Abstract
Osteoporosis, vertebral fractures, and spinal degenerative diseases are common conditions that often coexist in older adults. This study aimed to determine the factors influencing low back pain and its impact on activities of daily living (ADL) and physical performance in older individuals with multiple comorbidities. This cross-sectional study was part of a large-scale population-based cohort study in Japan, involving 1009 participants who underwent spinal magnetic resonance imaging (MRI) to assess cervical cord compression, radiographic lumbar spinal stenosis, and lumbar disc degeneration. Vertebral fractures in the thoracolumbar spine were evaluated using sagittal MRI with a semi-quantitative method. Bone mineral density was measured using dual-energy X-ray absorptiometry. Low back pain, Oswestry Disability Index (ODI), and physical performance tests, such as one-leg standing time, five times chair-stand time, maximum walking speed, and maximum step length, were assessed. Using clinical conditions as objective variables and image evaluation parameters as explanatory variables, multiple regression analysis showed that vertebral fractures were significantly associated with low back pain and ODI. Vertebral fractures and osteoporosis significantly impacted physical performance, whereas osteoporosis alone did not affect low back pain or ODI. Our findings contribute to new insights into low back pain and its impact on ADL and physical performance.
Similar content being viewed by others
Introduction
Many countries, especially developed ones, have been facing rapid population aging1,2. Declining musculoskeletal health is a significant concern as it can be an initiating factor for other systemic problems. Studies have shown that musculoskeletal disorders not only cause pain and disability but also lead to secondary health issues such as cardiovascular diseases and mental health disorders due to reduced physical activity and chronic pain3,4. Additionally, musculoskeletal disorders are among the most prevalent health conditions worldwide, affecting millions of people and placing a substantial burden on healthcare systems3,4. Furthermore, older individuals generally have multiple coexisting conditions. For example, limited to spinal disease, include osteoarthritis, cervical and lumbar spinal stenosis, and osteoporotic vertebral fracture often coexist in the elderly5. These coexisting conditions can complicate treatment and management, making it even more critical to address musculoskeletal health proactively6.
Therefore, establishing a strategy for the early treatment and prevention of musculoskeletal diseases to improve the healthy life expectancy of people is crucial. In addition, understanding and addressing musculoskeletal decline in the geriatric population are essential for promoting healthy aging, improving the quality of life (QOL) for older individuals, and managing the associated healthcare challenges4,7,8. In musculoskeletal disorders, osteoporosis and spinal degenerative disorders are important clinical conditions affecting older individuals and are the focus of our current study. There have been reports indicating that adult sagittal malalignment influences the stresses and loads on lumbar radiographic degenerative changes, which may interact with low back pain9. Additionally, studies have shown that low back pain and decreased walking ability are independently associated with severe vertebral fractures, and decreased walking ability is associated with multiple vertebral fractures in women10. Therefore, it is expected that the presence of osteoporosis itself is associated with low back pain, as osteoporosis increases the risk of vertebral compression fractures. On the other hand, osteoporotic vertebral fractures result in low back pain and affect individuals’ activities of daily living (ADL) and QOL11,12,13,14. Older individuals generally have multiple coexisting conditions. Although the prevalence of these conditions and their association with clinical symptoms have been previously reported15,16,17,18,19, the influence of comorbid conditions on clinical symptoms remains unknown. Furthermore, no large cohort studies have examined which of these spinal degenerative disorders has the greatest impact.
In 2008, we initiated “the Wakayama Spine Study,” a population-based cohort study aimed at, determining the prevalence of low back pain, osteoporosis, and spinal degenerative diseases, and assessing their impact on ADL/QOL in the general population. The Wakayama Spine Study facilitated the diagnosis of osteoporosis, vertebral fractures, and cervical and lumbar spinal stenosis, thereby allowing us to address the aforementioned objectives. This study aimed to evaluate the coexistence of osteoporosis and spinal degenerative disorders in the general population, and to determine the actual factors influencing low back pain and its impact on ADL and physical performance in older individuals with multiple comorbidities. It is important to note that addressing osteoporosis and spinal degeneration often requires a multidisciplinary approach, which may include lifestyle modification, physical therapy, pharmacotherapy, and surgical intervention. We hope that the results of our study will provide valuable insights to benefit patients in need.
Results
Table 1 shows the characteristics of the 1011 participants, including their ages and anthropometric measurement data obtained in this study. The mean age and prevalence of low back pain did not differ significantly between men and women; however, the body mass index (BMI) was significantly lower in women than in men. Among the image evaluation parameters, cervical cord compression, vertebral fractures, and osteoporosis were significantly different between the sexes (all P < 0.05), whereas radiographic lumbar spinal stenosis.
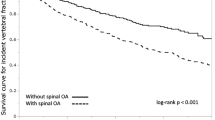
Multiple regression analysis or multiple logistic regression analysis was performed with low back pain, Oswestry Disability Index (ODI), and physical performance tests as objective variables and image evaluation parameters (all predictors in the left column in Tables 2, 3 and 4) as explanatory variables. After adjusting for sex, age, BMI, and other image evaluation predictors (in Model 3), rLSS, LDD, and vertebral fractures were found to be associated with low back pain (P = 0.0034, 0.0027, and 0.0321, respectively) but not with cervical cord compression and osteoporosis. Similarly, cervical cord compression and vertebral fractures were associated with the ODI (P = 0.0119 and 0.0066, respectively). In addition, the same multiple logistic regression analysis was performed for physical performance tests. No parameter was significantly associated with one-leg standing time (OLS). Five times chair-stand time (CST) was significantly associated with cervical cord compression and vertebral fractures (P = 0.0021 and P = 0.0080, respectively). Four of the five image evaluation parameters (cervical cord compression, LDD, vertebral fractures, and osteoporosis) were significantly associated with 6-m walking time at a maximal pace (maximum walking speed) prolongation (P = 0.0001, 0.0270, 0.0016, and 0.0144, respectively). Furthermore, cervical cord compression and osteoporosis were associated with a decrease in step length at a maximal pace (maximum step length) (P = 0.0004 and 0.0272, respectively).
Discussion
This study demonstrated that rLSS, LDD, and vertebral fractures were significantly associated with low back pain, whereas cervical cord compression and vertebral fractures were significantly associated with ODI. However, osteoporosis was not significantly associated with low back pain and low back pain-related ADL disorders, as measured using the ODI in the general population. Several previous studies have investigated the osteoporosis and low back pain. Some basic experimental studies have shown a link between osteoporosis and low back pain20,21,22,23, and certain clinical studies have suggested that osteoporosis can lead to chronic low back pain24. However, the true association between osteoporosis and low back pain in a large population-based cohort remains poorly understood. Our finding that osteoporosis was not independently associated with low back pain in our general population cohort study is novel. In contrast, vertebral fractures were identified as independent factors associated with low back pain and low back pain-related ADL disorders. Previous studies have also reported an association between vertebral fractures and low back pain25,26,27,28, ADL, and health-related quality of life (HRQoL)11,12,13,14, which is consistent with our findings.
Furthermore, we measured and evaluated several physical performance indicators of locomotive syndrome, including OLS, CST, maximum walking speed, and maximum step length. We analyzed the relationships between these indices and osteoporosis as well as spinal degenerative disorders (cervical cord compression, rLSS, LDD, and vertebral fractures). In the physical performance test, none of the predictors was associated with OLS, but cervical cord compression and vertebral fractures were associated with CST delay. Cervical cord compression, LDD, vertebral fractures, and osteoporosis were associated with maximum walking speed prolongation, and cervical cord compression and osteoporosis with maximum step length. Focusing on vertebral fractures and osteoporosis, the results indicated that vertebral fractures was significantly associated with CST delay and maximum walking speed prolongation, whereas osteoporosis was significantly associated with maximum walking speed prolongation and step length. In other words, both vertebral fractures and osteoporosis affect physical performance. Stanghelle et al.29 emphasized the importance of pain management and exercise interventions in older women with osteoporosis and vertebral fractures, as both pain and walking speed were independently associated with HRQoL, which aligns with our study results. Moreover, by comparing the standardized partial regression coefficient, we estimated that physical performance was more strongly associated with vertebral fractures than with osteoporosis.
In summary, our findings suggest that vertebral fractures influence low back pain, low back pain-related ADL, and physical performance. Several studies have shown a relationship between low back pain and radiographic degenerative changes30,31,32, and some have reported that low bone mineral density is associated with kyphotic deformity. For example, The Framingham Study, which involved spinal computed tomography on approximately 2000 adolescents and young adults, revealed a strong association between low bone density and thoracic kyphosis. It suggested that this factor may be predominantly genetic in origin33. In addition, Tanishima et al.34 reported that decreased bone density was independently associated with kyphosis in older individuals living in a mountain area. Therefore, kyphotic deformity may be observed in older individuals due to subclinical vertebral fractures caused by low bone density. Furthermore, based on our previous studies35,36, which revealed that spinal malalignment, particularly kyphotic deformity, was associated with low back pain, we infer that kyphotic deformity resulting from vertebral fractures causes low back pain, low back pain-related ADL disorders, and poor physical performance. The prevalence of vertebral fractures has been reported as a risk factor for new vertebral fractures37,38, and vertebral fractures are associated with mortality and life expectancy39,40. Together with our results, these findings highlight the importance of preventing vertebral fractures as a critical clinical concern. Although osteoporosis itself was not associated with low back pain or low back pain-related ADL disorders in this study, early intervention for the treatment of osteoporosis, a condition preceding the development of spinal kyphotic deformities, is crucial. According to Sinaki et al.41 individuals with osteoporosis-related kyphosis exhibited significantly higher balance abnormalities than those in the control group, and thoracic hyperkyphosis, in combination with reduced muscle strength, plays a central role in increasing body sway, gait unsteadiness, and the risk of falls in osteoporosis patients. Therefore, improving physical performance is an important factor in preventing vertebral fractures.
This study had some limitations. First, although it included over 1000 participants, they may not fully represent the general population, as they were recruited from only two areas in Japan. However, we compared the anthropometric measurements of the study participants with those of the general Japanese population42 and found no significant differences in BMI for either men (BMI: 23.71 [3.41] and 23.95 [2.64] kg/m2, P = 0.33, respectively) or women (BMI: 23.06 [3.42] and 23.50 [3.69] kg/m2, P = 0.07, respectively). Second, this was a cross-sectional study, which limited our ability to establish causal relationships between osteoporosis and physical performance. The ongoing Wakayama Spine Study, a longitudinal survey, will provide further insight into these causal relationships. Third, we did not examine the psychosocial factors associated with low back pain. Nevertheless, we believe that this study is superior to previous studies, as it evaluated bone mineral density (BMD) using dual-energy X-ray absorptiometry (DXA) and performed spinal magnetic resonance imaging (MRI) assessments in the general population. In addition, we performed a multidimensional evaluation of low back pain, low back pain-related ADLs, and physical performance.
In conclusion, we found that osteoporosis was not significantly associated with low back pain and related ADL disorders (ODI) and that vertebral fractures were related to low back pain, ADL disturbance, and agility decline. These results suggest that the prevention of vertebral fractures is crucial. These findings contribute to multidimensional research on low back pain, low back pain-related ADLs, and physical performance. Needless to say, it is important to note that addressing osteoporosis and spinal degeneration often requires a multidisciplinary approach, which may include lifestyle modification, physical therapy, pharmacotherapy, and surgical intervention. We hope that the results of our study will provide valuable insights to benefit patients in need. Further investigations, along with follow-up surveys, should be conducted to elucidate the causes of low back pain and related disorders.
Methods
Ethical statement
All procedures in this study involving human participants were performed in accordance with the ethical standards of the institutional and national research committee and the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was conducted with the approval of the ethical committees of the University of Tokyo (nos. 1264 and 1326) and Tokyo Metropolitan Institute of Gerontology (no. 5). Informed consent was obtained from all the study participants.
Participants
This population-based study of degenerative spinal diseases, titled the Wakayama Spine Study, was conducted as a sub-cohort of a large-scale Population-based cohort study named the Research on Osteoarthritis/Osteoporosis Against Disability (ROAD). ROAD is a nationwide prospective study of bone and joint diseases, comprising population-based cohorts from various communities in Japan. A detailed profile of the ROAD study has been previously described43,44,45,46. The baseline database for this study included clinical and genetic information of 3040 inhabitants (1061 men and 1979 women; mean age: 70.6 years; age range: 23–95 years). Participants were recruited from resident registration listings in three communities with different characteristics: an urban region in Itabashi, Tokyo; a mountainous region in Hidakagawa, Wakayama; and a coastal region in Taiji, Wakayama. The participants completed an interviewer-administered questionnaire consisting of 400 items, including lifestyle information such as occupational career, smoking habits, alcohol consumption, family history, medical history, physical activity, reproductive variables, and health-related QOL. However, not all surveys were utilized in the present study; instead, only essential sections were analyzed.
Here, we briefly summarize the profile of the present study. The second visit of the ROAD study began in 2008 and was completed in 2010. All participants in the baseline study were invited to participate in the second visit. In addition to the former participants, inhabitants aged 60 years and older in the urban area and those aged 40 years and younger in the mountainous and coastal areas who were willing to participate in the ROAD survey were also included in the second visit (both the mountainous and coastal areas were in Wakayama prefecture). Finally, 2674 individuals (900 men, 1774 women) participated in the second visit of the ROAD study, comprising 1067 individuals (353 men, 714 women) in the urban area, 742 individuals (265 men, 477 women) in the mountainous area, and 865 individuals (282 men, 583 women) in the coastal area. Among these three communities in the ROAD study, the mountainous and coastal areas, from which we invited all 1607 participants (547 men, 1060 women) to the Wakayama Spine Study, are located in Wakayama prefecture. However, 1063 participants responded to the invitation for the Wakayama Spine Study, and 52 participants declined; therefore, a total of 1011 individuals provided written informed consent and attended the Wakayama Spine Study with MRI examinations. A mobile MRI unit (Excelart 1.5 T, Toshiba, Tokyo, Japan) was used, and a total spinal MRI was performed for all participants on the same day as the clinical examination. Two participants for whom MRI was contraindicated due to the presence of a pacemaker were excluded; thus, 1009 individuals (335 men and 674 women; mean age: 66.3 years; age range: 21–97 years) participated in this study (Fig. 1). BMD was measured at the femoral neck using DXA (with Hologic Discovery DXA system; Hologic, Waltham, MA, USA).
Definition of low back pain
Experienced board-certified orthopedic surgeons asked all the participants the following question regarding low back pain: “Have you experienced low back pain on most days during the past month, in addition to now?” Those who answered “yes” were defined as having low back pain, as previously described43,47,48,49,50. Low back pain in this study is defined as pain persisting for at least 1 day, located in the posterior aspect of the trunk, between the 12th rib and the lower border of the gluteal sulcus. It may or may not be accompanied by radiating pain in one or both lower limbs51.
ODI
The ODI, derived from the Oswestry Low Back Pain Questionnaire52,53,54, was used by clinicians and researchers to quantify the level of disability due to low back pain. The patient questionnaire included several questions related to pain intensity, ability to walk, sit, stand, self-care, travel, sexual function, lifting, social life, and sleep quality. Participants selected responses that most closely resembled their symptoms. The index scores ranged from 0 to 100, with “0” indicating no disability and “100” indicating the most severe. In this study, we considered ODI as low back pain-related ADL disorders.
Evaluation of cervical cord compression
Cervical cord compression was defined as the compression of the anterior and posterior components of the spinal cord, as previously described55. Cervical cord compression was evaluated at each intervertebral level from C2/3 to C7/Th1 and graded as follows: grade 0, no compression of the spinal cord, but the subarachnoid space was present; grade 1, no compression of the spinal cord without the subarachnoid space; grade 2, compression of less than one-third of the spinal cord; grade 3, compression of more than one-third but less than two-thirds of the spinal cord; and grade 4, compression of more than two-thirds of the spinal cord. Cervical cord compression was defined as grade 2 or higher at the most severely affected intervertebral disc level and was analyzed accordingly (Fig. 2). Intra- and inter-observer variabilities for cervical cord compression, evaluated using kappa analysis, were 0.78 and 0.72, respectively, and were deemed sufficient for assessment55.
Evaluation of rLSS
The severity of rLSS was assessed using qualitative measurements performed by a well-experienced orthopedic surgeon. Axial images at each lumbar intervertebral level (L1/2 to L5/S1) were obtained from the films, as previously described56. The severity of central stenosis was assessed according to general guidelines (Suri classification)57. According to the Suri classification, the rLSS was divided into four levels: grade 0, no narrowing; grade 1, mild narrowing of less than one–third of the normal area; grade 2, moderate narrowing of one–third to two–thirds of the normal area; and grade 3, severe narrowing of more than two–thirds of the normal area. rLSS was defined as grade 3 at the most severely affected lumbar intervertebral disc level and was analyzed accordingly (Fig. 3). Intra- and inter-observer variabilities for rLSS, evaluated using kappa analysis, were 0.82 and 0.77, respectively, and were deemed sufficient for assessment56.
Evaluation of LDD
The degree of LDD on MRI (Fig. 4a) was classified into five grades based on the Pfirrmann classification system58, as previously described59. The total score (5–25), which was the sum of each intervertebral grade at L1/2–5/S, was used as the index. Intra- and inter-observer variabilities for LDD, evaluated using kappa analysis, were 0.94 and 0.94, respectively, and were deemed sufficient for assessment59.
Evaluation of vertebral fractures in the thoracolumbar spine
Vertebral fractures and their severity were assessed using the Genant semi-quantitative (SQ) method60 with sagittal MR images of the Th11-L1 vertebrae (Fig. 4b). The SQ method was graded from 0 to 3, defined as follows: grade 0 = normal; grade 1 = mildly deformed (approximately 20–25% reduction in anterior, middle, and posterior height, and a 10–20% reduction in area); grade 2 = moderately deformed (approximately 25–40% reduction in height and a 20–40% reduction in area); and grade 3 = severely deformed (approximately 40% reduction in height and area). The total score (0–9) was used as an index by summing the respective grades of the Th11-L1 vertebrae. The prevalence of vertebral fractures was reported to be highest in Th11-L1 lesions10. To evaluate the intra-observer variability, 100 randomly selected MRIs of the entire spine were rescored by the same observer (MT) more than 1 month after the first reading. Furthermore, to evaluate inter-observer variability, 100 other MRIs were scored by two experienced orthopedic surgeons (MT and RK) using the same SQ method. Intra- and inter-observer variabilities for vertebral fractures, evaluated using kappa analysis, were 0.87 and 0.84, respectively, and were deemed sufficient for assessment.
Evaluation of osteoporosis
Osteoporosis was defined as BMD < 70% of the peak bone mass, according to the criteria of the Japanese Society for Bone and Mineral Research61. BMD at the femoral neck < 0.604 g/cm2 in men and < 0.551 g/cm2 in women indicated osteoporosis and was analyzed accordingly. In this study, femoral neck osteoporosis was used to assess the incidence of osteoporosis.
Physical performance tests
Several tests were performed to evaluate physical performance, as previously reported55,56. In this study, the following four items were selected: OLS, CST, maximum walking speed, and maximum step length. The OLS for each leg was measured using a stopwatch (upper limit, 60 s), and the mean time for both legs was used for further analysis. OLS appears to be a significant and easy-to-administer predictor of injurious falls reported by a previous study62; therefore, the present study adopted it. The time taken for five consecutive chair rises without the use of hands was recorded. CST is a specific test used in assessing functional capacity, particularly focusing on lower limb strength and endurance. This test is commonly employed in populations such as older individuals to evaluate their functional abilities63,64. Walking speed was measured by recording the time taken to walk 6 m at the usual pace in a hallway. Similarly, the 6-m walking time at the maximal pace was measured. The participants were provided with a full explanation of each test but were not provided with any training. Walking speed and step length are effective indicators of physical performance, providing valuable information across various contexts. In older individuals, both are associated with fall risk and survival65,66. In this current study, we evaluated their maximum values. Finally, these four physical tests were effective for the evaluation of physical performance indicators of the locomotive syndrome, respectively67.
Statistical analyses
Five image evaluation parameters (cervical cord compression, rLSS, LDD, vertebral fractures, and osteoporosis) were analyzed. Six clinical conditions and parameters, namely low back pain, ODI, and four physical performance tests (OLS, CST, maximum walking speed, and maximum step length), were also evaluated. Baseline characteristics between the sexes were compared using a non-paired Student’s t-test for numerical variables. Multiple logistic regression analysis was used to estimate the association between clinical conditions (low back pain, ODI, OLS, CST, maximum walking speed, and maximum step length) and image evaluation parameters (cervical cord compression, rLSS, LDD, vertebral fractures, and osteoporosis), after adjusting for age, sex, and BMI (kg/m2). Clinical conditions were used as objective variables, whereas image evaluation parameters were used as explanatory variables. All statistical tests were performed at a two-sided significance level of 0.05. Data were analyzed using JMP version 14 (SAS Institute Japan, Tokyo, Japan).
Data availability
All data generated or analyzed during this study are available from the corresponding author upon reasonable request.
References
Lutz, W., Warren, S. & Sergei, S. The coming acceleration of global population ageing. Nature 451, 716–719 (2008).
Christensen, K., Doblhammer, G., Rau, R. & Vaupel, J. W. Ageing populations: The challenges ahead. Lancet 374, 1196–1208 (2009).
Vos, T. et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 380, 2163–2196 (2012).
Woolf, A. D. & Pfleger, B. Burden of major musculoskeletal conditions. Bull. World Health Organ. 81, 646–656 (2003).
Nakamura, K. A “super-aged” society and the “locomotive syndrome”. J. Orthop. Sci. 13, 1–2 (2008).
Marengoni, A. et al. Aging with multimorbidity: A systematic review of the literature. Ageing Res. Rev. 10, 430–439 (2011).
Briggs, A. M. et al. Musculoskeletal health conditions represent a global threat to healthy aging: A report for the 2015 World Health Organization world report on ageing and health. Gerontologist 56, 243–255 (2016).
Lewis, R. et al. Strategies for optimising musculoskeletal health in the 21st century. BMC Musculoskelet. Disord. 20, 164 (2019).
Teraguchi, M. et al. Association between modic changes, disc degeneration, and pelvic incidence–lumbar lordosis mismatch in a large population based cohort: the Wakayama spine study. Eur. Spine J. https://doi.org/10.1007/s00586-023-07702-8 (2023).
Horii, C. et al. Differences in prevalence and associated factors between mild and severe vertebral fractures in Japanese men and women: The third survey of the ROAD study. J. Bone Miner. Metab. 37, 844–853 (2019).
Tosteson, A. N. et al. Impact of hip and vertebral fractures on quality-adjusted life years. Osteoporos. Int. 12, 1042–1049 (2001).
Cockerill, W. et al. Health-related quality of life and radiographic vertebral fracture. Osteoporos. Int. 15, 113–119 (2004).
Katzman, W. B., Vittinghoff, E., Ensrud, K., Black, D. M. & Kado, D. M. Increasing kyphosis predicts worsening mobility in older community-dwelling women: A prospective cohort study. J. Am. Geriatr. Soc. 59, 96–100 (2011).
Al-Sari, U. A., Tobias, J. & Clark, E. Health-related quality of life in older people with osteoporotic vertebral fractures: A systematic review and meta-analysis. Osteoporos. Int. 27, 2891–2900 (2016).
Cooper, C. Epidemiology of osteoporosis. Osteoporos. Int. 9, S2–S8 (1999).
Yoshimura, N. et al. Prevalence of vertebral fractures in a rural Japanese population. J. Epidemiol. 5, 171–175 (1995).
Martinelli, T. A. & Wiesel, S. W. Epidemiology of spinal stenosis. Instr. Course Lect. 41, 179–181 (1992).
Irvine, D. H., Foster, J. B., Newell, D. J. & Klukvin, B. N. Prevalence of cervical spondylosis in a general practice. Lancet 1, 1089–1092 (1965).
Battié, M. C., Videman, T. & Parent, E. Lumbar disc degeneration: Epidemiology and genetic influences. Spine 29, 2679–2690 (2004).
Yoshimura, M. Analgesic mechanism of calcitonin. J. Bone Miner. Metab. 18, 230–233 (2000).
Ito, A. et al. Mechanisms for ovariectomy-induced hyperalgesia and its relief by calcitonin: Participation of 5-HT1A-like receptor on C-afferent terminals in substantia gelatinosa of the rat spinal cord. J. Neurosci. 20, 6302–6308 (2000).
Nagae, M. et al. Osteoclasts play a part in pain due to the inflammation adjacent to bone. Bone 39, 1107–1115 (2006).
Orita, S. et al. The effects of risedronate and exercise on osteoporotic lumbar rat vertebrae and their sensory innervation. Spine 35, 1974–1982 (2010).
Ohtori, S. et al. Risedronate decreases bone resorption and improves low back pain in postmenopausal osteoporosis patients without vertebral fractures. J. Clin. Neurosci. 17, 209–213 (2010).
Glassman, S. D. et al. The impact of positive sagittal balance in adult spinal deformity. Spine 30, 2024–2029 (2005).
Schwab, F. et al. Scoliosis Research Society—Schwab adult spinal deformity classification: A validation study. Spine 37, 1077–1082 (2012).
Matsuyama, Y. Surgical treatment for adult spinal deformity: Conceptual approach and surgical strategy. Spine Surg. Relat. Res. 1, 56–60 (2017).
Iwata, A. et al. Is bone nonunion, vertebral deformity, or spinopelvic malalignment the best therapeutic target for amelioration of low back pain after osteoporotic vertebral fracture?. Spine 45, E760–E767 (2020).
Stanghelle, B., Bentzen, H., Giangregorio, L., Pripp, A. H. & Bergland, A. Associations between health-related quality of life, physical function and pain in older women with osteoporosis and vertebral fracture. BMC Geriatr. 19, 298 (2019).
Kelsey, J. L. & White, A. A. Epidemiology and impact of low-back pain. Spine 5, 133–142 (1980).
Luoma, K. et al. Low back pain in relation to lumbar disc degeneration. Spine 25, 487–492 (2000).
Hartvigsen, J. et al. What low back pain is and why we need to pay attention. Lancet 391, 2356–2367 (2018).
Yau, M. S. et al. Heritability of thoracic spine curvature and genetic correlations with other spine traits: The Framingham study. J. Bone. Miner. Res. 31, 2077–2084 (2016).
Tanishima, S., Hagino, H., Matsumoto, H., Tanimura, C. & Nagashima, H. Relationship among osteoporosis, sarcopenia, locomotive syndrome, and spinal kyphosis in older individuals living in a local mountain area. Asian Spine J. 17, 1074–1081 (2023).
Asai, Y. et al. Sagittal spino-pelvic alignment in adults: The Wakayama spine study. PLOS One 12, e0178697 (2017).
Asai, Y. et al. Relationship between age-related spinopelvic sagittal alignment and low back pain in adults of population-based cohorts: The ROAD study. J. Pain Res. 15, 33–38 (2022).
Lindsay, R. et al. Risk of new vertebral fracture in the year following a fracture. JAMA 285, 320–323 (2001).
Katzman, W. B. et al. Thoracic kyphosis and rate of incident vertebral fractures: The fracture intervention trial. Osteoporos. Int. 27, 899–903 (2016).
Ensrud, K. E. et al. Prevalent vertebral deformities predict mortality and hospitalization in older women with low bone mass. Fracture intervention trial research group. J. Am. Geriatr. Soc. 48, 241–249 (2000).
Van Staa, T. P., Dennison, E. M., Leufkens, H. G. M. & Cooper, C. Epidemiology of fractures in England and Wales. Bone 29, 517–522 (2001).
Sinaki, M., Brey, R. H., Hughes, C. A., Larson, D. R. & Kaufman, K. R. Balance disorder and increased risk of falls in osteoporosis and kyphosis: Significance of kyphotic posture and muscle strength. Osteoporos. Int. 16, 1004–1010 (2005).
Ministry of Health, Labour and Welfare. The Report of National Health and Nutrition Survey http://www.mhlw.go.jp/bunya/kenkou/eiyou07/01.html.
Muraki, S. et al. Prevalence of radiographic lumbar spondylosis and its association with low back pain in elderly subjects of population-based cohorts: The ROAD study. Ann. Rheum. Dis. 68, 1401–1406 (2009).
Muraki, S. et al. Prevalence of radiographic knee osteoarthritis and its association with knee pain in the elderly of Japanese population-based cohorts: The ROAD study. Osteoarthr. Cartil. 17, 1137–1143 (2009).
Yoshimura, N. et al. Prevalence of knee osteoarthritis, lumbar spondylosis, and osteoporosis in Japanese men and women: The research on osteoarthritis/osteoporosis against disability study. J. Bone Miner. Metab. 27, 620–628 (2009).
Yoshimura, N. et al. Cohort profile: Research on osteoarthritis/osteoporosis against disability study. Int. J. Epidemiol. 39, 988–995 (2010).
Dionne, C. E. et al. A consensus approach toward the standardization of back pain definitions for use in prevalence studies. Spine 33, 95–103 (2008).
Muraki, S. et al. Impact of knee and low back pain on health-related quality of life in Japanese women: The research on osteoarthritis against disability (ROAD). Mod. Rheumatol. 20, 444–451 (2010).
Muraki, S. et al. Health-related quality of life in subjects with low back pain and knee pain in a population-based cohort study of Japanese men: The research on osteoarthritis against disability study. Spine 36, 1312–1319 (2011).
Muraki, S. et al. Incidence and risk factors for radiographic lumbar spondylosis and lower back pain in Japanese men and women: The ROAD study. Osteoarthr. Cartil. 20, 712–718 (2012).
Shirado, O. et al. Formulation of Japanese Orthopaedic Association (JOA) clinical practice guideline for the management of low back pain—The revised 2019 edition. J. Orthop. Sci. 27, 3–30 (2022).
Fairbank, J. C., Couper, J., Davies, J. B. & O’Brien, J. P. The Oswestry low back pain disability questionnaire. Physiotherapy 66, 271–273 (1980).
Fairbank, J. C. T. & Pynsent, P. B. The Oswestry disability index. Spine 25, 2940–2952 (2000).
Tonosu, J. et al. The normative score and the cut-off value of the Oswestry disability index (ODI). Eur. Spine J. 21, 1596–1602 (2012).
Nagata, K. et al. Prevalence of cervical cord compression and its association with physical performance in a population-based cohort in Japan: The Wakayama spine study. Spine 37, 1892–1898 (2012).
Ishimoto, Y. et al. Associations between radiographic lumbar spinal stenosis and clinical symptoms in the general population: The Wakayama Spine Study. Osteoarthr. Cartilage 21, 783–788 (2013).
Suri, P., Rainville, J., Kalichman, L. & Katz, J. N. Does this older adult with lower extremity pain have the clinical syndrome of lumbar spinal stenosis?. JAMA 304, 2628–2636 (2010).
Pfirrmann, C. W., Metzdorf, A., Zanetti, M., Hodler, J. & Boos, N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine 26, 1873–1878 (2001).
Teraguchi, M. et al. The association of combination of disc degeneration, end plate signal change, and Schmorl node with low back pain in a large population study: The Wakayama Spine Study. Spine J. 15, 622–628 (2015).
Genant, H. K., Wu, C. Y., van Kuijk, C. & Nevitt, M. C. Vertebral fracture assessment using a semiquantitative technique. J. Bone Miner. Res. 8, 1137–1148 (1993).
Orimo, H. et al. Diagnostic criteria for primary osteoporosis: Year 2000 revision. J. Bone Miner. Metab. 19, 331–337 (2001).
Vellas, B. J. et al. One-leg balance is an important predictor of injurious falls in older persons. J. Am. Geriatr. Soc. 45, 735–738 (1997).
Bohannon, R. W., Shove, M. E., Barreca, S. R., Masters, L. M. & Sigouin, C. S. Five-repetition sit-to-stand test performance by community-dwelling adults: A preliminary investigation of times, determinants, and relationship with self-reported physical performance. Isokine. Exerc. Sci. 15, 77–81 (2007).
Buatois, S. et al. Five times sit to stand test is a predictor of recurrent falls in healthy community-living subjects aged 65 and older. J. Am. Geriatr. Soc. 56, 1575–1577 (2008).
Verghese, J., Holtzer, R. & Lipton, R. B. Quantitative gait markers and incident fall risk in older adults. J. Gerontol. A Biol. Sci. Med. Sci. 64, 896–901 (2009).
Studenski, S. et al. Gait speed and survival in older adults. JAMA 305, 50–58 (2011).
Yoshimura, N. et al. Association between new indices in the locomotive syndrome risk test and decline in mobility: Third survey of the ROAD study. J. Orthop. Sci. 20, 896–905 (2015).
Acknowledgements
The authors thank Mrs. Tamako Tsutsumi, Mrs. Kanami Maeda, and other members of the Public Office in Taiji Town for their assistance with the ___location and scheduling of the examinations.
Funding
This study was funded by H-25-Choujyu-007 (Director, Noriko Yoshimura), H25-Nanchitou (Men)-005 (Director, Sakae Tanaka), 201417014A (Director, Noriko Yoshimura), and 21FA1006 (Director, Hiroshi Yamada) from the Ministry of Health, Labour and Welfare; a Grant-in-Aid for Scientific Research (B26293139 and B23390172 to Noriko Yoshimura, B2629333, C26462249 and 21K0936 to Hiroshi Hashizume, and C25462305 to Hiroshi Yamada); a Grant-in-Aid for Young Researchers (B25860448 to Yuyu Ishimoto, B26861286 to Masatoshi Teraguchi, B26860419 to Ryohei Kagotani, and B15K20013 to Hiroki Iwahashi); and a Grant-in-Aid for Challenging Exploratory Research (15K15219 to Noriko Yoshimura and 24659666 to Hiroyuki Oka) from the JSPS KAKENHI grant and Collaborating Research with NSF 08033011- 00262 (Director, Noriko Yoshimura) from the Ministry of Education, Culture, Sports, Science, and Technology in Japan. This study was also supported by grants from the Japan Osteoporosis Society (Noriko Yoshimura and Hiroyuki Oka) and JA Kyosai Research Institute (Hiroyuki Oka). The study sponsors played no role in the study design, collection, analysis, and interpretation of data, writing of the report, or decision to submit the manuscript for publication. The corresponding author had full access to all data and made the final decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
H.H., N.Y., H.O., S.T., M.Y., and H.Y. conceived and designed this study. S.I. wrote the manuscript. H.H., N.Y., H.O., H.I., Y.I., K.N., M.T., R.K., and T.S. collected the data. S.I., H.H., H.O., and N.Y. analyzed the data. All authors have seen the original study data, reviewed the data analysis, and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Iwata, S., Hashizume, H., Yoshimura, N. et al. Osteoporosis, spinal degenerative disorders, and their association with low back pain, activities of daily living, and physical performance in a general population. Sci Rep 14, 15860 (2024). https://doi.org/10.1038/s41598-024-64706-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-64706-0
Keywords
This article is cited by
-
Osteoporosis in adjacent cervical segments exacerbates disc herniation
Scientific Reports (2025)
-
Activities of daily living limitations in relation to the presence of pain in community-dwelling older adults
Scientific Reports (2025)
-
Age-threshold for increased risk of developing back disorders: prospective cohort with 74 000 individuals from the UK Biobank
European Spine Journal (2025)
-
Design and radiological confirmation of three-column cortical bone trajectory in the lower thoracic vertebrae
European Spine Journal (2025)
-
A quantitative review of finite element-based biomechanics of lumbar decompression surgery
Biomechanics and Modeling in Mechanobiology (2025)