Abstract
After the global approval of atezolizumab plus bevacizumab and chemotherapy as first-line metastatic nonsquamous non-small-cell lung cancer (nsqNSCLC) treatment, the IMpower151 (NCT04194203) trial was conducted in China to address regional differences. Chemotherapy-naive patients with metastatic nsqNSCLC (N = 305) were randomized 1:1 to receive either atezolizumab, bevacizumab, carboplatin and paclitaxel or pemetrexed (ABCPem/Pac; n = 152) or placebo plus bevacizumab, carboplatin and pemetrexed or paclitaxel (BCPem/Pac; n = 153). The primary endpoint was investigator-assessed progression-free survival (INV-PFS); secondary endpoints included subgroup analyses of INV-PFS, independent review facility-assessed PFS, overall survival, and investigator-assessed objective response rate and duration of response per RECIST v.1.1. Most patients (97%) received pemetrexed, and 53% had EGFR+ tumors. Median INV-PFS for ABCPem/Pac versus BCPem/Pac was 9.5 versus 7.1 months (stratified hazard ratio: 0.84; 95% confidence interval: 0.65, 1.09; P = 0.184). INV-PFS across subgroups and independent review facility-assessed PFS were consistent with INV-PFS in the intention-to-treat population. Median overall survival was 20.7 versus 18.7 months in the ABCPem/Pac versus BCPem/Pac arms, respectively (stratified hazard ratio: 0.93; 95% confidence interval: 0.67, 1.28). Confirmed objective response rate with ABCPem/Pac versus BCPem/Pac was 48% versus 50%, respectively; median duration of response was 11.3 versus 8.3 months. Adverse events of special interest for atezolizumab were observed in 68% (grades 3 and 4: 11%) and 71% (grades 3 and 4: 7%) of patients receiving ABCPem/Pac and BCPem/Pac, respectively. The most common adverse events of special interest for atezolizumab in the ABCPem/Pac and BCPem/Pac arms were hepatitis (driven by laboratory abnormalities; mostly low grade), hypothyroidism and rash. Overall, IMpower151 did not meet its primary endpoint (INV-PFS) in metastatic nsqNSCLC. ABCPem/Pac was generally well tolerated, with no new safety signals. Trial registration number: ClinicalTrials.gov, NCT02366143
Similar content being viewed by others
Main
Lung cancer remains a leading cause of cancer mortality worldwide, with non-small-cell lung cancer (NSCLC) accounting for approximately 83% of all cases1,2. In China in 2022, an estimated 1,060,600 patients were newly diagnosed with lung cancer and 733,300 patients with lung cancer died3.
The phase 3 IMpower150 study (NCT02366143) met both of its primary endpoints, demonstrating significant progression-free survival (PFS) and overall survival (OS) improvement with atezolizumab versus placebo combined with bevacizumab plus carboplatin and paclitaxel (ABCPac versus BCPac) in patients with metastatic nonsquamous (nsq) NSCLC without epidermal growth factor receptor (EGFR) or anaplastic lymphoma kinase (ALK) genomic alterations4. PFS benefit was also observed in patients with EGFR/ALK genomic alterations (14% of patients), the majority of whom experienced failure on one line of prior tyrosine kinase inhibitor (TKI)4,5. In the intention-to-treat (ITT) population, an improvement in OS favoring ABCPac over BCPac was observed across several baseline characteristics subgroups, with a greater OS benefit seen in male than in female patients5. Results from IMpower150 led to approval of this combination in the United States, the European Union and other regions as a first-line treatment for metastatic nsqNSCLC with or without EGFR/ALK genomic alterations6,7.
Asian and Western patients with lung cancer have different characteristics for epidemiology (for example, risk factors, demographics and genetic susceptibility), clinical presentation, tumor biomarkers (for example, EGFR and Kirsten rat sarcoma virus mutation) and prognosis8. The exact mechanisms behind these differences are not clear8. In China, pemetrexed is used more commonly for the first-line treatment of nsqNSCLC than paclitaxel9.
To address regional differences in patients’ genomic composition and clinical practice, the phase 3 IMpower151 study (NCT04194203) was conducted in China to evaluate the efficacy and safety of atezolizumab plus bevacizumab, carboplatin and pemetrexed or paclitaxel (ABCPem/Pac) versus placebo plus bevacizumab, carboplatin and pemetrexed or paclitaxel (BCPem/Pac) as a first-line treatment of metastatic nsqNSCLC regardless of sensitizing EGFR/ALK genomic alterations (henceforth referred to as EGFR mutations). In this article, we present the efficacy and safety results from the primary analysis of IMpower151, alongside observations from exploratory biomarker analyses.
Results
Patient disposition and baseline characteristics
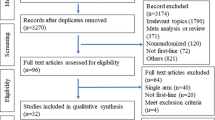
From 9 April 2020 to 18 March 2022, a total of 305 patients (ITT population) out of 626 patients screened were enrolled in IMpower151 at 24 sites distributed across China and randomized to the ABCPem/Pac (n = 152) and BCPem/Pac (n = 153) arms (Fig. 1 and Supplementary Table 1). Baseline characteristics in the ITT population were generally well balanced between both arms (Table 1). The median age was 61 years (range: 30–76). Of the patients, 59% were male, 51% never smoked and 81% had an Eastern Cooperative Oncology Group performance status (ECOG PS) of 1. Programmed death ligand-1 (PD-L1) expression status was tumor cell (TC) ≥ 1% and TC ≥ 50% in 52% and 30% of patients, respectively, and EGFR mutations were detected in 53% of patients. Approximately 97% of patients were selected by their investigator to receive pemetrexed. Of 162 patients, 81 (50%) received ≥2 prior lines of EGFR or ALK TKI treatment. Of 157 patients who received prior EGFR TKI treatment, 66% received a third-generation TKI.
Primary and secondary efficacy outcomes
At clinical cutoff (2 February 2023), the minimum and median follow-up durations were 10.5 and 14.0 months, respectively. A total of 239 PFS events occurred (Fig. 2a). Median investigator-assessed PFS (INV-PFS; primary outcome) was 9.5 months with ABCPem/Pac and 7.1 months with BCPem/Pac (stratified hazard ratio (HR): 0.84; 95% confidence interval (CI): 0.65, 1.09; P = 0.184) (Fig. 2a). Results from the sensitivity analysis were consistent with those from the primary analysis (Supplementary Table 2). Subgroup analyses of INV-PFS are presented in Fig. 2b. No difference in PFS was observed by PD-L1 status in the TC < 1% (unstratified HR: 0.80; 95% CI: 0.56, 1.15), TC ≥ 1% (unstratified HR: 0.86; 95% CI: 0.60, 1.23), TC < 50% (unstratified HR: 0.83; 95% CI: 0.62, 1.12) and TC ≥ 50% (unstratified HR: 0.90, 95% CI: 0.56, 1.46) subgroups. Unstratified HR for PFS comparing ABCPem/Pac with BCPem/Pac was 0.72 (95% CI: 0.52, 1.00) in male patients and 1.07 (95% CI: 0.71, 1.61) in female patients. Median INV-PFS was similar between the ABCPem/Pac and BCPem/Pac arms in the EGFR mutation subgroup (8.5 versus 8.3 months; unstratified HR: 0.86, 95% CI: 0.61, 1.21) and showed numerical differences in the wild-type (WT) subgroup (10.4 versus 7.0 months; unstratified HR: 0.81; 95% CI: 0.55, 1.19) (Extended Data Fig. 1a,b). In patients with tumors carrying EGFR mutations, INV-PFS improvement with ABCPem/Pac versus BCPem/Pac was generally similar across subgroups (Extended Data Fig. 1c). Median independent review facility-assessed PFS (IRF-PFS) was 9.5 months and 8.2 months in the ABCPem/Pac and BCPem/Pac arms, respectively (stratified HR: 0.88; 95% CI: 0.68, 1.15), consistent with INV-PFS (Extended Data Fig. 2).
a, Kaplan–Meier curves in the ITT population. b, Forest plot in key patient subgroups. Data markers in b represent HRs, with error bars indicating 95% CIs. aStratified log-rank. bUnstratified HR is reported. cIncludes patients with ALK WT tumors. dIncludes patients with sensitizing EGFR mutations exon 19 del (n = 96); L858R (n = 57); S768I, L861Q and G719X (n = 7); and ALK rearrangement (n = 5). ePrior lines were counted only when the reason for stopping was disease progression. fOne patient with EGFR mutation received EGFR TKI, but the reason for stopping was not disease progression. gOne patient was wrongly randomized as EGFR WT in the interactive voice- or web-based response system and had received no prior TKI treatment.
OS was relatively immature with 49% events at clinical cutoff due to the short follow-up duration. Median OS was 20.7 months in the ABCPem/Pac arm and 18.7 months in the BCPem/Pac arm (stratified HR: 0.93; 95% CI: 0.67, 1.28) (Fig. 3a). OS was generally balanced between arms across key patient subgroups (Fig. 3b). No difference in OS was observed by level of PD-L1 expression or by sex. The unstratified HR of OS was 0.78 (95% CI: 0.49, 1.22) in the EGFR mutation subgroup and 1.11 (95% CI: 0.70, 1.75) in the WT subgroup (Extended Data Fig. 3a, b). In patients with tumors harboring EGFR mutations, OS improvement with ABCPem/Pac versus BCPem/Pac was generally similar across subgroups (Extended Data Fig. 3c).
a, Kaplan–Meier curves in the ITT population. b, Forest plot of OS in key patient subgroups. Data markers in b represent HRs, with error bars indicating 95% CIs. aUnstratified HR is reported. bIncludes patients with ALK WT tumors. cIncludes patients with sensitizing EGFR mutations exon 19 del (n = 96); L858R (n = 57); S768I, L861Q and G719X (n = 7); and ALK rearrangement (n = 5). dPrior lines were counted only when the reason for stopping was disease progression. eOne patient with EGFR mutation received EGFR TKI, but the reason for stopping was not disease progression. fOne patient was wrongly randomized as EGFR WT in the interactive voice- or web-based response system and had received no prior TKI treatment.
Confirmed objective response rate (ORR) was 48% in the ABCPem/Pac arm (73 of 152 patients) and 50% in the BCPem/Pac arm (76 of 153 patients) (Extended Data Table 1). Confirmed complete response occurred in 0 and 1 (1%) of patients in the ABCPem/Pac and BCPem/Pac arms, respectively. In patients who had a confirmed response, median duration of response (DOR) was 11.3 months with ABCPem/Pac and 8.3 months with BCPem/Pac. ORR was similar in both treatment arms regardless of EGFR mutation status (Extended Data Table 2). DOR was 11.3 months with ABCPem/Pac and 8.0 months with BCPem/Pac in the EGFR mutation subgroup and 11.7 and 9.7 months, respectively, in the WT subgroup.
Follow-up anticancer treatment was administered to 79 of 152 patients (52%) in the ABCPem/Pac arm and 101 of 153 patients (66%) in the BCPem/Pac arm (Extended Data Table 3). In the EGFR mutation subgroup, 63% of patients receiving ABCPem/Pac and 70% of patients receiving BCPem/Pac underwent follow-up anticancer therapy. In the WT subgroup, 39% and 62% of patients receiving ABCPem/Pac and BCPem/Pac, respectively, underwent follow-up anticancer therapy. The most common follow-up anticancer treatment received in the EGFR mutation subgroup was targeted therapy (ABCPem/Pac: 39 of 51 patients; BCPem/Pac: 47 of 57 patients), whereas most patients in the WT subgroup received chemotherapy (ABCPem/Pac: 18 of 28 patients; BCPem/Pac: 31 of 44 patients).
Due to study termination in June 2024, updated OS data (in the ITT population and by EGFR mutation status) at the final data cut (data snapshot: 16 August 2024) were available, with an additional 18 months of follow up (Supplementary Data 1).
Safety
The safety-evaluable population was composed of 152 patients in the ABCPem/Pac arm and 153 patients in the BCPem/Pac arm (Table 2). At clinical cutoff, the median treatment duration was 7.6 months with atezolizumab, 6.3 months with bevacizumab, 2.1 months with carboplatin, 6.3 months with pemetrexed and 2.2 months with paclitaxel in the ABCPem/Pac arm. In patients receiving BCPem/Pac, the median treatment duration was 6.3 months with placebo, 6.1 months with bevacizumab, 2.1 months with carboplatin, 6.2 months with pemetrexed and 2.1 months with paclitaxel.
All-grade adverse events (AEs) occurred in 99% of patients receiving ABCPem/Pac (grades 3 and 4: 66%) and 100% of patients receiving BCPem/Pac (grades 3 and 4: 61%) (Table 2). The most common AEs in the ABCPem/Pac and BCPem/Pac arms were decreased neutrophil count (76% and 75%), anemia (75% and 76%) and decreased white blood cell count (61% and 62%) (Extended Data Table 4). AEs that led to discontinuation of any treatment were observed in 23% and 15% of patients receiving ABCPem/Pac and BCPem/Pac, respectively (Table 2). All-cause grade 5 AEs occurred in 8% of patients in the ABCPem/Pac arm (treatment related: 6%) and 8% of patients in the BCPem/Pac arm (treatment related: 7%).
AEs of special interest (AESIs) for atezolizumab were observed in 68% (grades 3 and 4: 11%) and 71% (grades 3 and 4: 7%) of patients receiving ABCPem/Pac and BCPem/Pac, respectively. The most common AESIs for atezolizumab in the ABCPem/Pac and BCPem/Pac arms, respectively, were hepatitis (diagnosis and laboratory abnormalities: 55% and 59%), hypothyroidism (16% and 11%) and rash (13% and 8%) (Extended Data Table 5). The majority of AESIs under the medical concept of hepatitis (diagnosis and laboratory abnormalities) were hepatitis (laboratory abnormalities: 53% and 58%).
Exploratory biomarker analyses
The biomarker-evaluable population for RNA sequencing included 123 patients in the ABCPem/Pac arm and 127 patients in the BCPem/Pac arm (Extended Data Table 6). Key demographics and baseline characteristics in the biomarker-evaluable population were generally similar across both treatment arms except for a numerically higher percentage of patients with brain metastasis in the BCPem/Pac arm.
RNA sequencing analysis showed that the EGFR mutation subgroup had statistically significant increased expression of genes involved in cell cycling and apoptosis (for example, SMC1B and HSPB6). The WT subgroup had statistically significant increased expression of effector T cell and natural killer (NK)-cell genes (for example, NKG7 and GZMB) (Fig. 4a). Gene set enrichment analysis (GSEA) showed that genes in cell proliferation (for example, E2F targets and G2M checkpoint) and metabolism (for example, oxidative phosphorylation and fatty acid metabolism) were expressed at higher levels in the EGFR mutation subgroup, and genes in immune response (for example, TNF signaling and inflammatory response), tumor suppressor pathway (P53 pathway) and tumor suppressor–promoter dual role pathway (for example, lymphotoxin-alpha signaling) were enriched in the WT subgroup (Fig. 4b). Analysis of signatures that reflect the status of the tumor microenvironment showed a significantly lower level of effector T cells, NK cells, plasma cells and neutrophils, and a higher level of type-2 conventional dendritic cells and DNA damage response signature in the EGFR subgroup, indicating a colder immune status than in the WT subgroup (Fig. 4c).
a, Volcano plot of differentially expressed genes. The log2FC indicates the fold change in the expression level for each gene. Each dot represents one gene. |FC| of 2 and unadjusted P value of 0.01 were used to define genes that are differentially expressed at statistically significant levels. Genes that were significantly up or down regulated were labeled in red. b, Hallmark analysis of differentially expressed genes. The enriched gene sets in the EGFR mutation and WT subgroups were labeled in red and blue, respectively. Asterisks denote the level of statistical significance. c, Gene expression signature analysis. The gene signatures that are expressed at higher levels in the EGFR mutation and WT subgroups were labeled in red and blue, respectively. Asterisks denote the level of statistical significance. All P values reported are two sided. The CAMERA method was used to adjust P values in b and c to account for multiple hypothesis testing. CAF, cancer-associated fibroblast; cDC, conventional dendritic cell; DDR, DNA damage response; EMT, epithelial-to-mesenchymal transition; FC, fold change; MDSC, myeloid-derived suppressor cells; MHC, major histocompatibility complex; Mono_CD14, CD14+ monocytes; Mono_CD16, CD16+ monocytes; NES, normalized enrichment score; Pan_F_TBRS, pan-fibroblast TGF-β response signature; TAM, tumor-associated macrophages; Teff, effector T cell; TH1, T helper 1 cell; TH2, T helper 2 cell; Treg, regulatory T cell.
In the ABCPem/Pac arm, RNA sequencing analysis showed that long PFS (≥median) was associated with statistically significant increased expression of genes involved in immune response (for example, SFTPA1 and HOPX) and in IL2 signaling (for example, CCL4 and CD69). Short PFS (<median) was associated with statistically significant increased expression of genes involved in cell cycle and migration (for example, COL7A and KRT17) and genes correlated with worse cancer prognosis (for example, HASPIN and DEFB1) (Extended Data Fig. 4a). In the BCPem/Pac arm, RNA sequencing analysis showed that long PFS was associated with statistically significant increased expression of genes involved in immune response (for example, SFTPA1 and GLB1L3) and in the inhibition of PI3K signaling (for example, SLC34A2). Short PFS was associated with statistically significant increased expression of genes involved in cell cycle and migration (for example, COL7A1 and KRT17), and genes promoting cancer proliferation and invasion (for example, ANXA8 and L1CAM) (Extended Data Fig. 4b). The association between hallmark pathway expression levels and PFS in each arm is shown in Extended Data Fig. 4c. Pathways that were differentially expressed in the EGFR mutation and WT subgroups and were associated with PFS in both the ABCPem/Pac and BCPem/Pac arms include E2F targets, G2M checkpoint, mitosis, oxidative phosphorylation, allograft rejection, inflammatory response, IL-6–JAK–STAT signaling and interferon-γ response. TNF and IL-2 pathways, which had lower gene expression levels in the EGFR mutation subgroup than in the WT subgroup, were correlated with long PFS in the ABCPem/Pac arm only. These results could explain the numerically shorter median PFS between patients receiving ABCPem/Pac who have EGFR-mutant tumors versus WT tumors (Extended Data Fig. 1).
Tumor microenvironment signature analysis indicated that high gene expression levels of T cells, conventional dendritic cells, major histocompatibility complex II, tumor-associated macrophages and CD16-positive monocytes were correlated with long PFS in the ABCPem/Pac arm (Extended Data Fig. 4d). Of note, macrophages and monocytes are typically considered as immunosuppressive cells. Expression of the abovementioned immune cell types were not associated with PFS in the BCPem/Pac arm.
Post hoc analyses of the impact of the COVID-19 pandemic
At the clinical cutoff date, the coronavirus disease 2019 (COVID-19) pandemic was assessed by the sponsor to have had a minor impact on the primary analysis of IMpower151. The benefit–risk profile of ABCPem/Pac and BCPem/Pac could be conclusively established, as both efficacy and safety data were robust and interpretable.
Discussion
The approval of ABCPac for first-line treatment of metastatic nsqNSCLC with or without EGFR genomic alterations in the United States, the European Union and other regions has advanced the treatment landscape6,7. However, the exact mechanisms behind differences between Asian and Western patients, as well as their impact on treatment response, remains to be elucidated. Here, we report findings from IMpower151, which was designed to address regional differences in patient genomic composition and clinical practice. IMpower151 did not meet its primary endpoint of INV-PFS in the ITT population. Additionally, in the ITT population, OS did not show clinically meaningful improvement with ABCPem/Pac versus BCPem/Pac at the primary analysis; OS results were relatively immature due to the short follow-up duration.
The results of the IMpower151 study are inconsistent with the significant PFS and OS improvements seen with ABCPac in IMpower150 (ref. 4). IMpower151 was conducted in China and all enrolled patients were Asian, whereas IMpower150 took place in 26 countries globally and 14% and 12% of patients in the ABCPac (n = 400) and BCPac (n = 400) arms, respectively, were Asian4. The percentage of patients who never smoked was 51% in IMpower151 and 20% in IMpower150 (ABCPac: 21%; BCPac: 19%)4. The percentage of patients who had tumors with EGFR mutations was 53% in IMpower151 and 14% in IMpower150 (ABCPac: 11%; BCPac: 16%)4. The prevalence of EGFR mutations in both studies is consistent with that reported in screening studies conducted in Asian and Caucasian populations with NSCLC10,11,12. Almost all patients (97%) in IMpower151 received pemetrexed, and this is reflective of the clinical practice in China9. On the other hand, all patients in IMpower150 received paclitaxel per the study protocol4. Previous studies have shown greater PFS benefit with bevacizumab plus platinum-based chemotherapy plus pemetrexed than with bevacizumab plus platinum-based chemotherapy plus paclitaxel13,14. It is, therefore, possible that the chemotherapy backbone has an impact on the efficacy of bevacizumab–chemotherapy combinations, potentially reducing the relative treatment effect observed with ABCPem/Pac versus BCPem/Pac in IMpower151. Additionally, the standard of care for TKI treatment was different during the periods when the studies were conducted. When IMpower150 was ongoing (March 2015 to December 2016), the standard-of-care first-line therapy for patients with EGFR plus NSCLC was first- and second-generation TKIs. By the time IMpower151 was initiated in 2020, the treatment paradigm for EGFR+ metastatic nsqNSCLC had shifted from first- and second-generation to third-generation TKIs (for example, osimertinib15,16). In addition, a higher proportion of patients enrolled in IMpower151 had received ≥2 lines of TKI therapy than in IMpower150. Notably, 66% of patients with tumors carrying EGFR mutations in IMpower151 had received a third-generation TKI. These factors could contribute to the PFS and OS results observed when atezolizumab was added to bevacizumab plus chemotherapy in IMpower151.
The subsequent anticancer therapy may also have affected OS results. Regardless of EGFR mutation status, a higher percentage of patients in the BCPem/Pac arm received follow-up targeted therapy and chemotherapy compared with the ABCPem/Pac arm. In the WT subgroup, a higher percentage of patients in the BCPem/Pac arm than ABCPem/Pac arm received follow-up anticancer therapy across various therapy categories; the largest difference between both arms was seen with subsequent immunotherapy. This discrepancy seen in the WT subgroup could be attributed to the availability of standard-of-care therapies as the next line of treatment after treatment discontinuation. Consequently, the OS benefit with ABCPem/Pac versus BCPem/Pac in the WT subgroup could potentially be reduced, contributing to a diminished OS benefit in the ITT population.
Overall, findings in the EGFR mutation subgroup were consistent with those of other prospective phase 3 studies that investigated the combination of immune checkpoint inhibitors and chemotherapy in a similar patient population (that is, patients with tumors harboring EGFR mutations post TKI failure)17,18. The KEYNOTE-789 study did not meet both its co-primary endpoints of PFS and OS with pembrolizumab plus chemotherapy versus placebo plus chemotherapy18. Similarly, the CheckMate 722 study also did not meet its primary endpoint of PFS with nivolumab plus chemotherapy versus chemotherapy alone17. However, in CheckMate 722, there was a trend favoring nivolumab plus chemotherapy over chemotherapy in patients with tumors carrying EGFR-sensitizing mutations, one line of previous EGFR TKI or both18. These observations were not found in IMpower151, which could be due to the limited size of the subgroups. Nonetheless, IMpower151 is one of a few prospective phase 3 studies investigating the combination of immune checkpoint inhibitors and chemotherapy in patients with tumors carrying EGFR mutations, adding further insight to the management of this population and the development of new clinical trial designs.
Although the IMpower151 study lacks significant positive findings, other studies investigating the combination of immunotherapy with anti-vascular endothelial growth factor (VEGF) plus chemotherapy have shown treatment benefit in Chinese patients with EGFR-mutant metastatic nsqNSCLC whose disease had progressed after EGFR–TKI treatment19,20. In the second interim analysis of the phase 3 ORIENT-31 study, prolonged PFS was demonstrated with the combination of sintilimab (PD-1 inhibitor) and IBI305 (a bevacizumab biosimilar) plus chemotherapy compared with chemotherapy (HR: 0.51; 95% CI: 0.39, 0.67)19. Similar PFS benefit was also seen with sintilimab plus chemotherapy versus chemotherapy alone (HR: 0.72; 95% CI: 0.55, 0.94). No significant OS benefit was seen with the sintilimab–IBI305–chemotherapy combination (HR: 0.98; 95% CI: 0.72, 1.34) nor with sintilimab plus chemotherapy (HR: 0.97; 95% CI: 0.71, 1.32) versus chemotherapy alone. In the first interim analysis of the HARMONi-A study, ivonescimab (anti-PD-1/VEGF bispecific antibody) in combination with chemotherapy significantly prolonged PFS versus placebo plus chemotherapy (HR: 0.46; 95% CI: 0.34, 0.62)20. Most patients (>85%) had received prior third-generation EGFR–TKI treatment. Unlike IMpower151, neither of these studies included anti-VEGF in the control arm. Further investigation is needed to confirm if the benefit attributed by anti-VEGF outweighs that by immunotherapy in this setting.
In IMpower150 and other studies in NSCLC, greater survival benefit with immune checkpoint inhibitors was seen in male than in female patients5,21. However, due to the small sample size of the subgroups by sex in IMpower151, such interpretations of data should be made with caution.
Exploratory biomarker analyses were performed to understand the association of these markers with study treatment response. RNA sequencing analysis of gene signatures in the tumor microenvironment indicated a colder immune status in the EGFR mutation subgroup compared with the WT subgroup. In the ABCPem/Pac arm, but not in the BCPem/Pac arm, elevated gene signatures of T cells, dendritic cells and major histocompatibility complex, as well as myeloid families, were associated with prolonged PFS. The presence of immunosuppressive tumor-associated myeloid cells (TAMCs), such as macrophages and myeloid-derived suppressor cells22,23, has been strongly correlated with CD8+ T cell exhaustion and correlated with poor immuno-oncology treatment efficacy in multiple disease settings24,25,26. In the phase 2 IMmotion150 study of renal cell carcinoma, less PFS benefit with atezolizumab monotherapy was seen in patients with high effector T cell and high myeloid cell gene expression than in patients with high effector T cell and low myeloid cell gene expression27. However, patients with high effector T cell and high myeloid cell gene expression showed better PFS with atezolizumab plus bevacizumab than with atezolizumab alone27. The improved PFS seen with the addition of bevacizumab to atezolizumab in this subgroup may be due to the blockade of VEGF or VEGF receptor, which led to the reduction of myeloid-derived suppressor cells in the tumor microenvironment, as shown in other research on preclinical tumor models and human cancers28,29,30. TAMCs play complex roles in antitumor immunity, with different subsets having opposing effects due to heterogeneity of TAMCs. For example, in our RNA sequencing analysis, CD16+ monocyte signatures correlated with longer PFS, potentially through NK cell recruitment that could be further activated by atezolizumab31. On the other hand, CD14+ monocyte signatures were not correlated with longer PFS as CD14+ monocytes may promote cancer via the mechanisms that atezolizumab and bevacizumab could not inhibit effectively, including remodeling extracellular matrix and differentiating into immune suppressive tumor-associated macrophages32,33. Further investigations into the underlying mechanisms are needed to shed light on new therapeutic strategies and biomarker development. Results from our biomarker analysis also showed that tumor-promoting hallmark gene sets in lung cancer and other cancer types, but not any immune signatures, were associated with shorter PFS in the ABCPem/Pac arm but not in the BCPem/Pac arm. Findings from these exploratory analyses are limited by the small sample size and warrant further investigation in other cohorts of tumor tissues and in blood samples to validate these results and evaluate the potential clinical value of RNA biomarkers. Notably, analytical, bioinformatic and regulatory challenges exist for using RNA sequencing to select or stratify patients in clinical trials. Hence, it is critical to establish benchmark standards, optimize assays for clinical conditions and demonstrate assay reproducibility. Future work may also focus on utilizing RNA sequencing findings to identify biomarkers that can be detected on diagnostic platforms that are more clinically developed, such as polymerase chain reaction, immunohistochemistry or NanoString.
ABCPem/Pac was generally well tolerated, with no new safety signals identified. In IMpower151, all-grade AESIs were predominantly due to the medical concept of hepatitis, which included both hepatitis (diagnosis) and hepatitis (laboratory abnormalities; for example, increased alanine transaminase and increased aspartate transaminase). The majority of these hepatitis AESIs were laboratory abnormalities, which occurred at higher rates than in IMpower150 (ABCP: 12%; BCP: 7%)4. Most of the AESIs in IMpower151 were low grade, and the ≥grade 3 AESI rates were comparable to those in IMpower150 (ref. 4).
Limitations of this study include the small sample size, lack of statistical power to detect the desired effect size in subgroups by baseline characteristics (including EGFR mutation and sex) and the small sample sizes in the exploratory biomarker subgroup analyses. A small number of patients (n = 11) had TKI treatments between sampling and randomization, which could have altered their tumor PD-L1 level, EGFR mutation status and RNA sequencing expressions. Another limitation is that the study was conducted during COVID-19, resulting in COVID-19 related AEs, protocol deviations and missing tumor assessments. However, sensitivity analysis to account for missing data showed similar PFS results as the primary analysis, indicating minimal impact of the pandemic on the primary endpoint. In addition, self-selection bias or other biases in the recruitment process was minimized by ensuring that the study sites reflected a good geographical representation of the diverse patient population in China and by using a central interactive voice- and web-response system for patient identification and treatment assignment.
Despite not meeting its primary endpoint, IMpower151 provided insights on the efficacy and safety of ABCPem/Pac versus BCPem/Pac in patients with nsqNSCLC in China, where baseline demographics and clinical practices are different from those in global studies. This study highlights the need for more efforts to elucidate the mechanisms behind the differences in epidemiologic characteristics between Asian and Western patients with lung cancer.
Methods
Study design and patient population
IMpower151 (ClinicalTrials.gov, NCT04194203) was conducted according to the International Conference on Harmonisation E6 guideline for Good Clinical Practice and the principles of the Declaration of Helsinki. Approval of the protocols was obtained from independent review boards or ethics committees at each study site, and from regulatory authorities per local requirements (Supplementary Table 1). All patients provided written informed consent. All relevant requirements by China’s Ministry of Science and Technology related to the export of genetic information and materials for this work have been fulfilled.
IMpower151 is a phase 3, randomized, multicenter, double-blind study investigating bevacizumab, carboplatin and investigator’s choice of either pemetrexed or paclitaxel in combination with atezolizumab (ABCPem/Pac) or placebo (BCPem/Pac) in the first-line treatment of metastatic nsqNSCLC. Patients aged ≥18 years with stage IV nsqNSCLC who had not received prior treatment or systemic therapy in the metastatic nsq setting (adjuvant or neoadjuvant chemotherapy, radiotherapy or chemoradiotherapy was permitted if the duration between the last treatment administration and the date of randomization was ≥6 months) and who had measurable disease per Response Evaluation Criteria in Solid Tumors (RECIST) v.1.1 and ECOG PS of 0 or 1 were enrolled by investigators at clinical sites in China (Supplementary Table 1). Patients needed to have a representative tumor sample that could be evaluated for prospective central testing of PD-L1 TC expression (SP263 PD-L1 immunohistochemical assay; Ventana Medical Systems) and the presence of EGFR mutations and ALK gene rearrangements. Recruitment of patients to the WT subgroup was limited to 50% of the sample size to reflect the natural prevalence in the Chinese population with advanced nsqNSCLC10,11. Patients with sensitizing EGFR mutations or ALK gene rearrangements must have experienced disease progression (during or after treatment) or were intolerant to treatment with one or more TKIs that were appropriate for the treatment of EGFR-mutant NSCLC. Patients were excluded if life expectancy was less than 3 months or if there was evidence of bleeding diathesis or coagulopathy, tumor invasion or abutting of major blood vessels. The study design only considered the sex of the patients, which was self-reported. The full protocol can be accessed in the Supplementary Information.
Procedures and interventions
For eligible patients, the study site obtained the patient’s identification number and treatment assignment from a central interactive voice- and web-response system to minimize self-selection bias. Enrolled patients were randomized 1:1 to the ABCPem/Pac or BCPem/Pac arms using a stratified block method (block size of four). Patients received 21-day cycles of atezolizumab or placebo (1,200 mg) plus bevacizumab (15 mg per kg), carboplatin (area under the concentration curve 6 mg per ml per min) and paclitaxel (175 mg per m2) or pemetrexed (500 mg per m2) intravenously for four cycles, followed by atezolizumab or placebo maintenance treatment until unacceptable toxicity or loss of clinical benefit, and bevacizumab and pemetrexed (if given during induction) until progression per RECIST v.1.1. The use of paclitaxel or pemetrexed was determined by the investigator and documented before randomization and was not permitted to be changed during the study. Randomization was stratified by genotype of EGFR or ALK gene (genomic alterations versus WT) and PD-L1 expression (TC < 50% versus TC ≥ 50% by the SP263 immunohistochemistry assay).
Study site personnel and patients were blinded to treatment assignment during the study. The sponsor and its agents were also blinded to treatment assignment, except for individuals who required access to fulfill their job roles during a clinical trial. Unblinding was permitted for medical emergencies and for select non-medical emergencies, such as at the time of unequivocal disease progression by RECIST v.1.1 and study treatment discontinuation to help guide decisions on subsequent treatment, provided conditions in the protocol were met.
Study endpoints and assessments
The primary endpoint was INV-PFS (defined as the time from randomization to the first occurrence of disease progression or death from any cause, whichever occured first) per RECIST v.1.1 in the ITT population. Secondary endpoints included INV-PFS by EGFR mutation and PD-L1 status, IRF-PFS in the ITT population, OS (defined as the time from randomization to death from any cause) in the ITT population, ORR (defined as the proportion of patients with a complete or partial response on two consecutive occasions ≥4 weeks apart as determined by the investigator per RECIST v.1.1) and DOR (defined as the time from the first occurrence of a documented objective response to disease progression or death from any cause, whichever occured first, as determined by the investigator per RECIST v.1.1). ORR was analyzed in all randomized patients with measurable disease at baseline. DOR was assessed in patients with a complete or partial response on two consecutive occasions ≥4 weeks apart as determined by the investigator per RECIST v.1.1.
Exploratory objectives included INV-PFS rate at 6 months and 1 year, and OS rate at 1 and 2 years. Patients underwent tumor assessments during screening, every 6 weeks from day 1 of cycle 1 for the first 12 months, and every 9 weeks thereafter until the occurrence of disease progression per RECIST v.1.1 (loss of clinical benefit among patients who continued to receive treatment after disease progression), withdrawal of consent, death or study termination by the sponsor, whichever occured first.
Exploratory biomarker objectives included OS by EGFR mutation and PD-L1 status, ORR and DOR by EGFR mutation status, and RNA sequencing analyses of hallmark pathways and gene signatures by EGFR mutation status and PFS (≥median or <median). The biomarker-evaluable population included patients with available tumor tissue samples and evaluable data for PD-L1 status, EGFR mutation status and RNA sequencing analyses. For RNA sequencing analyses, RNA sequencing data had to meet criteria on depth and correlation on the principal component analysis plot.
Safety objectives were to evaluate the incidence, nature and severity of AEs or AESIs suggesting an autoimmune cause, graded according to the National Cancer Institute Common Terminology Criteria for Adverse Events (v.5.0). The safety-evaluable population was defined as all randomized patients who received any amount of any component of study treatment.
Statistical analyses
IMpower151 was planned to randomize approximately 306 patients, assuming a 1:1 randomization ratio, one-sided significance level of 0.025, a dropout (no further data on disease progression status and survival can be collected during the study period) rate of 5% per 12 months for PFS, 90% power to detect an HR of 0.65 (corresponding to an improvement in median PFS from 6.8 to 10.5 months in the ITT population) and exponentially distributed event times. The final PFS analysis was to be conducted when approximately 227 PFS events in the ITT population had occurred or ≥10 months after the last patient was enrolled, whichever occurs last. This event number would allow for a minimum detectable difference corresponding to an HR of approximately 0.77 in the ITT population. The recruitment period was anticipated to be approximately 20 months, and the final PFS analysis was expected to occur approximately 30 months after the first patient was randomized.
Kaplan–Meier methodology was used to estimate median PFS and OS for each treatment arm. HRs were estimated using a stratified Cox regression model, using the same stratification factors that were used during randomization. The Brookmeyer–Crowley methodology was used to calculate the 95% CIs34. All subgroup analyses presented were unstratified due to the small sample size and their exploratory nature.
The estimate of ORR and its 95% CI was calculated using the Clopper–Pearson method. ORR was compared between the two treatment arms using the stratified Mantel–Haenszel test and 95% CIs were determined using the normal approximation to the binomial distribution. Formal hypothesis testing will not be performed for DOR, and comparisons between treatment arms will be made for descriptive purposes.
No data were excluded from analyses. For missing PFS data, patients without a date of disease progression were analyzed as censored observations on the date of the last tumor assessment. Missing OS data from patients who were not reported as having died were censored on the date they were last known to be alive. If no post-baseline tumor assessment was available, PFS and OS were censored at the date of randomization.
For missing ORR data, patients without any post-baseline assessment were considered nonresponders. Missing DOR data for patients who had not progressed and who had not died at the time of analysis were censored at the time of the last tumor assessment. If no tumor assessments were performed after the date of the first occurrence of a complete or partial response, DOR was censored at the date of the first occurrence of a complete or partial response.
Baseline characteristics of the ITT and biomarker-evaluable populations, safety data and information on follow-up anticancer treatment were summarized. Sensitivity analysis was conducted based on interval censoring to evaluate the impact of missed or delayed tumor assessments on INV-PFS (Supplementary Methods 1). Data from case report forms were collected using Medidata Classic Rave (v.2022.3.2) and non-case report form data (including IxRS and laboratory data) were obtained using the Edison Platform (pRED Informatics, F. Hoffmann-La Roche Ltd). Statistical analyses were conducted using SAS (v.9.4). The full statistical analysis plan can be accessed in the Supplementary Information.
RNA sequencing
Total RNA was extracted from formalin-fixed paraffin-embedded (FFPE) samples using the AllPure FFPE DNA/RNA Kit (Magen Biotechnology Co., Ltd) and quantified using the Qubit RNA High Sensitivity Assay (Thermo Fisher Scientific Inc.). RNA quality was assessed using the Qsep100 Bio-Fragment Analyzer (BiOptic Inc.) and RNA cartridge. RNA sequencing was performed using the TruSeq RNA Access Library Prep Kit (Illumina, Inc. (cat. no. RS-301-2001 and RS-301-2002); PCR primer cocktail was included in the kit). RNA sequencing reads were first aligned to ribosomal RNA sequences to remove ribosomal reads. The remaining reads were then aligned to the human reference genome (NCBI Build 38) using GSNAP v.2013-11-01. The number of reads mapped to the exons of each gene was calculated using the R/Bioconductor package GenomicAlignments to quantify gene expression levels. Raw counts for genes were normalized by trimmed mean of M-values based on size factors as calculated using CalcNormFactors in the edgeR package. Trimmed mean of M-values-normalized counts were subsequently voom transformed using the voom function in the R package limma, resulting in normalized log2 (counts per million (CPM)-mapped reads) data. Genes with low expressions were filtered out if the summarized gene expressions were less than 0.5 CPM in the smallest comparison subgroup. All RNA sequencing measurements were taken from distinct sets of FFPE tumor tissue slides and were only measured once due to the limitation of number of slides. Only one set of FFPE tumor tissue slides was collected from each patient who provided these samples.
Differential gene expression was performed using the R package limma, comparing patients with tumors carrying EGFR mutations and patients with WT tumors, or between patients with long and short PFS. Volcano plots for these analyses were plotted using the EnhancedVolcano R package. Significant differential gene expression was defined as an absolute log2 fold-change of ≥1 and unadjusted P ≤ 0.05. Gene signature scores were calculated for each sample as the arithmetic mean of log2 (CPM) expression of all genes in a given signature, which included the Hallmark gene set collection from the MSigDB database and the other signatures from internal and public literatures. GSEA was performed using the fgsea package v.1.14.0. and the signatures using a differential expression linear model as the input. The CAMERA method was used to adjust P values to account for multiple hypothesis testing. All RNA sequencing analyses were conducted in R (v.4.0.3).
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
For eligible studies, qualified researchers can request access to individual-patient-level clinical data through a data request platform. At the time of writing, this request platform is Vivli (https://vivli.org/ourmember/roche/). For up-to-date details on Roche’s Global Policy on the Sharing of Clinical Information and how to request access to related clinical study documents, see https://go.roche.com/data_sharing. Individual-patient-level RNA sequencing data are made available to qualified researchers at the European Genome-phenome Archive platform. Anonymized records for individual patients across more than one data source external to Roche cannot, and should not, be linked due to a potential increase in risk of patient re-identification. Datasets from clinical trials including RNA sequencing can be requested after August 2026 per Roche’s Policy (18 months after completion of clinical study report). The data sharing shall also comply with applicable local regulations. Gene signatures were included from the Hallmark gene set collection from the MSigDB database and from internal and public literatures. Source data are provided with this paper.
References
Sung, H. et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249 (2021).
Ganti, A. K., Klein, A. B., Cotarla, I., Seal, B. & Chou, E. Update of incidence, prevalence, survival, and initial treatment in patients with non-small cell lung cancer in the US. JAMA Oncol. 7, 1824–1832 (2021).
Han, B. et al. Cancer incidence and mortality in China, 2022. J. Natl Cancer Cent. 4, 47–53 (2024).
Socinski, M. A. et al. Atezolizumab for first-line treatment of metastatic nonsquamous NSCLC. N. Engl. J. Med. 378, 2288–2301 (2018).
Reck, M. et al. Atezolizumab plus bevacizumab and chemotherapy in non-small-cell lung cancer (IMpower150): key subgroup analyses of patients with EGFR mutations or baseline liver metastases in a randomised, open-label phase 3 trial. Lancet Respir. Med. 7, 387–401 (2019).
Tecentriq (atezolizumab), package insert (Genentech, 2024); https://www.gene.com/download/pdf/tecentriq_prescribing.pdf
Tecentriq (atezolizumab), summary of product characteristics (Roche, 2024); https://www.ema.europa.eu/en/documents/product-information/tecentriq-epar-product-information_en.pdf
Zhou, W. & Christiani, D. C. East meets West: ethnic differences in epidemiology and clinical behaviors of lung cancer between East Asians and Caucasians. Chin. J. Cancer 30, 287–292 (2011).
Durbin, L. et al. Treatment patterns in non-small-cell lung cancer in China: results from the CancerMPact survey 2020. Cancer Treat. Res Commun. 29, 100462 (2021).
Sun, M. et al. Analysis of real-word mutations of lung cancer driver genes in five regions of China. Transl. Cancer Res. 8, 2581–2592 (2019).
Shi, Y. et al. A prospective, molecular epidemiology study of EGFR mutations in Asian patients with advanced non-small-cell lung cancer of adenocarcinoma histology (PIONEER). J. Thorac. Oncol. 9, 154–162 (2014).
Rosell, R. et al. Screening for epidermal growth factor receptor mutations in lung cancer. N. Engl. J. Med. 361, 958–967 (2009).
Patel, J. D. et al. PointBreak: a randomized phase III study of pemetrexed plus carboplatin and bevacizumab followed by maintenance pemetrexed and bevacizumab versus paclitaxel plus carboplatin and bevacizumab followed by maintenance bevacizumab in patients with stage IIIB or IV nonsquamous non-small-cell lung cancer. J. Clin. Oncol. 31, 4349–4357 (2013).
Udagawa, H. et al. Bevacizumab plus platinum-based chemotherapy in advanced non-squamous non-small-cell lung cancer: a randomized, open-label phase 2 study (CLEAR). Transl. Lung Cancer Res. 10, 3059–3070 (2021).
Tagrisso (osimertinib), package insert (AstraZeneca, 2024); https://www.azpicentral.com/tagrisso/tagrisso.pdf#page=1
Tagrisso (osimertinib), summary of product characteristics (AstraZeneca, 2024); https://www.ema.europa.eu/en/documents/product-information/tagrisso-epar-product-information_en.pdf
Mok, T. et al. Nivolumab plus chemotherapy in epidermal growth factor receptor-mutated metastatic non-small-cell lung cancer after disease progression on epidermal growth factor receptor tyrosine kinase inhibitors: final results of CheckMate 722. J. Clin. Oncol. 42, 1252–1264 (2024).
Yang, J. C.-H. et al. Phase III KEYNOTE-789 study of pemetrexed and platinum with or withoutpembrolizumab for tyrosine kinase inhibitor‒resistant, EGFR–mutant, metastatic nonsquamous non–small cell lung cancer. J. Clin. Oncol. 42, 4029–4039 (2024).
Lu, S. et al. Sintilimab plus chemotherapy for patients with EGFR-mutated non-squamous non-small-cell lung cancer with disease progression after EGFR tyrosine–kinase inhibitor therapy (ORIENT-31): second interim analysis from a double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Respir. Med. 11, 624–636 (2023).
Fang, W. et al. Ivonescimab plus chemotherapy in non-small cell lung cancer with EGFR variant: a randomized clinical trial. JAMA 332, 561–570 (2024).
Wang, C. et al. Effect of sex on the efficacy of patients receiving immune checkpoint inhibitors in advanced non-small cell lung cancer. Cancer Med. 8, 4023–4031 (2019).
O’Donnell, J. S. et al. Cancer immunoediting and resistance to T cell-based immunotherapy. Nat. Rev. Clin. Oncol. 16, 151–167 (2019).
Beatty, G. L. et al. Exclusion of T cells from pancreatic carcinomas in mice is regulated by Ly6C(low) F4/80(+) extratumoral macrophages. Gastroenterology 149, 201–210 (2015).
Timperi, E. et al. Lipid-associated macrophages are induced by cancer-associated fibroblasts and mediate immune suppression in breast cancer. Cancer Res. 82, 3291–3306 (2022).
Weide, B. et al. Myeloid-derived suppressor cells predict survival of patients with advanced melanoma: comparison with regulatory T cells and NY-ESO-1- or melan-A-specific T cells. Clin. Cancer Res. 20, 1601–1609 (2014).
Möller, M. et al. Myeloid-derived suppressor cells in peripheral blood as predictive biomarkers in patients with solid tumors undergoing immune checkpoint therapy: systematic review and meta-analysis. Front Immunol. 15, 1403771 (2024).
McDermott, D. F. et al. Clinical activity and molecular correlates of response to atezolizumab alone or in combination with bevacizumab versus sunitinib in renal cell carcinoma. Nat. Med. 24, 749–757 (2018).
Kusmartsev, S. et al. Oxidative stress regulates expression of VEGFR1 in myeloid cells: link to tumor-induced immune suppression in renal cell carcinoma. J. Immunol. 181, 346–353 (2008).
Osada, T. et al. The effect of anti-VEGF therapy on immature myeloid cell and dendritic cells in cancer patients. Cancer Immunol. Immunother. 57, 1115–1124 (2008).
Draghiciu, O., Nijman, H. W., Hoogeboom, B. N., Meijerhof, T. & Daemen, T. Sunitinib depletes myeloid-derived suppressor cells and synergizes with a cancer vaccine to enhance antigen-specific immune responses and tumor eradication. Oncoimmunology 4, e989764 (2015).
Bruix, J. et al. Adjuvant sorafenib for hepatocellular carcinoma after resection or ablation (STORM): a phase 3, randomised, double-blind, placebo-controlled trial. Lancet Oncol. 16, 1344–1354 (2015).
Porrello, A. et al. Factor XIIIA-expressing inflammatory monocytes promote lung squamous cancer through fibrin cross-linking. Nat. Commun. 9, 1988 (2018).
Schmall, A. et al. Macrophage and cancer cell cross-talk via CCR2 and CX3CR1 is a fundamental mechanism driving lung cancer. Am. J. Respir. Crit. Care Med. 191, 437–447 (2015).
Brookmeyer, R. & Crowley, J. A confidence interval for the median survival time. Biometrics 38, 29–41 (1982).
Acknowledgements
We thank the patients who participated in the trial, the patients’ families and the investigators and staff at all clinical study sites. The IMpower151 study was sponsored by F. Hoffmann-La Roche, Ltd. The funder had a role in study design, data collection, data analysis, data interpretation and writing of the report. Medical writing assistance for this manuscript was provided by B. Lim, of Nucleus Global, an Inizio Company, and funded by F. Hoffmann-La Roche, Ltd.
Author information
Authors and Affiliations
Contributions
Conceptualization: C.Z., C.S., M.B. and M.K.S. Methodology: C.Z., I.Y., X.H. and C.S. Software: X.H. Formal analysis: C.Z., I.Y., X.H. and M.K. Investigation: C.Z., X.D., Zhehai Wang, X.W., Y.Y., Y.C., H.P., X.Z., J. Cui, L.W., X.L., Ziping Wang, Q. Wang, J.H., M.W., C.S. and M.B. Resources: C.Z., X.D., Zhehai Wang., X.W., Y.Y., Y.C., H.P., X.Z., L.W., X.L., Ziping Wang., J.H., M.W. and M.B. Data curation: X.H. and C.S. Writing—original draft: I.Y. and C.S. Writing—review and editing: all authors. Visualization: X.H. and C.Z. Supervision: C.Z. and M.B. Project administration: C.Z., X.D., Y.Y., H.P., X.Z., L.W., Ziping Wang, J.H. and M.W.
Corresponding author
Ethics declarations
Competing interests
C.Z. received honoraria as a speaker/consultant from Alice, Amoy Diagnostics, AnHeart, Boehringer Ingelheim, C-Stone, Eli Lilly China, Hengrui, Innovent Biologics, LUYE Pharma, Merck Sharp & Dohme, Qilu, Roche, Sanofi and TopAlliance Biosciences Inc. along with advisor fees from Hengrui, Innovent Biologics, Qilu and TopAlliance Biosciences Inc. C.Z. declares non-financial competing interests as the IASLC President-Elect. I.Y., M.X., X.H., J. Cai and Q.Wu are employees of Roche (China) Holding Ltd and own stocks from Roche. L.Q. and C.S. are employees of Roche (China) Holding Ltd. M.B., M.K., M.K.S. are employees of Genentech and own stocks from Roche. The other authors declare no competing interests.
Peer review
Peer review information
Nature Medicine thanks Gregory A. Masters, Giorgio Scagliotti, Ming Wang and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editor: Liam Messin, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Investigator-assessed PFS by EGFR mutation status.
Kaplan-Meier curves in patients with (a) EGFR mutation and (b) EGFR WT. EGFR mutation status was based on the presence of EGFR genomic alterations or ALK rearrangements. Sensitizing EGFR mutations include exon 19 del, L858R, S768I, L861Q, and G719X. (c) Investigator-assessed PFS in key patient subgroups of the EGFR mutation group. Data markers in (c) represent HRs, with error bars indicating 95% CIs. a Unstratified HR is reported. b Includes patients with sensitizing EGFR mutations S768I, L861Q and G719X (n = 7). c Two patients in the ABCPem/Pac arm had both sensitizing EGFR mutations exon19 del and L858R. d One patient was wrongly randomized as EGFR WT in the interactive voice- or web-based response system and had received no prior TKI treatment. e Prior lines were counted only when the reason for stopping was disease progression. f One patient with EGFR mutation received EGFR TKI but the reason for stopping was not disease progression. 1G, first generation; 2G, second generation; 3G, third generation; ABCPem/Pac, atezolizumab plus bevacizumab, carboplatin, and pemetrexed or paclitaxel; ALK, anaplastic large-cell lymphoma kinase; BCPem/Pac, placebo plus bevacizumab, carboplatin, and pemetrexed or paclitaxel; CI, confidence interval; EGFR, epidermal growth factor receptor; HR, hazard ratio; TKI, tyrosine kinase inhibitor; WT, wild type.
Extended Data Fig. 2 IRF-assessed PFS.
Kaplan-Meier curves in the intention-to-treat population. ABCPem/Pac, atezolizumab plus bevacizumab, carboplatin, and pemetrexed or paclitaxel; BCPem/Pac, placebo plus bevacizumab, carboplatin, and pemetrexed or paclitaxel; CI, confidence interval; HR, hazard ratio; IRF, independent review facility.
Extended Data Fig. 3 OS by EGFR mutation status.
Kaplan-Meier curves in patients with (a) EGFR mutation and (b) EGFR WT. EGFR mutation status was based on the presence of EGFR genomic alterations or ALK rearrangements. Sensitizing EGFR mutations include exon 19 del, L858R, S768I, L861Q, and G719X. (c) OS in key patient subgroups of the EGFR mutation group. Data markers in (c) represent HRs, with error bars indicating 95% CIs. a Unstratified HR is reported. b Includes patients with sensitizing EGFR mutations S768I, L861Q and G719X (n = 7). c Two patients in the ABCPem/Pac arm had both sensitizing EGFR mutations exon19 del and L858R. d One patient was wrongly randomized as EGFR WT in the interactive voice- or web-based response system and had received no prior TKI treatment. e Prior lines were counted only when the reason for stopping was disease progression. f One patient with EGFR mutation received EGFR TKI but the reason for stopping was not disease progression. 1G, first generation; 2G, second generation; 3G, third generation; ABCPem/Pac, atezolizumab plus bevacizumab, carboplatin, and pemetrexed or paclitaxel; ALK, anaplastic large-cell lymphoma kinase; BCPem/Pac, placebo plus bevacizumab, carboplatin, and pemetrexed or paclitaxel; CI, confidence interval; EGFR, epidermal growth factor receptor; HR, hazard ratio; NE, not estimable; TKI, tyrosine kinase inhibitor; WT, wild type.
Extended Data Fig. 4 RNA sequencing comparison of patients with long PFS (≥ median) vs short PFS (< median) in the ITT population.
(a) Volcano plot of differentially expressed genes in the ABCPem/Pac arm. The log2 FC indicates the fold change in the expression level for each gene. Each dot represents one gene. |FC| of 2 and unadjusted P value of 0.01 were used to define genes that are differentially expressed at statistically significant levels. Genes that were significantly up or down regulated were labeled in red. (b) Volcano plot of differentially expressed genes in the BCPem/Pac arm. The log2 FC indicates the fold-change in the expression level for each gene. Each dot represents one gene. |FC| of 2 and unadjusted P value of 0.01 were used to define genes that are differentially expressed at statistically significant levels. Genes that were significantly up or down regulated were labeled in red. (c) Hallmark analysis of differential gene expression in the ABCPem/Pac and BCPem/Pac arms. The enriched gene sets in the long and short PFS subgroups were labeled in red and blue, respectively, for both the ABCPem/Pac and BCPem/Pac arms. Asterisks denote the level of statistical significance. (d) Gene expression signature analysis in the ABCPem/Pac and BCPem/Pac arms. The gene signatures that are expressed at higher levels in the long and short PFS subgroups were labeled in red and blue, respectively, for both the ABCPem/Pac and BCPem/Pac arms. Asterisks denote the level of statistical significance. All P values reported are 2 sided. The CAMERA method was used to adjust P values in (c) and (d) to account for multiple hypothesis testing. ABCPem/Pac, atezolizumab plus bevacizumab, carboplatin, and pemetrexed or paclitaxel; BCPem/Pac, placebo plus bevacizumab, carboplatin, and pemetrexed or paclitaxel; CAF, cancer-associated fibroblast; cDC, conventional dendritic cell; DDR, DNA damage response; EGFR, epidermal growth factor receptor; EMT, epithelial-to-mesenchymal transition; FC, fold change; ITT, intention to treat; MDSC, myeloid-derived suppressor cells; MHC, major histocompatibility complex; Mono_CD14, CD14+ monocytes; Mono_CD16, CD16+ monocytes; NES, normalized enrichment score; Pan_F_TBRS, pan-fibroblast TGF-β response signature; PFS, progression-free survival; TAM, tumor-associated macrophages; Teff, effector T cell; TH1, T helper 1 cell; TH2, T helper 2 cell; Treg, regulatory T cell; WT, wild type.
Supplementary information
Supplementary Information
Supplementary Tables 1–2, Data 1, Methods 1, Protocol and Statistical Analysis Plan.
Source data
Source Data Fig. 4
Exact P values for Fig. 4b,c.
Source Data Extended Data Fig. 4
Exact P values for Extended Data Fig. 4c,d.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhou, C., Dong, X., Chen, G. et al. Atezolizumab plus bevacizumab and chemotherapy in metastatic nonsquamous NSCLC: the randomized double-blind phase 3 IMpower151 trial. Nat Med (2025). https://doi.org/10.1038/s41591-025-03658-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41591-025-03658-y