Abstract
Recently, the prevalence of diabetes mellitus (DM) in the world continues to rise, which has seriously threatened human health. Enhanced pancreatic β-cell death is one of the important factors in the pathogenesis of type 1 diabetes mellitus (T1DM). Berberine, an alkaloid, plays a series of pharmacological functions in many disease. The purpose of this study was to explore the specific mechanisms of berberine in the high glucose (HG) stimulated pancreatic β-cell. The 30 mM D-glucose stimulated mouse pancreatic β cells (NIT-1) was used to estabilish T1DM model in vitro. Then the cell viability was detected by CCK-8 assay. The lactic dehydrogenase (LDH), reactive oxygen species (ROS), Iron, malondialdehyde (MDA), glutathione (GSH), and glutathione peroxidase 4 (GPX4) levels were determined by corresponding kits. The cell death was evaluated by PI staining. Western blot was performed to measure the O-linked N-acetylglucosamine (O-GlcNAc) and O-GlcNAc transferase (OGT) protein levels. The results showed that berberine treatment significantly increased the cell viability, GPX4 activity and GSH levels, and decreased the ROS, Iron, MDA levels and PI positive cells in the HG stimulated NIT-1 cells. Additionally, the molecular docking analysis showed that berberine could bind to OGT. Berberine treatment significantly decreased the global O-GlcNAc levels and OGT protein expression in the HG stimulated NIT-1 cells. Furthermore, OGT overexpression reversed the role of berberine in the HG stimulated NIT-1 cells. This study demonstrated that berberine treatment inhibited the ferroptosis of pancreatic β-cell under high-glucose condition via decreasing the OGT expressions.
Similar content being viewed by others
Introduction
In recent years, the prevalence of diabetes mellitus (DM) in the world continues to rise, which has seriously threatened human health1. With the improvement of life, the prevalence of diabetes among Chinese people has continued to rise, accounting for 7.5% of the total population 1%, higher than the global average, ranking first in the world2. In diabetes, type 1 diabetes mellitus (T1DM) accounts for more than 5% of the total number of patients3. Insulin resistance and impaired pancreatic β-cell function are the two most important factors in the pathogenesis of T1DM4. According to previous reports, impaired function β cell is closely related to the decrease of β cell number. In the T1DM progression, the decrease of β cells was due to cell death rather than the decrease of newborn B cells5,6. Therefore, explore the specific mechanisms of islets β cells plays an important role in the prevention and treatment of T1DM.
Coptis chinensis is a widely used medicinal material for the treatment of traditional Chinese medicine (TCM) diseases, which was demonstrated to have the effect of clearing away heat and toxic material7,8,9. Western medicine confirmed that the main component of coptis chinensis is berberine, an alkaloid, which plays a series of pharmacological functions as an active ingredient in many medicinal materials10. In addition to the antibacterial, antiviral, anti-inflammatory, and anti diarrhea functions11,12, berberine also has significant improvement effects on metabolic, neurological, and heart diseases13,14. Previous studies have demonstrated that berberine plays an important role in the growth of islets β cells15,16. However, the specific mechanisms of berberine in T1DM remains unclear.
Posttranslational modification of proteins enables cells to respond quickly to internal and external signals through direct and dynamic control of protein function17. O-glycosylation is a nonclassical glycosylation involving a single O-linked N-acetylglucosamine (O-GlcNAc) partially connecting to serine and threonine residues of cytoplasmic, nuclear, and mitochondrial proteins18. Unlike phosphorylation, which is regulated by hundreds of kinases, there is only one intracellular O-GlcNAc glycosyltransferase (OGT) and O-GlcNAc glycosidase (OGA) that regulate the O-GlcNAc modification process19. Under the catalytic action of OGT, UDP GlcNAc is connected to the exposed silk/threonine residue of the protein to complete O-GlcNAc modification20; Under the action of OGA, GlcNAc is hydrolyzed from the peptide chain of protein to complete the degradation of glycosylation21. Previous studies have demonstrated that OGT mediated O-GlcNAc aggravated the DM development22,23. Therefore, we speculated whether berberine can regulate the O-GlcNAc modification in DM progression, thereby inhibiting cell death of islets β cells.
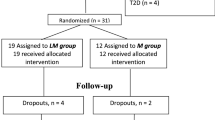
Therefore, in this study, mouse pancreatic β cells were treated with high glucose to establish the DM model in vitro to explore the role of berberine in the injury of mouse pancreatic β cells. NIT-1 cell line was derived from murine pancreatic β-cells line derived from the hybrid rat insulin-promoter/SV40 large T-antigen Non-Obese Diabetic (NOD) mouse24. Our use of this cell line provides a relevant in vitro model for investigating the mechanisms underlying β-cell dysfunction and death, including ferroptosis, in the context of T1DM. We hypothesized that berberine inhibited the cell death of β cells through inhibiting the OGT mediated O-GlcNAc.
Materials and methods
Cell culture and treatment
Mouse pancreatic β cells (NIT-1) were purchased from Procell (Wuhan, China). The DMEM-F12 medium containing 10% fetal bovine serum was used to perform the cell culture. The cultivation condition of the humidified incubator was set to 95% air, 5% CO2 and 37 °C. After incubation, the cells were treated with 30 mM D-glucose to establish the DM injury model (high glucose, HG group), and the cells in the control group were cultured in the normal medium (normal control, NC group). For berberine treatment, the cells were cultured in the medium containing different dose of berberine (0.2, 0.4 and 0.6 µM) for 24 h, respectively. For cell transfection, the OGT overexpressed vector and empty vector were acquired from Genepharma (Shanghai, China), and transfected into the cells using Lipofectamine 3000 (Invitrogen) for 48 h. Then, the cells were collected for the next experiments.
CCK-8 assay
After treatment, the cells were resuspended to 3 × 105 cells/ml. Then 200 µl of cells were seeded into a 24-well plate and treated with 10 µl of CCK-8 regents for 2 h. Subsequently, cell viability was determined using microplate at the wavelength of 450 nm.
Determination of LDH, ROS, iron, MDA, GSH, and GPX4 levels
The lactic dehydrogenase (LDH), reactive oxygen species (ROS), Iron, malondialdehyde (MDA), glutathione (GSH), and glutathione peroxidase 4 (GPX4) levels in the cells of each group were determined using Corresponding kits, which were purchased from the Nanjing Jiangcheng Bioengineering Institute (Nanjing, China). The Iron levels were detected using Iron determination kit, which was purchased from Beckman Coulter, Inc. (USA). The ROS levels were measured using Reactive Oxygen Species (ROS) Fluorometric Assay Kit, which was purchased from the Elabscience Biotechnology Co., Ltd (Wuhan, China). All operations shall be carried out in strict accordance with the kit instructions.
DAPI/PI double staining
DAPI/PI double staining was performed to evaluate cell death. The cells in each group were centrifuged and suspended with 1 mL cell staining buffer, followed by 5 µL DAPI staining solution (Beyotime, Shanghai, China) and 5 µL PI staining solution (Beyotime). Next, the cells were stained in dark for 30 min at 4℃. Finally, the cells were washed with PBS for 2 times and observed with fluorescence microscope (TE2000, Nikon, Japan).
Western blot
Cells were lysed in RIPA lysis buffer (Beyotime). Then the protein concentration was detected using a BCA kit (Beyotime). Equal proteins (20 µg/lane) were separated by 15% SDS-polyacrylamide gel and transferred to PVDF membrane (Millipore). Next, the membranes were blocked with 5% skim milk, and then incubated with primary antibodies (anti-OGA, 1:1200, Abcam; anti-OGT, 1:1000, Abcam; anti-O-GlcNAc, 1:2000, Abcam; anti-FTH1, 1:1500, Abcam; anti-NCOA44, 1:2000, Abcam; anti-DMT1, 1:1000, Abcam; anti-GAPDH, 1:2500, Abcam) at 4 °C overnight, followed by incubated with secondary antibody at 37 °C for 1 h. The bands were observed using ECL reagent (Beyotime).
Molecular docking
Protein crystal structure of OGT was downloaded from RCSB PDB database (https://www1.rcsb.org/) and the pdb file was obtained. The mol2 files of berberine were downloaded from TCMSP database, and AutoDock Tools was used to process protein crystals and compound structures, including separating protein structures and original ligands, removing water molecules, adding charges to structures. Finally the files were converted into PDBQT format and molecular docking was conducted. The docking results are visualized by PyMOL software.
Statistical analysis
The statistical analysis was performed using SPSS v.19.0 software (IBM). All experiments were performed in triplicate (N = 3) and all data are presented as means ± SD. Student’s t-test was used to analyze the differences between two groups and one-way ANOVA followed by Tukey test was used for multiple groups. Statistical significance was set at p < 0.05.
Results
Selection of optimal dose of berberine
The chemical structural formula of berberine was shown in Fig. 1A. To select the most suitable dose of berberine for subsequent experiments, the NIT-1 cells were treated with different dose of berberine (0.2, 0.4 and 0.6 µM) for 24 h. Then we found that 0.4 and 0.6 µM dose of berberine significantly increased the cell viability of the NIT-1 cells (Fig. 1B), while 0.6 µM dose of berberine significantly increased the LDH release (Fig. 1C) in the NIT-1 cells. Therefore, 0.4 µM dose of berberine was selected for the next experiments.
Berberine treatment relieved HG stimulation induced ferroptosis in the NIT-1 cells
Then the NIT-1 cells were stimulated with 30 mM D-glucose to establish the DM injury model. We found that HG stimulation significantly decreased the cell viability (Fig. 2A), increased the ROS (Fig. 2B), Iron (Fig. 2C) and MDA (Fig. 2D), and decreased GPX4 activity (Fig. 2E) and GSH levels (Fig. 2F) in the NIT-1 cells. Additionally, we found that HG treated increased the PI positive cells in the NIT-1 cells (Fig. 2G). Furthermore, we found that the protein levels of ASCL4, TFRC, NCOA4 and DMT1 were increased, while SCL7A11 and FTH1 were decreased in the HG stimulated NIT-1 cells (Fig. 2H). These results indicated that the HG stimulation might induced the ferroptosis of the NIT-1 cells. Subsequently, the HG stimulated NIT-1 cells were treated with 0.4 µM dose of berberine. The results showed that berberine treatment significantly increased the cell viability (Fig. 2A), decreased the ROS (Fig. 2B), Iron (Fig. 2C), MDA (Fig. 2D) levels, increased GPX4 activity (Fig. 2E) and GSH levels (Fig. 2F), and decreased PI positive cells (Fig. 2G) in the HG stimulated NIT-1 cells. Furthermore, berberine treatment decreased ASCL4, TFRC, NCOA4 and DMT1 protein levels, and increased SCL7A11 and FTH1 in the HG stimulated NIT-1 cells (Fig. 2H).
Berberine treatment relieved HG stimulation induced ferroptosis in the NIT-1 cells. The HG stimulated NIT-1 cells were treated with 0.4 µM dose of berberine. (A) Then the cell viability was determined by CCK-8 assay. The ROS (B), Iron (C), MDA (D), GPX4 (E) and GSH (F) levels were detected by corresponding kits. (G) The cell death was detected by PI staining. (H) The protein levels of FTH1, NCOA4, DMTA, ACSL4, TFRC and SCL7A11 were detected by western blot. N = 3. *P < 0.05, **P < 0.01, ***P < 0.001.
Berberine treatment decreased the OGT mediated O-GlcNAc modification
The molecular docking results of berberine (BBR) with OGT protein are illustrated in Fig. 3A. The top panel shows the surface electrostatic potential of the OGT protein, with red and blue regions indicating positive and negative charges, respectively. BBR, depicted in stick representation with a combination of red and white colors, is docked into a specific binding pocket on the surface of the OGT protein. The bottom panel provides a detailed view of the interaction between BBR and OGT. The OGT protein is represented as a green ribbon structure, highlighting the region where BBR binds. Berberine forms hydrogen bonds with an aspartic acid residue (ASP-152) in the OGT protein, as indicated by the yellow dashed lines. This interaction suggests that BBR may modulate the function or activity of OGT by stabilizing its conformation through these hydrogen bonds. Additionally, we found that HG stimulation significantly increased the global O-GlcNAc levels and OGT protein expression, while showed no effects on the OGA protein levels. Berberine treatment significantly decreased the global O-GlcNAc levels and OGT protein expression (Fig. 3B).
Overexpression of OGT reversed the Berberine roles in the HG stimulated NIT-1 cells
Finally, the OGT levels were overexpressed to explore whether berberine played role in the HG stimulated NIT-1 cells through targeting the OGT levels. OGT overexpression significantly decreased the cell viability (Fig. 4A), increased the ROS (Fig. 4B), Iron (Fig. 4C), MDA (Fig. 4D) levels, decreased GPX4 activity (Fig. 4E) and GSH levels (Fig. 4F), and increased PI positive cells (Fig. 4G) in the HG stimulated NIT-1 cells after berberine treatment. Besides, OGT overexpression significantly decreased the SCL7A11 and FTH1 protein levels, and increased ASCL4, TFRC, NCOA4 and DMT1 in the HG stimulated NIT-1 cells after berberine treatment (Fig. 4H). In addition, we also found that OGT overexpression significantly increased the global O-GlcNAc levels in HG stimulated and berberine treated NIT-1 cells (Supplementary Fig. 1). Bessides, in the normal NIT-1 cells and HG stimulated NIT-1 cells, OGT knockdown showed no effects on ferroptosis of normal NIT-1 cells, while OGT knockdown rinhibited the ferroptosis of HG stimulated NIT-1 cells (Supplementary Fig. 2).
Overexpression of OGT reversed the berberine roles in the HG stimulated NIT-1 cells. The HG stimulated NIT-1 cells were treated with 0.4 µM dose of berberine and transfected with OGT overexpressed vector. (A) Then the cell viability was determined by CCK-8 assay. The ROS (B), Iron (C), MDA (D), GPX4 (E) and GSH (F) levels were detected by corresponding kits. (G) The cell death was detected by PI staining. (H) The protein levels of FTH1, NCOA4, DMTA, ACSL4, TFRC and SCL7A11 were detected by western blot. N = 3. *P < 0.05, **P < 0.01, ***P < 0.001.
Discussion
DM is a common metabolic disease, which is caused by the imbalance between the production and consumption of glucose in the body25. The loss of pancreatic β-cells have been demonstrated to be one of the key factors during DM progression26. In current study, we demonstrated that berberine treatment relieved the ferroptosis in the HG stimulated NIT-1 cells through decreaseing the OGT expression levels. OGT overespression reversed the effects of berberine on the ferroptosis in the HG stimulated NIT-1 cells.
Berberine has been previously confirmed to exert antioxidant27, anti-inflammatory28 and inhibitory effects on cell death29, which has attracted the attention of researchers. Recently, Yi et al.30 found that berberine relieved the liver fibrosis development through inhibiting the ROS-mediated ferroptosis of hepatic stellate cells, which showed that berberine also exert inhibitory effect on ferroptosis. Ferroptosis is different from apoptosis, necrosis, autophagy, and pyroptosis in morphology, biochemical characteristics, and genetics, which is characterized by the accumulation of that iron dependent lipid peroxides31. Ferroptosis is widely involved in pathophysiological processes such as tumor inhibition and drug resistance, neurodegeneration, ischemia reperfusion injury and metabolic diseases32,33. In DM progression, pancreatic β-cell can express low levels of antioxidant enzymes such as superoxide dismutase, GPX, and catalase, making them susceptible to oxidative stress. The accumulation reactive oxygen species (ROS) during this progress leads to various forms of cell death, including ferroptosis34. Previous study have shown that the induction of ferroptosis can lead to impaired islet function, which further aggravates the DM progression. Krümmel et al.35 found that GPX4 silencing led to ferroptosis in rat pancreatic β-cell, manifested by the increase of lipid peroxidation, decrease of GSH levels, and degradation of GPX4, while overexpression of GPX4 can significantly reduce pancreatic β-cell death. In vitro experiments, significant death occurred in pancreatic β-cell after ferroptosis inducers Erastin and RSL3 treatment, while ferristatin or desferriamine treatment improved the ferroptosis of pancreatic β-cell36. In this study, we found that berberine treatment significantly increased the cell viability, GPX4 activity and GSH levels, and decreased the ROS, Iron, MDA levels and PI positive cells in the HG stimulated NIT-1 cells. Our results indicated that berberine promoted the NIT-1 cells growth through preventing the ferroptosis development. These researches indicated that ferroptosis is associated with impaired insulin secretion. Preventing ferroptosis occurrence might be a promising method for treating DM.
Previous studies demonstrated that the emerging roles of protein modification via O-GlcNAc modification have been linked to the pathogenesis of DM and its complications37. OGT, as the key factor in the up-regulation of O-GlcNAc modification, promoted the DM progression through enhancing the O-GlcNAc modification. Runager et al.38 suggested that OGT silencing enhanced the rate of wound closure in patients with diabetic skin ulcers through decreasing the levels of O-GlcNAc modification. Nobuyuki et al.39 found O-GlcNAc modification activated the nitric oxide synthase and aggravated glucose-induced impairment in endothelial cells of T2DM patient. Thus it can be seen that O-GlcNAc modification played an important role in DM progression. However, the regulatory effect of O-GlcNAc modification on pancreatic β-cell is still poorly studied. Here, through the molecular docking analysis, we found that berberine could bind to OGT. Furthermore, we also found that berberine treatment significantly decreased the global O-GlcNAc levels and OGT protein expression in the HG stimulated NIT-1 cells. The rescue experiment showed that OGT overexpression reversed the role of berberine in the HG stimulated NIT-1 cells. However, the relationship between OGT and ferroptosis remains unclear. As reported by Tang et al.40, inhibition of ubiquitin specific peptidase 8 inhibited the progression of hepatocellular carcinoma and induce ferroptosis via decreasing the stability of OGT, which was contrary to our research findings. This may be due to the different target genes that OGT acts on, as well as the inherent specificity of tumor diseases. But more research is needed in the future to prove the specific mechanism of OGT regulating ferroptosis.
However, this study represents a preliminary investigation into the involvement of berberine in the regulation of ferroptosis through modulation of O-GlcNAcylation mediated by OGT. A more comprehensive confirmation of this conclusion will require additional research, such as in vivo experiments (high-fat diet induced C57Bl/6J treated with berberine) and the use of O-GlcNAcylation inhibitors. This will be a key focus of our future research endeavors.
In conclusion, this study demonstrated the protective effects of berberine on the ferroptosis of the pancreatic β-cell in DM progression. Mechanistically, berberine treatment inhibited the OGT mediated O-GlcNAc levels in the pancreatic β-cells. Our research provided a solid theoretical basis for the promotion and application of berberine and precise treatment of DM in the future.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Harreiter, J. & Roden, M. Diabetes mellitus-definition, classification, diagnosis, screening and prevention (update 2019). Wien Klin. Wochenschr. 131, 6–15 (2019).
Juan, J. & Yang, H. Prevalence, Prevention, and Lifestyle Intervention of Gestational Diabetes Mellitus in China (2020).
Riddell, M. C. & Peters, A. L. Exercise in adults with type 1 diabetes mellitus. Nat. Reviews Endocrinol. 19, 98–111 (2023).
Eizirik, D. L., Pasquali, L. & Cnop, M. Pancreatic beta-cells in type 1 and type 2 diabetes mellitus: different pathways to failure. Nat. Rev. Endocrinol. 16, 349–362 (2020).
Liu, Y. T., He, T., Li, H. Q. & Jiang, P. Liraglutide improves pancreatic islet beta cell apoptosis in rats with type 2 diabetes mellitus by inhibiting the Ikkepsilon/Nf-Kappab pathway. Eur. Rev. Med. Pharmacol. Sci. 25, 4818–4828 (2021).
Lee, K. et al. Xbp1 maintains beta cell identity, represses beta-to-alpha cell transdifferentiation and protects against diabetic beta cell failure during metabolic stress in mice. Diabetologia 65, 984–996 (2022).
Liu, Y. et al. Analysis of the Coptis chinensis genome reveals the diversification of protoberberine-type alkaloids. Nat. Commun. 12, 3276 (2021).
Chen, Q. et al. Coptis chinensis Franch polysaccharides provide a dynamically regulation on intestinal microenvironment, based on the intestinal flora and mucosal immunity. J. Ethnopharmacol. 267, 113542 (2021).
Gan, Z. et al. Excitatory amino acid transporter supports inflammatory macrophage responses. Sci. Bull. (Beijing). 69, 2405–2419 (2024).
Wang, Z. et al. Berberine improves ovulation and endometrial receptivity in polycystic ovary syndrome. Phytomedicine 91, 153654 (2021).
Majdalawieh, A. F., Yousef, S. M., Abu-Yousef, I. A. & Nasrallah, G. K. Immunomodulatory and anti-inflammatory effects of Berberine in lung tissue and its potential application in prophylaxis and treatment of covid-19. Front. Biosci. 27, 166 (2022).
Nguyen, H. T. et al. Antibacterial activity of a Berberine nanoformulation. Beilstein J. Nanotechnol. 13, 641–652 (2022).
Shou, J. W. & Shaw, P. C. Therapeutic efficacies of Berberine against neurological disorders: an update of Pharmacological effects and mechanisms. Cells 11, 1 (2022).
Jia, X., Shao, W. & Tian, S. Berberine alleviates myocardial ischemia-reperfusion injury by inhibiting inflammatory response and oxidative stress: the key function of Mir-26B-5P-mediated Ptgs2/Mapk signal transduction. Pharm. Biol. 60, 652–663 (2022).
Bao, L. et al. Berberine regulates Gpx4 to inhibit ferroptosis of islet beta cells. Planta Med. 89, 254–261 (2023).
Li, M. et al. Berberine protects against palmitate induced beta cell injury via promoting mitophagy. Genes Genom. 44, 867–878 (2022).
Chen, N., Kong, X., Zhao, S. & Xiaofeng, W. Post-translational modification of baculovirus-encoded proteins. Virus Res. 279, 197865 (2020).
Magalhães, A., Duarte, H. O. & Reis, C. A. The role of O-glycosylation in human disease. Mol. Aspects Med. 79, 100964 (2021).
Chatham, J. C., Zhang, J. & Wende, A. R. Role of O -linked N -acetylglucosamine protein modification in cellular (patho)physiology. Physiol. Rev. 101, 427–493 (2021).
Shen, H. et al. O-Glcnac transferase Ogt regulates embryonic neuronal development through modulating Wnt/beta-catenin signaling. Hum. Mol. Genet. 31, 57–68 (2021).
Kositzke, A. et al. Elucidating the protein substrate recognition of O-glcnac transferase (Ogt) toward O-glcnacase (Oga) using a Glcnac electrophilic probe. Int. J. Biol. Macromol. 169, 51–59 (2021).
Mohan, R. et al. Ogt regulates mitochondrial biogenesis and function via diabetes susceptibility gene Pdx1. Diabetes 70, 2608–2625 (2021).
Fang, N., Li, P. & O-Linked N-acetylglucosaminyltransferase Ogt inhibits diabetic nephropathy by stabilizing histone methyltransferases Ezh2 via the Hes1/Pten axis. Life Sci. 274, 119226 (2021).
Hamaguchi, K., Gaskins, H. R. & Leiter, E. H. Nit-1, a pancreatic beta-cell line established from a Transgenic Nod/Lt mouse. Diabetes 40, 842–849 (1991).
Biondi, B., Kahaly, G. J. & Robertson, R. P. Thyroid dysfunction and diabetes mellitus: two closely associated disorders. Endocr. Rev. 40, 789–824 (2019).
Memon, B. & Abdelalim, E. M. Stem cell therapy for diabetes: beta cells versus pancreatic progenitors. Cells (Basel Switz.) 9, 283 (2020).
Liu, Y. et al. Synthesis and antioxidant activities of Berberine 9-O-benzoic acid derivatives. RSC Adv. 11, 17611–17621 (2021).
Chen, C. Y., Kao, C. L. & Liu, C. M. The cancer prevention, anti-inflammatory and anti-oxidation of bioactive phytochemicals targeting the Tlr4 signaling pathway. Int. J. Mol. Sci. 19, 1 (2018).
Liu, J. et al. Berberine induces autophagic cell death in acute lymphoblastic leukemia by inactivating Akt/Mtorc1 signaling. Drug Des. Dev. Ther. 14, 1813–1823 (2020).
Yi, J. et al. Berberine alleviates liver fibrosis through inducing ferrous redox to activate ros-mediated hepatic stellate cells ferroptosis. Cell. Death Discov. 7, 374 (2021).
Hirschhorn, T. & Stockwell, B. R. The development of the concept of ferroptosis. Free Radic Biol. Med. 133, 130–143 (2019).
Mou, Y. et al. Ferroptosis, a new form of cell death: opportunities and challenges in cancer. J. Hematol. Oncol. 12, 34 (2019).
Li, Y. et al. Ischemia-induced Acsl4 activation contributes to ferroptosis-mediated tissue injury in intestinal ischemia/reperfusion. Cell. Death Differ. 26, 2284–2299 (2019).
Li, D. et al. Quercetin alleviates ferroptosis of pancreatic beta cells in type 2 diabetes. Nutrients 12 (2020).
Krummel, B., Plotz, T., Jorns, A., Lenzen, S. & Mehmeti, I. The central role of glutathione peroxidase 4 in the regulation of ferroptosis and its implications for pro-inflammatory cytokine-mediated beta-cell death. Biochim. Biophys. Acta-Mol Basis Dis. 1867, 166114 (2021).
Bruni, A. et al. Ferroptosis-inducing agents compromise in vitro human islet viability and function. Cell. Death Dis. 9, 595 (2018).
Nie, H. & Yi, W. O-Glcnacylation, a sweet link to the pathology of diseases. J. Zhejiang Univ. B Sci. 20, 437–448 (2019).
Runager, K., Bektas, M., Berkowitz, P. & Rubenstein, D. S. Targeting O-glycosyltransferase (Ogt) to promote healing of diabetic skin wounds. J. Biol. Chem. 289, 5462–5466 (2014).
Masaki, N. et al. O-Glcnacylation mediates glucose-induced alterations in endothelial cell phenotype in human diabetes mellitus. J. Am. Heart Assoc. 9, e14046 (2020).
Tang, J. et al. Targeting Usp8 inhibits O-Glcnacylation of Slc7a11 to promote ferroptosis of hepatocellular carcinoma via stabilization of Ogt. Adv. Sci. 10, e2302953 (2023).
Author information
Authors and Affiliations
Contributions
All authors participated in the design, interpretation of the studies and analysis of the data and review of the manuscript. C Y drafted the work and revised it critically for important intellectual content; Y Q, D Y, W Z and J W were responsible for the acquisition, analysis, or interpretation of data for the work; J Y made substantial contributions to the conception or design of the work. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yu, C., Qiu, Y., Yan, D. et al. Berberine treatment inhibits ferroptosis in NIT-1 murine pancreatic cell line via inhibiting OGT expression levels. Sci Rep 15, 18504 (2025). https://doi.org/10.1038/s41598-025-03537-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-03537-z