Abstract
Prevention of subsequent fracture is a major public health challenge in the field of osteoporosis prevention and treatment, and older women are at high risk for osteoporotic fractures. This study aimed to examine factors associated with subsequent fracture in older Chinese women with osteoporosis. We collected data on 9212 older female patients with osteoporotic fractures from 580 medical institutions in 31 provinces of China. Higher odds of subsequent fractures were associated with age of 70–79 years (OR 1.218, 95% CI 1.049–1.414), age ≥ 80 (OR 1.455, 95% CI 1.222–1.732), index fracture site was vertebrae (OR 1.472, 95% CI 1.194–1.815) and hip (OR 1.286, 95% CI 1.041–1.590), index fracture caused by fall (OR 1.822, 95% CI 1.281–2.591), strain (OR 1.587, 95% CI 1.178–2.139), no inducement (OR 1.541, 95% CI 1.043–2.277), and assessed as high risk of fracture (OR 1.865, 95% CI 1.439–2.416), BMD T-score ≤ −2.5 (OR 1.725, 95% CI 1.440–2.067), history of surgery (OR 3.941, 95% CI 3.475–4.471) and trauma (OR 8.075, 95% CI 6.941–9.395). Low risk of fall (OR 0.681, 95% CI 0.513–0.904), use of anti-osteoporosis medication (AOM, OR 0.801, 95% CI 0.693–0.926), and women who had received fall prevention health education (OR 0.583, 95% CI 0.465–0.730) associated with lower risk. The areas under the curve of the prediction model was 0.818. The sensitivity was 67.0% and the specificity was 82.0%. The prediction model showed a good ability to predict the risk of subsequent fracture in older women with osteoporotic fractures and are suitable for early self-measurement which may benefit post-fracture management.
Similar content being viewed by others
Introduction
Osteoporotic fractures (OPFs), also known as fragility fractures, are fractures that occur after low-energy external forces due to increased bone fragility caused by decreased bone mass and destruction of the bone microstructure1. WHO data show that, globally, one-third of women and one-fifth of men over the age of 50 suffer one or more osteoporotic fractures, resulting in severe disability and 20% death rate within one year, and a 50% permanent disability rate2. Women are more likely than men to develop osteoporosis 5–10 years after menopause due to estrogen deficiency3. The incidence of hip fracture is twice as high in older women as in men4. The prevalence of osteoporosis is highest among postmenopausal women in the older population, with a prevalence of 51.6% in women over 65 years of age5. In recent years, some progress has been made in the orthopaedic treatment of osteoporotic fractures, but the prevention of subsequent fracture is still unsatisfactory. The main reason is that only 6.5% of patients in China received medications for treatment of osteoporosis within 6 months after a fracture, and the majority of patients are exposed to an extremely high risk of subsequent fracture6.
In 2013, the International Osteoporosis Foundation (IOF) stated in its "Global Initiative to Break the Cycle of Osteoporotic Fractures" that 50% of patients with osteoporotic fractures will suffer a subsequent fracture6. The risk of subsequent fracture increases exponentially in patients with osteoporotic fractures7,8. Compared with the index fracture, subsequent fracture are more harmful, and increases the risk of death by 55%9. Numerous studies have confirmed that subsequent fracture after a major osteoporotic fracture occurs within 2 years of the fracture and that 2 years is the "imminent" risk period for subsequent fracture10. The risk of subsequent fracture is 2.7 times higher within the first year of the first fracture than in patients with no history of fracture, with 67.1% of subsequent fractures occurring in the first year, of which 51.1% occurred within 6 months of the initial fracture11,12. Therefore, it is important to develop predictive models to determine the risk of subsequent fracture and identify controllable factors as early as possible after a fracture.
The risk factors for osteoporosis have been widely studied13. The risk factors for subsequent fracture are complex and multidimensional12. A Swedish research included 242,108 patients with osteoporotic fractures showed that advanced age and spinal fracture were independent risk factors for subsequent fracture, and the risk of subsequent fracture in patients with spinal fracture was 2.72 times higher than in patients with hip fracture14. Population-based registries in Denmark have identified female sex, older age, excessive alcohol consumption, living alone, and fracture history as risk factors for a second hip fracture15. Some studies have also found interactions between individual common independent risk factors, for example, Awal et al. found a cumulative effect of gender, age and skeletal pathology on the occurrence of subsequent fracture16.
Risk factors for subsequent fracture of osteoporotic fractures vary among populations in different regions, and effective risk screening and prevention can reduce the incidence of subsequent fracture. The predictive models FRAX (Fracture risk assessment tool), QFracture, and Garvan, which have been developed based on population data from the USA, UK, and Australia respectively, are utilized for identifying the risk of osteoporotic fractures17. FRAX does not incorporate important factors such as falls and medications, which may underestimate fracture risk. QFracture contains 31 risk factors and is suitable for patients with multiple chronic diseases17. The applicability of these two models in the Chinese population needs to be further verified. Garvan is suitable for individuals at high risk of falls, but Garvan is not a good predictor of risk in postmenopausal women18. In addition, the OSTA (osteoporosis self-assessment tool for Asians) is a simple assessment tool for self-screening for osteoporosis in postmenopausal women. The tool uses age and weight to calculate a risk index that guides the patient in determining the need for BMD testing. However, this tool has few indicators and low specificity19. Another method is to use diagnostic techniques such as dual-energy X-ray bone densitometry and quantitative CT to predict the risk of osteoporosis and determine the risk of fracture and fracture-prone areas accordingly. The implementation of this method is constrained by the uneven distribution of medical resources and the limited emphasis on preventive measures.
Although these tools can predict fracture risk, their predictive efficacy in the Chinese population remains to be explored. In addition, there are insufficient studies on the risk factors of subsequent fracture, and few literatures can systematically investigate and analyze the influence of multiple factors on the occurrence of subsequent fracture in older adults. We focused on the key population of osteoporotic fractures in older women and explored the influencing factors of the occurrence of subsequent fracture. At the same time, based on Chinese patient data, a localized older female subsequent fracture influencing factor model was constructed to provide a basis for clinical implementation of accurate risk prediction, prevention and management of subsequent fracture.
Results
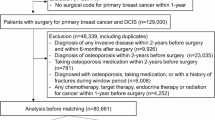
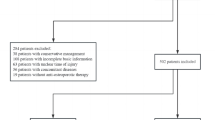
Characteristics of patients and disease
A total of 9212 older female were included in this study (Fig. 1). Data were obtained from 594 medical institutions in 31 provinces of China, with 77.7% in tertiary hospitals (the highest grade according to the Hospital Classification and Management Standards) and the remaining 22.3% in secondary hospitals. Descriptive characteristics for the participants are summarized in Table 1. The mean age of the patients was (74 ± 8.449) years, of which 75.7% were under 80 years of age and 24.3% were above 80 years of age. The BMI of older women was 22.91 ± 3.63.
There were 7551 patients with index fractures and 1661 with subsequent fractures. Compared with index fracture, subsequent fracture patients were on average older and had a higher number of comorbidity (P < 0.001). Patients in the subsequent fracture group had a higher percentage of surgical history, trauma history and family history than those in the first fracture group (P < 0.001). There was no statistically significant difference between the two groups in the comparison of smoking history (P = 0.803), while the percentage of alcohol consumption in the subsequent fracture group was more than that in the index fracture group (P = 0.011). In addition, the differences between two groups were significant in terms of occupation, educational, marital status, and number of children. There was no statistically significant difference between groups in terms of family income (P = 0.117).
Severe osteoporosis was diagnosed by BMD in 36.5% of patients. The highest percentage of fracture site was vertebral (45.5%), followed by hip (36.8%). Due to fall, 68.9% of the patients had fracture. Anti-osteoporosis medication (AOM) was applied to 47.7% of the patients, and complications occurred in 4.4% of the patients. The differences between the two groups were significant when comparing fracture site, cause of fracture, severity of osteoporosis, use of AOM, complication rate, and self-care ability (P < 0.001).
With regard to the prevention of subsequent fractures, 37.4% of patients were assessed for risk of falls and only 6.7% for risk of fracture. After a fracture 56.6% of patients used crutches, walkers or wheelchairs, 28.8% of women used calcium or vitamin D. There were significant differences between the two groups in the use of mobility aids, calcium or vitamin D, medication adherence, and receipt of fall prevention education (Table 1).
Risk factors of subsequent fracture
The univariate analyses of the association between independent variables and subsequent fracture in Table 2. The results found that the factors, including age, BMI, comorbidity, surgical history, trauma history, drinking history, occupation, education, marital status, number of children, and self-care ability were related to the risk of subsequent fracture.
Table 3 shows the results of multivariate logistic regression analyses of subsequent fracture based on univariate analyses results. Multivariate analysis showed that age, index fracture site, index fracture causes, risk assessment, BMD T-score ≤ −2.5, AOM use, fall prevention health education, surgical history, trauma history were associated with subsequent fracture. Individuals aged 70–79 years (OR 1.218, 95% CI 1.049–1.414) or aged ≥ 80 (OR 1.455, 95% CI 1.222–1.732) had a higher likelihood of experiencing subsequent fracture. Index fracture site of vertebrae (OR 1.472, 95% CI 1.194 to 1.815) and hip (OR 1.286, 95% CI 1.041–1.590) lead to higher risk of subsequent fracture. Index fracture of women caused by fall (OR 1.822, 95% CI 1.281–2.591), strain (OR 1.587, 95% CI 1.178–2.139), no inducement (OR 1.541, 95% CI 1.043–2.277) were more likely to suffer from subsequent fractures. Higher odds of subsequent fractures were also associated with high risk of fracture (OR 1.865, 95% CI 1.439–2.416), BMD T-score ≤ −2.5 (OR 1.725, 95% CI 1.440–2.067), history of surgery (OR 3.941, 95% CI 3.475–4.471) and trauma (OR–8.075, 95% CI 6.941–9.395). Patients who assessed as low risk of fall (OR 0.681, 95% CI 0.513–0.904), use of AOM (OR 0.801, 95% CI 0.693–0.926), and had received fall prevention health education (OR 0.583, 95% CI 0.465–0.730) were less likely to suffer from subsequent fractures.
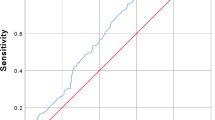
Construction of subsequent fracture risk prediction model and effect analysis
The risk prediction model was constructed using the results of multivariate analysis as predictors. The model demonstrated good predictive power with an area under the ROC curve (AUC) of 0.818 (95% CI 0.806–0.829), p < 0.001 (Fig. 2). The maximum value of Youden index was used to determine the optimal cutoff value of the prediction model. The maximum Youden index of the ROC curve was 0.494, and the optimal cutoff value was 0.207, in which the sensitivity was 67.0% and the specificity was 82.0%.
Discussion
Preventing subsequent fracture is a priority in reducing the harms of osteoporosis. 20% of patients with osteoporotic fracture will have a subsequent fracture within 1 year, which is 55% higher than the risk of death from the initial fracture, and 6.2 times higher than the economic burden20,21. The occurrence of subsequent fracture is detrimental to fracture healing, rehabilitation, self-care ability, and psychological expectations. At the same time, subsequent fracture leads to an increase in disability, incapacity, mortality and a decrease in the quality of life of the older population22. Taking hip fracture as an example, the morbidity and mortality rate within 1 year after fracture is as high as 36%, of which more than 70% of patients die due to subsequent fracture2. In our study, age, index fracture site, index fracture cause, fracture risk assessment and fall risk assessment, BMD T-score, AOM use, fall prevention health education, surgical history, trauma history were found to be independent risk factors for the occurrence of subsequent fracture.
The incidence of subsequent fractures in older women in our study was 18%. This result is lower than the findings of Yang et al. in OP patients over 65 years of age in Hebei, China (3-year postoperative subsequent fracture rate of 25.96%)23. However, the incidence of subsequent fracture in all-age OP in a meta-analysis was 13.4%24. Compared with all-age OP, the incidence of subsequent fracture in older females of our study is clearly higher. Consistent with our study, in a French cohort study of 560,499 patients with OF analyzed retrospectively, the incidence of subsequent fracture in women who experienced at least one subsequent fracture that resulted in hospitalisation was 17.9%11. The American Association of Clinical Endocrinologists (AACE) and American College of Endocrinology (ACE) 2020 edition of the Clinical Practice Guidelines for the Management of Postmenopausal Osteoporosis specify the definition of patients at very high risk of fracture and pharmacologic treatment options. For the prevention of subsequent fracture in postmenopausal women, the guidelines recommend standardized OP treatment, full follow-up, and monitoring of efficacy and adherence25. However, risk assessment methods for subsequent fracture have not been mentioned, and more research is urgently needed to optimize the risk assessment and management of subsequent fracture in this priority population.
It has been suggested that age is an important factor in increasing the risk of morbidity for all types of osteoporotic fractures13. The results of a retrospective study suggest that the effects of oestrogen deficiency on bone loss and impaired microstructure of bone tissue in postmenopausal women are more severe with age and that the risk of subsequent fracture increases with age3. Our study also validates this idea. senior older women over 80 years of age bear a greater risk of subsequent fracture than patients in the < 70 and 70–79 age groups. The magnitude of the risk of subsequent fracture varies depending on the ___location of the previous fracture and varies. Our study found a higher risk of subsequent fracture in vertebral fractures than in patients with hip fractures and fractures at other sites. Several cohort studies have found that patients with vertebral fractures have the highest risk of subsequent fracture among the types of previous fracture, and the lowest risk after tibia/fibula and ankle fractures2,26. Lindsay et al.27 suggested that patients with vertebral fractures have a five times higher incidence of secondary vertebral fractures than patients with no history of previous fracture. Our result suggests that the site of fracture is one of the important factors in the assessment of the risk of subsequent fracture. Patients with vertebral fractures should also be included in the focus of attention in the prevention of subsequent fracture.
Second, in our results, patients with fractures caused by falls, strain, no inducement had a greater risk of subsequent fractures than those caused by slight strike. Among these causes, falls accounted for the largest proportion of subsequent fractures (65.2%), and falls were controllable factors. Several guidelines state that falls are an independent risk factor for subsequent fracture28; and age and medication-induced imbalances also increase the risk of fracture from falls7. We found that patients who underwent assessment of low fall risk were less likely to suffer from subsequent fractures, suggesting that timely assessment of fall risk after fracture can be used as a means of subsequent fracture prevention. The 2013 UK Fracture Liaison Services (FLS) Code of Practice for the management of falls suggests that falls risk assessment is central to the prevention and treatment of subsequent fractures. Assessing falls risk and preventing falls is now available as a non-pharmacological intervention programme for the prevention of subsequent fractures8. Also, our study confirms that falls prevention health education is a protective factor in the occurrence of subsequent fracture. Multinational studies and consensus suggest that important non-pharmacological interventions for OF include fall risk assessment and health education to help patients understand the severity of subsequent fracture, the optimal time to prevent it, preventive and curative measures, and functional exercise29.
BMD is a non-invasive test that reflects bone mineral content, and a T-score ≤ −2.5 is the basis for osteoporosis diagnosis. The guideline indicates that T-score ≤ −2.5 with fracture is considered severe osteoporosis, and in China, BMD testing has been included in the routine physical examination of people over 40 years of age30. We found that patients with T-score ≤ −2.5, assessed as high risk of fracture, and those not using AOM had a higher risk of subsequent fracture. In our study 49.2% of OPF patients and 40.6% of subsequent fractures patients were treated with AOM, 93.3% were not assessed for fracture risk. This is a gap with the recommended strategies for the care of women with osteoporotic fractures in the guidelines5. Guidelines recommend that women over 65 years of age with pre-existing fragility fractures be considered for treatment without further evaluation5. In younger postmenopausal women, BMD test results can be used as a standard for medication5. Multiple consensus recommends that patients treated with anti-osteoporotic medications after a fracture should undergo annual BMD testing to assess fracture risk28,31,32. At present, unclear management responsibilities of subsequent fracture prevention and treatment lead to low risk assessment and treatment rates33. Secondly, many orthopaedic doctors still have a weak concept of prevention and management of subsequent fracture after osteoporotic fracture33. Moreover, patients’ concerns about the cost of diagnosis and treatment, adverse drug reactions and efficacy led to poor compliance with the management of subsequent fracture prevention and treatment34. Therefore, more effective strategies are urgently needed to regulate post-fracture management and reverse the disease burden of osteoporosis.
Patients with a history of trauma and surgery are at greater risk of subsequent fracture. The risk of subsequent fracture was 8.15 times higher in patients with a history of trauma than in those without a history of trauma. Siris et al.35 found that postmenopausal women with a history of previous fracture were more prone to secondary fracture and the risk increased with the number of previous fractures. Previous trauma leads to disruption of the bone structure and changes in the structure of the bone cortex and trabeculae, which in turn leads to a decrease in bone strength36. The risk of subsequent fracture in patients with a history of surgery is 3.98 times higher than in patients without a history of surgery. For example, percutaneous vertebroplasty (PVP) and percutaneous kyphoplasty (PKP) have a high incidence of secondary fractures after surgery22. Inadequate cement injection and excessive number of operated vertebrae lead to increased and unevenly distributed loading stresses on adjacent vertebrae, resulting in subsequent fracture37. Comorbidities and economic status were not included in the final model in this study, probably due to their correlation. Evidence suggests that patients with poor economic level have a tendency to have greater multimorbidity38. And economic level was correlated with patient frailty. Whereas high BMI and malnourishment are both associated with comorbidities and economic level38. Whether there is a mediating effect between these factors and fracture risk remains to be confirmed. In addition, the effect of alcohol consumption on subsequent fracture was not significant, probably due to the lower alcohol consumption of female patients in our study with a mean of 53.66 ± 18.890 ml/d. Guidelines indicate that excessive alcohol consumption is associated with increased fracture risk, where alcohol intake of more than 3 units/d (90 ml/d of spirits) is considered excessive30.
The principle of rehabilitation in the management of subsequent fracture is to balance two factors "promoting fracture healing" and "preventing bone loss". It is necessary to prevent premature rehabilitation training from affecting fracture healing, as well as complications such as bone loss, disuse induced muscle atrophy, pneumonia, and lower limb venous thrombosis caused by long-term immobilization. Therefore, OPF patients should be predicted for subsequent fracture risk as early as possible on the basis of standardized treatment, and high-risk groups should be screened for individualized rehabilitation interventions.
In comparison, the prediction model constructed in our study covers 10 pre-discharge static indicators, and the information is easy to obtain and simple to operate. It has been internally validated to show good discriminatory performance and is expected to form a clinically usable tool after further validation and optimisation. Although we included a large national sample, limitations remain. First, we did not collect complete surgical treatment modalities. Although some studies have shown a high incidence of secondary fractures after percutaneous vertebro plasty (PVP) and percutanouskyphoplasty (PKP) for osteoporotic vertebral compression fracture (OVCF)22. Secondly, self-reported form of data collection may be subject to recall bias, leading to possible inaccurate BMD reporting results and the time difference between subsequent and index fractures. Therefore, registration and long-term follow-up of patients with osteoporotic fractures is relevant to explore the pattern of subsequent fracture occurrence. Third, this data from 31 provinces of the country were not followed up, limiting our study to the analysis of out-of-hospital risk factors in this population. Fourth, this study was limited to inpatients and did not include patients attending outpatient clinics, which may have led to an underestimation of the incidence of subsequent fractures. To address these shortcomings, a subsequent fracture cohort could be established in the future to further explore the effects of surgical approach, type of trauma, BMD, nutrition, and health behaviours on subsequent fractures and time to occurrence. Furthermore, this study demonstrated that patients with AOM had a lower risk of subsequent fracture. This suggests that we should focus on the effects of AOM dose, duration of treatment and compliance on the occurrence of subsequent fractures. In the future, we will externally validate the model and develop user-friendly tools such as mobile phones or web application to enhance the promotional value of the model.
In this study, we collected data based on patient self-report, and 10 independent risk factors were included in the final prediction model, including age, index fracture site, index fracture cause, fracture risk assessment and fall risk assessment, BMD T-score, AOM use, fall prevention health education, surgical history, trauma history. These risk factors are easy to collect and help older adults self-assess and identify subsequent fracture risk. The results of this study highlight the critical importance of better managing older women with osteoporotic to improve screening for high risk of subsequent fracture as well as developing effective strategies to reduce the risk of subsequent fracture. This study provides clinicians and patients with an easy subsequent fracture risk assessment tool that is expected to yield benefits in reducing subsequent fracture incidence and osteoporotic mortality.
Methods
Study design and data collection
This national study was conducted by the Orthopedic Nursing Committee of Chinese Nursing Association. In order to take into account factors such as regional distribution and regional economy, 580 medical institutions in 31 provinces of China were selected by multistage sampling method for data collection. From September 2023 to December 2023, we included data on 9212 older women hospitalized for osteoporotic fractures.
The method of multistage sampling was adopted in our study. The first stage, we divided into four regions, northeast, east, central and west, according to the division of China's economic regions. In accordance with the principle of geographic decentralization and economic diversity, a number of cities were selected from each region and all provinces were covered. In the second stage, 2 to 3 hospitals were selected from each city. Considering the feasibility of the study, the selected hospitals should have administrators who are members of the orthopedic Nursing Professional Committee of the Chinese Nursing Association. In the third stage, the investigators of each hospital were responsible for including patients and collecting data in orthopedic wards according to inclusion criteria and exclusion criteria.
Participants
We defined older patients as aged ≥ 60 years. Inclusion criteria: (1) People aged ≥ 60 years; (2) Patients diagnosed with osteoporotic fracture and undergoing (hip/vertebral/humerus/radius) osteoporotic fracture surgery; (3) Patients in stable condition after surgery, in the recovery period, and not yet discharged from the hospital. (4) The first fracture and recurrent fracture were fractures caused by non-violent factors (e.g. fall, daily activities or minor trauma) and supported by clinical records (e.g. surgical reports, clinical records, previous or current X-rays). (5) The person agreed and cooperated to participate in the research and could understand the researcher's instructions. Exclusion criteria: (1) Pathological fracture (pathological fracture caused by malignant tumour, tuberculosis and other bone metabolic diseases that can cause fracture); (2) Serious traumatic fracture; (3) People with combined mental disorders; (4) Patients with combined other bone diseases such as osteoarthrosis; (5) People with severe anxiety, depression, and other emotions unable to cooperate in completing the questionnaire. This study was approved by the Ethics Committee of Chinese PLA General Hospital (No. S2023-621-01). The Orthopedic Nursing Professional Committee has designated personnel responsible for data collection, and has obtained ethical approval from various hospitals before data collection. All methods in this research were performed in accordance with the Declaration of Helsinki.
Variables
Variables analyzed as risk factors for subsequent fracture were derived from clinical risk factors (CRFs) that may have an independent effect on fracture risk in clinical practice and literature studies. (1) General Information: age, BMI, comorbidity, trauma history, surgical history, family history of osteoporosis, smoking, alcohol consumption, occupation, education, marital status, average annual household income, and characteristics of the hospital where the patient was admitted (e.g. hospital level, hospital type, mode of admission). Trauma history mainly includes musculoskeletal injury caused by falls or other reasons. Surgical history refers to the history of orthopedic surgery in this study. (2) Characteristics of index fracture: fracture site, cause of fracture, BMD T-score. (3) Prevention information after index fracture: use of AOM, Use of calcium or vitamin D, fall risk assessment, fracture risk assessment, walking aids, fall prevention health education.
Sample size
The sample size for Logistic regression was calculated empirically and we took 10 to 20 times of the risk factors. There were 35 suspected potential factors. Assuming a non-response rate of 10% for the study population, then the minimum sample size of events required was 385–770. The actual number of patients included was 9212.
Statistical analysis
Data with > 30% missing information were excluded in our study. All variables that were to be included in the regression analysis were used in the imputation process. Then, duplicates and orphaned data were removed and irrational data were corrected.
In this study, a comprehensive statistical analysis approach was utilized to ensure the robustness and reliability of our predictive model. Initially, data analysis was conducted using SPSS 25.0 for quantitative and categorical data. Quantitative data were described using mean ± SD and analyzed with independent samples t-tests to compare differences across groups. Categorical data were expressed as percentages and subjected to χ2 tests, Fisher's exact test, or contingency tables analysis, as deemed appropriate.
Further analytical depth was added by including CRFs in univariate analyses to calculate ORs for various risk factors, identifying those significant with a P-value less than 0.05. These significant variables were subsequently incorporated into a multivariate logistic regression model to pinpoint independent risk factors, employing R 4.1.3. Internal validation of the model was further strengthened through 1000 bootstrap resamplings, aiming to estimate Harrell's C-index. This provided a quantitative measure of the model's predictive performance, reinforcing the validity of our findings.
Additionally, the discriminative ability of the model was evaluated by calculating the Area Under the ROC curve (AUC). The AUC assess the model's sensitivity and specificity at different thresholds, while the overall classification accuracy offered a comprehensive measure of the model's overall ability to correctly classify samples within the CV framework. In statistical terms, a P-value less than 0.05 was adopted as the criterion for significant differences, ensuring that improvements in model performance were statistically significant.
Ethics approval statement
This study was approved by the Ethics Committee of Chinese PLA General Hospital (No. S2023-621-01). All methods in this research were performed in accordance with the Declaration of Helsinki.
Consent for publication
The informed consents were obtained from participants.
Data availability
The data could be obtained from corresponding author.
References
Hernlund, E. et al. Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch. Osteoporos. 8, 136. https://doi.org/10.1007/s11657-013-0136-1 (2013).
Adachi, J. D. et al. Fragility fracture identifies patients at imminent risk for subsequent fracture: real-world retrospective database study in Ontario, Canada. BMC Musculoskelet. Disorders 22, 224. https://doi.org/10.1186/s12891-021-04051-9 (2021).
Zhu, X. et al. Risk factors of primary and recurrent fractures in postmenopausal osteoporotic Chinese patients: A retrospective analysis study. BMC Womens Health 22, 465. https://doi.org/10.1186/s12905-022-02034-z (2022).
Dennison, E., Cole, Z. & Cooper, C. Diagnosis and epidemiology of osteoporosis. Curr Opin. Rheumatol. 17, 456–461. https://doi.org/10.1097/01.bor.0000166384.80777.0d (2005).
Kanis, J. A., Cooper, C., Rizzoli, R. & Reginster, J. Y. European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos. Int 30, 3–44. https://doi.org/10.1007/s00198-018-4704-5 (2019).
Wang, L. et al. Prevalence of osteoporosis and fracture in China: the China osteoporosis prevalence study. JAMA Netw Open 4, e2121106. https://doi.org/10.1001/jamanetworkopen.2021.21106 (2021).
Akesson, K. et al. Capture the Fracture: A Best Practice Framework and global campaign to break the fragility fracture cycle. Osteoporos. Int. 24, 2135–2152. https://doi.org/10.1007/s00198-013-2348-z (2013).
Javaid, M. K. et al. A patient-level key performance indicator set to measure the effectiveness of fracture liaison services and guide quality improvement: a position paper of the IOF Capture the Fracture Working Group, National Osteoporosis Foundation and Fragility Fracture Network. Osteoporos. Int. 31, 1193–1204. https://doi.org/10.1007/s00198-020-05377-1 (2020).
Sobolev, B., Sheehan, K. J., Kuramoto, L. & Guy, P. Excess mortality associated with second hip fracture. Osteoporos. Int. 26, 1903–1910. https://doi.org/10.1007/s00198-015-3104-3 (2015).
Roux, C. & Briot, K. Imminent fracture risk. Osteoporos. Int. 28, 1765–1769. https://doi.org/10.1007/s00198-017-3976-5 (2017).
Roux, C. et al. Refracture and mortality following hospitalization for severe osteoporotic fractures: The Fractos Study. JBMR plus 5, e10507. https://doi.org/10.1002/jbm4.10507 (2021).
Ma, X. et al. Re-fracture and correlated risk factors in patients with osteoporotic vertebral fractures. J. Bone Miner. Metab 37, 722–728. https://doi.org/10.1007/s00774-018-0974-4 (2019).
Silva, B. C. et al. Definition and management of very high fracture risk in women with postmenopausal osteoporosis: a position statement from the Brazilian Society of Endocrinology and Metabolism (SBEM) and the Brazilian Association of Bone Assessment and Metabolism (ABRASSO). Arch. Endocrinol. Metab. 66, 591–603. https://doi.org/10.20945/2359-3997000000522 (2022).
Rosengren, B. E., Björk, J., Cooper, C. & Abrahamsen, B. Recent hip fracture trends in Sweden and Denmark with age-period-cohort effects. Osteoporos. Int. 28, 139–149. https://doi.org/10.1007/s00198-016-3768-3 (2017).
Ryg, J., Rejnmark, L., Overgaard, S., Brixen, K. & Vestergaard, P. Hip fracture patients at risk of second hip fracture: a nationwide population-based cohort study of 169,145 cases during 1977–2001. J. Bone Miner. Res. 24, 1299–1307. https://doi.org/10.1359/jbmr.090207 (2009).
Awal, R., Ben Hmida, J., Luo, Y. & Faisal, T. Study of the significance of parameters and their interaction on assessing femoral fracture risk by quantitative statistical analysis. Med. Biol. Eng. Comput. 60, 843–854. https://doi.org/10.1007/s11517-022-02516-0 (2022).
Agarwal, A. et al. Predictive performance of the Garvan Fracture Risk Calculator: A registry-based cohort study. Osteoporos. Int. 33, 541–548. https://doi.org/10.1007/s00198-021-06252-3 (2022).
Crandall, C. J. et al. Predicting fracture risk in younger postmenopausal women: Comparison of the Garvan and FRAX risk calculators in the women’s health initiative study. J. Gen. Internal Med. 34, 235–242. https://doi.org/10.1007/s11606-018-4696-z (2019).
Gao, C., Song, H., Chen, B., Zhang, Z. & Yue, H. The assessment of the osteoporosis self-assessment tool for asians and calcaneal quantitative ultrasound in identifying osteoporotic fractures and falls among Chinese people. Front. Endocrinol. Lausanne 12, 684334. https://doi.org/10.3389/fendo.2021.684334 (2021).
Balasubramanian, A. et al. Risk of subsequent fracture after prior fracture among older women. Osteoporos. Int. 30, 79–92. https://doi.org/10.1007/s00198-018-4732-1 (2019).
Borgström, F. et al. Fragility fractures in Europe: Burden, management and opportunities. Arch. Osteoporos. 15, 59. https://doi.org/10.1007/s11657-020-0706-y (2020).
Dai, C., Liang, G., Zhang, Y., Dong, Y. & Zhou, X. Risk factors of vertebral re-fracture after PVP or PKP for osteoporotic vertebral compression fractures, especially in Eastern Asia: A systematic review and meta-analysis. J. Orthop. Surg. Res. 17, 161. https://doi.org/10.1186/s13018-022-03038-z (2022).
Yang, Z. et al. Epidemiological investigation of 387 individuals over 65 years old with osteoporotic fractures. Altern Ther Health Med 29, 207–211 (2023).
Wu, C. H. et al. Fracture liaison services improve outcomes of patients with osteoporosis-related fractures: A systematic literature review and meta-analysis. Bone 111, 92–100. https://doi.org/10.1016/j.bone.2018.03.018 (2018).
Camacho, P. M. et al. American association of clinical endocrinologists/american college of endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis-2020 update. Endocr. Pract. 26, 1–46. https://doi.org/10.4158/gl-2020-0524suppl (2020).
Toth, E. et al. History of previous fracture and imminent fracture risk in Swedish women aged 55 to 90 years presenting with a fragility fracture. J. Bone Miner. Res. 35, 861–868. https://doi.org/10.1002/jbmr.3953 (2020).
Lindsay, R. et al. Risk of new vertebral fracture in the year following a fracture. JAMA 285, 320–323. https://doi.org/10.1001/jama.285.3.320 (2001).
Chan, D. D. et al. Consensus on best practice standards for Fracture Liaison Service in the Asia-Pacific region. Arch. Osteoporos. 13, 59. https://doi.org/10.1007/s11657-018-0463-3 (2018).
Ebeling, P. R. et al. Secondary prevention of fragility fractures in Asia Pacific: An educational initiative. Osteoporos. Int. 31, 805–826. https://doi.org/10.1007/s00198-019-05197-y (2020).
Research, C. S. O. O. A. B. M. Guidelines for the diagnosis and treatment of primary osteoporosis (2022). Chin. J. Endocrinol. Metab. 39, 377–406 (2023).
Sanchez-Rodriguez, D. et al. The Belgian Bone Club 2020 guidelines for the management of osteoporosis in postmenopausal women. Maturitas 139, 69–89. https://doi.org/10.1016/j.maturitas.2020.05.006 (2020).
Laura, I. et al. Which treatment to prevent an imminent fracture?. Bone Rep 15, 101105. https://doi.org/10.1016/j.bonr.2021.101105 (2021).
Osuna, P. M., Ruppe, M. D. & Tabatabai, L. S. Fracture liaison services: Multidisciplinary approaches to secondary fracture prevention. Endocr Pract. 23, 199–206. https://doi.org/10.4158/ep161433.Ra (2017).
Hiligsmann, M. et al. Determinants, consequences and potential solutions to poor adherence to anti-osteoporosis treatment: results of an expert group meeting organized by the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO) and the International Osteoporosis Foundation (IOF). Osteoporos. Int. 30, 2155–2165. https://doi.org/10.1007/s00198-019-05104-5 (2019).
Siris, E. S. et al. Enhanced prediction of fracture risk combining vertebral fracture status and BMD. Osteoporos. Int. 18, 761–770. https://doi.org/10.1007/s00198-006-0306-8 (2007).
Greising, S. M., Corona, B. T. & Call, J. A. Musculoskeletal regeneration, rehabilitation, and plasticity following traumatic injury. Int. J. Sports Med. 41, 495–504. https://doi.org/10.1055/a-1128-7128 (2020).
Ding, J. K., Zhao, B. & Zhai, Y. F. Subsequent fractures after vertebroplasty in osteoporotic vertebral fractures: A meta-analysis. Neurosurg. Rev. 45, 2349–2359. https://doi.org/10.1007/s10143-022-01755-x (2022).
Kay, R. S., Ho, L., Clement, N. D., Duckworth, A. D. & Hall, A. J. The incidence of subsequent contralateral hip fracture and factors associated with increased risk: The IMPACT Contralateral Fracture Study. Osteoporos. Int. 35, 903–909. https://doi.org/10.1007/s00198-024-07039-y (2024).
Acknowledgements
We would like to thank all the patients participating in our study and all the clinical staffs for their guidance and support. In addition, we would like to thank Dr. Yangyi Hu for his guidance on the methodology of this study.
Funding
National Natural Science Foundation of China, 72204262.
Author information
Authors and Affiliations
Contributions
Qingmei Wang, Qingqing Su, and Yuan Gao designed the study. Nan Tang, Ling Gao, and Jie Song collected the data. Yeyuan Li, Mi Song, Chen Qiu, Mengqi Shao, Jingru Chen, Shan Li, and Nan Tang drafted the manuscript. Yuan Gao and Nan Tang revised the manuscript. All authors contributed to the critical and substantial revisions and the final approval of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tang, N., Gao, L., Song, J. et al. Risk analysis for subsequent fracture of osteoporotic fractures in Chinese women over age 60: a nationwide cross-sectional study. Sci Rep 14, 13319 (2024). https://doi.org/10.1038/s41598-024-64170-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-64170-w