Abstract
Cardiometabolic index (CMI) is a novel anthropometric metric that integrates lipid and adiposity characteristics. The correlation between periodontitis development and CMI is ambiguous. The objective of this study was to establish the association between CMI and periodontitis by analyzing data from the NHANES (National Health and Nutrition Examination Survey) database. A cross-sectional study was conducted on a cohort of 6188 people selected from the NHANES database, covering the period from 2009 to 2014. The study employed multivariate logistic regression to examine the independent correlation between CMI and periodontitis. Subgroup data were analyzed and interaction tests were conducted to assess the impact of variables on the correlation between CMI and periodontitis. The CMI index was significantly and positively associated with the presence of periodontitis (β = 0.03, 95%CI(0.01, 0.05), p = 0.0092). In addition, a U-shaped relationship was found between CMI index and periodontitis severity in an older American population (65 < = age < = 80, with a folding point of 1.44, p = 0.008). This study demonstrates a significant correlation between CMI and periodontitis, positioning CMI as a crucial indicator for assessing periodontal health. Future efforts should prioritize oral hygiene interventions for patients with elevated CMI levels to facilitate early intervention and enhance overall health outcomes.
Similar content being viewed by others
Introduction
Periodontitis is a chronic non-communicable disease (NCD) that affects 11.2% of the worldwide population and is the sixth most widespread human illness. Its rates of prevalence range from 45 to 50% over the whole population1. There is substantial evidence indicating a direct connection between periodontitis and other systemic illnesses2,3,4,5. Severe periodontitis has a strong correlation with both all-cause and cardiovascular mortality, regardless of other contributing variables5,6. According to these studies, there is a direct connection between periodontitis and a wide variety of metabolic problems.
The waist-to-height ratio (WHtR) to high-density lipoprotein cholesterol (HDL-C) ratio7 is multiplied to determine the CMI, which was introduced in 2015. Obesity and lipid indicators, such as body mass index (BMI), waist circumference (WC), triglycerides (TG), and body mass index (BAI), are less effective in predicting metabolic disorders compared to CMI7,8,9.
The CMI is a more effective predictor of metabolic disorders as it integrates both the waist-to-height ratio (WHtR) and high-density lipoprotein cholesterol (HDL-C) levels, providing a comprehensive assessment of an individual’s metabolic health, particularly regarding the impact of abdominal fat distribution and the protective role of cholesterol, thereby outperforming traditional obesity and lipid indices.
Given the favorable diagnostic potential of CMI for a range of metabolic diseases. Furthermore, there exists a complex and inseparable connection between periodontitis and several systemic disorders. Hence, it is imperative to do more research on the possible contribution of CMI in the diagnosis of periodontitis, as no relevant studies have been documented thus far.
This study aims to investigate the potential role of the CMI in the assessment of periodontitis, utilizing data from the NHANES database.
Methods
Data sources and study population
The National Health and Nutrition Examination Survey (NHANES) gathered information on factors that people were exposed to and the resulting outcomes. This data was collected throughout three consecutive cycles from 2009 to 2014. You may find more information at https://www.cdc.gov/nchs/nhanes. The National Centre for Health Statistics (NCHS) is in charge of NHANES administration. The data were collected through health interviews conducted at participants’ residences, health checks carried out at mobile testing centres (MECs), and laboratory samples. There was no need for a supplementary ethical review for this manuscript, as NHANES underwent an ethical review by the National Ethical Review Board for Research in Health Statistics10.
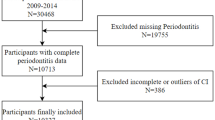
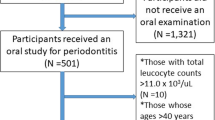
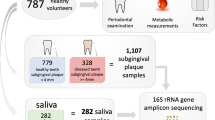
The study, which initially comprised 30,468 participants (NHANES 2009 through 2014), incorporated the most recent periodontal examination data for US adults. The eligibility of a subject to participate was determined based on the following criteria: (1) NHANES participants aged thirty years or older; (2) individuals who had undergone an oral periodontal examination; and (3) NHANES participants with available data on their waist-to-height ratio, triglycerides, and HDL-C. In the end, a grand total of 6188 individuals were enrolled in the research. Figure 1 depicts the procedure of data filtration.
Outcome variable
Clinical attachment loss (AL) and periodontal pocket probing depth (PD) are typical indicators for evaluating the severity of periodontitis11. The periodontist examined the 28 eligible participants’ teeth at the mobile examination center, exploring each tooth at six sites, but did not include the third molars12. This study employed the CDC/AAP classification criteria for periodontitis, which were created by Eke et al. in 201213. 2 neighboring AL ≥ 3 mm, ≥ 2 neighboring PD ≥ 4 mm (not on the same tooth), or 1 neighboring PD ≥ 5 mm were the criteria for mild periodontitis. A periodontitis that was classified as moderate was defined as two adjacent alveoli (AL) that were either ≥ 4 mm (not on the same tooth) or ≥ 2 mm (in the same tooth). Two neighboring sites AL ≥ 6 mm (not on the same tooth) and at least one neighboring site PD ≥ 5 mm were used to designate severe periodontitis. As per the aforementioned criteria, individuals are classified as having mild periodontitis, moderate periodontitis, severe periodontitis, or no periodontitis.
Exposure variable
Cardiometabolic Index was determined by employing the subsequent formula: CMI = TG(mmol/L)/HDL-C(mmol/L)*WHtR. The data was categorized into four categories based on quartiles: CMIQ1 (CMI less than 0.311), CMIQ2 (CMI between 0.311 and 0.534), CMIQ3 (CMI between 0.534 and 0.938), CMIQ4 (CMI more than or equal to 0.938).
Confounding variables
Covariates were chosen in accordance with clinical expertise and prior research. The missing data were imputed using multiple imputation. This study included the following covariates: gender, age, race, alcohol consumption history, smoking history, diabetes, glycohemoglobin, hypertension, heart disease, hypercholesterolemia, and cancer. Gender was categorized as male or female, and age was segmented into four categories to investigate the impact of CMI on periodontal disease across different age groups. The race categories included Mexican American, Other Hispanic, Non-Hispanic White, Non-Hispanic Black, and Other Race. Participants were classified into four groups based on their frequency of alcohol consumption in the past 12 months: no alcohol consumption (< 1), light drinking ( > = 1,<10), moderate drinking ( > = 10, < 20), and heavy drinking ( > = 20). Participants were divided into two groups based on whether they had smoked more than 100 cigarettes: YES or NO. Diabetes status was categorized into three groups: YES, NO, or Borderline, based on whether a doctor had diagnosed the participant with diabetes. Hypertension status was divided into two groups based on whether the participant had been told they had high blood pressure: YES or NO. Heart disease status was categorized into two groups based on whether the participant had been told they had coronary heart disease: YES or NO. Hypercholesterolemia status was split into two groups based on whether a doctor had diagnosed the participant with high cholesterol level: YES or NO. Cancer status was categorized into two groups based on whether the participant had been told they had cancer or malignancy: YES or NO.
Statistical analysis
The statistical analysis of the results was performed using the R software (R4.2.1, http://www.R-project.org) in combination with Empower Stats 4.1, which could be accessed at http://www.empowerstats.com. The Kruskal-Wallis H-test was used to evaluate statistical disparities among different CMI groups (quartiles) for continuous variables, while the chi-square test was performed for categorical variables. The study utilized multivariate logistic regression to investigate the independent association between CMI and periodontitis. Three models were employed: an unadjusted model, a model adjusted for age, gender, and race (model 1), and a model adjusted for age, gender, race, alcohol consumption, smoking, diabetes, hypertension, heart disease, hypercholesterolemia, and cancer (model 2). The robustness of the results was guaranteed by employing trend p values as sensitivity analyses14. Analyzed subgroups and conducted interaction tests to assess the influence of variables on the relationship between CMI and periodontitis15. In the end, we performed smoothed curve fitting and threshold effect experiments to examine the association between the CMI and periodontitis, as well as any potential nonlinear relationships.
Results
Baseline characteristics of the population
The Table 1 displays the fundamental features of the research population. The analysis covered a total of 6188 individuals. The average CMI was 0.81. The study classified CMI into four groups: CMIQ1 (CMI < 0.311), CMIQ2 (0.311 ≤ CMI < 0.534), CMIQ3 (0.534 ≤ CMI < 0.938), and CMIQ4 (CMI ≥ 0.938). The participants had an average age of 53.98 years, with 48.32% of them being male and up to 45.12% being Non-Hispanic White. Out of the sample, 3497 individuals, which represents 56.51% of the total, were not diagnosed with periodontitis. On the other hand, 161 patients (2.60%), 2153 patients (34.79%), and 377 patients (6.09%) had mild, moderate, and severe periodontitis, respectively.
Relationship between CMI index and periodontitis
In our study, we found a significant association between CMI and the risk of periodontitis(Table 2). In the unadjusted model, an increase in CMI was associated with an increased risk of periodontitis (β = 0.04, 95%CI: 1.02–1.06, P = 0.0004). This association remained significant even after adjusting for potential confounders such as age, gender, race, lifestyle factors, and chronic diseases (Model 1: β = 0.03, 95%CI: 1.01–1.06, P = 0.0022; Model 2: β = 0.03, 95%CI: 1.01–1.05, P = 0.0092), suggesting that CMI may be an independent predictor of periodontitis.
In the interaction test, we developed the age groups (AGEQ1 30 < = age < 41, AGEQ2 41 < = age < 53, AGEQ3 53 < = age < 65, AGEQ4 65 < = age < = 80) by four. The models were adjusted for gender, race, alcohol consumption, smoking, diabetes, glycohemoglobin, hypertension, heart disease, hypercholesterolemia, and cancer. Age was considered as the effect modifier. The results indicate that as age increases, the impact of increased CMI on the presence of periodontitis becomes more significant. The P-value for interaction is 0.00028, suggesting that age significantly modifies the relationship between CMI and periodontitis. The shift resulting from gender did not have a significant impact, as indicated by a P-value of 0.276 for the interaction (Table 3).
Figure 2 shows a smoothed curve analysis of the link between CMI and periodontitis. The analysis is grouped based on age, gender, diabetes, and alcohol consumption, as shown in Figs. 3, 4 and 5, and 6. The smoothed curve fit represents the nonlinear relationship between CMI and periodontitis. Once again, there is a notable and significant link between CMI and periodontitis.
The association between CMI and periodontitis stratified by alcohol consumption. CMI, cardiometabolic Index. Participants were categorized into four groups based on their alcohol consumption frequency over the past 12 months: non-drinkers (< 1), light drinkers ( > = 1, < 10), moderate drinkers ( > = 10, < 20), and heavy drinkers ( > = 20).
Relationship between CMI and periodontitis in an elderly population
To explore the relationship between periodontitis and CMI in older individuals, we divided them into four age subgroups. In general, it was noted that the seriousness of periodontitis increased gradually as the CMI levels rose. A special association was found between CMI and periodontitis in the senior population, following a U-shaped pattern, with a folding point of 1.44 (Table 4).
Discussion
Until now, there has been no investigation into the correlation between periodontitis and CMI. Periodontitis and several metabolic disorders have inflammation as a shared etiology16. This research comprised a total of 6188 individuals. An evident and robust correlation was seen between the severity of periodontitis and the degree of CMI. This connection remained statistically significant even after accounting for potential confounding variables through the use of multivariate logistic regression. Subgroup analysis also revealed a same pattern. Our research indicates that CMI is a reliable indicator for predicting the presence of periodontitis, demonstrating excellent diagnostic accuracy.
Periodontitis is a prevalent global health issue17. Periodontitis is a condition where the tissues that support the teeth are gradually destroyed. This is generally identified by clinical attachment loss (CAL), loss of the bone that holds the teeth in place as shown on radiographic examinations or images, the development of pockets around the teeth, and bleeding of the gums18. Alveolar bone, periodontal ligament, dentin, and gums are all impacted by the inflammatory disease known as periodontitis19. Additionally, it is recognized to elevate the likelihood of systemic inflammation and disease in remote tissues20. The research conducted by Hasturk and Sanz identified several potential mechanisms through which periodontitis may impact the distal organs20,21. The first mechanism involves the direct migration and colonization of periodontal microorganisms into the distal region, which induces an inflammatory response that is distal to the point of invasion. The second mechanism includes systemic inflammation either by metastatic periodontal inflammation or the activation of soluble inflammatory pathways by periodontal microbes20,22 .
Periodontitis has a relationship with metabolic disorders21,23,24,25,26,27. CMI serves as a dependable indicator of metabolic disorders28,29,30,31. Originally employed for the detection of diabetes, CMI exhibited a robust association with gender7. A study done by Q.Y. in a Chinese population of middle-aged and older persons revealed a direct relationship between CMI and the likelihood of acquiring new-onset type 2 diabetes mellitus32. A high CMI was determined to be a causative element in the onset of type 2 diabetes mellitus within this particular group. There is a correlation between CMI and the likelihood of developing type 2 diabetes mellitus, as demonstrated by numerous investigations8,9,33. Multiple inquiries have also substantiated a correlation between CMI and medical illnesses including hyperuricemia, stroke, and obstructive sleep apnea (OSA)28,34,35. As the CMI increases, the severity of the metabolic disorder also increases.
The precise mechanism by which CMI impacts the progression of periodontitis is still not fully understood and might be linked to systemic inflammatory reactions. A research conducted by Se. et al. discovered that in persons who are obese and have a high WHtR, an excess of free fatty acids hinders the effectiveness of insulin in regulating glucose metabolism36, leading to the development of diabetes mellitus. Dandona et al. discovered that individuals with diabetes and obesity had elevated levels of IL-6 and TNF-α in their bloodstream compared to the general population37. IL-6 and TNF-α are essential inflammatory mediators38,39; however, the pattern and rate of periodontitis development are determined by the sum of inflammatory responses in systemic tissues40. This implies that an elevated CMI is likely to impact the progression of periodontitis.
The latest agreement on periodontal disease highlights the correlation between periodontitis and cardiovascular disease21.It is necessary to thoroughly investigate the association between CMI and periodontitis, as there is currently a lack of publications on this topic. The current investigation demonstrated a positive correlation between the severity of periodontitis and the rise in CMI. However, among the older population, there was a curvilinear link between CMI and periodontitis, characterized by a U-shape. The folding point of this relationship was seen at 1.44. The folding point may be due to the following: first, the assessment of periodontitis involves numerous factors, including the probing depth (PD) and clinical attachment loss (AL) of periodontal pockets. Additionally, tooth loss is a severe end-stage manifestation of periodontitis that is most prevalent in older individuals. The current investigation established the degree of periodontitis by evaluating the depth of periodontal pockets (PD) and the amount of clinical attachment loss (AL). When a tooth is removed, the first severe symptoms of periodontitis, including as periodontal disease and attachment loss, are no longer present. The presence of a folding point in CMI does not indicate an improvement in periodontitis; in fact, it may indicate the onset of significant tooth loss. To summarize, the presence of the folding point did not impact the observed strong positive connection between CMI and periodontitis. Additionally, extensive research is needed in the future to further clarify the significance of CMI in periodontitis.
This study is the first to demonstrate a substantial positive relationship between CMI and periodontitis. Furthermore, the sample size is vast and reliable. Nevertheless, this investigation was conducted retrospectively and in a cross-sectional manner, preventing us from evaluating the causal connection between periodontitis and CMI. While efforts were made to account for various confounding factors, there is always a possibility that unaccounted confounders might affect the relationship between periodontitis and CMI.
Conclusion
To conclude, the presence of periodontitis in the US population is significantly and clearly correlated with an increase in CMI, even after controlling for other variables. The use of CMI as a novel and dependable anthropometric measure may be utilized to accurately forecast the occurrence of periodontitis.
Data availability
Publicly available datasets were analyzed in this study. This data can be found here: www.cdc.gov/nchs/nhanes/.
References
Kassebaum, N. J. et al. Global burden of severe periodontitis in 1990–2010: A systematic review and meta-regression. J. Dent. Res. 93, 1045–1053 (2014).
Zheng, X. et al. Periodontitis is associated with stroke. J. Transl Med. 21, 697 (2023).
Simpson, T. C. et al. Treatment of periodontitis for glycaemic control in people with diabetes mellitus. Cochrane Database Syst. Rev. 4, CD004714 (2022).
Linden, G. J., Lyons, A. & Scannapieco, F. A. Periodontal systemic associations: Review of the evidence. J. Clin. Periodontol. 40 (Suppl 14), S8–19 (2013).
Sharma, P., Dietrich, T., Ferro, C. J., Cockwell, P. & Chapple, I. L. C. Association between periodontitis and mortality in stages 3–5 chronic kidney disease: NHANES III and linked mortality study. J. Clin. Periodontol. 43, 104–113 (2016).
Linden, G. J. et al. All-cause mortality and periodontitis in 60-70-year-old men: A prospective cohort study. J. Clin. Periodontol. 39, 940–946 (2012).
Wakabayashi, I. & Daimon, T. The ‘cardiometabolic index’ as a new marker determined by adiposity and blood lipids for discrimination of diabetes mellitus. Clin. Chim. Acta. 438, 274–278 (2015).
Wang, Z., He, S. & Chen, X. Capacity of different anthropometric measures to predict diabetes in a Chinese population in southwest China: A 15-year prospective study. Diabet. Med. 36, 1261–1267 (2019).
Liu, X. et al. Cardiometabolic index: A new tool for screening the metabolically obese normal weight phenotype. J. Endocrinol. Invest. 44, 1253–1261 (2021).
Iranpour, S. & Sabour, S. Inverse association between caffeine intake and depressive symptoms in US adults: Data from National Health and Nutrition Examination Survey (NHANES) 2005–2006. Psychiatry Res. 271, 732–739 (2019).
Manresa, C., Sanz-Miralles, E. C., Twigg, J. & Bravo, M. Supportive periodontal therapy (SPT) for maintaining the dentition in adults treated for periodontitis. Cochrane Database Syst. Rev. 1, CD009376 (2018).
Page, R. C. & Eke, P. I. Case definitions for use in population-based surveillance of periodontitis. J. Periodontol. 78, 1387–1399 (2007).
Eke, P. I., Page, R. C., Wei, L., Thornton-Evans, G. & Genco, R. J. Update of the case definitions for population-based surveillance of periodontitis. J. Periodontol. 83, 1449–1454 (2012).
Jin, F. et al. Association between skull bone mineral density and periodontitis: Using the National Health and Nutrition Examination Survey (2011–2014). PLoS One. 17, e0271475 (2022).
Chen, X. et al. Association between life’s essential 8 and periodontitis: A population-based study. BMC Oral Health. 24, 19 (2024).
Dietrich, T., Sharma, P., Walter, C., Weston, P. & Beck, J. The epidemiological evidence behind the association between periodontitis and incident atherosclerotic cardiovascular disease. J. Clin. Periodontol. 40 (Suppl 14), S70–84 (2013).
GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: A systematic analysis for the global burden of Disease Study 2016. Lancet. 390, 1211–1259 (2017).
Papapanou, P. N. et al. Consensus report of workgroup 2 of the 2017 World workshop on the classification of Periodontal and Peri-implant diseases and conditions. J. Periodontol. 89 (Suppl 1), S173–S182 (2018). Periodontitis.
Slots, J. Periodontitis: Facts, fallacies and the future. Periodontology 2000. 75, 7–23 (2017).
Hasturk, H. & Kantarci, A. Activation and resolution of periodontal inflammation and its systemic impact. Periodontology 2000. 69, 255–273 (2015).
Sanz, M. et al. Periodontitis and cardiovascular diseases: Consensus report. J. Clin. Periodontol. 47, 268–288 (2020).
Hegde, R. & Awan, K. H. Effects of periodontal disease on systemic health. Dis. Mon. 65, 185–192 (2019).
Bassani, B. et al. Neutrophils’ contribution to periodontitis and periodontitis-associated cardiovascular diseases. Int. J. Mol. Sci. 24, 15370 (2023).
Herrera, D. et al. Association between periodontal diseases and cardiovascular diseases, diabetes and respiratory diseases: Consensus report of the Joint Workshop by the European Federation of Periodontology (EFP) and the European arm of the World Organization of Family doctors (WONCA Europe). J. Clin. Periodontol. 50, 819–841 (2023).
Irwandi, R. A. et al. The roles of neutrophils linking periodontitis and atherosclerotic cardiovascular diseases. Front. Immunol. 13, 915081 (2022).
Czesnikiewicz-Guzik, M. et al. Causal association between periodontitis and hypertension: Evidence from mendelian randomization and a randomized controlled trial of non-surgical periodontal therapy. Eur. Heart J. 40, 3459–3470 (2019).
Genco, R. J. & Sanz, M. Clinical and public health implications of periodontal and systemic diseases: An overview. Periodontol 2000. 83, 7–13 (2020).
Li, F. E. et al. Association between cardiometabolic index and stroke: A population- based cross-sectional study. Curr. Neurovasc Res. 18, 324–332 (2021).
Song, J. et al. Non-linear associations of cardiometabolic index with insulin resistance, impaired fasting glucose, and type 2 diabetes among US adults: A cross-sectional study. Front. Endocrinol. 15 (2024).
Sun, Q. et al. Cardiometabolic Index (CMI), lipid accumulation products (LAP), Waist triglyceride Index (WTI) and the risk of acute pancreatitis: A prospective study in adults of North China. Lipids Health Dis. 22, 190 (2023).
Zha, F. et al. The nonlinear correlation between the cardiometabolic index and the risk of diabetes: A retrospective Japanese cohort study. Front. Endocrinol. 14, (2023).
Qiu, Y. et al. Transition of cardiometabolic status and the risk of type 2 diabetes mellitus among middle-aged and older Chinese: A national cohort study. J. Diabetes Investig. 13, 1426–1437 (2022).
Liu, A.-B. et al. Associations of the cardiometabolic index with insulin resistance, prediabetes, and diabetes in U.S. adults: a cross-sectional study. BMC Endocr. Disord. 24, 217 (2024).
Cai, X. et al. Associations of the cardiometabolic index with the risk of cardiovascular disease in patients with hypertension and obstructive sleep apnea: Results of a longitudinal cohort study. Oxid. Med. Cell. Longev. 2022, 4914791 (2022).
Wang, H. et al. Body adiposity index, lipid accumulation product, and cardiometabolic index reveal the contribution of adiposity phenotypes in the risk of hyperuricemia among Chinese rural population. Clin. Rheumatol. 37, 2221–2231 (2018).
Se, K., Rl, H. & Km, U. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature 444 (2006).
Dandona, P., Aljada, A. & Bandyopadhyay, A. Inflammation: The link between insulin resistance, obesity and diabetes. Trends Immunol. 25, 4–7 (2004).
Akash, M. S. H., Rehman, K. & Liaqat, A. Tumor necrosis Factor-Alpha: Role in development of insulin resistance and Pathogenesis of type 2 diabetes Mellitus. J. Cell. Biochem. 119, 105–110 (2018).
Unver, N. & McAllister, F. IL-6 family cytokines: Key inflammatory mediators as biomarkers and potential therapeutic targets. Cytokine Growth Factor. Rev. 41, 10–17 (2018).
Kinane, D. F., Preshaw, P. M., Loos, B. G. & Working Group 2 of Seventh European Workshop on Periodontology. Host-response: Understanding the cellular and molecular mechanisms of host-microbial interactions–consensus of the seventh European workshop on Periodontology. J. Clin. Periodontol. 38 (Suppl 11), 44–48 (2011).
Acknowledgements
Thanks to Ajay Velu and Kiran Jain for corrections to the manuscript, and to Aleksandra Klisic for reviewing it.
Funding
This study was funded by the Health Commission of Hebei Province (20240105).
Author information
Authors and Affiliations
Contributions
1.LSN was involved in the study design, literature review, data analysis, and manuscript preparation. 2. ZZY and YW was involved in the development of the concept and was responsible for the critical review of the manuscript. 3. LJL carried out the data collection. 4. FXH were involved in the development of the concept and were responsible for the critical review of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shuning, L., Zhiyong, Z., Wei, Y. et al. Association between periodontitis and cardiometabolic index (CMI): a study from NHANES 2009–2014. Sci Rep 14, 28503 (2024). https://doi.org/10.1038/s41598-024-78382-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-78382-7