Abstract
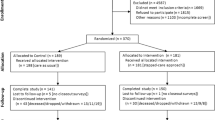
The COmmunicating Narrative Concerns Entered by RNs (CONCERN) early warning system (EWS) uses real-time nursing surveillance documentation patterns in its machine learning algorithm to identify deterioration risk. We conducted a 1-year, multisite, pragmatic trial with cluster-randomization of 74 clinical units (37 intervention; 37 usual care) across 2 health systems. Eligible adult hospital encounters were included. We tested if outcomes differed between patients whose care teams were and patients whose care teams were not informed by the CONCERN EWS. Coprimary outcomes were in-hospital mortality (examined as instantaneous risk) and length of stay. Secondary outcomes were cardiopulmonary arrest, sepsis, unanticipated intensive care unit transfers and 30-day hospital readmission. Among 60,893 hospital encounters (33,024 intervention; 27,869 usual care), intervention group encounters had 35.6% decreased instantaneous risk of death (adjusted hazard ratio (HR), 0.64; 95% confidence interval (CI), 0.53–0.78; P < 0.0001), 11.2% decreased length of stay (adjusted incidence rate ratio, 0.91; 95% CI, 0.90–0.93; P < 0.0001), 7.5% decreased instantaneous risk of sepsis (adjusted HR, 0.93; 95% CI, 0.86–0.99; P = 0.0317) and 24.9% increased instantaneous risk of unanticipated intensive care unit transfer (adjusted HR, 1.25; 95% CI, 1.09–1.43; P = 0.0011) compared with usual-care group encounters. No adverse events were reported. A machine learning-based EWS, modeled on nursing surveillance patterns, decreased inpatient deterioration risk with statistical significance. ClinicalTrials.gov registration: NCT03911687.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
27,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
209,00 € per year
only 17,42 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
We will make our de-identified outcomes data publicly available within 6 months of publication with no anticipated end date. This will include data dictionaries, study protocol, statistical analysis plan and de-identified individual shift-level and encounter-level data for our primary and secondary outcomes. We will make the data available under the Creative Commons Attribution 4.0 International License on a public repository, such as PhysioNet, that provides functionality for users to register, agree to terms of use and provide evidence of human subjects research training before downloading. Users will be able to access the data upon agreeing to the Creative Commons Attribution 4.0 International License and the public repository terms of use. Access will be granted according to the time frame for processing requests provided by the public repository. Our study website (www.concernearlywarningscore.org) will provide study team contact information and a link to the public repository to support findability. Prior to our data being uploaded on a public repository please contact the corresponding author for data requests. The CONCERN study team can also be contacted directly at [email protected]. The conditions and purposes for sharing include that requesting individuals provide proof of a training program in human research subject protections and HIPAA regulations, not being from a for-profit organization and agreeing to criteria consistent with the PhysioNet Credentialed Health Data Use Agreement 1.5.0. The CONCERN study team will process data requests within 1 month of receipt of a data sharing request that meets the above stated criteria. The CONCERN EWS algorithm is considered intellectual property that will not be shared but is described in our online supplement.
Code availability
We will share our SAS statistical analysis code, along with our data as mentioned above, within 6 months of publication on a public repository such as PhysioNet that provides functionality for users to register, agree to terms of use and provide evidence of human subjects research training before downloading. Prior to our code being uploaded on a public repository please contact the corresponding author for data requests. The conditions and purposes for sharing include that requesting individuals provide proof of a training program in human research subject protections and HIPAA regulations, not being from a for-profit organization and agreeing to criteria consistent with the PhysioNet Credentialed Health Data Use Agreement 1.5.0. The CONCERN study team will process code requests within 1 month of receipt of a code request that meets the above stated criteria.
References
American Hospital Association. Report: Rising patient acuity driving up hospital costs as payments fall. AHA News https://www.aha.org/news/headline/2022-08-15-report-rising-patient-acuity-driving-hospital-costs-payments-fall (2022).
Hogan, H. et al. Preventable deaths due to problems in care in English acute hospitals: a retrospective case record review study. BMJ Qual. Saf. 21, 737–745 (2012).
Patient safety. The Joint Commission www.jointcommission.org/facts_about_patient_safety/ (2015).
Wan, Y.-K. J. et al. Information displays for automated surveillance algorithms of in-hospital patient deterioration: a scoping review. J. Am. Med. Inform. Assoc. 31, 256–273 (2023).
Schmidt, P. E. et al. Impact of introducing an electronic physiological surveillance system on hospital mortality. BMJ Qual.Saf. 24, 176–177 (2015).
Lee, T. C., Shah, N. U., Haack, A. & Baxter, S. L. Clinical implementation of predictive models embedded within electronic health record systems: a systematic review. Informatics (MDPI) 7, 25 (2020).
Bates, D. W., Saria, S., Ohno-Machado, L., Shah, A. & Escobar, G. Big data in health care: using analytics to identify and manage high-risk and high-cost patients. Health Aff. (Millwood) 33, 1123–1131 (2014).
Fu, L. et al. Development and validation of early warning score system: a systematic literature review. J. Biomed. Inform. 105, 103410 (2020).
Drew, B. J. et al. Insights into the problem of alarm fatigue with physiologic monitor devices: a comprehensive observational study of consecutive intensive care unit patients. PLoS ONE 9, e110274 (2014).
Rossetti, S. et al. Healthcare process modeling to phenotype clinician behaviors for exploiting the signal gain of clinical expertise (HPM–ExpertSignals): development and evaluation of a conceptual framework. J. Am. Med. Inform. Assoc. 28, 1242–1251 (2021).
Halverson, C. C. & Scott Tilley, D. Nursing surveillance: a concept analysis. Nurs. Forum 57, 454–460 (2022).
Collins, S. A., Fred, M. R., Wilcox, L. & Vawdrey, D. K. Workarounds used by nurses to overcome design constraints of electronic health records. NI 2012 2012, 93–97 (2012).
Collins, S. A. et al. Relationship between nursing documentation and mortality. Am. J. Crit. Care. 22, 306–313 (2013).
Endsley, M. R. Toward a theory of situation awareness in Dynamic Systems. Hum. Factors J. Hum. Factors Ergon. Soc. 37, 32–64 (1995).
Tokareva, I. & Romano, P. Failure to rescue. PSNet https://psnet.ahrq.gov/primer/failure-rescue (2025).
Odell, M., Victor, C. & Oliver, D. Nurses’ role in detecting deterioration in ward patients: systematic literature review. J. Adv. Nurs. 65, 1992–2006 (2009).
Burns, P. B., Rohrich, R. J. & Chung, K. C. The levels of evidence and their role in evidence-based medicine. Plast. Reconstr. Surg. 128, 305–310 (2011).
Agency for Healthcare Research and Quality. Rapid Response Systems https://psnet.ahrq.gov/primer/rapid-response-systems (2019).
Cioffi, J. Recognition of patients who require emergency assistance: a descriptive study. Heart Lung 29, 262–268 (2000).
Jones, L., King, L. & Wilson, C. A literature review: factors that impact on nurses’ effective use of the Medical Emergency Team (MET). J. Clin. Nurs. 18, 3379–3390 (2009).
Collins, S. A. & Vawdrey, D. K. “Reading between the lines” of flowsheet data: nurses’ optional documentation associated with cardiac arrest outcomes. Appl. Nurs. Res. 25, 251–257 (2012).
Opitz, D. & Maclin, R. Popular ensemble methods: an empirical study. J. Artif. Intell. Res. 11, 169–198 (1999).
Hobensack, M. et al. Identifying barriers to the implementation of Communicating Narrative Concerns Entered by Registered Nurses (CONCERN), an early warning system smartapp. Appl Clin Inform 15, 295–305 (2024).
Singh, K. et al. Evaluating a widely implemented proprietary deterioration index model among hospitalized patients with COVID-19. Ann. Am. Thorac. Soc. 18, 1129–1137 (2021).
Sashegyi, A. & Ferry, D. On the interpretation of the hazard ratio and communication of survival benefit. Oncologist 22, 484–486 (2017).
Adams, R. et al. Prospective, multi-site study of patient outcomes after implementation of the TREWS machine learning-based early warning system for sepsis. Nat. Med. 28, 1455–1460 (2022).
Escobar, G. J. et al. Automated identification of adults at risk for in-hospital clinical deterioration. N. Engl. J. Med. 383, 1951–1960 (2020).
Levin, M. A. et al. Real-time machine learning alerts to prevent escalation of care: a nonrandomized clustered pragmatic clinical trial. Crit. Care Med. 52, 1007–1020 (2024).
Churpek, M. M. et al. Multicenter comparison of machine learning methods and conventional regression for predicting clinical deterioration on the wards. Crit. Care Med. 44, 368–374 (2016).
Plana, D. et al. Randomized clinical trials of machine learning interventions in health care: a systematic review. JAMA Netw. Open 5, e2233946 (2022).
Moher, D. et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. Brit. Med. J. 340, c869 (2010).
Liu, X., Cruz Rivera, S., Moher, D., Calvert, M. J. & Denniston, A. K. on behalf of SPIRIT-AI and CONSORT-AI Working Group. Reporting guidelines for clinical trial reports for interventions involving artificial intelligence: the CONSORT-AI extension. Lancet Digit. Health 2, e537–e548 (2020).
Campbell, M. K., Piaggio, G., Elbourne, D. R. & Altman, D. G. CONSORT Group. Consort 2010 statement: extension to cluster randomised trials. Brit. Med. J. 345, e5661 (2012).
Zwarenstein, M. et al. Improving the reporting of pragmatic trials: an extension of the CONSORT statement. Brit. Med. J. 337, a2390 (2008).
Kiekkas, P. et al. Delayed admission to the intensive care unit and mortality of critically ill adults: systematic review and meta-analysis. Biomed. Res. Int. 2022, 4083494 (2022).
Churpek, M. M. et al. Association between intensive care unit transfer delay and hospital mortality: A multicenter investigation. J. Hosp. Med. 11, 757–762 (2016).
Solomon, R. S., Corwin, G. S., Barclay, D. C., Quddusi, S. F. & Dannenberg, M. D. Effectiveness of rapid response teams on rates of in-hospital cardiopulmonary arrest and mortality: A systematic review and meta-analysis. J. Hosp. Med. 11, 438–445 (2016).
Hu, W., Chan, C. W., Zubizarreta, J. R. & Escobar, G. J. An examination of early transfers to the ICU based on a physiologic risk score. Manuf. Serv. Oper. Manag. 20, 531–549 (2018).
Grieve, R. et al. Analysis of benefit of intensive care unit transfer for deteriorating ward patients: a patient-centered approach to clinical evaluation. JAMA Netw. Open 2, e187704 (2019).
Hripcsak, G. & Albers, D. J. Next-generation phenotyping of electronic health records. J. Am. Med. Inform. Assoc. 20, 117–121 (2013).
Albers, D. J. & Hripcsak, G. Using time-delayed mutual information to discover and interpret temporal correlation structure in complex populations. Chaos 22, 13111 (2012).
Albers, D. J. & Hripcsak, G. A statistical dynamics approach to the study of human health data: resolving population scale diurnal variation in laboratory data. Phys. Lett. A 374, 1159–1164 (2010).
Pivovarov, R., Albers, D. J., Hripcsak, G., Sepulveda, J. L. & Elhadad, N. Temporal trends of hemoglobin A1c testing. J. Am. Med. Inform. Assoc. 21, 1038–1044 (2014).
Pivovarov, R., Albers, D. J., Sepulveda, J. L. & Elhadad, N. Identifying and mitigating biases in EHR laboratory tests. J. Biomed. Inform. 51, 24–34 (2014).
Schwartz, J. M. et al. Factors influencing clinician trust in predictive clinical decision support systems for in-hospital deterioration: qualitative descriptive study. JMIR Hum Factors 9, e33960 (2022).
Wong, A. et al. External validation of a widely implemented proprietary sepsis prediction model in hospitalized patients. JAMA Intern. Med. 181, 1065–1070 (2021).
Sankey, C. B., McAvay, G., Siner, J. M., Barsky, C. L. & Chaudhry, S. I. “Deterioration to door time”: an exploratory analysis of delays in escalation of care for hospitalized patients. J. Gen. Intern. Med. 31, 895–900 (2016).
Office of Surgeon General. Addressing Health Worker Burnout: The U.S. Surgeon General’s Advisory on Building a Thriving Health Workforce (US Department of Health and Human Services, 2022).
Lewis, A. E. et al. Electronic health record data quality assessment and tools: a systematic review. J. Am. Med. Inform. Assoc. 30, 1730–1740 (2023).
Weiskopf, N. G., Bakken, S., Hripcsak, G. & Weng, C. A data quality assessment guideline for electronic health record data reuse. EGEMS (Wash DC) 5, 14 (2017).
Singer, M. et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 315, 801–810 (2016).
Yale New Haven Health Services Corporation – Center for Outcomes Research and Evaluation (YNHHSC/CORE). 2023 Hospital-Wide Readmission Measure Updates and Specifications Report – Version 12.0. (2023); https://qpp.cms.gov/resources/document/fab5e228-1667-4e8f-9b49-ea04fb3cfd81
Shcherbatykh, I., Holbrook, A., Thabane, L., Dolovich, L. & COMPETE III investigators. Methodologic issues in health informatics trials: the complexities of complex interventions. J. Am. Med. Inform. Assoc. 15, 575–580 (2008).
Rossetti, S. C. et al. The Communicating Narrative Concerns Entered by Registered Nurses (CONCERN) clinical decision support early warning system: protocol for a cluster randomized pragmatic clinical trial. JMIR Res. Protoc. 10, e30238 (2021).
Rossetti S. C. et al. Leveraging clinical expertise as a feature - not an outcome - of predictive models: evaluation of an early warning system use case. In AMIA Annual Symposium Proc. 323–332 (AMIA, 2019).
Collett D. Modelling Survival Data in Medical Research 3rd edn (Chapman and Hall/CRC, 2014).
Jolliffe I. T. & Stephenson D. B. Forecast Verification: A Practitioner’s Guide in Atmospheric Science (Wiley, 2012).
Fu, L.-H. et al. Utilizing timestamps of longitudinal electronic health record data to classify clinical deterioration events. J. Am. Med. Inform. Assoc. 28, 1955–1963 (2021).
Abbey, E. J., Mammen, J. S. R., Soghoian, S. E., Cadorette, M. A. F. & Ariyo, P. In-hospital mortality and the predictive ability of the modified early warning score in Ghana: single-center, retrospective study. JMIRx Med. 2, e24645 (2021).
Delgado-Hurtado, J. J., Berger, A. & Bansal, A. B. Emergency department modified early warning score association with admission, admission disposition, mortality, and length of stay. J Community Hosp. Intern. Med. Perspect. 6, 31456 (2016).
Kao, C.-C. et al. Prognostic significance of emergency department modified early warning score trend in critical ill elderly patients. Am. J. Emerg. Med. 44, 14–19 (2021).
Kim W. Y. et al. Modified early warning score changes prior to cardiac arrest in general wards. PLoS ONE https://doi.org/10.1371/JOURNAL.PONE.0130523 (2015).
Knoery, C. et al. Modified early warning score and risk of mortality after acute stroke. Clin. Neurol. Neurosurg. 202, 106547 (2021).
Lee, J.-R. et al. Derivation and validation of modified early warning score plus SpO2/FiO2 score for predicting acute deterioration of patients with hematological malignancies. Korean J. Intern. Med. 35, 1477–1488 (2020).
Martín-Rodríguez, F. et al. Early warning scores in patients with suspected COVID-19 infection in emergency departments. J. Pers. Med. https://doi.org/10.3390/jpm11030170 (2021).
Monzon, L. D. R. & Boniatti, M. M. Use of the modified early warning score in intrahospital transfer of patients. Rev. Bras. Ter. Intensiva 32, 439–443 (2020).
Takada, K. et al. Association between Intraoperative early warning score and mortality and in-hospital stay in lower gastrointestinal spontaneous perforation. Anesthesiol. Res. Pract. 2023, 8910198 (2023).
Quan, H. et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med. Care. 43, 1130–1139 (2005).
Figueiredo, S. in Stroke Engine (eds Zeltzer, L. et al.) (Canadian Partnership for Stroke Recovery Heart & Stroke Foundation, 2009); https://strokengine.ca/en/assessments/charlson-comorbidity-index-cci
Hosmer, D. W., Lemeshow, S. & May, S. Applied Survival Analysis: Regression Modeling of Time-To-Event Data (Wiley, 2008).
Austin, P., Rothwell, D. & Tu, J. A comparison of statistical modeling strategies for analyzing length of stay after CABG surgery. Health Serv. Outcomes Res. Methodol. 3, 107–133 (2002).
Acknowledgements
This study was funded by the National Institute of Nursing Research (NINR R01NR016941, COmmunicating Narrative Concerns Entered by RNs (CONCERN): Clinical Decision Support Communication for Risky Patient States) (S.C.R., P.C.D., C.K., S.C., J.W., G.L., D.A., R.Y.L., H.J., S.B., M.J.K., F.Y.C., L.Z., T.D., F.L., M.T., S.M.A.B., J.T., K.D.C.) and Reducing Health Disparities Through Informatics (T32NR007969) (J.W., R.Y.L., S.B., J.S.D.). The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We thank all the nurses, prescribing providers and patients who participated in this study. We also acknowledge B. Westra for serving on our Advisory Board and the American Nurses Foundation Reimagining Nursing Initiative funding for sharing and evaluating the implementation of CONCERN EWS to additional study sites. We thank C. Stillwell for her contribution to the design of tables and figures and L. Schweig for editorial review.
Author information
Authors and Affiliations
Contributions
S.C.R. and K.D.C. had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. More than one author (K.D.C., S.C.R., G.L., H.J., M.T., J.W. and R.Y.L.) have directly accessed and verified the underlying data reported in the paper. The research concept was designed by S.C.R. and K.D.C. System development and study design was provided by S.C.R., K.D.C., P.C.D., C.K., S.C., D.A., G.L., S.B., M.J.K., F.Y.C., L.Z., J.W., H.J., F.L. and J.S.D. Acquisition, analysis or interpretation of data was performed by S.C.R., K.D.C., P.C.D., C.K., S.C., D.A., G.L., S.B., J.W., H.J., F.L., R.Y.L., T.D., M.T., S.M.A.B. and J.T. The paper was drafted by S.C.R., R.Y.L., K.D.C. and P.C.D. All authors contributed to the critical review of the paper for important intellectual content. Statistical analysis was carried out by H.J., K.D.C. and D.A. Funding was obtained by S.C.R. and K.D.C. Administrative, technical or material support was provided by S.C.R., K.D.C., P.C.D., R.Y.L., T.D. and F.L. Supervision was carried out by S.C.R., K.D.C., P.C.D. and S.B.
Corresponding author
Ethics declarations
Competing interests
Columbia University has filed a US nonprovisional patent application (US Patent Application No. 18/814,823) related to the technology that is the subject of this article. S.C.R., C.K. and K.D.C. are named inventors on the patent application and are entitled to revenue sharing with the university per the terms of the university’s patent policy. The university and the named inventors are committed to making the technology freely available upon request for academic noncommercial research purposes. Any entity interested in obtaining a license to practice the technology for commercial purposes may contact Columbia Technology Ventures at [email protected]. D.W.B. reports grants and personal fees from EarlySense, personal fees from CDI Negev, equity from ValeraHealth, equity from Clew, equity from MDClone, personal fees and equity from AESOP, personal fees and equity from FeelBetter, personal fees and equity from Guided Clinical Solutions and grants from IBM Watson Health, outside the submitted work. The other authors declare no competing interests.
Peer review
Peer review information
Nature Medicine thanks Alessio Crippa, Rupert Pearse, Jean-Louis Vincent and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editor: Lorenzo Righetto, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 CONCERN Predictive Model Conceptual Modeling Approach.
Figure adapted from ref. 10 under a Creative Commons license CC BY 40.
Extended Data Fig. 2 Percentage of Time Intervention and Usual Care Hospital Encounters Spent in Each Area 42 Hours Before Deterioration Event or Discharged Alive (N = 60,893).
This scatter plot visualizes the distribution of hours spent in the usual care (control) area (x-axis) and intervention area (y-axis) 42 h prior to an in-hospital deterioration event or being discharged alive for patients in the Control Group (blue) and Intervention Group (red).
Supplementary information
Supplementary Information
Supplementary Table 1, Methods 1–2, Fig. 1 and References.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rossetti, S.C., Dykes, P.C., Knaplund, C. et al. Real-time surveillance system for patient deterioration: a pragmatic cluster-randomized controlled trial. Nat Med 31, 1895–1902 (2025). https://doi.org/10.1038/s41591-025-03609-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-025-03609-7