Abstract
Flooding greatly endangers public health and is an urgent concern as rapid population growth in flood-prone regions and more extreme weather events will increase the number of people at risk. However, an exhaustive analysis of mortality following floods has not been conducted. Here we used 35.6 million complete death records over 18 years (2001–2018) from the National Center for Health Statistics in the United States, highly resolved flood exposure data and a Bayesian conditional quasi-Poisson model to estimate the association of flooding with monthly county-level death rates for cancers, cardiovascular diseases, infectious and parasitic diseases, injuries, neuropsychiatric conditions and respiratory diseases up to 3 months after the flood. During the month of flooding, very severe heavy rain-related floods were associated with increased infectious disease (3.2%; 95% credible interval (CrI): 0.1%, 6.2%) and cardiovascular disease (2.1%; 95% CrI: 1.3%, 3.0%) death rates and tropical cyclone-related floods were associated with increased injury death rates (15.3%; 95% CrI: 12.4%, 18.1%). During the month of very severe tropical cyclone-related flooding, increases in injury death rate were higher for those ≥65 years old (24.9; 95% CrI: 20.0%, 29.8%) than for those aged <65 years (10.2%; 95% CrI: 6.6%, 13.8%) and for females (21.2%; 95% CrI: 16.3%, 26.1%) than for males (12.6%; 95% CrI: 9.1%,16.1%). Effective public health responses are critical now and with projected increased flood severity driven by climate change.
Similar content being viewed by others
Main
Flooding, the inundation of water onto typically dry land, is an urgent global health concern1,2. The number of people living in flood-prone areas has increased by 58–86 million worldwide between 2000 and 2015 (ref. 3), and human settlements in areas with the highest flood risk have grown by 121% since 1985 (ref. 4). Climate change will likely lead to more frequent river, coastal and flash floods globally, compounding population-driven risk1. In the United States, population growth alone is projected to result in an estimated 72% increase in the population exposed to floods annually by 2050, before accounting for the effect of climate change on flooding5. Flooding has been associated with increased rates of injuries6, cardiovascular diseases7, infectious diseases8 and mental health conditions9. However, most previous work has focused on specific flooding case studies related to tropical cyclones10,11, floods over a short period of time12 or on fatalities attributed to acute flash floods13,14. Although tropical cyclones are an important driver of increased flood risk, atmospheric warming, the intensification of the global water cycle and sea-level rise will also lead to more catastrophic floods independent of tropical cyclones15. Identifying health outcomes associated with distinct flood causes is critical for effective disaster and public health preparedness as development patterns and climate change amplify flood risk16.
Floods can affect health through direct and indirect pathways that may function at different time scales leading to both acute and delayed health effects17,18. A storm surge, for example, can cause acute direct effects, including drownings and injuries2,19, whereas standing floodwater that contaminates drinking water sources or facilitates mold growth can lead to delayed direct effects on infectious disease and respiratory outcomes20,21. Rapid displacement can drive acute indirect effects including traffic accidents, stress-induced cardiovascular events, and infectious disease transmission related to overcrowding17,18. Disruptions to critical infrastructure, meanwhile, can lead to delayed indirect effects when people are unable to meet basic needs including access to healthcare, food, and shelter19,22. Most flood-related health outcomes are not restricted to a single exposure pathway or timeline; cardiovascular events, for example, can be triggered by direct exposure to storm surges or occur after periods of chronic disaster-related stress11,17.
Flood cause and severity likely affect the association between exposure and specific health outcomes. Mild or moderate floods, for example, may have a negligible effect on mortality; in some cases, general flood exposure has been associated with decreased overall mortality23. Among snowmelt-related floods, however, even moderate events have longer average durations compared to other flood causes24,25 and may have an effect on health comparable to more severe floods.
Characterizing exposure to floods at a spatial scale appropriate for mortality analyses is a central challenge for studying flood-related health effects as it can be difficult to determine the magnitude and timing of flood events. Here, we address this gap using a validated flood exposure dataset3 to comprehensively examine the association of large floods with death rates for six major causes of death (cancers, cardiovascular disease, infectious and parasitic diseases, injuries, neuropsychiatric conditions and respiratory diseases) over an 18-year period (2001–2018) at the county level across the United States. We evaluated whether these associations differed by flood cause (heavy rain, tropical cyclone, snowmelt and ice jam or dam break) and severity (mild, moderate, severe and very severe); further, we examined the association of flood exposure with cause-specific mortality by age group and sex.
Results
Deaths
There were 35,613,398 deaths from the 6 causes of death in counties that experienced floods during 2001–2018, representing 86.2% of all deaths in these counties (Fig. 1). Total deaths in these counties represented 77.8% of all deaths nationally during the study period. Cardiovascular diseases were the leading cause of death (n = 13,709,850), followed by cancers (n = 9,587,570) and neuropsychiatric conditions (n = 4,390,885) (Supplementary Table 1). Seasonality in death rates varied among the causes of death; death rates were greatest for cardiovascular disease, neuropsychiatric conditions and respiratory disease from December to March (peaking in January), whereas cancer and infectious disease mortality was relatively consistent throughout the year. Injury deaths were more common among younger males (≤54 years old; 43.5% of all injury deaths) for whom death rates peaked between June and August. During 2001–2018, long-term trends in death rates also differed among the causes of death; age-standardized death rates increased by 87.0% for neuropsychiatric conditions and by 12.0% for injuries but substantially decreased for cardiovascular diseases (−34.8%), cancers (−25.9%) and respiratory diseases (−16.0%) (Extended Data Fig. 1).
Flood events
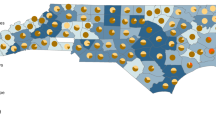
There were 93 large flood events, each typically affecting multiple counties (Supplementary Table 2), which occurred throughout 2,711 counties during 2001–2018 (Fig. 2). The median number of floods per county was 7 (mean: 7.4, range: 1–28). Of the 93 flood events, the majority (61; 65.6% of all floods) were due to heavy rain (Supplementary Table 3). These floods occurred throughout the United States—particularly evident in Appalachia and along the Mississippi River-Ohio River junction—and throughout the year (Extended Data Fig. 2). Tropical cyclone-related flooding was the second-most common flood cause (18; 19.4% of all floods) and primarily occurred along the Gulf and southeastern Atlantic Coasts during the Atlantic hurricane season (June 1 to November 30)26. Snowmelt-related (9; 9.7% of all floods) and ice jam or dam break-related floods (5; 5.3% of all floods) were concentrated in Upper Midwest and Mountain West counties during the late winter and early spring.
Specific flood causes and all-cause death rates
Very severe heavy rain-related floods were associated with increased all-cause death rates during the flood month (1.5%; 95% credible interval (CrI): 1.0%, 2.0%) in addition to 2 months (1.0%; 95% CrI: 0.4%, 1.3%) and 3 months (0.6%; 95% CrI: 0.2%, 1.0%) after the flood (Fig. 3). All other flood severity types, however, were associated with decreased death rates during the flood month. Moderate (1.0%; 95% CrI: 0.4%, 1.2%) and severe (0.4%; 95% CrI: 0.0%, 0.8%) heavy rain-related floods were associated with delayed increases in all-cause death rates 1 and 2 months after the flood, respectively. Severe (−1.6%; 95% CrI: −3.0%, 0.0%) and very severe (−1.3%; 95% CrI: −2.6%, 0.0%) ice jam or dam break-related floods were associated with slight decreases in all-cause death rates during the flood month but with slightly increased death rates 2 and 3 months after the flood.
Snowmelt-related floods of all severity levels were associated with increased all-cause death rates, with mild floods exhibiting the strongest association (8.9%; 95% CrI: 7.6%, 10.1%). Tropical cyclone-related floods were associated with decreased death rates for mild (−2.5%; 95% CrI: −3.4%, −1.5%), moderate (−1.9%; 95% CrI: −2.8%, −1.0%) and severe (−2.0%; 95% CrI: −2.8%, −1.1%) events during the flood month. Death rates increased, however, 1 month after moderate flooding events (1.1%; 95% CrI: 0.7%, 1.6%) and 2 months after very severe flooding events (1.0%; 95% CrI: 0.5%, 1.4%).
Heavy rain-related floods and cause-specific death rates
Very severe heavy rain-related floods were associated with increased death rates for infectious and parasitic diseases (3.2%; 95% CrI:0.1%, 6.2%) and cardiovascular diseases (2.1%; 95% CrI: 1.3%, 3.0%) during the flood month and, for infectious diseases (4.7%; 95% CrI: 2.4%, 7.1%) and injuries (2.6%; 95% CrI: 1.0%, 4.2%), 1 month after flooding events (Fig. 4). The association of heavy rain-related floods with respiratory disease death rates varied by flood severity. Death rates increased 2 months after the event for severe floods (1.9%; 95% CrI: 0.7%, 3.1%) but decreased during the flood month for mild (−2.5%; 95% CrI: −4.1%, −1.0%) and moderate floods (−2.1%; 95% CrI: −3.7%, −1.0%). Mild and moderate heavy rain-related floods were also associated with decreased death rates for neuropsychiatric conditions (−2.1%; 95% CrI: −3.7%, −1.0%) and infectious diseases (−6.3%; 95% CrI: −9.3%, −3.2%), respectively, during the flood month. Cancer death rates showed some evidence of increase 2 (0.8%; 95% CrI: 0.0%, 1.6%) and 3 months (1.1%; 95% CrI: 0.0%, 1.9%) after very severe heavy rain-related flooding, though all associations were close to null.
Ice jam or dam break-related floods and cause-specific death rates
Very severe ice jam or dam break-related floods were associated with decreased death rates during the flood month for infectious and parasitic diseases (−11.0%; 95% CrI: −17.6%, −4.3%), respiratory diseases (−8.3%; 95% CrI: −11.9%, −4.7%) and neuropsychiatric conditions (−5.6%; 95% CrI: −9.0%, −2.1%) (Fig. 4). In the month after very severe floods, death rates increased for infectious diseases (4.4%; 95% CrI: 1.9%, 6.9%) and injuries (3.0%; 95% CrI: 1.4%, 4.7%). Severe ice jam or dam break floods were also associated with decreased infectious disease (−9.7%; 95% CrI: −17.7%, −1.6%) and injury (−7.7; 95% CrI: −13.2%, −2.2%) death rates during the flood month.
Snowmelt-related floods and cause-specific death rates
Death rates increased during snowmelt-related flood months for all causes of death except cancer (Fig. 4). Mild floods were associated with the largest death rate increases for respiratory diseases (22.3%; 95% CrI: 19.0%, 25.5%), neuropsychiatric conditions (15.9%; 95% CrI: 12.5%, 19.3%) and cardiovascular diseases (8.9%; 95% CrI: 6.9%, 11.0%), though rates increased for all flood severity levels for these causes of death. Increases in death rates for infectious and parasitic diseases (12.3%; 95% CrI: 6.4%, 18.3%) and injuries (6.1%; 95% CrI: 2.0%, 10.2%) were largest for moderate snowmelt-related floods.
Tropical cyclone-related floods and cause-specific death rates
Tropical cyclone-related floods were associated with increased injury death rates during the flood month for severe (4.7%; 95% CrI:1.8%, 7.6%) and very severe (15.3%; 95% CrI:12.4%, 18.1%) floods (Fig. 4). For very severe floods, injury death rates remained elevated 1 month after tropical cyclone events (3.2%; 95% CrI: 1.5%, 4.9%). Infectious and parasitic disease death rates also increased 1 month after very severe floods (4.8%; 95% CrI: 2.3%, 7.3%), with only a marginally significant association during the actual flood month (3.7%; 95% CrI: −0.9%, 8.4%). The most delayed association was with respiratory disease death rates, which increased 2 months after severe floods (1.8%; 95% CrI: 0.5%, 3.0%). Mild tropical cyclone-related floods, conversely, were associated with decreased death rates for cardiovascular diseases (−2.7%; 95% CrI: −4.3%, −1.1%) and neuropsychiatric conditions (−5.3%; 95% CrI: −7.9%, −2.8%) during the flood month.
Floods and cause-specific death rates by sex
During very severe flood months, increases in tropical cyclone-related injury death rates were higher for females (21.2%; 95% CrI:16.3%, 26.1%) than for males (12.6%; 95% CrI: 9.1%, 16.1%) (Fig. 5). Infectious and parasitic disease death rates increased for males (8.4%; 95% CrI: 4.9%, 11.8%) but not for females (1.2%; 95% CrI: −2.4%, 4.9%) 1 month after heavy rain-related flooding events; this disparity was consistent across all flood causes. Neuropsychiatric death rates decreased for females during months with tropical cyclone-related floods (−3.1%; 95% CrI: −6.3%, 0.0%) but not for males (1.9%; 95% CrI: −2.0%, 5.6%), though credible intervals overlapped.
Floods and cause-specific death rates by age group
Increases in injury death rates during very severe tropical cyclone-related floods months were higher for those aged ≥65 years old (24.9; 95% CrI: 20.0%, 29.8%) than for people <65 years old (10.2%; 95% CrI: 6.6%, 13.8%) (Fig. 6). The positive association of all causes of death except cancer with very severe snowmelt-related flooding was likely driven by increased death rates among adults ≥65 years old, though credible intervals overlapped.
Combined analyses of floods and cause-specific death rates
The analysis of all flood events was largely consistent with heavy rain- and tropical cyclone-related floods analyses, though these associations were attenuated. For snowmelt- and ice jam or dam break-related floods, however, the combined analysis with all flood events masked distinct associations (Extended Data Fig. 3). Compared with analyses by flood cause, there were also slight, delayed associations between very severe floods and cancer mortality 2 (1.0%; 95% CrI: 0.1%, 1.7%) and 3 (1.0%; 95% CrI: 0.2%, 1.8%) months after the event.
Additional deaths per million associated with flood exposure
Cardiovascular disease was the leading cause of additional monthly deaths associated with very severe heavy rain-related (3.65; 95% CrI: 2.06, 5.25 deaths per million (DPM)) and snowmelt-related (8.24; 95% CrI: 4.76, 11.72 DPM) floods during the flood month (Supplementary Table 9). Injuries were the leading cause of additional monthly deaths for very severe tropical cyclone-related floods during the flood month (7.3; 95% CrI: 5.95, 8.65 DPM) and 1 month after the flood event (1.96; 95% CrI: 1.15, 2.78 DPM). Injuries were also the leading cause of additional monthly deaths for very severe ice jam-related floods 1 month after the flood event (1.91; 95% CrI: 1.09, 2.72 DPM).
Discussion
Using nearly two decades of highly resolved flood exposure data, we found that flooding events were associated with increased death rates for cardiovascular diseases, infectious and parasitic diseases, injuries and respiratory diseases, with generally greater associations for more severe floods compared with less severe. Injury death rates were higher for females and older adults associated with acute exposure to tropical cyclone-related flooding, and infectious disease mortality was elevated for males associated with exposure to all flood causes, particularly tropical cyclone- and heavy rain-related floods. Analyses stratified by flood cause identified associations that were attenuated, or for snowmelt-related floods entirely obscured, compared to the all-flood analysis. The value of the stratified analysis is that flood cause categories encompass events with similar characteristics (for example, duration, ___location and extent) that may drive associations with mortality.
We observed higher infectious and parasitic disease death rates 1 month after very severe events for all floods, which suggests that exposure pathways may be similar across flood causes. The delay likely reflects disruptions to drinking water and sewage infrastructure that can lead to waterborne disease transmission27,28. Floodwater can directly contaminate drinking water sources with pathogens, particularly untreated private wells29 or inadequately treated groundwater sources30, and/or inundate drinking water treatment infrastructure leading to backflow contamination or insufficient disinfection31. For example, the largest drinking water treatment plant in Jackson, Mississippi, with a population size of 173,500, was rendered inoperable by heavy rain-related river flooding in 2022 after the city had been under a federal consent decree since 2012 due to consistent failures to maintain operational and maintenance standards32. Flooding can also damage wastewater treatment plants and cause combined sewer overflows, resulting in the direct discharge of untreated sewage into the environment33,34.
Immediate direct contact with contaminated floodwater may be another important exposure pathway, the importance of which varies by flood cause and severity. There is often advance warning for tropical cyclone- or ice jam-related floods that allows people to avoid exposure35,36. Direct contact may be more likely, however, with floods unrelated to these extreme events, including river floods due to heavy precipitation or snowmelt, because they typically do not generate an equivalent emergency response. Supporting evidence is provided by the variability in short-term associations between infectious disease mortality and specific flood causes; increased death rates were observed after very severe heavy rain-related and moderate snowmelt-related floods but not with the more severe tropical cyclone- and ice jam-related events. Heavy rain and snowmelt often cause river floods, which are of particular concern in agricultural regions, as floodwaters can mobilize bacterial and parasitic pathogens in fertilizer or animal slurry37. Direct contact with pathogenic floodwater may be an important waterborne disease transmission pathway during floods and may help explain the variability in infectious disease death rates by flood cause.
Injury mortality associated with very severe floods increased in the month after floods. The lagged association could be driven by people succumbing to injuries sustained during the flood, delaying wound care in the aftermath of a catastrophic flood38 or acquiring injuries during cleanup efforts39. For tropical cyclone-related flooding, however, injury mortality was most strongly associated with acute flood exposure, which is consistent with previous work that found most deaths directly attributable to tropical cyclones were due to storm surges and heavy rain18. Tropical cyclones are multihazard events that are defined by high windspeeds accompanied by heavy precipitation and storm surges. Determining the effect of specific hazards on health outcomes within a multihazard event is a fundamental challenge in disaster epidemiology40, and our study design did not attempt to distinguish specific hazard-related associations. Windspeed and precipitation intensity are not highly correlated after tropical cyclones that make landfall41, however, and are not interchangeable exposure metrics42. Findings here likely reflect the combined associations of tropical cyclone-related hazards with mortality, which is inherent to these events.
Both infectious disease and injury death rates varied by sex and age with different demographic groups at greater risk for distinct flood events. Infectious disease death rate increases after a flood were higher among males compared to females for all flood causes, with the greatest difference after heavy rain-related flood exposure. This finding is consistent with previous work that has found males are overrepresented in fatalities associated with rain-related floods and has been explained by risk-taking behavior in males and greater likelihood of working in emergency services13,43. Males may also be more likely to work on recovery or cleanup efforts, which increases the risk of direct contact with contaminated floodwater and potential infectious disease transmission. Females had higher increases in death rates associated with tropical cyclone-related flood exposure than males, which is also consistent with previous findings44. The dynamics underling this association are not well understood, but qualitative research suggests that the increased risk may be due to child and elder care responsibilities that are disproportionately borne by females45,46. We found that the timing of increased injury mortality differed by age group for very severe tropical cyclone-related floods. Higher mortality was observed for older adults during the flood month before returning to baseline, whereas young people had elevated death rates over the ensuing months. Increased injury death rates for young people in the months after a flood were seen for all flood causes, which further suggests that the cleanup period is a time of heightened risk for very severe floods regardless of the cause and should be a focus of disaster preparedness policies.
Examining associations by flood cause and severity can provide insight into the pathways through which floods may affect the other causes of death (cardiovascular diseases, respiratory diseases and neuropsychiatric conditions) over time. For example, snowmelt often leads to river floods that move slower than storm surges during tropical cyclones but generate persistent standing water, leading to longer flood events24,47. The mechanisms underlying snowmelt-related associations are likely due the duration and size of these events. Even mild floods can lead to prolonged disruptions that cause chronic stress, which can adversely affect short- and long-term health through inflammation, oxidative stress, and mitochondrial dysfunction48, and destabilize healthcare infrastructure49. Mild snowmelt-related floods were associated with the largest increases in mortality for respiratory diseases, neuropsychiatric conditions, and cardiovascular diseases, whereas for all flood causes, mild floods were associated with decreased or unchanged death rates. These causes of death primarily occur among people ≥75 years old, which suggests that age is a crucial risk factor for snowmelt-related mortality. The associations also demonstrate how ___location informs our understanding flood-related health risks; snowmelt-related floods are concentrated in the Upper Midwest, particularly Minnesota and the Dakotas, which has among the highest percentages of adults ≥65 years old in the United States50. The combination of extensive, persistent snowmelt-related floods and a population that is predominantly rural, older, and often more socially isolated makes this region especially vulnerable to flood-related mortality51,52.
Specific flood causes may also engender distinct behavioral responses to floods. The frequency of events varies among flood causes, which could influence individual risk perception, emergency preparedness and mitigation strategies. Comparing cardiovascular disease death rates associated with heavy rain- and tropical cyclone-related floods may elucidate how flood cause affects behavior. Mortality increased with both flood causes 1 and 2 months after flood events, however, only heavy rain-related floods were associated with acute increased cardiovascular disease mortality during the flood month. This difference could be due to lowered risk perception in riverine regions, such as Appalachia and the Midwest, where large heavy rain-related floods are common53. Perceiving floods as low risk, people living in these areas may not move away from or prepare for large heavy rain-related floods and are thus more likely to experience acute cardiovascular strain preparing for or during floods54.
Sociodemographic factors could also drive increased acute cardiovascular disease mortality in areas that experience relatively frequent flooding. An analysis of flood risk behavior in riverine regions found that communities characterized by ‘risk enduring’ behavior—areas less likely to have flood defenses and more reliant on migration during floods—had higher poverty and a lower proportion of white residents compared to those in ‘risk-averse’ communities53. Riverine communities are disproportionately low-income55 and as a result may attract inadequate federal responses, which are typically more robust in highly populated or wealthier areas56,57. Insufficient mitigation policies could compound the risk stemming from individual- or community-level risk perception.
We found that flood exposure was associated with decreased death rates for some causes of death, which could be due to vulnerable people evacuating before a flood. Evacuation may modify health risks associated with floods, but its short- to long-term influence on specific health outcomes is nuanced, and research is hampered by the absence of public health surveillance and mobility data58. Conversely, lower death rates may not reflect a genuine reduction in risk but, rather, result from displaced people dying outside their county of residence. Information on where people evacuate, and the duration of their displacement, is needed to evaluate how mobility affects flood-related mortality.
This study has several limitations. First, misclassification bias could occur if decedents lived outside of their official county of residence during a flood or if their residence within the county did not match their exposure classification. This type of exposure misclassification is likely nondifferential and, therefore, would bias results toward the null59. Second, we cannot account for evacuation or displacement. Flood-driven population movement, however, would likely lead to an underestimation of the associations between flood and cause-specific mortality as the true population during the flood would be smaller than the official county population58. Third, the Global Flood Database (GFD) does not include all floods that occurred during the study period; Moderate Resolution Imaging Spectroradiometer (MODIS) satellite imagery has limitations with resolving urban floods and thus they are underrepresented in the dataset3. As a result, some tropical cyclones that affected the East Coast were not included in the analysis, though cause-specific mortality associated with tropical cyclone exposure has been studied elsewhere and is consistent with these findings6. Fourth, floods often coincide with storms that cause other hazards including high winds and tornadoes, which are not included in the analysis and could affect mortality. Fifth, the spatial unit of analysis was county and counties contain exposure disparities that are not captured by the analysis. Populations within counties are also heterogeneous, and the ability to mitigate health effects related to flooding varies by demographic and socioeconomic factors60. Future work may be able to study associations by smaller areal units as appropriate demographic and outcome data become available. Sixth, short-term changes are summarized into monthly associations due to the temporal resolution of the mortality data. Our objective was to examine the association of large, persistent floods on mortality over multiple months, and as such, the monthly resolution is appropriate for the analysis. Nevertheless, this analysis does not address immediate (that is, days after flood) associations; further work evaluating the short-term effect of persistent floods on daily and weekly mortality is necessary and would complement this analysis. Seventh, the difference between the geographic range for tropical cyclone-related flooding and the other flood causes introduces the potential for spatial effect modification, though our stratified model approach allows flexibility in model parameter estimation to account for this.
Our analysis finds that the association of flooding with mortality was comparable to impactful climate-related disasters such as hurricanes and other tropical cyclones and varied by cause of death, sex, age group, flood cause and severity. These observations address the gap in our understanding of post-flood changes in cause-specific mortality. Preparing for flood-related health effects is a systemic public policy challenge made urgent by population growth in flood-prone regions and the intensification of flooding due to climate change3,4,5. Sea-level rise, rapid snowpack melt and more powerful cyclonic storms will increase flood severity1, but flooding unrelated to hurricanes may be less likely to trigger an adequate disaster management response. Effective and equitable preparation and response to flooding risk in the United States is necessary to mitigate risks to public health.
Methods
This study was reviewed and approved by the Columbia University Institutional Review Board and was classified non-human subjects research, though not exempt from an ethics review (protocol IRB-AAAT9710).
Flood exposure data
We obtained data on flood exposure in the continental United States from the GFD that provides satellite-derived flood maps from 2001–20183. The GFD was developed using the Dartmouth Flood Observatory (DFO), a geospatial event catalog of large floods from 1985 to present61, to identify the ___location and timing of global flood events using satellite data61. The DFO defines large floods as those that generate media coverage, which typically include floods that cause structural damage, harm crops, and/or cause fatalities. Satellite imagery from MODIS, operated by NASA and available since 2000, was acquired for dates and watersheds identified as a flood event in the DFO catalog3. MODIS is frequently used to map inundation62,63,64 and provides two satellite images per day with global coverage. We analyzed every MODIS image over the relevant watershed for each day in the event date range reported by the DFO. To determine flooded areas from MODIS imagery, surface reflectance values in the visible, near-infrared, and short-wave infrared wavelengths were selected and harmonized at a spatial resolution of 250-meters3. A flood detection algorithm relying on the reflectance values from these bands used a threshold approach to classify each pixel as water or not water in every MODIS image over the relevant watershed and dates reported in the DFO catalog. Specifically, reflectance values from the near-infrared, red, and short-wave-infrared bands were compared to fixed threshold reflectance values that were empirically determined from United States Geological Survey river gauge discharge data62. To reduce the possibility of false detections primarily arising from cloud shadows, a landscape feature similar to surface water, daily flood footprints were composited over 3 days to ensure that pixel-level classifications (water or not water) were consistent over multiple days. Inundated pixels were defined as those where surface water was identified outside of permanent water bodies as defined by the Global Surface Water dataset65.
In this study, we calculated flood exposure for each county by intersecting the GFD flood event maps with gridded population estimates from the Global Human Settlement Layer (GHSL) available for 2000 and 2015 at 250-m resolution66,67. For floods occurring in years without available gridded population data from GHSL, we used the closest year of available GHSL data to estimate the percentage of the exposed population3. We categorized flood causes as events resulting from heavy rain, tropical cyclone, snowmelt or ice jam or dam break floods, consistent with the DFO classification (Supplementary Table 4). Because our objective was to evaluate the association between flood exposure and mortality, we restricted our analysis to counties that experienced at least one flood event during the study period.
Flood severity
For each flood event in the GFD, counties that experienced no flooding were defined as unexposed; among counties that experienced any flooding, we determined the severity of the flood exposure. Flood severity has no universal definition68, and multiple factors can be used to define flood severity. We used the proportion of the population affected by a flood event to define flood severity, because this approach standardizes severity estimates across diverse flood causes and geographic regions. For each county and flood (‘county-flood’) event, the GFD included the population in the inundated pixels and the total county population based on estimates from the GHSL69. With this pixel-level flood and population data, we calculated the proportion of the county population residing in flooded areas for each county-flood event during 2001–2018. We generated a population exposure distribution using these values for all flood events collectively and for separate flood causes (Supplementary Table 5). For each county-flood event, we compared the percent of the population exposed to the all-flood and flood cause-specific distributions to define exposure severity (Supplementary Table 6). Mild floods were defined as those with population exposure in <25th percentile, moderate floods were defined as those with population exposure in ≥25th and <50th percentile, severe floods were defined as those with population exposure in ≥50th percentile and <75th percentile and very severe floods were defined as those with population exposure in ≥75th percentile.
For each flood cause, we found the median and median maximal flood duration (Supplementary Table 7); here, the median maximal duration in a county is defined as the median of the pixels with the longest flood duration across all flood cause-specific events. We assessed median and median maximal duration by geographic region (Extended Data Figs. 4 and 5).
Temperature data
We obtained temperature data from the Parameter-elevation Regressions on Independent Slopes Model (PRISM), which collects climate observations from a range of monitoring networks70. The model uses quality control measures to generate a national temperature dataset with full space and time coverage during the study period. We used gridded daily estimates at 4-km resolution to generate area-weighted monthly average temperatures by county. Previous work comparing gridded climate datasets has found that the validity of PRISM data are equivalent to71 or outperform72 alternatives and are well suited for studies that involve complex and variable terrain73, such as throughout the continental United States.
Outcomes
We used complete national death records from the National Center for Health Statistics (NCHS) to identify monthly total and cause-specific deaths by age group, sex and county in the United States (2001–2018). To calculate monthly death rates by county, we linearly interpolated county-, sex- and age group-specific annual population counts from the NCHS bridged-race dataset (https://www.cdc.gov/nchs/nvss/bridged_race.htm)6.
Cause-specific mortality outcomes
We coded the underlying causes of death according to the International Classification of Diseases (ICD) system (10th revision), and World Health Organization Global Health Estimate cause categories74. We grouped the death records into six primary causes of death—cancers, cardiovascular disease, infectious and parasitic diseases, injuries, neuropsychiatric conditions and respiratory diseases—that comprise 86.2% of all deaths in included counties during the study period (Supplementary Table 8).
Statistical methods
We used a Bayesian formulation of the conditional quasi-Poisson model to analyze the county-level association between the number of flood events per month and monthly death rates, building on previous analyses6,75, that accounted for overdispersion in the mortality data. The conditional approach examines differences within matched strata (here, county-months) like a case-crossover study design, which removes confounding bias due to factors that vary across strata76. Bayesian inference enables the ‘borrowing of information’ across county units and for the full distributional estimation of the parameters of interest77.
The percentage change in death rates associated with flood exposure is modeled as:
where deathsct is the number of all-cause or cause-specific deaths in county c and month-year time t (ranging from 1 to 216, the total number of months in the study period); α0 is the overall intercept and \({\alpha }_{{cm}(t)}\) is the county-month specific intercept, which is not estimated in the conditional Poisson model, where m(t) is a function that extracts the calendar month for time t; βl is the lag-specific coefficient (log rate ratio) for flood exposure in lagged month l; Exposurelct is the count of flood events in lagged month l, county c, at time t; ns(t) is a natural spline term with 3 degrees of freedom per year to account for seasonality and long-term trends; \({\tau }_{{{\rm{temp}}}_{{ct}}}\) is a second-order random walk term to flexibly model the temperature-mortality relationship where tempct is the area-weighted monthly average temperature in county c and time t; and \({\rm{Population}}_{{ct}}\) is the population in county c and time t, included as a population offset.
As in previous related work6,78, we used weakly informative priors for parameter estimation. For the county-month intercepts αc and the second-order random walk term τ, hyper-priors were defined on the logarithm of the precision (1/σ2) and modeled as logGamma(θ, δ) distributions with shape θ = 1 and rate δ = 0.001. All of the other terms, including the βl parameters, were modeled with Gaussian priors N(0, 1000).
All-cause and cause-specific mortality associated with flood events is likely differential by flood cause and severity; therefore, we conducted analyses separately by all-cause and cause-specific mortality (cancers, cardiovascular diseases, infectious and parasitic diseases, injuries, neuropsychiatric conditions, and respiratory diseases), flood cause (all floods, heavy rain, tropical cyclone, snowmelt, and ice jam or dam break), and flood severity (mild, moderate, severe, and very severe). Because very severe flood events were most strongly associated with increased mortality across all flood causes and mortality groups, we further analyzed associations stratified by age group (0–64 years and ≥65 years) and sex (female and male) for very severe floods only. We presented results as percent changes in death rates per unit increase in flood events in a month. As a supplementary analysis, we calculated deaths per million due to flood exposure for each flood and cause of death for each lag period (0–3 months). Monthly deaths per million was calculated by multiplying effect estimates by monthly 2018 age-standardized death rates. We used the R-INLA (version 23.9.9) and splines (version 4.3.1) packages to conduct the statistical analyses in R (version 3.6.3).
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The Global Flood Database (GFD) flood event data and Global Human Settlement Layer (GHSL) population data can be downloaded from https://global-flood-database.cloudtostreet.ai/. Data for individual floods are available with no restrictions. Cause-specific mortality data with geographic information can be requested through the National Center for Health Statistics (NCHS) at https://www.cdc.gov/nchs/nvss/nvss-restricted-data.htm. Applicants must submit a project review form (https://www.cdc.gov/nchs/data/nvss/nchs-research-review-application.pdf) to [email protected] and allow four to six weeks for processing. Parameter-elevation Regression on Independent Slopes Model (PRISM) temperature data can be downloaded from https://prism.oregonstate.edu/recent/ with no restrictions.
Code availability
The R code for the statistical analysis is available on the SPARK Lab GitHub repo at https://github.com/sparklabnyc/usa_floods_mortality_2024.
References
IPCC. Summary for policymakers. In Climate Change 2023: Synthesis Report Contribution of Working Groups I (2023); https://doi.org/10.59327/IPCC/AR6-9789291691647.001
Paterson, D. L., Wright, H. & Harris, P. N. A. Health risks of flood disasters. Clin. Infect. Dis. 67, 1450–1454 (2018).
Tellman, B. et al. Satellite imaging reveals increased proportion of population exposed to floods. Nature 596, 80–86 (2021).
Rentschler, J. et al. Global evidence of rapid urban growth in flood zones since 1985. Nature 622, 87–92 (2023).
Wing, O. E. J. et al. Inequitable patterns of US flood risk in the Anthropocene. Nat. Clim. Change 12, 156–162 (2022).
Parks, R. M. et al. Association of tropical cyclones with county-level mortality in the US. JAMA 327, 946–955 (2022).
Yan, M. et al. Community-wide mortality rates in Beijing, China, during the July 2012 flood compared with unexposed periods. Epidemiology 31, 319–326 (2020).
Quist, A. J. et al. Hurricane flooding and acute gastrointestinal illness in North Carolina. Sci. Total Environ. 809, 151108 (2022).
Makwana, N. Disaster and its impact on mental health: a narrative review. J. Fam. Med. Prim. Care 8, 3090 (2019).
Ebi, K. L. et al. Extreme weather and climate change: population health and health system implications. Annu. Rev. public health 42, 293–315 (2021).
Saulnier, D. D., Ribacke, K. B. & von Schreeb, J. No calm after the storm: a systematic review of human health following flood and storm disasters. Prehosp. Disaster Med. 32, 568–579 (2017).
Ban, J., Sutton, C., Ma, Y., Lin, C. & Chen, K. Association of flooding exposure with cause-specific mortality in North Carolina, United States. Nat. Water 1, 1027–1034 (2023).
Jonkman, S. N. & Kelman, I. An analysis of the causes and circumstances of flood disaster deaths. Disasters 29, 75–97 (2005).
Doocy, S., Daniels, A., Murray, S. & Kirsch, T. D. The human impact of floods: a historical review of events 1980-2009 and systematic literature review. PLoS Curr. 5, ecurrents.dis.f4deb457904936b07c09daa98ee8171a (2013).
Canadell, J. G. et al. Global carbon and other biogeochemical cycles and feedbacks [Supplementary Material]. In Climate Change 2021: The Physical Science Basis. Contribution of Working Group I to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change (2021).
Najibi, N. & Devineni, N. Recent trends in the frequency and duration of global floods. Earth Syst. Dynam. 9, 757–783 (2018).
Du, W., FitzGerald, G. J., Clark, M. & Hou, X.-Y. Health impacts of floods. Prehosp. disaster Med. 25, 265–272 (2010).
Rappaport, E. N. Fatalities in the United States from Atlantic tropical cyclones: new data and interpretation. Bull. Am. Meteorol. Soc. 95, 341–346 (2014).
Alderman, K., Turner, L. R. & Tong, S. Floods and human health: a systematic review. Environ. Int. 47, 37–47 (2012).
Levy, K., Woster, A. P., Goldstein, R. S. & Carlton, E. J. Untangling the impacts of climate change on waterborne diseases: a systematic review of relationships between diarrheal diseases and temperature, rainfall, flooding, and drought. Environ. Sci. Technol. 50, 4905–4922 (2016).
Mendell, M. J., Mirer, A. G., Cheung, K., Tong, M. & Douwes, J. Respiratory and allergic health effects of dampness, mold, and dampness-related agents: a review of the epidemiologic evidence. Environ. Health Perspect. 119, 748–756 (2011).
Carroll, B., Balogh, R., Morbey, H. & Araoz, G. Health and social impacts of a flood disaster: responding to needs and implications for practice. Disasters 34, 1045–1063 (2010).
Milojevic, A. et al. Long-term effects of flooding on mortality in England and Wales, 1994-2005: controlled interrupted time-series analysis. Environ. Health 10, 11 (2011).
Michaud, J. D., Hirschboeck, K. K. & Winchell, M. Regional variations in small-basin floods in the United States. Water Resour. Res. 37, 1405–1416 (2001).
Gaál, L. et al. Flood timescales: understanding the interplay of climate and catchment processes through comparative hydrology. Water Resour. Res. 48, 4 (2012).
National Hurricane Center. Tropical Cyclone Climatology. https://www.nhc.noaa.gov/climo/
Craun, G. F. et al. Causes of outbreaks associated with drinking water in the United States from 1971 to 2006. Clin. Microbiol. Rev. 23, 507–528 (2010).
De Man, H. et al. Quantitative assessment of infection risk from exposure to waterborne pathogens in urban floodwater. Water Res. 48, 90–99 (2014).
Allaire, M., Wu, H. & Lall, U. National trends in drinking water quality violations. Proc. Natl Acad. Sci. USA 115, 2078–2083 (2018).
Andrade, L., O’Dwyer, J., O’Neill, E. & Hynds, P. Surface water flooding, groundwater contamination, and enteric disease in developed countries: a scoping review of connections and consequences. Environ. Pollut. 236, 540–549 (2018).
FEMA. Fact Sheet 4.1: Drinking Water Systems (2022).
Kim, M. et al. Boil water alerts and their impact on the unexcused absence rate in public schools in Jackson, Mississippi. Nat. Water 1, 359–369 (2023).
Su, X., Liu, T., Beheshti, M. & Prigiobbe, V. Relationship between infiltration, sewer rehabilitation, and groundwater flooding in coastal urban areas. Environ. Sci. Pollut. Res. 27, 14288–14298 (2020).
Gibson, C. J. III, Stadterman, K. L., States, S. & Sykora, J. Combined sewer overflows: a source of Cryptosporidium and Giardia? Water Sci. Technol. 38, 67–72 (1998).
Thompson, R. R., Garfin, D. R. & Silver, R. C. Evacuation from natural disasters: a systematic review of the literature. Risk Anal. 37, 812–839 (2017).
Liu, M. et al. Hazard assessment and prediction of ice-jam flooding for a river regulated by reservoirs using an integrated probabilistic modelling approach. J. Hydrol. 615, 128611 (2022).
Nicholson, F. A., Groves, S. J. & Chambers, B. J. Pathogen survival during livestock manure storage and following land application. Bioresour. Technol. 96, 135–143 (2005).
Sheppa, C. M., Stevens, J., Philbrick, J. T. & Canada, M. The effect of a class IV hurricane on emergency department operations. Am. J. Emerg. Med. 11, 464–467 (1993).
Waddell, S. L. et al. Perspectives on the health effects of hurricanes: a review and challenges. Int. J. Environ. Res. Public Health 18, 2756 (2021).
Leonard, M. et al. A compound event framework for understanding extreme impacts. Wiley Interdiscip. Rev. Clim. Change 5, 113–128 (2014).
Xi, D., Wang, S. & Lin, N. Analyzing relationships between tropical cyclone intensity and rain rate over the ocean using numerical simulations. J. Clim. 36, 81–91 (2023).
Lynch, V. D. & Shaman, J. Waterborne infectious diseases associated with exposure to tropical cyclonic storms, United States, 1996–2018. Emerg. Infect. Dis. 29, 1548 (2023).
Lowe, D., Ebi, K. L. & Forsberg, B. Factors increasing vulnerability to health effects before, during and after floods. Int. J. Environ. Res. Public Health 10, 7015–7067 (2013).
Chowdhury, A. M. R., Bhuyia, A. U., Choudhury, A. Y. & Sen, R. The Bangladesh cyclone of 1991: why so many people died. Disasters 17, 291–304 (1993).
Tapsell, S. M., Penning-Rowsell, E. C., Tunstall, S. M. & Wilson, T. L. Vulnerability to flooding: health and social dimensions. Philos. Trans. A Math. Phys. Eng. Sci. 360, 1511–1525 (2002).
Tunstall, S., Tapsell, S., Green, C., Floyd, P. & George, C. The health effects of flooding: social research results from England and Wales. J. Water Health 4, 365–380 (2006).
Brunner, M. I. & Fischer, S. Snow-influenced floods are more strongly connected in space than purely rainfall-driven floods. Environ. Res. Lett. 17, 104038 (2022).
Prada, D. et al. Climate change and health: understanding mechanisms will inform mitigation and prevention strategies. Nat. Med. 30, 1522–1524 (2024).
Yu, D. et al. Disruption of emergency response to vulnerable populations during floods. Nat. Sustainability 3, 728–736 (2020).
Caplan, Z. & Rabe, M. The Older Population: 2020 (U.S. Department of Commerce, U.S. Census Bureau, 2023).
Barnes, T. L. et al. Loneliness, Social Isolation, and All-Cause Mortality in a Large Sample of Older Adults. J. Aging Health 34, 883–892 (2022).
Cudjoe, T. K. M., Prichett, L., Szanton, S. L., Roberts Lavigne, L. C. & Thorpe, R. J. Jr Social isolation, homebound status, and race among older adults: findings from the National Health and Aging Trends Study (2011–2019). J. Am. Geriatr. Soc. 70, 2093–2100 (2022).
Knighton, J., Hondula, K., Sharkus, C., Guzman, C. & Elliott, R. Flood risk behaviors of United States riverine metropolitan areas are driven by local hydrology and shaped by race. Proc. Natl Acad. Sci. USA. 118, e2016839118 (2021).
Duclos, P. & Isaacson, J. Preventable deaths related to floods. Am. J. Public health 77, 1474 (1987).
Qiang, Y. Disparities of population exposed to flood hazards in the United States. J. Environ. Manag. 232, 295–304 (2019).
Loughran, K. & Elliott, J. R. Residential buyouts as environmental mobility: examining where homeowners move to illuminate social inequities in climate adaptation. Popul. Environ. 41, 52–70 (2019).
Weber, A. & Moore, R. Going Under: Long Wait Times for Post-Flood Buyouts Leave Homeowners Underwater (National Resources Defense Council, 2019).
Centers for Disease Control and Prevention. A Primer for Understanding the Principles and Practices of Disaster Surveillance in the United States: First Edition (Centers for Disease Control and Prevention, 2016).
Carroll, R. J. Measurement Error in Nonlinear Models: A Modern Perspective. Second Edition (Chapman and Hall/CRC, 2006).
Brunkard, J., Namulanda, G. & Ratard, R. Hurricane Katrina Deaths, Louisiana, 2005. Disaster Med. Public Health Prep. 2, 215–223 (2008).
Brakenridge, G. R. Global Active Archive of Large Flood Events (DFO - Flood Observatory, University of Colorado, USA); http://floodobservatory.colorado.edu/Archives/
Brakenridge, R. & Anderson, E. MODIS-based flood detection, mapping and measurement: the potential for operational hydrological applications. In Transboundary Floods: Reducing Risks through Flood Management 1–12 (Springer, 2006).
Boschetti, M., Nutini, F., Manfron, G., Brivio, P. A. & Nelson, A. Comparative analysis of normalised difference spectral indices derived from MODIS for detecting surface water in flooded rice cropping systems. PloS One 9, e88741 (2014).
Klein, I., Dietz, A., Gessner, U., Dech, S. & Kuenzer, C. Results of the Global WaterPack: a novel product to assess inland water body dynamics on a daily basis. Remote Sens. Lett. 6, 78–87 (2015).
Pekel, J.-F., Cottam, A., Gorelick, N. & Belward, A. S. High-resolution mapping of global surface water and its long-term changes. Nature 540, 418–422 (2016).
Freire, S., MacManus, K., Pesaresi, M., Doxsey-Whitfield, E. & Mills, J. Development of new open and free multi-temporal global population grids at 250 m resolution. Population 250, (2016).
Schiavina, M., Freire, S., Carioli, A. & MacManus, K. GHS-POP R2023A–GHS Population Grid Multitemporal (1975–2030) (Joint Research Centre, 2023).
NOAA National Weather Service. Floods: The Awesome Power (NOAA, 2005).
European Commission, Joint Research Center. GHS-POP R2015A - GHS population grid, derived from GPW4, multitemporal (1975, 1990, 2000, 2015) - OBSOLETE RELEASE (JRC, 2015).
Daly, C., Smith, J. I. & Olson, K. V. Mapping atmospheric moisture climatologies across the conterminous United States. PLoS One 10, e0141140 (2015).
Durre, I., Arguez, A., Schreck, C. J. III, Squires, M. F. & Vose, R. S. Daily high-resolution temperature and precipitation fields for the contiguous United States from 1951 to present. J. Atmos. Ocean. Technol. 39, 1837–1855 (2022).
Spangler, K. R., Weinberger, K. R. & Wellenius, G. A. Suitability of gridded climate datasets for use in environmental epidemiology. J. Expo. Sci. Environ. Epidemiol. 29, 777–789 (2019).
Daly, C. PRISM High-Resolution Spatial Cilmate Data for the United States: Max/Min Temp, Dewpoint, Precipitaiton (NSF/NCAR, 2023); https://climatedataguide.ucar.edu/climate-data/prism-high-resolution-spatial-climate-data-united-states-maxmin-temp-dewpoint
Boerma, T. & Mathers, C. D. The World Health Organization and global health estimates: improving collaboration and capacity. BMC Med. 13, 50 (2015).
Parks, R. M. et al. Tropical cyclone exposure is associated with increased hospitalization rates in older adults. Nat. Commun. 12, 1545 (2021).
Armstrong, B. G., Gasparrini, A. & Tobias, A. Conditional Poisson models: a flexible alternative to conditional logistic case cross-over analysis. BMC Med. Res. Methodol. 14, 122 (2014).
Gelman, A., Carlin, J. B., Stern, H. S. & Rubin, D. B. Bayesian Data Analysis (Chapman and Hall/CRC, 1995).
Kontis, V. et al. Magnitude, demographics and dynamics of the effect of the first wave of the COVID-19 pandemic on all-cause mortality in 21 industrialized countries. Nat. Med. 26, 1919–1928 (2020).
Acknowledgments
V.D.L. is supported by National Institute of Environmental Health Sciences (NIEHS) grant T32 ES007322. V.D.L. and R.M.P. are supported by NIEHS grant R00 ES033742. V.D.L., R.M.P., M-A.K. and A.E.N. are supported by NIEHS grant P30 ES009089. R.M.P. and M-A.K. are supported by NIEHS grant P20 AG093975. S.A. is supported by NIEHS Training grant T32 ES007142.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study design or interpretation of results. V.D.L. and R.M.P. organized mortality files. V.D.L. organized the flood data from the dataset provided by J.A.S. R.M.P. and V.D.L. developed the statistical model, which was implemented by V.D.L. V.D.L. performed the analysis with input from R.M.P., J.A.S., A.B.F., A.N. and M-A.K. V.D.L. and R.M.P. wrote the first draft of the paper; all authors contributed to revising and finalizing the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Medicine thanks the anonymous reviewers for their contribution to the peer review of this work. Primary Handling Editor: Ming Yang, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Age-standardized death rates during 2001–2018.
Age-standardized death rates per 100,000 by month and year for each cause of death and by sex during 2001–2018.
Extended Data Fig. 2 Count of flood events by month and flood cause during 2001–2018.
Number of flood events by flood cause (heavy rain, tropical cyclone, snowmelt, and ice jam or dam break) and month during 2001–2018.
Extended Data Fig. 3 Percentage change in death rates.
Percentage change in death rates per flood event by cause of death, flood severity, and lag time. Lag time is measured in months after flood. Dots show point estimates and error bars represent 95% credible intervals.
Extended Data Fig. 4 Median flood duration in days.
Median flood duration in days by county and flood cause during 2001–2018. Panel A: heavy rain flood events (n = 61); Panel B: tropical cyclone flood events (n = 18); Panel C: snowmelt flood events (n = 9); Panel D: ice jam or dam break flood events (n = 5).
Extended Data Fig. 5 Median maximum flood duration in days.
Median maximum flood duration in days by county and flood cause during 2001–2018. Panel A: heavy rain flood events (n = 61); Panel B: tropical cyclone flood events (n = 18); Panel C: snowmelt flood events (n = 9); Panel D: ice jam/dam break flood events (n = 5).
Supplementary information
Supplementary Information
Supplementary Tables 1–9.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lynch, V.D., Sullivan, J.A., Flores, A.B. et al. Large floods drive changes in cause-specific mortality in the United States. Nat Med 31, 663–671 (2025). https://doi.org/10.1038/s41591-024-03358-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-024-03358-z