Abstract
Hashimoto’s thyroiditis (HT) is an autoimmune disease, characterized by abnormal elevation in thyroid peroxidase antibody (TPO-Ab) and/or thyroglobulin antibody (TG-Ab). Patients have multiple symptoms despite adequate hormone substitution. In the present study, we aimed to quantify the relationship between thyroid antibodies and multiple symptoms, inflammation and health-related life quality. A total of 108 HT patients with clinical euthyroid status and 57 heathy controls were recruited. Clinical parameters were determined by laboratory examination, and the symptoms burden and life quality were obtained by a Hashimoto’s Thyroiditis Symptom Questionnaire and a SF-36 Questionnaire, respectively. Compared with healthy controls, multiple extrathyroidal symptoms were significantly more serious in HT patients despite euthyroid status, mainly including that related to digestive system (abdominal distension, constipation and diarrhea), endocrine system (chilliness, gain weight and facial edema), neuropsychiatric system (forgetfulness, anxiety, depressed, fatigue, insomnia, irritability, and indifferent) and mucocutaneous system (dry skin, pruritus, and hair loss). Furthermore, serum TPO-Ab and TG-Ab were both inversely correlated with health-related life quality of general health and vitality parameters, and positively correlated with pro-inflammatory factors of TNF-α and IFN-γ, as well as severity of abdominal distension, diarrhea, chilliness, forgetfulness and fatigue. Moreover, TG-Ab level was positively associated with depressed, insomnia and indifferent. HT patients suffered from a variety of symptoms, and the elevated thyroid antibodies were inversely associated with health-related life quality and positively associated with inflammation and multiple extrathyroidal symptoms.
Similar content being viewed by others
Introduction
Hashimoto’s thyroiditis (HT), also known as chronic lymphocytic thyroiditis, is one of the most common autoimmune disease worldwide1. It is diagnosed according to the presence of hypoechogenic structure of the thyroid gland in the ultrasonography, and elevated serum concentration of thyroglobulin antibody (TG-Ab) and/or thyroid peroxidase antibody (TPO-Ab)2. Women are more susceptible to the disease than men, with 7–10 times of incidence rate3. As the mistaken attacks on thyroid gland from body’s self-immune system, the thyroid parenchyma is infiltrated with lymphocytes, which can eventually lead to hypothyroidism4,5. Patients with hypothyroidism are usually treated with L-thyroxine (L-T4) replacement therapy, to restore normal levels of thyroid hormone (FT3 and FT4) and thyroid-stimulating hormone (TSH)6. However, no specific treatment exits to improve the immune dysfunction in HT patients and prevent further development of Hashimoto disease.
Patients with HT often report multiple symptoms, such as profound fatigue, memory loss, poor sleep quality, muscle and joint tenderness, dry eyes, and forgetfulness7,8,9. Some symptoms can be relieved by adequate thyroid hormone substitution, while some are persistent despite patients’ euthyroid status9. The persistent symptoms are hypothesized to be associated with autoimmune disease, rather than hypothyroidism10. However, to date, the evidences directly demonstrating the association between abnormally elevated thyroid antibodies in HT patients and their extrathyroidal manifestations are still limited.
Thus, in the present study, the clinical parameters, multiple symptoms and life quality were determined in HT patients who were kept in euthyroid status, as well as in healthy controls. In addition, the association between thyroid antibodies (TPO-Ab and TG-Ab) and inflammatory factors, multiple symptoms and life quality was analyzed to investigate the influence of elevated thyroid antibodies on HT patients.
Methods
Study design and population
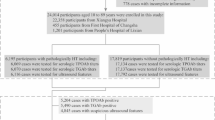
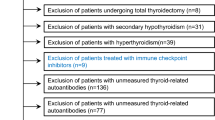
A total of 108 patients with Hashimoto’s thyroiditis and 57 healthy subjects were enrolled for the present study. Among them, 51 HT patients and 22 healthy participants were recruited at Affiliated Hospital of Qingdao University in northern China, and the others were recruited at Zhejiang Chinese Medical University in southern China. The study protocol was approved by the Ethics Committee of Qingdao University (Approval Number: QDU-20201107-1). All methods were performed in accordance with relevant guidelines and regulations, as well as the Declaration of Helsinki. Written informed consent has been provided by each participant.
Key inclusion criteria for HT patients were as follows: (a) age between 18–60 years old; (b) diagnosed by at least one endocrinologist according to clinical parameters and color ultrasonography; (c) positive TG-Ab or positive TPO-Ab while in euthyroid status without hormone substitution. The healthy controls were recruited at the physical examination centers of Zhejiang Hospital and Affiliated Hospital of Qingdao University through a health-check program. The main inclusion criteria for the control group were: (a) do not suffer from any type of thyroid disease, such as goiter, hyperthyroidism, hypothyroidism and thyroid tumor; (b) match the age and gender with the patients. Key exclusion criteria, for both groups, included: (a) pregnancy or lactation; (b) alcohol addiction; (c) with other kind of autoimmune disease, such as rheumatoid arthritis or multiple sclerosis; (d) with serious chronic diseases, such as cancer or heart disease; (e) use of anti-inflammatories or immunosuppressant drugs. Demographic data of patients and healthy subjects were obtained with a face-to-face interview. Each participant provided written informed consent and received no financial compensation or gifts.
Blood collection and assessment of biochemical indicators
Fasting blood from participants were centrifuged with 3000 rpm in 4 °C for 10 min to separate serum and erythrocytes. Serum levels of TPO-Ab, TG-Ab, TSH, FT3 and FT4 were determined by chemiluminescent immunoassays (Siemens Healthcare Diagnostics, Munich, Germany). The levels of interleukin (IL)-4, IL-6, IL-10, IL-17A, tumor necrosis factor (TNF)-α and interferon (IFN)-γ were determined by a flow cytometer (BD Biosciences, Franklin Lakes, USA). Serum biomarkers of liver and kidney function and lipid profiles were measured with an automatic analyzer (HITACHI 7020, Sysmex Kobe, Japan). T lymphocyte subpopulations were measured with blood samples by a flow cytometry (BD, USA). Laboratory assays were performed in duplicate to minimize analytical errors, and the presented values are the average of two measurements. All measurements were performed at the end of the study to minimize variability.
Survey of health-related life quality and severity of non-hypothyroid symptom
Health-related life quality was determined with Short Form 36 Health Survey (SF-36), which is made up of 36 questions11. The SF-36 has 8 domains: physical functioning, role physical, role emotional, bodily pain, general health, vitality, mental health and social functioning. The obtained score was transferred as (obtained score—the lowest possible score of the ___domain) / the difference between the highest possible score and the lowest possible score of the ___domain] × 100, so that the score of each ___domain is within (0,100) and comparably reflects health-related life quality. The higher of the score in each ___domain, the better of health status7,12.
Severity of multiple extrathyroidal manifestations was determined with the Hashimoto’s Thyroiditis Symptom Questionnaire. It has 8 domains, related to digestive, respiratory, circulatory, endocrine, neuropsychiatric, movement, reproductive and mucocutaneous system, respectively. Totally, the questionnaire is made up of 49 items, each of which need to be answered with score from 0 to 10 (0 means no symptom, 10 means the symptom seriously affect life quality).
Statistical analysis
Data are described as means ± standard deviations for normally distributed variables, as medians (interquartile ranges) for non-normally distributed variables, and as counts (percentages) for categorical variables. The difference between groups was analyzed by unpaired t test, Mann–Whitney U test and chi-square test, respectively. The correlation between thyroid antibodies and various symptoms as well as health-related quality of life was analyzed using Spearman’s correlation test, with adjustment for age, BMI, marriage, and family history of HT. To control for potential Type I errors due to multiple comparisons, the Benjamini–Hochberg procedure was applied to adjust the p-values, thereby controlling the false discovery rate. P < 0.05 was considered statistically significant, and all analyses were performed with the SPSS version 27.0.
The sample size calculation was based on the formula: \(n=\frac{{Z}_{crit}^{2}p\left(1-p\right)}{{e}^{2}}\)13, where Zcrit is 1.96 for a 5% level of significance in two-sided tests, p represents the estimate of the prevalence rate, and e denotes the margin of error. According to previous studies, the prevalence of Hashimoto’s thyroiditis is approximately 7.5%14. With a tolerable error set at 5%, at least 106 patients with Hashimoto’s thyroiditis were required. Healthy subjects were matched to cases using a 2:1 case-to-control ratio.
Results
Characteristics of participants
Demographic data of participants are shown in Table 1. There was no significant difference between HT patients and healthy subjects in age, gender, body mass index, smoking and drinking. The proportion of married people in HT group was significantly higher than that in healthy controls. Subjects with family history of HT in HT group were more than that in control group.
Clinical parameters of participants are shown in Table 2. Without thyroid hormone substitution, parameters related to thyroid function (FT3, FT4 and TSH) of HT patients were similar with healthy controls, only TPO-Ab and TG-Ab in HT group were remarkably higher than that in control group. In addition, lipid metabolism biomarkers (TC and LDL-C), pro-inflammatory factors (TNF-α and IFN-γ), hepatic function index (AST, TP and ALB) and hsCRP levels were significantly increased in HT patients compared with healthy controls, while all of them were still within normal ranges.
Survey of health-related life quality and severity of non-hypothyroid symptom
Health-related life quality was significantly decreased in HT patients compared with healthy controls, especially in terms of general health, vitality, bodily pain, social functioning and mental health (Table 3). Furthermore, despite patients’ euthyroid status, multiple symptoms were still much more serious in HT patients than in healthy controls, including the symptoms related to digestive system (abdominal distension, constipation, and diarrhea), circulatory system (chest tightness), endocrine system (chilliness, gain weight, and facial edema), neuropsychiatric system (forgetfulness, anxiety, depressed, fatigue, insomnia, irritability, and indifferent), movement system (joint pain and swelling) and mucocutaneous system (dry skin, pruritus, and hair loss) (Table 4).
The correlation between TPO-Ab and health-related life quality, inflammatory factors and multiple symptoms
The results of correlation analysis showed serum TPO-Ab was inversely correlated with general health score, and vitality score (Fig. 1A, B, Supplement Table 1), and was positively correlated with TNF-α, and IFN-γ (Fig. 2A, B, Supplement Table 2), and severity of symptoms related to endocrine system, neuropsychiatric system, and movement system (Fig. 3A-C). In detail, with the increase of serum TPO-Ab, symptoms of abdominal distension, diarrhea, chilliness, facial edema, forgetfulness, swelling, gain weight, and dry skin were more serious, while menorrhagia was alleviated (Fig. 4A-I, Supplement Table 3).
The correlation between thyroid antibodies and the 36-Item Short Form Health Survey scores. (A, B): Serum TPO-Ab levels and general health and vitality scores. (C-F): Serum TG-Ab levels and bodily pain, general health, vitality, and social functioning scores. Abbreviations: TPO-Ab, thyroid peroxidase antibody; TG-Ab, thyroglobulin antibody.
The correlation between thyroid antibodies and inflammatory factors. (A, B): Serum TPO-Ab levels and TNF-α and IFN-γ. (C, D): Serum TG-Ab levels and TNF-α and IFN-γ. Abbreviations: TPO-Ab, thyroid peroxidase antibody; TG-Ab, thyroglobulin antibody; IFN-γ, interferon-γ; TNF-α, tumor necrosis factor-α.
The correlation between thyroid antibodies and systematic symptom scores. (A-C): Serum TPO-Ab levels and endocrine system symptom scores, neuropsychiatric system symptom scores, and movement system symptom scores. (D-H): Serum TG-Ab levels and endocrine system symptom scores, neuropsychiatric system symptom scores, mucocutaneous system symptom scores, digestive system scores, movement system scores. Abbreviations: TPO-Ab, thyroid peroxidase antibody; TG-Ab, thyroglobulin antibody.
The correlation between TG-Ab and health-related life quality, inflammatory factors and multiple symptoms
Correlation analysis showed serum TG-Ab level was inversely correlated with scores of bodily pain, general health, vitality, and social functioning (Fig. 1C-F, Supplement Table 1), and was positively correlated with TNF-α, and IFN-γ (Fig. 2C-D, Supplement Table 2), and severity of symptoms related to endocrine system, neuropsychiatric system, mucocutaneous system, digestive system, and movement system (Fig. 3D-H). In detail, with the increase of serum TG-Ab, symptoms of abdominal distension, diarrhea, chilliness, gain weight, forgetfulness, depressed, fatigue, insomnia, and indifferent were more serious (Fig. 5A-I, Supplement Table 3).
Discussion
To the best of our knowledge, this is the first study to quantify the relationship between thyroid antibodies (TPO-Ab and TG-Ab) and inflammatory factors, health-related life quality, as well as multiple symptoms in Hashimoto’s thyroiditis patients. We found that both serum TPO-Ab and TG-Ab were inversely associated with life quality and positively associated with various extrathyroidal symptoms and inflammation, even though all the patients were in euthyroid status without hormone substitution.
It has been reported that common symptoms accompanied with HT patients typically included chronic fatigue, dry hair, dysphagia, irritability, and nervousness8,15,16. Clinically, there are still many other symptoms reported by HT patients, even when they were in euthyroid status. However, their relationships with Hashimoto disease have not been confirmed. In the present study, we used the Hashimoto’s Thyroiditis Symptom Questionnaire containing 49 items, which included more detailed symptoms related to digestive, respiratory, circulatory, endocrine, neuropsychiatric, movement, reproductive and mucocutaneous system. The results showed that symptoms of abdominal distension, constipation and diarrhea that related to digestive system, as well as symptoms of forgetfulness, anxiety, depressed, fatigue, insomnia, multiple dreams, irritability and indifferent that related to neuropsychiatric system, were significantly more serious than healthy controls. These findings provided us more comprehensive information about symptoms of HT patients, and also provided guidance for clinician to diagnose the etiology of these extrathyroidal symptoms. Furthermore, due to the euthyroid status of all enrolled participants, these findings also confirmed that these symptoms were caused by autoimmune disease, rather than hypothyroidism.
The precise mechanism of various extrathyroidal symptoms in HT patients was uncertain, but likely associated with elevated TPO-Ab17. It has been proposed that positive TPO-Ab may result in cross-reaction with other tissues, as activated TPO-Ab-producing lymphocytes may leave the thyroid gland and invade other distant tissue, contributing to extrathyroidal symptoms and inflammation18,19. Furthermore, clearance of TPO-Ab always occurs in parallel with a decline in other immunologic mediators20. A previous study has demonstrated that intervention of both levothyroxine and selenomethionine on HT patients for 6 months significantly reduced serum TPO-Ab titers, as well as decreased levels of IFN-γ, TNF-α, IL-1β, IL-2 and high sensitivity C-reactive protein (hsCRP) by about 50%21. Of interest, our study showed that levels of IFN-γ, TNF-α and hsCRP were higher in HT patients than in healthy controls, and increase of IFN-γ and TNF-α were both associated with higher TPO-Ab. Thus, the reduction in serum TPO-Ab is probably a surrogate marker for the modification of the systemic inflammation and extrathyroidal symptoms. In addition, our results also showed that TG-Ab was comparable with TPO-Ab when it come to their relationship with aforementioned proinflammatory factors. However, even though TG-Ab has been known to be associated with HT, its potential function as a predictive marker for inflammation and extrathyroidal symptoms is relatively unexplored.
The symptoms that had been proved to be associated with higher serum TPO-Ab level primarily included fatigue, dry skin, arthralgia, irritability and nervousness22,23. A randomized trial in Norway has showed that normalization of serum TPO-Ab titers of HT patients by total thyroidectomy significantly relieved extrathyroidal symptom burden, especially fatigue, and improved health-related life quality7. However, to date, limited study has given attention to intestinal symptoms in HT patients, let alone its relationship with TPO-Ab. The present study firstly found that abdominal distension, constipation and diarrhea were more serious in HT patients, and both TPO-Ab and TG-Ab were positively associated with severity of abdominal distension and diarrhea, indicating a possibility that reducing serum TPO-Ab and TG-Ab may be an effective way to modify these intestinal symptoms.
Intestinal leakage has been proposed to be an essential condition for the occurrence and development of autoimmune disease24,25,26. Several studies have demonstrated that the leaky gut promotes inflammatory cytokines release, and the latter aggravate an increased intestinal permeability27,28. This vicious circle favors the activation of adaptive and innate immunity in the gut mucosa, and can induce a tolerance breakdown. The activated immune cells may remain in the gut mucosa, or migrate to distant organs, participating in chronic inflammatory and resulting in autoimmune diseases, such as HT29. Furthermore, both abdominal distension and diarrhea are the main common symptoms of intestinal leakage30. Thus, abdominal distension and diarrhea seemed to be unescapable symptoms of Hashimoto disease. However, their close relationship has always been overlooked. The serious intestinal symptoms reported by HT patients in the present study confirmed the assumption, and raised a possibility that both the intestinal symptoms and HT could be cured from the perspective of improving the leaky gut.
In addition, we also found that TPO-Ab and TG-Ab were positively associated with severity of multiple other symptoms related to neuropsychiatric system, such as forgetfulness, depressed, fatigue, insomnia and indifferent. Except fatigue, the relationship between the other symptoms and thyroid antibodies were reported for the first time in this study. However, the mechanisms were uncertain and warranted further investigation.
As the heavy symptom load in HT patients and its positive correlation with thyroid antibodies, it is not a surprise that higher levels of TPO-Ab and TG-Ab were also associated with decreased health-related life quality. For various health parameters in SF-36 questionnaire, bodily pain, general health, vitality, social functioning and mental health were significantly affected by the HT disease. Furthermore, TPO-Ab and TG-Ab were both inversely associated with general health and vitality scores. Obviously, these results reflected an altered health perception of HT patients and may be due to the higher symptom burden.
Strengths of the present study include the study design, where all cases are kept at euthyroid status, thus the observed difference was free of hypothyroidism. Furthermore, not only TPO-Ab, we also paid close attention to TG-Ab, which has been known to be associated with HT, but was seldom involved in other relevant studies. Several limitations also should be noted. First, the present study cannot demonstrate the causal relationship between increased thyroid antibodies and pro-inflammatory factors, as well as multiple symptoms. For example, we observed multiple symptoms related to neuropsychiatric system in HT patients, such as anxiety, depressed, insomnia and irritability, but not sure whether these symptoms were the cause or result of HT disease. Second, the sample size in the study was relatively small, even though this was a multicenter study, which represented participants from both northern and southern China. Future prospective studies with large sample size are still needed. Third, the use of a Likert scale to evaluate specific symptoms, such as diarrhea, asthma and bradycardia, may potentially overstate the significance of certain findings, as the ordinal nature of Likert data may not accurately capture the true intensity of symptoms. Therefore, results from symptom ratings should be interpreted with caution, considering these potential sources of inaccuracy.
In conclusion, the present study demonstrated that HT patients were accompanied with multiple symptoms, especially those related to intestine and mood, even though they were in a euthyroid state. Furthermore, TPO-Ab and TG-Ab levels were inversely associated with general health and vitality scores, and positively associated with pro-inflammatory factors, as well as severity of several intestinal and psychiatric symptoms. These results highlight the symptoms burden that HT patients are suffering from, and are of great significance as they shed light on the clinical picture of HT. Future research that aiming to explore the causes of Hashimoto disease, or develop treatment strategies to decrease antibodies of HT patients is sorely needed.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- HT:
-
Hashimoto’s thyroiditis
- TPO-Ab:
-
Thyroid peroxidase antibody
- TG-Ab:
-
Thyroglobulin antibody
- LT-4:
-
L-thyroxine
- TSH:
-
Thyroid-stimulating hormone
- IL:
-
Interleukin
- TNF:
-
Tumor necrosis factor
- IFN:
-
Interferon
- SF-36:
-
Short Form 36 Health Survey
References
McLeod, D. S. A. & Cooper, D. S. The incidence and prevalence of thyroid autoimmunity. Endocrine 42(2), 252–265 (2012).
Karanikas, G. et al. Relation of anti-TPO autoantibody titre and T-lymphocyte cytokine production patterns in Hashimoto’s thyroiditis. Clin. Endocrinol. 63(2), 191–196 (2005).
Klubo-Gwiezdzinska, J., Wartofsky, L. Hashimoto thyroiditis: an evidence-based guide to etiology, diagnosis and treatment. Pol. Arch. Intern. Med. 132(3) (2022).
Dayan, C. M., Daniels, G. H. Chronic autoimmune thyroiditis. N. Engl. J. Med. 335(2) (1996).
Pearce, E. N., Farwell, A. P. & Braverman, L. E. Thyroiditis. N. Engl. J. Med. 348(26), 2646–2655 (2003).
Sharma, R., Theiler-Schwetz, V., Trummer, C., Pilz, S., Reichhartinger, M. Automatic levothyroxine dosing algorithm for patients suffering from Hashimoto’s thyroiditis. Bioengineering 10(6) (2023).
Guldvog, I. et al. Thyroidectomy versus medical management for euthyroid patients with Hashimoto disease and persisting symptoms: A randomized trial. Ann. Intern. Med. 170(7), 453–464 (2019).
Ott, J. et al. Hashimoto’s thyroiditis affects symptom load and quality of life unrelated to hypothyroidism: A prospective case-control study in women undergoing thyroidectomy for benign goiter. Thyroid 21(2), 161–167 (2011).
Harris, E. Thyroidectomy for persistent Hashimoto disease symptoms. JAMA 330(24), 2331 (2023).
Milo, T., Korem Kohanim, Y., Toledano, Y. & Alon, U. Autoimmune thyroid diseases as a cost of physiological autoimmune surveillance. Trends Immunol. 44(5), 365–371 (2023).
Winther, K. H. et al. Disease-specific as well as generic quality of life is widely impacted in autoimmune hypothyroidism and improves during the first six months of levothyroxine therapy. PLoS One 11(6), e0156925 (2016).
Hedman, C., Djärv, T., Strang, P. & Lundgren, C. I. Effect of thyroid-related symptoms on long-term quality of life in patients with differentiated thyroid carcinoma: A population-based study in Sweden. Thyroid 27(8), 1034–1042 (2017).
Wang, X. & Ji, X. Sample size estimation in clinical research: From randomized controlled trials to observational studies. Chest. 158(1S), S12–S20 (2020).
Hu, X. et al. Global prevalence and epidemiological trends of Hashimoto’s thyroiditis in adults: A systematic review and meta-analysis. Front. Public Health 10, 1020709 (2022).
Yuan, J. et al. Local symptoms of Hashimoto’s thyroiditis: A systematic review. Front. Endocrinol. 13, 1076793 (2022).
Martino, G. et al. Alexithymia, emotional distress, and perceived quality of life in patients with Hashimoto’s thyroiditis. Front. Psychol. 12, 667237 (2021).
Du Puy, R. S. et al. Associations of elevated antithyroperoxidase antibodies with thyroid function, survival, functioning, and depressive symptoms in the oldest old: The Leiden 85-plus study. Thyroid 29(9), 1201–1208 (2019).
Mikoś, H., Mikoś, M., Obara-Moszyńska, M. & Niedziela, M. The role of the immune system and cytokines involved in the pathogenesis of autoimmune thyroid disease (AITD). Endokrynol. Pol. 65(2), 150–155 (2014).
Kristensen, B. Regulatory B and T cell responses in patients with autoimmune thyroid disease and healthy controls. Dan Med. J. 63(2) (2016).
Rostami, R., Aghasi, M. R., Mohammadi, A. & Nourooz-Zadeh, J. Enhanced oxidative stress in Hashimoto’s thyroiditis: Inter-relationships to biomarkers of thyroid function. Clin Biochem. 46(4–5), 308–312 (2013).
Krysiak, R. & Okopien, B. The effect of levothyroxine and selenomethionine on lymphocyte and monocyte cytokine release in women with Hashimoto’s thyroiditis. J. Clin. Endocrinol. Metab. 96(7), 2206–2215 (2011).
Groenewegen, K. L., Mooij, C. F. & van Trotsenburg, A. S. P. Persisting symptoms in patients with Hashimoto’s disease despite normal thyroid hormone levels: Does thyroid autoimmunity play a role? A systematic review. J. Transl. Autoimmun. 4, 100101 (2021).
van Zuuren, E. J., Albusta, A. Y., Fedorowicz, Z., Carter, B. & Pijl, H. Selenium supplementation for Hashimoto’s thyroiditis. Cochrane Database Syst. Rev. 6, CD010223 (2013).
Lin, H. et al. Polymeric immunoglobulin receptor deficiency exacerbates autoimmune hepatitis by inducing intestinal dysbiosis and barrier dysfunction. Cell Death Dis. 14(1), 68 (2023).
Ma, L. & Morel, L. Loss of gut barrier integrity in lupus. Front. Immunol. 13, 919792 (2022).
Camilleri, M. Leaky gut: Mechanisms, measurement and clinical implications in humans. Gut 68(8), 1516–1526 (2019).
Fasano, A. Zonulin and its regulation of intestinal barrier function: The biological door to inflammation, autoimmunity, and cancer. Physiol. Rev. 91(1), 151–175 (2011).
Hiippala, K., Jouhten, H., Ronkainen, A., Hartikainen, A., Kainulainen, V., Jalanka, J. et al. The potential of gut commensals in reinforcing intestinal barrier function and alleviating inflammation. Nutrients 10(8) (2018).
Zheng, H. et al. A Global regulatory network for dysregulated gene expression and abnormal metabolic signaling in immune cells in the microenvironment of graves’ disease and Hashimoto’s thyroiditis. Front. Immunol. 13, 879824 (2022).
Romero-Calvo, I. et al. Intestinal inflammation and the enterocyte transportome. Biochem. Soc. Trans. 39(4), 1096–1101 (2011).
Funding
This work was supported by the National Natural Science Foundation of China (NSFC: 82103843, 82273625 & 81973041); Natural Science Foundation of Zhejiang Province (ZCLY24H2602) and Zhejiang Provincial Xinmiao Talents Program (2024R410B062).
Author information
Authors and Affiliations
Contributions
J.L. and D.L. conceived and designed the study; J.L., Q.H., S.S., X.W., CS., and S.F. collected the blood samples in hospital; Q.H., K.P., Y.Z., K.Z. and Y.W. conducted the laboratory work; Q.H., and K.P. collected the questionnaire; S.S., Y.Z., K.Z. and Y.W. analyzed the data; J.L. and Q.H. drafted the initial manuscript; Q.H., S.F. and S.L. critically reviewed the manuscript; and all authors approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study protocol was approved by the Ethics Committee of Qingdao University (Approval Number: QDU-20201107-1). Written informed consent has been provided by each participant.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, J., Huang, Q., Sun, S. et al. Thyroid antibodies in Hashimoto’s thyroiditis patients are positively associated with inflammation and multiple symptoms. Sci Rep 14, 27902 (2024). https://doi.org/10.1038/s41598-024-78938-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-78938-7