporins, vasopressin, and aging: current perspectives. Endocrinology 156, 777–788 (2015).
Carter, P. G., Cannon, A., McConnell, A. A. & Abrams, P. Role of atrial natriuretic peptide in nocturnal polyuria in elderly males. Eur. Urol. 36, 213–220 (1999).
Matthiesen, T. B., Rittig, S., Norgaard, J. P., Pedersen, E. B. & Djurhuus, J. C. Nocturnal polyuria and natriuresis in male patients with nocturia and lower urinary tract symptoms. J. Urol. 156, 1292–1299 (1996).
Johnson, T. M. II, Miller, M., Pillion, D. J. & Ouslander, J. G. Arginine vasopressin and nocturnal polyuria in older adults with frequent nighttime voiding. J. Urol. 170, 480–484 (2003).
Asplund, R., Sundberg, B. & Bengtsson, P. Oral desmopressin for nocturnal polyuria in elderly subjects: a double-blind, placebo-controlled randomized exploratory study. BJU Int. 83, 591–595 (1999).
Mohandas, R., Douma, L. G., Scindia, Y. & Gumz, M. L. Circadian rhythms and renal pathophysiology. J. Clin. Invest. 132, e148277 (2022).
Graugaard-Jensen, C., Rittig, S. & Djurhuus, J. C. Nocturia and circadian blood pressure profile in healthy elderly male volunteers. J. Urol. 176, 1034–1039 (2006).
Weiss, J. P., Monaghan, T. F., Epstein, M. R. & Lazar, J. M. Future considerations in nocturia and nocturnal polyuria. Urology 133S, 34–42 (2019).
Fujii, T. et al. Circadian rhythm of natriuresis is disturbed in nondipper type of essential hypertension. Am. J. Kidney Dis. 33, 29–35 (1999).
Sachdeva, A. & Weder, A. B. Nocturnal sodium excretion, blood pressure dipping, and sodium sensitivity. Hypertension 48, 527–533 (2006).
Matsuo, T., Miyata, Y. & Sakai, H. Effect of salt intake reduction on nocturia in patients with excessive salt intake. Neurourol. Urodyn. 38, 927–933 (2019).
Okumura, Y. et al. Dietary sodium restriction reduces nocturnal urine volume and nocturnal polyuria index in renal allograft recipients with nocturnal polyuria. Urology 106, 60–64 (2017).
Nakamura, S. et al. Circadian changes in urine volume and frequency in elderly men. J. Urol. 156, 1275–1279 (1996).
Summers, S. J. et al. Male voiding behavior: insight from 19,824 at-home uroflow profiles. J. Urol. 205, 1126–1132 (2021).
Kono, J. et al. Urothelium-specific deletion of connexin43 in the mouse urinary bladder alters distension-induced ATP release and voiding behavior. Int. J. Mol. Sci. 22, 1594 (2021).
Herrera, G. M. & Meredith, A. L. Diurnal variation in urodynamics of rat. PLoS ONE 5, e12298 (2010).
Negoro, H. et al. Development of diurnal micturition pattern in mice after weaning. J. Urol. 189, 740–746 (2013).
Langdale, C. L., Degoski, D., Milliken, P. H. & Grill, W. M. Voiding behavior in awake unrestrained untethered spontaneously hypertensive and Wistar control rats. Am. J. Physiol. Renal Physiol. 321, F195–F206 (2021).
Ihara, T. et al. Intermittent restraint stress induces circadian misalignment in the mouse bladder, leading to nocturia. Sci. Rep. 9, 10069 (2019).
Kimura, Y. et al. The circadian rhythm of bladder clock genes in the spontaneously hypersensitive rat. PLoS ONE 14, e0220381 (2019).
Wu, C. et al. Local receptors as novel regulators for peripheral clock expression. FASEB J. 28, 4610–4616 (2014).
Christie, S. & Zagorodnyuk, V. Time-of-day dependent changes in guinea pig bladder afferent mechano-sensitivity. Sci. Rep. 11, 19283 (2021).
Witjes, W. P., Wijkstra, H., Debruyne, F. M. & de la Rosette, J. J. Quantitative assessment of uroflow: is there a circadian rhythm? Urology 50, 221–228 (1997).
Hiramatsu, I. et al. Maximum flow rate is lowest in the early morning in hospitalized men with nocturia evaluated over 24 hours by toilet uroflowmetry. Urology 166, 196–201 (2022).
Negoro, H. et al. Diurnal differences in urine flow in healthy young men in a light-controlled environment: a randomized crossover design. J. Physiol. Anthropol. 42, 27 (2023).
Huppertz, N. D., Kirschner-Hermanns, R., Tolba, R. H. & Grosse, J. O. Telemetric monitoring of bladder function in female Göttingen minipigs. BJU Int. 116, 823–832 (2015).
White, R. S. et al. Evaluation of mouse urinary bladder smooth muscle for diurnal differences in contractile properties. Front. Pharmacol. 5, 293 (2014).
Negoro, H., Kanematsu, A., Yoshimura, K. & Ogawa, O. Chronobiology of micturition: putative role of the circadian clock. J. Urol. 190, 843–849 (2013).
Ihara, T. et al. The Circadian expression of Piezo1, TRPV4, Connexin26, and VNUT, associated with the expression levels of the clock genes in mouse primary cultured urothelial cells. Neurourol. Urodyn. 37, 942–951 (2018).
Ihara, T. et al. The oscillation of intracellular Ca2+ influx associated with the circadian expression of Piezo1 and TRPV4 in the bladder urothelium. Sci. Rep. 8, 5699 (2018).
Ihara, T. et al. The time-dependent variation of ATP release in mouse primary-cultured urothelial cells is regulated by the clock gene. Neurourol. Urodyn. 37, 2535–2543 (2018).
Ihara, T. et al. Clock genes regulate the circadian expression of Piezo1, TRPV4, Connexin26, and VNUT in an ex vivo mouse bladder mucosa. PLoS ONE 12, e0168234 (2017).
Birder, L. A. & Van Kerrebroeck, P. E. V. Pathophysiological mechanisms of nocturia and nocturnal polyuria: the contribution of cellular function, the urinary bladder urothelium, and circadian rhythm. Urology 133S, 14–23 (2019).
Dalghi, M. G., Montalbetti, N., Carattino, M. D. & Apodaca, G. The urothelium: life in a liquid environment. Physiol. Rev. 100, 1621–1705 (2020).
Ali, A. A. H., Avakian, G. A. & Gall, C. V. the role of purinergic receptors in the circadian system. Int. J. Mol. Sci. 21, 3423 (2020).
Thoma, C. Urinary incontinence: the bladder sets its own clock. Nat. Rev. Urol. 11, 544 (2014).
Stokkan, K. A., Yamazaki, S., Tei, H., Sakaki, Y. & Menaker, M. Entrainment of the circadian clock in the liver by feeding. Science 291, 490–493 (2001).
Ikeda, Y. et al. Glucagon and/or IGF-1 production regulates resetting of the liver circadian clock in response to a protein or amino acid-only diet. EBioMedicine 28, 210–224 (2018).
Chihara, I. et al. Glucocorticoids coordinate the bladder peripheral clock and diurnal micturition pattern in mice. Commun. Biol. 6, 81 (2023).
Noh, J. Y. et al. Presence of multiple peripheral circadian oscillators in the tissues controlling voiding function in mice. Exp. Mol. Med. 46, e81 (2014).
Ihara, T. et al. The Clock mutant mouse is a novel experimental model for nocturia and nocturnal polyuria. Neurourol. Urodyn. 36, 1034–1038 (2017).
Belancio, V. P., Blask, D. E., Deininger, P., Hill, S. M. & Jazwinski, S. M. The aging clock and circadian control of metabolism and genome stability. Front. Genet. 5, 455 (2014).
Silva-Ramos, M. et al. Urinary ATP may be a dynamic biomarker of detrusor overactivity in women with overactive bladder syndrome. PLoS ONE 8, e64696 (2013).
Homma, Y., Yamaguchi, O. & Hayashi, K. An epidemiological survey of overactive bladder symptoms in Japan. BJU Int. 96, 1314–1318 (2005).
Goessaert, A. S., Krott, L., Walle, J. V. & Everaert, K. Exploring nocturia: gender, age, and causes. Neurourol. Urodyn. 34, 561–565 (2015).
Presicce, F. et al. Variations of nighttime and daytime bladder capacity in patients with nocturia: implication for diagnosis and treatment. J. Urol. 201, 962–966 (2019).
Iwamoto, T. et al. Reduced salt intake partially restores the circadian rhythm of bladder clock genes in Dahl salt-sensitive rats. Life Sci. 306, 120842 (2022).
Griffett, K. & Burris, T. P. The mammalian clock and chronopharmacology. Bioorg. Med. Chem. Lett. 23, 1929–1934 (2013).
Ruan, W., Yuan, X. & Eltzschig, H. K. Circadian rhythm as a therapeutic target. Nat. Rev. Drug. Discov. 20, 287–307 (2021).
LeGates, T. A., Fernandez, D. C. & Hattar, S. Light as a central modulator of circadian rhythms, sleep and affect. Nat. Rev. Neurosci. 15, 443–454 (2014).
Gooley, J. J. Treatment of circadian rhythm sleep disorders with light. Ann. Acad. Med. Singap. 37, 669–676 (2008).
Gehlbach, B. K. et al. The effects of timed light exposure in critically Ill patients: a randomized controlled pilot clinical trial. Am. J. Respir. Crit. Care Med. 198, 275–278 (2018).
Ono, H., Taguchi, T., Kido, Y., Fujino, Y. & Doki, Y. The usefulness of bright light therapy for patients after oesophagectomy. Intensive Crit. Care Nurs. 27, 158–166 (2011).
Taguchi, T., Yano, M. & Kido, Y. Influence of bright light therapy on postoperative patients: a pilot study. Intensive Crit. Care Nurs. 23, 289–297 (2007).
Yang, J. et al. Bright light therapy as an adjunctive treatment with risperidone in patients with delirium: a randomized, open, parallel group study. Gen. Hosp. Psychiatry 34, 546–551 (2012).
Challet, E. The circadian regulation of food intake. Nat. Rev. Endocrinol. 15, 393–405 (2019).
Sutton, E. F. et al. Early time-restricted feeding improves insulin sensitivity, blood pressure, and oxidative stress even without weight loss in men with prediabetes. Cell Metab. 27, 1212–1221.e3 (2018).
Chaix, A., Zarrinpar, A., Miu, P. & Panda, S. Time-restricted feeding is a preventative and therapeutic intervention against diverse nutritional challenges. Cell Metab. 20, 991–1005 (2014).
Mrosovsky, N. & Salmon, P. A. A behavioural method for accelerating re-entrainment of rhythms to new light-dark cycles. Nature 330, 372–373 (1987).
Reid, K. J. et al. Aerobic exercise improves self-reported sleep and quality of life in older adults with insomnia. Sleep. Med. 11, 934–940 (2010).
Buxton, O. M., Lee, C. W., L’Hermite-Baleriaux, M., Turek, F. W. & Van Cauter, E. Exercise elicits phase shifts and acute alterations of melatonin that vary with circadian phase. Am. J. Physiol. Regul. Integr. Comp. Physiol. 284, R714–R724 (2003).
Meyer, N., Harvey, A. G., Lockley, S. W. & Dijk, D. J. Circadian rhythms and disorders of the timing of sleep. Lancet 400, 1061–1078 (2022).
Panda, S. The arrival of circadian medicine. Nat. Rev. Endocrinol. 15, 67–69 (2019).
Yu, F. et al. Recent advances in circadian-regulated pharmacokinetics and its implications for chronotherapy. Biochem. Pharmacol. 203, 115185 (2022).
Burgess, H. J., Revell, V. L. & Eastman, C. I. A three pulse phase response curve to three milligrams of melatonin in humans. J. Physiol. 586, 639–647 (2008).
Zhao, M., Zhao, H., Deng, J., Guo, L. & Wu, B. Role of the CLOCK protein in liver detoxification. Br. J. Pharmacol. 176, 4639–4652 (2019).
Winter, C. et al. Chrono-pharmacological targeting of the CCL2-CCR2 axis ameliorates atherosclerosis. Cell Metab. 28, 175–182.e5 (2018).
Levi, F. & Schibler, U. Circadian rhythms: mechanisms and therapeutic implications. Annu. Rev. Pharmacol. Toxicol. 47, 593–628 (2007).
Humphries, P. S. et al. Carbazole-containing amides and ureas: discovery of cryptochrome modulators as antihyperglycemic agents. Bioorg. Med. Chem. Lett. 28, 293–297 (2018).
Miller, S. et al. Isoform-selective regulation of mammalian cryptochromes. Nat. Chem. Biol. 16, 676–685 (2020).
Hirota, T. et al. Identification of small molecule activators of cryptochrome. Science 337, 1094–1097 (2012).
Dong, Z. et al. Targeting glioblastoma stem cells through disruption of the circadian clock. Cancer Discov. 9, 1556–1573 (2019).
Solt, L. A. et al. Regulation of circadian behaviour and metabolism by synthetic REV-ERB agonists. Nature 485, 62–68 (2012).
Banerjee, S. et al. Pharmacological targeting of the mammalian clock regulates sleep architecture and emotional behaviour. Nat. Commun. 5, 5759 (2014).
He, B. et al. The small molecule nobiletin targets the molecular oscillator to enhance circadian rhythms and protect against metabolic syndrome. Cell Metab. 23, 610–621 (2016).
EE, M., AC, B. & MW, H. Citrus flavonoids as regulators of lipoprotein metabolism and atherosclerosis. Annu. Rev. Nutr. 36, 275–299 (2016).
Shinozaki, A. et al. Potent effects of flavonoid nobiletin on amplitude, period, and phase of the circadian clock rhythm in PER2::LUCIFERASE mouse embryonic fibroblasts. PLoS ONE 12, e0170904 (2017).
Ihara, T. et al. Different effects of GsMTx4 on nocturia associated with the circadian clock and Piezo1 expression in mice. Life Sci. 278, 119555 (2021).
Kira, S. et al. Urinary metabolites identified using metabolomic analysis as potential biomarkers of nocturia in elderly men. World J. Urol. 38, 2563–2569 (2020).
Ihara, T. et al. Effects of fatty acid metabolites on nocturia. Sci. Rep. 12, 3050 (2022).
Ihara, T. et al. G protein-coupled receptor 55 activated by palmitoylethanolamide is associated with the development of nocturia associated with circadian rhythm disorders. Life Sci. 332, 122072 (2023).
Ito, H. et al. Effectiveness and safety of a mixture of nobiletin and tangeretin in nocturia patients: a randomized, placebo-controlled, double-blind, crossover study. J. Clin. Med. 12, 2757 (2023).
Pauwaert, K. et al. Does hormonal therapy affect the bladder or the kidney in postmenopausal women with and without nocturnal polyuria: results of a pilot trial? Maturitas 160, 61–67 (2022).
Simonneaux, V. et al. Daily rhythm and regulation of clock gene expression in the rat pineal gland. Brain Res. Brain Res. Mol. Brain Res. 120, 164–172 (2004).
von Gall, C. et al. Clock gene protein mPER1 is rhythmically synthesized and under cAMP control in the mouse pineal organ. J. Neuroendocrinol. 13, 313–316 (2001).
Ono, D., Honma, S. & Honma, K. Differential roles of AVP and VIP signaling in the postnatal changes of neural networks for coherent circadian rhythms in the SCN. Sci. Adv. 2, e1600960 (2016).
Author information
Authors and Affiliations
Contributions
Q.-X.S., S.O.S., H.N., H.-H.J. and R.J. researched data for the article. All authors contributed substantially to discussion of the content. All authors wrote the article. All authors reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Urology thanks Irina Verbakel and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Song, QX., Suadicani, S.O., Negoro, H. et al. Disruption of circadian rhythm as a potential pathogenesis of nocturia. Nat Rev Urol 22, 276–293 (2025). https://doi.org/10.1038/s41585-024-00961-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41585-024-00961-0
This article is cited by
-
Reply to ‘The disruption of circadian rhythm as a potential mechanism of nocturia-like symptoms — a paediatric urology perspective’
Nature Reviews Urology (2025)
-
Association between nocturia and sleep issues, incorporating the impact of lifestyle habits perceived as promoting sleep in an internet survey
Scientific Reports (2025)
-
The disruption of circadian rhythm as a potential mechanism of nocturia-like symptoms — a paediatric urology perspective
Nature Reviews Urology (2025)