Abstract
After ending the three-year zero COVID policy in China, the epidemiology of other respiratory pathogens has been affected. This study aimed to characterize of common respiratory pathogen infections in pediatric patients hospitalized for acute respiratory tract infections (ARTIs) in Suzhou before and after ending the zero COVID policy. Nasopharyngeal aspirates (NPAs) were obtained from children with ARTIs (aged ≤ 16 years) at the Children’s Hospital of Soochow University for the detection of respiratory syncytial virus (RSV), influenza A (FluA), FluB, human parainfluenza virus (HPIV), adenovirus (ADV), human rhinovirus (HRV), bocavirus (BoV), human metapneumovirus (HMPV), and mycoplasma pneumoniae (MP). The data were compared between two periods: January 2020 to December 2022 (before ending the zero COVID policy) and January 2023 to May 2024 (after ending the zero COVID policy). Patients were divided into four groups: 0–2, ≥ 3–5, ≥ 6–10, and ≥ 11–16 years. A total of 42,379 patients were enrolled and the top four pathogens identified were MP, HRV, RSV and HPIV with positive rates of 20.2%, 19.5%, 15.1%, and 6.9%, respectively. A total of 28,352 positive cases were detected, with positive rates of 54.0% (n = 11,850/21,941) and 80.7% (n = 16,502/20,438) before and after ending the zero COVID policy, respectively. Total RSV, HRV, HPIV, and MP positivity increased by 27.8%, 39.0%, 12.3%, and 322.7%, respectively, after ending the zero COVID policy compared to positivity before the policy. After ending the zero COVID policy, the positive rates of RSV, HRV, and HPIV increased most in children aged 0–2 years, with increases by 88.8% (OR: 2.3, 95% CI: 2.2–2.5), 50.0% (OR: 1.6, 95% CI: 1.5–1.7), and 69.6% (OR: 1.8, 95% CI: 1.6-2.0), respectively. The greatest increase in MP positivity was 316.9% in the 3–5 years (OR: 5.5, 95% CI: 4.9–6.1). After ending the zero COVID policy, the RSV-positive rate increased most in summer, while HRV was predominantly circulated in spring and the MP-positive rate peaked in autumn. Ending the zero COVID policy facilitated the transmission of common respiratory pathogens in children. Post-pandemic surveillance and control of respiratory pathogens must be strengthened to reduce health risks.
Similar content being viewed by others
Introduction
During the coronavirus disease 2019 (COVID-19) pandemic, China enforced a stringent “zero COVID policy”, characterized by extensive lockdowns and rigorous social distancing measures1. Against the backdrop of evolving global pandemic dynamics and the rising domestic vaccination rates in China, the government announced on December 27, 2022, a shift away from this policy towards a more adaptable public health strategy2. Such a 3-year public health restriction had never been imposed in China before. The implementation of the zero COVID policy has not only effectively limited the spread of COVID-19, but has also significantly reduced the spread of airborne or faecal-oral infectious diseases such as the common cold, gastroenteritis and bronchiolitis3,4. These changes may arise from the ecological competition between severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and other respiratory pathogens, and more likely resulting from improved community hygiene practices such as mask use, social distancing and disinfection5.
Acute respiratory tract infections (ARTIs) pose a significant health burden on children, as evidenced by the elevated rates of hospitalization and mortality6. The symptoms of ARTIs typically manifest as inflammation and damage to the upper and lower respiratory tract, and the immune system’s response tends to exacerbate airway inflammation and allergic reactions7,8. In severe cases, patients may develop systemic symptoms and other complications9,10,11. Most ARTIs are caused by respiratory pathogens. A study of nasopharyngeal swab specimens from 4956 children with ARTIs during the 3 years of the COVID-19 pandemic in Kunming, China, found that bocavirus (BoV), human parainfluenza virus (HPIV) and respiratory syncytial virus (RSV) were the predominant respiratory viruses in children aged 3 ≤ years, mycoplasma pneumoniae (MP) was the predominant respiratory pathogen in children aged > 3 years, and human rhinovirus (HRV) had the highest prevalence and was predominant in mixed infections12. A nationwide prospective study in China showed a viral positive rate of 46.9% in children under 5 years of age and school-aged children. The top three viral pathogens identified were influenza virus, RSV and HRV13. In addition, MP is one of the main causes of community-acquired pneumonia14. The introduction of non-pharmaceutical interventions (NPIs) targeting COVID-19 has led to a significant decline in the global detection rate of MP and a delay in the prevalence of MP in many countries after the end of COVID-1915.
The prolonged implementation of social distancing measures during the pandemic has resulted in inadequate natural immunity of children to common respiratory pathogens, which compromises their ability to combat pathogens like RSV, leading to a surge in cases16,17. This phenomenon, termed as “immunity debt”, underscores the vulnerability of children to certain pathogens after prolonged isolation18,19. Previous result from our research group showed a significant increase in RSV infection rates in children aged 2–4 years after the pandemic, coinciding with an increase in RSV-related mortality and a decrease in intensive care unit (ICU) admissions20. In addition, it is plausible that pandemic-related restrictions have contributed to diminished antibody levels against RSV in children, which has potentially fueled the surge in RSV cases21.
The resurgence of respiratory pathogens after the COVID-19 pandemic has received considerable attention. In this study, the prevalence of common respiratory pathogens in children with ARTIs after ending of the zero COVID policy (January 2023 to May 2024) in Suzhou, China was examined and compared with the data collected before ending the zero COVID policy (January 2020 to December 2022).
Materials and methods
Research object
In this retrospective study, data were collected from pediatric patients aged ≤ 16 years who were diagnosed with ARTIs and hospitalized at the Children’s Hospital of Soochow University from January 2020 to May 2024. ARTIs in children were diagnosed by experienced physicians based on the Diagnostic Criteria for Hospital-acquired Infections ([2001] 2) issued by the Chinese Ministry of Health. To ensure data accuracy, stringent exclusion criteria were implemented in the study; thus, patients with multiple clinic visits in the past week, those receiving immunosuppressive therapy, and those with hospital-acquired infections, COVID-19 infection, hematologic cancers, chronic infectious diseases, or severe malnutrition were excluded. The patients were assigned to four groups: under 2 years of age (0–2 years), 3–5 years of age (≥ 3–5 years), 6–10 years of age (≥ 6–10 years), and 11–16 years of age (≥ 11–16 years). The demographics and etiology of all pediatric patients were retrospectively analyzed.
Surveillance of common respiratory pathogens
Nasopharyngeal aspirates (NPAs) were obtained within 24 h of the patient’s admission to hospital by trained staff using aseptic negative pressure according to standard operating procedures. A sterile plastic suction tube was inserted into the patient’s nasal cavity to a depth of 7–8 cm, and 1–2 mL of secretions were aspirated. The real time reverse transcription-PCR (RT-PCR) method has been widely used for the detection of respiratory pathogens due to its high sensitivity22. Instruments used for the detection of respiratory pathogens included an Applied Biosystems 3500 Dx analyser (Thermo Fisher Scientific, USA) and an A300 thermal cycle PCR instrument (Hangzhou LongGene Scientific Instruments Co, Ltd, China). A Multiplex real time RT-PCR assay using Taqman probes (X-ABT, Beijing, China) was used to detect nine respiratory pathogens: RSV, influenza A (FluA), FluB, HPIV, adenovirus (ADV), HRV, BoV, human metapneumovirus (HMPV), and MP. The programme was 45 °C for 10 min, 95 °C for 5 min and the 45 cycles of 95 °C for 15s and 60 °C for 45s. The test results were interpreted according to the instructions of the manufacturer’s test kit. The number of positive cases for these pathogens and the corresponding number of hospitalizations for ARTIs were carefully recorded daily.
Ethical approval
The study protocol was approved and waived informed consent by the Medical Ethics Committee of the Children’s Hospital of Soochow University (2013002). The study was conducted in accordance with relevant guidelines and regulations.
Statistical analysis
Chi-square, Fisher’s exact test are statistical methods for analyzing categorical data, especially comparing differences in proportions between two or more categories23. Binary logistic regression is a method for investigating the effect of independent variable(s) on a dichotomous dependent variable. In this study, categorical variables were represented as numbers (proportions), and the categorical data were analyzed using either Chi-square test or Fisher’s exact test. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated using univariate binary logistic regression. The proportion of tests positive for respiratory pathogens after ending the zero COVID policy was compared with the average level before ending the zero COVID policy by calculating the percentage change as follows:
Where, Pbefore represents the average positive rate before ending the zero COVID policy, while Pafter denotes the average positive rate after ending the zero COVID policy.
Based on the monthly positive cases from 2020 to 2022, a time series analysis was conducted to predict the monthly positive cases for 2023–2024, along with their corresponding 95% CIs. Linear models were used based on the observed patterns of change in counts prior to 2023 and the associated model fit indices. The observed and expected numbers for 2023–2024 were compared by calculating the percentage difference between these 2 numbers using the following equation:
All analyses were performed using SPSS 27.0 (SPSS Inc., Chicago, IL, USA), OriginPro 2021 (OriginLab Corporation, Northampton, MA, USA), and GraphPad Prism 9 (GraphPad Software, San Diego, CA). A two-sided P < 0.05 was considered statistically significant.
Results
The prevalence of respiratory pathogens among children after ending the zero COVID policy
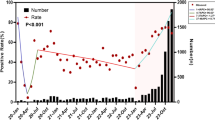
After China implemented a national lockdown on January 24, 2020, there was a significant decrease in the number of ARTIs and the positive rate of total respiratory pathogens. As lockdown measures were gradually relaxed, the number of ARTI cases began to increase. From February to June 2022, Suzhou, China experienced a second wave of COVID-19, leading to another significant decrease in the number of ARTI cases and the positive rate of total respiratory pathogens. On December 27, 2022, China ended its zero COVID policy, leading to a rapid nationwide outbreak of COVID-1924. During this period, people were mainly isolated and treated at home. After that, people’s daily activities largely returned to pre-epidemic patterns. After ending the zero COVID policy, there was a marked upward trend in the number of ARTI cases and the positive rate for total respiratory pathogens, with particularly high levels persisting after March 2023 (Fig. 1).
Characteristics of children with ARTIs
A total of 42,379 children diagnosed with ARTIs were enrolled in the study between January 2020 and May 2024. Of these children, 21,941 cases (51.8%) were diagnosed before ending the zero COVID policy, and 20,438 cases (48.2%) were diagnosed after ending the zero COVID policy (Table 1). Before and after ending the zero COVID policy, the number of boys with ARTIs was 12,642 (57.6%) and 10,958 (53.6%), respectively, with a significant difference (P < 0.05). After ending the zero COVID policy, the number of ARTIs among children aged 0–2 and 3–5 years decreased, whereas that among children aged 6–10 and 11–16 years increased compared to pre-policy levels (P < 0.05). There was a statistically significant increase in the number of children with ARTIs who had fever, cough and wheezing (clinical symptoms) after ending the zero COVID policy (P < 0.05). Overall, the incidence of ARTIs was highest in winter (28.4%) and lowest in summer (20.1%). Compared with the data before ending the zero COVID policy, the incidence of ARTIs increased in spring (before: 13.8% VS after: 36.2%) and decreased in summer (before: 22.2% VS after: 17.8%), autumn (before: 32.3% VS after: 21.2%) and winter (before: 31.7% VS after: 24.8%) after ending the zero COVID policy, with a significant difference (P < 0.05).
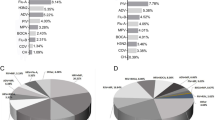
Overall detection of respiratory pathogens
A total of 42,379 NPAs from children with ARTIs were tested and 28,352 samples (66.9%) were found to be positive for respiratory pathogens. The top four pathogens detected were MP (13.3%), RSV (11.7%), HRV (11.1%), and HPIV (4.4%). The positive rate of mixed infections of pathogens was 13.6% (Fig. 2). As shown in Table 1, the positive rate of total positive cases was 54.0% (n = 11,850/21,941) and 80.7% (n = 16,502/20,438) before and after ending the zero COVID policy, respectively. There was a significant increase in the positive rates of RSV, FluA, FluB, HPIV, ADV, HRV, MP and cases of mixed infection after ending the zero COVID policy compared with before ending the zero COVID policy (P < 0.05) (Table 1; Fig. 3). After ending the zero COVID policy, the number of total positive cases increased sharply (Fig. 4A). From April to July 2020, no RSV cases were reported, and from May to November 2022, the number of RSV cases and the RSV positive rate remained low. The peak of RSV epidemic occurred from July to September 2023. No FluA cases were reported from February 2020 to April 2022. FluA outbreak occurred from February to April 2023. There were two short FluB epidemics in the winter and spring of 2021/2022 and 2023/2024. From January to August 2020 and from January to April 2023, few HPIV cases were reported, while other time periods showed fluctuations. The ADV positive rate is low from January 2020 to September 2023 and tends to rise after October 2023. HRV is the dominant pathogen in this study, accounting for 30.3% (3,594/11,850) and 28.2% (4,655/16,502) of total positive cases before and after ending the zero COVID policy, respectively. After 2023, the peak positive rate of BoV was lower than during the epidemic. The peak of HMPV epidemic occurred from July to December 2022. After ending the zero COVID policy, there was a significant increase in MP infections, with the positive rate accounting for 41.4% (6,829/16,502) of the total positive cases (Fig. 4B-J, Table 1). In addition, the co-infection of two or more pathogens increased after ending the zero COVID policy, with the co-infection rate of HRV and MP as high as 7.07% (Fig. 5).
Positive cases and infection rates of respiratory pathogens in hospitalized children with ARTIs from January 2020 to May 2024. (A) Total positive cases and infection rates for all respiratory pathogens; (B) Positive cases and infection rates of RSV; (C) Positive cases and infection rates of FluA; (D) Positive cases and infection rates of FluB; (E) Positive cases and infection rates of HPIV; (F) Positive cases and infection rates of ADV; (G) Positive cases and infection rates of HRV; (H) Positive cases and infection rates of BoV; (I) Positive cases and infection rates of HMPV; (J) Positive cases and infection rates of MP.
Comparison of the co-infection patterns before (A) and after (B) ending the zero COVID policy. Co-infection rates were calculated pairwise for pathogens 'X' and 'Y'. The numerator represents the number of patients co-infected with 'X' and 'Y', while the denominator includes the total number of patients tested for both 'X' and 'Y'.
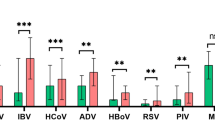
Age distribution of respiratory pathogens
Changes in the positive rates of respiratory pathogens among children of different age groups were further observed (Table 2). A noticeable increase in the positive rates of RSV, FluA, ADV, HRV, and MP along with a marked decrease in the positive rate of BoV was observed across all age groups after ending the zero COVID policy. We also looked at changes in positive rates for the four main respiratory pathogens: RSV, HRV, HPIV and MP, stratified by age (Fig. 6). The largest increase in the annual cumulative total positive rate was observed for MP, with an increased by 322.8% (from 7.9 to 33.4%, OR = 5.8, 95% CI: 5.5–6.2), followed by HRV with an increased by 39.0% (from 16.4 to 22.8%, OR = 1.5, 95% CI: 1.4–1.6), RSV with an increased by 27.8% (from 13.3 to 17.0%, OR = 1.3, 95% CI:1.2–1.4), and HPIV with an increased by 12.3% (from 6.5 to 7.3%, OR = 1.1, 95% CI: 1.0-1.2). For RSV, HRV, and HPIV, the cumulative increase were most significant in children aged 0–2 years, with increase of 88.8% (OR: 2.3, 95% CI:2.2–2.5), 50.0% (OR: 1.6, 95% CI: 1.5–1.7), and 69.6% (OR: 1.8, 95% CI:1.6-2.0), respectively. In particular, in children aged 3–5 years, the number of MP-positive cases increased from 484 to 1,616, and the positive rate for MP increased by 316.9% (from 7.1 to 29.6%, OR: 5.5, 95% CI: 4.9–6.1).
Seasonal distribution of respiratory pathogens
Suzhou is located in the south-eastern part of the Yangtze River Delta, which has four distinct seasons. For the purpose of this study, spring is considered to be from March to May, summer from June to September, autumn from September to December and winter from December of the current year to February of the following year. As shown in Table 3, the positive rate of total positive cases was higher in autumn compared to the other seasons, with 62.6% (n = 4,436/7,091) and 82.4% (n = 3,571/4,335) before and after ending the zero COVID policy, respectively. Figure 7 further illustrates that RSV had a higher positive rate (23.5%) in winter before ending the zero COVID policy and a higher positive rate (19.2%) in summer after ending the zero COVID policy. Before ending the zero COVID policy, the positive rate of HRV was significantly higher than that of other respiratory pathogens in spring, summer and autumn, and the peak of the positive rate (30.2%) of HRV occurred in spring after ending the zero COVID policy. The positive rate of MP was significantly higher than that of other respiratory pathogens in autumn and winter after ending the zero COVID policy, and the peak of the positivity rate occurred in autumn (52.8%).
Changes in absolute number of respiratory pathogen infections
Based on the historical average monthly number of respiratory pathogen infections from 2020 to 2022, the average monthly number of cases in 2023 and 2024 was projected (Table 4). In 2023, compared with expected counts, the monthly numbers of RSV, FluA, ADV, HRV, MP, and total positive cases increased by 123.1%, 855.4%, 128.8%, 46.7%, 446.9%, and 58.3%, respectively, whereas the monthly numbers of FluB, HPIV, BoV, and HMPV decreased by 55.2%, 4.9%, 44.8%, and 73.2%, respectively (P < 0.01). In 2024, compared with expected counts, the monthly numbers of RSV, FluA, FluB, HPIV, ADV, HRV, MP, and total positive cases increased by 217.9%, 161.6%, 287.0%, 2.7%, 934.3%, 99.2%, 280.1%, and 84.0%, respectively, while the monthly numbers of BoV and HMPV decreased by 83.0% and 30.3%, respectively (P < 0.01).
Discussion
On December 27, 2022, China decided to end the three-year zero COVID policy by stopping a series of NPIs, such as home isolation, strict mask wearing, working at home, maintaining social distance, etc. Residents have returned to their pre-epidemic activities for over a year, and many residents continue to maintain good hygiene habits, such as wearing masks in public places and maintaining hand hygiene. In this study, data from children with ARTIs admitted to the Children’s Hospital of Soochow University from January 2020 to May 2024 were retrospectively analyzed to comprehensively examine the changes in respiratory pathogens before and after ending the zero COVID policy. This study found that the positive rate for respiratory pathogens increased significantly to 80.7% after ending the zero COVID policy. It is interesting to note that the number of hospitalizations for ARTIs in children under 5 years of age decreased after the end of the zero COVID policy, but a high rate of respiratory pathogen positivity occurred. The outbreak of respiratory pathogens after the COVID-19 pandemic can be attributed to the strict implementation of the zero COVID policy, which destroyed the seasonal regularity of these pathogens. In addition, the “immunity debt” during the epidemic can have a negative impact, making people more susceptible to pathogens after the relaxation of public health control measures25. After pathogen infection, the immune system is activated to fight against pathogenic microorganisms26. Infants and young children rely mainly on a large amount of antibodies passively obtained from the mother to maintain their immunity27. In particular, the implementation of NPIs during the COVID-19 pandemic may have resulted in a more pronounced “immunity debt” for infants and young children born during the epidemic, who had less exposure to susceptible pathogens or less uptake of relevant vaccines. This may explain the increased susceptibility of younger age groups to respiratory pathogens after the COVID-19 pandemic28.
In this study, respiratory pathogens resuscitated in the first wave after ending the zero COVID policy included RSV, FluA, and HPIV. Before the COVID-19 epidemic, RSV and FluA typically displayed distinct seasonal peaks, with RSV being more prevalent in autumn and winter and FluA more common in winter29,30,31. The epidemic season of HPIV varies depending on its subtypes, especially types I, II, and IV, which are mainly prevalent in autumn32. Past studies in several countries have found that the incidence of respiratory viruses decreased during the COVID-19 epidemic, and even RSV and influenza viruses disappeared33,34,35. In addition, the COVID-19 pandemic led to significant changes in the age distribution and seasonal patterns of respiratory virus infections worldwide36,37. The end of the zero COVID policy in China coincided with the start of the typical influenza and RSV epidemic season, which increased public awareness of these viruses. Li et al. conducted a cross-sectional observational study and found a rapid outbreak of RSV in Henan Province, China, between March and June 2023, particularly in children under 3 years of age38. After assessing the prevalence of RSV in more than 120,000 Chinese children at different stages of the COVID-19 pandemic, Hu et al. reported that the seasonal pattern was significantly disrupted by the relaxation of COVID-19 restrictive measures, and the age range of children susceptible to RSV was broadened39. These results are consistent with the recovery trend of RSV and FluA observed in our study after the COVID-19 epidemic. Our study shows that the surge in RSV, FluA, and HPIV cases began in March 2023, the first spring after ending the zero COVID policy. The timing of this event suggests a potential ecological competition between SARS-CoV-2 and other respiratory pathogens in the human respiratory epithelium40, which may have contributed to the delayed outbreak of other respiratory pathogens such as RSV, FluA, and HPIV.
This study found that before and after ending the zero COVID policy, HRV remained the predominant pathogen and was easily mixed with other pathogens. A study in Brazil reported that HRV and RSV were the most prevalent viruses during the COVID-19 pandemic41. Similarly, a study in Qatar indicated that rhinovirus remained a major virus during and after the COVID-19 epidemic, which is consistent with our results42. Studies have shown that the effectiveness of surgical masks in controlling the spread of HRV is not satisfactory, albeit their effectiveness in preventing the spread of coronavirus and influenza43. A study in South Africa indicated that the prevalence of mixed rhinovirus/enterovirus infections was highest among severe ARTIs in children under the age of 5 years during the COVID-19 pandemic44. These results further demonstrate that HRV is a dominant virus in children with ARTIs during and after the epidemic and that the prevalence of COVID-19 has a limited impact on the prevalence of HRV.
In this study, the positive rate for FluB and ADV was generally low, but they were largely suppressed during the COVID-19 epidemic, which is consistent with the results of previous studies45. Children infected with ADV are prone to severe complications and long-term pulmonary sequelae46. It was found that the positive rate of ADV has been increased since the implementation of the zero COVID policy. Therefore, we should strengthen our vigilance against the outbreak of ADV and related severe pneumonia cases.
Global prospective surveillance data show that after more than three years of implementation of COVID-19 pandemic restrictions, Europe and Asia have experienced delayed outbreaks unique to MP, accompanied by a decline in MP-specific IgM and IgG antibody levels15. Our study also found that MP has been on the rise since March 2023, maintaining a high positive rate and delaying the peak of the epidemic compared to other respiratory pathogens. The delayed outbreak of MP may be attributed to its slow generation time and long latency period, which requires a longer time for reconstruction14. Currently, Suzhou, China is still in the epidemic period of MP, so the monitoring of the epidemic characteristics of MP should continue to be strengthened.
The strength of this study lies in the use of a large number of cases (42,379 children), stratified by four age groups and different seasons, to compare the epidemiology of nine common respiratory pathogens after the ending the zero COVID policy with that during the COVID-19 pandemic. The increase in respiratory pathogen positive rates observed after the COVD-19 pandemic is a new challenge for the public health system, requiring health workers to further focus on the prevalence of respiratory pathogens in the post-epidemic period, especially among young children at risk. Gradual promotion of effective vaccination programmes, strengthening of sanitary protection and improvement of individual immunity can be seen as attempts to reduce the ‘immunity debt’.
Our study has several limitations that should be considered. First, the sample was limited to hospitalized children in the Suzhou area, which may not fully represent the broader population of children with ARTIs, including those treated in the outpatient or emergency settings. Second, the reliance on discharge codes to identify target subjects may have resulted in potential participants being omitted due to input errors. Lastly, the study included only 9 common respiratory pathogens, which may have overlooked the infection burden of other pathogens. To address these limitations, future research should consider expanding the geographical scope to include a broader range of regions and healthcare settings. Longitudinal studies covering a longer period of time can provide a more comprehensive understanding of the trends in respiratory pathogen infections among children.
Conclusions
After ending the zero COVID policy, it was observed that the spread of several respiratory pathogens has increased. The initial resurgence includes RSV, FluA, and HPIV, while MP exhibits a distinct delayed outbreak. The seasonal epidemic patterns of common respiratory pathogens have not fully reverted to their pre-epidemic levels. As a result, it is imperative for health professionals to strengthen surveillance measures to prevent the resurgence of certain pathogenic respiratory infections following the relaxation of COVID-19 restrictions. These findings have important implications for the formulation of prevention and treatment strategies for childhood respiratory infections during future public health crises.
Data availability
All data analyzed during this study are included in this published article.
Abbreviations
- COVID-19:
-
Coronavirus disease 2019
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- ARTIs:
-
Acute respiratory tract infections
- NPAs:
-
Nasopharyngeal aspirates
- NPIs:
-
Non-pharmaceutical intervention
- ICU:
-
Intensive care unit
- RSV:
-
Respiratory syncytial virus
- FluA:
-
Influenza A
- FluB:
-
Influenza B
- HPIV:
-
Human parainfluenza virus
- ADV:
-
Adenovirus
- HRV:
-
Human rhinovirus
- BoV:
-
Bocavirus
- HMPV:
-
Human metapneumovirus
- MP:
-
Mycoplasma pneumoniae
References
Hsiang, S. et al. The effect of large-scale anti-contagion policies on the COVID-19 pandemic. Nature 584, 262–267. https://doi.org/10.1038/s41586-020-2404-8 (2020).
Burki, T. Moving away from zero COVID in China. Lancet Respiratory Med. 11, 132. https://doi.org/10.1016/s2213-2600(22)00508-2 (2023).
Pan, A. et al. Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. Jama 323, 1915–1923. https://doi.org/10.1001/jama.2020.6130 (2020).
Angoulvant, F. et al. Coronavirus disease 2019 pandemic: Impact caused by school closure and national lockdown on pediatric visits and admissions for viral and nonviral infections-a time series analysis. Clin. Infect. Diseases: Official Publication Infect. Dis. Soc. Am. 72, 319–322. https://doi.org/10.1093/cid/ciaa710 (2021).
Wang, Y. et al. Reduction of secondary transmission of SARS-CoV-2 in households by face mask use, disinfection and social distancing: A cohort study in Beijing, China. BMJ Global Health. 5 https://doi.org/10.1136/bmjgh-2020-002794 (2020).
Williams, B. G., Gouws, E., Boschi-Pinto, C., Bryce, J. & Dye, C. Estimates of world-wide distribution of child deaths from acute respiratory infections. Lancet Infect. Dis. 2, 25–32. https://doi.org/10.1016/s1473-3099(01)00170-0 (2002).
Henrickson, S. E. et al. Genomic circuitry underlying immunological response to pediatric acute respiratory infection. Cell. Rep. 22, 411–426. https://doi.org/10.1016/j.celrep.2017.12.043 (2018).
Lefkowitz, R. B., Miller, C. M., Martinez-Caballero, J. D. & Ramos, I. Epigenetic Control of innate immunity: Consequences of acute respiratory virus infection. Viruses 16 https://doi.org/10.3390/v16020197 (2024).
Tabatabai, J. et al. Viral etiology and clinical characteristics of acute respiratory tract infections in hospitalized children in southern Germany (2014–2018). Open. Forum Infect. Dis. 10, ofad110. https://doi.org/10.1093/ofid/ofad110 (2023).
Mastrolia, M. V., Rubino, C., Resti, M., Trapani, S. & Galli, L. Characteristics and outcome of influenza-associated encephalopathy/encephalitis among children in a tertiary pediatric hospital in Italy, 2017–2019. BMC Infect. Dis. 19, 1012. https://doi.org/10.1186/s12879-019-4636-5 (2019).
Jantarabenjakul, W. et al. Neurological complications associated with influenza in hospitalized children. Influenza Other Respir. Viruses. 17, e13075. https://doi.org/10.1111/irv.13075 (2023).
Zhang, G. et al. Epidemiological changes in respiratory pathogen transmission among children with acute respiratory infections during the COVID-19 pandemic in Kunming, China. BMC Infect. Dis. 24, 826. https://doi.org/10.1186/s12879-024-09733-y (2024).
Li, Z. J. et al. Etiological and epidemiological features of acute respiratory infections in China. Nat. Commun. 12, 5026. https://doi.org/10.1038/s41467-021-25120-6 (2021).
Waites, K. B. & Talkington, D. F. Mycoplasma pneumoniae and its role as a human pathogen. Clin. Microbiol. Rev. 17, 697–728. https://doi.org/10.1128/cmr.17.4.697-728.2004 (2004). table of contents.
Meyer Sauteur, P. M. & Beeton, M. L. Mycoplasma pneumoniae: Delayed re-emergence after COVID-19 pandemic restrictions. Lancet Microbe. 5, e100–e101. https://doi.org/10.1016/s2666-5247(23)00344-0 (2024).
Chuang, Y. C., Lin, K. P., Wang, L. A., Yeh, T. K. & Liu, P. Y. The impact of the COVID-19 pandemic on respiratory syncytial virus infection: a narrative review. Infect. drug Resist. 16, 661–675. https://doi.org/10.2147/idr.S396434 (2023).
Leung, C., Konya, L. & Su, L. Postpandemic immunity debt of influenza in the USA and England: an interrupted time series study. Public. Health. 227, 239–242. https://doi.org/10.1016/j.puhe.2023.12.009 (2024).
Cohen, R. et al. Immune debt: recrudescence of disease and confirmation of a contested concept. Infect. Dis. now. 53, 104638. https://doi.org/10.1016/j.idnow.2022.12.003 (2023).
Abu-Raya, B., Viñeta Paramo, M., Reicherz, F. & Lavoie, P. M. Why has the epidemiology of RSV changed during the COVID-19 pandemic? EClinicalMedicine 61, 102089. https://doi.org/10.1016/j.eclinm.2023.102089 (2023).
Jiang, M. L. et al. Changes in endemic patterns of respiratory syncytial virus infection in pediatric patients under the pressure of nonpharmaceutical interventions for COVID-19 in Beijing, China. J. Med. Virol. 95, e28411. https://doi.org/10.1002/jmv.28411 (2023).
Jiang, W., Xu, L., Wang, Y. & Hao, C. Exploring immunity debt: Dynamic alterations in RSV antibody levels in children under 5 years during the COVID-19 pandemic. J. Infect. https://doi.org/10.1016/j.jinf.2023.10.019 (2023).
Malhotra, B., Swamy, M. A., Reddy, P. V., Kumar, N. & Tiwari, J. K. Evaluation of custom multiplex real - time RT - PCR in comparison to fast - track diagnostics respiratory 21 pathogens kit for detection of multiple respiratory viruses. Virol. J. 13, 91. https://doi.org/10.1186/s12985-016-0549-8 (2016).
Hess, A. S. & Hess, J. R. Understanding tests of the association of categorical variables: The Pearson Chi-square test and Fisher’s exact test. Transfusion 57, 877–879. https://doi.org/10.1111/trf.14057 (2017).
Liang, J. et al. Infection rates of 70% of the population observed within 3 weeks after release of COVID-19 restrictions in Macao, China. J. Infect. 86, 402–404. https://doi.org/10.1016/j.jinf.2023.01.029 (2023).
Cohen, R. et al. Pediatric Infectious Disease Group (GPIP) position paper on the immune debt of the COVID-19 pandemic in childhood, how can we fill the immunity gap? Infect. Dis. now. 51, 418–423. https://doi.org/10.1016/j.idnow.2021.05.004 (2021).
Scudiero, O. et al. Exercise immune system, nutrition, respiratory and cardiovascular diseases during COVID-19: A complex combination. Int. J. Environ. Res. Public Health. 18. https://doi.org/10.3390/ijerph18030904 (2021).
Tregoning, J. S. & Schwarze, J. Respiratory viral infections in infants: causes, clinical symptoms, virology, and immunology. Clin. Microbiol. Rev. 23, 74–98. https://doi.org/10.1128/cmr.00032-09 (2010).
Rubin, R. From immunity debt to immunity theft-how COVID-19 might be tied to recent respiratory disease surges. Jama 331, 378–381. https://doi.org/10.1001/jama.2023.26608 (2024).
Rose, E. B., Wheatley, A., Langley, G., Gerber, S. & Haynes, A. Respiratory syncytial virus seasonality - United States, 2014–2017. MMWR Morb. Mortal. Wkly Rep. 67, 71–76. https://doi.org/10.15585/mmwr.mm6702a4 (2018).
Xu, Z. W., Li, Z. J. & Hu, W. B. Global dynamic spatiotemporal pattern of seasonal influenza since 2009 influenza pandemic. Infect. Dis. Poverty. 9 https://doi.org/10.1186/s40249-019-0618-5 (2020).
Cohen, R., Babushkin, F., Geller, K. & Finn, T. Characteristics of hospitalized adult patients with laboratory documented Influenza A, B and respiratory syncytial virus: A single center retrospective observational study. PloS One. 14, e0214517. https://doi.org/10.1371/journal.pone.0214517 (2019).
Han, J. Y., Suh, W. & Han, S. B. Seasonal epidemiological and clinical characteristics of pediatric patients with human parainfluenza virus infection by serotype: A retrospective study. Virol. J. 19, 141. https://doi.org/10.1186/s12985-022-01875-2 (2022).
Kışlal, F. M., Hanilçe, Y., Altaş, B., Büyükbaşaran, Z. E. & Güven, D. The disappearance of respiratory syncytial virus and influenza viruses in children during the second year of the COVID-19 pandemic: Are non-pharmaceutical interventions as effective as vaccines? Eur. Rev. Med. Pharmacol. Sci. 27, 3777–3783. https://doi.org/10.26355/eurrev_202304_32178 (2023).
Leija-Martínez, J. J., Esparza-Miranda, L. A., Rivera-Alfaro, G. & Noyola, D. E. Impact of nonpharmaceutical interventions during the COVID-19 pandemic on the prevalence of respiratory syncytial virus in hospitalized children with lower respiratory tract infections: A systematic review and Meta-analysis. Viruses 16 https://doi.org/10.3390/v16030429 (2024).
Vittucci, A. C. et al. The disappearance of respiratory viruses in children during the COVID-19 pandemic. Int. J. Environ. Res. Public Health. 18 https://doi.org/10.3390/ijerph18189550 (2021).
Wu, R., Zhang, J. & Mo, L. Analysis of respiratory virus detection in hospitalized children with acute respiratory infection during the COVID-19 pandemic. Virol. J. 20, 253. https://doi.org/10.1186/s12985-023-02218-5 (2023).
Chow, E. J., Uyeki, T. M. & Chu, H. Y. The effects of the COVID-19 pandemic on community respiratory virus activity. Nat. Rev. Microbiol. 21, 195–210. https://doi.org/10.1038/s41579-022-00807-9 (2023).
Li, X., Chen, N., Wang, X. & Li, T. Epidemiology of respiratory syncytial virus outbreak among children after the COVID-19 pandemic. J. Med. Virol. 95, e29017. https://doi.org/10.1002/jmv.29017 (2023).
Hu, L. et al. Epidemiological characteristics of respiratory syncytial virus infection in pediatric patients before, during the COVID-19 pandemic and after easing of COVID-19 restrictive measures in China. J. Med. Virol. 96, e29374. https://doi.org/10.1002/jmv.29374 (2024).
Pinky, L. & Dobrovolny, H. M. Coinfections of the respiratory tract: viral competition for resources. PloS One. 11, e0155589. https://doi.org/10.1371/journal.pone.0155589 (2016).
Lima, A. K. S. et al. Seasonal respiratory virus trends in pediatric patients during the COVID-19 pandemic in Brazil. Brazilian J. Microbiology: [publication Brazilian Soc. Microbiology]. 54, 1827–1834. https://doi.org/10.1007/s42770-023-01087-y (2023).
Abushahin, A. et al. Impact of COVID–19 pandemic restrictions and subsequent relaxation on the prevalence of respiratory virus hospitalizations in children. BMC Pediatr. 24, 91. https://doi.org/10.1186/s12887-024-04566-9 (2024).
Leung, N. H. L. et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat. Med. 26, 676–680. https://doi.org/10.1038/s41591-020-0843-2 (2020).
Ogunbayo, A. E. et al. Pathogen profile of children hospitalised with severe acute respiratory infections during COVID-19 pandemic in the Free State Province, South Africa. Int. J. Environ. Res. Public Health. 19 https://doi.org/10.3390/ijerph191610418 (2022).
Ippolito, G. et al. Disappearance of Seasonal Respiratory viruses in Children under two Years Old during COVID-19 pandemic: a Monocentric Retrospective Study in Milan, Italy. Front. Pead. 9, 721005. https://doi.org/10.3389/fped.2021.721005 (2021).
Fu, Y. et al. Human adenovirus type 7 infection causes a more severe disease than type 3. BMC Infect. Dis. 19 https://doi.org/10.1186/s12879-018-3651-2 (2019).
Acknowledgements
All authors wish to thank the children and their parents in this study.
Funding
This work was supported by the National Natural Science Foundation of China (Grant No.82270018, 81573167, and 82070009), the Jiangsu Province Key Research and Development Program (Social Development Project) (Grant No. BE2021656).
Author information
Authors and Affiliations
Contributions
XX and CH were responsible for the study concept and design. YZ and XX collected clinical information and acquired the data. XX and LX performed an analysis and interpretation of the data. WJ and XX drafted the manuscript and made substantial revisions for important intellectual content. All authors reviewed and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study protocol was approved and waived informed consent by the Medical Ethics Committee of the Children’s Hospital of Soochow University (2013002).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xu, X., Zhang, Y., Xu, L. et al. Analysis of respiratory pathogen detection in hospitalized children with acute respiratory tract infections after ending the zero COVID policy. Sci Rep 14, 31784 (2024). https://doi.org/10.1038/s41598-024-82660-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-82660-9