Abstract
Inconsistent findings exist regarding the potential association between polluted air and Parkinson’s disease (PD), with unclear insights into the role of inherited sensitivity. This study sought to explore the potential link between various air pollutants and PD risk, investigating whether genetic susceptibility modulates these associations. The population-based study involved 312,009 initially PD-free participants with complete genotyping data. Annual mean concentrations of PM2.5, PM10, NO2, and NOx were estimated, and a polygenic risk score (PRS) was computed to assess individual genetic risks for PD. Cox proportional risk models were employed to calculate hazard ratios (HR) and 95% confidence intervals (CI) for the associations between ambient air pollutants, genetic risk, and incident PD. Over a median 12.07-year follow-up, 2356 PD cases (0.76%) were observed. Compared to the lowest quartile of air pollution, the highest quartiles of NO2 and PM10 pollution showed HRs and 95% CIs of 1.247 (1.089–1.427) and 1.201 (1.052–1.373) for PD incidence, respectively. Each 10 μg/m3 increase in NO2 and PM10 yielded elevated HRs and 95% CIs for PD of 1.089 (1.026–1.155) and 1.363 (1.043–1.782), respectively. Individuals with significant genetic and PM10 exposure risks had the highest PD development risk (HR: 2.748, 95% CI: 2.145–3.520). Similarly, those with substantial genetic and NO2 exposure risks were over twice as likely to develop PD compared to minimal-risk counterparts (HR: 2.414, 95% CI: 1.912–3.048). Findings suggest that exposure to air contaminants heightens PD risk, particularly in individuals genetically predisposed to high susceptibility.
Similar content being viewed by others
Introduction
With a global impact on over 6 million individuals, Parkinson’s disease (PD) stands as the second most prevalent neurodegenerative disorder1. Unfortunately, its incidence has significantly increased over the last three decades, with a 2.5-fold rise2. PD has prominent clinical manifestations, including resting tremor, bradykinesia, rigidity, and postural instability. Such indicators have a significant effect on the quality of life of PD patients. Given the progressive and irreversible nature of this disease, the prevention of PD is of paramount importance. However, despite extensive research, PD’s underlying risk factors remain poorly understood. It highlights the urgent need for further investigation and intervention to improve our understanding and develop effective strategies for prevention.
Various environmental factors have been considered potential triggers for PD development for many years. According to the Braak hypothesis, alpha-synuclein’s pathological aggregation commences in the gastrointestinal tract and olfactory bulb prior to extending toward the central nervous system3. Consequently, exposure to environmental contaminants, including pesticides, metals, and microorganisms, has been suggested to potentially contribute to the early pathology of PD and ultimately increase the risk of developing the disease4. Despite air pollution still being the most prevailing environment-related risk to the health of human beings, the findings of epidemiological research looking into the association between the said pollution type and PD are varied5,6,7,8,9,10,11,12,13,14,15. While recent studies have suggested a potential association between long-term exposure to air pollution and the onset of PD, the significance of this relationship remains inconclusive due to limitations such as small sample sizes7,10, a low number of cases6, short exposure or follow-up durations6,7,9,11,12,14,15, and a lack of adjustments for other exposure factors, such as smoking5,15,16. Therefore, there is a need for more extensive population-based cohort research to investigate this possible link thoroughly.
In addition to environmental exposures, genetic susceptibility has been demonstrated as another significant risk factor for PD17. Recent genome-wide association studies (GWAS) have uncovered numerous genetic variants associated with an increased PD risk18,19. In this context, formulating polygenic risk scores (PRS) by aggregating multiple variants demonstrates the capacity to identify susceptible individuals20. The occurrence and progression of PD are influenced by both genetic and environmental factors20,21, with the modifying role of genetic susceptibility in the relationship between air pollution and PD risk still largely unknown. In this context, we formulated specific hypotheses to guide our investigation. First, we hypothesized that prolonged exposure to various air pollutants (i.e., PM2.5, PM10, NO2, and NOx) is positively correlated with the incidence of PD. Second, we postulated that there are synergistic effects and interactions between genetic factors and air pollutant exposure, potentially modifying the overall risk of PD.
Results
Descriptive results
Over 2,685,412 person-years and 2356 incident PD events were recorded (median follow-up: 12.07 years, range: 10.46–15.01 years). Table 1 provides the baseline properties of the research subjects. Those who developed PD had a greater probability of being elderly, less affluent, with higher BMI, with a greater risk genetics-wise, and with exposure to more pollutants in the air. Pearson correlation results and summarized statistics for air pollutants are displayed in Supplementary Table 1.
Association between different air pollutants and subsequent Parkinson’s disease
We examined the link between significant air pollutants and PD risk. In the final multivariable-adjusted model, we found that participants exposed to the highest NO2 quartile had a markedly increased PD risk than those exposed to the lowest quartile, with HRs of 1.247 and 95% CI between 1.089 and 1.427. Equally important, subjects exposed to the highest quartile of PM10 showed a 20.1% increased risk of PD compared to subjects in the lowest quartile (HRs = 1.201; 95% CI: 1.052–1.373). On the other hand, our study found no significant correlations between other air pollutants (e.g., PM2.5 and NOx) and the incidence of PD (Table 2). The risk of PD increased by 8.9% for every 10 μg/m3 rise in NO2 exposure (HR: 1.089; 95% CI: 1.026–1.155) and by 36.3% for every 10 μg/m3 rise in PM10 exposure (HR: 1.363; 95% CI: 1.043–1.782). The sensitivity analyses did not significantly alter these results (Supplementary Tables 2–4). As depicted in Supplementary Fig. 1, we investigated the dose-response relationship between each air pollutant and PD events, and NO2 showed a relatively strong effect (nonlinear P = 0.007). Moreover, we conducted additional stratified analyses and observed a robust correlation between PM10 and NO2 exposure and the risk of developing PD in the population under 65 but not in those aged 65 or older. In a similar fashion, PM10 and NO2 were found to have significance alongside PD risk in males but not in females. Notably, significant correlations between air pollution and PD risk were also evident within populations with a higher Townsend deprivation index and an increased count of long-term morbidities (Supplementary Table 5).
Joint effect of PD-PRS and air pollution on Parkinson’s disease risk
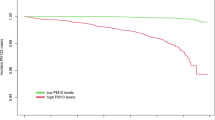
Supplementary Table 6 in the Supplementary Information overviews the PRS’s association with PD risk. A multivariable-adjusted model established a statistically significant link between the PRS and PD (HR: 1.482, 95% CI: 1.352–1.623). Moreover, the high genetic risk group exhibited a substantially elevated incidence of PD, with an HR (95% CI) of 2.182 (1.952–2.438) compared to the low genetic risk group. These findings retained their stability across various multivariate-adjusted models. Figure 1 depicts the risk of developing PD concerning combined exposure to air pollutants and genetic risk. Individuals with elevated air pollutant exposure levels and heightened genetic risk were found to face an increased risk of developing PD [PM10: 2.748 (2.145–3.520), NO2: 2.414 (1.912–3.048), NOx: 2.294 (1.822–2.890)], in contrast to those with low air pollutant exposure levels and minimal genetic risk. Significant interactions between the PRS and NO2, NOx, PM2.5, and PM10 were detected (all P-Multiplicative interactions < 0.001), underscoring their synergistic effects.
The joint associations of long-term NO2 (a), NOx (b), PM2.5 (c), and PM10 (d) exposure and PRS with the risk of incident PD. Cox regression models adjusted for age, sex, BMI, alcohol status, smoking status, education level, employment status, household income, Townsend deprivation index, genotyping array, the number of long-term morbidities, and the first 10 principal components of ancestry. Error bars represent HR with 95% confidence intervals (95% CI).
Discussion
Within this research endeavor, we scrutinized the correlation between air pollutants and the risk of developing PD while factoring in genetic susceptibility. Our investigation unveiled a noteworthy connection between overall air pollution levels and an escalated risk of PD onset. Notably, persistent exposure to NO2 and PM10 emerged as autonomous risk factors for the subsequent manifestation of PD. Upon evaluating the compounded effects of genetic predisposition and air pollutant exposure, we detected a considerable amplification in the risk of PD among participants possessing heightened genetic susceptibility and concurrently exposed to elevated air pollutant concentrations. Furthermore, we identified a substantial association between genetic-based sensitivity and exposure to air pollution. The consequences of protracted air pollution on PD may be exacerbated by genetic susceptibility.
Little is known about the relationship between exposure to air pollution and PD development. The link between long-term air pollutant exposure and PD incidence was extensively examined. According to previous research, we calculated long-term exposures using data on air pollution from 2010. The levels of air pollution in the United Kingdom are still quite stabilized, and the majority of temporal air pollution tendencies are commonly stable throughout the duration covered by the research. Hence, mean air pollution may serve as a surrogate for long-term exposure. Using average levels of air pollution as an analysis estimate further demonstrates the validity of this method. In prospective research involving 78,830 Korean participants, scholars discovered a 42% increased PD risk among subjects exposed to the highest NO2 quartile versus the lowest quartile6. Our findings are consistent with these findings. Notably, that study did not find a correlation between PM2.5 exposure and PD incidence. Similarly, Canadian prospective cohort research detected a correlation between NO2 exposure and the incidence of PD15. Our findings, however, contradict those of various other investigations. Zhu et al. determined that exposure to ambient PM2.5, but not NO2 or PM10, for the long term, was related to PD development22. These inconsistencies may be attributed to differences in study design and other factors, such as the number of PD outcomes, including or excluding other gaseous pollutants, and variations in the constituent factors in PM across different regions. Our study contributes new evidence to the epidemiological study of PD-associated atmospheric pollution. Our findings have consequences for policies and clinical tests, as variations in policies and personal behavior may aid in mitigating air pollution, which may lead to a decrease in PD.
Several potential mechanisms could help explain the connection between air pollution and PD. One of these mechanisms involves the induction of neuroinflammation and oxidative stress by air pollutants, which can promote the onset and development of PD23,24. Air pollutants can enter the circulatory system through penetration of the olfactory mucosa or interstitial lung tissue compartments, resulting in the central nervous system’s inflammation and oxidative stress25,26. Moreover, air pollution may compromise the blood-brain barrier’s integrity, increasing its permeability to toxic substances entering circulation27. Notably, a mouse experiment found that air pollution increased the expression of specific inflammatory genes in the olfactory bulb, a brain region where PD pathology commonly appears early28,29,30. An increasing body of research indicates that environmental toxins entering the gastrointestinal tract may cause the formation of pathological alpha-syn in the gut, which can then spread to the central nervous system and cause the loss of dopaminergic neurons31,32. However, direct evidence supporting this theory is scarce. Thus, additional research is required to ascertain the precise mechanisms underlying the pathogenesis of PD due to air pollution.
For this research, we investigated the link between air pollutants and the incidence of PD in the UK Biobank using PRS. Our results signify that increased air pollution and PD-PRS are related to an increased PD risk, with a substantial interaction between air pollution and PRS categories observed in both joint and stratified analyses. It implies a gene-environment interaction in the occurrence of PD. In addition, individuals with lower levels of air pollution had a significantly lower risk of PD occurrence across all PRS tertiles. Therefore, our findings imply that reducing air pollution levels would provide a potential benefit for individuals who are genetically predisposed to PD.
Our study has multiple strengths. To the best of our knowledge, our investigation represents the initial exploration of the impact of genetic susceptibility on the correlation between exposure to air pollution and the likelihood of developing PD. Our outcomes are more credible due to the magnitude of our sample and the length of our follow-up. In addition, the data provided by the UK Biobank enabled us to consider many confounding factors, mainly genetic susceptibility to PD. Nevertheless, our study has some limitations. As one limitation, certain risk factors for PD, including exposure to 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine and other neurotoxins that may result in motor and non-motor PD symptoms, could be excluded in the statistical modeling due to insufficient pertinent data from the UK Biobank. Another limitation is that the spectrum of air pollutants was insufficient to detect exposure to carbon monoxide, sulfur dioxide, and ozone. Moving forward, other air contaminants may need to be incorporated. Thirdly, exposure evaluation according to a specific address did not rule out exposure misclassification when considering outdoor tasks. Additional research with more precise evaluations is vital to corroborate our outcomes. Fourthly, we must recognize that covariate influence cannot be ruled out, singular contaminant associations may not exhibit independence, and our findings must be cautiously interpreted. Fifth, future global genomic studies may identify additional variants associated with PD, and incorporating more SNPs into future research may enhance genetic risk evaluation. Even though we controlled for many possible confounders in the analyses, unmeasured or unknown variables can still be residual confounders. Additionally, this study differentiated individuals into low, medium, and high-risk groups based on PRS calculated from multiple SNP loci associated with Parkinson’s disease. While this method is commonly employed in previous literature33,34,35, it has limitations as it does not distinguish populations based on specific risk loci. Future research could consider stratifying populations using information from specific loci to validate the findings more comprehensively. Furthermore, since the majority of the subjects in our study were of European descent, our results concerning the association between exposure to air pollution, genetic sensitivity to cataracts, and other populations should be interpreted with caution.
Our study leveraged prospective data to confirm the detrimental, chronic impact of PM10 and NO2 on PD development. Significantly, we discovered that individuals with elevated genetic susceptibility and heightened exposure to air pollutants faced a markedly heightened risk of PD. Therefore, applying effective techniques for mitigating air pollution as soon as possible is crucial in order to protect individuals, particularly those having a high genetic sensitivity, from a higher risk of PD development.
Methods
Study population
The UK Biobank provided the data for this prospective cohort research. The design and survey methodologies of the investigation have already been discussed36. Between 13 March 2006 and 01 October 2010, the baseline survey was administered at 22 testing centres in urbanized regions of Wales, Scotland, and England36. Above half a million subjects gave extensive demographic, socioeconomic, and health data via touchscreen-based surveys and anthropometric assessments37. The NorthWest Multi-center Research Ethics Committee (REC reference 11/NW/0382) endorsed the UK Biobank study, and prior to participation, informed consent was obtained in written form.
This investigation precluded (N = 64,940) persons with a history of baseline PD and those with confirmed PD based on medical data. Therefore, participants with incomplete genetic information (N = 48,778) and air pollution information (N = 34,263) were excluded. Additionally, we excluded individuals of non-White descent (self-reported by participants; N = 39,906), as the genetic instrument used in this study was constructed based on data from White participants. Ultimately, data from 312,009 individuals was available for the final analysis (Supplementary Fig. 2). All study participants gave informed consent in written form to guarantee participation.
Outcomes
We used the algorithm recommended by the UK Biobank to identify participants with PD38. Disease information was extracted from electronic health records of hospital admissions and death registers, accessed through the Hospital Episode Statistics England, Scottish Morbidity Records, or Welsh Patient Case Databases. Following the exclusion of individuals with PD at baseline, PD occurrences were identified by analyzing admission data during subsequent follow-up visits, utilizing the International Classification of Diseases, Ninth Revision (ICD-9), or Tenth Revision (ICD-10) codes. Follow-up time was computed from baseline up to the earliest of the following: PD diagnosis, mortality, stoppage of follow-up, or censorship. Supplementary Table 7 provides data on the codes used for identifying PD cases in this research.
Estimation of air pollutants
The UK Biobank diligently collected estimates of ambient air pollutants, including PM2.5, PM10, NO2, and NOx, spanning 2005 to 2007 and specifically focusing on 2010. During 2005–2007, comprehensive data on ambient air pollution were acquired from European Union-wide maps featuring a precise resolution of 100 × 100 meters. Systematically, the UK Biobank associated each participant’s residential address with these maps, extracting detailed air pollution concentrations within 100 × 100-meter grid cells. Moving forward to 2010, the annual average air pollution concentration was intricately calculated using an advanced land-use regression (LUR) model39,40. This model seamlessly integrated residential addresses collected during participants’ baseline visits and monitoring data meticulously gathered from the European Study of Cohorts for Air Pollution Effects (ESCAPE) from January 26, 2010, to January 18, 2011. The LUR model, a crucial component of the ESCAPE project, underwent thorough validation, the details of which can be found at (http://www.escapeproject.eu/)39. The model’s performance was assessed using the leave-one-out cross-validation method, and the cross-validation R2 for PM2.5, PM10, NO2, and NOx were 77%, 88%, 87%, and 88%, respectively39.
Yearly PM2.5 and NOx concentration data were only accessible for 2010, while NO2 concentration data were accessible for 2005–2007 and 2010. Lastly, PM10 information for 2007 and 2010 was accessible. For pollutants for which only yearly concentration data from 2010 were available, the respective baseline exposure variable was directly stated. In the meantime, we used the average of multiple annual concentrations as the exposure variable for pollutants for which multiple years of annual concentration data were available within the baseline period. For PM10, for example, the exposure level was determined using the mean annual concentrations in 2007 and 2010.
Polygenic risk score
In the present study, the PRS was calculated by summing the weighted risk estimate, which corresponded to the β coefficient of 44 single-nucleotide polymorphisms (SNPs) obtained from the reported PD Genome-Wide Association Study (GWAS)41. Thompson et al. generated a Standard PRS Set, calculated on all UKB individuals, for 28 diseases and eight quantitative traits by meta-analyzing multiple external GWAS sources42. Detailed information on genotyping and quality control can be found in previous studies43. We used the weighted calculation method to get the Parkinson’s disease PRS (PD-PRS), as illustrated by the following Eq. (1):
Where β is per allele log odds ratio (ORs) for PD-associated with SNP, which was obtained from the existing GWAS research42; SNP was documented as 0, 1, and 2 in terms of the number of risk alleles; n was the total of selected SNPs in the current study. The ORs were derived from a former GWAS study. For this study, subjects were classified into three categories, namely low (<−0.584), intermediate (−0.584–0.289), and high (>0.289) genetic risk33,34,35. These categories were determined using the PRS values’ tertile distribution as analyzed.
Covariates
Covariates in this study included age (in years, continuous), sex (i.e., female, male), ethnicity (i.e., White or other), average total household income before tax (i.e., <£18,000, £18,000–£29,999, £30,000–£51,999, £52,000–£100,000, >£100,000), educational level (i.e., college or university degree, others), employment status (i.e., employed or retired, others), smoking status (i.e., current, previous, never), alcohol status (i.e., current, previous, never), and body mass index (BMI, in kg/m2). The Townsend deprivation index was computed using the previous national census output regions where the participant’s postcode was determined, with a greater score indicating a greater degree of deprivation socioeconomically44. Participants’ demographic attributes (such as birth date, sex, and ethnicity) were acquired from respective NHS Primary Care Trust registries prior to their entry at the assessment center. Touch-screen questionnaires were used to collect sociodemographic data (mean overall household income before taxes, level of education, and occupational status) and behavioral information (alcohol and smoking status) at the baseline assessment center visit36. Height and weight were assessed by nurses with sufficient training, and BMI was calculated by the quotient of weight (in kg) and height (in m2). We considered the number of long-term morbidities, as this index is associated with lifespan. Detailed definitions can be found in Supplementary Table 8. We included PD-PRS, a genotyping array, and the first ten ancestry principal components as covariates. The missing data proportions for covariates were as follows: 14.4% for household income, less than 1% for employment status, alcohol status, smoking status, and the Townsend Deprivation Index. To address this, we conducted multiple imputations using the fully conditional specification (FCS) method to impute the missing covariate data45,46,47.
Statistical analyses
Mean ± standard deviation (SD) and number (percentage) were used to represent continuous and categorical variables. Using Cox proportional hazard regression models, the hazard ratio (HR) and 95% confidence interval (CI) for the links between the pollutants of ambient air and genetic risk with incident PD were calculated. The proportionality assumptions were evaluated using Schoenfeld residuals (Supplementary Figs. 3–6). Model 1 utilized a Cox regression model with no adjustments. Model 2 was regulated with respect to sex, age, alcohol consumption, BMI, educational level, smoking status, household income, employment status, and the Townsend deprivation index. Model 3 was modified to take model 2 and the long-term morbidity count into account. Moreover, we performed multiple sensitivity analyses to evaluate the outcomes’ validity. To compare the results of multiple imputations, we first restrict the analysis to subjects with complete data on age, sex, ethnicity, education level, employment status, household income, and Townsend deprivation index covariates. To reduce the impact of reverse causation, we did not include those participants who developed PD during the initial two follow-up years. Third, we made additional adjustments for other covariates (BMI, alcohol consumption, smoking status, the number of long-term morbidities, Parkinson’s disease polygenic risk score, genotyping array, and the first ten principal components of ancestry) to avoid potential confounding. Lastly, we conducted stratified analyses to explore how air pollutants are associated with incident PD, considering age (<65; ≥65), sex (male; female), BMI (high: above median value; low: below median value; median = 26.85), Townsend deprivation index (high: above median value; low: below median value; median = −2.3464), and the count of long-term morbidities (none, one, two or more).
We investigated the dose-response association between pollutants in air and PD risk using restricted cubic spline regressions (knot = 3, degree of freedom = 9). As a reference group, we analyzed the coupled effect of pollutants in air and PD-PRS on the probability of developing PD using subjects in the lowest quartile of air pollution and lowest PRS. Within a 4 × 3 grouping framework, we were able to comprehensively analyze the relationship between air pollutants and genetic-based PD risk. A fully adjusted model with a multiplicative interaction term was used to assess the association between pollutants in air and PRS tertiles. Furthermore, we assessed the association between air pollution and PD by stratifying the data based on PD-PRS tertiles.
All information was analyzed using R (version 4.2.3), and the statistical significance (two-tailed) was established to a P value less than 0.05.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
The data used in the present study are available from UKB with restrictions applied. Data were used under license and are thus not publicly available. Access to the UKB data can be requested through a standard protocol (https://www.ukbiobank.ac.uk/register-apply/). Data used in this study are available in the UK Biobank under application number 19542. All data supporting the findings described in this manuscript are available in the article and in the Supplementary Information and from the corresponding author upon request.
Code availability
The code for reproducing the results can be found on [https://github.com/yihezuiji/hymdata/blob/main/airpollution_COX.md].
References
Group, G. B. D. N. D. C. Global, regional, and national burden of neurological disorders during 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Neurol. 16, 877–897 (2017).
Collaborators, G. B. D. P. s. D. Global, regional, and national burden of Parkinson’s disease, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 17, 939–953 (2018).
Braak, H. et al. Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol. Aging 24, 197–211 (2003).
Chen, H. & Ritz, B. The search for environmental causes of Parkinson’s disease: moving forward. J. Parkinsons Dis. 8, S9–S17 (2018).
Chen, C. Y. et al. Long-term exposure to air pollution and the incidence of Parkinson’s disease: a nested case-control study. PLoS ONE 12, e0182834 (2017).
Jo, S. et al. Association of NO2 and other air pollution exposures with the risk of Parkinson’s disease. JAMA Neurol. 78, 800–808 (2021).
Kirrane, E. F. et al. Associations of ozone and PM2.5 concentrations with Parkinson’s disease among participants in the agricultural health study. J. Occup. Environ. Med. 57, 509–517 (2015).
Lee, H. et al. Short-term air pollution exposure aggravates Parkinson’s disease in a population-based cohort. Sci. Rep. 7, 44741 (2017).
Lee, P. C. et al. Traffic-related air pollution increased the risk of Parkinson’s disease in Taiwan: a nationwide study. Environ. Int. 96, 75–81 (2016).
Lee, P. C. et al. Gene-environment interactions linking air pollution and inflammation in Parkinson’s disease. Environ. Res. 151, 713–720 (2016).
Liu, R., Young, M. T., Chen, J. C., Kaufman, J. D. & Chen, H. Ambient air pollution exposures and risk of Parkinson’s disease. Environ. Health Perspect. 124, 1759–1765 (2016).
Palacios, N. et al. Air pollution and risk of Parkinson’s disease in a large prospective study of men. Environ. Health Perspect. 125, 087011 (2017).
Ritz, B. et al. Traffic-related air pollution and Parkinson’s disease in Denmark: a case-control study. Environ. Health Perspect. 124, 351–356 (2016).
Salimi, F. et al. Associations between long-term exposure to ambient air pollution and Parkinson’s disease prevalence: a cross-sectional study. Neurochem. Int. 133, 104615 (2020).
Shin, S. et al. Effects of ambient air pollution on incident Parkinson’s disease in Ontario, 2001 to 2013: a population-based cohort study. Int. J. Epidemiol. 47, 2038–2048 (2018).
Cerza, F. et al. Residential exposure to air pollution and incidence of Parkinson’s disease in a large metropolitan cohort. Environ. Epidemiol. 2, e023 (2018).
Blauwendraat, C., Nalls, M. A. & Singleton, A. B. The genetic architecture of Parkinson’s disease. Lancet Neurol. 19, 170–178 (2020).
Kia, D. A. et al. Identification of candidate Parkinson’s disease genes by integrating genome-wide association study, expression, and epigenetic data sets. JAMA Neurol. 78, 464–472 (2021).
Nalls, M. A. et al. Identification of novel risk loci, causal insights, and heritable risk for Parkinson’s disease: a meta-analysis of genome-wide association studies. Lancet Neurol. 18, 1091–1102 (2019).
Jacobs, B. M. et al. Parkinson’s disease determinants, prediction and gene-environment interactions in the UK Biobank. J. Neurol. Neurosurg. Psychiatry 91, 1046–1054 (2020).
Bloem, B. R., Okun, M. S. & Klein, C. Parkinson’s disease. Lancet 397, 2284–2303 (2021).
Zhu, Z. et al. Residential greenness, air pollution and incident neurodegenerative disease: a cohort study in China. Sci. Total Environ. 878, 163173 (2023).
Jayaraj, R. L., Rodriguez, E. A., Wang, Y. & Block, M. L. Outdoor ambient air pollution and neurodegenerative diseases: the neuroinflammation hypothesis. Curr. Environ. Health Rep. 4, 166–179 (2017).
Kempuraj, D. et al. Brain and peripheral atypical inflammatory mediators potentiate neuroinflammation and neurodegeneration. Front. Cell. Neurosci. 11, 216 (2017).
Oberdörster, G. et al. Translocation of inhaled ultrafine particles to the brain. Inhal. Toxicol. 16, 437–445 (2004).
Bond, J. A. et al. Disposition and metabolism of [14C]dibenzo[c,g]carbazole aerosols in rats after inhalation. Fundam. Appl. Toxicol. 7, 76–85 (1986).
Oppenheim, H. A. et al. Exposure to vehicle emissions results in altered blood-brain barrier permeability and expression of matrix metalloproteinases and tight junction proteins in mice. Part. Fibre Toxicol. 10, 62 (2013).
Wong, J., Magun, B. E. & Wood, L. J. Lung inflammation caused by inhaled toxicants: a review. Int J. Chron. Obstruct Pulmon Dis. 11, 1391–1401, (2016).
Levesque, S. et al. Diesel exhaust activates and primes microglia: air pollution, neuroinflammation, and regulation of dopaminergic neurotoxicity. Environ. Health Perspect. 119, 1149–1155 (2011).
Levesque, S., Surace, M. J., McDonald, J. & Block, M. L. Air pollution & the brain: subchronic diesel exhaust exposure causes neuroinflammation and elevates early markers of neurodegenerative disease. J. Neuroinflammation 8, 105 (2011).
Anselmi, L. et al. Ingestion of subthreshold doses of environmental toxins induces ascending Parkinsonism in the rat. NPJ Parkinsons Dis. 4, 30 (2018).
Pan-Montojo, F. et al. Environmental toxins trigger PD-like progression via increased alpha-synuclein release from enteric neurons in mice. Sci. Rep. 2, 898 (2012).
Zhang, J. et al. Association of combined exposure to ambient air pollutants, genetic risk, and incident rheumatoid arthritis: a prospective cohort study in the UK Biobank. Environ. Health Perspect. 131, 37008 (2023).
Ma, Y. et al. Air pollution, genetic susceptibility, and the risk of atrial fibrillation: a large prospective cohort study. Proc. Natl Acad. Sci. USA 120, e2302708120 (2023).
Li, D. et al. Genetic susceptibility and lifestyle modify the association of long-term air pollution exposure on major depressive disorder: a prospective study in UK Biobank. BMC Med. 21, 67 (2023).
Sudlow, C. et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 12, e1001779 (2015).
Collins, R. What makes UK Biobank special? Lancet 379, 1173–1174 (2012).
Biobank, U. Algorithmically-defined outcomes (ADOs) Version 2.0. Accessed February 3, 2023.
Eeftens, M. et al. Development of Land Use Regression Models for PM2.5, PM2.5 Absorbance, PM10 and PMcoarse in 20 European study areas; results of the ESCAPE project. Environ. Sci. Technol. 46, 11195–11205 (2012).
Beelen, R. et al. Development of NO2 and NOx land use regression models for estimating air pollution exposure in 36 study areas in Europe - The ESCAPE project. Atmos. Environ. 72, 10–23 (2013).
Chang, D. et al. A meta-analysis of genome-wide association studies identifies 17 new Parkinson’s disease risk loci. Nat. Genet. 49, 1511–1516 (2017).
Thompson, D. J. et al. UK Biobank release and systematic evaluation of optimised polygenic risk scores for 53 diseases and quantitative traits. Preprint at https://doi.org/10.1101/2022.06.16.22276246 (2022).
Bycroft, C. et al. The UK Biobank resource with deep phenotyping and genomic data. Nature 562, 203–209 (2018).
Foster, H. M. E. et al. The effect of socioeconomic deprivation on the association between an extended measurement of unhealthy lifestyle factors and health outcomes: a prospective analysis of the UK Biobank cohort. Lancet Public Health 3, e576–e585 (2018).
Enders, C. K. Multiple imputation as a flexible tool for missing data handling in clinical research. Behav. Res. Ther. 98, 4–18 (2017).
Li, P., Stuart, E. A. & Allison, D. B. Multiple imputation: a flexible tool for handling missing data. JAMA 314, 1966–1967 (2015).
Sterne, J. A. et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ 338, b2393 (2009).
Acknowledgements
This study was supported by grants from the National Natural Science Foundation of China (grant number 82071201, 81971032, 82071997), Shanghai Municipal Science and Technology Major Project (grant number 2018SHZDZX01), Research Start-up Fund of Huashan Hospital (grant number 2022QD002), Excellence 2025 Talent Cultivation Program at Fudan University (grant number 3030277001), the Shanghai Rising-Star Program (grant number 21QA1408700), and ZHANGJIANG LAB, Tianqiao and Chrissy Chen Institute, and the State Key Laboratory of Neurobiology and Frontiers Center for Brain Science of Ministry of Education, Fudan University. The grant funding bodies had no roles in the design, conduct, or data analysis of the study nor in manuscript preparation and approval.
Author information
Authors and Affiliations
Contributions
Concept and design: J.T.Y., L.T.; Acquisition, analysis, or interpretation of data: All authors; Drafting of the manuscript: Y.M.H.; Critical revision of the manuscript for important intellectual content: All authors; Statistical analysis: Y.M.H., Y.H.M., and P.Y.G.; Chart design: Y.M.H.; Obtained funding: J.T.Y.; Administrative, technical, or material support: J.T.Y., L.T.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Huang, YM., Ma, YH., Gao, PY. et al. Genetic susceptibility modifies the association of long-term air pollution exposure on Parkinson’s disease. npj Parkinsons Dis. 10, 23 (2024). https://doi.org/10.1038/s41531-024-00633-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41531-024-00633-1