Abstract
Parkinson’s disease (PD) is an incurable, progressive and common movement disorder that is increasing in incidence globally because of population aging. We hypothesized that the landscape of rare, protein-altering variants could provide further insights into disease pathogenesis. Here we performed whole-exome sequencing followed by gene-based tests on 4,298 PD cases and 5,512 controls of Asian ancestry. We showed that GBA1 and SMPD1 were significantly associated with PD risk, with replication in a further 5,585 PD cases and 5,642 controls. We further refined variant classification using in vitro assays and showed that SMPD1 variants with reduced enzymatic activity display the strongest association (<44% activity, odds ratio (OR) = 2.24, P = 1.25 × 10−15) with PD risk. Moreover, 80.5% of SMPD1 carriers harbored the Asian-specific p.Pro332Arg variant (OR = 2.16; P = 4.47 × 10−8). Our findings highlight the utility of performing exome sequencing in diverse ancestry groups to identify rare protein-altering variants in genes previously unassociated with disease.
Similar content being viewed by others
Main
Parkinson’s disease (PD) is a common neurodegenerative disease that is unrelenting and progressive. It presents as a movement disorder characterized by slowness of movement, tremors, stiffness and difficulty with balance, together with a broad array of non-motor symptoms1,2. Although levodopa and other adjunctive medications alleviate the symptoms of PD, no cure has yet been found. The incidence of PD is expected to rise rapidly in the coming decades because of the aging population. There is, thus, a pressing need for new therapeutic approaches, with the hope that biological insights arising from molecular genetic studies could illuminate these otherwise elusive drug targets.
Owing to reports of positive family histories in many affected individuals, PD has long been suspected to be heritable. Genome-wide association studies (GWASs) of PD have identified close to 100 loci associated with disease risk3,4,5,6,7,8,9. Although these studies highlighted key genes and biological pathways that play a role in the pathogenesis of PD, they also underscore the very heterogeneous nature of the disease in terms of causative mechanisms.
The genomic/risk loci identified by GWASs of PD mostly have modest effect sizes (odds ratios (ORs) < 1.4) and were often located in non-coding regions of the human genome9. Their non-coding nature makes pinpointing the effector genes challenging. In contrast, analysis of protein-altering genetic variants using whole-exome sequencing (WES) has identified causative genes and facilitated advances in the treatment of other diseases through the identification and development of new drug targets10,11. In studies on familial, early-onset PD, several genes containing rare functionally deficient genetic variants have been found12,13,14,15,16,17,18,19,20,21,22,23,24,25,26. Such variants were highly penetrant and were seldom seen in patients with sporadic PD27. In the case of adult-onset sporadic PD, the effect of individual rare genetic variants remains difficult to assess, but the aggregation of rare variant counts within each gene could allow for detection of statistically significant differences in mutational ‘burden’ between cases and controls. These gene-based tests of mutational burden are often limited by constraints in accuracy of pathogenicity prediction using bioinformatic algorithms28 because not all variants that are predicted to impair protein function actually do so. Conversely, variants that are predicted to be benign could result in a loss of function of the encoded protein.
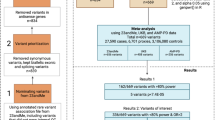
The objective of this study was to assess the contribution of rare coding sequence genetic variants to the pathogenesis of PD. We performed WES on 9,810 participants of Asian ancestry (4,298 PD cases and 5,512 unaffected controls) from Singapore (SG), Malaysia (MAL), Hong Kong (HK), South Korea (KR) and Taiwan (TW). We attempted to replicate two significantly associated genes in a further 11,227 participants (5,585 PD cases and 5,642 controls) from three independently ascertained collections of Asian and European ancestry. We used functional assays to validate and refine gene-based mutational burden tests.
Results
Rare coding variants identified by WES
We recruited 4,915 PD cases together with 5,971 ancestry-matched and geographically matched controls from five regions across East Asia (SG, MAL, HK, KR and TW) and analyzed a total of 4,298 PD cases and 5,512 controls by WES after stringent quality control filtering (total n = 9,810; Supplementary Tables 1–3 and Supplementary Fig. 1). Only samples confirmed by principal component analysis (PCA) to be of Han Chinese and South Korean ancestries were retained (Supplementary Figs. 2 and 3). We identified a total of 721,643 non-synonymous variants across 17,396 autosomal genes, of which 701,048 were rare (minor allele frequency (MAF) < 1%) in the sequenced dataset as well as in publicly available datasets (Genome Aggregation Database (gnomAD) East Asian samples). After annotation with the PolyPhen-2 and LOFTEE algorithms, 367,878 potentially pathogenic variants (hereafter termed ‘qualifying variants’) remained for further analysis.
Gene-level association testing revealed exome-wide significant PD associations with carriage of qualifying variants in GBA1, HLA-DRB1 and SMPD1 (Fig. 1, Extended Data Fig. 1 and Supplementary Table 4). All three genes were expressed in the human midbrain (Supplementary Results, Supplementary Tables 5–7 and Supplementary Figs. 4–6).
a, Quantile–Quantile plot of observed and expected CMH P for autosomal genes with OR > 1. b, Forest plot of SMPD1 association in assessed populations. CMH without continuity correction was used across strata. Data are presented as OR and 95% CI. All P values presented are unadjusted. Exome-wide significance was set at P < 2.5 × 10−6 (two-tailed), taking into account multiple hypothesis testing correction for an estimated 20,000 protein-coding genes in the human genome.
GBA1 and SMPD1 qualifying variants are associated with higher PD risk
At GBA1, 128 of 4,298 PD cases (2.98%) carried qualifying variants compared to 16 of 5,512 controls (0.29%; OR = 10.28, 95% confidence interval (CI) = 5.96–17.75, P = 4.07 × 10−25; Supplementary Table 8 and Extended Data Fig. 2). The carriage of 22 East Asian–specific rare deleterious GBA1 variants was strongly and consistently associated with increased risk of PD (OR = 25.83, P = 6.19 × 10−11) compared to non-carriers (Supplementary Table 9).
Turning to SMPD1, 100 of 4,298 PD cases (2.33%) carried qualifying variants compared to 69 of 5,512 controls (1.25%; OR = 2.32, 95% CI = 1.68–3.20, P = 1.37 × 10−7; Table 1, Fig. 1 and Supplementary Tables 10 and 11). The SMPD1 association was driven by one particular variant (p.Pro332Arg) in the Discovery cohort (allele frequency: PD cases = 0.8%, controls = 0.4%; OR = 2.39; P = 5.01 × 10−6). When we excluded p.Pro332Arg from the analysis, the significant association between burden of SMPD1 qualifying variants and increased PD risk remained (OR = 2.31, P = 0.00369), suggesting that the association between rare, independent genetic variants in SMPD1 was not confined to p.Pro332Arg alone.
We did not observe significant differences in effect sizes between males and females at GBA1 (males: OR = 10.03, 95% CI = 4.53–22.21; females: OR = 9.90, 95% CI = 4.75–20.62; Phet = 0.981) or SMPD1 (males: OR = 2.63, 95% CI = 1.68–4.12, females: OR = 1.96, 95% CI = 1.22–3.14; Phet = 0.376).
We did not observe significant association at genes previously implicated in autosomal dominant, recessive29,30,31 or X-linked PD32 (Supplementary Tables 12 and 13) or genes identified by a recent WES study in individuals of European ancestry27 (Supplementary Table 14). We also did not observe significant PD associations (P < 0.00058, Bonferroni correction for 86 tested genes) in genes involved in lysosomal storage disorders (Supplementary Table 15)33,34.
Validation of qualifying SMPD1 variants associated with increased PD risk
As the association between rare GBA1 variants and increased PD risk has been confirmed26, we focused on evaluating whether the association between rare SMPD1 variants and PD could be replicated in additional independent samples. We pursued validation in 5,585 PD cases and 5,642 controls from three studies of Asian and European ancestry (Supplementary Table 16). Participants from these three studies have undergone whole-exome or whole-genome sequencing, with documented equal re-sequencing of cases and controls35, and had SMPD1 data available. Stratified meta-analysis of the three Replication collections showed that carriers of SMPD1 qualifying variants remain overrepresented in PD cases (139 carriers in 5,585 PD cases, 2.5%) compared to controls (87 carriers in 5,642 controls, 1.5%) (OR = 1.45, P = 0.0071). When all Discovery and Replication samples were meta-analyzed (9,883 PD cases and 11,154 controls across seven independent strata), genome-wide significant association between carriage of SMPD1 qualifying variants and susceptibility to PD was observed (OR = 1.77, P = 4.94 × 10−8; Fig. 1 and Supplementary Table 17).
We observed significant heterogeneity (I2 index for heterogeneity = 79.6%, P = 0.027) in OR between the Discovery (OR = 2.32) and Replication (OR = 1.45) cohorts, which could be due to misclassification of qualifying variants by the PolyPhen-2/LOFTEE algorithm. Resolving this would necessitate the design of functional assays to measure the activity of each SMPD1 allele for comparison against wild-type SMPD1. Alleles that demonstrate significant loss of function compared to wild-type would be included in the revised gene-based burden test. Conversely, alleles that show indistinguishable functional activity from wild-type SMPD1 would be excluded from gene-based burden tests regardless of PolyPhen-2/LOFTEE prediction. SMPD1 encodes for acid sphingomyelinase (ASM), an enzyme responsible for breaking down sphingomyelin to ceramide and phosphorylcholine36. Complete deficiency of ASM leads to Niemann–Pick disease type A/B (NPD-A/B). We designed enzymatic assays to measure ASM activity for 125 SMPD1 genetic variants detected across Discovery and Replication samples (Fig. 2a,b, Supplementary Figs. 7–10, Supplementary Table 17 and Supplementary Results). For the assays, we created 126 HEK293T stable cell lines expressing each SMPD1 genetic variant and ‘wild-type’ ASM. Confocal microscopy confirmed correct localization of wild-type ASM to the lysosomes in the HEK293T cell line (Fig. 2c and Supplementary Fig. 11).
a, Activity levels are presented as percentage of wild-type ASM activity; error bars represent standard deviation. Each variant was assayed in technical replicates of 3–6. b, Predicted deleterious variants (75 variants) have significantly lower ASM activity than predicted benign variants (47 variants). Median, 25th–75th quartiles; whiskers of 1.5× IQR shown in boxplot. *** Two-sided t-test P < 0.001. Red dotted line: 100% activity of wild-type variants. Blue dotted line: activity level (43.58%) significantly associated with variant carrier frequency in case and control. Details are provided in Supplementary Table 17. c, SMPD1 wild-type protein localizes to the lysosome. Representative image from three captured fields of view is shown (Supplementary Fig. 11). Yellow signal: SMPD1. Magenta signal: lysosome. Cyan signal: nuclei. Scale bar, 10 µm. IQR, interquartile range; WT wild-type.
The functional spectrum of ASM activity for all tested SMPD1 variants ranged from normal (>90% of wild-type activity) to severe loss of function (<20% of wild-type activity). Two of the variants tested are causative of NPD-A/B (SMPD1 p.Leu304Pro (or p.Leu302Pro37) and p.Arg498Leu38) and, thus, served as positive controls for our experiment. Unsurprisingly, both variants ranked in the bottom 10th percentile of ASM activity (p.Leu304Pro: 8.7% activity, p.Arg498Leu: 5.6% activity) in our assay. Across 125 variants tested, we observed that PolyPhen-2/LOFTEE-predicted damaging variants correlated significantly, albeit imperfectly, with lower ASM activity levels compared to predicted benign variants (t-test P = 1.11 × 10−5). We observed that carriage of SMPD1 variants with less than 44% enzymatic activity (corresponding to >56% loss of function) showed the strongest association with PD risk in both the Discovery (OR = 2.37, P = 4.35 × 10−7) and Replication (OR = 2.18, P = 4.80 × 10−10) cohorts and the combined Discovery and Replication cohorts (OR = 2.24, P = 1.25 × 10−15; Fig. 3a, Extended Data Figs. 3 and 4, Supplementary Fig. 12 and Supplementary Results). In our East Asian Discovery cohort, the p.Pro332Arg variant (30.4% activity) was the most prevalent, observed in 70 of 87 (80.5%) SMPD1 case carriers with less than 44% enzymatic activity relative to wild-type (Fig. 3b). p.Pro332Arg alone showed genome-wide significant association with PD risk (OR = 2.16; P = 4.47 × 10−8) in the Discovery and Replication cohorts combined (Supplementary Results).
Forty-four of the 125 SMPD1 variants assayed were reported in patients with NPD-A or NPD-B and were also classified in ClinVar as pathogenic (n = 18), benign (n = 5) or uncertain significance (n = 21) (Supplementary Table 17). Fourteen of 18 (77.78%) ClinVar pathogenic variants reported in patients with NPD-A/B had less than 44% enzymatic activity relative to wild-type SMPD1, thus confirming that the functionally deficient set is enriched for pathogenic variants.
PD onset age and polygenic risk scores of SMPD1 and GBA1 carriers
We sought to determine if carriers of SMPD1 or GBA1 variants from our Discovery samples had an earlier age of PD diagnosis compared to non-carriers. Carriers of GBA1 qualifying variants were diagnosed with PD almost 7 years younger than non-carriers, but the effect was smaller for carriers of SMPD1 qualifying variants and carriers of functionally deficient SMPD1 variants (activity levels ≤43.58%; carriers: median = 60 years of age, range = 32–86 years of age; non-carriers: median = 62 years of age, range = 22–92 years of age; t-test P = 0.216) (Extended Data Fig. 5). We examined the polygenic risk score profile of 87 SMPD1 functionally deficient variant carriers calculated using 67 GWAS-identified single-nucleotide polymorphisms (SNPs) selected in our East Asian GWAS39 and observed no significant difference between PD cases and controls, suggesting that polygenic risk score was not a modifier of risk among SMPD1 functionally deficient variant carriers (Extended Data Fig. 6).
Rare coding variants in genes associated with decreased PD risk
We observed exome-wide significant association of qualifying variants in HLA-DRB1 with decreased PD risk. Qualifying variants in HLA-DRB1 were observed in 15 of 4,298 PD cases (0.35%) compared to 73 of 5,512 controls (1.32%; OR = 0.20, 95% CI = 0.11–0.35, P = 1.05 × 10−9; Supplementary Table 18 and Extended Data Fig. 7). This association was largely driven by lead variant p.Ala14Pro (OR = 0.13, 95% CI = 0.07–0.26, P = 4.71 × 10−11) located in the signal peptide of the full length HLA-DRB1 protein and not linked to any classical HLA-DRB1 allele. This variant was present in 10 PD cases (0.23%) and 68 controls (1.23%) in our Discovery cohort and appeared to be independent of GWAS-associated SNPs40,41 at the HLA-DRB1 locus, including rs601945, rs504594 or rs3104413, and amino acid 13 (r2 = 0). However, given the difficulty in calling and validating variants in the HLA region by short-read sequencing, further work will be needed to ascertain the association of altered epitope binding or antigen presentation effects of these HLA-DRB1 variants with reduced PD risk40,41. We also observed a nominally significant association at ATP5B (OR = 0.19, 95% CI = 0.08–0.43, P = 9.46 × 10−6), but this association was not consistent in the South Korean dataset (Extended Data Fig. 7).
Monogenic gene mutations are rare in East Asian sporadic PD cases
We investigated how many East Asian sporadic PD cases carried known or likely pathogenic variants (ClinVar) in monogenic PD genes. In autosomal recessive PD genes, only one PD case (onset age = 44 years) was homozygous for pathogenic variant PRKN p.Cys441Arg, which was reported for autosomal recessive juvenile PD (ClinVar accession: VCV000963190). Sixteen PD cases and six controls (OR = 3.845, P = 0.00375) were homozygotes or compound heterozygotes for qualifying variants excluding those listed as non-pathogenic in ClinVar (benign, conflicting interpretations or uncertain significance) in PRKN (two cases), ATP13A2 (one case), DNAJC6 (one control) and VPS13C (13 cases and five controls) (Supplementary Table 12). These carriers had PD onset ranging from 28 years to 79 years of age (average = 59.5 ± 14.1 years, median = 60 years; n = 14; two missing).
Although there was no significant enrichment of qualifying variants in autosomal dominant PD genes, we identified carriers of pathogenic LRRK2 variants p.Arg1441Cys (four cases, disease onset age = 56 ± 4.3 years) and p.Arg1067Gln (four cases and two controls) that activate Rab10 phosphorylation42 (Supplementary Tables 12 and 13).
Seven of the 4,298 cases in our study carried known or potential pathogenic variants in known monogenic PD genes, and another 15 were potential homozygotes or compound heterozygotes for qualifying variants in monogenic PD genes. This is consistent with previous reports that these monogenic PD mutations account for a very small percentage (~0.5%) of sporadic PD cases.
Protein-truncating variants in East Asian PD cases and controls
Inaccurate functional prediction of missense variants may dilute the association signals in genes with highly penetrant loss-of-function variants with large effects. To assess this, we conducted gene-based association testing in the Discovery cohort on protein-truncating variants (PTVs) predicted to cause loss of function43. No gene reached exome-wide significance, although GBA1 remained strongly associated (OR = 10.8, P = 0.0024; Supplementary Results and Supplementary Table 19). We observed PTVs in the recently reported ITSN1 gene44 in only three cases in our Discovery cohort (P = 0.093).
Discussion
Our observations from WES, replication in independent, cross-ancestry samples and functional enzymatic assays suggest that heterozygous carriage of deficient SMPD1 alleles is associated with 2.2-fold higher odds of PD. The top two genes emerging from WES, GBA1 and SMPD1, are both involved in lysosomal storage diseases (Gaucher’s disease45 and NPD46) that present early in life with severe clinical symptoms.
GBA1 has been extensively evaluated since its identification as a PD risk gene26, with patients carrying rare, protein-altering variants robustly associating with increased PD risk and more severe clinical phenotype47. Conversely, the association between protein-altering SMPD1 variants and PD had been inconsistent. The first study linking SMPD1 with PD reported that carriage of the p.Leu304Pro variant was associated with nine-fold increased odds of disease48. SMPD1 p.Leu304Pro was a loss-of-function, founder mutation in individuals of Ashkenazi Jewish ancestry48,49 and was not present in nearly all other ancestry groups, including East Asians50. Since then, other smaller studies have shown equivocal evidence in support for other SMPD1 variants33,34,48,51,52, and others have reported no significant association between SMPD1 variants and susceptibility to PD22,53,54,55. SMPD1 was not identified in the largest WES study of European ancestry samples, which reported strong association at GBA1 and LRRK2 (driven by the rare p.Gly2019Ser variant that is absent in Asian populations)27. We suspect that these inconsistent SMPD1 reports were due to the limitations of the bioinformatic algorithms used to predict and identify ‘damaging’ genetic variants. Indeed, incorrect functional classification of genetic variants markedly reduces statistical power for rare variant burden tests28. The different SMPD1 rare variants represented at different allele frequency spectra between Asian and European cohorts may also explain the heterogeneity observed in the combined Discovery and Replication analysis.
We used laboratory assays based on ASM activity to evaluate the functional effect of all 125 SMPD1 alleles detected in this study. This assay was adequately controlled for, as it was able to correctly classify mutations known to cause NPD-A/B. The inclusion of only functionally impaired variants in the gene-based burden test is a major step forward from the current use of predictive bioinformatic algorithms to distinguish variants that impair protein function from ‘benign’ variants. Our analysis suggests that carrying one functionally defective copy of SMPD1 was sufficient to associate with more than two-fold increased risk of sporadic, adult-onset PD. In contrast, complete loss of SMPD1 function causes childhood-onset NPD-A/B. Bearing in mind that ASM encoded by SMPD1 catalyzes the conversion of sphingomyelin to phosphocholine and ceramide36, previous investigators observed significant differences in sphingomyelin and ceramide lipid species between postmortem brains from PD cases compared to brains from non-PD donors56,57. Taken together, the spectrum of functional SMPD1 alleles detected in our large-scale sequencing study affirm a role for ASM in the pathobiology of neurodegenerative diseases.
Limitations
Our study has several limitations. First, we were unable to assess the effects of co-carrying functionally deficient variants in both GBA1 and SMPD1, as we observed only eight individuals who carried protein-altering variants in both GBA1 and SMPD1. Of these, two were PD cases who carried a known pathogenic variant in GBA1 (p.Leu483Pro) with SMPD1 (p.Pro332Arg). Their variable age of disease onset (48 years and 62 years) is in keeping with the high genetic heterogeneity observed in sporadic PD. Future work involving more participants carrying mutations in both genes will be needed to resolve the question of possible interaction between both genes. Second, the concordance between our in vitro ASM activity assays and previously reported measurements based on dried blood spots was approximately 50%58. This discordance could reflect variability in laboratory techniques as well as opportunities to perform experiments in multiple biological replicates for more accurate ascertainment of enzymatic activity. Reassuringly, one such discordant variant (SMPD1 p.Ala487Val) was re-assayed by a third party, and their conclusions agreed with our findings that this variant does not qualify as functionally deficient59. Finally, large sample sizes are typically required for rare variant association studies. In our current Discovery cohort, we had more than 90% power (Extended Data Fig. 8) to detect genes such as GBA1 with large effect sizes (OR > 5) and at combined carrier frequencies of approximately 0.5% in the population and also genes such as SMPD1 with smaller effect sizes (OR ~ 2) but at higher combined carrier frequencies of 1–1.5% in the population (contributed, in part, by the p.Pro332Arg variant). Larger multi-center studies will facilitate the discovery of genes with similar effect sizes to GBA1 and SMPD1 but present at lower carrier frequencies in the population.
Conclusion
From our study, we suggest that rare independent alleles in SMPD1 that impair ASM activity are associated with increased risk of PD. Our findings will inform further work on understanding the role of sphingolipid and ceramide metabolism as well as the role of rare, functionally deficient alleles in associated genes in PD pathogenesis.
Methods
Study design and participants
Discovery exome sequencing
PD cases together with ancestry-matched and geographically matched controls were recruited by six independent study groups from five regions across East Asia (SG, MAL, HK, KR and TW). A total of 4,298 PD cases and 5,512 controls were included in the final analysis (Supplementary Tables 1 and 2). A diagnosis of PD was reached using the United Kingdom Parkinson’s Society Brain Bank Criteria. The controls were healthy individuals who do not have any overt neurological diseases. Written informed consent was obtained from each participant in strict adherence to the Declaration of Helsinki. This study was approved by the ethics committees or institutional review boards of the respective institutions (SingHealth Centralized Institutional Review Board CIRB 2002/008/A and 2019/2334 and Nanyang Technological University Institutional Review Board IRB-2016-08-011). The study was conducted from 1 January 2016 to 31 December 2022. This study followed the Strengthening the Reporting of Genetic Association Studies (STREGA) guidelines.
Replication datasets
Published sequencing data from 5,585 PD cases and 5,642 controls from China, the United States and the International PD Genomics Consortium (IPDGC, samples from the United States and Europe) were evaluated for replication of significant findings from the Discovery WES analysis (Supplementary Table 16).
For the Chinese dataset, a total of 1,440 sporadic early-onset PD cases, 477 autosomal dominant or autosomal recessive PD cases, 1,962 sporadic late-onset PD cases and 2,931 controls from Changsha were included33 (referred to as the ‘Zhao’ dataset/stratum). For the IPDGC dataset, a total of 691 sporadic early-onset PD cases, 465 early-onset PD cases with positive family history of PD and 1,679 controls of Northern and Western European ancestry were included34 (referred to as the ‘Robak’ stratum). For the United States dataset, a total of 550 PD cases and 284 controls from New York were enrolled58. This dataset was enriched with an additional 748 controls from neighboring Boston60 (referred to as the ‘Alcalay-Boston’ stratum). SMPD1 variants analyzed in all 11,227 Replication samples were from sequencing data obtained using similar experimental methods from both PD cases and controls. No population databases (for example, gnomAD or UK Biobank) were used in lieu of sequenced controls, which circumvented the introduction of bias in coverage and variant calling.
Whole-exome capture and sequencing
Peripheral venous blood was drawn from each consenting participant, and DNA extraction was performed using routine laboratory methods. DNA for WES was sheared using a Covaris LE220 Focused-ultrasonicator, and libraries were prepared using NEBNext Ultra II DNA Library Prep Kit for Illumina (New England Biolabs (NEB)). Exomes were captured using SeqCap EZ Human Exome Library version 3.0 kits or KAPA HyperExome Probes (both from Roche NimbleGen). Libraries from PD cases and controls were barcoded and sequenced together in batches of 96 samples using 2 × 151-bp paired-end reads on Illumina instruments (HiSeq 4000 and NovaSeq 6000 systems) to achieve an average of 63× coverage depth across captured target regions, with at least 95% of targeted exons covered by at least 10 reads. All samples were processed in the same laboratory.
Bioinformatics processing, variant calling and quality control filtering
For the Discovery WES dataset, raw DNA sequence reads from all samples (with case–control status blinded) were mapped to the human reference genome build hg19 (GRCh37) using the Burrows–Wheeler Aligner MEM algorithm (BWA version 0.7.17)61 (Supplementary Fig. 1). Variant calling was performed using the Genome Analysis Tool Kit (GATK, version 3.7)62 and the Picard software package (version 2.21.7, http://broadinstitute.github.io/picard/) following GATK Best Practices Guidelines63. Variant quality score recalibration (VQSR) was performed to exclude low-quality variant calls.
Additional quality control procedures were performed using VCFtools (version 0.1.16)64, BCFtools (version 1.9)65, PLINK (version 1.9)66 and the Fratools PERL package (version 1, https://github.com/atks/fratools) at genotype, variant call and sample quality check levels. Low-quality genotype calls (read depth (DP) < 8 and genotype quality score (GQ) < 20) were excluded. Variants with low call rates in PD cases/controls/all samples (<95%), failed tests for Hardy–Weinberg equilibrium (P < 1 × 10−6) and high differential missingness between PD cases and controls (P < 1 × 10−4) were excluded from further analyses. We removed PD cases with sex discordance between genetically inferred sex from WES and patient records and samples showing poor genotyping concordance (<95% concordance) between WES data and genome-wide association arrays. Samples with excessive heterozygosity (>3.5 s.d. from mean), unusually high exome-wide singleton counts and low genotyping completion rate (<95%) were also excluded. We used identity-by-descent (IBD) analysis to identify related sample pairs up to the third degree (IBD > 0.125). For these pairs, the sample with the lower call rate was removed. Lastly, samples with outlying genetic ancestry as visualized using ancestry PCA with 2,141 samples from the 1000 Genomes Project reference panel67 and 268 samples from the Singapore Genome Variation Project reference panel68 were also removed. Variant calling and filtering was done across all samples equally regardless of affection status. All steps related to sample quality checks are summarized in Supplementary Table 3.
Identification of rare damaging genetic variants
Single-nucleotide variants and small insertions/deletions were annotated using Ensembl Variant Effect Predictor (VEP) software (version 104)69. Variant annotation was based on canonical transcripts defined in Ensembl VEP. Rare variants were defined based on ≤1% allele frequency in the WES dataset and the gnomAD East Asian population50. Functional predictions for missense variants were derived from PolyPhen-2 (version 2.2.3r406)70, and the VEP plugin LOFTEE (version 1.0.3)71 was used for functional prediction of stop-gain/loss, splice site and frameshift variants. Rare variants predicted to be pathogenic (probably or possibly damaging) by PolyPhen-2/LOFTEE were termed ‘qualifying’ variants. Rare variants predicted as loss of function (LOFTEE ‘high confidence’ prediction) were termed PTVs. For the Replication datasets, published variant lists from whole-exome and whole-genome sequencing of GBA1 and SMPD1 were re-annotated based on the listed variant position in the same way as the Discovery dataset using PolyPhen-2/LOFTEE and Ensembl VEP software.
Validation by Sanger capillary sequencing
DNA samples from rare SMPD1 allele carriers were polymerase chain reaction (PCR) amplified and capillary sequenced to confirm the rare allele calls from WES. PCR primers were designed using Primer3 (https://primer3.ut.ee/; Supplementary Tables 11 and 20).
ASM activity assay
To assess ASM activity associated with SMPD1 variants observed, we generated HEK293T cell lines that contain individual SMPD1 variants (Supplementary Table 21 and Supplementary Methods) and conducted a fluorescence-based assay to measure ASM activity.
We transduced HEK293T cell lines with individual SMPD1 variants cloned into the lentiviral pLVX-CMV vector containing a puromycin selection marker72 by standard lentiviral transduction methods. Fragments containing SMPD1 variants were generated by one of the three approaches. In the first approach, SMPD1 allele was generated from two separate overlapping fragments containing the variant-specific mutation. These two fragments were amplified from the open reading frame of the SMPD1 canonical transcript ENST00000342245.4 using primer pairs (Supplementary Table 21). One fragment will be generated from amplification with the forward end primer (SMPD1_FWD) and variant-specific reverse primer, whereas the other fragment will be generated from amplification with the variant-specific forward primer and reverse end primer (SMPD1_REV). Both fragments and the linearized pLVX-CMV vector were joined by Gibson assembly (NEB, E2621S). In the second approach, a single fragment for SMPD1 alleles close to the 3′ or 5′ ends of the SMPD1 open reading frame was produced by incorporating the variant-specific mutation into the variant-specific primer by PCR. The single fragment and the linearized pLVX-CMV vector were joined by Gibson assembly (NEB, E2621S). In the third approach, fragments for SMPD1 alleles that were technically challenging to generate with the PCR-based approach were synthesized using the GenBrick synthesis service from GenScript, before restriction digestion and ligation with the linearized pLVX-CMV vector. Sanger sequencing was conducted on all generated plasmids to confirm variant sequences before transduction into HEK293T cells.
Transduced cells underwent selection in puromycin-containing media for 4 d. Western blotting was conducted with anti-SMPD1 antibody (R&D Systems, MAB5348) to verify successful transduction by ascertainment of SMPD1 expression. A total of 126 cell lines expressing wild-type SMPD1 and 125 individual protein-altering SMPD1 genetic variants were made (122 rare variants and three common variants; Supplementary Table 17).
To measure ASM activity associated with each SMPD1 genetic variant, cells were sonicated with protease inhibitor (Roche, 05056489001). Then, 10 μg of extract was tested for ASM activity in replicates (n = 3–6) using a fluorescence assay with synthetic substrate HMU-PC (Biosynth, EH31028)73. We measured the ASM activity of each SMDP1 allele as the amount of fluorescent signal generated over 1 h at 37 °C. Measured activity for each variant was presented as percentage reduction in activity as compared to wild-type SMPD1 that was calculated based on log2 fold change of signal per replicate by the average wild-type signal.
In silico structural analysis of p.Pro282Thr, p.Tyr500His and p.Asn177Tyr variants
Steric clashes due to p.Pro282Thr, p.Tyr500His and p.Asn177Tyr mutations were evaluated using the mutagenesis toolbox in PyMol (version 2.5.2) based on the atomic coordinates of human ASM bounded with zinc and phosphocholine (Protein Data Bank (PDB) ID: 5I85).
Expression of PD-associated genes in single-cell transcriptomics dataset
Single-nuclei transcriptomics data from four midbrain or substantia nigra studies, which consisted of 17 PD cases and 27 controls74,75,76,77, were downloaded from the Gene Expression Omnibus (Supplementary Table 5).
Quality control and filtering were conducted with Seurat (version 4.3.0.1)78 to retain cells with mitochondrial gene content less than 5%, 200–5,000 total genes expressed and singlets as identified with scDblFinder (version 1.15.2)79. A total of 117,338 single cells from 17 PD cases and 156,035 single cells from 27 controls remained after quality control and filtering. Gene expression measurements for retained cells were normalized with the SCTransform function and integrated. Dimensionality reduction by PCA and Uniform Manifold Approximation and Projection (UMAP) embedding was performed, followed by visualization of clustering stability with clustree (version 0.5.0). Cell clusters were annotated with known cell type markers for neuronal, glial, endothelial cell and immune cell types (Supplementary Table 7). The expression of PD-associated genes was assessed across the annotated cell types. Differential gene expression between PD and control for each cell type was assessed with the Seurat FindMarkers function using the Wilcoxon rank-sum test.
Postmortem midbrain samples
Snap-frozen human postmortem brain tissue samples were acquired from the Multiple Sclerosis and Parkinson’s Tissue Bank (Imperial College London, Hammersmith Campus). Samples from the substantia nigra pars compacta (SNpc) region were obtained from two PD cases and one control (no PD clinical history and no PD-associated neuropathology). Written informed consent was obtained from each donor in strict adherence to the Declaration of Helsinki. All neuropathological diagnoses were made based on the BrainNet Europe protocol80,81,82. This research was approved by the Nanyang Technological University Institutional Review Board (IRB-2016-12-029 and IRB-2018-09-052) and the National Research Ethics Committee (08/MRE09/31 and National Health Service REC no. 18/SW/0029).
Protein expression of GBA1 and SMPD1 in brain tissues
Western blotting and immunohistochemistry were conducted for SMPD1 and GBA1 on snap-frozen postmortem SNpc sections from two PD cases and one control by lysis in RIPA buffer (Thermo Fisher Scientific) containing protease and phosphatase inhibitors (Thermo Fisher Scientific) on ice for 20 min, followed by 15-min centrifugation at 12,000g at 4 °C. Then, 5% 2-mercaptoethanol (Sigma-Aldrich) and 2× Laemmli sample buffer (Bio-Rad) were added to the protein lysates before heating at 95 °C for 5 min. Western blotting was then conducted on 35 μg of tissue lysate with anti-SMPD1 antibody (1:1,000 dilution; R&D Systems, MAB5348), anti-GBA1 antibody (1:100 dilution; Santa Cruz Biotechnology, sc-166407) and anti-GAPDH antibody (1:1;000 dilution; Bio-Rad, VMA00046).
Immunohistochemistry was conducted on snap-frozen postmortem SNpc tissues from the same two PD cases and one control by fixing snap-frozen tissue sections (10 μm thick) with 10% neutral buffered formalin for 30 min and cold methanol for 10 min. Blocking was conducted for 1 h with 2.5% normal goat serum (Vector Laboratories) before incubation with anti-SMPD1 antibody (1:500 dilution; R&D Systems, MAB5348), anti-GBA1 antibody (1:50 dilution; Santa Cruz Biotechnology, sc-166407), anti-GAPDH antibody (1:1,000 dilution; Bio-Rad, VMA00046), anti-TH (1:200 dilution; Abcam, ab137869) and anti-HuC/D (1:500 dilution; Life Technologies, A-21271) overnight at 4 °C. Sections were incubated in 0.3% hydrogen peroxide for 10 min before adding ImmPRESS horseradish peroxidase polymer reagent (Vector Laboratories) for 1 h. The slides were subsequently developed with an ImmPACT-DAB substrate kit (Vector Laboratories) with Mayer’s hematoxylin as counterstain. Sequential dehydration in 70%, 90% and 100% IMS was done, followed by clearing in 100% xylene. The sections were then mounted with DPX mountant (Sigma-Aldrich).
Immunostaining for SMPD1 co-localization with lysosomes
Immunostaining for SMPD1 was conducted on LysoTracker Red–stained HEK293T wild-type SMPD1 cells and HEK293T cells containing empty vector. HEK293T wild-type SMPD1 cells and HEK293T cells containing empty vector were seeded on Cell-Tak-coated coverslips (Corning, 354240) and cultured for 48 h. Cells were then treated with 5 nM LysoTracker Red DND-99 (Thermo Fisher Scientific, L7528) for 45 min and fixed with 4% (v/v) paraformaldehyde (Thermo Fisher Scientific, FB002) for 15 min at room temperature. Cells were permeabilized with 0.1% Triton X-100 (Sigma-Aldrich, T9284) for 10 min and blocked with 5% BSA (Sigma-Aldrich, SRE0036) for 1 h (both at room temperature). Incubation with anti-SMPD1 antibody (1:500 dilution; R&D Systems, MAB5348) was conducted overnight at 4 °C, followed by incubation with goat anti-mouse Alexa Fluor Plus 488 (1:500 dilution; Thermo Fisher Scientific, A32723) for 2 h at room temperature. DAPI counterstaining was conducted, and coverslips were mounted for confocal imaging on a Zeiss LSM 800 confocal laser scanning microscope, with image acquisition with the ×63 objective.
Statistics and reproducibility
Gene-based association testing
We tested whether any of the 17,396 autosomal genes across the human exome bear an excess or deficit of ‘damaging’ mutational burden in PD cases compared to controls. For the Discovery cohorts, a stratified Cochran–Mantel–Haenszel (CMH) test without continuity correction was used to evaluate gene-based burden across the exomes of participants from the five countries studied (Supplementary Table 2). Singapore and Malaysia (SG/MAL) samples were considered as one stratum due to the similarity in genetic background (as evidenced by PCA of SG/MAL samples; Supplementary Figs. 2 and 3). Haldane–Anscombe correction on OR was applied on carrier count matrices with at least one zero count83,84. We also evaluated gene-based burden with SKAT-O85 after adjustment for per-sample variant counts, average per-sample coverage and principal components (PC1–PC3) as covariates.
Exome-wide significance was preset at P ≤ 2.5 × 10−6 (two-tailed), based on multiple hypothesis testing correction for an estimated 20,000 protein-coding genes in the human genome. Genome-wide significance threshold was set at 5 × 10−8, following the standard threshold in GWASs.
Replication of SMPD1 and GBA1 association
For the Replication cohorts, the same CMH test without continuity correction was conducted on a total of 5,585 PD cases and 5,642 controls from China, the United States and the IPDGC (Supplementary Table 16) in a stratified meta-analysis as performed for the Discovery cohorts. Gene-based testing of SMPD1 qualifying variants was conducted across seven strata consisting of four Discovery cohorts (SG/MAL, HK, KR and TW) and three Replication cohorts (Zhao, Robak and Alcalay-Boston) with SMPD1 data available. Gene-based testing of GBA1 qualifying variants was conducted across six strata consisting of four Discovery cohorts (SG/MAL, HK, KR and TW) and two Replication cohorts (Zhao and Robak) with GBA1 data available. Data are presented as OR and 95% CI. All P values presented are unadjusted.
Association of variant carrier status with PD onset
Association testing of SMPD1, HLA-DRB1 and GBA1 variant carrier status with age of PD onset was conducted with two-tailed t-tests on 4,149 of 4,298 PD cases that have available information on PD onset age.
Association of SMPD1 variant carrier status with polygenic risk score
Association testing of SMPD1 variant carrier status with polygenic risk score was also conducted using a two-tailed t-test. Polygenic risk score was based on a total of 67 genome-wide significant loci from both East Asian and European studies presented in our analysis. This included 11 loci reaching genome-wide significance in the East Asian GWAS39 and 78 European risk loci from Nalls et al.7. At nine loci that overlap between East Asian and European, the East Asian risk SNP was used, as described in Foo et al.39. Of all 80 (78 + 11 − 9) unique SNPs that were considered, 67 were polymorphic and passed genotyping/imputation quality control filtering in the PD case and control samples analyzed in this study39,86.
ASM activity assay
Cell lines bearing SMPD1 variant alleles were assayed across different plates. To correct for plate-to-plate variation, a reference cell line expressing wild-type SMPD1 alleles was always assayed together with the cell lines bearing SMPD1 variant alleles. This allowed for direct comparison of fluorescent signal from SMPD1 variant-containing cell extracts with that from the SMPD1 wild-type reference cell line within each batch of experiment.
To assess passage-to-passage activity variation, we randomly selected eight cell lines containing eight different SMPD1 variants and measured their resultant ASM activities using the same ASM activity assay in technical triplicates. The measured ASM activity of all eight variants relative to wild-type SMPD1 remained highly concordant between passages (Supplementary Fig. 7).
Association of SMPD1 variant ASM activity levels with ___domain localization
Rare SMPD1 variants were classified by their localization to protein domains across the ASM protein and their effect on protein tertiary structure integrity based on protein crystallography studies (PDB: 5I81). Two-sided t-tests were used to compare ASM activity levels across each category.
Statistical analysis of ASM activity in Discovery and Replication cohorts
Because ASM enzymatic activity was measured as a continuous variable, we used iterative linear discriminant analysis to explore enzymatic activity thresholds in which variants below a tested threshold would be classified as ‘impaired function’. This was done to obtain the best discrimination (in terms of P value) between PD cases and controls. Only functionally impaired variants with enzymatic activities below the defined threshold were included in the revised stratified CMH test for SMPD1.
Immunostaining for SMPD1 co-localization with lysosomes
Each cell line was plated for immunostaining assay on coated coverslips in three wells across a six-well plate. After culturing and immunostaining procedures described above, one field of view was captured from each well, resulting in three fields of view captured per condition.
Protein expression and immunostaining of GBA1 and SMPD1 in brain tissues
The substantia nigra region was present in only 2–3 slices (10 µm) in each brain tissue block. As such, one slice per sample (two PD cases and one control) was lysed for western blotting for GBA1, SMPD1 and GAPDH protein expression, and one other slice per sample (two PD cases and one control) was used for immunohistochemistry for SMPD1, GBA1, TH and HuC/D.
Reporting Summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
All unrestricted data are available from the corresponding author upon reasonable request. Summary statistics can be found in Supplementary Table 22. Western blots are provided as Supplementary Data. Acid sphingomyelinase (ASM) enzymatic activity assay absorbance readings are provided as Source Data. Individual-level genotype data are not publicly available because of consent and privacy issues but will be made available upon reasonable request to J.N.F. ([email protected]; response timeframe of 1 month) and after approval by the relevant institutional review board. Midbrain single-nuclei RNA sequencing datasets used are available from the Gene Expression Omnibus as detailed in Supplementary Table 5. Protein crystallography of ASM tertiary structure is available from the Protein Data Bank (ID: 5I85).
Code availability
The codes used in this study can be found on GitHub (https://github.com/fjnlab/PD_exome-seq). Software and software packages used include the following: R (version 4.0.2) and R packages data.table (version 1.14.0), dplyr (version 1.0.5), tidyr (version 1.1.2), ggplot2 (version 3.3.6), forestplot (version 2.0.1), stats (mantelhaen.test, version 4.3.1) and SKAT (version 2.2.5); BWA (version 0.7.17); GATK (version 3.7); Picard (version 2.21.7); VCFtools (version 0.1.16); BCFtools (version 1.9); PLINK (version 1.9); Fratools PERL package (version 1, https://github.com/atks/fratools); Ensembl Variant Effect Predictor (VEP) software (version 104); ANNOVAR (version dated 2020-06-07); VEP plugin LOFTEE (version 1.0.3); PolyPhen-2 (version 2.2.3r406); dbNSFP (version 3.5a); Seurat (version 4.3.0.1); scDblFinder (version 1.15.2); clustree (version 0.5.0); and PyMol (version 2.5.2).
References
Nutt, J. G. & Wooten, G. F. Clinical practice. Diagnosis and initial management of Parkinson’s disease. N. Engl. J. Med. 353, 1021–1027 (2005).
Bloem, B. R., Okun, M. S. & Klein, C. Parkinson’s disease. Lancet 397, 2284–2303 (2021).
Satake, W. et al. Genome-wide association study identifies common variants at four loci as genetic risk factors for Parkinson’s disease. Nat. Genet. 41, 1303–1307 (2009).
Simón-Sánchez, J. et al. Genome-wide association study reveals genetic risk underlying Parkinson’s disease. Nat. Genet. 41, 1308–1312 (2009).
Nalls, M. A. et al. Imputation of sequence variants for identification of genetic risks for Parkinson’s disease: a meta-analysis of genome-wide association studies. Lancet 377, 641–649, (2011).
Nalls, M. A. et al. Large-scale meta-analysis of genome-wide association data identifies six new risk loci for Parkinson’s disease. Nat. Genet. 46, 989–993 (2014).
Nalls, M. A. et al. Identification of novel risk loci, causal insights, and heritable risk for Parkinson’s disease: a meta-analysis of genome-wide association studies. Lancet Neurol. 18, 1091–1102 (2019).
Chang, D. et al. A meta-analysis of genome-wide association studies identifies 17 new Parkinson’s disease risk loci. Nat. Genet. 49, 1511–1516 (2017).
Kim, J. J. et al. Multi-ancestry genome-wide association meta-analysis of Parkinson’s disease. Nat. Genet. 56, 27–36 (2024).
Cohen, J. C., Boerwinkle, E., Mosley, T. H. Jr. & Hobbs, H. H. Sequence variations in PCSK9, low LDL, and protection against coronary heart disease. N. Engl. J. Med. 354, 1264–1272 (2006).
Minikel, E. V. et al. Evaluating drug targets through human loss-of-function genetic variation. Nature 581, 459–464 (2020).
Polymeropoulos, M. H. et al. Mapping of a gene for Parkinson’s disease to chromosome 4q21-q23. Science 274, 1197–1199 (1996).
Zimprich, A. et al. A mutation in VPS35, encoding a subunit of the retromer complex, causes late-onset Parkinson disease. Am. J. Hum. Genet. 89, 168–175 (2011).
Vilariño-Güell, C. et al. VPS35 mutations in Parkinson disease. Am. J. Hum. Genet. 89, 162–167 (2011).
Kitada, T. et al. Mutations in the parkin gene cause autosomal recessive juvenile parkinsonism. Nature 392, 605–608 (1998).
Bonifati, V. et al. Mutations in the DJ-1 gene associated with autosomal recessive early-onset parkinsonism. Science 299, 256–259 (2003).
Valente, E. M. et al. Hereditary early-onset Parkinson’s disease caused by mutations in PINK1. Science 304, 1158–1160 (2004).
Ramirez, A. et al. Hereditary parkinsonism with dementia is caused by mutations in ATP13A2, encoding a lysosomal type 5 P-type ATPase. Nat. Genet. 38, 1184–1191 (2006).
Morgan, N. V. et al. PLA2G6, encoding a phospholipase A2, is mutated in neurodegenerative disorders with high brain iron. Nat. Genet. 38, 752–754 (2006).
Di Fonzo, A. et al. FBXO7 mutations cause autosomal recessive, early-onset parkinsonian-pyramidal syndrome. Neurology 72, 240–245 (2009).
Quadri, M. et al. Mutation in the SYNJ1 gene associated with autosomal recessive, early-onset Parkinsonism. Hum. Mutat. 34, 1208–1215 (2013).
Deng, H. X. et al. Identification of TMEM230 mutations in familial Parkinson’s disease. Nat. Genet. 48, 733–739 (2016).
Saini, P. et al. Association study of DNAJC13, UCHL1, HTRA2, GIGYF2, and EIF4G1 with Parkinson’s disease. Neurobiol. Aging 100, 119.e7–119.e13 (2021).
Paisán-Ruíz, C. et al. Cloning of the gene containing mutations that cause PARK8-linked Parkinson’s disease. Neuron 44, 595–600 (2004).
Zimprich, A. et al. Mutations in LRRK2 cause autosomal-dominant parkinsonism with pleomorphic pathology. Neuron 44, 601–607 (2004).
Sidransky, E. et al. Multicenter analysis of glucocerebrosidase mutations in Parkinson’s disease. N. Engl. J. Med. 361, 1651–1661 (2009).
Makarious, M. B. et al. Large-scale rare variant burden testing in Parkinson’s disease. Brain 146, 4622–4632 (2023).
Zuk, O. et al. Searching for missing heritability: designing rare variant association studies. Proc. Natl Acad. Sci. USA 111, E455–E464 (2014).
Correia Guedes, L., Mestre, T., Outeiro, T. F. & Ferreira, J. J. Are genetic and idiopathic forms of Parkinson’s disease the same disease? J. Neurochem. 152, 515–522 (2020).
Day, J. O. & Mullin, S. The genetics of Parkinson’s disease and implications for clinical practice. Genes (Basel) 12, 1006 (2021).
Klein, C. & Westenberger, A. Genetics of Parkinson’s disease. Cold Spring Harb. Perspect. Med. 2, a008888 (2012).
Di Lazzaro, G. et al. X-linked Parkinsonism: phenotypic and genetic heterogeneity. Mov. Disord. 36, 1511–1525 (2021).
Zhao, Y.-W. et al. The association between lysosomal storage disorder genes and Parkinson’s disease: a large cohort study in Chinese mainland population. Front. Aging Neurosci. 13, 749109 (2021).
Robak, L. A. et al. Excessive burden of lysosomal storage disorder gene variants in Parkinson’s disease. Brain 140, 3191–3203 (2017).
Full spectrum genetics. Nat. Genet. 44, 1 (2011).
Kornhuber, J., Rhein, C., Müller, C. P. & Mühle, C. Secretory sphingomyelinase in health and disease. Biol. Chem. 396, 707–736 (2015).
Levran, O., Desnick, R. J. & Schuchman, E. H. Identification and expression of a common missense mutation (L302P) in the acid sphingomyelinase gene of Ashkenazi Jewish type A Niemann–Pick disease patients. Blood 80, 2081–2087 (1992).
Levran, O., Desnick, R. J. & Schuchman, E. H. Niemann–Pick disease: a frequent missense mutation in the acid sphingomyelinase gene of Ashkenazi Jewish type A and B patients. Proc. Natl Acad. Sci. USA 88, 3748–3752 (1991).
Foo, J. N. et al. Identification of risk loci for Parkinson disease in Asians and comparison of risk between Asians and Europeans: a genome-wide association study. JAMA Neurol. 77, 746–754 (2020).
Le Guen, Y. et al. Multiancestry analysis of the HLA locus in Alzheimer’s and Parkinson’s diseases uncovers a shared adaptive immune response mediated by HLA-DRB1*04 subtypes. Proc. Natl Acad. Sci. USA 120, e2302720120 (2023).
Naito, T. et al. Trans-ethnic fine-mapping of the major histocompatibility complex region linked to Parkinson’s disease. Mov. Disord. 36, 1805–1814 (2021).
Kalogeropulou, A. F. et al. Impact of 100 LRRK2 variants linked to Parkinson’s disease on kinase activity and microtubule binding. Biochem. J 479, 1759–1783 (2022).
Wang, Q. et al. Rare variant contribution to human disease in 281,104 UK Biobank exomes. Nature 597, 527–532 (2021).
Spargo, T. P. et al. Haploinsufficiency of ITSN1 is associated with Parkinson’s disease. Preprint at medRxiv https://doi.org/10.1101/2024.07.25.24310988 (2024).
Beutler, E. Gaucher disease: new molecular approaches to diagnosis and treatment. Science 256, 794–799 (1992).
Schuchman, E. H. The pathogenesis and treatment of acid sphingomyelinase-deficient Niemann–Pick disease. J. Inherit. Metab. Dis. 30, 654–663 (2007).
Lim, J. L. et al. Glucocerebrosidase (GBA) gene variants in a multi-ethnic Asian cohort with Parkinson’s disease: mutational spectrum and clinical features. J. Neural Transm. (Vienna) 129, 37–48 (2022).
Gan-Or, Z. et al. The p.L302P mutation in the lysosomal enzyme gene SMPD1 is a risk factor for Parkinson disease. Neurology 80, 1606–1610 (2013).
Wu, R. M., Lin, C. H. & Lin, H. I. The p.L302P mutation in the lysosomal enzyme gene SMPD1 is a risk factor for Parkinson disease. Neurology 82, 283 (2014).
Chen, S. et al. A genomic mutational constraint map using variation in 76,156 human genomes. Nature 625, 92–100 (2024).
Foo, J.-N. et al. A rare lysosomal enzyme gene SMPD1 variant (p.R591C) associates with Parkinson’s disease. Neurobiol. Aging 34, 2890.e2813–2890.e2815 (2013).
Gan-Or, Z. et al. The emerging role of SMPD1 mutations in Parkinson’s disease: implications for future studies. Parkinsonism Relat. Disord. 21, 1294–1295 (2015).
Chen, Y. P. et al. Rare variants analysis of lysosomal related genes in early-onset and familial Parkinson’s disease in a Chinese cohort. J. Parkinsons Dis. 11, 1845–1855 (2021).
Mao, C. Y. et al. SMPD1 variants in Chinese Han patients with sporadic Parkinson’s disease. Parkinsonism Relat. Disord. 34, 59–61 (2017).
Ylönen, S. et al. Genetic risk factors in Finnish patients with Parkinson’s disease. Parkinsonism Relat. Disord. 45, 39–43 (2017).
Abbott, S. K. et al. Altered ceramide acyl chain length and ceramide synthase gene expression in Parkinson’s disease. Mov. Disord. 29, 518–526 (2014).
Xicoy, H., Brouwers, J. F., Wieringa, B. & Martens, G. J. M. Explorative combined lipid and transcriptomic profiling of substantia nigra and putamen in Parkinson’s disease. Cells 9, 1966 (2020).
Alcalay, R. N. et al. SMPD1 mutations, activity, and α-synuclein accumulation in Parkinson’s disease. Mov. Disord. 34, 526–535 (2019).
Rhein, C. et al. The acid sphingomyelinase sequence variant p.A487V is not associated with decreased levels of enzymatic activity. JIMD Rep. 8, 1–6 (2013).
Li, Z. et al. Association of rare CYP39A1 variants with exfoliation syndrome involving the anterior chamber of the eye. JAMA 325, 753–764 (2021).
Li, H. Aligning sequence reads, clone sequences and assembly contigs with BWA-MEM. Preprint at arXiv https://doi.org/10.48550/arXiv.1303.3997 (2013).
McKenna, A. et al. The Genome Analysis Toolkit: a MapReduce framework for analyzing next-generation DNA sequencing data. Genome Res. 20, 1297–1303 (2010).
Van der Auwera, G. & O’Connor, B. Genomics in the Cloud (O’Reilly Media, Inc., 2020).
Danecek, P. et al. The variant call format and VCFtools. Bioinformatics 27, 2156–2158 (2011).
Li, H. A statistical framework for SNP calling, mutation discovery, association mapping and population genetical parameter estimation from sequencing data. Bioinformatics 27, 2987–2993 (2011).
Chang, C. C. et al. Second-generation PLINK: rising to the challenge of larger and richer datasets. Gigascience 4, 7 (2015).
Delaneau, O. et al. Integrating sequence and array data to create an improved 1000 Genomes Project haplotype reference panel. Nat. Commun. 5, 3934 (2014).
Teo, Y. Y. et al. Singapore Genome Variation Project: a haplotype map of three Southeast Asian populations. Genome Res. 19, 2154–2162 (2009).
McLaren, W. et al. The Ensembl Variant Effect Predictor. Genome Biol. 17, 122 (2016).
Adzhubei, I. A. et al. A method and server for predicting damaging missense mutations. Nat. Methods 7, 248–249 (2010).
Karczewski, K. J. et al. The mutational constraint spectrum quantified from variation in 141,456 humans. Nature 581, 434–443 (2020).
Wang, Z. et al. Methionine is a metabolic dependency of tumor-initiating cells. Nat. Med. 25, 825–837 (2019).
van Diggelen, O. P. et al. A new fluorimetric enzyme assay for the diagnosis of Niemann–Pick A/B, with specificity of natural sphingomyelinase substrate. J. Inherit. Metab. Dis. 28, 733–741 (2005).
Lee, A. J. et al. Characterization of altered molecular mechanisms in Parkinson’s disease through cell type-resolved multiomics analyses. Sci. Adv. 9, eabo2467 (2023).
Smajić, S. et al. Single-cell sequencing of human midbrain reveals glial activation and a Parkinson-specific neuronal state. Brain 145, 964–978 (2022).
Agarwal, D. et al. A single-cell atlas of the human substantia nigra reveals cell-specific pathways associated with neurological disorders. Nat. Commun. 11, 4183 (2020).
Kamath, T. et al. Single-cell genomic profiling of human dopamine neurons identifies a population that selectively degenerates in Parkinson’s disease. Nat. Neurosci. 25, 588–595 (2022).
Hao, Y. et al. Integrated analysis of multimodal single-cell data. Cell 184, 3573–3587 (2021).
McGinnis, C. S., Murrow, L. M. & Gartner, Z. J. DoubletFinder: doublet detection in single-cell RNA sequencing data using artificial nearest neighbors. Cell Syst. 8, 329–337 (2019).
Alafuzoff, I. et al. Staging of neurofibrillary pathology in Alzheimer’s disease: a study of the BrainNet Europe Consortium. Brain Pathol. 18, 484–496 (2008).
Alafuzoff, I. et al. Assessment of β-amyloid deposits in human brain: a study of the BrainNet Europe Consortium. Acta Neuropathol. 117, 309–320 (2009).
Attems, J. et al. Neuropathological consensus criteria for the evaluation of Lewy pathology in post-mortem brains: a multi-centre study. Acta Neuropathol. 141, 159–172 (2021).
Anscombe, F. J. On estimating binomial response relations. Biometrika 43, 461–464 (1956).
Haldane, J. B. S. The mean and variance of χ2, when used as a test of homogeneity, when expectations are small. Biometrika 31, 346–355 (1940).
Lee, S. et al. Optimal unified approach for rare-variant association testing with application to small-sample case–control whole-exome sequencing studies. Am. J. Hum. Genet. 91, 224–237 (2012).
Khor, C. C. et al. Genome-wide association study identifies five new susceptibility loci for primary angle closure glaucoma. Nat. Genet. 48, 556–562 (2016).
Acknowledgements
We thank W.-Y. Meah (Genome Institute of Singapore), S. H. Ng (National Neuroscience Institute), W. L. Beh, W. Tay, K. Wong and A. Ang (Nanyang Technological University Singapore) for administrative support. We thank S. W. Lim and Y. W. Y. Oo for assistance in structural modeling. We also thank P. C. Ng and H. Liany for their work on the early version of the variant annotation and analysis pipeline. This work is supported by the Singapore Ministry of Health’s National Medical Research Council Open Fund Large Collaborative Grant (MOH-000207 to E.-K.T.; MOH-001072 to T.A. and C.C.K.); the Open Fund Individual Research Grant (MOH-000559 to J.N.F.; MOH-001110 to Z.W. and Y.S.H.; MOH-001214 to Y.X.); the Singapore Translational Research Investigator Award (STaR) (MOH-000435 to. T.A. and Z.W.); the Open Fund Young Individual Research Grant (MOH-001329 to E.GY.C); and the Singapore Ministry of Education Academic Research Fund Tier 2 (MOE-T2EP30220-0005 to J.N.F.; MOE-T2EP30220-0008 to Y.X.) and Tier 3 (MOE-MOET32020-0004 to J.N.F. and Y.X.). C.C.K. is supported by the Singapore National Research Foundation Investigatorship (NRF-NRFI2018-01). S.-Y.L. and A.H.T. are supported by the University of Malaya Parkinson’s Disease and Movement Disorders Research Program (PV035-2017). Y.S.H. and E.KL.P. are supported by the Agency for Science, Technology and Research (A*STAR). R.N.A.’s research is funded by the Michael J. Fox Foundation, the Silverstein Foundation and the Parkinson’s Foundation. Collection of DNA samples by J.L.W. was funded by National Institutes of Health (NIH) EY015473 and NIH P30 EY014104. Work by M.A.N. and C.B. was supported, in part, by the Intramural Research Program of the NIH, National Institute on Aging, NIH, Department of Health and Human Services (project no. ZO1 AG000534); the National Institute of Neurological Disorders and Stroke; the Office of Intramural Research; and the NIH Office of the Director; and used the computational resources of the NIH STRIDES Initiative (https://cloud.nih.gov) through the Other Transaction agreement: Azure: OT2OD032100, Google Cloud Platform: OT2OD027060, Amazon Web Services: OT2OD027852 and the NIH HPC Biowulf cluster (https://hpc.nih.gov). This work was also supported by the A*STAR Computational Resource Center through the use of its high-performance computing facilities.
Author information
Authors and Affiliations
Contributions
The study was conceptualized by E.-K.T., C.C.K., Z.W. and J.N.F. Sample collection and patient assessments were conducted by S.J.C., E.Y.N., L.CS.T., L.L.C., Y.C., W.-L.A., K.M.P., J.L.L., Y.W.T., V.M., A.YY.C., J.-J.L., B.S.J., A.H.T., A.A.A., S.-Y.L. and E.-K.T. K.S., C.C.T., C.P.P., J.A., K.H.P., J.L.W., T.A., M.B.M., C.B., M.A.N., L.A.R., R.N.A. and Z.G.-O. contributed data. Experiments were designed by E.GY.C., Z.L., M.T., Y.J.H., W.L.C., T.J.T., E.KL.P., Y.S.H., C.H.C., T.X.P., R.R., Y.X., C.C.K., E.-K.T., Z.W. and J.N.F. Experiments were performed by E.GY.C., Z. Liu, M.T., Y.J.H., W.L.C., T.J.T., E.KL.P., X.Y.C., E.YT.L., C.H.C., J.-J.L. and T.X.P. Data analysis was conducted by E.GY.C., Z. Liu, Z. Li, M.M.L., M.T., Y.J.H., W.L.C., T.J.T., E.KL.P., Y.S.H., X.Y.C., E.YT.L., C.H.C., J.-J.L., T.X.P., J.L.W., L.A.R., R.R., Y.X., C.C.K., Z.W. and J.N.F. E.GY.C., C.C.K., Z.W. and J.N.F drafted the paper, with input from all other authors. All authors critically assessed the paper.
Corresponding authors
Ethics declarations
Competing interests
Z.G.-O. received consultancy fees from Lysosomal Therapeutics, Idorsia, Prevail Therapeutics, Ono Therapeutics, Denali, Handl Therapeutics, Neuron23, Bial Biotech, Bial, UCB, Capsida, Vanqua Bio, Congruence Therapeutics, Takeda, Jazz Pharmaceuticals, Guidepoint, Lighthouse and Deerfield. R.N.A. received consultation fees from Biogen, Biohaven, Capsida, Gain Therapeutics, Genzyme/Sanofi, Janssen, Servier, SK Biopharmaceuticals, Takeda and Vanqua Bio. Y.X. holds a stock option in NeoCytogen Therapeutics where she is scientific co-founder and Chief Scientific Officer. M.A.N.’s participation in this project was part of a competitive contract awarded to DataTecnica, LLC by the National Institutes of Health to support open science research. M.A.N. also owns stock in Character Bio, Inc. and Neuron23, Inc. The other authors declare no competing interests.
Peer review
Peer review information
Nature Aging thanks Huw Morris and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data tables and figures
Extended Data Fig. 1 Quantile-Quantile plot of all autosomal genes from the Discovery dataset.
A stratified CMH test without continuity correction was used to evaluate gene-based burden across the exomes of the study participants from the 5 countries studied (“PCMH”) and indicated by blue circles. SKAT-O gene-based burden after adjustment for principal components (PC1-PC3), per sample variant counts and average per sample coverage (“Padj”) indicated by red circles. Details in Supplementary Table 22.
Extended Data Fig. 2 Replication of GBA1 association in Chinese and European datasets based on rare predicted pathogenic variants.
CMH without continuity correction used across strata. Data presented as OR and 95% confidence interval (CI).
Extended Data Fig. 3 Distribution of ASM enzymatic activity levels of rare SMPD1 variants in relation to protein ___domain localisation and tertiary structure integrity.
(a) Each rare SMPD1 variant was classified by its localization to protein domains across the ASM protein, namely the signalling peptide (12 variants), saponin (12 variants), proline linker (7 variants), metallophosphate (70 variants), and C terminus (19 variants). (b) Each rare SMPD1 variant was classified by its effect on ASM protein tertiary structure integrity as benign (15 variants), deleterious (27 variants) and uncertain (7 variants). Analysis for both panels are based on protein crystallography of ASM tertiary structure (PDB: 5i81). Median, 25th-75th quartiles, whiskers of 1.5× IQR shown in boxplot. Two-sided t-test: P < 0.05 indicated by *, P < 0.01 indicated by **; P < 0.001 indicated by ***.
Extended Data Fig. 4 Forest plot of PD associations with rare SMPD1 variants from Discovery and Replication datasets that (a) affect ASM tertiary structure, (b) localized to the signaling peptide, (c) localized to the saponin ___domain, (d) localized to the proline-rich linker, (e) localized to the catalytic metallophosphate ___domain, and (f) localized to the C terminus.
Effect of variants on ASM tertiary structure and localisation based on protein crystallography of ASM tertiary structure (PDB: 5I85). CMH without continuity correction used across strata. Data presented as OR and 95% confidence interval (CI).
Extended Data Fig. 5 Onset ages of Parkinson’s disease cases that carry rare deleterious variants in GBA1 and SMPD1.
(a) Carriers of GBA1 qualifying variants were diagnosed with Parkinson’s disease almost 7 years younger than non-carriers (carriers: median = 55.0 years of age, range = 29-78 years of age; non-carriers: median = 62.0 years of age, range = 22-92 years of age; t-test P = 3.32 × 10-11). (b) Carriers of SMPD1 qualifying variants had similar onset age as non-carriers (carriers: median = 60.0 years of age, range = 32-86 years of age; non-carriers: median = 62.0 years of age, range = 22-92 years of age; t-test P = 0.426). (c) Onset ages in carriers of both GBA1 and SMPD1 qualifying variants. Median, 25th-75th quartiles, whiskers of 1.5× IQR shown in boxplot. *** indicates two-sided t-test P = 3.32 ×10-11.
Extended Data Fig. 6 Polygenic risk scores of individuals based on SMPD1 functionally deficient variant carrier status.
Polygenic risk scores of 60 cases and 27 controls which carry SMPD1 functionally deficient variant shown. Median, 25th-75th quartiles, whiskers of 1.5× IQR shown in boxplot.
Extended Data Fig. 7 Forest plots of PD associations with (a) HLA-DRB1 qualifying variants and (b) ATP5B qualifying variants.
CMH without continuity correction used across strata. Data presented as OR and 95% confidence interval (CI).
Extended Data Fig. 8 Statistical power to identify Parkinson’s disease-associated genes at exome-wide significance.
Statistical power to identify PD-associated genes at exome-wide significance (alpha = 2.5 × 10-6) is dependent on sample size, the combined carrier frequency in the population and effect size (odds ratio) of the variants in each gene. Based on our current Discovery cohort size of 4,298 PD cases and 5,512 controls, we had >90% power to detect genes like GBA1 with large effect sizes (OR > 5) and at combined carrier frequencies ~ 0.5% in the population, and also genes like SMPD1 with smaller effect size (OR ~ 2) but at higher combined carrier frequencies of 1-1.5% in the population (contributed in part by the SMPD1 p.Pro332Arg variant). Genes with similar variant effect sizes as SMPD1 may be missed if they are present at lower combined carrier frequencies of 0.9% or less. Similarly, genes with variant effect sizes comparable with GBA1 will be missed if they are present at combined carrier frequencies of 0.1% or less.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chew, E.G., Liu, Z., Li, Z. et al. Exome sequencing in Asian populations identifies low-frequency and rare coding variation influencing Parkinson’s disease risk. Nat Aging 5, 205–218 (2025). https://doi.org/10.1038/s43587-024-00760-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s43587-024-00760-7
This article is cited by
-
Clinical and functional evidence for the pathogenicity of the LRRK2 p.Arg1067Gln variant
npj Parkinson's Disease (2025)