Abstract
This is an interim analysis of the Beta-blocker (Propranolol) use in traumatic brain injury (TBI) based on the high-sensitive troponin status (BBTBBT) study. The BBTBBT is an ongoing double-blind placebo-controlled randomized clinical trial with a target sample size of 771 patients with TBI. We sought, after attaining 50% of the sample size, to explore the impact of early administration of beta-blockers (BBs) on the adrenergic surge, pro-inflammatory cytokines, and the TBI biomarkers linked to the status of high-sensitivity troponin T (HsTnT). Patients were stratified based on the severity of TBI using the Glasgow coma scale (GCS) and HsTnT status (positive vs negative) before randomization. Patients with positive HsTnT (non-randomized) received propranolol (Group-1; n = 110), and those with negative test were randomized to receive propranolol (Group-2; n = 129) or placebo (Group-3; n = 111). Propranolol was administered within 24 h of injury for 6 days, guided by the heart rate (> 60 bpm), systolic blood pressure (≥ 100 mmHg), or mean arterial pressure (> 70 mmHg). Luminex and ELISA-based immunoassays were used to quantify the serum levels of pro-inflammatory cytokines (Interleukin (IL)-1β, IL-6, IL-8, and IL-18), TBI biomarkers [S100B, Neuron-Specific Enolase (NSE), and epinephrine]. Three hundred and fifty patients with comparable age (mean 34.8 ± 9.9 years) and gender were enrolled in the interim analysis. Group 1 had significantly higher baseline levels of IL-6, IL-1B, S100B, lactate, and base deficit than the randomized groups (p = 0.001). Group 1 showed a significant temporal reduction in serum IL-6, IL-1β, epinephrine, and NSE levels from baseline to 48 h post-injury (p = 0.001). Patients with severe head injuries had higher baseline levels of IL-6, IL-1B, S100B, and HsTnT than mild and moderate TBI (p = 0.01). HsTnT levels significantly correlated with the Injury Severity Score (ISS) (r = 0.275, p = 0.001), GCS (r = − 0.125, p = 0.02), and serum S100B (r = 0.205, p = 0.001). Early Propranolol administration showed a significant reduction in cytokine levels and TBI biomarkers from baseline to 48 h post-injury, particularly among patients with positive HsTnT, indicating the potential role in modulating inflammation post-TBI.
Trial registration: ClinicalTrials.gov NCT04508244. It was registered first on 11/08/2020. Recruitment started on 29 December 2020 and is ongoing. The study was partly presented at the 23rd European Congress of Trauma and Emergency Surgery (ECTES), April 28–30, 2024, in Estoril, Lisbon, Portugal.
Similar content being viewed by others
Introduction
Traumatic brain injury (TBI) is a significant public health concern, accounting for a substantial burden of physical and cognitive disability and mortality worldwide1,2. Notably, TBI pathophysiology is biphasic. It encompasses the primary insult caused by the direct impact of the brain, worsened by events such as hypoxia, hypotension, and intracranial hypertension that increase the risk of secondary brain injury initiated by inflammatory cascade and further tissue damage3,4. The underlying biological processes involved in TBI can significantly differ based on clinical factors such as injury ___location, type, and severity of injury or underlying pathology and host response5. The two most used scores for defining and classifying the brain injury severity after trauma are the head Abbreviated Injury Score (HAIS) and the Glasgow Coma Scale (GCS). The AIS is an anatomic tool based on the computerized tomography (CT) scan or operative findings. At the same time, the GCS is a physiologic scale based on clinical examination (level of consciousness), regardless of the CT scan findings6. Generally, the GCS is the first classification of TBI by prehospital personnel or upon admission to acute care, although it does not offer specifics on the pathophysiology mechanisms involved7,8. Evaluating the severity of TBI is of utmost significance, as moderate-to-severe TBIs are prone to experiencing an upsurge in inflammatory responses. This, in turn, leads to elevated production of inflammatory cytokines and injury-specific markers9.
Earlier studies have reported that an increase in serum troponin levels in trauma patients also correlates with the severity of the injury and may be indicative of an adrenergic response to stress, even without any apparent direct cardiac injury10,11. Studies have revealed that high-sensitivity troponin (HsTnT) tests can detect even milder cardiac troponin elevations in plasma beyond the threshold of conventional troponin-T tests12. Notably, the acute inflammatory response triggered by TBI also depends upon the duration and strength of the catecholamine (neurotransmitters) surge, which may contribute to poor outcomes13. TBI results in changes in autonomic tone and widespread catecholamine release. Although sympathetic activation may initially be protective by preserving blood flow to the brain and other organs, this may eventually become maladaptive and result in systemic vasoconstriction and cardiac dysfunction, thus driving cardiovascular, pulmonary, and renal dysfunction14,15.
The adrenergic surge following TBI involves an increase in the circulating levels of catecholamines, corresponding to the severity of traumatic injury. This surge may persist beyond a week and contribute to inflammation and secondary injury, which is an extension of the injured territory by physiological responses16,17. Although no therapeutic intervention proved to prevent the progression of secondary neural injury, prior data showed that propranolol could slow the progression of such injury and lower the mortality rate even when compared with other beta-blockers (BBs)18,19,20,21. It has been speculated that diminishing the beta-adrenergic response could improve the outcome after trauma22.
TBI induces a substantial systemic inflammatory response, leading to the continuous production of inflammatory mediators, which can determine the injury's extent and persistence23. Moreover, biomarkers of TBI are not specific proteins that serve as indicators of numerous physiological processes, so inflammatory and TBI biomarkers may help in primary diagnosis to determine the severity of injury and prognostication24,25,26. The inflammatory mediators such as tumor necrosis factor-α (TNF-α), interleukin-6 (IL-6), interleukin-8, (IL-8), and interleukin-10 (IL-10) are potentially pivotal in influencing outcomes after TBI27. In adults, serum Neuron-Specific Enolase (NSE) (half-life of 48 h) and S100B (half-life of 2 h) levels have been reported as markers of neuronal damage and adverse outcomes after TBI28. Also, the expression of S100B is confined to the central nervous system and expressed in peripheral nervous tissue, muscle tissues, and adipocytes29. Multiple studies have confirmed NSE as a marker of intracranial injury30,31,32. Nevertheless, it is essential to recognize that the immune response to injury is an intricate and dynamic process, so exploration of the inflammatory characteristics is crucial. While prior research has linked inflammatory cytokine levels with TBI severity, the immunomodulatory role of BBs and TBI-specific biomarkers remains unclear.
This study sought to determine the effects of early administration of BBs (Propranolol) after TBI of varying degrees of severity. Considering the crucial role of the sympathetic nervous system in regulating physiological parameters following traumatic injury, we hypothesized that administering a daily dose of propranolol (1 mg intravenously or 40 mg orally on the first day of admission and continue for 6 days) would reduce the prolonged activation of the hyper-adrenergic state in patients with TBI. Also, the study aimed to ascertain whether propranolol administration effectively modulates the inflammatory cascade following TBI, as detected at baseline, 24- and 48-h post-injury in the interventional group, compared to a placebo group. Herein, we sought to perform an interim analysis at this stage, after attaining 50% of the study sample size, to ensure patient safety, confirm study feasibility, monitor the efficacy of therapy administration, which could guide the potential adjustments in trial conduct or early termination, optimize the resources use and uphold ethical standards. Moreover, early data from an interim analysis offer insights into the laboratory settings, feasibility, and biomarkers status following TBI and treatment. Additionally, interim analysis is a part of the study protocol requirement.
Methods
The “BBTBBT” is an ongoing prospective, single-center, double-blind, placebo-controlled randomized clinical trial investigating the clinical implications of early BBs administration (propranolol) in patients with TBI according to the HsTnT status. The target sample size is 771 TBI patients. The recruitment of the study commenced in January 2021 and is ongoing at the Hamad Level I Trauma Centre in Qatar.
The detailed study protocol, methodology, and sample size estimation have been described earlier11 and shown in Fig. 1. The current investigation is based on the interim analysis of the BBTBBT (samples collected from January 2021 to February 2023). It focuses on the pathophysiological importance of the cardiac, brain, and inflammatory biomarkers after TBI. This interim analysis included the first batch of recruited patients (n = 350).
Trial registration
ClinicalTrials.gov NCT 04508244. It was registered first on 11/08/2020. Recruitment for the study started on 29 December 2020 and is still ongoing. The study conforms to the CONSORT 2010 guidelines and the study protocol (Related files).
Study population
Adults with isolated or polytraumatic blunt TBI (head AIS scores of 1–5 or GCS scores of 3–15) enrolled within the first 24 h of the injury were eligible to participate. Exclusion criteria included: (i) non-survivable TBI patients (ii) uncontrollable hemorrhage, (iii) systolic blood pressure (SBP) of 100 mmHg or lower (or a mean arterial pressure (MAP) of less than 70 mmHg) who did not respond to initial resuscitation (iv) received continuous vasopressor support for persistently low blood pressure (for up to 24 h); (v) patients with bradycardia (heart rate < 60 beats per minute, with reassessment every 2 h); (vi) pregnant women; (vii) prisoners; (viii) patients with a history of severe bronchial asthma or cardiac disorders; and (ix) those in need of any emergent surgery within 6 h Patients on prior BBs or alcohol intoxication were excluded to avoid results bias and misleading GCS, respectively. Patients who were excluded from the study received the full standard of care.
All participants had HsTnT levels on admission, and if the initial result was within the normal range, the test was repeated after a 6-h interval if it was negative or inconclusive. HsTnT was assayed using Elecsys (Roche Diagnostics International Ltd.), and cut-off values of 14 ng/L and above were considered positive.
Patient recruitment and randomization
All the patients with mild-to-severe TBI necessitating hospitalization were screened for enrollment. The eligible patients were approached for consent before recruitment. Further, enrolled patients were stratified into three groups based on HsTnT findings, i.e., all patients with a positive HsTnT result received propranolol if there were no contraindications (Group-1) without randomization. Cardiology consultation would exclude the diagnosis of acute cardiac ischemia using serial cardiac markers, ECG, and echocardiographic examination. The study randomization was done for patients with two negative HsTnT results to receive propranolol (Group-2) or placebo (Group-3). The GCS on admission served as the primary clinical measure to define the severity of TBI, quantifying the brain injury severity on a numerical scale ranging from 3 to 15 (severe TBI: GCS 3–8; moderate TBI: GCS 9–12 and mild TBI: GCS 13–15)33. Patients were categorized according to GCS score at the time of admission before the randomization process. Therefore, we will have 257 TBI patients in each severity group at the end of the study to complete the study enrollment (771 patients). Severity based on the head AIS was defined as mild (1–2), moderate (3–4), and severe (≥ 5)34.
Rationale for propranolol selection and dosages
Propranolol is ideal for stressful conditions due to its non-selective inhibition and lipophilic properties, potentially reducing secondary injury and stress after TBI35,36. It is cost-effective and has a short plasma half-life, with easy administration through both intravenous and oral routes37. Notably, the existing literature lacks information about the optimal timing and duration of BB administration following sepsis and traumatic insults. In the current study, propranolol was administered during the initial 6 days post-injury. The intervention was administered within the first 24 h of hospital admission at 1 mg intravenously every 8 h for 2 days, followed by 1 mg intravenously every 12 h for another 2 days, and finally to 1 mg every 24 h for 2 days.
Oral propranolol (40 mg) was given to alert patients who could swallow medication safely.
The infusion duration was capped at 6 days from enrollment, considering the critical period for the initial development of cerebral edema post-TBI. This protocolized dosage regimen relies on clinical judgment regarding the peak sympathetic activation time and understanding the typical course of intracranial hypertension38,39. It ensures the primary research question is addressed during the period of greatest potential hemodynamic instability, avoiding unnecessary extended exposure to the drug or placebo. The subsequent use of propranolol or other beta-blockers was decided by the treating physician after cardiology consultation in patients with positive biomarkers.
Study consent procedure
The Institutional Review Board (IRB) approved four kinds of consent for this study due to the urgency of blood sampling and intervention for TBI patients who may be unconscious or incapable of immediate consent: (1) direct informed consent from patient who is conscious and able to comprehend and sign a consent; (2) unconscious or incapable of immediate consent, the legally authorized representative (NOK/LAR) can sign a consent; (3) if the NOK/LAR is unattainable, a deferred consent (approved by the institutional IRB) to be taken by two physicians (wherein one of the physicians must not be a part of the study team), (4) patient who later on regained cognitive function were given the option for delayed informed consent .
Data acquisition and collection
The prospectively collected clinical data was retrieved for each participant from the Qatar National Trauma Registry at HGH, Qatar. Data included demographics, initial vital signs at trauma resuscitation unit, head AIS, injury severity score, revised trauma score, and routine laboratory parameters such as WBC, hemoglobin, platelet count, international normalized ratio (INR), prothrombin time, activated partial thromboplastin time, serum urea, serum creatinine, serum sodium, potassium, blood glucose, HbA1C levels, HsTnT (initial and repeated after six h), C-reactive protein, lactate and base deficit. All participants enrolled in the study were subjected to a thorough assessment, complete history-taking, a comprehensive physical examination, including vital signs, and various investigative procedures, as mentioned above.
Sample collection and processing
For quantification of serum pro-inflammatory cytokines (IL-1β, IL-6, IL-8, and IL-18) and serum NSE, blood specimens were collected at three-time points, i.e., at baseline, after 24 h, and 48 h after enrollment in the study. Epinephrine levels were quantified at baseline and after 24 h, whereas the serum S100B levels were assayed at baseline only. Blood was collected in serum separator tubes, which were allowed to clot at room temperature for 15–30 min. The specimens were then centrifuged for 15 min at 3000 rpm, and the separated serum was aliquoted and stored at − 80 °C until further analysis.
Analysis of serum epinephrine, brain, and pro-inflammatory markers
Inflammatory cytokines and NSE were assayed using Human Magnetic Luminex Assay, 5-plex Kit (Target: human NSE, IL-1B, IL-6, IL-8, IL-18; Catalogue # LXSAHM-05; R&D Systems, Inc.) following the manufacturer’s instructions. Similarly, serum levels of S100B were quantified using Human Magnetic Luminex Assay, 1-Plex (Targets: Human S100B; Catalogue # LXSAHM-01; R&D Systems, Inc.). Briefly, the Bio-Plex employs flow cytometry principles to measure the analytes. This is achieved by directing a fluid flow that arranges beads in a single-file fashion through a cuvette. Dual lasers are used to stimulate each bead, and the fluorescence emitted by the beads is detected using avalanche photodiodes for bead identification and a photomultiplier tube for the reporter signal. The detection range and the sensitivity i.e., the mean minimum detectable dose for each analyte in the 5-plex assay panel was as follows: IL-1β: 17.7–4300 pg/ml (sensitivity: 0.8 pg/ml), IL-6: 4.53–1100 pg/ml (sensitivity: 1.7 pg/ml), IL-8: 4.12–1000 pg/ml (sensitivity: 1.8 pg/ml), IL-18: 7.12–1730 pg/ml (sensitivity: 1.93 pg/ml), and NSE: 514–125,000 pg/ml (sensitivity: 140 pg/ml). Moreover, the detection range for the S100B (1-plex) assay was 40.4–9800 pg/ml (sensitivity: 4.34 pg/ml). According to the manufacturer's protocols, serum epinephrine levels were measured through an ELISA kit (cat. no. NBP2-62,867; Novus Biologicals Inc.). The assay's sensitivity was 18.75 pg/ml, and the detection range was 31.25–2000 pg/ml. All specimens were assayed in duplicate using Luminex and the ELISA method.
Statistical analysis
All analyses were conducted using an intention-to-treat approach. As appropriate, data were presented in proportions, means, and 95% confidence intervals. Descriptive statistics for serum biomarkers were provided for the three study groups. The Kolmogorov–Smirnov test assessed whether continuous variables followed a normal distribution or were skewed. Given significant deviations from normality, non-parametric tests were used for inflammatory mediators and TBI biomarker data. Differences in categorical variables were examined using the χ2 test, and Yates’ corrected chi-square was utilized for categorical variables with expected cell frequencies below 5. Non-parametric group differences were assessed using the Mann–Whitney U-test or the Kruskal–Wallis independent samples test. For related samples, the Wilcoxon signed-rank test was conducted (with p values determined by Friedman ANOVA) separately for the three study groups to see the trend within the group for IL-6, IL-8, IL-18, IL-1β, and NSE levels at baseline, after 24 h and 48 h (three-time points) and Epinephrine levels at baseline, and after 24 h (two-time points).
Additionally, patients with TBI were categorized into two groups based on the type of head injury (polytrauma vs. isolated head injury), study treatment arms (propranolol vs. placebo), and troponin results (positive vs. negative). Correlation coefficient analyses were performed to determine the relationship between troponin level and other parameters. A two-tailed p value < 0.05 was considered statistically significant. Data analysis was conducted using the Statistical Package for Social Sciences version 21 (SPSS Inc., Chicago, IL, USA) and Prism version 8.0.1 (GraphPad, La Jolla, CA, USA).
Institutional review board statement
The Institutional Review Board of the Medical Research Center (MRC) (# IRGC-05-SI-18-293 and the Ministry of Public Health (IRB-MoPH Assurance: IRB-A-HMC-2019-0014) at Hamad Medical Corporation (HMC), Doha, Qatar, approved the study protocol. All methods were performed in accordance with the relevant guidelines and regulations at HMC.
Informed consent
Informed consent was obtained from subjects or NOK/LAR involved in the study.
Results
Overall, 350 adult patients with TBI were eligible for the interim analysis, of which 97% were males with a mean age of 34.8 ± 9.9 years. The frequent mechanisms of injury included traffic-related (41.7%), falls from height (35.4%), and pedestrians (12.0%). Echocardiography was done for 82 (23.4%) patients. Overall, 96 patients developed transient bradycardia after enrollment, and none of them required intervention, whereas seven patients developed hypotension, of which only four required interventions to normalize the SBP. Only three patients received massive transfusions, and three patients died during hospitalization.
Biomarkers in Randomized and non-randomized groups analysis
The characteristics of patients stratified into three groups based on HsTnT findings and randomization are compared in Table 1. The three groups did not differ in age and gender. Patients with positive HsTnT (non-randomized) who received propranolol (Group 1) were more likely to have higher mean heart rate (90, 87, vs. 85 bpm) (p = 0.04) and diastolic blood pressure (75, 79, vs. 76 mmHg) than Gp 2 and 3 (p = 0.002). They sustained severe injuries as indicated by higher head AIS (3.5, 3.1, vs. 3.3) than Gp 2 and 3 (p = 0.01), ISS (23,16, vs. 17.5) (p = 0.001), and lower RTS (6.4, 7.0, vs. 7.4) (p = 0.001) than the other groups. Moreover, Group 1 had higher mean initial blood glucose levels (8.8, 7.3, vs 6.7 mmol/l) than Gp 2 and Gp 3 (p = 0.001). However, HbA1c was comparable among the three groups, with a mean of 5.7%. Patients in Gp1 were more likely to have polytrauma (p = 0.001), frequently requiring ICP insertion (p = 0.004) and blood transfusion (p = 0.001), as compared to other groups. There were no significant differences in terms of the type of brain lesion among the three groups except for the higher rate of brain contusion in Gp1.
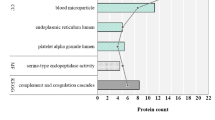
Table 2 and Fig. 2 show a trend analysis of the inflammatory mediators such as IL-6, IL-8, IL-18, IL-1β, and NSE at three time points for each group and across the three groups. The mean IL-6 levels at baseline, after 24 and 48 h, were significantly higher in Group 1 compared to the other groups, with a decreasing trend observed in Group 1 (p = 0.001) and Group 2 (p = 0.004). In contrast, the placebo group showed a significant increase (p = 0.001). Notably, IL-18 levels decreased significantly from baseline to 24 h and 48 h in Group 1 (p = 0.02) and Group 3 (p = 0.002). Similarly, IL-1β levels decreased significantly from the baseline to 24 h and 48 h in Group 1 (p = 0.001) and Group 3 (p = 0.01), though Group 1 had higher baseline levels compared to the other groups (p = 0.02). IL-8 levels increased consistently in Group 1 and Group 3 from baseline to 48 h. A notable reduction in epinephrine levels from baseline to 24 h was observed in Group 1 (p = 0.02).
Regarding the brain injury marker, Group 1 had significantly higher baseline concentrations of S100B compared to the other groups (p = 0.01). Moreover, enolase levels significantly declined from baseline to 24 h and at 48 h in Group 1 and Group 2.
Comparison of biomarkers across the TBI severity
Table 3 and Fig. 3 compare the levels of pro-inflammatory cytokines and markers of brain injury based on the severity of head injury. Most patients had mild TBI (66.6%), with 14.3% having moderate and 19.1% severe TBI. Severe TBI patients exhibited higher mean serum levels of troponin T (p = 0.001), C-reactive protein (p = 0.01), and base deficit (p = 0.001) compared to mild or moderate TBI. IL-6 levels significantly decreased post-injury in moderate (p = 0.004) and severe TBI (p = 0.001) groups, with higher baseline and 24-h levels in severe TBI cases. A significant decrease in IL-1β levels at 24 h and 48 h was observed in mild (p = 0.001) and severe TBI (p = 0.01). However, at baseline, severe TBI cases exhibited significantly higher IL-1β levels than the other two groups (p = 0.02). No significant trends were observed for IL-8, IL-18, and epinephrine levels. NSE levels significantly decreased from baseline to 48 h in the mild and moderate TBI group (p = 0.001).
The correlation coefficient among the cohort
HsTnT levels significantly correlated with ISS (r = 0.275, p = 0.001), GCS (r = − 0.125, p = 0.02), and serum S100B (r = 0.205, p = 0.001).
Biomarkers in isolated versus polytrauma TBI
Table 4 compares pro-inflammatory cytokines among polytrauma and isolated head injury cases. Polytrauma cases had significantly higher mean levels of HsTnT (p = 0.001), base deficit (p = 0.001), IL-6 at different time points (p = 0.001 for all), and baseline IL-8 levels (p = 0.01) as compared to the isolated TBI cases.
Biomarkers in patients with negative versus positive HsTnT
Table 5 compares inflammation and head injury markers based on initial troponin findings.
The IL-6 levels persistently and significantly decreased over time in both groups (p = 0.001), with higher values in the Troponin positive group at each time point. Furthermore, there was a significant decrease in IL-1β (p = 0.001), epinephrine (p = 0.01), and NSE (p = 0.004) levels from the baseline to 24 h and 48 h in the troponin-positive group.
Biomarkers in patients received propranolol versus placebo
A total of 239 (68.3%) TBI patients received propranolol and 111 (31.7%) received placebo in the study (Table 6). The two groups were comparable for all inflammatory mediators and markers of brain injury (Fig. 4). However, the mean serum levels of IL-6, IL-1β, epinephrine, and NSE decreased significantly from the baseline to 24 h and 48 h in the propranolol group (p = 0.001).
Biomarkers in patients who received propranolol versus placebo (moderate-severe TBI only based on the GCS)
In patients with moderate to severe TBI, those who were treated with propranolol showed a significant decrease in t IL-6, IL-18, and IL-1β levels from baseline to 48 h (p = 0.001, p = 0.002, 0.009, respectively), indicating an anti-inflammatory effect which was not observed in the placebo group (Table 7). IL-8 levels increased in both groups from baseline to 48 h without significant differences. The propranolol group showed a significant reduction in epinephrine levels at 24 h (p = 0.03), highlighting an impact on stress response modulation, a phenomenon not observed in the placebo group. With respect to brain injury markers, NSE levels in the Propranolol group significantly decreased at 48 h (p = 0.001), while the placebo group did not show a significant change.
Discussion
The BBTBBT study investigates the association between adrenergic blockade, inflammation, cardiac, and brain injury biomarkers in patients with mild-to-severe TBI. This study intends to explore whether the protocolized use of propranolol in TBI mitigates the adrenergic surge post-injury. Notably, BBs are commonly administered for cardiovascular conditions such as myocardial ischemia, cardiomyopathy and tachyarrhythmia. Therefore, we did not include the troponin-positive patients in the randomization process. All these patients received propranolol unless there were contraindications, and further cardiology consultations were made to rule out acute ischemia. The clinical utility of BBs was also explored in the acute management of patients with trauma11,14. It is evident that post-TBI, there is a notable surge in catecholamine and cytokine levels, and the severity of the injury is directly linked to the blood levels of these neurotransmitters15. However, we should consider the inconsistent effects of catecholamines on the immune system, as they generally are regarded as immunosuppressive agents. Prior reports showed that catecholamines contribute to severe immune dysregulation during septic shock40,41. Epinephrine inhibits the production of type 1/pro-inflammatory cytokines, whereas it stimulates the production of type 2/anti-inflammatory cytokines42. The current interim analysis found that patients with TBI positive for HsTnT had significantly elevated IL‑6 levels than the troponin-negative patients, and these levels decreased more profoundly from the baseline to the 48 h-level in those who received propranolol.
Additionally, there was a notable decrease in the epinephrine levels from the initial baseline measurement to the 24 h-level in the troponin-positive group that received propranolol. These findings corroborate the increasing evidence indicating the potential use of propranolol in modulating the adrenergic response during critical illness43, including acute TBI14,42. The possible mechanism is related to a decline in catecholamines, implying that BBs could attenuate the effects of catecholamines following TBI, perhaps leading to a decrease or slowing in secondary damage progression15.
Although the acute inflammatory response is essential for immune protection, it can also have significant negative consequences if it leads to systemic inflammation, triggering secondary injury cascades, and organ failure44. Following TBI, numerous inflammatory cytokines are released as part of the neuro-inflammatory response. Among these, IL-6 is produced by microglia, astrocytes, and neurons in response to the acute neurotrauma, which can be easily detected in the serum within 1 h, with levels peaking between 2 and 8 h post-injury45. Similarly, IL-1β is another pro-inflammatory cytokine, which is significantly elevated soon after TBI, primarily released by activated microglia and, to a lesser extent, by damaged endothelial cells and astrocytes46. Notably, the acute and delayed phases of TBI are characterized by high expression of pro-inflammatory cytokines such as IL-1β, IL-6, and interferon-gamma, and the anti-inflammatory cytokine IL-447. Also, the degree of injury is directly linked to the production of IL-6 and IL-1β45,46.
Consequently, evaluating cytokine profiles after TBI can provide insight into the extent of tissue damage. In our study, the baseline IL-1β levels were significantly elevated in the Troponin-positive group compared to the troponin-negative group. Evidence suggests that even without direct myocardial injury, elevated serum troponin levels reflect the severity of injury and myocardial damage due to stress-induced adrenergic surge11. Moreover, an experimental study demonstrated that within 1 h of moderate or severe TBI, there is an increase in IL-1β mRNA and protein levels in both the cortex and subcortical regions of rats48. This suggests that elevated troponin levels may be indicative of a severe overall injury, with elevated IL-1β levels serving as a marker of the inflammatory response to traumatic events.
Furthermore, our study found that the baseline levels of IL-6, IL-1β, and S100B were higher in Troponin positive patients than in Troponin negative patients. This suggests a potential correlation between elevated o biomarker levels and the presence of cardiac Troponin, indicating an interplay between injury severity and acute inflammatory response after TBI49. Consistent with our findings, earlier research has shown a significant correlation between IL-6 levels and specific neurological biomarkers related to TBI, including nerve growth factor, S100B, and NSE50,51. We also observed a significant correlation between the HsTnT levels, GCS, and serum S100B.
In the present study, individuals with severe TBI showed a higher levels of Troponin, C-reactive protein, IL-6, and IL-1β than those with mild or moderate TBI. This indicates that severe TBI is associated with a more pronounced physiological response, reflected by increased levels of these biomarkers52,53. These findings suggest a more intense and systemic impact on various physiological processes in severe TBI cases compared to less severe forms of brain injury. Supporting our findings, a prospective study demonstrated a correlation between IL-6 levels and various parameters used to diagnose TBI33, highlighting the potential role of IL-6 in assessing localized neural tissue damage and systemic pathology in TBI. As IL-6 is produced by activated astrocytes, microglial cells, neurons, and brain epithelial cells, it plays complex roles in neuroprotection and neuronal regeneration54. Elevated IL-6 levels during the acute stages of TBI appear beneficial54,55. However, prolonged high IL-6 levels may indicate a poor prognosis after TBI55. Additionally, a meta-analysis showed that excessive IL-6 release predicts poor outcomes in TBI patients56. An animal study showed that catecholamines used to maintain adequate cerebral perfusion pressure induced a sustained IL-6 release, and potentially worsened the brain edema57.
IL-8 peaks shortly after TBI and shows sustained elevation from baseline to 24 h and 48 h, suggesting a manifestation of the secondary injury phase. Numerous studies have observed a rapid and persistent increase in IL-8 levels following moderate to severe traumatic brain injury58,59. Consistent with our findings, Maier et al.59 reported a significant early increase in CSF and plasma IL-8 levels after trauma compared to baseline levels. Interestingly, we observed a trend of decreasing IL-8 levels with lower GCS scores, although this elevation of IL-8 levels did not reach statistical significance. However, an earlier study by Polat et al.60, found no significant association between serum IL-8 levels and GCS scores.
A previous study demonstrated a relationship between serum S100B levels and polytrauma, with the highest baseline level observed in polytrauma patients without TBI (495 pg/mL) followed by TBI patients with polytrauma (333 pg/mL) and isolated TBI (71 pg/mL)44. Consistent with these observations, our cohort showed that S100B levels were slightly higher, though not significantly, in TBI patients with polytrauma compared to those with isolated TBI. In our cohort, baseline NSE levels were non-significantly higher in isolated TBI than in polytrauma patients. However, there was a noticeable trend of decreasing NSE levels over the initial 3 days post-injury. This could be attributed to isolated TBI potentially causing a more direct and intense impact on neural tissue, leading to a higher release of NSE from damaged neurons. Contrarily, Schindler et al.44 reported higher serum levels in polytrauma patients with or without TBI as compared to isolated TBI. The authors suggested hemolysis after polytrauma or the release of NSE due to reperfusion damage in polytrauma as the possible explanation for these observations.
TBI associated with polytrauma in our study exhibited higher initial levels of IL-6 and IL-8 compared to cases with isolated TBI. Of note, IL-6 possesses both pro-inflammatory and anti-inflammatory properties61. Consistent with our results, Seekamp et al.62 showed elevated serum levels of IL-6, IL-8, and IL-10 at baseline in polytrauma patients with or without TBI compared to isolated TBI. Prolonged systematic inflammation can persist even after mild TBI, as shown by Chaban et al.63. Patients with mild TBI showed a prolonged increase in blood cytokines, including IL-8 and TNF, from admission to 1-year post-injury compared to healthy subjects.
Limitations
Although interim analysis is valuable in clinical trials64, this analysis has some limitations that need to be considered. Firstly, despite having a substantial TBI population for examining troponin release in relation to brain biomarkers and cytokines, the number of moderate-to-severe TBI cases is currently limited due to the interim nature of our analysis (only 50% of the targeted sample). Secondly, due to three deaths during the study period so far, we did not analyze inflammatory cytokine levels in relation to the primary outcome (mortality) after TBI. This relatively low mortality is attributed to 66.6% of the cohort having mild TBI. Further, the fact that our study is being undertaken at a single site limits the possible generalizability. Prior reports showed that the GCS total score may not be optimal for defining TBI severity or monitoring recovery, and even the GCS subscales have limitations due to their exclusion of certain behaviors65. Moreover, the head AIS scoring tool has its limitations; however, at the end of the study, the findings of the head CT scan will be utilized for the study's tertiary outcomes. Additionally, due to budget constraints, biomarkers were not assessed continuously during the first 6 days post-enrollment in line with treatment, which influenced our decision to focus on the most informative four interleukins.
Moreover, in the current study, we administered propranolol within 24 h post-injury for 6 days. However, the optimal timing and specific duration for propranolol administration following a brain injury remains uncertain. Nonetheless, no studies have explored the optimal and protocolized timing, dosages, type, and route of BBs post-TBI to date. The full 6 days medication regimen was not attained in some patients because of early discharge (134 mild cases), three early mortality, two patients refused to continue medications, 21 patients did not achieve it because of delayed preparation and dispensing of the medication, and the physician stopped the medications in 51 cases because of transient bradycardia. Finally, the acute inflammatory response following TBI is an intricate and multifaceted process with substantial individual variations among the involved molecules66. A limited number of cytokines cannot adequately capture its comprehensive description, so a more extensive array of pro- and anti-inflammatory cytokines panels is needed to understand their crosstalk, interaction, and response to BBs in TBI patients. However, the outcomes based on these biomarkers will be more evident after completing the targeted study population. Also, at this stage, the findings could be sex-biased, as 97% of our patients were male. Most trauma-related studies in Qatar showed that females represent ≤ 10% of hospitalized patients with head injuries67,68,69.
In conclusion, early BB administration showed reduced cytokine levels and TBI biomarkers from baseline to 48 h post-injury, particularly among patients with positive Troponin, indicating its potential role in modulating stress response and inflammation post-TBI. Moreover, elevated levels of IL-6, IL-1B, S100B, HsTnT, and CRP were associated with severe head injuries. These findings underscore the potential modulation of the inflammation-mediated immune responses in TBI patients. This analysis indicates that TBI triggers a specific temporal inflammatory response when combined with polytrauma. Given this finding, involving more moderate-to-severe TBI patients at the end of the study will enable a better understanding of the relationship between troponin release following TBI and its association with a broader array of inflammatory cytokines and biomarkers.
Data availability
All data were presented in the manuscript, tables, and figures.
References
Haarbauer-Krupa, J. et al. Epidemiology of chronic effects of traumatic brain injury. J. Neurotrauma 38(23), 3235–3247 (2021).
Demlie, T. A. et al. Incidence and predictors of mortality among traumatic brain injury patients admitted to Amhara region Comprehensive Specialized Hospitals, northwest Ethiopia, 2022. BMC Emerg. Med. 23(1), 55 (2023).
Brett, B. L. et al. Traumatic brain injury and risk of neurodegenerative disorder. Biol. Psychiatr. 91(5), 498–507 (2022).
Ng, S. Y. & Lee, A. Y. W. Traumatic brain injuries: Pathophysiology and potential therapeutic targets. Front. Cell. Neurosci. 13, 528 (2019).
Adrian, H., Mårten, K., Salla, N., et al. Biomarkers of traumatic brain injury: Temporal changes in body fluids. eNeuro. 3(6) (2016).
Stead, L. G. et al. TBI surveillance using the common data elements for traumatic brain injury: A population study. Int. J. Emerg. Med. 6(5), 1–7 (2013).
Rogers, S. & Trickey, A. W. Classification of traumatic brain injury severity using retrospective data. J. Nurs. Educ. Pract. https://doi.org/10.5430/jnep.v7n11p23 (2017).
Saatman, K. E. et al. Classification of traumatic brain injury for targeted therapies. J. Neurotrauma 25(7), 719–738 (2008).
Kumar, R. G. et al. Acute CSF interleukin-6 trajectories after TBI: Associations with neuroinflammation, polytrauma, and outcome. Brain Behav. Immun. 45, 253–262 (2015).
Dou, L. W. et al. Changes and significance of serum troponin in trauma patients: A retrospective study in a level I trauma center. World J. Emerg. Med. 13(1), 27–31 (2022).
El-Menyar, A. et al. Beta blocker use in traumatic brain injury based on the high-sensitive troponin status (BBTBBT): Methodology and protocol implementation of a double-blind randomized controlled clinical trial. Trials. 22(1), 890 (2021).
Bikdeli, B. et al. High-sensitivity vs conventional troponin cut-offs for risk stratification in patients with acute pulmonary embolism. JAMA Cardiol. 9(1), 64–70 (2024).
Wiles, M. D. Management of traumatic brain injury: A narrative review of current evidence. Anaesthesia. 77(Suppl 1), 102–112 (2022).
El-Menyar, A. et al. Brain–heart interactions in traumatic brain injury. Cardiol. Rev. 25(6), 279–288 (2017).
Rizoli, S. B. et al. Catecholamines as outcome markers in isolated traumatic brain injury: The COMA-TBI study. Crit. Care (London, England). 21(1), 37 (2017).
Naredi, S. et al. Increased sympathetic nervous activity in patients with nontraumatic subarachnoid hemorrhage. Stroke 31, 901–906 (2000).
Lozano, D. et al. Neuroinflammatory responses to traumatic brain injury: Etiology, clinical consequences, and therapeutic opportunities. Neuropsychiatr. Dis. Treat. 11, 97–106 (2015).
Alali, A. S. et al. Beta-blockers and traumatic brain injury: A systematic review and meta-analysis. Ann. Surg. 266, 952–961 (2017).
Ley, E. J. et al. Beta blockers in critically ill patients with traumatic brain injury: Results from a multicenter, prospective, observational American association for the surgery of trauma study. J. Trauma Acute Care Surg. 84, 234–244 (2018).
Hart, S. et al. Beta blockers in traumatic brain injury: A systematic review and meta-analysis. Trauma Surg. Acute Care Open 8(1), e001051. https://doi.org/10.1136/tsaco-2022-001051 (2023).
Khalili, H. et al. Beta-blocker therapy in severe traumatic brain injury: A prospective randomized controlled trial. World J. Surg. 44(6), 1844–1853 (2020).
Loftus, T. J. et al. β-blockade use for traumatic injuries and immunomodulation: A review of proposed mechanisms and clinical evidence. Shock (Augusta, GA). 46(4), 341–351 (2016).
Woodcock, T. & Morganti-Kossmann, M. C. The role of markers of inflammation in traumatic brain injury. Front. Neurol. 4, 18 (2013).
Edalatfar, M. et al. Biofluid biomarkers in traumatic brain injury: A systematic scoping review. Neurocrit. Care 35(2), 559–572 (2021).
Ghaith, H. S. et al. A literature review of traumatic brain injury biomarkers. Mol. Neurobiol. 59(7), 4141–4158 (2022).
Hier, D. B. et al. Blood biomarkers for mild traumatic brain injury: A selective review of unresolved issues. Biomark. Res. 9(1), 70 (2021).
Abboud, A. et al. Inflammation following traumatic brain injury in humans: Insights from data-driven and mechanistic models into survival and death. Front. Pharmacol. 7, 342 (2016).
Stefanović, B. et al. Elevated serum protein S100B and neuron specific enolase values as predictors of early neurological outcome after traumatic brain injury. J. Med. Biochem. 36(4), 314–321 (2017).
Störmann, P. et al. Monotrauma is associated with enhanced remote inflammatory response and organ damage, while polytrauma intensifies both in porcine trauma model. Eur. J. Trauma Emerg. Sur. Off. Publ. Eur. Trauma Soc. 46(1), 31–42 (2020).
Cheng, F. et al. The prognostic value of serum neuron-specific Enolase in traumatic brain injury: systematic review and meta-analysis. PloS One. 9(9), e106680 (2014).
Mercier, E. et al. Predictive value of neuron-specific Enolase for prognosis in patients with moderate or severe traumatic brain injury: A systematic review and meta-analysis. CMAJ Open. 4(3), E371–E82 (2016).
Thelin, E. P. et al. Utility of neuron-specific Enolase in traumatic brain injury; relations to S100B levels, outcome, and extracranial injury severity. Crit. Care (London, England). 8(20), 285 (2016).
Tsitsipanis, C. et al. Inflammation biomarkers IL-6 and IL-10 may improve the diagnostic and prognostic accuracy of currently authorized traumatic brain injury tools. Exp. Ther. Med. 26(2), 364 (2023).
Savitsky, B., Givon, A., Rozenfeld, M., Radomislensky, I. & Peleg, K. Traumatic brain injury: It is all about definition. Brain Inj. 30(10), 1194–1200 (2016).
Ko, A. et al. Early propranolol after traumatic brain injury is associated with lower mortality. J. Trauma Acute Care Surg. 80(4), 637–642. https://doi.org/10.1097/TA.0000000000000959 (2016).
Neil-Dwyer, G., Bartlett, J., McAinsh, J. & Cruickshank, J. M. Beta-adrenoceptor blockers and the blood-brain barrier. Br. J. Clin. Pharmacol. 11(6), 549–553 (1981).
Schroeppel, T. J. et al. Traumatic brain injury and β-blockers: Not all drugs are created equal. J. Trauma Acute Care Surg. 76(2), 504–509 (2014).
Unterberg, A. et al. Edema and brain trauma. Neuroscience. 129, 1021–1029. https://doi.org/10.1016/j.neuroscience.2004.06.046 (2004).
Stein, D. et al. Timing of intracranial hypertension following severe traumatic brain injury. Neurocrit. Care. 18, 332–340 (2013).
Bergmann, M. & Sautner, T. Immunomodulatory effects of vasoactive catecholamines. Wien. Klin. Wochenschr. 114, 752–761 (2002).
Flierl, M. A., Rittirsch, D., Huber-Lang, M., Sarma, J. V. & Ward, P. A. Catecholamines-crafty weapons in the inflammatory arsenal of immune/inflammatory cells or opening pandora’s box?. Mol. Med. 14(3–4), 195–204 (2008).
Ilia, J. Elenkov: Effects of catecholamines on the immune response. NeuroImmune Biol. 7, 189–206 (2007).
Bruning, R. et al. Beta-adrenergic blockade in critical illness. Front. Pharmacol. 12, 735841 (2021).
Chindler, C. R. et al. Severe traumatic brain injury (TBI) modulates the kinetic profile of the inflammatory response of markers for neuronal damage. J. Clin. Med. 9(6), 1667 (2020).
Ooi, S. Z. Y. et al. Interleukin-6 as a prognostic biomarker of clinical outcomes after traumatic brain injury: A systematic review. Neurosurg. Rev. 45(5), 3035–3054 (2022).
Ozen, I. et al. Interleukin-1 beta neutralization attenuates traumatic brain injury-induced microglia activation and neuronal changes in the globus pallidus. Int. J. Mol. Sci. 21(2), 387 (2020).
Holmin, S. & Höjeberg, B. In situ detection of intracerebral cytokine expression after human brain contusion. Neurosci. Lett. 369(2), 108–114 (2004).
Kinoshita, K. et al. Interleukin-1beta messenger ribonucleic acid and protein levels after fluid-percussion brain injury in rats: importance of injury severity and brain temperature. Neurosurgery. 51(1), 195–203 (2002).
Dash, P. K. et al. Biomarkers for the diagnosis, prognosis, and evaluation of treatment efficacy for traumatic brain injury. Neurotherap. J. Am. Soc. Exp. NeuroTherap. 7(1), 100–114 (2010).
Chiaretti, A. et al. Interleukin-6 and nerve growth factor upregulation correlates with improved outcome in children with severe traumatic brain injury. J. Neurotrauma 25(3), 225–234 (2008).
Raheja, A. et al. Serum biomarkers as predictors of long-term outcome in severe traumatic brain injury: Analysis from a randomized placebo-controlled Phase II clinical trial. J. Neurosurg. 125(3), 631–641 (2016).
Gerber, K. S. et al. Biomarkers of neuroinflammation in traumatic brain injury. Clin. Nurs. Res. 31(7), 1203–1218 (2022).
Johnson, N. H. et al. Inflammatory biomarkers of traumatic brain injury. Pharmaceuticals (Basel, Switzerland). 15(6), 660 (2022).
Kummer, K. K., Zeidler, M., Kalpachidou, T. & Kress, M. Role of IL-6 in the regulation of neuronal development, survival and function. Cytokine. 144, 155582. https://doi.org/10.1016/j.cyto.2021.155582 (2021).
Ley, E. J., Clond, M. A., Singer, M. B., Shouhed, D. & Salim, A. IL6 deficiency affects function after traumatic brain injury. J. Surg. Res. 170(2), 253–256 (2011).
Ooi, S. Z. Y. et al. Interleukin-6 as a prognostic biomarker of clinical outcomes after traumatic brain injury: A systematic review. Neurosurg. Rev. 45(5), 3035–3054 (2022).
Stover, J. F. et al. Norepinephrine infusion increases interleukin-6 in plasma and cerebrospinal fluid of brain-injured rats. Med. Sci. Monit. 9(10), BR382–BR388 (2003).
Whalen, M. J. et al. Interleukin-8 is increased in cerebrospinal fluid of children with severe head injury. Crit. Care Med. 28(4), 929–934 (2000).
Maier, B. et al. Differential release of interleukines 6, 8, and 10 in cerebrospinal fluid and plasma after traumatic brain injury. Shock (Augusta, GA). 15(6), 421–426 (2001).
Polat, Ö. et al. Is IL-8 level an indicator of clinical and radiological status of traumatic brain injury?. Turk. J. Trauma Emerg. Surg. TJTES. 25(2), 193–197 (2019).
Scheller, J. et al. The pro- and anti-inflammatory properties of the cytokine interleukin-6. Biochim. Biophys. Acta. 1813(5), 878–888 (2011).
Seekamp, A. et al. Serum IL-6, IL-8 and IL-10 levels in multiple trauma compared to traumatic brain injury and combined trauma. Eur. J. Trauma 28, 183–189 (2002).
Chaban, V. et al. Systemic inflammation persists the first year after mild traumatic brain injury: Results from the prospective trondheim mild traumatic brain injury study. J. Neurotrauma 37(19), 2120–2130 (2020).
Ciolino, J. D., Kaizer, A. M. & Bonner, L. B. Guidance on interim analysis methods in clinical trials. J. Clin. Transl. Sci. 7(1), e124. https://doi.org/10.1017/cts.2023.552 (2023).
Bodien, Y. G. et al. Diagnosing level of consciousness: The limits of the glasgow coma scale total score. J. Neurotrauma 38(23), 3295–3305 (2021).
El-Menyar, A. et al. Beta-adrenergic receptor polymorphism and patho-genetics of trauma: A transformational frontier of personalized medicine in neurotrauma. J. Neurotrauma. https://doi.org/10.1089/neu.2023.0432 (2023).
Parchani, A. et al. Traumatic subarachnoid hemorrhage due to motor vehicle crash versus fall from height: A 4-year epidemiologic study. World Neurosurg. 82(5), e639–e644 (2014).
El-Menyar, A. et al. Gender discrepancy in patients with traumatic brain injury: A retrospective study from a level 1 trauma center. Biomed. Res. Int. 18(2022), 3147340. https://doi.org/10.1155/2022/3147340 (2022).
Asim, M. et al. Rotterdam and Marshall scores for prediction of in-hospital mortality in patients with traumatic brain injury: An observational study. Brain Inj. 35(7), 803–811 (2021).
Acknowledgements
The authors thank all the staff of the Trauma Surgery Department, and Mr Muhamed Ibnas, RN at Hamad General Hospital, Doha, Qatar.
Funding
This research was funded by the Medical Research Center of Hamad Medical Corporation, Qatar under the category of grant funding ‘Internal Research Grant Competition’ (Grant No.: IRGC-05-SI-18-293).
Author information
Authors and Affiliations
Contributions
Conceptualization, methodology, draft manuscript: A.E., data collection: I.M., M.A.L., A.K., A.A., S.H., B.Y., I.T., H.J., T.S., A.H., N.A., M.T., A.B., K.A., S.A.; lab analysis: S.U., K.P., N.K., M.A., Data analysis, interpretation, visualization, M.A., N.K., Review and editing: I.C., H.A., S.R., A.E. All authors have read and agreed to publish the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
El-Menyar, A., Asim, M., Khan, N. et al. Systemic and cerebro-cardiac biomarkers following traumatic brain injury: an interim analysis of randomized controlled clinical trial of early administration of beta blockers. Sci Rep 14, 19574 (2024). https://doi.org/10.1038/s41598-024-70470-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-70470-y