Abstract
Programmed cell deaths (PCDs) are crucial for tumor progression. By analyzing 18 PCDs, we generated a robust multigene signature, Combined Cell Death Index (CCDI), comprising necroptosis and autophagy genes for non-small cell lung cancer (NSCLC). The CCDI accurately stratified patients by survival prognosis and predicted immunotherapy responses. We validated CCDI and prioritized CCDI genes using five single-cell RNA sequencing and two spatial transcriptomics datasets. CCDI positively correlates with tumor malignancy, invasiveness, and immunotherapy resistance. Four necroptosis genes (PTGES3, MYO6, CCT6A, and CTSH) may affect cancer cell evolution. In vitro, CTSH overexpression or PTGES3 knockdown inhibited NSCLC cell proliferation and migration while inducing necroptosis with necrosome formation. Moreover, we observed diminished CTSH, heightened PTGES3, and low necroptosis activity in 12 pairs of NSCLC tumors and normal tissues. CTSH overexpression or PTGES3 knockdown induced necroptosis and improved anti-PD1 therapy efficiency in syngeneic cancer mouse models. These findings indicate necroptosis genes as potential therapeutic targets in cancer treatments.
Similar content being viewed by others
Introduction
Non-small cell lung cancer (NSCLC), constituting about 85% of lung cancers, is a major cause of cancer mortality. Its high mortality is largely due to late diagnosis, tumor aggressiveness, and treatment resistance1. The 5-year survival rate for NSCLC is about 25%, dropping to 5–10% in advanced stages2. Immunotherapy is promising in treating NSCLC, yet reliable biomarkers to predict response are lacking3. Effective markers can tailor treatments to individuals, enhancing efficacy and reducing toxicity.
Multigene predictive models surpass single genes in forecasting prognosis and drug responses in cancers4. These models could reveal biological effects and prognostic information missed by single-gene analyses. Numerous multigene signature models have been developed over the years, with some already implemented in clinical practice, such as the application of Oncotype DX in breast cancer, a 21-gene assay5,6. However, NSCLC multigene panels are still in early development.
Programmed cell death (PCD) is a regulated process of controlled self-destruction. PCDs have long been associated with tumor development, metastasis, immunogenicity, and therapy response, driving the development of many prognostic signatures7,8,9,10. Eighteen forms of PCD have been identified, including intrinsic11 and extrinsic apoptosis12, necroptosis13, cuproptosis14, oxeiptosis15, ferroptosis16, alkaliptosis17, pyroptosis18, parthanatos19, autophagic cell death (ACD)20, lysosome-dependent cell death (LCD)21, disulfidptosis22, immunogenic cell death (ICD)23, entosis13, anoikis24, NETosis25, methuosis26, and paraptosis27 (Table 1). We collected PCD-related genes to develop and compare various prognostic models. Ultimately, the model integrating 9 ACD and 11 necroptosis genes demonstrated superior predictive capabilities. Autophagy is a crucial cellular process that degrades and recycles components to support cell survival. Necroptosis is a programmed necrotic cell death28. Autophagy and necroptosis are intricately linked to tumor immunity, affecting tumor development and the immune response29. Thus, we investigated the robustness of CCDI in predicting response to immunotherapy, validated across seven ICI clinical trials in various cancers30,31,32,33,34,35,36.
Unlike bulk RNA-seq, which averages gene expression from mixed cells, single-cell RNA sequencing (scRNA-seq) detects RNA from individual cells, revealing diverse cell populations in a tumor. Additionally, spatial transcriptomics (ST) integrates gene expression analysis with spatial context, mapping gene profiles to specific tissue locations. We then identified key CCDI genes using scRNA-seq and ST datasets. We analyzed five public scRNA-seq data comparing normal tissue with primary tumors, primary tumors with metastatic tumors, and metastatic tumors with lymph node and brain metastases, as well as immunotherapy responders vs. nonresponders. We tracked cell differentiation and developmental trajectories, dynamically monitoring CCDI gene expression across different cell states and transitions in the tumor microenvironment (TME). Moreover, using ST data, we mapped CCDI gene expression to tissue architecture, visualizing gene expression patterns and cell distribution in situ. We identified CCDI genes CTSH and PTGES3 as key regulators of cell differentiation and fate. Finally, we analyzed the two genes’ functions in vitro and their impact on NSCLC sensitivity to anti-PD-1 antibodies in a mouse model.
Results
Establishing and validating models for 18 PCDs and CCDI
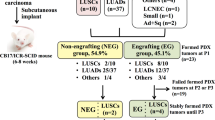
As shown in the graphical summary (Fig. 1a and Supplementary Fig. 1), we first established and evaluated prognostic models for each PCD form using univariable and multivariable Cox regression analyses (Supplementary Fig. 2a–r). To create combined models, we selected five signatures (ACD, necroptosis, LCD, ICD, and oxeiptosis) with AUCs exceeding 0.7 at four or more time points over 5 years, ensuring robust predictive power and stability across long-term dynamic cancer progression intervals (Fig. 1b). The model integrating ACD and necroptosis achieved the highest predictive accuracy (AUC = 0.800) (Fig. 1c), which was termed the combined cell death index (CCDI) for subsequent analysis. CCDI assigned each patient a risk score (range: 0–1) based on gene expression and weights, with a cutoff of >0.34 indicating high risk while ≤0.34 indicating low risk. A higher CCDI risk score is associated with a worse patient prognosis. Henceforth, ‘CCDI’ refers to ‘CCDI risk score,’ and ‘ACD’ and ‘necroptosis’ are used similarly. The time-dependent ROC curves demonstrated that CCDI consistently showed robust performance in predicting survival at 1, 2, 3, 4, and 5 years (Fig. 1d). Kaplan–Meier survival curves for the TCGA-LUAD cohort indicated that CCDI better stratifies survival outcomes than individual ACD and necroptosis signatures (Fig. 1e). UMAP analysis confirmed CCDI’s effectiveness in distinguishing patients with favorable and poor prognoses (Fig. 1f). CCDI contains 9 ACD (RAC1, PRKCD, MBTPS2, EIF4G1, EIF2AK3, CCR2, BNIP3L, ATIC, ATG12) and 11 necroptosis genes (TP53I3, PTGES3, PLEC, PKP2, MYO6, GSK3A, FLNC, CTSH, CD40LG, CCT6A, AURKA) (Supplementary Fig. 3). The CCDI model outperformed ACD and necroptosis models in prognosis prediction, validated in five NSCLC datasets (Supplementary Fig. 4a–c).
a The graphic abstract of the study. b Area under the curve (AUC) values of time-dependent ROC curves for 1- to 5-year survival predictions of 18 PCD models are shown, with each point representing the AUC and vertical lines indicating the 95% confidence interval (CI). c ROC curves for autophagic cell death (ACD), necroptosis, and combined cell death index (CCDI) models for overall survival (OS). d Time-dependent ROC curves for the CCDI model at 1, 2, 3, 4, and 5 years. e Kaplan–Meier curves for high-risk and low-risk patient subgroups classified by risk scores of ACD, necroptosis, and CCDI models. Dashed lines represent the 95% CI of survival curves. (The high-risk and low-risk groups were distinguished by the minimum p-value method; log-rank test, P < 0.0001). f Assessment of the ability of ACD, necroptosis, and CCDI models discriminating between low-risk and high-risk groups with Uniform Manifold Approximation and Projection (UMAP). PCD programmed cell death, DSP digital spatial profiling, ICI immune checkpoint inhibitor, ICD immunogenic cell death, LCD lysosome-dependent cell death, SC single-cell, ST spatial transcriptomic, ROI regions of interest, AIS adenocarcinoma in situ, MIA minimally invasive adenocarcinoma, IAC invasive adenocarcinoma, NMPR non-major pathological response, MPR major pathological response, T tumor in situ, M metastatic tumor, LDH lactate dehydrogenase, Co-IP co-immunoprecipitation. *P < 0.05, **P < 0.01, ***P < 0.001.
Predicting responses to ICIs in NSCLC patients using CCDI
Given ACD and necroptosis’s link to tumor immunogenicity and immunotherapy29, we evaluated CCDI’s ability to predict ICI response. We first examined the association between CCDI and various immune-related genes out of 47 immune checkpoints or regulatory factors (Supplementary Fig. 5a, b). The immunophenotype score (IPS) evaluates immunotherapy sensitivity, with higher scores indicating greater sensitivity37. The low-risk group had higher IPS and greater responsiveness to anti-PD-1/L1/L2 therapies than the high-risk group (Fig. 2a). Third, the ImmuCellAI also indicated that the low-risk group might have better ICI responses (Fig. 2b and Supplementary Fig. 5c–g). By adopting three NSCLC ICI trials with known therapy responses as training sets, the SubMap algorithm verified that CCDI could successfully predict ICI response in the TCGA-LUAD cohort (Fig. 2c and Supplementary Fig. 5h–l). Finally, we substantiated the CCDI’s capacity to predict immunotherapy response with seven additional clinical trials with ICIs (Fig. 2d–l). In the IMvigor210 dataset (n = 310, metastatic urothelial carcinoma treated with anti-PD-L1)30, CCDI significantly stratified patients by survival (Fig. 2d–f). Moreover, low-risk patients tended to respond to ICIs than high-risk counterparts across melanoma31, renal cell carcinoma32, esophageal adenocarcinoma (EAC)33, and NSCLC34,35,36, with lower CCDI in responders than nonresponders (Fig. 2g–l), indicating CCDI’s potential for selecting ICI candidates across cancers.
a Box plot showing the difference in immunophenotype score (IPS) and response to ICIs between high- and low-risk subgroups of TCGA-LUAD cohort (n = 514) separated by CCDI. A higher IPS indicates greater tumor immunogenicity and a higher likelihood of responding to IPS. b The proportion of patients predicted by ImmuCellAI to respond to ICIs in high-risk and low-risk TCGA-LUAD subgroups. c The ICI response of high- and low-risk TCGA-LUAD subgroups was predicted using the SubMap algorithm with three NSCLC ICI trials as training sets. d–l Validation of CCDI’s ability to distinguish between ICI responders and nonresponders across various cancer types. Kaplan–Meier survival curves for the high and low-risk subgroups of the IMvigor210 cohort defined by CCDI (log-rank test, P < 0.0001) (Bladder urothelial carcinoma, n = 310) (d) and distribution and average values of CCDI among these patients with complete response (CR), partial response (PR), stable disease (SD), progressive disease (PD), and those not estimated (NE) (e, f). The differences in anti-PD-1/L1 treatment response and CCDI between high and low-risk subgroups across different cohorts: GSE78220 (melanoma, n = 28) (g), GSE67501 (human renal cell carcinoma, n = 11) (h), GSE165252 (esophageal adenocarcinoma, n = 40) (i), GSE126044 (NSCLC, n = 16) (j), GSE135222 (NSCLC, n = 27) (k), and GSE190265 (NSCLC, n = 34) (l). *P < 0.05, **P < 0.01, ***P < 0.001.
Differences in tumor-immune microenvironment between the high and low-risk groups
When applying ESTIMATE in the TCGA-LUAD dataset, we observed higher immune and stromal scores in the low-risk group (Supplementary Fig. 6a, b), while CCDI was negatively correlated with these scores (Supplementary Fig. 6c, d). The MCP counter identified significant differences in NK, B, stromal cells, and neutrophils between the two groups (Supplementary Fig. 6e) and the correlation between CCDI and these cells (Supplementary Fig. 6f). Reduced NK cells in the high-risk group might reflect impaired antitumor immunity. Moreover, CIBERSORT-ABS, EPIC, CIBERSORT, QUANTISEQ, TIMER, and XCELL confirmed different immune cell infiltration patterns between the groups and correlations between risk scores and immune cell subgroups (Supplementary Fig. 6g, h).
Dynamic alterations of CCDI and its genes during lung cancer cell state transition
In a LUAD scRNA-seq dataset by Philip Bischoff et al. (n = 24)38 (Fig. 3a and Supplementary Fig. 7a), CopyKAT, evaluating epithelial cells’ single-cell CNV, was used to distinguish malignant (aneuploid) from non-malignant (diploid) cells (Fig. 3b). Malignant cells were further clustered into C1–C3 subgroups, with the CCDI scores increasing (Fig. 3c). GSVA revealed increased activity in tumor-promoting (EMT, cell cycle, angiogenesis, Wnt) and decreased activity in tumor-suppressive pathways (e.g., necroptosis, apoptosis, and p53) in C3 vs. C1 cells (Fig. 3d). Differential expression analysis revealed upregulation of CCDI genes CCT6A and PTGES3 in C2 and C3, whereas CTSH was upregulated in C1 and downregulated in C2 and C3 (Fig. 3e). Slingshot’s trajectory analysis revealed dynamic changes in PTGES3, CCT6A, CTSH, and MYO6 expression during malignant epithelial cell progression (Fig. 3f, g). Consistent results were observed in another LUAD scRNA-seq dataset (GSE123902, n = 17) (Fig. 3h, i and Supplementary Fig. 7b–g). Therefore, these CCDI genes may regulate lung cancer cell evolution.
a The t-distributed stochastic neighbor embedding (t-SNE) plot shows the main cell groups from Philip Bischoff’s LUAD scRNA-seq dataset (n = 12). b The Uniform Manifold Approximation and Projection (UMAP) plot of epithelial cells exhibits diploid tumor cells and aneuploid normal cells, as inferred from scRNA-seq data using the Copy Number Karyotyping of Tumors (CopyKAT) algorithm. c The UMAP plot illustrates the distinct subpopulations of malignant epithelial cells. d This heatmap visualizes the pathway activity scores for different malignant epithelial cell subpopulations, as determined by Gene Set Variation Analysis (GSVA). e Volcano plot of differentially expressed genes (DEGs) in malignant epithelial cell subpopulations. f Trajectory analysis of malignant cells inferred by slingshot, mapping the progression of cells through different states over time or differentiation. g Gene pseudotime expression map demonstrated the dynamic changes in CCDI gene expression during the malignant epithelial cell progression. Each plot tracks the expression profiles of a CCDI gene along the inferred cellular trajectory. The x-axis represents pseudotime or progression stages, while the y-axis denotes gene expression levels. Color gradients or line plots depict the shifts in gene expression, highlighting key regulatory changes that occur as malignant epithelial cells evolve. h, i The above analysis was validated in the GSE123902 cohort (LUAD, n = 17).
Association of lung cancer metastasis with CCDI and constituent genes
The scRNA-seq data (GSE131907) involved biopsies from 44 patients with lung cancer in situ (tLung), lung cancer with metastasis (tL/B) and lymph node metastasis (mLN), and brain metastases (mBrain) (Fig. 4a, b and Supplementary Fig. 8)39. GSVA indicated increased activity in some tumor-related pathways (orange rectangle) and elevated CCDI in tumor cells of the tL/B and mLN groups, while immune responses progressively decreased (Fig. 4c). High-risk patients were more likely to develop lymph node and brain metastasis and progress to stage IV tumors than the low-risk group (Fig. 4d, e), suggesting CCDI’s potential in distinguishing early- and late-stage lung cancer. The tL/B and mLN tumor cells with the highest CCDI were further clustered into C1 to C4 subpopulations (Fig. 4f). CCDI and tumor-related pathway activity (orange rectangle) increased from C1 to C4 (Fig. 4g). Slingshot analysis mapped a pseudotemporal transition from C1 to C4 (Fig. 4h), aligning with CCDI gene expression variations (Fig. 4i). Moreover, another DSP dataset (GSE200563) confirmed increased tumor pathway activity and CCDI in mLN (Fig. 4a, j, k), suggesting a correlation between CCDI and the metastatic transition of cancer cells.
a Flowchart for this part of the study consisting of a scRNA-seq dataset (GSE131907, n = 58) and a digital spatial profiling (DSP) dataset (GSE200563, n = 109). b The t-SNE plot shows major cell populations derived from the scRNA-seq data of lung cancer in situ (tLung), lung cancer with metastasis (tL/B), metastatic lymph node (mLN), and brain metastases (mBrain) (GSE131907, n = 32). c Heatmap of pathway activity scores estimated by GSVA and CCDI for different tissue types. d, e Forty-four patients were assigned CCDI scores and divided into low- and high-risk groups, with histograms showing the percentages of patients with tLung, tL/B and mLN, and mBrain (d) and patients in I to IV clinical stages (e) for the two subgroups. f Malignant cells were split into C1–C4 subgroups. g This heatmap illustrates pathway activity scores derived from GSVA and CCDI across C1–C4 cancer cell subpopulations, along with their correlation. h The trajectories of malignant cells derived from the Slingshot trajectory inference method. i CCDI gene expression levels shift along the trajectory of LUAD malignant epithelial subgroups. The CCDI was also applied to a DSP dataset of LUAD (GSE200563), containing the primary lung carcinoma (L), metastatic lymph node (mLN), and brain metastasis (LB) tissues. Overall, 109 regions of interest (ROIs) were picked separately from areas enriched with tumor cells and areas infiltrated with immune cells in tumor samples and were subjected to transcriptomic analysis. j The heatmap was used to visualize pathway activity scores evaluated by GSVA and CCDI for tumor cell-enriched ROIs in indicated tissues. k The difference in CCDI levels among tumor cells of indicated tissues. *P < 0.05, **P < 0.01, ***P < 0.001.
Spatial distribution of CCDI and its genes during the LUAD invasion
We analyzed the LUAD scRNA-seq dataset (GSE189357) comprising 88,411 cells from in situ (AIS), minimally invasive (MIA), and invasive adenocarcinoma (IAC), with two samples per tumor state40 (Fig. 5a and Supplementary Fig. 9a, b). The same tissues also underwent Visium spatial analysis (GSE189487). GSVA indicated increasing tumor malignancy and CCDI levels from AIS to MIA to IAC (Fig. 5b). CCDI negatively correlated with mast cells, fibroblasts, neutrophils, and DCs (Supplementary Fig. 9c), along with correlations for the four CCDI genes (Supplementary Fig. 9d). Given the importance of cell spatial distribution in cancer malignancy41,42, we used cell type markers from matched scRNA-seq data to annotate the 17,022 Visium spots, mapping cells to their tissue locations (Fig. 5c). Spatial gene expression analysis showed that as LUAD progressed from AIS to IAC, PTGES3 and CCDI levels increased, while CTSH levels decreased in tumor tissue structures (Fig. 5d). We isolated and analyzed C1–C3 tumor cell subgroups from an IAC sample, and the original study identified C3 as highly malignant40. PTGES3 expression increased from C1 to C3 (Fig. 5e, f), suggesting its role in regulating the transition from the less malignant C1 and C2 to the highly malignant C3. Overall, CCDI is closely related to LUAD progression.
The LUAD tissues from which the scRNA-seq dataset (GSE189357, n = 6) was obtained were the same as those used for the Visium spatial transcriptomic dataset (GSE189487, n = 6). a The t-SNE plot shows major cell types inferred from LUAD scRNA-seq data, including lung adenocarcinoma in situ (AIS), minimally invasive adenocarcinoma (MIA), and invasive adenocarcinoma (IAC) (GSE189357). b This heatmap presents pathway activity scores and CCDI for tumors at different stages, as evaluated by GSVA. c Using cell type markers identified from the above scRNA-seq data to annotate the spatial gene expression data from Visium, thereby mapping cell types to their locations within the tissue section, two samples for each tumor status (GSE189487). d Using Visium spatial transcriptomic data to map the levels of CCDI and CCDI genes back to tissue structures for indicted samples (Each point represents the expression level of CCDI-related genes and CCDI scores in each spot; The color depth indicates the relative expression level of the corresponding indicator). e Malignant epithelial cells were extracted from an IAC sample for subpopulation analysis (C1–C3) and spatial trajectory analysis, and then the cell subpopulations were mapped back to tissue architecture. f The dynamic increase in expression levels of PTGES3 during the evolution of spatial trajectories. *P < 0.05, **P < 0.01, ***P < 0.001.
Dynamics of CCDI in NSCLC treated with PD-1 blockade and chemotherapy
We retrieved scRNA-seq data from 8 LUAD patients undergoing chemotherapy combined with PD-1 blockade, involving 45,408 single cells (GSE207422, n = 8) (Fig. 6a and Supplementary Fig. 10a, b). The GSVA unveiled more active immune-related pathways and lower CCDI in the major pathological response (MPR) than in the non-MPR (NMPR) group, potentially explaining their differential responses to chemoimmunotherapy (Fig. 6b). The ROC curve showed that CCDI effectively assessed chemoimmunotherapy efficacy (Fig. 6c). Differential analysis also reveals MYO6 upregulation in the MPR group and elevated CCT6A in the NMPR group (Fig. 6d). T-cell analysis revealed that the MPR group had more NK cells and less CD4+ T-cell exhaustion (Tex) than the NMPR group (Fig. 6e and Supplementary Fig. 10c). CCDI was negatively correlated with NK cells and positively with CD4+ Tex cells (Fig. 6f, g). Subgroup analysis of myeloid cells and B cells indicated increased plasma cells and decreased M1 macrophages and cDC1 cells in the MPR group, with CCDI negatively correlated with these cell types (Fig. 6h–l and Supplementary Fig. 10d, e). This suggests that variations in tumor-immune cell infiltration may impact chemoimmunotherapy efficacy, with CCDI potentially predicting this efficacy. Using ‘Copykat’ and ‘inferCNV’, we found that tumor cells have higher CNV than normal lung cells, with CCDI positively correlated with CNV (Fig. 6m–p and Supplementary Fig. 10f, g). This may partly explain the association between CCDI and poor prognosis, likely reflecting increased tumor malignancy and reduced treatment sensitivity.
a Landscape of main cell types from a LUAD scRNA-seq dataset, as visualized in the t-SNE plot. Patients underwent chemoimmunotherapy, with three responders reaching major pathologic response (MPR) and five nonresponders (non-MPR, NMPR) (GSE207422, n = 8). b Heatmap of pathway activity scores and CCDIs for each responder and nonresponder. c ROC curve analysis of the CCDI model illustrates its predictive performance for immunotherapy outcomes. d Volcano plot exhibiting differentially expressed genes (DEGs) between MPR and NMPR groups (The black dots represent the positions of CCDI-related genes). e–l The association of immune cell subsets with chemoimmunotherapy response and CCDI. UMAP plot of T cell (e), myeloid cell (h), and B cell (k) subsets. Histogram showing the percentage of major immune cell subsets between NMPR and MPR groups (e, h, k). Scatterplot of the correlation between CCDI and NK (f), CD4+ Tex (g), M1 macrophage (i), cDC1 (j), and plasma cell (l) in the TCGA-LUAD cohort. m. UMAP plots showing the major cell types of lung epithelial cells. n The Copykat assesses the benignity and malignancy of epithelial cells. o CNV (Copy Number Variation) levels among epithelial cell subgroups. p Scatterplot of the correlation between CCDI and CNV of malignant cells. *P < 0.05, **P < 0.01, ***P < 0.001.
Functional analysis of CTSH and PTGES3
We analyzed PTGES3 and CTSH levels in indicated cell lines (Fig. 7a) and confirmed CTSH overexpression and PTGES3 knockdown in NSCLC cells (Fig. 7b, c). CTSH overexpression or PTGES3 depletion inhibited the proliferation and migration of NSCLC cells (Fig. 7d–g). Such gene manipulations also caused membrane disruption and cell death, reversible by NSA and RIPA-56 (Fig. 7h–k). Moreover, the same genetic manipulations could activate the kinases like Receptor-Interacting Protein Kinase 1 (RIPK1)/RIPK3/pseudokinase Mixed Lineage Kinase Domain-Like protein (MLKL) necroptotic pathway, which was reversed in a concentration-dependent manner by necroptosis inhibitors NSA and RIPA-56 (Fig. 7l–o). Necrosome, indicated by RIPK1-RIPK3 complex assembly, is a hallmark of necroptosis41. Co-IP results show enhanced necrosome formation in NSCLC cells with CTSH overexpression or PTGES3 knockdown (Fig. 7p, q). Additionally, we detected reduced CTSH and increased PTGES3 in tumors, correlating with decreased RIPK3 and MLKL expression, indicating reduced necroptosis (Fig. 8a–i). Necroptosis has immunogenic potential42. In vivo study indicated that Ctsh overexpression and Ptges3 knockdown inhibited tumor growth, induced necroptosis, and enhanced ICI therapy efficacy, as shown by necroptosis makers, tumor growth curves, and weight measurements (Fig. 8j–r). IHC analysis showed that overexpressing CTSH and silencing PTGES3 genes significantly increased CD8+ cytotoxic T cells and CD4+ helper T cells while reducing FOXP3+ regulatory T cells in tumor tissues compared to controls. These effects were further enhanced with PD-1 antibody treatment, suggesting a synergistic boost in antitumor immunity. Thus, regulating Ptges3 and Ctsh could inhibit tumor growth and modulate the TME to boost immunotherapy (Fig. 9a–d).
a CTSH and PTGES3 in normal lung epithelial cells and indicated NSCLC cell lines were analyzed using Western blot. b, c The efficacy of CTSH overexpression in H1299 cells and PTGES3 knockdown in A549 cells was confirmed by qRT-PCR (b) and Western blot analysis (c). d, e CCK-8 assays evaluated the impact of CTSH overexpression (d) and PTGES3 knockdown (e) on NSCLC cell proliferation. f, g Transwell assays (f) and wound healing assays (g) were conducted to investigate the effects of CTSH overexpression and PTGES3 knockdown on cell migration against their respective controls. h–k LDH release assays measured cell membrane damage resulting from CTSH overexpression (h, i) or PTGES3 knockdown (j, k) and the counteractive effects of NSA (15 μM) and RIPA-56 (1.0 μM). l–o Western blot analysis detected levels of necroptosis biomarkers in cells with CTSH overexpression (l, m) and PTGES3 knockdown (n, o), following treatment with varying concentrations of necrosulfonamide (NSA) and RIPA-56, necroptosis inhibitors, for 24 h. p, q Co-immunoprecipitation (Co-IP) results demonstrated that CTSH overexpression (p) and PTGES3 knockdown (q) enhanced the interaction of RIPK3 and MLKL with RIPK1. *P < 0.05, **P < 0.01, ***P < 0.001.
a Western blot was used to assess the expression of CTSH, PTGES3, RIPK3, and MLKL in normal and adjacent non-tumor tissues from patients with NSCLC. b–i The transcripts of these genes were measured with qRT-PCR (b–e), followed by correlation analysis (f–i). j Schematic diagram of the animal experiment design. Immune-competent wild-type C57BL/6 mice were subcutaneously injected with genetically manipulated Lewis lung carcinoma 1 (LLC1) cells to establish syngeneic mouse models of lung adenocarcinoma. k, l Representative tumors treated with Ctsh overexpression/shPtges3, mouse anti-PD-1 antibodies, and their combination. m, n Western blot analysis to measure necroptosis markers in tumors with the indicated treatment. o–r Weights (o, p) and volume growth curves (q, r) of LLC1 lung tumors. *P < 0.05, **P < 0.01, ***P < 0.001.
Immunohistochemical (IHC) analysis of CD8, CD4, and FOXP3 expression in syngeneic mouse lung cancer tumor tissues following Ptges3 silencing and Ctsh overexpression accompanying PD-1 antibody treatment. a–d Representative IHC staining images and quantitative analysis demonstrated that silencingPtges3 and overexpressing Ctsh significantly increased CD8+ and CD4+ T-cell infiltration while decreasing FOXP3+ regulatory T cells compared to the control group. These effects were further amplified in the PD-1 antibody-treated group, indicating enhanced antitumor immunity. Data are presented as mean ± SD, with statistical significance indicated. *P < 0.05, **P < 0.01, ***P < 0.001.
Discussion
This CCDI, including necroptosis and ACD genes, remarkably improves patient classification for survival prognoses and ICI therapy predictions, validated through multiple bulk RNA-seq, scRNA-seq, and spatial transcriptomics datasets. Key CCDI genes, MYO6, CCT6A, CTSH, and PTGES3, are related to tumor cell differentiation and fate. Furthermore, CTSH and PTGES3 regulate necroptosis and boost the efficacy of anti-PD-1 therapy when manipulated to induce necroptosis.
Recent efforts have developed predictive models using single PCD signature genes, but their success in predicting cancer prognosis and drug response remains moderate9,43,44,45,46,47. A single PCD type-based model is inadequate to capture tumor features due to the redundancy and crosstalk in cell death pathways48. Therefore, predicting models incorporating multiple PCD types have merged lately49,50,51,52. The combined multi-cell death forms model offers a comprehensive view of disease complexity and adapts better to patient heterogeneity. The current CCDI with an AUC of 0.8 surpassed many existing LUAD prognostic signatures, such as the aneuploidy-based gene signature53, vitamin metabolism clustering-related gene signature54, glycosyltransferase gene signature55, immune-related lncRNA pair signature56, m6A RNA methylation regulators57, and signature derived from diverse cell death patterns58.
Despite the promising performance of ICIs, effective biomarkers for patient selection remain lacking. Biomarkers, such as PD-L1 expression, microsatellite status (MSI-H), and tumor mutational burden (TMB), face limitations and lack uniform testing protocols59. Given the selective efficacy and frequent serious toxicities60, accurate biomarkers are crucial for selecting suitable patients for ICIs. The CCDI’s ability to predict responses to ICIs was validated via seven ICI cancer trials, including NSCLC, EAC, melanoma, urothelial carcinoma, and renal cell carcinoma30,31,32,33,34,35,36. CCDI shows great potential for survival prediction and personalized ICI therapies.
The robustness of CCDI is further underscored by its validation across multiple high-dimensional datasets, including scRNA-seq and spatial transcriptomics. scRNA-seq provides precise insights by analyzing individual cell gene expressions and leading to a more accurate understanding of biological processes and disease mechanisms61,62,63. We included four LUAD scRNA-seq datasets to validate CCDI involving normal tissue, non-metastatic and metastatic primary tumors, corresponding lymph node and brain metastases, tumors at different invasion and metastasis stages, and tumors undergoing immunotherapy38,39,64. Consistently, we found that CCDI increased as cancer cells progressed into more malignant phenotypes. scRNA-seq analysis showed elevated CCDI levels in tumor cells from metastatic lung cancer and its metastases (lymph nodes and brain) compared to non-metastatic lung cancer. Moreover, cancer cells responsive to ICIs exhibit lower CCDI than their resistant counterparts. Further analysis of immune cell subsets revealed that CCDI was inversely related to NK cells, M1 macrophages, cDC1, and plasma cells but directly related to CD4+ Tex cells, implying a potential link between CCDI and an immunosuppressive TME. Using scRNA-seq data, we validated that CCDI can predict tumor cell malignancy and responsiveness to ICI therapy.
Unlike scRNA-seq, spatial transcriptomics retains the tissue architecture and permits the analysis of how gene expression varies across different tumor regions, enabling the study of intratumoral heterogeneity in situ. Using two spatial transcriptomics datasets with tumor tissues at different stages of invasion and metastasis40,65, we confirmed that CCDI increases with tumor malignancy and invasiveness in the spatial structures. Overall, validation across bulk, scRNA-seq, and spatial transcriptomics enhances the CCDI’s reliability in predicting patient outcomes and guiding therapeutic decisions.
To comprehend the discrepant ICI responses among the two risk groups, we compared the TIME of the two groups and observed differences in IPS, immune scores, stromal scores, and immune cell infiltration patterns. These parameters are all known to be associated with immunotherapy efficacy37,50,66. The CCDI comprised genes related to necroptosis and autophagy, suggesting that differences in necroptosis and autophagy activities may influence TIME. Including necroptosis and autophagy-related genes in the CCDI underscores the complex nature of tumor cell death mechanisms and their combined effect on cancer progression and treatment response. Necroptosis and autophagy/ACD are crucial in cancer biology and immunogenicity. ACD can occur under severe nutrient deprivation or specific cancer treatments. Autophagy may boost immune activation by aiding in the processing and presentation of tumor antigens, helping the immune system recognize and target tumor cells67,68. Conversely, in specific contexts, autophagy can suppress immune responses by regulating inflammation or inhibiting the production of specific cytokines. Mitophagy removes damaged mitochondria, preventing the release of cytosolic mitochondrial DNA that can activate the cGAS-STING pathway and IFN-I secretion, thereby enhancing T-cell cross-priming and boosting the immune response69. Necroptosis is triggered by various stimuli, including death receptor activation and pattern recognition receptors (PRRs)70, featured by necrosome form from RIPK1 and RIPK3 interaction and cell membrane rupture. The resulting release of intracellular contents, including DAMPs (e.g., HMGB1, ATP)71,72, which boost antigen uptake by phagocytes and trigger dendritic cells (DC) maturation, causing efficient CD8+ T-cell cross-priming and enhanced antitumor immunity72.
During tumor progression, cancer cells often advance to more malignant states due to genetic and epigenetic changes, microenvironmental influences, and clonal selection73,74,75. It is indispensable to understand the mechanisms underpinning the heterogeneity and plasticity of cancer cells. scRNA-seq can identify rare cell populations, elucidate cellular interactions, and track dynamic gene expression changes76. Trajectory analysis is crucial for identifying genes driving critical cell state transitions, providing key insights into tumor progression and heterogeneity77. We identified that four necroptosis-related CCDI genes (PTGES3, MYO6, CCT6A, and CTSH) exhibited dynamic expression changes across different tumor cell subpopulations. This strategy aids in deciphering tumor evolution and discovering new biomarkers and potential therapeutic targets related to PCDs. Similarly, we previously found that necroptosis genes HOOK and CUL4A changed with ESCC cell state transitions and verified them as independent predictors of ESCC prognosis50. Using single-cell and functional analyses, Kong et al. revealed that PLK1 drove an immunosuppressive TME in LUAD78. Furthermore, validation with ST datasets strengthens the findings by preserving the spatial context of gene expression.
ST data show that CTSH and PTGES3 vary remarkably across tumor progression and invasion stages. In vitro analyses demonstrated that CTSH overexpression or PTGES3 knockdown inhibited the proliferation and migration of NSCLC cells while inducing necroptosis. Prostaglandin E Synthase 3 (PTGES3) is an enzyme converting prostaglandin endoperoxide H2 (PGH2) into prostaglandin E2 (PGE2). Bioinformatics analysis demonstrates elevated PTGES3 levels in various tumors79,80,81, with its overexpression in LUAD linked to poor prognosis and increased immune cell infiltration79. Drugs like gedunin, genistein, and diethylstilbestrol could target PTGES3 to inhibit breast cancer cell proliferation80. In acute respiratory distress syndrome, the PTGES3/p23 could activate RIPK3/MLKL, driving endothelial cell necroptosis82. Cathepsin H (CTSH) is a lysosomal cysteine proteinase essential for breaking down lysosomal proteins. Our results align with previous studies showing decreased CTSH levels in lung tumors compared to non-tumorous lung tissue, suggesting CTSH may act as a tumor suppressor in LUAD83,84. We also found diminished CTSH and heightened PTGES3 in tumors, along with decreased RIPK3 and MLKL expression, implying lower necroptosis activity. Moreover, the present study demonstrated that altering CTSH and PTGES3 to trigger necroptosis significantly improves the efficacy of anti-PD-1 therapy and enhances antitumor immunnity. ICI’s effectiveness is restricted by primary and acquired resistance, originating from genetic, epigenetic, and metabolic changes that hinder T-cell movement to the tumor, disrupt immune cell function, and impair antigen presentation85. ICI therapy’s success heavily depends on the presence of intratumoral CD8+ T cells. However, ICI alone often fails to significantly increase CD8+ TIL numbers86. Inflammatory PCDs (e.g., pyroptosis and necroptosis) release DAMPs and cytokines, promoting DCs to engulf dying cells, attracting and activating CD8+ T cells. Therefore, ICIs combined with therapies inducing inflammatory cell death may work synergistically87,88. Necroptosis influences the TME by modulating immune cell infiltration and activity, consequently enhancing antitumor immune, potentially making cancer cells more susceptible to immunotherapy42,89. Overall, the induction of necroptosis may be a promising strategy to enhance anti-PD-1 efficacy.
The limitations of the study should be addressed. First, since many publicly stored high-throughput datasets are not accessible, we included clinical trials with heterogeneous treatments, such as immunotherapy alone, chemotherapy combined with immunotherapy, and neoadjuvant chemoimmunotherapy. Second, although our results demonstrate that CCDI shows clinical significance across these datasets, this study is exploratory. Intensive validations are required before its clinical translation, especially in large, well-designed prospective studies. Third, while we acknowledge the significance of known predictors of ICI response, such as PD-L1 expression and the presence of oncogenic drivers (e.g., EGFR and ALK alterations), we chose not to correct the CCDI model for these factors but consider CCDI as a complementary and independent model. Finally, the CCDI model was constructed using bulk RNA sequencing data. We further validate the clinical relevance of CCDI in tumor subpopulations using publicly available scRNA-sequencing datasets. However, accurately quantifying the proportion of CCDI gene expression from non-tumor cells in TME is currently unfeasible. Although this study provides critical insights into tumor-immune interactions, it is inherently limited by its preclinical focus. Future work will explore CCDI’s clinical utility through multicenter cohort studies and integrative analyses with established biomarkers, such as PD-L1 and oncogenic driver status.
In conclusion, CCDI is a comprehensive tool for prognostic and ICI therapeutic prediction. Identifying CTSH and PTEGS3 as key factors in tumor progression and therapy response underscores their potential as novel therapeutic targets, paving the way for more personalized and effective treatments and improving cancer prognosis.
Methods
Data source
Twenty RNA sequencing (RNA-seq) datasets and clinical information were retrieved from several public big data repositories, including the CODE OCEAN (https://codeocean.com/), the Gene Expression Omnibus (GEO) (https://www.ncbi.nlm.nih.gov/geo), the Cancer Genome Atlas (TCGA) (https://www.cancer.gov/tcga/), and the International Cancer Genome Consortium (ICGC) (https://dcc.icgc.org/). Thirteen of them are bulk RNA-seq datasets: TCGA-LUAD (n = 569), ICGC-LUAD (n = 425), GSE31210 (n = 226), GSE72094 (n = 442), GSE50081 (n = 181), GSE37745 (n = 196), GSE78220 (n = 28), GSE67501 (n = 11), GSE190265 (n = 34), GSE126044 (n = 16), GSE135222 (n = 27), GSE165252 (n = 77), and the IMvigor210 cohort (n = 310)30 (Table 2). Additionally, five scRNA-seq datasets were included: GSE123902 (n = 17), GSE189357 (n = 6), GSE131907 (n = 58), GSE207422 (n = 8), and Philip Bischoff’s study (n = 24)38. Furthermore, the study incorporated one digital spatial profiling (DSP) dataset (GSE200563, n = 109) and a Visium spatial transcriptomic (ST) dataset (GSE189487, n = 6) (Table 2).
The signature gene sets and sources for 18 PCD are detailed in Supplementary Table 1, including intrinsic apoptosis (n = 500), extrinsic apoptosis (n = 500), disulfidptosis (n = 10), necroptosis (n = 500), cuproptosis (n = 17), oxeiptosis (n = 146), ferroptosis (n = 283), alkaliptosis (n = 73), pyroptosis (n = 387), parthanatos (n = 23), ACD (n = 232), LCD (n = 194), ICD (n = 500), entosis (n = 23), anoikis (n = 338), NETosis (n = 24), methuosis (n = 8), and paraptosis (n = 23).
Construction and validation of the CCDI model
TCGA-LUAD dataset served as the training set for developing and optimizing the predictive models. Initially, univariate Cox analysis identified significant prognostic genes from PCD signature genes based on overall survival (OS). Multivariate Cox regression then constructed prognostic models for each type of PCD using these gene coefficients by ‘survminer’ (v.0.4.9) and ‘survival’ (v.3.5-8) R packages.
To construct the multivariate Cox regression model, we used the ‘stepAIC’ function from the ‘MASS’ (v.7.3-60.2) R package with ‘bidirectional’ stepwise selection and Akaike Information Criterion (AIC) minimization to determine the optimal model. This approach ensures the robustness and reliability of the prognostic model90. We first constructed and compared prognostic models from individual PCDs and assessed their discriminating accuracy using the Receiver Operating Characteristic (ROC) approach. Both ROC (‘pROC’ R package, v.1.18.5) and time-dependent ROC (‘survivalROC’ R package, v.1.0.3.1) curves at 1, 2, 3, 4, and 5 years were plotted, calculating the Area Under the Curve (AUC). The time-dependent AUCs evaluated each model’s predictive power over different time horizons, providing insight into the models’ effectiveness in distinguishing survival status at specific time points. Higher AUC values indicate better performance. A threshold of AUC > 0.7 was adopted. We considered PCD models with AUC > 0.7 across four or five intervals to be stable and effective. The resulting five models with consistently high performance were used further to build combined models. Next, a series of combination models, comprising 2–5 multigene signatures, were constructed using logistic regression. Among these, one model, integrating ACD and necroptosis, achieved the lowest AIC value and the highest AUC, thus being selected for further investigation and named after CCDI90. The CCDI risk score was calculated using the formula: Risk score \({\rm{CCDI}}=\frac{\exp ({{\rm{\beta }}}_{0}+{{\rm{\beta }}}_{1}{{\rm{\chi }}}_{{ACD}}+{{\rm{\beta }}}_{2}{{\rm{\chi }}}_{{necroptosis}})}{1+\exp ({{\rm{\beta }}}_{0}+{{\rm{\beta }}}_{1}{{\rm{\chi }}}_{{ACD}}+{{\rm{\beta }}}_{2}{{\rm{\chi }}}_{{necroptosis}})}\) for each LUAD patient. In this context, \({{\rm{\beta }}}_{0}\) acts as the intercept, with \({{\rm{\beta }}}_{1}\) and \({{\rm{\beta }}}_{2}\) as the logistic regression coefficients. The risk scores, χACD and χnecroptosis, are derived from “\({{\rm{\chi }}}_{{\rm{ACD}}}={\sum }_{i=1}^{n}{\beta }_{i}{x}_{i}\)” and “\({{\rm{\chi }}}_{{\rm{Necroptosis}}}={\sum }_{j=1}^{n}{\beta }_{j}{x}_{j}\)”, respectively. The minimum P-value method was applied to the Kaplan–Meier curve to determine the CCDI score’s cutoff value, which stratified LUAD patients into high and low-risk groups. The ‘umap’ (v.0.2.10.0) R package was adopted to visualize the distribution disparities in risk scores between high- and low-risk groups as defined by the ACD, necroptosis, and CCDI models. A 1000-fold bootstrap validation was conducted internally for the 18 PCD models and CCDI. Additionally, external validations were performed across five independent datasets (ICGC-LUAD, GSE31210, GSE72094, GSE50081, and GSE37745).
Assessing the ability of the CCDI model’ ability to predict ICI responses
Several approaches were used to verify CCDI’s capacity to predict immune checkpoint inhibitor (ICI) responses. First, a total of reported 47 immune checkpoint (ICP) genes were used91. Second, Immunophenoscore (IPS) is a computational metric generated to evaluate tumor immunogenicity by integrating effector cells, immune suppressor cells, major histocompatibility complex (MHC) molecules (antigen processing), and checkpoint/immune modulators. IPS was developed to quantify the capability of a tumor to elicit an immune response and predict the potential effectiveness of ICIs. The IPS scale spans from 0 to 10, indicating a range from minimal to maximal immunogenicity. IPS for LUAD patients was retrieved from The Cancer Immunome Atlas (TCIA) (https://tcia.at/home)37. Third, the Immune Cell Abundance Identifier (ImmuCellAI, http://bioinfo.life.hust.edu.cn/web/ImmuCellAI/) is a web-based computational tool that estimates the abundance of 24 immune cell types in bulk RNA sequencing (RNA-seq) and microarray data. ImmuCellAI predicts patient responses to ICIs by assuming ICI therapy effectiveness is influenced by specific immune cell types92. Fourth, the Subclass Mapping (SubMap) algorithm compares gene expression profiles from tumor samples with those of patients who have responded to ICIs. By identifying overlaps between new patient cohorts and known responders, SubMap predicts potential responders to similar therapies93. The submap algorithm was used to compare gene expression profiles between individual training datasets and the validation datasets, including TCGA-LUAD, ICGC-LUAD, GSE31210, GSE72094, GSE50081, and GSE37745, to find similarities or “consensus” between them. This evaluation aimed to determine the accuracy of CCDI in predicting responses to ICIs. Three independent clinical trials involving ICIs for the treatment of NSCLC were used as training sets, including GSE126044 (n = 16)34, GSE135222 (n = 27)35, and GSE190265 (n = 34)36.
Finally, we applied CCDI to seven independent immunotherapy trials to assess differences in immunotherapy responses between high- and low-risk groups, including the IMvigor210 dataset (n = 310, metastatic urothelial carcinoma, anti-PD-L1 therapy)30, GSE78220 (n = 28, melanoma, anti-PD-1 therapy)31, GSE67501 (n = 11, renal cell carcinoma, anti-PD-1 therapy)32, GSE165252 (n = 77, esophageal adenocarcinoma, anti-PD-L1 therapy)33, GSE126044 (n = 16, NSCLC,anti-PD-1 therapy)34, GSE135222 (n = 27, NSCLC, anti-PD-1/PD-L1 therapy)35, and GSE190265 (n = 34, NSCLC, chemotherapy and anti-PD-1/PD-L1 therapy)36.
scRNA‑seq data and ST data processing
The raw gene expression matrix obtained from scRNA-seq was transformed into a Seurat object using the ‘Seurat’ (v.4.4.0) R package94. The ‘CreateSeuratObject’ function from the package generated a Seurat object by taking the gene expression matrix as input and organizing it into a structured format suitable for downstream analysis. The Seurat object allows for the efficient handling of scRNA-seq data, enabling advanced functionalities such as quality control, normalization, clustering, and visualization. Cells exhibiting less than 500 genes per cell, more than 2500 genes per cell, or a mitochondrial gene content exceeding 20% were classified as low quality and removed from the analysis. Batch effects were addressed through the application of the ‘RunHarmony’ function from the ‘harmony’ (v.1.2.1) R package95. Dimensionality reduction was undertaken using ‘Seurat’ R package’s ‘RunPCA’, ‘UMAP’, and ‘TSNE’ functions. The “FindClusters” function was used to perform unsupervised clustering (Louvain algorithm), which automatically identifies clusters by optimizing modularity values based on the cell neighborhood network. The final subgroups were determined by integrating dimensionality reduction visualization, stability evaluation, and the expression of specific marker genes. In cluster annotation, reference data for cell annotation were retrieved and integrated from CellMarker (http://xteam.xbio.top/CellMarker/), SingleR (v.2.6.0), and published literature96,97.
Zhu et al. performed both scRNA-seq and Visium spatial transcriptomic analysis on the same LUAD tissues, and the resulting data were deposited as a scRNA-seq dataset (GSE189357) and a Visium ST dataset (GSE189487)40. The ST datasets were imported into Seurat using the ‘Load10X_Spatial’ function. Batch effect correction was implemented utilizing the ‘SCTransform’ function within the ‘Seurat’ R package. Subsequent steps in dimensionality reduction followed a processing workflow akin to that applied to scRNA-seq data. We analyzed and integrated scRNA-seq and spatial transcriptomic data of LUAD of these public LUAD datasets by comparing gene expression profiles from single cells with those in specific spatial regions to infer cell type locations within the tissue. For the cellular-type deconvolution analysis of spatial transcriptomic data, an analysis pipeline based on Robust cellular-type deconvolution (RCTD) was employed to analyze reference data and Visium spatial transcriptomic data98. The doublet mode was set to full mode. Then, we mapped scRNA-seq data back to the original tissue context, visualizing the expression and distribution patterns of targeted genes and CCDI. The CCDI score for each cell or spot was calculated by extracting the expression matrix of the model-related genes and applying it to the risk formula of the model.
Cell trajectory prediction
A trajectory analysis of scRNA‑seq data was conducted using “slingshot” (v.2.12.0) R package to delineate the developmental trajectory of cells and determine the lineage differentiation of distinct cell populations99. For the ST data, cellular evolutionary trajectories were deduced using the R package ‘Monocle’ (v.2.32.0). This input data was a gene-cell matrix at the UMI count scale, derived from the Seurat subset, which was processed with default parameters after downscaling and cell sorting100.
Discrimination of malignant and non-malignant epithelial cells
We identified malignant and non-malignant epithelial cells by using the “copykat” (v.1.1.0)101 and “infercnv” (v.1.20.0)102 R packages. Specifically, “copycat” was run with default settings to identify polyploid and diploid cells. In “infercnv,” cells from the TME were used as normal reference cells according to the “Using 10× data” guidelines, and their copy number variation (CNV) estimates were used to set the baseline. A gene sorting file was generated from the human CRCh38 assembly, incorporating the chromosomal start and end positions for each gene. In the CNV inference analysis, the minimum average read count for each gene in the reference cells was set to 0.1, and the output results underwent denoising to ensure the accurate prediction of CNV levels.
Identifying differentially expressed genes
The Seurat “FindAllMarkers” function, identifying markers of clusters in scRNA-seq data, was employed to detect differentially expressed genes (DEGs) between different groups of cells by clustering algorithms. Wilcoxon rank-sum tests were used to determine the statistical significance. Genes with an absolute log2 fold change (log2FC) ≥ 0.58 and a false discovery rate (FDR) < 0.05 were considered differential within the cellular subgroups by default.
Gene set variation analysis (GSVA)
Gene enrichment analysis was performed using curated gene sets from the Molecular Signatures Database (MSigDB)103. GSVA was implemented through the “GSVA” (v.1.52.3) R package, utilizing gene expression profiles to assess the activity scores for each cell type or sample104. The differences in activity scores were quantified to elucidate variations among different immune cell subtypes, signaling pathways, biological states, and processes across distinct cell clusters or samples.
Evaluation of tumor-immune microenvironment
The “ESTIMATE” (v.1.0.13) R package (Estimation of STromal and Immune cells in MAlignant Tumor tissues using Expression data) was utilized to evaluate differences in stromal scores and immune scores between high and low-risk groups103. The MCP counter method105 and CIBERSORT105 analysis were used to assess immune cell infiltration differences between high- and low-risk groups. These differences were further explored using five methods from the TIMER 2.0 website, including TIMER106, XCell107, EPIC108, QUANTISEQ109, and CIBERSORT-ABS10. The comparison between the high-risk and low-risk groups was conducted using the Wilcoxon test to evaluate significant differences in immune scores, stromal scores, and immune cell infiltration levels between the two groups. The pie chart was drawn based on the relative proportions of each cell type in the high-risk and low-risk groups. The denominator was defined as the total infiltration value of the specific cell type across both groups (i.e., the sum of the infiltration values in the high-risk and low-risk groups), and the relative proportions for the high-risk and low-risk groups were then calculated accordingly. Pearson correlation analysis was conducted to assess the correlations between risk scores and immune scores, as well as their association with immune-infiltrating cells.
Cell culture and reagents
Human lung bronchial epithelial cells (BEAS-2B, cat# CBP60577) were obtained from COBIOER Biosciences Co., Ltd. (Nanjing, China). NSCLC cell lines, including A549 (cat# SCSP-503), PC-9 (cat# SCSP-5085), HCC827 (cat# SCSP-538), NCI-H1299 (cat# SCSP-589), and H1650 (cat# SCSP-592), were sourced from the Cell Bank of the Chinese Academy of Science (Shanghai, China). Murine Lewis lung Carcinoma 1 (LLC1/CL-0140) cells were acquired from Procell Life Science & Technology Co., Ltd. (Wuhan, China). BEAS-2B and LLC1 cells were cultured in DMEM medium (PM150210, Procell, China), while other cell lines in RPMI-1640 medium (PM150110, Procell, China), both supplemented with 10% fetal bovine serum (164210, Procell, China) and 1% penicillin-streptomycin solution (PB180120, Procell, China). Cells were incubated at 37 °C in 5% CO2 with humidity. RIPA-56 (HY-101032, MedChemExpress, Monmouth Junction, NJ, USA), a RIPK3 inhibitor, and necrosulfonamide (NSA) (HY-100573, MedChemExpress, Monmouth Junction, NJ, USA), an MLKL inhibitor, were used to treat A549 and H1299 cells for 24 h to inhibit necroptosis.
Lentivirus infection and plasmid transfection
All the lentiviral vectors and plasmids were obtained from GeneChem Biotechnology Co., Ltd. (Shanghai, China). Regarding human gene manipulation, the CTSH plasmids were used to express CTSH ectopically. The PTGES3 knockdown plasmid, constructed with three unique shRNA sequences: 9893-1 (5′-CGAAGGGACTATGTCTTCATT-3′), 9894-2 (5′-TGTCTCGGAGGAAGTGATAAT-3′), and 9895-1 (5′-GAAGACAGTAAGGATGTTAAT-3′), and the shControl (shCtrl) (CMV-enhancer-MCS-3FLAG-SV40-Puromycin) were used for the loss-of-function study. When the cells reached 70% to 80% confluence, the plasmids (50 nM) were transfected into the human NSCLC cells in 6-well plates using jetPRIME® transfection reagent (101000027, Polyplus Transfection Inc., New York, NY, USA). After 24 h, the expression levels of CTSH and PTGES3 were measured by qRT-PCR and Western blot analysis.
Lentiviral vectors containing the full-length cDNA of mouse Ctsh and an empty vector (Ubi-MCS-3FLAG-SV40-puromycin) were used to overexpress Ctsh in LLC1 cells. We also obtained the shControl (shCtrl) (hU6-MCS-CMV-puromycin) and lentiviral vectors carrying three different shRNA sequences to target the mouse Ptges3 gene: 132643-1 (5′-CGTTTCTCTGAGATGATGGAT-3′), 132644-2 (5′-GCTGTAATTTCATGTATTTAC-3′), and 132645-1 (5′-TACTGGAATGGAGTTTGGTTT-3′). LLC1 cells were cultured in 6-well plates. When cells reached 70% confluence, each well received 8 µl of lentivirus carrying either the Ctsh cDNA or shPtges3 sequences, followed by a 24-h incubation. Stable cell lines were established by adding a puromycin-containing medium (LabGeni, Beijing, China). Protein expression levels of CTSH and PTGES3 in LLC1 cells were then assessed by Western blot analysis.
Quantitative reverse transcription PCR (qRT-PCR)
Total RNA was extracted using TRIzol reagent (Thermo Fisher Scientific, Waltham, MA, USA), and its concentration was determined with a NanoDrop1000 spectrophotometer (NanoDrop, Madison, WI, USA). One μg of RNA was reverse-transcribed into cDNA using the SureScript™ First-Strand cDNA Synthesis Kit (Genecopoeia, Guangzhou, China). qPCR was conducted in a 20 μL reaction volume on a qTOWER 3 Real-Time PCR Thermal Cycler (Analytik, Jena, Germany) containing 10 μL of 2× BeyoFast™ SYBR Green qPCR Mix (Beyotime, Shanghai, China), 2 μL of primers, 2 μL of cDNA templates, and 6 μL of ddH2O. The primers used in this study were as follows: CTSH (Forward primer: 5′-ACTGGTCCCTACCCACCTTC-3′, Reverse primer: 5′-ACAACTGAGGCTGCAAGGAC-3′), PTGES3 (Forward primer: 5′-ACCGGAGAGAAAAAGCGGAG-3′, Reverse primer: 5′-AGAAGCAGGCTGCATTGTGA-3′), RIPK3 (Forward primer: 5′-AAAATGCCCGAGCCTTACCA-3′, Reverse primer: 5′-TGTCTCTCAGCCCCCTGATT-3′), MLKL (Forward primer: 5′-TTTCCCTCAGGAGGCGGT-3′, Reverse primer: 5′-TAACTTCTCAGAGGGCACGC-3′), and GAPDH (Forward primer: 5′-ACAGCCTCAAGATCATCAGC-3′, Reverse primer: 5′-GGTCATGAGTCCTTCCACGAT-3′). Gene expression levels in cells were normalized to GAPDH. The relative gene expression levels were calculated using the formula 2^(-ΔΔCt).
Western blot analysis
Cells were lysed with RIPA buffer (P0013B, Beyotime, China) on ice for 20 min. After centrifugation, the supernatant was collected, and protein concentration was determined using a BCA Protein Assay Kit (P0012S, Beyotime, China). We standardized protein concentration by adding the appropriate amount of loading buffer (P0015, Beyotime, China) to each sample. Equal volumes of protein samples were separated by SDS-PAGE (PG112, Epizyme Biotech, Shanghai, China) and transferred to PVDF membranes (ISEQ00010, Millipore, USA). After blocking, the membranes were incubated with the following primary antibodies under specified conditions: CTSH (1:1000, Cat#10315-1-AP, RRID: AB_2087534, Proteintech, Wuhan, China), PTGES3 (1:1000, Cat#15216-1-AP, RRID: AB_2284772, Proteintech, Wuhan, China), MLKL (1:1000, Cat.#: 380559, Zen Biotechnology Co., Ltd., Chengdu, China), Phospho-MLKL (Ser358) (1:1250, Cat# 382136, Zen Biotechnology Co., Ltd., Chengdu, China), RIPK3 (1:1000, Cat# AF4808, RRID: AB_2844793, Affinity Biosciences, China), Phospho-RIPK3 (1:5000, Cat# 93654, RRID: AB_2800206, Cell Signaling Technology, China), RIPK1 (1:1000, Cat.# 3493, RRID: AB_2305314, Cell Signaling Technology, China), and GAPDH (1:2000, Cat.# 60004-1-Ig, RRID: AB_2107436, Proteintech, Wuhan, China). The following secondary antibodies were used to amplify the signal of the target protein: HRP-conjugated Affinipure Goat Anti-Mouse IgG (H+L) (1:2000, Cat#SA00001-1, RRID: AB_2722565) and HRP-conjugated Affinipure Goat Anti-Rabbit IgG (H+L) (1:2000, Cat#SA00001-2, RRID: AB_2722564, Proteintech, China).
Co-immunoprecipitation (Co-IP)
Cells were lysed on ice using IP lysis buffer (P0013, Beyotime, China) supplemented with PMSF protease inhibitor (ST505, Beyotime, China). Lysates were spun at 13,500 rpm for 5 min to obtain supernatants for the next stage; meanwhile, magnetic agarose beads coated with protein A/G were allowed to conjugate with anti-RIPK1 antibody (Cat# 3493, RRID: AB_2305314, Cell Signaling Technology, China) or IgG (Cat# AC005, ABclonal, Wuhan, China). The resulting complexes were incubated with supernatants overnight at 4 °C. Next day, the immunoprecipitants were washed thoroughly three times, eluted with 1× loading buffer (P0015A, Beyotime, China), and boiled at 99 °C for 5 min. Magnetic beads were removed using a magnetic stand, and the samples were subjected to Western blot analysis. The detection of target proteins was performed using antibodies specifically raised against RIPK1 (Cat# 3493, RRID: AB_2305314, Cell Signaling Technology, China), RIPK3 (Cat# AF4808, RRID: AB_2844793, Affinity Biosciences, China), MLKL (Cat# 380559, Zen Biotechnology Co., Ltd., Chengdu, China), or GAPDH (Cat# 60004-1-Ig, RRID: AB_2107436, Proteintech, Wuhan, China).
Proliferation and migration assay
The Dojindo Cell Counting Kit-8 (CCK-8, GK10001, GlpBio, USA) assay was used to assess cell proliferation, while wound healing and Transwell assays were adopted to evaluate cell migration capabilities. For the CCK-8 assay, 5000 cells were introduced into each well of a 96-well plate (3599, Corning, Tewksbury, MA, USA). Once the cells had fully adhered, cell viability was measured at 0, 24, 48, and 72 h using the CCK-8 assay. Moreover, cells were plated into 6-well plates for the wound healing assay. When the cells reached 95% confluence, a scratch was made to create a wound in the cell monolayer using a pipette tip. The cells were maintained in RPMI-1640 medium (PM150110, Procell, China). Images were captured at 0 and 24 h to measure the scratch gap. During the Transwell migration assay, cells at a density of 3 × 104 per well in serum-free suspension were introduced into the upper chambers of 8 μm Transwell inserts (3422, Corning, Tewksbury, MA, USA). Medium with 10% FBS (164210, Procell, Wuhan, China) was added to the lower chambers. After 24 h, migrated cells were fixed with 4% paraformaldehyde, stained with 0.1% crystal violet, and counted using a microscope.
LDH release assay
Cells were seeded into a 96-well cell culture plate (3599, Corning, Tewksbury, MA, USA) at an appropriate density. Upon cells reaching 80% confluence, lactate dehydrogenase (LDH) levels of the culture medium were measured using an LDH Cytotoxicity Assay Kit (C0016, Beyotime, China) in accordance with the manufacturer’s protocol.
In vivo treatments
Female C57BL/6 mice aged between four and six weeks were purchased from Huachuang Sino (Jiangsu, China). Housing and handling procedures followed protocols approved by the Institutional Review Board at Harbin Medical University. A total of 1 × 106 murine LLC1 cells with Ctsh overexpression or Ptges3 knockdown and control cells were subcutaneously implanted into the right flank of mice. Mouse anti-PD-1 antibody (10 mg/kg, BE0146, BioXcell, Lebanon, NH, USA) or IgG (A7050, Beyotime, China) was intraperitoneally administrated three times a week, beginning on the seventh day after cell implantation. Tumor dimensions were measured with calipers, and the volume was determined using the formula: 0.5 × length × width × height. At the end of the experiment, mice were euthanized using CO2 inhalation followed by cervical dislocation to ensure humane sacrifice in accordance with institutional animal care guidelines.
All research procedures were approved by the Ethics Committee of Harbin Medical University (No. HMUIRB2024009). Written informed consent was obtained from each patient prior to sample collection. Research involving humans has been performed in accordance with the Declaration of Helsinki.
Immunohistochemistry staining (IHC)
The synegenic mouse tumor specimens were fixed, embedded in paraffin, and sectioned into 4 µm thick slices using a Leica microtome. After standard deparaffinization, antigen retrieval, and blocking of nonspecific binding sites, the tissue sections were incubated overnight at 4 °C with primary antibodies against CK (Cat# 10164-2-AP, RRID: AB_2134679, Proteintech), NK (Cat# AG2387, Beyotime), CD11B (Cat# AF6396, Beyotime), CD3 (Cat# 17617-1-AP, RRID: AB_1939430, Proteintech), CD4 (Cat# AG1393, Beyotime), CD8 (Cat# AG1411, Beyotime), and FOXP3 (Cat# 22228-1-AP, RRID: AB_11182376, Proteintech). Next day, HRP-conjugated secondary antibodies (Cat# RGAR011, RRID: AB_3094534, Proteintech) were applied for detection. DAB chromogen (50:1, Novus Biologicals, Centennial, CO, USA) was used for the visualization, followed by hematoxylin counterstaining for nuclear contrast. Sections without the primary antibody were used as negative controls. The stained tumor tissue sections were imaged under a high-resolution microscope, and quantitative analysis was performed using ImageJ (version 1.43) and QuPath (version 0.5.1) software. Representative tumor areas were selected for analysis. The percentage of positive cells was then calculated relative to the total cell count.
Statistics
All statistical analyses were performed using R (version 4.4.0, specific R packages are mentioned in the “Methods” section) and GraphPad Prism (version 9.0). Continuous variables between two groups with equal variances and normal distribution were analyzed using the Student’s t-test; otherwise, the Wilcoxon rank-sum test was used. For comparisons among three or more groups with equal variances and normal distribution, one-way analysis of variance (ANOVA) was used; otherwise, the Kruskal–Wallis test was applied. The Chi-square test was used to assess differences in proportions across multiple groups. All experiments were repeated at least three times, and results for continuous variables are presented as mean ± standard deviation (SD). Unless otherwise stated, P < 0.05 was considered statistically significant.
Data availability
Public data used in this work can be acquired from (TCGA, https://www.cancer.gov/tcga/), the International Cancer Genome Consortium (ICGC, https://dcc.icgc.org/), CODE OCEAN (https://codeocean.com/), and Gene Expression Omnibus (GEO, http://www.ncbi.nlm.nih.gov/geo/). The raw experimental data supporting the conclusions of this article will be made available by the corresponding author.
Code availability
The code involved in the research is reasonably available from the corresponding author.
Abbreviations
- ACD:
-
Autophagic cell death
- AIC:
-
Akaike Information Criterion
- APCs:
-
Antigen-presenting cells
- ATG:
-
Autophagy-related genes
- AUC:
-
Area Under the Curve
- cDC1:
-
Conventional dendritic cell type 1
- CCDI:
-
Combined Cell Death Index
- CCK-8:
-
Cell Counting Kit-8
- cDNA:
-
Complementary DNA
- CNV:
-
Copy number variation
- CR:
-
Complete response
- DCs:
-
Dendritic cells
- DEGs:
-
Differentially expressed genes
- DMEM:
-
Dulbecco’s Modified Eagle Medium
- DSP:
-
Digital Spatial Profiling
- DAMPs:
-
Damage-associated molecular patterns
- EAC:
-
Esophageal adenocarcinoma
- ESCC:
-
Esophageal squamous cell carcinoma
- ESTIMATE:
-
Estimation of STromal and Immune cells in MAlignant Tumor tissues using Expression data
- FDR:
-
False discovery rate
- GEO:
-
Gene Expression Omnibus
- GSVA:
-
Gene Set Variation Analysis
- IAC:
-
Invasive adenocarcinoma
- ICGC:
-
International Cancer Genome Consortium
- ICD:
-
Immunogenic cell death
- ICIs:
-
Immune checkpoint inhibitors
- IHC:
-
Immunohistochemistry
- IPS:
-
Immunophenoscore
- IPR:
-
Immune Phenotype Repertoire
- LDH:
-
Lactate Dehydrogenase
- LCD:
-
Lysosome-dependent cell death
- LLC1:
-
Lewis Lung Carcinoma 1
- LUAD:
-
Lung Adenocarcinoma
- MHC:
-
Major histocompatibility complex
- MIA:
-
Minimally invasive adenocarcinoma
- MIP:
-
Minimum inhibitory power
- MLKL:
-
Mixed Lineage Kinase Domain-Like protein
- MMP:
-
Matrix metalloproteinase
- MPR:
-
Major pathological response
- mRNA:
-
Messenger RNA
- MSI-H:
-
Microsatellite instability-high
- MSigDB:
-
Molecular Signatures Database
- NMPR:
-
Non-major pathological response
- NK:
-
Natural killer
- NSCLC:
-
Non-small cell lung cancer
- PBMCs:
-
Peripheral blood mononuclear cells
- PCD:
-
Programmed cell death
- PD-1:
-
Programmed Death 1
- PD-L1:
-
Programmed Death-Ligand 1
- PGH2:
-
Prostaglandin endoperoxide H2
- PGE2:
-
Prostaglandin E2
- PR:
-
Partial response
- PRRs:
-
Pattern recognition receptors
- PVDF:
-
Polyvinylidene difluoride;
- RIPA:
-
Radioimmunoprecipitation Assay
- RIPK1:
-
Receptor-Interacting Protein Kinase 1
- RIPK3:
-
Receptor-Interacting Protein Kinase 3
- ROC:
-
Receiver Operating Characteristic
- RCTD:
-
Robust cellular-type deconvolution
- scRNA-seq:
-
Single-cell RNA sequencing
- SD:
-
Standard deviation
- ST:
-
Spatial transcriptomics
- TCGA:
-
The Cancer Genome Atlas
- TCIA:
-
The Cancer Immunome Atlas
- TEX:
-
T cell exhaustion
- TIME:
-
Tumor immune microenvironment
- TME:
-
Tumor microenvironment
- TMB:
-
Tumor mutational burden
- UMAP:
-
Uniform Manifold Approximation and Projection
- UMI:
-
Unique molecular identifiers
References
Rotow, J. & Bivona, T. G. Understanding and targeting resistance mechanisms in NSCLC. Nat. Rev. Cancer 17, 637–658 (2017).
Bray, F. et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 74, 229–263 (2024).
Mountzios, G. et al. Immune-checkpoint inhibition for resectable non-small-cell lung cancer - opportunities and challenges. Nat. Rev. Clin. Oncol. 20, 664–677 (2023).
Nicolini, A., Ferrari, P. & Duffy, M. J. Prognostic and predictive biomarkers in breast cancer: Past, present and future. Semin. Cancer Biol. 52, 56–73 (2018).
Cronin, M. et al. Analytical validation of the Oncotype DX genomic diagnostic test for recurrence prognosis and therapeutic response prediction in node-negative, estrogen receptor-positive breast cancer. Clin. Chem. 53, 1084–1091 (2007).
Albanell, J. et al. Prospective transGEICAM study of the impact of the 21-gene Recurrence Score assay and traditional clinicopathological factors on adjuvant clinical decision making in women with estrogen receptor-positive (ER+) node-negative breast cancer. Ann. Oncol. 23, 625–631 (2012).
Yang, Z. et al. Ferroptosis-related lncRNAs: Distinguishing heterogeneity of the tumour microenvironment and predicting immunotherapy response in bladder cancer. Heliyon 10, e32018 (2024).
Zhao, H., Huang, Y., Tong, G., Wu, W. & Ren, Y. Identification of a novel oxidative stress- and anoikis-related prognostic signature and its immune landscape analysis in non-small cell lung cancer. Int J. Mol. Sci. 24, 16188 (2023).
Ling, X. et al. Development of a cuproptosis-related signature for prognosis prediction in lung adenocarcinoma based on WGCNA. Transl. Lung Cancer Res. 12, 754–769 (2023).
Newman, A. M. et al. Robust enumeration of cell subsets from tissue expression profiles. Nat. Methods 12, 453–457 (2015).
Lindsten, T. et al. The combined functions of proapoptotic Bcl-2 family members bak and bax are essential for normal development of multiple tissues. Mol. Cell. 6, 1389–1399 (2000).
Ashkenazi, A. & Dixit, V. M. Death receptors: signaling and modulation. Science 281, 1305–1308 (1998).
Overholtzer, M. et al. A nonapoptotic cell death process, entosis, that occurs by cell-in-cell invasion. Cell 131, 966–979 (2007).
Tsvetkov, P. et al. Copper induces cell death by targeting lipoylated TCA cycle proteins. Science 375, 1254–1261 (2022).
Holze, C. et al. Oxeiptosis, a ROS-induced caspase-independent apoptosis-like cell-death pathway. Nat. Immunol. 19, 130–140 (2018).
Dixon, S. J. et al. Ferroptosis: an iron-dependent form of nonapoptotic cell death. Cell 149, 1060–1072 (2012).
Tang, D., Kang, R., Berghe, T. V., Vandenabeele, P. & Kroemer, G. The molecular machinery of regulated cell death. Cell Res. 29, 347–364 (2019).
Shi, J., Gao, W. & Shao, F. Pyroptosis: gasdermin-mediated programmed necrotic cell death. Trends Biochem Sci. 42, 245–254 (2017).
Wang, Y. et al. Poly(ADP-ribose) (PAR) binding to apoptosis-inducing factor is critical for PAR polymerase-1-dependent cell death (parthanatos). Sci. Signal. 4, ra20 (2011).
Kroemer, G. & Levine, B. Autophagic cell death: the story of a misnomer. Nat. Rev. Mol. Cell Biol. 9, 1004–1010 (2008).
Aits, S. & Jaattela, M. Lysosomal cell death at a glance. J. Cell Sci. 126, 1905–1912 (2013).
Zheng, T., Liu, Q., Xing, F., Zeng, C. & Wang, W. Disulfidptosis: a new form of programmed cell death. J. Exp. Clin. Cancer Res. 42, 137 (2023).
Kroemer, G., Galluzzi, L., Kepp, O. & Zitvogel, L. Immunogenic cell death in cancer therapy. Annu. Rev. Immunol. 31, 51–72 (2013).
Taddei, M. L., Giannoni, E., Fiaschi, T. & Chiarugi, P. Anoikis: an emerging hallmark in health and diseases. J. Pathol. 226, 380–393 (2012).
Papayannopoulos, V. Neutrophil extracellular traps in immunity and disease. Nat. Rev. Immunol. 18, 134–147 (2018).
Maltese, W. A. & Overmeyer, J. H. Non-apoptotic cell death associated with perturbations of macropinocytosis. Front. Physiol. 6, 38 (2015).
Sperandio, S., de Belle, I. & Bredesen DE An alternative, nonapoptotic form of programmed cell death. Proc. Natl Acad. Sci. USA 97, 14376–14381 (2000).
Yan, J., Wan, P., Choksi, S. & Liu, Z. G. Necroptosis and tumor progression. Trends Cancer 8, 21–27 (2022).
Gao, W., Wang, X., Zhou, Y., Wang, X. & Yu, Y. Autophagy, ferroptosis, pyroptosis, and necroptosis in tumor immunotherapy. Signal Transduct. Target. Ther. 7, 196 (2022).
Necchi, A. et al. Atezolizumab in platinum-treated locally advanced or metastatic urothelial carcinoma: post-progression outcomes from the phase II IMvigor210 study. Ann. Oncol. 28, 3044–3050 (2017).
Hugo, W. et al. Genomic and transcriptomic features of response to anti-PD-1 therapy in metastatic melanoma. Cell 165, 35–44 (2016).
Ascierto, M. L. et al. The intratumoral balance between metabolic and immunologic gene expression is associated with anti-PD-1 response in patients with renal cell carcinoma. Cancer Immunol. Res. 4, 726–733 (2016).
van den Ende, T. et al. Neoadjuvant chemoradiotherapy combined with atezolizumab for resectable esophageal adenocarcinoma: a single-arm phase II feasibility trial (PERFECT). Clin. Cancer Res. 27, 3351–3359 (2021).
Cho, J. W. et al. Genome-wide identification of differentially methylated promoters and enhancers associated with response to anti-PD-1 therapy in non-small cell lung cancer. Exp. Mol. Med. 52, 1550–1563 (2020).
Jung, H. et al. DNA methylation loss promotes immune evasion of tumours with high mutation and copy number load. Nat. Commun. 10, 4278 (2019).
Limagne, E. et al. MEK inhibition overcomes chemoimmunotherapy resistance by inducing CXCL10 in cancer cells. Cancer Cell. 40, 136–52.e12 (2022).
Charoentong, P. et al. Pan-cancer immunogenomic analyses reveal genotype-immunophenotype relationships and predictors of response to checkpoint blockade. Cell Rep. 18, 248–262 (2017).
Bischoff, P. et al. Single-cell RNA sequencing reveals distinct tumor microenvironmental patterns in lung adenocarcinoma. Oncogene 40, 6748–6758 (2021).
Kim, N. et al. Single-cell RNA sequencing demonstrates the molecular and cellular reprogramming of metastatic lung adenocarcinoma. Nat. Commun. 11, 2285 (2020).
Zhu, J. et al. Delineating the dynamic evolution from preneoplasia to invasive lung adenocarcinoma by integrating single-cell RNA sequencing and spatial transcriptomics. Exp. Mol. Med. 54, 2060–2076 (2022).
Pasparakis, M. & Vandenabeele, P. Necroptosis and its role in inflammation. Nature 517, 311–320 (2015).
Aaes, T. L. et al. Vaccination with necroptotic cancer cells induces efficient anti-tumor immunity. Cell Rep. 15, 274–287 (2016).
Ba, Y. et al. Pyroptosis-derived long noncoding RNA profiles reveal a novel signature for evaluating the prognosis of patients with lung adenocarcinoma. JCO Precis Oncol. 8, e2300405 (2024).
Mao, X., Huang, W., Xue, Q. & Zhang, X. Prognostic impact and immunotherapeutic implications of NETosis-related prognostic model in clear cell renal cell carcinoma. J. Cancer Res Clin. Oncol. 150, 278 (2024).
Zhang, K., Li, J. & Yuan, E. A necroptosis-related gene signature to predict prognosis and immune features in hepatocellular carcinoma. BMC Cancer 23, 660 (2023).
Li, C., Weng, J., Yang, L., Gong, H. & Liu, Z. Development of an anoikis-related gene signature and prognostic model for predicting the tumor microenvironment and response to immunotherapy in colorectal cancer. Front. Immunol. 15, 1378305 (2024).
Liu, Y. et al. Prognostic implications of autophagy-associated gene signatures in non-small cell lung cancer. Aging 11, 11440–11462 (2019).
Hanggi, K. & Ruffell, B. Cell death, therapeutics, and the immune response in cancer. Trends Cancer 9, 381–396 (2023).
Zou, Y. et al. Leveraging diverse cell-death patterns to predict the prognosis and drug sensitivity of triple-negative breast cancer patients after surgery. Int. J. Surg. 107, 106936 (2022).
Cao, K. et al. Analysis of multiple programmed cell death-related prognostic genes and functional validations of necroptosis-associated genes in oesophageal squamous cell carcinoma. EBioMedicine 99, 104920 (2024).
Liu, X. et al. Panoramic analysis of cell death patterns reveals prognostic and immune profiles of head and neck squamous cell carcinoma. Am. J. Cancer Res. 14, 2584–2607 (2024).
Wu, Z., Jin, M., Xin, P. & Zhang, H. Leveraging diverse cell-death related signature predicts the prognosis and immunotherapy response in renal clear cell carcinoma. Front. Immunol. 14, 1293729 (2023).
Wang, X. et al. Integrated bulk and single-cell RNA sequencing identifies an aneuploidy-based gene signature to predict sensitivity of lung adenocarcinoma to traditional chemotherapy drugs and patients’ prognosis. PeerJ 12, e17545 (2024).
Chen, Y. et al. Identification of a novel prognostic signature based on vitamin metabolism clustering-related genes in lung adenocarcinoma. Transl. Lung Cancer Res. 13, 1084–1100 (2024).
Zhou, J. et al. Identification and validation of a glycosyltransferase gene signature as a novel prognostic model for lung adenocarcinoma. Heliyon 10, e29383 (2024).
Cao, K. et al. Prediction of prognosis and immunotherapy response with a robust immune-related lncRNA pair signature in lung adenocarcinoma. Cancer Immunol. Immunother. 71, 1295–1311 (2022).
Liu, Y. et al. Contributions and prognostic values of m(6) A RNA methylation regulators in non-small-cell lung cancer. J. Cell Physiol. 235, 6043–6057 (2020).
Wang, S. et al. Machine learning reveals diverse cell death patterns in lung adenocarcinoma prognosis and therapy. NPJ Precis. Oncol. 8, 49 (2024).
Holder, A. M. et al. Defining clinically useful biomarkers of immune checkpoint inhibitors in solid tumours. Nat. Rev. Cancer 24, 498–512 (2024).
Postow, M. A., Sidlow, R. & Hellmann, M. D. Immune-related adverse events associated with immune checkpoint blockade. N. Engl. J. Med. 378, 158–168 (2018).
Xue, Q. et al. Promising immunotherapeutic targets in lung cancer based on single-cell RNA sequencing. Front. Immunol. 14, 1148061 (2023).
Traynor, S. et al. Single-cell sequencing unveils extensive intratumoral heterogeneity of cancer/testis antigen expression in melanoma and lung cancer. J. Immunother. Cancer 12, e008759 (2024).
De Zuani, M. et al. Single-cell and spatial transcriptomics analysis of non-small cell lung cancer. Nat. Commun. 15, 4388 (2024).
Laughney, A. M. et al. Regenerative lineages and immune-mediated pruning in lung cancer metastasis. Nat. Med. 26, 259–269 (2020).
Zhang, Q. et al. The spatial transcriptomic landscape of non-small cell lung cancer brain metastasis. Nat. Commun. 13, 5983 (2022).
Yoshihara, K. et al. Inferring tumour purity and stromal and immune cell admixture from expression data. Nat. Commun. 4, 2612 (2013).
Hahn, T. & Akporiaye, E. T. alpha-TEA as a stimulator of tumor autophagy and enhancer of antigen cross-presentation. Autophagy 9, 429–431 (2013).
Li, Y. et al. The vitamin E analogue alpha-TEA stimulates tumor autophagy and enhances antigen cross-presentation. Cancer Res. 72, 3535–3545 (2012).
White, E., Lattime, E. C. & Guo, J. Y. Autophagy regulates stress responses, metabolism, and anticancer immunity. Trends Cancer 7, 778–789 (2021).
Zhang, T., Wang, Y., Inuzuka, H. & Wei, W. Necroptosis pathways in tumorigenesis. Semin. Cancer Biol. 86, 32–40 (2022).
Kaczmarek, A., Vandenabeele, P. & Krysko, D. V. Necroptosis: the release of damage-associated molecular patterns and its physiological relevance. Immunity 38, 209–223 (2013).
Ahmed, A. & Tait, S. W. G. Targeting immunogenic cell death in cancer. Mol. Oncol. 14, 2994–3006 (2020).
Hanahan, D. & Weinberg, R. A. Hallmarks of cancer: the next generation. Cell 144, 646–674 (2011).
Greaves, M. & Maley, C. C. Clonal evolution in cancer. Nature 481, 306–313 (2012).
Polyak, K. Tumor heterogeneity confounds and illuminates: a case for Darwinian tumor evolution. Nat. Med. 20, 344–346 (2014).
Rood, J. E., Maartens, A., Hupalowska, A., Teichmann, S. A. & Regev, A. Impact of the human cell atlas on medicine. Nat. Med. 28, 2486–2496 (2022).
Trapnell, C. et al. The dynamics and regulators of cell fate decisions are revealed by pseudotemporal ordering of single cells. Nat. Biotechnol. 32, 381–386 (2014).
Kong, Y. et al. Single-cell analysis identifies PLK1 as a driver of immunosuppressive tumor microenvironment in LUAD. PLoS Genet. 20, e1011309 (2024).
Gao, P. et al. High expression of PTGES3 is an independent predictive poor prognostic biomarker and correlates with immune infiltrates in lung adenocarcinoma. Int. Immunopharmacol. 110, 108954 (2022).
Yin, Q. et al. The integration of multidisciplinary approaches revealed PTGES3 as a novel drug target for breast cancer treatment. J. Transl. Med. 22, 84 (2024).
Wang, H. et al. Comprehensive pan-cancer analysis of PTGES3 and its prognostic role in hepatocellular carcinoma. Front. Oncol. 13, 1158490 (2023).
Yu, X. et al. A cytosolic heat shock protein 90 and co-chaperone p23 complex activates RIPK3/MLKL during necroptosis of endothelial cells in acute respiratory distress syndrome. J. Mol. Med. 98, 569–583 (2020).
Schweiger, A. et al. Cysteine proteinase cathepsin H in tumours and sera of lung cancer patients: relation to prognosis and cigarette smoking. Br. J. Cancer 82, 782–788 (2000).
Du, Z. et al. A prognostic model of drug tolerant persister-related genes in lung adenocarcinoma based on single cell and bulk RNA sequencing data. Heliyon 9, e20708 (2023).
Bell, H. N. & Zou, W. Beyond the barrier: unraveling the mechanisms of immunotherapy resistance. Annu.p Rev. Immunol. 42, 521–550 (2024).
Tumeh, P. C. et al. PD-1 blockade induces responses by inhibiting adaptive immune resistance. Nature 515, 568–571 (2014).
Rosenbaum, S. R., Wilski, N. A. & Aplin, A. E. Fueling the fire: inflammatory forms of cell death and implications for cancer immunotherapy. Cancer Discov. 11, 266–281 (2021).
Li, S. et al. Targeted therapy for non-small-cell lung cancer: New insights into regulated cell death combined with immunotherapy. Immunol. Rev. 321, 300–334 (2024).
Luo, R. et al. Necroptosis-dependent Immunogenicity of Cisplatin: Implications for Enhancing the Radiation-induced Abscopal Effect. Clin. Cancer Res. 29, 667–683 (2023).
Aho, K., Derryberry, D. & Peterson, T. Model selection for ecologists: the worldviews of AIC and BIC. Ecology 95, 631–636 (2014).
Huang, X., Zhang, G., Tang, T. & Liang, T. Identification of tumor antigens and immune subtypes of pancreatic adenocarcinoma for mRNA vaccine development. Mol. Cancer 20, 44 (2021).
Miao, Y. R. et al. ImmuCellAI: a unique method for comprehensive T-cell subsets abundance prediction and its application in cancer immunotherapy. Adv. Sci.7, 1902880 (2020).
Hoshida, Y., Brunet, J. P., Tamayo, P., Golub, T. R. & Mesirov, J. P. Subclass mapping: identifying common subtypes in independent disease data sets. PLoS ONE 2, e1195 (2007).
Butler, A., Hoffman, P., Smibert, P., Papalexi, E. & Satija, R. Integrating single-cell transcriptomic data across different conditions, technologies, and species. Nat. Biotechnol. 36, 411–420 (2018).
Korsunsky, I. et al. Fast, sensitive and accurate integration of single-cell data with harmony. Nat. Methods 16, 1289–1296 (2019).
Aran, D. et al. Reference-based analysis of lung single-cell sequencing reveals a transitional profibrotic macrophage. Nat. Immunol. 20, 163–172 (2019).
Liu, Z. et al. Progenitor-like exhausted SPRY1(+)CD8(+) T cells potentiate responsiveness to neoadjuvant PD-1 blockade in esophageal squamous cell carcinoma. Cancer Cell. 41, 1852–70.e9 (2023).
Cable, D. M. et al. Robust decomposition of cell type mixtures in spatial transcriptomics. Nat. Biotechnol. 40, 517–526 (2022).
Street, K. et al. Slingshot: cell lineage and pseudotime inference for single-cell transcriptomics. BMC Genomics 19, 477 (2018).
Qiu, X. et al. Reversed graph embedding resolves complex single-cell trajectories. Nat. Methods 14, 979–982 (2017).
Gao, R. et al. Delineating copy number and clonal substructure in human tumors from single-cell transcriptomes. Nat. Biotechnol. 39, 599–608 (2021).
Li, B. et al. Cumulus provides cloud-based data analysis for large-scale single-cell and single-nucleus RNA-seq. Nat. Methods 17, 793–798 (2020).
Subramanian, A. et al. Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. Proc. Natl Acad. Sci. USA 102, 15545–15550 (2005).
Hanzelmann, S., Castelo, R. & Guinney, J. GSVA: gene set variation analysis for microarray and RNA-seq data. BMC Bioinform. 14, 7 (2013).
Petitprez, F. et al. The murine Microenvironment Cell Population counter method to estimate abundance of tissue-infiltrating immune and stromal cell populations in murine samples using gene expression. Genome Med. 12, 86 (2020).
Li, B. et al. Comprehensive analyses of tumor immunity: implications for cancer immunotherapy. Genome Biol. 17, 174 (2016).
Aran, D., Hu, Z. & Butte, A. J. xCell: digitally portraying the tissue cellular heterogeneity landscape. Genome Biol. 18, 220 (2017).
Racle, J., de Jonge, K., Baumgaertner, P., Speiser, D. E. & Gfeller, D. Simultaneous enumeration of cancer and immune cell types from bulk tumor gene expression data. eLife 6, e26476 (2017).
Finotello, F. et al. Molecular and pharmacological modulators of the tumor immune contexture revealed by deconvolution of RNA-seq data. Genome Med. 11, 34 (2019).
Acknowledgements
This work was supported by the Natural Science Foundation of China [82172786 and 82072985], Heilongjiang Provincial Natural Science Foundation of China [ZD2024H003], Beijing Xisike Clinical Oncology Foundation (Y-2024AZ(EGFR)MS-0187), the National Cancer Center Climbing Fund of China [NCC201908B06], and the Climbing Program of Harbin Medical University Cancer Hospital [PDYS2024-02], Heilongjiang Province Innovation Base Award Project [JD2023SJ03], Nn10 Project of Harbin Medical University Cancer Hospital [Nn102024-05].
Author information
Authors and Affiliations
Contributions
All authors contributed to the study's conception and design. Data preparation, collection, and analysis were performed by Kui Cao, Shenshui Wei, Tianjiao Ma, Jinhong Zhu, Jianqun Ma, Hongxue Meng, Xinxin Yang, Mengdi Lu, Yuwen Bai, Yuning Wang, Cuicui Qi, Xiangrong He, Luquan Zhang, and Lijuan Li. Jinhong Zhu and Mengdi Lu accessed and verified the underlying data. Reconciliation of underlying data was solved by Jianqun Ma and Jinhong Zhu. The draft of the manuscript was written by Jinhong Zhu, Kui Cao, and Jianqun Ma. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Cao, K., Wei, S., Ma, T. et al. Integrating bulk, single-cell, and spatial transcriptomics to identify and functionally validate novel targets to enhance immunotherapy in NSCLC. npj Precis. Onc. 9, 112 (2025). https://doi.org/10.1038/s41698-025-00893-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41698-025-00893-x