Abstract
UDP-N-acetylglucosamine-undecaprenyl-phosphate N-acetylglucosaminephosphotransferase (TarO) has been found to simultaneously contribute to β-lactam resistance and virulence of Methicillin-resistant Staphylococcus aureus (MRSA). However, optimization of hit compounds targeting TarO has been hindered due to their high lipophilicity and the poor correlation between the enzyme activity inhibition and β-lactam sensitization. In this study, 31 analogues of Tarocin A were designed, synthesized and evaluated by a luminescence-based reporter preliminary screening. In the subsequent β-lactams synergy test, a good correlation was observed between the results obtained from these two methods. Finally, analog 18a with more potential against TarO and an improved hydrophilicity (clogP = 3.2) was obtained. Compared with Tarocin A, 18a shows stronger β-lactam sensitizing and anti-biofilm activities in vitro, as well as potent anti-virulence and synergistic potency with imipenem in vivo. These results suggest that TarO is a promising target for combating MRSA, and 18a can serve as a lead molecule.
Similar content being viewed by others
Introduction
Methicillin-resistant Staphylococcus aureus (MRSA) is one of the most significant pathogens in both hospital and community settings1,2. Since its isolation in the 1960s, it has posed a serious threat to human and has become a global public health concern3,4,5. Based on the route of MRSA infection, it can be classified into healthcare associate MRSA (HA-MRSA) and community associate MRSA (CA-MRSA)3. Besides the widespread resistance to β-lactams, many CA-MRSA strains also exhibit strong virulence, making them more likely to cause serious infections6,7,8. Due to the increasing resistance of MRSA strains and sluggish progress in the development of new antibiotics, there is an urgent need for exploring new antimicrobial strategies9,10. Among them, the development of β-lactam sensitizers and anti-virulence agents holds significant promise for future development of anti-bacterial drugs8,11,12,13.
Wall teichoic acid (WTA) is an anionic glycophosphate polymer covalently attached to peptidoglycan of bacterial cell14. It is one of the main components of the cell wall for gram-positive bacteria, and plays critical roles in drug resistance and virulence of MRSA12,15. WTA can serve as a scaffold for the localization of penicillin-binding proteins (PBPs), including PBP2, PBP2a and PBP4, thereby influencing peptidoglycan cross-linking and resistance to β-lactams15,16,17,18. Additionally, WTA modulates the expression of major virulence factors such as phenol-soluble modulins (PSMs) and staphylococcal protein A (SpA) by interfering with the function of the two-component signal transduction systems, such as AgrCA, VraSR, and SaeSR8,19,20,21,22, thereby facilitating MRSA in colonization, immune evasion and spread in the host. Biofilms are communities of microorganisms in which cells adhere to a surface and are encased in a matrix composed of extracellular polymeric substances (EPS). Like many human pathogens, S. aureus also has the capability to form biofilms on implanted medical devices and host tissues, resulting in chronic or recurrent infections23. The absence of WTA reduces biofilm formation under both steady and flow conditions, likely by impairing the initial attachment to abiotic surfaces12,24.
The biosynthesis of WTA begins in the cytoplasm, where it is synthesized and subsequently translocated to the cell membrane surface14. TarO, an early-stage enzyme involved in WTA biosynthesis, catalyzes the transfer of N-acetylglucosamine-1-phosphate to a membrane-anchored undecaprenyl-phosphate carrier lipid25,26,27. Unlike late-stage enzymes in the WTA biosynthetic pathway, TarO is not essential for the survival of S. aureus but is critical for WTA biosynthesis15,28,29,30,31. Therefore, inhibiting TarO can prevent the biosynthesis of WTA, thereby reducing virulence, β-lactam resistance and biofilm formation capacity of MRSA11,12,15,22,31.
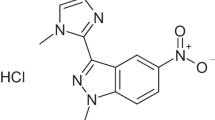
Although TarO is a theoretically promising drug target31, reports on TarO inhibitors are limited and the development of such inhibitors faces significant challenges, resulting in slow progress. For example, as a multi-spanning membrane protein11, expression and purification of TarO are difficult and no successful reports have been documented thus far. This often leads to an indirect and potentially inaccurate evaluations on enzymatic activity inhibition in vitro. Meanwhile, only a few TarO inhibitors have been proven to be β-lactam sensitizers11,31,32, the expected anti-biofilm and anti-virulence activities remain to be validated. Tunicamycin, a natural product isolated from Streptomyces lysosuperficus, was the first compound identified with TarO inhibitory activity32. However, the significant cytotoxicity in eukaryotic cells has hindered its further development11,33,34. Subsequently, Ticlopidine and its analogues were reported to have low to moderate TarO inhibitory activity, but their metabolic stability issues were proved to be difficult to overcome35. In 2016, Lee et al. discovered two series of compounds, with oxazolidin-2-one and benzimidazole scaffold, respectively, exhibit TarO inhibitory activity through high-throughput screening (HTS)11. These compounds exhibit good TarO inhibitory activity and lower cytotoxicity compared to tunicamycin, indicating their potential for further optimization. Although the representative compound, Tarocin A and B showed good performance in TarO inhibition, two major issues remain unresolved. The first is the relatively high lipophilicity (clogP > 7.0) of these compounds and the second is the poor correlation between the enzyme inhibitory activity and sensitizing efficacy to β-lactams. Subsequently, series of modifications were attempted to improve the drug-like properties of these compounds36,37,38. The best performed compound Tarocin A2, which shows better water solubility (lower clogP) but attenuated TarO inhibiting activity compared with Tarocin A, is still not ideal and failed in further investigation38 (Fig. 1).
The existing method for determining the IC50 of TarO inhibitors is indirect, relying on measuring the inhibition of the product generated by cell membrane extracts containing TarO11,31. Although this approach allowed for a quantitative assessment of the inhibitors, there might be inaccuracies in the biochemical assay due to the unavoidable interference from other membrane proteins present in the complex mixtures during the reaction.
In a previous study, we found that targeting TarO rapidly triggers the expression of vraX22, a gene encoding an important immune evasion factor39. This was achieved via the VraSR two-component signal transduction system under cell wall stress stimulation22,40. Specifically, targeting TarO leads to the loss of WTA, causing the mislocalization of penicillin-binding protein 2 (PBP2) and thus blocks peptidoglycan synthesis. The cell wall stress resulting from the ineffective cell wall biosynthesis activates the VraSR system, and the corresponding response regulator VraR dimerizes41 and subsequently binds to the promoter region of vraX to upregulate its expression22. Consequently, a lux-based bioluminescence system was constructed by expressing the lux operon under the control of the vraX promoter (vraXpro-lux)22. This reporter system was used for the preliminary screening of new synthetic TarO inhibitors, considering that the expression of vraX will be induced once the activity of TarO is effectively hindered, thereby a lack of WTA. Considering this and also the high lipophilicity of the compounds may lead to significant differences in inhibitory activity between the cellular and enzymatic levels, we attempt to discover TarO inhibitors at the cellular level directly in preliminary screening, by using the vraXpro-lux bioluminescence reporter system.
With these concerns in mind, we attempted to further optimize the TarO inhibitors based on the previously discovered structure-activity relationship (SAR) of Tarocin A. Thus, 31 analogues of Tarocin A were designed, synthesized and preliminary evaluated via the reporter system. The promising hits were subsequently validated by a β-lactams synergy test, and a strong correlation was observed between the results from these two methods. In the end, a more potent and hydrophilic compound, designated 18a, was obtained and demonstrated well β-lactam sensitization, anti-virulence and anti-biofilm activities against MRSA. This study provides further insights into the SAR of Tarocin A, and highlights the utility and convenience of the luminescence-based reporter system for the preliminary screening of TarO inhibitors.
Results
Design
Modification of Tarocin A is divided into three regions as shown in Fig. 2. By introducing heteroatoms or hydrophilic groups respectively to explore possible substitutable sites of compounds. Then, through advantageous structure splicing, attempts are made to obtain compounds that can improve the hydrophilicity while retain the good TarO inhibitory activity.
Chemistry
The synthesis of oxazolidine-2-one intermediates 31a-d proceeded according to the reported route (Scheme 1)38. The aryl bromides 28a-d reacted with Weinreb amide 29 under the action of i-PrMgCl to obtain ketones 30a-d, which were then stereoselectively reduced under Meerwein-Ponndorf-Verley conditions and cyclized with KOH to form 31a-d. Compounds 1–7 were obtained from 31a-d reacted with the corresponding acyl halides in the presence of n-BuLi and treated with the corresponding nucleophiles. Compounds 8–16, 17a-d, 18a-b were synthesized by condensation of 31a-d with corresponding carboxylic acids under basic conditions via condensation agent 2-chloro-1-methylpyridinium iodide (CMPI) and catalyst 4-dimethylaminopyridine (DMAP). Compound 15 were involved in the protection and deprotection of -Boc protecting group.
Reagents and conditions: (I) i-PrMgCl, THF, -10 °C to rt, 16 h; (II) Al(O-i-Pr)3, toluene, 2-propanol, 50 °C, 20 h, then KOH, H2O, rt, 10 h, 34–49% (2 steps); (III) acyl halides, n-BuLi, THF, −78 °C to rt, 2 h, then Et3N, nucleophiles, rt, overnight, 26–56%; (IV) carboxylic acids, CMPI, DMAP, Et3N, DMF, rt, overnight, 40–68%.
The preparation of compounds 19–22 was carried out according to Scheme 2. 31a reacted with acrylic anhydride under the action of LiCl and Et3N to give 32a42. 32a underwent aza-Michael addition with the corresponding Michael donors under the action of NaH or Et3N to obtain 19–22.
As shown in Scheme 3, oximes 23–27 were obtained by condensation of compound 12 or 14 with corresponding hydroxylamines in the presence of acetic acid.
Validation of the evaluation model with known TarO inhibitors
As expected, addition of tunicamycin or Tarocin A, the previously discovered TarO inhibitor, to MRSA USA300 LAC strain could induce the expression of vraXpro-lux during the exponential growth phase in a concentration-dependent manner (Fig. 3A–D). Meanwhile, compared to wild-type strain, it was reported that the tarO mutant exhibits enhanced autolysis in the late growth stage, resulting in a reduced cell density, reflected by the optical density at 600 nm (OD600)22. In fact, after entering the post-exponential growth phase, treating with tunicamycin or Tarocin A effectively reduced the bacterial growth density, there by a lower OD600 value (Fig. 3E, F). Based on these features, we presume that when an inhibitor acts on TarO, the plateau growth curve of the treated wild-type strain will be between the untreated wild-type strain and the tarO mutant, along with raised expression of vraXpro-lux. By choosing the twentieth hour (determined by multiple tests) as the sampling point during the plateau phase, relative inhibition rate of different concentrations of active compounds was obtained and used to plot a dose-response curve, and the IC50 was calculated.
Data from n = 2 biological replicates and reported as the mean ± SD. A, B Expression of vraXpro-lux induced by different concentrations of tunicamycin and Tarocin A, respectively. C, D Enlarged figure of (A) and (B) for the first five hours after induction. E, F The corresponding growth curve treated by tunicamycin or Tarocin A. Growth curve of a tarO null mutant of USA300 LAC strain was also illustrated as a positive control, and the black arrow indicated the time at which OD600 was recorded and used for IC50 calculation. In (E) and (F), data from WT control and the isogenic ΔtarO strain was derived from the same two biological replicates, respectively.
TarO inhibitors can achieve dual guarantees of low lipophilicity and high activity
To explore whether TarO inhibitors are able to maintain activity with a low lipophilicity, we modified Tarocin A regionally to test the tolerance range of each part. clogP was used as rough estimate of the lipophilicity of compounds.
Initially, attempts were made to modify the linker between the oxazolidine-2-one and the naphthalene (Table 1). As expected, a positive correlation between compound lipophilicity and activity was generally observed. The introduction of a sulfur atom with better lipophilicity resulted in compound 2 exhibiting potent TarO inhibitory activity, while the introduction of groups with more water-soluble led to varying degrees of decreased activity (compounds 3, 4, 5 and 7), see Supplementary Fig. 1 and 2. Additionally, the flexibility of the alkyl chain is essential for TarO inhibitory activity, as replacement with azetidine (compound 6) resulted in loss of activity.
Due to the challenges associated with modifying the linker, we turned our attention to the naphthyl group (Table 2). First, we attempted to replace the aromatic ring with a saturated alkyl ring, but the resulting compound 8 was inactive, implying that there might be crucial π-π interactions in this region. Furthermore, when a strongly hydrophilic thiomorpholine-1,1-Dioxide was fused to the benzene ring, compound 9 exhibited potent inhibition activity comparable to Tarocin A while compound 19 without aromatic ring on the right part lost its activity. Therefore, we further explored the TarO inhibition activity with various benzene-fused cycloalkyl compounds containing hydrogen bond acceptors (compounds 10–15, 17a), among which, compounds 12, 14, and 17a displayed increased activity with reduced clogP. Except highly lipophilic compound 2 (clogP = 7.6), Compound 10 exhibited most potent TarO inhibiting activity in vitro (Fig. 4 and Table 2), it was selected for further investigation to verify this assay. Since compound 17a successfully lowered the clogP with potent activity, we continued to explore the modification at position 6/7 on the quinolin-4(1H)-one of 17a (compounds 20–22), as well as the introduction of more hydrophilic hydrogen bond acceptors at the carbonyl positions of compounds 12 and 14 to explore their effects on activity (compounds 23–27). Unfortunately, these further substitution derivatives all led to decreased or lost activity (Supplementary Fig. 1 and 2), possibly due to the limited binding pocket space for the naphthalene ring. To further explore the chemical space of compound 17a, we replaced the benzene ring with heterocycles (16, 18a), and we were pleased to find that compared with Tarocin A and A2, compound 18a has a much lower clogP, while also improved the inhibition activity to some extent (Fig. 4 and Table 2). Additionally, the water solubility of compound 18a (20 μg/mL) was significantly improved compared to Tarocin A (almost insoluble in pure water).
A–C Expression of vraXpro-lux induced by different concentrations of compound 10, 18a and 18b, respectively. D–F Enlarged figure of (A–C) for the first five hours after induction. G–I Corresponding growth curve treated by compound 10, 18a or 18b. J–L Doses–response curve generated by different concentrations of the three compounds and TarO inhibition rate, data was obtained from two biological replicates.
For the 3,5-bis(trifluoromethyl)phenyl segment, we attempted to replace it with several structures reported in the literature (compounds 17b-d, 18b)38. As shown in Table 3, the activity of the compounds decreased to varying degrees. Among them, 6-methoxy-4(trifluoromethyl)pyridine had a more balanced effect on the compound’s activity and clogP, ultimately resulting in compound 18b with comparable activity to Tarocin A and a lower clogP of 1.7 (Fig. 4 and Table 3).
Further validation of the TarO inhibitor
Since compounds that induce cell wall stress without targeting TarO may also trigger vraXpro-lux expression and inhibit the growth of S.aureus, two other experiments were performed to confirm the target of these new Tarocin A derivatives. First, a chemical suppression experiment of the growth inhibition by depleting late-state WTA biosynthesis was conducted. This strategy based on the previously paradoxical observation that while genes for late WTA synthesis steps are essential, they become dispensable in strains lacking early-step genes, such as tarO or tarA (encoding for N-acetylglucosaminyldiphospho-undecaprenol-N-acetyl-β-D-mannosaminyltransferase)43. The suppression test has been used to identify inhibitors of early steps for WTA biosynthesis, and several different scaffolds of compounds, including the TarO inhibitors, have been described11,38,44. Consistent with the previous report, Targocil could inhibit the growth of S.aureus with a MIC value about 8 μg/mL (Fig. 5) by targeting TarG, which involved in the late-step of WTA biosynthesis and thus plays an essential role in S.aureus survival45. As expected, Targocil did not exhibit a lethal effect on the tarO mutant (Fig. 5), since the early-step of WTA biosynthesis was disrupted. Surprisingly, compound 18a could effectively alleviate the growth inhibition of Targocil on WT strain at a concentration as low as 0.25 μg/mL. This suggested that 18a may target an early step of WTA biosynthesis.
Second, the vraXpro-lux induction and growth inhibition experiment were conducted using a tarO mutant, as we assumed that a compound with other targets may still change the growth characteristic and the vraXpro-lux expression pattern of the mutant, whereas a TarO inhibitor would not, as its target is absent in the mutant. Indeed, neither Tarocin A nor 18a further changed the vraXpro-lux expression pattern as well as the growth characteristics of the mutant (Fig. 6).
A, D Expression of vraXpro-lux induced by different concentrations of Tarocin A and compound 18a, respectively. B, E Enlarged figure of (A) and (D) for the first five hours after induction. C, F Corresponding growth curve treated by Tarocin A and compound 18a. TntarO, S.aureus JE2 harbors a vraXpro-lux reporter system with a transposon inserted in tarO, causing this gene disrupted. S.aureus JE2, a derivative of USA300 LAC strain after all three native plasmids were cured for facilitating genetic manipulation50.
TarO inhibitors exhibit no eukaryotic cell toxicity
Excellent antibacterial adjuvants should avoid toxicity to both bacteria and eukaryotic cells in order to minimize bacterial survival pressure and maximize the safety. To assess whether the new derived TarO inhibitors have bacteriostatic potential toward S.aureus, minimum inhibitory concentration (MIC) of some representatives, including compounds 10, 18a, and 18b, were tested against three MRSA strains (USA300 LAC, USA400 MW2 and HS663). As shown in Table 4, all compounds showed no anti-S.aureus activity, as MIC of these compounds were above 256 μg/mL. Furthermore, no significant eukaryotic cell toxicity was observed, as the IC50 of these compounds was above 20 μM for all three tested cell lines.
New TarO inhibitors can effectively increase the sensitivity of MRSA to β-lactams
To determine whether the compounds identified as positive hits in preliminary screening can enhance the sensitivity of MRSA to β-lactam antibiotics, compounds 10, 18a, and 18b were evaluated for their synergistic inhibitory effects against various MRSA strains in combination with different β-lactam antibiotics (USA300 with oxacillin, USA400 with oxacillin, or HS663 with imipenem) using a checkerboard assay. As shown in Table 5, fractional inhibitory concentration index (FICI) of the compounds with each corresponding antibiotic was less than or close to 0.50, indicating their potential to sensitize MRSA to β-lactams, as expected. Notably, the minimum sensitization concentration of the compounds is positively correlated with the inhibition ability determined in the preliminary screening. In other words, the lower the IC50 value of the compounds, the lower the concentration was required for sensitizing β-lactam antibiotics (in general, 10 < 18a < 18b ≈ Tarocin A). However, consistent with the previous report38, there is no correlation between the maximum sensitization fold for β-lactams and the IC50 value of the compounds, as shown in Table 6). Overall, the order for the maximum sensitization fold was Tarocin A < 10 < 18b < 18a. This trend was further confirmed by testing additional compounds, with the strongest sensitization effect exceeding 1024-fold, see Supplementary Table 1.
Anti-biofilm formation of the new TarO inhibitors
As WTA was important for the initial adhere of S.aureus cells to the surface of abiotic surfaces and essential for a full formation of the biofilms12, we also explored the anti-biofilm formation potential of the new TarO inhibitors via the crystal staining method. As expected, knockout of tarO significantly impaired biofilm formation of the USA300 LAC strain (Fig. 7A, B). However, Tarocin A did not reduce static biofilm formation in USA300 LAC within the tested concentration range (0.03 to 32 μg/mL), whereas both compound 18a and 18b can significantly reduce the biofilm formation at a concentration as low as 8 μg/mL. Particularly, compound 10, with the lowest IC50 value in preliminary screening, achieved over 90% and near a half inhibition of biofilm formation at a concentration of 0.5 or 0.125 μg/mL, respectively. These results suggest that blocking WTA biosynthesis by targeting TarO may be a promising strategy to combat biofilm formation.
S.aureus USA300 LAC (A) and the its isogenic ΔtarO strain (B) treated by DMSO were used as negative or positive control, respectively. Biofilms were stained with crystal violet (A–F) and released by glacial acetic acid. Absorbance at 560 nm (A560) was recorded and used to quantify the biofilm (G–J). Each experiment was performed with four biological replicates, and data was represented by mean ± SD; *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001, calculated by One-Way ANOVA with Dunnett test. In (G–J), data from WT and the isogenic ΔtarO strains was from the same four biological replicates.
Compound 18a significantly reduce the virulence and increase sensitivity of MRSA to β-lactams
Based on the in vitro data, we further chose compound 18a, as it showed an applaudably improved water solubility while still retained excellent inhibitory activity towards TarO, to evaluate its potential therapeutic effects in vivo using a Galleria mellonella larva infection model. As shown in Fig. 8A, a single administration of 18a at 8 mg/kg and 16 mg/kg significantly extended the survival time of the Galleria mellonella larvae, which was comparable to 20 mg/kg of imipenem. At a higher infection dose, the extension of survival time for 18a at 16 mg/kg was even higher than that of 20 mg/kg of imipenem treating group (Fig. 8B). This indicated that targeting TarO alone could lead to a significant reduce of the MRSA’s virulence. Furthermore, when administrated 18a at a concentration of 16 mg/kg in combination with 20 mg/kg imipenem, a further improvement in the survival rate of the infected Galleria mellonella larvae was observed compared with imipenem treated alone (Fig. 8B).
A The impact of administering 18a or imipenem alone on the survival rate of Galleria mellonella larvae infected; at a dose of 1.5 × 106 CFU. MIC of imipenem against HS663 was 64 μg/mL. B Impact of administering 18a or imipenem alone or in combination on the survival ability of Galleria mellonella larvae infected with HS663 at a dose of 2.0 × 106 CFU. For each group, eighteen larvae were included and the survival/deaths of the larvae was observed d every 12 h for 5 days. *P < 0.05, **P < 0.01, ***P < 0.001, by log-rank test.
Discussion
Antibiotics have empowered humans to combat bacterial infections. However, their misuse has accelerated the emergence of drug-resistant bacteria. Given that bacterial resistance evolves much more rapidly than the development of new antibacterial drugs, there is an urgent need to explore innovative antibacterial strategies. Developing adjuvants that target bacterial virulence or resistance mechanisms represents a promising strategy to combat the growing threat of drug-resistant pathogens.
Although TarO has been validated as a highly effective antibacterial target at the genetic level, research on TarO inhibitors has been progressing rather slowly. Here, utilizing the vraXpro-lux reporter system in hand, we designed, synthesized and efficiently screened the new Tarocin A derivatives for their TarO inhibitory activity. Overall, the novel TarO inhibitors identified in this study exhibited a strong correlation between their IC50 values at the cellular level and their ability to sensitize β-lactam antibiotics. Among the modified compounds, 18a and 18b demonstrated low lipophilicity while maintaining high activity levels. Notably, compound 18a showed excellent anti-biofilm, anti-virulence and sensitizing β-lactams capabilities both in vitro and in vivo. These results collectively underscore that TarO is a promising drug target for combating bacterial infections.
In this study, we further confirmed that the new Tarocin A analog, compound 18a, significantly prolongs the survival time of Galleria mellonella larvae infected with the MRSA HS663 strain. Given its MIC against HS663 exceeds 256 µg/mL, compound 18a does not possess direct antibacterial activity. Thus, its capacity to improve the survival rate likely results from targeting TarO, thereby influencing the expression of virulence or immune evasion factors of HS663. In future studies, testing the tarO mutant would clarify whether its efficacy is achieved by targeting TarO. Moreover, compared with Tarocin A, the newly obtained compounds 10, 18a, and 18b all exhibited antibiofilm activity, which was not reported in previous studies on the Tarocin A analogs.
However, this study has several limitations. First, although Tarocin A has been shown to target TarO, the target of these new inhibitors was just preliminary verified and still needs further confirmation. Secondly, 18a significantly improved its water solubility while maintaining good activity both in vitro and in vivo, this compound did not achieve the desired result in in vitro metabolic stability test (Supplementary Table 3). Future efforts could focus on identifying the metabolites of 18a and blocking its metabolic sites, potentially leading to the discovery of a more promising TarO inhibitor with enhanced metabolic stability and water solubility.
Methods
General procedure for synthesis of compounds 1–7
To a 25 mL two-necked flask equipped with a magnetic stirrer was added 31a (0.5 mmol, l.0 equiv). The flask was then placed at -78 °C and 5 mL anhydrous THF was added under nitrogen. Then, n-BuLi (0.6 mmol, 1.2 equiv) was slowly added to the solution. After the reaction mixture was stirred at -78 °C for 30 min, the corresponding acyl halide (0.6 mmol, 1.2 equiv) was added. Slowly heat the reaction mixture to room temperature and continue stirring for 2 h. Then, Et3N (1.0 mmol, 2.0 equiv) and corresponding nucleophile (0.6 mmol, 1.2 equiv) were added. The reaction mixture was stirred continuously overnight and completion of the reaction was detected by TLC. 15 mL saturated NH4Cl solution and 10 mL × 3 ethyl acetate were added to the reaction solution to separate phases. The organic phase was washed with 10 mL × 3 saturated saline and dried with anhydrous Na2SO4. The crude product was concentrated in vacuum and purified by column chromatography on silica gel to afford the desired product 1–7.
General procedure for synthesis of compounds 8–16, 17a-d, 18a-b
To a 25 mL pear-shaped flask equipped with a magnetic stirrer were added 31a-d (0.5 mmol, 1.0 equiv), corresponding carboxylic acid (0.6 mmol, 1.2 equiv), CMPI (0.6 mmol, 1.2 equiv), and DMAP (0.1 mmol, 0.2 equiv). Then, 5 mL DMF and Et3N (1.5 mmol, 3.0 equiv) was added. After completion of the addition, the reaction mixture was stirred continuously overnight at room temperature and completion of the reaction was detected by TLC. 15 mL saturated NH4Cl solution and 10 mL × 3 ethyl acetate were added to the reaction solution to separate phases. The organic phase was washed with 10 mL × 3 saturated saline and dried with anhydrous Na2SO4. The crude product was concentrated in vacuum and purified by column chromatography on silica gel to afford the desired product 8–16, 17a-d, 18a-b.
General procedure for synthesis of compounds 19–22
To a 25 mL pear-shaped flask equipped with a magnetic stirrer was added NaH (0.6 mmol, 1.2 equiv) (or Et3N for 19), corresponding Michael donors (0.6 mmol, 1.2 equiv) and 5 mL anhydrous DMF. The reaction mixture was stirred for 15 min at room temperature. And then, 32a (0.5 mmol, 1.0 equiv) was added. After completion of the addition, the reaction mixture was stirred for another 30 min and completion of the reaction was detected by TLC. 15 mL saturated NH4Cl solution and 10 mL × 3 ethyl acetate were added to the reaction solution to separate phases. The organic phase was washed with 10 mL × 3 saturated saline and dried with anhydrous Na2SO4. The crude product was concentrated in vacuum and purified by column chromatography on silica gel to afford the desired product 19–22.
General procedure for synthesis of compounds 23–27
To a 25 mL pear-shaped flask equipped with a magnetic stirrer was added 12 or 14 (0.1 mmol, 1.0 equiv), corresponding amine (0.15 mmol, 1.5 equiv), 50 μL acetic acid and 3 mL anhydrous methanol.The reaction mixture was stirred overnight at room temperature and completion of the reaction was detected by TLC. The reaction mixture was then concentrated in vacuum and purified by column chromatography on silica gel to afford the desired product 23–27.
General procedure for synthesis of compounds 31a-d
The synthesis of oxazolidine-2-one intermediates 31a-d proceeded according to the reported route38.
General procedure for synthesis of compounds 32a
To a 50 mL two-necked flask equipped with a magnetic stirrer was added 31a (2.0 mmol, 1.0 equiv), LiCl (2.4 mmol, 1.2 equiv). Then, 10 mL anhydrous THF, acrylic anhydride (2.4 mmol, 1.2 equiv) and Et3N (2.4 mmol, 1.2 equiv) was added under nitrogen. After completion of the addition, the reaction mixture was stirred for 6 h and completion of the reaction was detected by TLC. The reaction mixture was then concentrated in vacuum and purified by column chromatography on silica gel to afford the desired product 32a.
Synthesis of partial carboxylic acids
Most carboxylic acids are obtained via the general synthetic procedure (Such as 3-(4-oxoquinolin-1(4H)-yl)propanoic acid):
To a 25 mL pear-shaped flask equipped with a magnetic stirrer was added quinolin-4(1H)-one (2.0 mmol, 1.0 equiv) and methyl acrylate (4.0 mmol, 4.0 equiv) dissolved by 5 mL AcOH. The reaction mixture was placed in an oil bath, stirred at 110 °C for 16 h. Completion of the reaction was detected by TLC and then concentrated in vacuo.
The crude product and NaOH (4.0 mmol, 4.0 equiv) were added to another 25 mL pear-shaped flask equipped with a magnetic stirrer. Dissolved them by 2 mL H2O and 4 mL MeOH. The reaction mixture was stirred 2 h at room temperature and completion of the reaction was detected by TLC. 10 mL H2O and 10 mL × 3 DCM were added to the reaction mixture. Then, 3 mL HCl (2 M) and 10 mL × 3 n-butanol were added to the aqueous phase. And the organic phase was concentrated in vacuo to obtain the acid. The acid was used without further purification.
Synthesis of 3-(4-oxochroman-8-yl)propanoic acid:
To a 25 mL two-necked flask equipped with a magnetic stirrer was added 8-bromochroman-4-one (2.0 mmol, 1.0 equiv), Pd2(dba)3 (0.1 mmol, 0.05 equiv), tri-tert-butylphosphine tetrafluoroborate (TTBPF) (0.2 mmol, 0.1 equiv). Then, they were dissolved by 6 mL DMF under nitrogen and Et3N (2.4 mmol, 1.2 equiv) was added. Put the reaction mixture in an oil bath, stirred at 120 °C for 5 h. Completion of the reaction was detected by TLC. 20 mL water and 15 mL × 3 ethyl acetate were added to the reaction mixture, the organic phase was washed with saturated saline 15 mL× 3, dried over anhydrous sodium sulfate, then concentrated in vacuo. The crude product was purified by chromatography on silica gel (petroleum ether/ethyl acetate, 2:1) to afford 3-(4-oxochroman-8-yl)propanal.
To a 25 mL pear-shaped flask equipped with a magnetic stirrer was added NaClO2 (4.0 mmol, 4.0 equiv) and NaH2PO4 (2.0 mmol, 2.0 equiv) dissolved by 2 mL H2O, 3 mL t-BuOH and 3 mL 2-methyibut-2-ene. Then 3-(4-oxochroman-8-yl)propanal (1.0 mmol, 1.0 equiv) was added. The reaction mixture was stirred 1 h at room temperature and completion of the reaction was detected by TLC. 5 mL HCl (2 M) was added, and filtered to give 3-(4-oxochroman-8-yl)propanoic acid as a white solid. The acid was used without further purification.
Synthesis of 3-(1-(tert-butoxycarbonyl)-4-oxo-1,2,3,4-tetrahydroquinolin-8-yl)propanoic acid:
To a 50 mL two-necked flask equipped with a magnetic stirrer was added 8-bromo-2,3-dihydroquinolin-4(1H)-one (3.0 mmol, 1.0 equiv), Pd(OAc)2 (0.15 mmol, 0.05 equiv), Tri-o-tolylphosphine (0.9 mmol, 0.3 equiv). Then, they were dissolved by 4 mL DMF and 4 mL Et3N under nitrogen. Put the reaction mixture in an oil bath, stirred at 120 °C for 6 h. Completion of the reaction was detected by TLC. The reaction mixture was filtered. 20 mL water and 15 mL × 3 ethyl acetate were added to the filtrate, the organic phase was washed with saturated saline 15 × 3 mL, dried over anhydrous sodium sulfate, then concentrated in vacuo. The crude product was put into a 25 mL pear-shaped flask equipped with a magnetic stirrer and dissolved by 6 mL DCM. (Boc)2O (4.5 mmol, 1.5 equiv), DMAP (0.6 mmool, 0.2 equiv) and Et3N (3.0 mmol, 1.0 equiv) was added to the solution. Then, stirred overnight at room temperature. Completion of the reaction was detected by TLC. 20 mL water and 15 mL × 3 DCM were added to the reaction mixture, the organic phase was washed with saturated saline 15 mL × 3, dried over anhydrous sodium sulfate, then concentrated in vacuo. Then, the crude product was put into another 25 mL pear-shaped flask equipped with a magnetic stirrer. HCOONH4 (18.0 mmol, 6.0 equiv) and 6 mL EtOH were added. The reaction mixture was heated to reflux and stirred for 2 h and then concentrated in vacuo. The crude product was purified by chromatography on silica gel (petroleum ether/ethyl acetate, 5:1) to afford tert-butyl 8-(3-methoxy-3-oxopropyl)-4-oxo-3,4-dihydroquinoline-1(2H)-carboxylate.
To a 25 mL pear-shaped flask equipped with a magnetic stirrer was added tert-butyl 8-(3-methoxy-3-oxopropyl)-4-oxo-3,4-dihydroquinoline-1(2H)-carboxylate (1.0 mmol, 1.0 equiv) and NaOH (2.0 mmol, 2.0 equiv) dissolved by 2 mL H2O and 4 mL MeOH. The reaction mixture was stirred 2 h at room temperature and completion of the reaction was detected by TLC. 10 mL HCl (1 M) and 10 mL × 3 ethyl acetate were added to the reaction mixture, the organic phase was washed with saturated saline 10 mL × 3, dried over anhydrous sodium sulfate, then concentrated in vacuo to obtain the acid. The acid was used without further purification.
Deprotection of Boc was carried out according to literature methods46.
vraX pro -lux based preliminary screening
Generally, JE2::vraXpro-lux and its isogenic TntarO::vraXpro-lux reporter strains were used for preliminary screening and cellular-based target verification. JE2::vraXpro-lux was obtained by transduction of the vraXpro-lux fusions from RN4220 strain to JE2, a plasmid-cured derivative of the community-associated MRSA strain USA300 LAC. TntarO::vraXpro-lux was further obtained by transposon insertion mutation of the tarO gene using a mariner-based transposon in JE2 reporter strain41. Compounds were dissolved in DMSO to 5.12 mg/mL as the stock solution, and were further diluted with DMSO to a concentration of 100 times of the work solution. To monitor the vraXpro-lux expression level and the growth curve of the reporter strains, overnight cultures of the reporter strains were diluted to an OD600 ≈ 0.1 in fresh TSB (Tryptone Soya Broth) supplemented with or without test compounds, as indicated. Then, 200 μL aliquot of the samples were distributed to a 96-well black-wall clear-bottom plate (Costar, Corning Incorporated), and 45 μL saxoline was added to each well to prevent the evaporation of the medium. vraXpro-lux expression level and the growth curve were measured using a Cytation 1 Multi-Mode Microplate Reader (Biotek) at different time points as indicated.
Quantification the activity of the new TarO inhibitors
For quantification the activity of these new TarO inhibitors, OD600 of the twentieth hour post sub-cultivation was extracted and calculated the relative inhibitory rate (RIR) of the compound. The calculation formula is defined as: RIR = (control groupOD600 (20h) - inhibitor groupOD600 (20h)) / (control groupOD600 (20h) - ∆tarOOD600 (20h)). For each concentration of the inhibitors, two biological replicates were performed and the mean RIR of each concentration was submitted for IC50 calculation by Graphpad prism 9.5.1, using the nonlinear repression (curve fit) and choosing [inhibitor] VS. normalized response -variable slope.
Determination of Solubility of Compounds in Water
Weigh the sample in a 10 mL volumetric flask, dissolve in methanol up to the mark to obtain a reference solution of known concentration. Inject 5 μL into the HPLC, detect peak area at 254 nm wavelength. Prepare supersaturated aqueous solution of the sample, filter and inject 5 μL into the HPLC, detect peak area at 254 nm wavelength. The solubility of the compound in water (CA) is calculated according to the following formula: CS = CA × AB/AA (CA represents the concentration of the reference solution, AA represents the peak area of the reference solution, and AB represents the saturated peak area of the sample).
Antagonistic test of compound 18a against Targocil
The antagonistic effect of 18a against Targocil was tested through a checkerboard assay. The concentrations of 18a and Targocil varied along the rows and columns, respectively. The concentration range for 18a was from 128 μg/mL to 0.25 μg/mL, while the concentration range for Targocil was from 64 μg/mL to 2 μg/mL. Strains without the addition of 18a were used as controls. S.aureus was grown to mid log-phase and then diluted to an OD600 of 0.002 with fresh MHB (Mueller-Hinton broth, cation-adjusted, BD 212322) medium. 100 μL of this freshly diluted culture was added to all wells on the plate, expect for the first row which contained 190 μL diluted culture. 10 μL Targocil stock solution was added into the first row, and mixed several times by pipetting, followed by serial diluted at 1:2 to the lowest concentrations. For serially diluting 18a, 90 μL of the last column of the mixtures were transferred into the first column, and 10 μL 18a was added into the first column, after which the dilution was performed as the Targocil. Checkerboard MIC plates were incubated overnight at 37 °C.
MIC determination
MIC values of the compounds were measured by broth microdilution method with MHB medium. The compounds were dissolved with DMSO to 5.12 mg/mL as the stock, diluted to 256 μg/mL with culture medium, then serial diluted at 1:2 to further reach 128 to 0.0625 μg/mL concentration. 100 μL of dilutions were distributed into 96-well microfilter plates (Thermo scientific 167008) and then 5 μL of exponential phase cultured bacteria (about 105 CFUs) were added. The cultures were incubated at 37 °C for about 24 h. For negative control, same volume of DMSO was added and serially diluted as the test compounds. Vancomycin was used as a positive control. MIC values were defined as the lowest concentration that completely inhibit the growth of bacteria. The MIC of vancomycin was 1 μg/mL under these conditions.
Checkerboard MIC assay
In the checkerboard assay, concentrations of antibiotics, oxacillin and imipenem, and TarO inhibitors were simultaneously varied across columns and the rows, respectively. In such a condition, each well had a different combination of concentrations of both compounds. The range of each compound chosen for the checkerboard assay was according to their MIC value. The concentration of oxacillin against USA300 LAC and USA400 MW2 was varied from 16 μg/mL to 0.125 μg/mL, imipenem against HS663 was varied from 32 μg/mL to 0.25 μg/mL, while the inhibitors was varied from 32 μg/mL to 0.03125 μg/mL. S.aureus USA300 LAC, USA400 MW2 and HS663 were grown to mid log-phase and then diluted to an OD600 of 0.002 with fresh MHB medium. 100 μL of this freshly diluted culture was added to all wells on the plate, expect for the first row which contained 190 μL. 10 μL antibiotic stock solutions were added into the first row, and mixed several times by pipetting, followed by serial diluted at 1:2 to the lowest concentrations. For serially diluting the inhibitors, 90 μL of the last column of the mixtures were transferred into the first column, and 10 μL inhibitors stock solution was added into the first column, after which the dilution was performed as the antibiotics. Checkerboard MIC plates were incubated overnight at 37 °C. For each clear well observed on the checkerboard MIC plate, the fractional inhibitory concentration index (FICI) was calculated as follows: FICI = FIC (inhibitor) + FIC (antibiotic) = MIC inhibitor in combination/ MIC inhibitor alone + MIC antibiotic in combination/MIC antibiotic alone. FIC = Fractional Inhibitory Concentration. A FICI value of < 0.5 indicates synergy, a value between 0.5 and 2 indicates additivity or indifference, and a value > 2 indicates antagonism.
Cytotoxicity assay
The cytotoxicity was detected by Sulforhodamine B method. The human pancreatic cancer cell line Capan-1, human colon cancer cell line HCT-116 and human lung adenocarcinoma cell line NCI-H1373 were purchased from American Type Culture Collection (ATCC; Manassas, VA) and inoculated into 96-well plates in triplicate. The cells were treated with different concentrations of compounds in humidified incubator containing 5% CO2 for 72 h when they reached 70%-80% confluence. Vincristine was added as a positive control. Then, SRB staining agent was added and microplate analyzer was used to read the absorbance at 450 nm wavelength. The cytotoxicity of each compound is expressed as the concentration of the compound that reduces cell viability to 50% (IC50). The optical density (OD) at a wavelength of 450 nm was measured using an SpectraMax 190 Microplate Reader (Molecular Devices; USA). The IC50 value was calculated by the Logit method using Graphpad Prism 9.1.
Static biofilm inhibition assay
Static biofilm inhibition assays were generally performed in polystyrene 96-well plates as previously described47. S.aureus USA300 LAC and its isogenic ΔtarO strains were grown overnight in TSB at 37 °C with shaking at 250 rpm, and then diluted 1:100 in BHI (Brain Heart Infusion Medium) plus 1% glucose. Different concentrations of inhibitors were added to the bacteria dilutions, and 200 μL of the mixtures were distributed into the 96-well plate with 4 biological replicates. DMSO treated WT and ΔtarO samples were used as negative or positive control, respectively. After 24 h static culture at 37 °C, the supernatants were removed carefully and the biofilms were washed with phosphate buffer solution (PBS) for 3 times gently, followed by drying at 65 °C for 1 h. Subsequently, 150 μL methanol was used to fix the biofilm for 30 min at room temperature. After which methanol was removed and the plate was dried again. For quantification, each well was stained with 150 μL of 5% (w/v) crystal violet for approximately 30 min, then washed with sterile ultrapure water for three times and dried. Finally, the biofilm was released into solution using 200 μL of 33% glacial acetic acid and the amount of biofilm was quantified by the absorbance was read at 560 nm.
Galleria mellonella larva infection assay
Galleria mellonella infection experiment was performed according to previous methods24. Generally, HS663 was grown overnight in TSB (Tryptone Soya Broth) at 37 °C with shaking at 250 rpm. Then cultures were diluted 1:100 into 10 ml fresh TSB, and were further grown for 3 h. The bacterial cells were harvested by centrifugation at 5700 g for 5 min, washed twice with sterilized PBS, and suspended with PBS. Galleria mellonella larvae (Tianjin HuiYuDe Biotechnological Co., Ltd.) about 300 mg was selected to infect. Compounds (18a and imipenem) were diluted with solvents containing 18% DMSO, 5% Tween 80 and 77% PBS. After infection for 1 h, the larvae were administrated with compounds or solvent only. Then the Galleria mellonella larvae was cultivated at 37 °C and survival rates were recorded every 12 h for 5 days to analyze the mortality data.
Data availability
The USA300 LAC strain used in this study has its genomic information available at the National Center for Biotechnology Information (NCBI) under the accession number CP055225.1 The authors declare that the data supporting the findings of this study are available within the paper and its Supplementary Information files. Should any raw data files be needed in another format they are available from the corresponding author upon reasonable request.
References
Turner, N. A. et al. Methicillin-resistant Staphylococcus aureus: an overview of basic and clinical research. Nat. Rev. Microbiol. 17, 203–218 (2019).
Murray, C. J. L. et al. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet 399, 629–655 (2022).
DeLeo, F. R., Otto, M., Kreiswirth, B. N. & Chambers, H. F. Community-associated meticillin-resistant Staphylococcus aureus. Lancet 375, 1557–1568 (2010).
Lee, A. S. et al. Methicillin-resistant Staphylococcus aureus. Nat. Rev. Dis. Primers. 4, 18033 (2018).
Mork, R. L. et al. Longitudinal, strain-specific Staphylococcus aureus introduction and transmission events in households of children with community-associated meticillin-resistant S aureus skin and soft tissue infection: a prospective cohort study. Lancet Infect. Dis. 20, 188–198 (2020).
Otto, M. Basis of virulence in community-associated methicillin-resistant Staphylococcus aureus. Annu. Rev. Microbiol. 64, 143–162 (2010).
Otto, M. Community-associated MRSA: what makes them special? Int. J. Med. Microbiol. 303, 324–330 (2013).
Foster, T. J. Can beta-lactam antibiotics be resurrected to combat MRSA? Trends Microbiol 27, 26–38 (2019).
Theuretzbacher, U., Outterson, K., Engel, A. & Karlén, A. The global preclinical antibacterial pipeline. Nat. Rev. Microbiol. 18, 275–285 (2019).
WHO. WHO Bacterial Priority Pathogens List, 2024: Bacterial Pathogens of Public Health Importance to Guide Research, Development and Strategies to Prevent and Control Antimicrobial Resistance (WHO, 2024).
Lee, S. H. et al. TarO-specific inhibitors of wall teichoic acid biosynthesis restore beta-lactam efficacy against methicillin-resistant staphylococci. Sci. Transl. Med. 8, 329ra332 (2016).
Jeong, G. J., Khan, F., Tabassum, N., Cho, K. J. & Kim, Y. M. Controlling biofilm and virulence properties of Gram-positive bacteria by targeting wall teichoic acid and lipoteichoic acid. Int. J. Antimicrob. Ag. 62, 106941 (2023).
Shree, P., Singh, C. K., Sodhi, K. K., Surya, J. N. & Singh, D. K. Biofilms: Understanding the structure and contribution towards bacterial resistance in antibiotics. Med. Microecol. 16, (2023).
Swoboda, J. G., Campbell, J., Meredith, T. C. & Walker, S. Wall teichoic acid function, biosynthesis, and inhibition. Chembiochem 11, 35–45 (2010).
Sewell, E. W. & Brown, E. D. Taking aim at wall teichoic acid synthesis: new biology and new leads for antibiotics. J. Antibiot. (Tokyo) 67, 43–51 (2014).
Leski, T. A. & Tomasz, A. Role of penicillin-binding protein 2 (PBP2) in the antibiotic susceptibility and cell wall cross-linking of Staphylococcus aureus: evidence for the cooperative functioning of PBP2, PBP4, and PBP2A. J. Bacteriol. 187, 1815–1824 (2005).
Srisuknimit, V., Qiao, Y., Schaefer, K., Kahne, D. & Walker, S. Peptidoglycan cross-linking preferences of Staphylococcus aureus penicillin-binding proteins have implications for treating MRSA infections. J. Am. Chem. Soc. 139, 9791–9794 (2017).
Atilano, M. L. et al. Teichoic acids are temporal and spatial regulators of peptidoglycan cross-linking in Staphylococcus aureus. Proc. Natl Acad. Sci. USA 107, 18991–18996 (2010).
Winstel, V. et al. Wall teichoic acid glycosylation governs Staphylococcus aureus nasal colonization. mBio 6, e00632 (2015).
Wanner, S. et al. Wall teichoic acids mediate increased virulence in Staphylococcus aureus. Nat. Microbiol. 2, 16257 (2017).
Brignoli, T. et al. Wall teichoic acids facilitate the release of toxins from the surface of Staphylococcus aureus. Microbiol. Spectr. 10, e0101122 (2022).
Lu, Y. et al. Modulation of MRSA virulence gene expression by the wall teichoic acid enzyme TarO. Nat. Commun. 14, 1594 (2023).
Davies, D. Understanding biofilm resistance to antibacterial agents. Nat. Rev. Drug. Discov. 2, 114–122 (2003).
Vergara-Irigaray, M. et al. Wall teichoic acids are dispensable for anchoring the PNAG exopolysaccharide to the Staphylococcus aureus cell surface. Microbiology. 154, 865–877 (2008).
Schertzer, J. W. & Brown, E. D. Use of CDP-glycerol as an alternate acceptor for the teichoic acid polymerase reveals that membrane association regulates polymer length. J. Bacteriol. 190, 6940–6947 (2008).
D’Elia, M. A., Henderson, J. A., Beveridge, T. J., Heinrichs, D. E. & Brown, E. D. The N-acetylmannosamine transferase catalyzes the first committed step of teichoic acid assembly in Bacillus subtilis and Staphylococcus aureus. J. Bacteriol. 191, 4030–4034 (2009).
Pasquina, L. W., Santa Maria, J. P. & Walker, S. Teichoic acid biosynthesis as an antibiotic target. Curr. Opin. Microbiol. 16, 531–537 (2013).
Campbell, J. et al. Synthetic lethal compound combinations reveal a fundamental connection between wall teichoic acid and peptidoglycan biosyntheses in Staphylococcus aureus. ACS Chem. Biol. 6, 106–116 (2011).
Lee, S. H. et al. Antagonism of chemical genetic interaction networks resensitize MRSA to beta-lactam antibiotics. Chem. Biol. 18, 1379–1389 (2011).
Brown, S. et al. Methicillin resistance in Staphylococcus aureus requires glycosylated wall teichoic acids. Proc. Natl Acad. Sci. USA 109, 18909–18914 (2012).
Farha, M. A. et al. Inhibition of WTA synthesis blocks the cooperative action of PBPs and sensitizes MRSA to β-lactams. ACS Chem. Biol. 8, 226–233 (2013).
Komatsuzawa, H., Suzuki, J., Sugai, M., Miyake, Y. & Suginaka, H. Effect of combination of oxacillin and non-β-lactam antibiotics on methicillin-resistant Staphylococcus aureus. J. Antimicrob. Chemoth. 33, 1155–1163 (1994).
Mashalidis, E. H. & Lee, S. Y. Structures of bacterial MraY and human GPT provide insights into rational antibiotic design. J. Mol. Biol. 432, 4946–4963 (2020).
Hakulinen, J. K. et al. MraY-antibiotic complex reveals details of tunicamycin mode of action. Nat. Chem. Biol. 13, 265–267 (2017).
Farha, M. A. et al. Designing analogs of ticlopidine, a wall teichoic acid inhibitor, to avoid formation of its oxidative metabolites. Bioorg. Med. Chem. Lett. 24, 905–910 (2014).
Labroli, M. A. et al. Discovery of potent wall teichoic acid early stage inhibitors. Bioorg. Med. Chem. Lett. 26, 3999–4002 (2016).
Yang, S. W. et al. Benzimidazole analogs as WTA biosynthesis inhibitors targeting methicillin resistant Staphylococcus aureus. Bioorg. Med. Chem. Lett. 26, 4743–4747 (2016).
Mandal, M. et al. Can we make small molecules lean? optimization of a highly lipophilic TarO inhibitor. J. Med. Chem. 60, 3851–3865 (2017).
Yan, J. et al. Staphylococcus aureus VraX specifically inhibits the classical pathway of complement by binding to C1q. Mol. Immunol. 88, 38–44 (2017).
Dengler, V., Meier, P. S., Heusser, R., Berger-Bächi, B. & McCallum, N. Induction kinetics of the Staphylococcus aureus cell wall stress stimulon in response to different cell wall active antibiotics. BMC Microbiol. 11, (2011).
Leonard, P. G., Golemi-Kotra, D. & Stock, A. M. Phosphorylation-dependent conformational changes and ___domain rearrangements in Staphylococcus aureus VraR activation. Proc. Natl Acad. Sci. USA 110, 8525–8530 (2013).
Pirenne, V. et al. p-Anisaldehyde-photosensitized sulfonylcyanation of chiral cyclobutenes: enantioselective access to cyclic and acyclic systems bearing all-carbon quaternary stereocenters. Org. Lett. 22, 575–579 (2020).
D’Elia, M. A. et al. Lesions in teichoic acid biosynthesis in Staphylococcus aureus lead to a lethal gain of function in the otherwise dispensable pathway. J. Bacteriol. 188, 4183–4189 (2006).
Farha, M. A. et al. Antagonism screen for inhibitors of bacterial cell wall biogenesis uncovers an inhibitor of undecaprenyl diphosphate synthase. Proc. Natl Acad. Sci. USA 112, 11048–11053 (2015).
Swoboda, J. G. et al. Discovery of a small molecule that blocks wall teichoic acid biosynthesis in Staphylococcus aureus. ACS Chem. Biol. 4, 875–883 (2009).
Kolcsár, V. J., Fülöp, F. & Szőllősi, G. Ruthenium(II)‐chitosan, an enantioselective catalyst for the transfer hydrogenation of N‐heterocyclic ketones. ChemCatChem. 11, 2725–2731 (2019).
Huan, X. et al. Design, synthesis, and biological evaluations of substituted pyrazoles as pyrrolomycin analogues against Staphylococcal biofilm. Eur. J. Med. Chem. 236, 114309 (2022).
Chen, F. et al. Small-molecule targeting of a diapophytoene desaturase inhibits S. aureus virulence. Nat. Chem. Biol. 12, 174–179 (2016).
Li, M. et al. MRSA epidemic linked to a quickly spreading colonization and virulence determinant. Nat. Med. 18, 816–819 (2012).
Ding, Y. et al. Metabolic sensor governing bacterial virulence in Staphylococcus aureus. Proc. Natl Acad. Sci. USA 111, E4981–E4990 (2014).
Acknowledgements
This work was supported by grants from the National Key Research and Development Program of China (grant no. 2023YFD1800100), the Shanghai Frontiers Science Center of Drug Target Identification and Delivery, School of Pharmaceutical Sciences, Shanghai Jiao Tong University (to F.C., grant no. ZXWH2170101) and the Research Funds of Hangzhou Institute for Advanced Study, UCAS (grant no. 2023HIAS-V006).
Author information
Authors and Affiliations
Contributions
Y.Z. and F.C. contributed equally to this work. Y.Z. designed and performed the synthesis and optimization of compounds, analyzed and interpreted the data, and drafted the manuscript. F.C. designed and performed the pharmacological experiment, analyzed and interpreted the data and drafted the manuscript. D.C. performed partial of the pharmacological experiment, Q.H. developed the analytic method for HPLC and LCMS. X.Z., L.L. and C.Y. designed the overall study, supervised the experiments, analyzed the results, and polished the paper. All authors contributed to the data analysis, manuscript preparation, and final approval of the version to be submitted.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhong, Y., Chen, F., Chen, D. et al. Design, synthesis and optimization of TarO inhibitors as multifunctional antibiotics against Methicillin-resistant Staphylococcus aureus. npj Antimicrob Resist 3, 28 (2025). https://doi.org/10.1038/s44259-025-00098-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s44259-025-00098-z