Abstract
SHP-1, a nonreceptor protein tyrosine phosphatase encoded by ptpn6, has been regarded as a regulatory protein of hematopoietic cell biology for years. However, there is now increasing evidence to support its role in tumors. Thus, the role of ptpn6 for prognosis and immune regulation across 33 tumors was investigated, aiming to explore its functional heterogeneity and clinical significance in pan-cancer. Differential expression of ptpn6 was found between cancer and adjacent normal tissues, and its expression was significantly correlated with the prognosis of tumor patients. In most cancers, ptpn6 expression was significantly associated with immune infiltration. This was further confirmed by ptpn6-related genes/proteins enrichment analysis. Additionally, genetic alterations in ptpn6 was observed in most cancers. As for epigenetic changes, it’s phosphorylation levels significantly altered in 6 tumors, while methylation levels significantly altered in 12 tumors. Notably, the methylation levels of ptpn6 were significantly decreased in 11 tumors, accompanied by its increased expression in 8 of them, suggesting that the hypomethylation may be related to its increased expression. Our results show that ptpn6 plays a specific role in tumor immunity and exerts a pleiotropic effect in a variety of tumors. It can serve as a prognostic factor for some cancers. Especially in LGG, KIRC, UCS and TGCT, the increased expression of ptpn6 is associated with poor prognosis and high immune infiltration. This aids in understanding the role of ptpn6 in tumor biology, and can provide insight into presenting a potential biomarker for poor prognosis and immune infiltration in cancers.
Similar content being viewed by others
Introduction
Cancer has been a leading cause of death and a significant obstacle affecting the quality of life for decades worldwide1. In recent years, advances in genomic methods have expanded our knowledge about gene expression, genetic, and epigenetic alterations at the pan-genomic level in various malignancies, thus accelerating the discovery of new tumor biomarkers and therapeutic targets2,3.
Protein phosphatases are key regulators that control the intracellular phosphorylation required for cellular homeostasis and have received great attention in recent years as the important potential therapeutic targets for cancers and other diseases4,5. Among those, the SH2 ___domain containing protein tyrosine phosphatase (PTP), SHP-1, is a cytosolic protein tyrosine phosphatase with 595-amino acid residue encoded by ptpn6, which has been shown to be involved in the regulation of hematopoietic cell biology6,7,8,9. Recently, accumulating evidence has suggested that SHP-1 also has an impact on the occurrence and development of tumors. Its coding gene, ptpn6, has been reported to be overexpressed in ovarian cancer and breast cancer in previous studies10,11,12. In contrast, its expression has been shown to be diminished or abolished in T-cell lymphomas, leukemias13,14,15, hepatocellular carcinoma (HCC)16 and some colorectal cancers17,18. Furthermore, ptpn6 has also been proven to be associated with tumor microenvironment (TME)19,20,21,22, which plays critical roles in tumor development involving the interaction between cancer cells, tumor infiltrating immune cells, and their supporting cells. In addition, tumor therapeutic drugs targeting SHP-1( such as several SHP-1 inhibitors) have been developed, however, results were disappointing23, indicating that the role of SHP-1 in tumor biology, especially in different TME, needs to be further clarified.
Taken together, increasing evidence suggests that SHP-1/ptpn6 is possibly an immuno-raleted factor in the TME, and may play roles in regulating tumor signal transduction. Nevertheless, most studies on the role of ptpn6 in tumors to date have been limited to a specific type of cancer. Our study carried out a pan-cancer analysis of ptpn6 based on multiple databases to explore the heterogeneity of ptpn6 in different cancers. We explored the expression, prognostic value, immune correlation, genetic alteration, epigenetic alteration, relevant cellular pathway and function of ptpn6 to reveal the potential molecular pathogenesis across 33 types of cancer, which helps in comprehending the role of ptpn6 in tumorigenesis and tumor progression from multiple perspectives.
Materials and methods
Differential expression analysis
The Tumor Immune Estimation Resource (TIMER) 2.0 (http://timer.cistrome.org/) is an online website used to investigate the gene expression, gene correlation and immune infiltration in tumors24. Difference of ptpn6 expression between tumors and adjacent normal tissues can be obtained through the “Gene_DE” module of TIMER2. The results were validated using Gene Expression Profiling Interactive Analysis 2 (GEPIA2) database (http://gepia2.cancer-pku.cn/). The expression of ptpn6 in different pathological stages of cancers was also obtained by GEPIA225.
Survival prognosis analysis
The heatmaps of overall survival (OS) and disease-free survival (DFS) of ptpn6 in all TCGA tumors were acquired through GEPIA2. The corresponding survival plots with their 95% confidence interval, p value and hazard ratio (HR) can be obtained by the Kaplan-Meier plotter database (https://kmplot.com/analysis/)26. To evaluate the expression of ptpn6 in predicting the prognosis of cancer patients, ROC analysis was conducted using the pROC package in R language (version 4.2.2).
Immune infiltration analysis
The correlation between ptpn6 expression and immune infiltration in pan-cancer was investigated using TIMER (https://cistrome.shinyapps.io/timer/)27. The tumor purity, B cells, CD8 + T cells, CD4 + T cells, macrophages, neutrophils and dendritic cells were selected. The results were visualized as scatter plots. Heatmaps and scatter plots of the correlation between ptpn6 expression and cancer associated fibroblasts (CAFs) were generated through TIMER228.
Enrichment analysis
Enrichment analysis helps to discover novel biological functions, genotype- phenotype relationships and disease mechanisms. Experimentally determined SHP-1-binding proteins can be obtained through the STRING database (https://string-db.org/), by the following parameters: minimum required interaction score[low confidence (0.150)], meaning of network edges (evidence), maximum number of interactors to show (no more than 50 interactors in 1st shell), and active interaction sources (experiments)29. The top 100 ptpn6-related genes, were obtained by GEPIA2 and the top five genes were selected to draw the correlation scatter plot with ptpn6. The heat map between the selected genes and different types of tumors can be acquired through TIMER2. In addition, the intersection analysis of SHP-1-binding proteins and ptpn6-related genes was conducted using Jvenn (https://bioinformatics.psb.ugent.be/webtools/Venn/)30. These two sets of data were also combined for Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway analysis31,32,33 and Gene Ontology (GO) analysis. The functional annotation data were obtained through the Database for Annotation, Visualization, and Integrated Discovery (DAVID, https://david.ncifcrf.gov/), and enriched pathways were visualized via bioinformatic (https://www.bioinformatics.com.cn/).
Relevance of ptpn6 across 14 functional states in distinct cancers
Single-cell RNA sequencing (scRNA-seq) can help researchers understand the functional specificity of cancer cells. CancerSEA (http://biocc.hrbmu.edu.cn/CancerSEA/) is a database for functional states of cancer cells at single-cell level, including angiogenesis, apoptosis, cell cycle, differentiation, DNA damage, DNA repair, EMT, hypoxia, inflammation, invasion, metastasis, proliferation, quiescence, and stemness34. The functional states of ptpn6 in multiple cancers were explored using CancerSEA. Correlations between ptpn6 expression and functional states in different single-cell datasets were filtered by the correlation strength > 0.3 and the p value < 0.05.
Genetic alteration analysis
The cBioPortal (http://www.cbioportal.org), a comprehensive database of cancer genomics datasets35, is applied to the analysis of ptpn6 genetic alteration. We explored the copy number alteration (CNA) and mutation status of ptpn6 across all TCGA tumors using cBioPortal. The results of the alteration frequency, mutation type and CNA in various cancers were derived from the ‘Cancer Types Summary’ module. The OS, DFS, progression free survival (PFS), and disease free survival (DSS) of patients with ptpn6 genetic altered were also obtained from cBioPortal.
Analysis of the methylation and phosphorylation of ptpn6
UALCAN performed protein expression analysis from the clinical proteomic tumor analysis consortium (CPTAC) dataset and the International Cancer Proteogenome Consortium (ICPC) datasets36. The methylation and phosphorylation levels of ptpn6 between different cancers and normal tissues was investigated by UALCAN database (http://ualcan.path.uab.edu/analysis.html).
Immunohistochemistry (IHC) staining
Human Protein Atlas (HPA) (https://www.proteinatlas.org/) is a database of proteins in human organs, tissues and cells based on multiple omics approaches37,38. To analyze the differential expression of ptpn6 at the protein level, the expression of ptpn6 proteins (SHP-1) in tumor tissues and their corresponding normal tissues was downloaded from HPA and analyzed. Furthermore, the IHC images of some typical immune markers were also acquired from HPA.
Statistical analysis
Alterations in ptpn6 expression levels in cancer and normal tissues were estimated using two sets of t-tests. The Kaplan-Meier curve and Cox regression model were used for survival analyses in this study. The Hazard Ratio was calculated by the Cox regression model. The correlation expression analysis between the two variables was analyzed using Spearman’s or Pearson’s test. P-value < 0.05 was considered statistically significant.
Results
The expression of ptpn6 and its correlation with cancer stage in pan-cancer
To determine differences in ptpn6 expression between tumor and normal tissues, the ptpn6 mRNA levels in different tumors and normal tissues were analyzed using the TIMER2 (http://timer.cistrome.org/) and GEPIA2 database (http://gepia.cancer-pku.cn/).
Among the 33 types of tumors shown in TIMER2 database, the ptpn6 expression was significantly increased in bladder urothelial carcinoma (BLCA), breast invasive carcinoma (BRCA), cervical squamous cell carcinoma and endocervical adenocarcinoma (CESC), cholangio carcinoma (CHOL), esophageal carcinoma (ESCA), glioblastoma multiforme (GBM), head and neck squamous cell carcinoma (HNSC), kidney renal clear cell carcinoma (KIRC), kidney renal papillary cell carcinoma (KIRP), liver hepatocellular carcinoma (LIHC), stomach adenocarcinoma (STAD), thyroid carcinoma (THCA), and uterine corpus endometrial carcinoma (UCEC), compared to the adjacent normal tissues (Fig. 1A). In addition, significantly lower expression was observed in colon adenocarcinoma (COAD), kidney chromophobe (KICH), lung adenocarcinoma (LUAD), pancreatic adenocarcinoma (PAAD), skin cutaneous melanoma (SKCM) and lung squamous cell carcinoma (LUSC) (Fig. 1A).
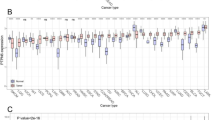
To further evaluate ptpn6 expression in human cancers, we also examined ptpn6 expression using the RNA-seq data from multiple malignancies in GEPIA2 database. Except for the differential expression between the tumor and adjacent normal tissues for ptpn6 in TIMER2 database mentioned above, ptpn6 expression was also significantly higher in acute myeloid leukemia (LAML), brain lower grade glioma (LGG), ovarian serous cystadenocarcinoma (OV), rectum adenocarcinoma (READ), testicular germ cell tumors (TGCT), and uterine carcinosarcoma (UCS) than that in paired normal tissues (Fig. 1B).
Furthermore, we performed IHC analysis of ptpn6 expression in cancer tissues and corresponding normal tissues from the HPA website. Representative IHC images revealed that ptpn6 was highly expressed in breast cancer, cervical cancer, glioma, testis cancer, liver cancer, stomach cancer, endometrial cancer, ovarian cancer and colorectal cancer tissues compared to their corresponding nontumorous tissue, and that its subcellular localization was in the nucleoplasm and cytoplasm (Fig. 1C).
The expression levels of ptpn6 in different types of human cancers. (A) Increased or decreased ptpn6 in datasets of different cancers compared with adjacent normal tissues in TIMER2 database. (B) The ptpn6 expression profile across all tumor samples and paired normal tissues from GEPIA2 database. Each dot represents the expression of the sample. The red box represents the primary tumor and the blue represents normal tissue. *p < 0. 05, **p < 0. 01, ***p < 0. 001. (C) The expression of ptpn6 proteins in cancer tissues and corresponding normal tissues by HPA database.
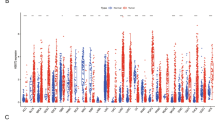
In view of the differential expression of ptpn6 between tumor and paired normal tissues in pan-cancer, we investigated the correlations between ptpn6 expression and cancer stage. Through the one-way ANOVA analysis of 33 tumors, we found that the expression of ptpn6 in BLCA, ESCA, HNSC, KIRC, LUAD, SKCM, STAD and UCS was significantly positively correlated with different tumor stages (Fig. 2, p < 0.05). We also found that ptpn6 expression was higher in stage III and IV compared with stage I and II in KIRC, and vice versa in LUAD, indicating that ptpn6 might play a complex role in tumor development. However, no significant correlations were observed between ptpn6 expression and tumor stage in the other 25 tumors.
The significant correlations were observed between the ptpn6 expression and the main pathological stages. The significance threshold was set as p < 0.05. The distribution of the data was given, with the white dots representing the median, and the black cylinder representing the most concentrated middle 50% of the data (i.e., 25–75% quantile). The larger the “profile” is, the more concentrated the data will be, and vice versa.
Prognostic potential of ptpn6 in cancers
To explore whether ptpn6 expression was related to the survival indicators of cancer patients, overall survival (OS) and disease free survival (DFS) analyses were performed. The cancer patients were divided into high-ptpn6-expression and low-ptpn6-expression groups, and the association of ptpn6 expression with the patient prognosis in multiple cancers was explored via Kaplan-Meier plotter database and GEPIA2 database. Cox regression analysis of the results from 33 types of cancer suggested that the ptpn6 expression significantly correlated with OS in 13 types of cancer, including BLCA, BRCA, CESC, KIRC, KIRP, LUAD, PAAD, READ, SARC, STAD, TGCT, THYM and UCEC ( Figure S1, all P < 0.05 ). The results from GEPIA2 datasets showed that high ptpn6 expression levels were associated with poor prognosis in KIRC (p = 0.0056), LGG (p = 0.001), UCS (p = 0.014) and UVM (p = 0.0023) (Fig. 3A-E). We also analyzed the prognostic values of ptpn6 in pan-cancer using Kaplan-Meier database, and found that high expression of ptpn6 were significantly correlated with the shortened OS of TGCT (p = 0.026) and READ patients (p = 0.034) (Fig. 3F-G). These results suggested that the ptpn6 expression had an impact on the prognosis in KIRC, LGG, UCS, UVM, TGCT and READ. Therefore, it is conceivable that high ptpn6 expression is an independent risk factor leading to poor prognosis of these 6 types, which we will focus on in the following studies.
Meanwhile, high ptpn6 expression was correlated with good prognosis in BLCA, PAAD, sarcoma (SARC), SKCM, STAD, BRCA, CESC, KIRP, LUAD, thymoma (THYM) and UCEC from GEPIA2 and Kaplan-Meier plotter database (Fig. 3A, S1-2, all P < 0.05), suggesting the complexity of the correlation between ptpn6 expression and prognosis of different tumor types.
The relationship between ptpn6 expression levels and OS/DFS in various cancer types through GEPIA2 and Kaplan-Meier. A hazard ratio (HR) greater than 1, which means the risk of death is higher in the high ptpn6 expression cohort than in the low ptpn6 expression cohort, is shown in red. And the reverse is shown in blue. The significant threshold was set as p < 0.05. (A) Correlation between ptpn6 expression and survival prognosis in 33 cancer types. The survival plots with positive results were given in GEPIA2, with borders indicating statistically significant results. The darker the color is, the further away the HR is from 1. (B–G) The correlation between high ptpn6 expression and prognosis of different tumor types were explored by GEPIA2 (B–E) and Kaplan-Meier (F,G) database.
Ptpn6 expression is correlated with immune infiltration in most types of cancer
A growing body of evidence suggests that tumor progression and prognosis are closely related to the TME. During tumor progression, a variety of immune cells are recruited into the microenvironment surrounding the tumor cells, infiltrate into the tumor and become tumor immune infiltration20,39,40. In addition, tumor purity is an important factor influencing the analysis of immune infiltration in clinical tumor samples by genomic approaches41, and low tumor purity is an independent risk factor for poor prognosis in some cancer types42,43. To investigate the relationship between ptpn6 expression and tumor immune infiltration, we assessed the correlations between ptpn6 expression and immune infiltration levels in 32 cancer types from TIMER. The results showed that ptpn6 expression was significantly correlated with tumor purity in 21 types of cancer (Table S1). In addition, ptpn6 expression was significantly correlated with infiltrating levels of B cell in 27 types of cancers, CD8 + T cells in 19 types of cancer, CD4 + T cells in 26 types of cancer, macrophages in 21 types of cancer, neutrophils in 23 types of cancer, and dendritic cells in 29 types of cancer (Table S1).
Notably, among the 6 cancers previously screened for which high ptpn6 expression was associated with poor prognosis, ptpn6 expression was significantly negatively related to tumor purity in 4 of them, including KIRC, LGG, TGCT and UCS (Fig. 4). In addition, ptpn6 expression had significant positive correlations with infiltrating levels of B cells, CD8 + T cells, CD4 + T cells, macrophages, neutrophils, and dendritic cells in KIRC and LGG (Fig. 4A-B). In terms of TGCT and UCS, it also had significant positive correlations with infiltrating levels of most types of cells, but no significant correlation with infiltrating level of CD8 + T cells and macrophages in TGCT, CD4 + T cells and macrophages in UCS (Fig. 4C-D). Ptpn6 expression was positively correlated with infiltrating levels of CD4 + T cells and Dendritic cells in READ, B cells in UVM (Table S1). These results showed that ptpn6 expression was correlated with immune infiltration in most types of cancer, and its high expression was correlated with poor prognosis and high immune infiltration in KIRC, LGG, TGCT, and UCS. All these revealed the specific role of ptpn6 in regulating immune infiltration and its aberrant expression may alter TME, directly or indirectly, thereby affecting tumor prognosis.
Correlation of ptpn6 expression with immune infiltration levels in KIRC, LGG, TGCT, and UCS. (A,B) Ptpn6 expression was significantly negatively correlated with tumor purity and positively correlated with infiltrating levels of B cells, CD8 + T cells, CD4 + T cells, macrophages, neutrophils, and dendritic cells in KIRC and LGG. (C) Ptpn6 expression had significant negative correlations with tumor purity and positive correlations with infiltrating levels of B cells, CD4 + T cells, macrophages, neutrophils, and dendritic cells in TGCT, except for CD8 + T cells and macrophages. (D) Ptpn6 expression was significantly negatively correlated with tumor purity, and positively correlated with infiltrating levels of B cells, CD8 + T cells, macrophages, neutrophils, and dendritic cells in UCS, but not significantly correlated with infiltrating level of CD4 + T cells and macrophages.
Enrichment analysis of ptpn6-related genes/proteins
The enrichment analysis of ptpn6-related genes and SHP-1 binding proteins was conducted to study the biological functions of ptpn6 in tumors, so as to further reveal its molecular mechanism in tumorigenesis and tumor progression. A batch of SHP-1-binding proteins supported by experimental evidence and ptpn6 expression-related genes were obtained by the STRING and GEPIA2 databases, respectively, from which the top 50 SHP-1-binding proteins (Fig. 5A) and the top 100 highest positively correlated genes with ptpn6 (hereinafter named as ptpn6-related genes) were selected for further study as described in previous studies44.
The interaction network of 50 SHP-1-binding proteins showed that many of them were involved in immune function and cancer signal transduction, such as IL4R, JAK1, CD33 (Fig. 5A). And most ptpn6-related genes were related to tumorigenesis, infiltration and immune regulation, including ARHGAP30, ARHGAP9, CORO1A, RAC2, FERMT3, VAV1, RASAL3, etc. According to the correlation coefficient (R), the top 5 genes were WAS (R = 0.76), ARHGAP30 (R = 0.75), ARHGAP9 (R = 0.74), CORO1A (R = 0.74) and RAC2 (R = 0.74) (Fig. 5B). Furthermore, the correlation scatter plots and corresponding heatmaps were generated between the five genes and ptpn6 in 33 cancers, respectively, and it indicated that ptpn6 was positively correlated with these five genes in the majority of cancer types (Fig. 5B-C). In addition, an intersection analysis of SHP-1-binding proteins and ptpn6-related genes was also conducted and two common members LCP2 and LAIR1 were found.
To further investigate the molecular mechanisms of ptpn6 in tumors, the ptpn6-related genes and SHP-1-binding proteins were combined for KEGG analysis and GO analysis. The KEGG results suggested that ptpn6 was closely related to several important cancer and immune related processes, such as JAK-STAT signaling pathway, PI3K-AKT signaling pathway, natural killer cell mediated cytotoxicity, B cell receptor signaling pathway, and PD-L1 expression and PD-1 checkpoint pathway in cancer (Fig. 5D). GO enrichment analysis revealed that many of these genes were enriched in peptidyl-tyrosine modification, protein autophosphorylation, lymphocyte differentiation, T cell activation and regulation of T cell activation (Fig. 5E).
All these results showed that most of ptpn6-related genes/proteins were involved in the occurrence and development of tumors, as well as the immunity, suggesting the important role of ptpn6 in tumors and their immunity.
The ptpn6-related genes/proteins enrichment analysis. (A) The available experimentally determined SHP-1-binding proteins from the STRING database and their interaction network. (B) The correlation of the expression between ptpn6 and the top five ptpn6-related genes, including WAS, ARHGAP30, ARHGAP9, CORO1A and RAC2 (R = 0.76, 0.75, 0.74, 0.74, 0.74). (C) The corresponding heatmap between these five genes and ptpn6 in the 33 types of cancer. The significant threshold was set as p < 0.05. Red indicates a positive correlation, while blue means the opposite. The darker the color is, the closer the absolute value of the correlation coefficient is to 1, and the higher the correlation is. (D,E) KEGG pathway analysis and GO enrichment analysis for the SHP-1-binding proteins and ptpn6-related genes.
Functional states of ptpn6 across different cancer types
The high functional heterogeneity of cancer cells plays a crucial role in cancer research, which is of great significance to comprehensively explore the different functional states of cancer cells at the single-cell level34. The functional states of ptpn6 were analyzed at single-cell resolution in 14 cancers, including LUAD, non-small cell lung cancer (NSCLC), renal cell carcinoma (RCC), acute lymphoblastic leukemia (ALL), prostate cancer (PC), retinoblastoma (RB), GBM, uveal melanoma (UVM/UM), colorectal cancer (CRC), OV, etc.
We observed that ptpn6 was correlated with multiple functional states in multiple cancers. In UVM/UM, 6 functional states were negatively correlated with the gene ptpn6, including Apoptosis (cor = -0.515), DNA damage (cor = -0.562), DNA repair (cor = -0.647), EMT (cor =-0.389), Invasion (cor = -0.507), and Metastasis (cor = -0.487) (Fig. 6). In GBM, there were 5 functional states, DNA repair (cor = -0.346), EMT (cor =-0.327), Hypoxia (cor =-0.376), Invasion (cor = -0.384), and Metastasis (cor = -0.323), negatively correlated with ptpn6 (Fig. 6). In addition, ptpn6 was negatively with Invasion in OV (cor = -0.387) (Fig. 6). On the other hand, the expression of ptpn6 was positively correlated with Angiogenesis (cor = 0.468), Differentiation (cor = 0.305) and Metastasis (cor = 0.373) in RB, DNA damage in ALL (cor = 0.305), Differentiation in RCC (cor = 0.398), and Apoptosis in PC (cor = 0.452) (Fig. 6). These results suggested that ptpn6 might play an important role by regulating multiple functions in pan-cancer.
Average correlations between ptpn6 and functional states in different cancers. The bar chart shows the number of datasets in which the gene ptpn6 was significantly related to the corresponding state. Correlations between ptpn6 expression and functional states in different single-cell datasets were screened using correlation strength (cor) > 0.3 and the p-value < 0.05. The different colors in the figure represent the positive (red) or negative (blue) correlation of ptpn6 expression and functional states, and the size of the dots represents correlation strength (cor).
The genetic alterations of ptpn6 in pan-cancer
In order to further investigate the molecular mechanism of ptpn6 in tumorigenesis, we used cBioPortal (https://www.cbioportal. org) to evaluate the genetic alteration of ptpn6 in different tumor samples of the TCGA cohorts. The alteration frequency, mutation type and copy number change (CNA) of ptpn6 were analyzed in 10,967 samples of 32 TCGA tumors. Genetic change of ptpn6 was found in 26 tumors, including “mutation”, “amplification”, “deep deletion”, “multiple alterations” and “fusion” (Fig. 7A). Notably, the majority of the investigated cancers exhibited either “amplification” or “mutation” as the predominant form of genetic alteration (Fig. 7A).
Among the 4 types of cancers selected previously, ptpn6 alteration frequency was relatively higher in UCS, TGCT and LGG, and the highest alteration frequency was observed in UCS patients, mainly characterized by “amplification” and “multiple alterations” (Fig. 7A). Similarly, the alteration of ptpn6 gene was mainly manifested as “amplification” in TGCT and LGG patients, and “mutation” in KIRC patients (Fig. 7A). Besides the tumor types described above, diffuse large B cell lymphoma (DLBC) was also found with higher frequency of ptpn6 alterations, with “mutation” as the only alteration type (Fig. 7A).
Subsequently, we investigated the sites and types of ptpn6 “mutation” through cBioPortal Mutations Module, and found that among the 99 “mutation” samples included in this database, the first ranked mutation type was missense mutation, with 83 recorded samples, among which, R554S/C missense mutation was the most frequent (Fig. 7B).
We further investigated the relationship between ptpn6 alteration and prognosis in pan-cancer, and found that tumor patients with genetic alterations in ptpn6 had worse OS (p = 8.571e-3) and DSS (p = 0.0412) than patients without alterations, but no difference in DFS (p = 0.994) and PFS (p = 0.0804) between the two groups (Fig. 7C). These findings suggested that the genetic alteration of ptpn6 might lead to poor clinical prognosis.
The genetic alteration of ptpn6 in different tumors using the cBioPortal database. (A) The alteration frequency and type of ptpn6 in 32 TCGA tumor types. (B) The map of types, sites and case numbers of ptpn6 mutation. (C) The effect of ptpn6 genetic alteration on OS, DSS, DFS and PFS. *p < 0. 05, **p < 0. 01, ***p < 0. 001.
The ptpn6 phosphorylation heterogeneity in pan-cancer
Posttranslational modification (PTM) is a key molecular mechanism of ptpn6 activation45, and phosphorylation is an important one. In previous studies, ptpn6 has been shown to possess the ability to phosphorylate the receptor through its SH2 ___domain, which is also a vital region for phosphorylation of itself46. In order to investigate the relationship between the alterations in ptpn6 phosphorylation and cancer progression, the ptpn6 phosphorylation were analyzed in tumor and normal tissues through UALCAN dataset.
The phosphorylation from UALCAN dataset indicated that significantly altered ptpn6 phosphorylation levels were observed in 6 tumors, including clear cell RCC (CCRCC), LUAD, HNSC, PAAD, colon cancer (CC) and LUSC, and the changes were mainly distributed in three sites, including S10, Y564 and S140 (Fig. 8). Compared with normal tissues, the phosphorylation level of S10 site of ptpn6 was significantly increased in CCRCC, LUAD, HNSC, CC, LUSC and PAAD tumor tissues (Fig. 8, all p < 0.05). In HNSC, the phosphorylation level of ptpn6 increased at Y564 and decreased at S140, but the difference was not significant (Fig. 8).
Phosphorylation analysis of ptpn6 in different tumors from the UALCAN database. The ptpn6 phosphorylation was analyzed between primary tissues of selected tumor and normal tissues, including breast cancer (A), clear cell RCC (B), HNSC (C), hepatocellular carcinoma (D), LUAD (E), PAAD (F), colon cancer (G) and LUSC (H). Z-values represent standard deviations from the median across samples for the given cancer type. The log2 Spectral count ratio values from CPTAC were first normalized within each sample profile, then normalized across samples. The red box indicates primary tumors, and the blue shows normal tissues. *p < 0. 05, **p < 0. 01, ***p < 0. 001.
The promoter methylation heterogeneity of ptpn6 exists in different tumors
DNA methylation is one of the most intensely studied epigenetic modifications affecting occurrence and progression of cancer, and changes in DNA methylation in cancer have been considered as important biomarkers for diagnosis and prognosis45,47. By UALCAN databases, we investigated the promoter methylation of ptpn6 in 32 kinds of tumors, thus to analyze the methylation heterogeneity of ptpn6 in cancer.
We found that the promoter methylation of ptpn6 was significantly different in 12 tumors compared to the corresponding normal tissues. Among them, the significant decrease in the promoter methylation levels of ptpn6 was observed in tissues of 11 tumors, including BLCA, BRCA, CESC, HNSC, KIRC, KIRP, LUAD, LUSC, prostate adenocarcinoma (PRAD), TGCT and UCEC, compared to normal tissues (Fig. 9). As described before, the expression of ptpn6 was significantly increased in 8 of these tumors (BLCA, BRCA, CESC, HNSC, KIRC, KIRP, TGCT and UCEC), than that in normal tissues. It was indicated that hypomethylation of ptpn6 may be related to its increased expression. Among those, as previously mentioned, the increased expression of ptpn6 in KIRC and TGCT is significantly correlated with poor prognosis and high immune infiltration, reflecting the potential associations of ptpn6 promoter methylation, gene expression, and its role in cancer prognosis and immune infiltration.
In addition, in pheochromocytoma and paraganglioma (PCPG), the methylation level of ptpn6 was significantly increased (Fig. 9). No significant differences were observed between COAD, ESCA, CHOL, GBM, LIHC, PAAD, READ, SARC, STAD, THCA and THYM tissues and matched normal tissues (Fig. 9).
The ptpn6 promoter methylation levels in different cancers were obtained from UALCAN. The Beta value indicates level of promotor methylation, ranging from 0 (unmethylated) to 1 (fully methylated). Different beta value cut-off has been considered to indicate hyper-methylation [Beta value: 0.7 − 0.5] or hypo-methylation [Beta-value: 0.3 − 0.25]. The red box indicates primary tumors, while blue box indicates normal tissues. The significant threshold was set as p < 0.05. *p < 0. 05, **p < 0. 01, ***p < 0. 001.
Discussion
Ptpn6 is a signaling molecule that regulates various cellular processes, including cell growth, differentiation, mitotic cycle and oncogenic transformation, and plays an important role in the occurrence and development of cancer16,48,49,50,51. In order to better investigate the heterogeneity of ptpn6 in tumors, we conducted a systematic pan-cancer analysis. Our results offer insight into the prognostic and immunological roles of ptpn6 across different tumors, indicating that ptpn6 exerts a pleiotropic effect on malignancy and it may play roles in many aspects of tumor biology.
Herein, we analyzed the difference in ptpn6 expression in 33 tumors and the normal tissues, and found that ptpn6 expression was significantly different in 25 tumors. Among them, the expression of ptpn6 was significantly higher in 20 tumors, and its high expression was associated with poor prognostic in 6 of them, including KIRC, LGG, UCS, UVM, TGCT and READ, which indicated that ptpn6 may have a cancer-promoting effect in some cancer types. This is consistent with the reports on cancer-promoting effects of ptpn6 in LGG and KIRC52,53. In addition, receiver-operating characteristic (ROC) curves were used to explore the expression of ptpn6 and the prediction of survival prognosis in 5 of those tumors, and it showed that ptpn6 expression had some predictive value for KIRC (AUC = 0.619), LGG (AUC = 0.572), TGCT (AUC = 0.606), and UVM (AUC = 0.617) (Figure S3). These results confirmed the prognostic role of ptpn6, which may be a valuable prognostic biomarker for some specific types of cancer.
TME features serve as markers for evaluating tumor cell responses to immunotherapy and influence clinical outcomes54. More and more studies have suggested that tumor immune infiltrating cells, including but not limited to B cells, T cells, neutrophils, macrophages, dendritic cell (DC), and tumor associated fibroblast (CAF), are closely associated with the tumor progression. Thus, the associations between ptpn6 expression and immune infiltration levels across 33 types of cancer was explored, and the results showed that ptpn6 expression was significantly associated with tumor immune infiltration in most cancers. Especially in LGG, KIRC, UCS and TGCT, the increased expression of ptpn6 was significantly associated with poor prognosis and high immune infiltration. We further carried out IHC analyses of typical immune markers in kidney cancer, testicular cancer, brain glioma and uterine carcinoma through HPA database, and it revealed that compared with the corresponding non-tumor tissues, the immune markers HIF1A, IDH1, AFP and VIM were highly expressed in these four cancer tissues, respectively (Figure S5A). And ptpn6 expression was significantly correlated with the markers HIF1A and IDH1(Figure S5B). All these suggested that ptpn6 plays a specific role in tumor immunity, such as a key regulatory role in the interaction between cancer cells and various components of TME, thereby affect immune escape of tumors and ultimately tumor proliferation, recurrence, or metastasis. In addition, we also investigated the correlation between CAFs and ptpn6 expression, and found that ptpn6 expression was positively correlated with CAFs in COAD, HNSC-HPV-, LGG and THCA, while negatively correlated with BRCA-LumA/LumB, mesothelioma (MESO) and THYM (Figure S4).
Subsequent studies on ptpn6-related genes and proteins obtained a large number of immune-related and tumor-related proteins, further confirming the role of ptpn6 in immunity and tumorigenesis. For example, CORO1A inhibited TLR-mediated signal activation in human macrophages55, RAC2 mutations led to different forms of primary immunodeficiencies56, RASAL3 served as a therapeutic target to regulate inflammatory responses in many inflammatory disease states57, ARHGAP30 and ARHGAP9 genetic alterations led to carcinogenesis of colorectal cancer (CRC)58, Vav1 accelerated Ras-driven lung cancer and modulates its tumor microenvironment59,60, and FERMT3 acted as a tumor suppressor gene in GBM and lung cancer61,62. Furthermore, our researches have found two important intersection proteins, LCP2 and LAIR1, which possibly had potential prognostic value or serve as immunotherapeutic targets for cancers. LCP2 had been confirmed to be an independent prognostic factor in DLBCL, LUAD and melanoma39,63,64. Previous studies have also demonstrated that LAIR1 induced T cell exhaustion through regulating the expression of ptpn6, leading to the occurrence and development of lung tumors19.
In addition, through the KEGG and GO enrichment analysis of the ptpn6-related genes and SHP-1-binding proteins, we could find that ptpn6 is involved in immune-related biological processes, such as natural killer cell mediated cytotoxicity, B cell receptor signaling pathway, T cell receptor signaling pathway, further indicating its critical role in immune function. However, it is still unclear about the correlation between ptpn6 and these genes/proteins. Therefore, further study of other ptpn6 expression-correlated genes/proteins, such as whether ptpn6 can regulate the expression of these genes, and affect the immune infiltration, thus affecting the occurrence and development of tumors, are of great significance.
In addition, genomic DNA methylation is an important epigenetic event in humans, and the alterations of methylation patterns may play important roles in tumorigenesis24,65,66. As one of the earliest molecular changes during the transformation process of normal cells into cancerous cells67, aberrant DNA methylation pattern may have potential applications in the early detection of malignancies. Currently, many studies have been devoted to evaluating epigenetic regulation of gene expression by promoter methylation, with the aim of identifying new biomarkers of cancer development. In our results from the database, the methylation levels of ptpn6 were significantly decreased in 11 types of tumors, along with the significantly higher expression of ptpn6 in 8 types of which, including BLCA, BRCA, CESC, HNSC, KIRC, KIRP, TGCT and UCEC, than that in normal tissues. In previous studies, the hypermethylation of the ptpn6 promoter was observed in leukemia and lymphoma14,68,69,70, esophageal squamous cell carcinoma71, gastric adenocarcinoma72, breast cancer73, endometrial carcinoma54, and nasopharyngeal carcinoma74. Moreover, the expression level of ptpn6 has a strong reverse correlation with promoter methylation, and the promoter hypermethylation has been proved to be the cause of ptpn6 silencing47. Here, the hypomethylation of ptpn6 was associated with increased expression of ptpn6. Notably, in KIRC and TGCT, the increased expression of ptpn6 was associated with its poor prognosis and high immunoinfiltration, accompanied by the promoter hypomethylation, reflecting the close relationship between epigenetic modifications (such as methylation) and gene expression, cancer immune environment and prognosis. Thus, we speculate that promoter hypomethylation of ptpn6 in some cancers may lead to its increased expression, which may be associated with the low prognosis and high immunoinfiltration, according to our results. Nevertheless, it is worth noting that the regulation of ptpn6 promoter methylation is complex and involved in multiple factors, such as environmental exposure, gene mutations, and epigenetic modifications. Therefore, it is necessary to conduct comprehensive and systematic research on the mechanisms of ptpn6 promoter methylation in cancer, in order to provide a scientific basis for its clinical application. Our findings can provide clues for further work related to ptpn6 methylation, which holds great promise for revealing the mechanism of ptpn6 in tumorigenesis and progression.
Our findings suggest that ptpn6 can be served as an independent prognostic factor of many tumors and for different tumors, its expression level will bring different or even completely opposite prognostic outcomes. In this study, the increased expression of ptpn6 was found to be significantly associated with poor prognosis and high immune infiltration in LGG, KIRC, UCS, and TGCT, suggesting its cancer-promoting role in some specific tumor types, as we have described previously. However, in BLCA, BRCA, CESC, STAD, KIRP, PAAD, and UCEC, its high expression was significantly associated with good prognosis(Figure S1-2). In previous functional verification experiments, it was confirmed that ptpn6 can restrict the growth of PAAD cells by reducing the phosphorylation of STAT3 and blocking the activation of STAT375. It was also found that increased ptpn6 levels blocked the JAK2/STAT3 pathway, leading to reduced proliferation, migration, and invasion of STAD72,76,77. These results further validated our findings regarding the role of ptpn6 in STAD and PAAD. These suggest a complex correlation between ptpn6 expression and the survival of different types of cancer, possibly due to its different biological backgrounds and roles in tumorigenesis. This might, at least in part, contribute to the disappointing results of drug discovery to date with SHP-1 as a tumor therapeutic target. The in-depth study of the specific role of ptpn6 in each cancer may have important implications for diagnosis and immunotherapy in the era of precision medicine.
Conclusions
In this study, we provide a comprehensive understanding of the roles of ptpn6 across different tumors, including the expression, prognosis, immune correlation, genetic alteration, epigenetic alterations, and relevant cellular pathways and functions. The results showed that ptpn6 can serve as a prognostic factor for a variety of cancers, and that ptpn6 can play an important role in tumor immunity by affecting tumor infiltrating immune cells. These findings aid in understanding the role of ptpn6 in tumorigenesis and development, presenting a potential biomarker for poor prognosis and immune infiltration in diverse cancer types.
Summary
SHP-1, a nonreceptor protein tyrosine phosphatase encoded by ptpn6, has been regarded as a regulatory protein of hematopoietic cell biology for years. Nowadays increasing evidence supports that ptpn6 plays a crucial role in the tumorigenesis and progression of some cancers. Nevertheless, most studies into its role in tumors to date have been limited to a specific type of cancer. Herein, the role of ptpn6 for prognosis and immune regulation across 33 tumors was investigated, aiming to explore its function heterogeneity in pan-cancer and the clinical significance. The results showed that ptpn6 can serve as a prognostic factor for a variety of cancers, and that it can play an important role in tumor immunity by affecting tumor infiltrating immune cells.
In this study, we not only have a landscape of the roles of ptpn6 across different tumors, including the expression, prognostic, immune correlation, genetic alteration, epigenetic alterations, relevant cellular pathway and function, but also provide insight into presenting a potential prognosis biomarker and immunotherapy target. It also reflects the close relationship between ptpn6 epigenetic modifications (such as methylation), ptpn6 gene expression, cancer immune environment and prognosis. Moreover, interestingly, ptpn6 can be served as an independent prognostic factor of many tumors and for different tumors, its expression level will bring different or even completely opposite prognostic outcomes. This suggest a complex correlation between ptpn6 expression and the survival of different types of cancer. These findings aid in understanding the role of ptpn6 in tumorigenesis and development, and have important implications for tumor diagnosis and immunotherapy in the era of precision medicine.
Data availability
All data generated or analyzed during this study are included in the specified repository (http://timer.cistrome.org/, http://gepia2.cancer-pku.cn/, https://kmplot.com/analysis/, https://cistrome.shinyapps.io/timer/, https://string-db.org/, https://david.ncifcrf.gov/, http://biocc.hrbmu.edu.cn/CancerSEA/ and http://www.cbioportal.org, http://ualcan.path.uab.edu/analysis.html).
References
Bray, F. et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Cancer J. Clin. 68, 394–424. https://doi.org/10.3322/caac.21492 (2018).
Dumitrescu, R. G. in Cancer Epigenetics for Precision Medicine: Methods and Protocols (eds Ramona G. Dumitrescu & Mukesh Verma) 3–17. (Springer New York, 2018).
Costa-Pinheiro, P., Montezuma, D., Henrique, R. & Jerónimo, C. Diagnostic and prognostic epigenetic biomarkers in cancer. Epigenomics 7, 1003–1015. https://doi.org/10.2217/epi.15.56 (2015).
Sharma, Y., Bashir, S., Bhardwaj, P., Ahmad, A. & Khan, F. Protein tyrosine phosphatase SHP-1: resurgence as new drug target for human autoimmune disorders. Immunol. Res. 64, 804–819. https://doi.org/10.1007/s12026-016-8805-y (2016).
He, R. J., Yu, Z. H., Zhang, R. Y. & Zhang, Z. Y. Protein tyrosine phosphatases as potential therapeutic targets. Acta Pharmacol. Sin. 35, 1227–1246. https://doi.org/10.1038/aps.2014.80 (2014).
Marín-Juez, R., Jong-Raadsen, S., Yang, S. & Spaink, H. P. Hyperinsulinemia induces insulin resistance and immune suppression via Ptpn6/Shp1 in zebrafish. J. Endocrinol. 222, 229–241. https://doi.org/10.1530/joe-14-0178 (2014).
Lorenz, U. SHP-1 and SHP-2 in T cells: two phosphatases functioning at many levels. Immunol. Rev. 228, 342–359. https://doi.org/10.1111/j.1600-065X.2008.00760.x (2009).
Abram, C. L. & Lowell, C. A. Shp1 function in myeloid cells. J. Leukoc. Biol. 102, 657–675. https://doi.org/10.1189/jlb.2MR0317-105R (2017).
Garg, M., Wahid, M. & Khan, F. D. Regulation of peripheral and central immunity: understanding the role of src homology 2 ___domain-containing tyrosine phosphatases, SHP-1 & SHP-2. Immunobiology 225, 151847. https://doi.org/10.1016/j.imbio.2019.09.006 (2020).
Wu, C., Guan, Q., Wang, Y., Zhao, Z. J. & Zhou, G. W. SHP-1 suppresses cancer cell growth by promoting degradation of JAK kinases. J. Cell. Biochem. 90, 1026–1037. https://doi.org/10.1002/jcb.10727 (2003).
Wang, F. et al. Comprehensive analysis of PTPN gene family revealing PTPN7 as a novel biomarker for immuno-hot tumors in breast cancer. Front. Genet. 13, 981603. https://doi.org/10.3389/fgene.2022.981603 (2022).
Mok, S. C., Kwok, T. T., Berkowitz, R. S., Barrett, A. J. & Tsui, F. W. Overexpression of the protein tyrosine phosphatase, nonreceptor type 6 (PTPN6), in human epithelial ovarian cancer. Gynecol. Oncol. 57, 299–303. https://doi.org/10.1006/gyno.1995.1146 (1995).
Xu, S. B. et al. DNA methylation regulates constitutive expression of Stat6 regulatory genes SOCS-1 and SHP-1 in colon cancer cells. J. Cancer Res. Clin. Oncol. 135, 1791–1798. https://doi.org/10.1007/s00432-009-0627-z (2009).
Li, Y. et al. Methylation and decreased expression of SHP-1 are related to disease progression in chronic myelogenous leukemia. Oncol. Rep. 31, 2438–2446. https://doi.org/10.3892/or.2014.3098 (2014).
Zhang, Q. et al. STAT3- and DNA methyltransferase 1-mediated epigenetic silencing of SHP-1 tyrosine phosphatase tumor suppressor gene in malignant T lymphocytes. Proc. Natl. Acad. Sci. U. S. A. 102, 6948–6953. https://doi.org/10.1073/pnas.0501959102 (2005).
Wen, L. Z. et al. SHP-1 acts as a tumor suppressor in Hepatocarcinogenesis and HCC Progression. Cancer Res. 78, 4680–4691. https://doi.org/10.1158/0008-5472.Can-17-3896 (2018).
Fang, H., Ma, W., Guo, X. & Wang, J. PTPN6 promotes chemosensitivity of colorectal cancer cells via inhibiting the SP1/MAPK signalling pathway. Cell Biochem. Funct. 39, 392–400. https://doi.org/10.1002/cbf.3604 (2021).
Wu, C., Sun, M., Liu, L. & Zhou, G. W. The function of the protein tyrosine phosphatase SHP-1 in cancer. Gene 306, 1–12. https://doi.org/10.1016/s0378-1119(03)00400-1 (2003).
Peng, D. H. et al. Collagen promotes anti-PD-1/PD-L1 resistance in cancer through LAIR1-dependent CD8(+) T cell exhaustion. Nat. Commun. 11, 4520. https://doi.org/10.1038/s41467-020-18298-8 (2020).
Acharya, N. et al. Endogenous glucocorticoid signaling regulates CD8(+) T cell differentiation and development of dysfunction in the Tumor Microenvironment. Immunity 53, 658–671e656. https://doi.org/10.1016/j.immuni.2020.08.005 (2020).
Zhang, L. et al. Novel targets for immunotherapy associated with exhausted CD8 + T cells in cancer. J. Cancer Res. Clin. Oncol. 149, 2243–2258. https://doi.org/10.1007/s00432-022-04326-1 (2023).
Snook, J. P., Soedel, A. J., Ekiz, H. A., O’Connell, R. M. & Williams, M. A. Inhibition of SHP-1 expands the Repertoire of Antitumor T Cells Available to Respond to Immune Checkpoint Blockade. Cancer Immunol. Res. 8, 506–517. https://doi.org/10.1158/2326-6066.Cir-19-0690 (2020).
Watson, H. A., Wehenkel, S., Matthews, J. & Ager, A. SHP-1: the next checkpoint target for cancer immunotherapy? Biochem. Soc. Trans. 44, 356–362. https://doi.org/10.1042/bst20150251 (2016).
Vasiljević, N., Scibior-Bentkowska, D., Brentnall, A. R., Cuzick, J. & Lorincz, A. T. Credentialing of DNA methylation assays for human genes as diagnostic biomarkers of cervical intraepithelial neoplasia in high-risk HPV positive women. Gynecol. Oncol. 132, 709–714. https://doi.org/10.1016/j.ygyno.2014.02.001 (2014).
Tang, Z., Kang, B., Li, C., Chen, T. & Zhang, Z. GEPIA2: an enhanced web server for large-scale expression profiling and interactive analysis. Nucleic Acids Res. 47, W556–w560. https://doi.org/10.1093/nar/gkz430 (2019).
Hou, G. X., Liu, P., Yang, J. & Wen, S. Mining expression and prognosis of topoisomerase isoforms in non-small-cell lung cancer by using Oncomine and Kaplan-Meier plotter. PloS One 12, e0174515. https://doi.org/10.1371/journal.pone.0174515 (2017).
Peng, L. et al. A Pan-cancer analysis of SMARCA4 alterations in human cancers. Front. Immunol. 12, 762598. https://doi.org/10.3389/fimmu.2021.762598 (2021).
Li, T. et al. TIMER2.0 for analysis of tumor-infiltrating immune cells. Nucleic Acids Res. 48, W509–w514. https://doi.org/10.1093/nar/gkaa407 (2020).
Szklarczyk, D. et al. The STRING database in 2021: customizable protein-protein networks, and functional characterization of user-uploaded gene/measurement sets. Nucleic Acids Res. 49, D605–d612. https://doi.org/10.1093/nar/gkaa1074 (2021).
Bardou, P., Mariette, J., Escudié, F., Djemiel, C. & Klopp, C. Jvenn: an interactive Venn diagram viewer. BMC Bioinform. 15, 293. https://doi.org/10.1186/1471-2105-15-293 (2014).
Kanehisa, M. Toward understanding the origin and evolution of cellular organisms. Protein Sci. Publ. Protein Soc. 28, 1947–1951. https://doi.org/10.1002/pro.3715 (2019).
Kanehisa, M., Furumichi, M., Sato, Y., Kawashima, M. & Ishiguro-Watanabe, M. KEGG for taxonomy-based analysis of pathways and genomes. Nucleic Acids Res. 51, D587–d592. https://doi.org/10.1093/nar/gkac963 (2023).
Kanehisa, M. & Goto, S. KEGG: kyoto encyclopedia of genes and genomes. Nucleic Acids Res. 28, 27–30. https://doi.org/10.1093/nar/28.1.27 (2000).
Yuan, H. et al. CancerSEA: a cancer single-cell state atlas. Nucleic Acids Res. 47, D900–d908. https://doi.org/10.1093/nar/gky939 (2019).
Cerami, E. et al. The cBio cancer genomics portal: an open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2, 401–404. https://doi.org/10.1158/2159-8290.Cd-12-0095 (2012).
Chandrashekar, D. S. et al. An update to the integrated cancer data analysis platform. Neoplasia (New York N Y) 25 UALCAN, 18–27. https://doi.org/10.1016/j.neo.2022.01.001 (2022).
Uhlén, M. et al. Proteomics. Tissue-based map of the human proteome. Science 347, 1260419. https://doi.org/10.1126/science.1260419 (2015).
Uhlen, M. et al. A pathology atlas of the human cancer transcriptome. Science 357https://doi.org/10.1126/science.aan2507 (2017).
Pan, T. et al. Identification and validation of a prognostic gene signature for diffuse large B-Cell lymphoma based on Tumor Microenvironment-related genes. Front. Oncol. 11, 614211. https://doi.org/10.3389/fonc.2021.614211 (2021).
Mao, X. et al. Crosstalk between cancer-associated fibroblasts and immune cells in the tumor microenvironment: new findings and future perspectives. Mol. Cancer 20, 131. https://doi.org/10.1186/s12943-021-01428-1 (2021).
Yao, J. et al. Development and validation of a prognostic gene signature correlated with M2 macrophage infiltration in esophageal squamous cell carcinoma. Front. Oncol. 11, 769727. https://doi.org/10.3389/fonc.2021.769727 (2021).
Zhang, C. et al. Tumor Purity as an underlying key factor in Glioma. Clin. Cancer Res. 23, 6279–6291. https://doi.org/10.1158/1078-0432.Ccr-16-2598 (2017).
Mao, Y. et al. Low tumor purity is associated with poor prognosis, heavy mutation burden, and intense immune phenotype in colon cancer. Cancer Manag. Res. 10, 3569–3577. https://doi.org/10.2147/CMAR.S171855 (2018).
Zhao, K., Ma, Z. & Zhang, W. Comprehensive Analysis to identify SPP1 as a Prognostic Biomarker in Cervical Cancer. Front. Genet. 12, 732822. https://doi.org/10.3389/fgene.2021.732822 (2021).
Koch, A. et al. Analysis of DNA methylation in cancer: ___location revisited. Nat. Rev. Clin. Oncol. 15, 459–466. https://doi.org/10.1038/s41571-018-0004-4 (2018).
Feng, G. S. et al. Receptor-binding, tyrosine phosphorylation and chromosome localization of the mouse SH2-containing phosphotyrosine phosphatase Syp. Oncogene 9, 1545–1550 (1994).
Wu, W. et al. SHP1 loss augments DLBCL cellular response to ibrutinib: a candidate predictive biomarker. Oncogene 42, 409–420. https://doi.org/10.1038/s41388-022-02565-7 (2023).
Shen, C. et al. The Analysis of PTPN6 for Bladder Cancer: An Exploratory Study Based on TCGA. Disease markers 4312629. https://doi.org/10.1155/2020/4312629 (2020).
Liu, C. Y. et al. Sorafenib analogue SC-60 induces apoptosis through the SHP-1/STAT3 pathway and enhances docetaxel cytotoxicity in triple-negative breast cancer cells. Mol. Oncol. 11, 266–279. https://doi.org/10.1002/1878-0261.12033 (2017).
Tao, T. et al. PDZK1 inhibits the development and progression of renal cell carcinoma by suppression of SHP-1 phosphorylation. Oncogene 36, 6119–6131. https://doi.org/10.1038/onc.2017.199 (2017).
Huang, Z. et al. Knockdown of RNF6 inhibits gastric cancer cell growth by suppressing STAT3 signaling. OncoTargets Therapy 11, 6579–6587. https://doi.org/10.2147/ott.S174846 (2018).
Sooman, L. et al. PTPN6 expression is epigenetically regulated and influences survival and response to chemotherapy in high-grade gliomas. Tumour Biol. J. Int. Soc. Oncodev. Biol. Med. 35, 4479–4488. https://doi.org/10.1007/s13277-013-1590-5 (2014).
Shanmugam, M. K. et al. Abrogation of STAT3 signaling cascade by zerumbone inhibits proliferation and induces apoptosis in renal cell carcinoma xenograft mouse model. Mol. Carcinog. 54, 971–985. https://doi.org/10.1002/mc.22166 (2015).
Sheng, Y. et al. Methylation of tumor suppressor gene CDH13 and SHP1 promoters and their epigenetic regulation by the UHRF1/PRMT5 complex in endometrial carcinoma. Gynecol. Oncol. 140, 145–151. https://doi.org/10.1016/j.ygyno.2015.11.017 (2016).
Marx, A. et al. Thymus and autoimmunity. Semin. Immunopathol. 43, 45–64. https://doi.org/10.1007/s00281-021-00842-3 (2021).
Lougaris, V., Baronio, M., Gazzurelli, L., Benvenuto, A. & Plebani, A. RAC2 and primary human immune deficiencies. J. Leukoc. Biol. 108, 687–696. https://doi.org/10.1002/jlb.5mr0520-194rr (2020).
Muro, R., Nitta, T., Kitajima, M., Okada, T. & Suzuki, H. Rasal3-mediated T cell survival is essential for inflammatory responses. Biochem. Biophys. Res. Commun. 496, 25–30. https://doi.org/10.1016/j.bbrc.2017.12.159 (2018).
Wang, J. et al. ArhGAP30 promotes p53 acetylation and function in colorectal cancer. Nat. Commun. 5, 4735. https://doi.org/10.1038/ncomms5735 (2014).
Sun, J. et al. ARHGAP9 inhibits colorectal cancer cell proliferation, invasion and EMT via targeting PI3K/AKT/mTOR signaling pathway. Tissue Cell. 77, 101817. https://doi.org/10.1016/j.tice.2022.101817 (2022).
Zhang, H. et al. ARHGAP9 suppresses the migration and invasion of hepatocellular carcinoma cells through up-regulating FOXJ2/E-cadherin. Cell Death Dis. 9https://doi.org/10.1038/s41419-018-0976-0 (2018).
Lu, C. et al. FERMT3 contributes to glioblastoma cell proliferation and chemoresistance to temozolomide through integrin mediated wnt signaling. Neurosci. Lett. 657, 77–83. https://doi.org/10.1016/j.neulet.2017.07.057 (2017).
Farago, M., Yarnitzky, T., Shalom, B. & Katzav, S. Vav1 mutations: what makes them oncogenic? Cell. Signal. 65, 109438. https://doi.org/10.1016/j.cellsig.2019.109438 (2020).
Fan, T., Li, C. & He, J. Prognostic value of immune-related genes and comparative analysis of immune cell infiltration in lung adenocarcinoma: sex differences. Biology sex. Differences 12, 64. https://doi.org/10.1186/s13293-021-00406-y (2021).
Wang, Z. & Peng, M. A novel prognostic biomarker LCP2 correlates with metastatic melanoma-infiltrating CD8(+) T cells. Sci. Rep. 11, 9164. https://doi.org/10.1038/s41598-021-88676-9 (2021).
Warnecke, P. M. & Bestor, T. H. Cytosine methylation and human cancer. Curr. Opin. Oncol. 12, 68–73. https://doi.org/10.1097/00001622-200001000-00012 (2000).
Parris, T. Z. et al. Frequent MYC coamplification and DNA hypomethylation of multiple genes on 8q in 8p11-p12-amplified breast carcinomas. Oncogenesis 3, e95. https://doi.org/10.1038/oncsis.2014.8 (2014).
El-Osta, A., Baker, E. K. & Wolffe, A. P. Profiling methyl-CpG specific determinants on transcriptionally silent chromatin. Mol. Biol. Rep. 28, 209–215. https://doi.org/10.1023/a:1015744625049 (2001).
Oka, T. et al. Gene silencing of the tyrosine phosphatase SHP1 gene by aberrant methylation in leukemias/lymphomas. Cancer Res. 62, 6390–6394 (2002).
Ding, K. et al. Plasma DNA methylation of p16 and shp1 in patients with B cell non-hodgkin lymphoma. Int. J. Clin. Oncol. 22, 585–592. https://doi.org/10.1007/s10147-017-1100-7 (2017).
Liu, J. et al. Promoter methylation attenuates SHP1 expression and function in patients with primary central nervous system lymphoma. Oncol. Rep. 37, 887–894. https://doi.org/10.3892/or.2016.5308 (2017).
Liu, L., Zhang, S., Liu, X. & Liu, J. Aberrant promoter 2 methylation–mediated downregulation of protein tyrosine phosphatase, non–receptor type 6, is associated with progression of esophageal squamous cell carcinoma. Mol. Med. Rep. 19, 3273–3282. https://doi.org/10.3892/mmr.2019.9971 (2019).
Joo, M. K. et al. Epigenetic regulation and anti-tumorigenic effects of SH2-containing protein tyrosine phosphatase 1 (SHP1) in human gastric cancer cells. Tumour Biol. J. Int. Soc. Oncodev. Biol. Med. 37, 4603–4612. https://doi.org/10.1007/s13277-015-4228-y (2016).
Hachana, M., Trimeche, M., Ziadi, S., Amara, K. & Korbi, S. Evidence for a role of the Simian Virus 40 in human breast carcinomas. Breast Cancer Res. Treat. 113, 43–58. https://doi.org/10.1007/s10549-008-9901-z (2009).
Challouf, S. et al. Patterns of aberrant DNA hypermethylation in nasopharyngeal carcinoma in Tunisian patients. Clin. Chim. Acta 413, 795–802. https://doi.org/10.1016/j.cca.2012.01.018 (2012).
Zhang, M. et al. SHP1 decreases level of P-STAT3 (Ser727) and inhibits Proliferation and Migration of Pancreatic Cancer cells. J. Environ. Pathol. Toxicol. Oncology: Official Organ. Int. Soc. Environ. Toxicol. Cancer 40, 17–27. https://doi.org/10.1615/JEnvironPatholToxicolOncol.2020035980 (2021).
Myers, D. R. et al. Shp1 loss enhances macrophage effector function and promotes Anti-tumor Immunity. Front. Immunol. 11. https://doi.org/10.3389/fimmu.2020.576310 (2020).
Chen, J., Zhao, X., Yuan, Y. & Jing, J. J. The expression patterns and the diagnostic/prognostic roles of PTPN family members in digestive tract cancers. Cancer Cell Int. 20, 238. https://doi.org/10.1186/s12935-020-01315-7 (2020).
Funding
This study was supported by the National Natural Science Foundation of China (NSFC 82002134), One Thousand of Young and Middle-aged Key Teachers Training Program in Guangxi Colleges and Universities (To Cui Ping) (DC2300017000), National Natural Science Foundation of Guangxi (2023GXNSFDA026036), 2022 Innovation and Entrepreneurship Training Program of Guangxi Medical University (202210598034).
Author information
Authors and Affiliations
Contributions
HL, JGH, and SQA designed the study. PC and JL contributed to manuscript writing and data analysis. PC, JL, YL and DSZ participated in the data acquisition. YL and LLL participated in data checking. LY and HC participated in interpreting the results. HL, JGH and SQA revised the article. All authors contributed to the article and approved the submitted version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cui, P., Lian, J., Liu, Y. et al. Pan-cancer analysis of the prognostic and immunological roles of SHP-1/ptpn6. Sci Rep 14, 23083 (2024). https://doi.org/10.1038/s41598-024-74037-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-74037-9