Abstract
Edentulous patients often experience difficult facemask ventilation during anesthesia induction, primarily due to inadequate facemask seal and air leakage. This randomized trial was designed to determine the efficacy and safety of an alternative ventilation strategy, namely the nasal airway ventilation technique, which involves the use of a nasal airway and a modified ventilation maneuver during anesthesia induction in edentulous patients. Eighty edentulous patients who underwent elective surgery with general anesthesia were randomly assigned to the nasal airway or facemask group. In the nasal airway group, a nasal airway was inserted and connected to the anesthesia ventilator, after which the mouth and nostrils were closed. In the facemask group, moistened gauzes were used to improve the facemask seal against hollow cheeks and the “VE-clamp” technique was applied for facemask ventilation. The primary outcome was the expired tidal volume during anesthesia induction. The expired tidal volume during anesthesia induction was significantly increased in the nasal airway group (median 5.6 mL/kg, interquartile range 5.0–5.9), compared with the facemask group (median 3.6 mL/kg, interquartile range 2.6–4.5), with a median difference of 1.9 mL/kg (95% confidence interval, 1.4 to 2.3; P < 0.001). A higher incidence of successful ventilation by a single anesthetist is observed in the nasal airway group than in the facemask group during anesthesia induction (100 vs. 82.5%; P = 0.018). There was no significant difference in the incidence of adverse events between groups. Our findings demonstrated that the nasal airway ventilation technique significantly and safely improved ventilation during anesthesia induction in edentulous patients. Thus, this technique can serve as a valuable alternative when facemask ventilation is inadequate in these patients.
Similar content being viewed by others
Introduction
With aging population, the predicted prevalence of complete edentulism in Chinese adults by 2030 is approximately 305 per 10,0001. Consequently, edentulous individuals are becoming a larger proportion of surgical patients. Airway management of edentulous patients undergoing general anesthesia presents a great challenge to anesthesiologists, especially facemask ventilation during anesthesia induction, a fundamental component of perioperative airway management.
It is reported that difficult facemask ventilation (DMV) occurs in 12–16% of edentulous patients, and the lack of dentition is an independent risk factor for DMV2,3. The lack of dentition can lead to the morphological changes of the face4 and affect the facemask-to-cheek contact. Thus, DMV often occurs because of massive air leakage from poor facemask seal2,3,5. Moreover, prolonged edentulism can lead to relative macroglossia and lateral tongue spreading6,7. These anatomical changes may further impair the patency of the upper airway and contribute to DMV under muscle relaxation following anesthesia induction, by allowing the enlarged tongue to move backward and obstruct the pharyngeal airway8,9,10,11. DMV may result in critical situations with potential serious adverse outcomes, such as brain damage and death12,13.
Up to now, various strategies, such as utilizing an oversized facemask to encompass the chin, integrating a toddler facemask with a nasal airway, and placing the caudal end of a facemask on the lower lip, have been attempted to improve facemask ventilation in edentulous patients2,14,15. However, the ventilation efficacies of these strategies are highly dependent on the facemask seal and are also usually unsatisfactory in the patients with gastric tube insertion, a common procedure for patients undergoing gastrointestinal surgery. According to Langeron et al.3 and Conlon et al.5, it was recommended that dentures should not be removed during facemask ventilation to provide facial support. This practice may benefit denture wearers, but is not applicable to edentulous individuals who do not wear dentures, a population that is common in developing countries.
Due to decreased lung function and the need for slow anesthesia induction to maintain hemodynamic stability, it is essential to ensure continuous oxygenation or ventilation prior to tracheal intubation in elderly patients. High-flow nasal cannula and supraglottic jet oxygenation and ventilation are important techniques for airway management during general anesthesia that may be effective for edentulous patients. Nevertheless, these methods require specialized equipment and skills, resulting in higher medical expenses. Another unconventional ventilation technique, utilizing a self-assembled nasal airway and a maneuver to seal the mouth and remaining nostril, was suggested for managing difficult airway in a technical communication16. This ventilation technique maintains upper airway patency and eliminates the need for a facemask; however, the sealing maneuver is inadequate for edentulous patients. Therefore, we employed a novel nasal airway and an improved sealing maneuver to achieve a convenient and effective seal in edentulous patients. This ventilation approach, referred to as the nasal airway ventilation technique in our article. There have been no clinical trials conducted to assess the ventilation efficacy and safety of this technique. Thus, we carried out a randomized trial to determine if the nasal airway ventilation technique could improve ventilation by increasing the expired tidal volume (Vte) during anesthesia induction (primary outcome) in edentulous patients, as compared to the conventional facemask ventilation technique. Additionally, we assessed the incidences of successful ventilation and adverse events including hypoxemia, mandibular dislocation, eye injury, nasal mucosal injury and esophagogastric reflux (secondary outcomes) during nasal airway and facemask ventilation.
Patients and methods
Trial design and ethics statements
This study was a single-blinded, randomized controlled clinical trial. The trial protocol was approved by the Ethics Committee of the First Affiliated Hospital of Zhengzhou University (27/01/2022, 2021-KY-1170-002), and prospectively registered on the Chinese Clinical Trials Registry (registration number: ChiCTR2200062471, date of registration: 08/08/2022) before the first participant was recruited. This study complied with the Declaration of Helsinki, and the report follows the Consolidated Standard of Reporting Trials (CONSORT) guidelines17.
Participants
Edentulous patients (those with an absence of all teeth and dentures), aged ≥ 60 years, with a body mass index (BMI) < 25 kg/m2, Mallampati Score I to II, and American Society of Anesthesiologists (ASA) physical status I to III, undergoing elective surgery with general anesthesia, were screened for this study. Exclusion criteria included contraindications to the use of nasal airway, the presence of other DMV predictors, severe respiratory or circulatory dysfunction, and refusal to participate. The patients were told the details of the trial protocol and the written informed consent was obtained from each patient included in the study.
Randomization and blinding
The random allocation sequence was generated by the computer at a 1:1 ratio with a block size of 8. A researcher not involved in patient recruitment sealed the random numbers in sequentially numbered opaque envelopes. The envelopes were opened in recruitment order at the start of anesthesia induction and the patients were assigned to the nasal airway or facemask group by investigators. In this study, patients were blinded to the trial protocol, while the investigators and attending anesthetists were not.
Anesthesia and airway management
Upon arrival at the operating room, routine monitoring, including electrocardiogram, pulse oxygen saturation (SpO2), noninvasive blood pressure and end-tidal partial pressure of CO2 (PETCO2) were commenced, with invasive blood pressure monitored if necessary. Both the nostrils of all patients were topically applied ephedrine. An inflatable facemask of suitable size (3 or 4) (Tuoren Medical Device Co., Ltd., Henan, China) was chosen to reach the best fit for each patient and connected to the breathing circuit (Tuoren Medical Device Co., Ltd., Henan, China) for preoxygenation (both groups) and for facemask ventilation (facemask group). After preoxygenation, etomidate (0.2–0.3 mg/kg), alfentanil (30–40 µg/kg), and rocuronium (0.6 mg/kg) were slowly administered intravenously for anesthesia induction. The patients were ventilated with one of the two ventilation techniques after the disappearance of eyelash reflex.
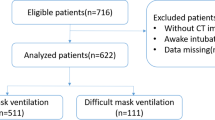
In the nasal airway group, an appropriately sized (6 or 7) and lubricated nasal airway (Naso-Flo®, Medis Medical Device Co., Ltd., Tianjin, China) was inserted through a clear nostril and directly connected to the breathing circuit, followed by an improved sealing maneuver, in which the mouth and lips were shut tightly by one hand of the operator and the nostrils were occluded with the thumb and forefinger of another hand, based on the maneuver previously described by Beattie16 (Fig. 1A). In the facemask group, moistened gauzes were placed at the hollow cheeks14 to improve the facemask seal and ventilation was performed using a two-handed “VE-clamp” technique, in which the facemask was held firmly over the face with the thumbs and thenar eminence of the operator along two sides of the facemask and a jaw-thrust maneuver was performed with the other fingers of both hands, as detailed in the previous study18 (Fig. 1B). A volume-controlled mode of the anesthesia ventilator (Primus Dräger, Lübeck, Germany) was used for ventilation, with a preset oxygen flow of 8 L/min, tidal volume of 8 mL/kg, ventilatory rate of 15 bpm, and a limit of peak inspiratory pressure of 25 cmH2O.
Two ventilation techniques. (A) The nasal airway ventilation technique, in which the mouth and lips were shut tightly by one hand of an operator and the nostrils were occluded with the thumb and forefinger of another hand. (B) The facemask ventilation technique, in which moistened gauzes were placed at the hollow cheeks and two-handed “VE-clamp” facemask ventilation was performed.
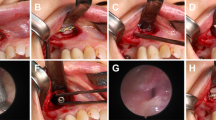
The ventilation procedures during anesthesia induction were performed by two experienced anesthetists. If adequately exhaled CO2 (i.e. PETCO2 ≥ 10 mmHg19 could not be achieved during a 1-minute attempt by an operator, it was defined as difficult ventilation. Subsequently, another operator would help seal either the mouth (nasal airway group) or the facemask (facemask group). If ventilation remained inadequate or SpO2 dropped below 90% (i.e. hypoxemia), urgent tracheal intubation would be performed. Tracheal intubation would be implemented 3 min later if ventilation was adequate. The details on the process of airway management were shown in (Fig. 2).
Measurements and data collection
The primary outcome was the Vte during anesthesia induction, which was defined as the average Vte per kilogram of body weight measured in the first minute after the cessation of spontaneous respiration and calculated by dividing the minute ventilation by a respiratory rate of 15 and the body weight. Secondary outcomes were as follows: (1) the incidence of successful ventilation during anesthesia induction, which was defined as the absence of difficult ventilation during single-person ventilation; (2) the incidence of adverse events during anesthesia induction, including hypoxemia, mandibular dislocation, eye injury, nasal mucosal injury and esophagogastric reflux.
Patient demographic and clinical parameters, including age, gender, BMI, ASA physical status, Mallampati Score, gastric tube insertion, and the Vte immediately after tracheal intubation, were also recorded.
Sample size calculation
The sample size was calculated according to the primary outcome. Based on our pilot study of 20 patients, the standard deviation of the Vte during anesthesia induction was 1.5 in the facemask group and average between-group difference was 1.2 mL/kg. Considering a dropout rate of 20%, a sample size of 40 patients per group was needed to achieve a power of 90% with a type I error of 0.05.
Statistical analyses
SPSS 26.0 (IBM, Armonk, NY, USA) and R version 4.3.0 (R Foundation for Statistical Computing, Vienna, Austria) were used for statistical analyses. Quantitative variables were presented as mean (standard deviation) or median (interquartile range, IQR) based on distribution, assessed using the Shapiro–Wilk test. Their between-group comparisons were performed by student t test or Mann–Whitney U test. Categorical variables were reported as number (percentage) and analyzed using χ2 test or Fisher exact test as appropriate. The primary outcome was also reported with median difference and 95% confidence interval. P < 0.05 was considered statistically significant (two-tails).
Post hoc exploratory analyses were conducted in the subgroups based on whether a gastric tube was inserted or not, which was considered to affect the facemask seal and the effect size of the intervention. Additionally, we assessed the effect of the intervention after adjusting for age, gender, BMI, and Mallampati Score. P-values were corrected for multiple comparisons (Bonferroni correction), and statistical significance was set at 0.025.
Results
Study population
From August 2022 to May 2023, a total of 156 elderly patients were screened for eligibility in the study, and 76 of them were excluded during enrollment (55 did not meet the inclusion criteria, 6 declined to participate, 5 had severe respiratory or circulatory dysfunction, 10 had contraindications to the use of nasal airway). The remaining 80 patients were randomized to the two groups and finally analyzed. The flow chart of included and excluded patients was shown in (Fig. 3). The two groups were comparable with respect to demographic and clinical characteristics of patients (Table 1).
Primary outcome
The Vte during anesthesia induction was significantly increased in the nasal airway group (median 5.6 mL/kg, IQR 5.0–5.9), compared with the facemask group (median 3.6 mL/kg, IQR 2.6–4.5), with a median difference of 1.9 mL/kg (95% CI 1.4 to 2.3; P < 0.001; Fig. 4).
Secondary outcomes
The incidence of successful ventilation during anesthesia induction was 40 out of 40 (100%) in the nasal airway group, compared with 33 out of 40 (82.5%) in the facemask group (P = 0.018; Table 2). In the facemask group, DMV occurred in 7 patients (17.5%) during single-person ventilation, 4 of whom were adequately ventilated using a two-person technique, while the remaining 3 required urgent tracheal intubation.
There was no significant difference in the incidence of adverse events during anesthesia induction between groups (P = 1.000; Table 2). Hypoxemia occurred in 2 of 3 patients who received urgent tracheal intubation in the facemask group with the lowest SpO2 ≥ 85%. Two patients experienced mandibular dislocation in the facemask group and manual reduction was performed immediately. In the nasal airway group, mild nasal mucosal injury was observed in 3 patients and no patient felt nasal uncomfortable during postoperative follow-up.
Exploratory analyses
Post hoc analyses were conducted to explore the effectiveness of the two ventilation techniques in subgroups based on whether a gastric tube was inserted or not. The results showed that the nasal airway ventilation was more effective than facemask ventilation in both subgroups, particularly in the subgroup with gastric tube insertion. The effect of the intervention remained consistent in both adjusted and unadjusted analyses (all P < 0.001; Table 3).
Discussion
To our best knowledge, this study was the first to quantitatively assess the efficacy and safety of the nasal airway ventilation technique during anesthesia induction in edentulous patients. Our results demonstrated that compared to the conventional facemask ventilation, the nasal airway ventilation significantly increased the Vte and the incidence of successful ventilation during anesthesia induction in edentulous patients. This finding was supported by a previous report in available literature16. Additionally, the patients in the nasal airway group only had minimal adverse events, primarily mild nasal mucosal injury, without the occurrences of hypoxemia and mandibular dislocation.
In addition to relieving upper airway obstruction, the nasal airway used in our study can be directly connected to the anesthesia ventilator. For effective ventilation, moreover, not only a patent airway but also a satisfactory seal of the ventilation system was required. Considering teeth loss and lips retraction in edentulous patients, we improved the maneuver of occluding the external nares and mouth by using two hands to obtain a sufficient upper airway seal, on the basis of the methods described by Beattie16. Our experience indicates that this technique may well meet the above requirements of successful ventilation and is more effective than facemask ventilation in edentulous patients.
The present study selected the Vte during anesthesia induction as primary outcome, because it can be objectively measured. The results showed that the median Vte was 5.6 mL/kg in the nasal airway group compared to 3.6 mL/kg in the facemask group. The increase of Vte in our study was smaller than that reported in previous work of Racine et al.2, who compared conventional facemask ventilation with another facemask ventilation maneuver—placing the caudal end of a facemask on the lower lip with two hands. In that study, however, the lower lip facemask placement was only used in edentulous patients experiencing DMV, which may explain the larger increase of Vte. As the ___location of the cephalad end of the facemask was not clearly provided in their article, moreover, it was unclear if the patient’s eyes might be pressed. In addition, this facemask ventilation technique may result in a mandibular dislocation because of requiring a powerful jawthrust maneuver to open airway and the relaxed temporomandibular joint in elderly people. In our study, two patients in the facemask group experienced a mandibular dislocation during ventilation, while no patient suffered this adverse event in the nasal airway group due to without a need of jawthrust maneuver.
The incidence of DMV in the facemask group was 17.5% in this study, with a hypoxemia episode in 2 patients, which are in agreement with findings of previous work2,3. In contrast, no patient in the nasal airway group experienced difficult ventilation and hypoxemia episode. Although all cases of DMV were managed with two-person mask ventilation and urgent tracheal intubation, there is often a lack of available anesthetists. Furthermore, urgent tracheal intubation can lead to significant hemodynamic instability, potentially triggering cardiovascular or cerebrovascular events in elderly patients. It must be noted that the definitions for DMV in the available literature are often subjective or complex13,20. The Lim and Nielsen scale, based on the best capnograph during ventilation, defines PETCO2 < 10 mmHg and no PETCO2 as DMV simply and objectively19. Therefore, this scale was chosen to evaluate ventilation outcomes in the current study.
In our study, successful ventilation, defined as the absence of difficult ventilation during single-person ventilation, was observed in 82.5% of patients in the facemask group, which was considerably higher than the 49% reported in Conlon et al.‘s study5. Except for the various definitions of successful ventilation in our and their studies, these different findings may be also attributable to the diverse facemask ventilation methods. In the present study, the moistened gauzes were placed at the hollow cheeks14 and a two-handed “VE-clamp” facemask ventilation technique was used to enhance facemask seal and prevent airway obstruction18,21,22, whereas only a one-handed “CE-clamp” facemask ventilation technique was applied in the previous study5. Furthermore, Conlon et al.5 demonstrated that leaving dentures in situ during facemask ventilation increased successful ventilation by 24%. However, this strategy is limited to patients with dentures and carries a risk of denture aspiration. Our findings showed that successful ventilation was achieved in all patients using the nasal airway ventilation technique, with only 3 patients experiencing mild nasal mucosal injury. Particularly, post hoc exploratory analyses indicated that the ventilation efficacy of this technique was superior in edentulous patients with gastric tube insertion, who were hard to be adequately ventilated with facemask strategies, due to challenges in achieving a proper facemask seal.
Our study introduced a nasal airway ventilation technique appropriate for edentulous patients during anesthesia induction. This approach ensures adequate ventilation before tracheal intubation, reducing the risk of hypoxemia and the need for urgent tracheal intubation, while also supporting hemodynamic stability. The technique is straightforward, requiring minimal skill and equipment, making it a valuable alternative to facemask ventilation. Additionally, it may benefit patients with beards or maxillofacial deformities.
This study had several limitations that need special attention. Firstly, both the investigators and attending anesthetists were not blinded to the group allocations. In order to decrease selection bias, investigators opened the allocation envelopes at the start of anesthesia induction. Secondly, this study did not include a group in which patients were ventilated using a facemask combined with an oral or nasal airway during anesthesia induction. However, we speculate that ventilation efficacy of using a facemask combined with an oral or nasal airway in edentulous patients would not be better than the nasal airway ventilation technique used in this study, because of inadequate facemask seal. However, further studies to confirm the speculation are needed. Lastly, this study did not record the age at which patients became edentulous. Available literature indicates that patients who are edentulous for many years tend to have more significant changes of facial morphology relative to progressive atrophy of the edentulous jaws4.
Conclusion
Our findings demonstrated that the nasal airway ventilation technique significantly and safely improved ventilation by increasing the Vte and the incidence of successful ventilation during anesthesia induction in edentulous patients. Thus, this technique can serve as a valuable alternative when facemask ventilation is inadequate and we recommend the preemptive preparation of a nasal airway prior to anesthesia induction in these patients.
Data availability
The data generated and analysed during this study are available from the corresponding author on reasonable request.
References
Qin, X. et al. Projecting trends in the disease burden of adult edentulism in China between 2020 and 2030: a systematic study based on the global burden of disease. Front. Public. Health 12, 1367138. https://doi.org/10.3389/fpubh.2024.1367138 (2024).
Racine, S. X. et al. Face mask ventilation in edentulous patients: a comparison of mandibular groove and lower lip placement. Anesthesiology 112, 1190–1193. https://doi.org/10.1097/ALN.0b013e3181d5dfea (2010).
Langeron, O. et al. Prediction of difficult mask ventilation. Anesthesiology 92, 1229–1236. https://doi.org/10.1097/00000542-200005000-00009 (2000).
Sutton, D. N., Lewis, B. R. K., Patel, M. & Cawood, J. I. Changes in facial form relative to progressive atrophy of the edentulous jaws. Int. J. Oral Maxillofac. Surg. 33, 676–682. https://doi.org/10.1016/S0901-5027(03)00132-2 (2004).
Conlon, N. P., Sullivan, R. P., Herbison, P. G., Zacharias, M. & Buggy, D. J. The effect of leaving dentures in place on bag-mask ventilation at induction of general anesthesia. Anesth. Analg. 105, 370–373. https://doi.org/10.1213/01.ane.0000267257.45752.31 (2007).
Bucca, C. et al. Tooth loss and obstructive sleep Apnoea. Respir. Res. 7, 8. https://doi.org/10.1186/1465-9921-7-8 (2006).
Cohen, A. M. & Vig, P. S. Lateral tongue spreading. J. Dent. 2, 32–34. https://doi.org/10.1016/s0300-5712(73)80007-7 (1973).
Sanders, A. E., Akinkugbe, A. A., Slade, G. D. & Essick, G. K. Tooth loss and obstructive sleep apnea signs and symptoms in the US population. Sleep. Breath. 20, 1095–1102. https://doi.org/10.1007/s11325-015-1310-z (2016).
Boidin, M. P. Airway patency in the unconscious patient. Br. J. Anaesth. 57, 306–310. https://doi.org/10.1093/bja/57.3.306 (1985).
Nandi, P. R., Charlesworth, C. H., Taylor, S. J., Nunn, J. F. & Doré, C. J. Effect of general anaesthesia on the pharynx. Br. J. Anaesth. 66, 157–162. https://doi.org/10.1093/bja/66.2.157 (1991).
Eastwood, P. R., Szollosi, I., Platt, P. R. & Hillman, D. R. Comparison of upper airway collapse during general anaesthesiaand sleep. Lancet 359, 1207–1209. https://doi.org/10.1016/S0140-6736(02)08224-7 (2002).
Cheney, F. W., Posner, K. L., Lee, L. A. Caplan, R. A. & Domino, K. B. Trends in anesthesia-related death and brain damage: A closed claims analysis. Anesthesiology 105, 1081–1086. https://doi.org/10.1097/00000542-200612000-00007 (2006).
Apfelbaum, J. L. et al. American society of anesthesiologists practice guidelines for management of the difficult airway. Anesthesiology 136, 31–81 https://doi.org/10.1097/ALN.0000000000004002 (2022).
Xue, F. S., Xiong, J., Yuan, Y. J., Wang, Q. & Liao, X. Face mask ventilation using a lower lip face mask placement in edentulous patients. Anesthesiology 114, 462–463. https://doi.org/10.1097/ALN.0b013e318204e140 (2011).
Rao, V., Kosik, E., Ganta, R. & Windrix, C. Mask ventilation in edentulous and bearded patients. Anesth. Analg. 112, 1513–1514. https://doi.org/10.1213/ANE.0b013e318215d34c (2011).
Beattie, C. The modified nasal trumpet maneuver. Anesth. Analg. 94, 467–469. https://doi.org/10.1097/00000539-200202000-00045 (2002).
Schulz, K. F., Altman, D. G. & Moher, D. Consort 2010 statement: updated guidelines for reporting parallel group randomised trials. BMC Med. 8, 18. https://doi.org/10.1186/1741-7015-8-18 (2010).
Fei, M. et al. Comparison of effectiveness of two commonly used two-handed mask ventilation techniques on unconscious apnoeic obese adults. Br. J. Anaesth. 118, 618–624. https://doi.org/10.1093/bja/aex035 (2017).
Lim, K. S. & Nielsen, J. R. Objective description of mask ventilation. Br. J. Anaesth. 117, 828–829. https://doi.org/10.1093/bja/aew368 (2016).
Han, R., Tremper, K. K., Kheterpal, S. & O’Reilly, M. Grading scale for mask ventilation. Anesthesiology 101, 267. https://doi.org/10.1097/00000542-200407000-00059 (2004).
Joffe, A. M., Hetzel, S. & Liew, E. C. A two-handed jaw-thrust technique is superior to the one-handed EC-clamp technique for mask ventilation in the apneic unconscious person. Anesthesiology 113, 873–879. https://doi.org/10.1097/ALN.0b013e3181ec6414 (2010).
Isono, S. One hand, two hands, or no hands for maximizing airway maneuvers? Anesthesiology 109, 576–577. https://doi.org/10.1097/ALN.0b013e3181870a5d (2008).
Acknowledgements
We thank all participating patients and our colleagues in operating room for their support during this trial.
Author information
Authors and Affiliations
Contributions
L.-L. W.: study design, study implementation, data analyses, and writing—original draft.X.-G. G.: study design, data analyses, and writing—review & editing.Y. L.: study implementation, data curation, and writing—original draft. F.-S. X.: writing—review & editing.J.-J. Y.: study design, project administration, supervision, and writing—review & editing. All authors read and approved the final manuscript to be submitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, LL., Guo, XG., Li, Y. et al. A randomized controlled trial of nasal airway ventilation technique in edentulous patients during anesthesia induction. Sci Rep 15, 14828 (2025). https://doi.org/10.1038/s41598-025-99789-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-99789-w