Abstract
Secondary BRAF variations have been identified as a mechanism of resistance to tyrosine kinase inhibitors (TKIs) in patients with driver gene-positive NSCLC. Nevertheless, there is still a lack of consensus regarding the characteristics and subsequent treatment strategies for these patients. We retrospectively reviewed the medical records of patients with driver gene-positive NSCLC who received TKIs therapy at Zhejiang Cancer Hospital between May 2016 and December 2023. The clinical and genetic characteristics of these patients were assessed, along with the impact of various treatment strategies on survival. This study enrolled 27 patients with advanced NSCLC, in whom BRAF variations occurred at a median time of 28 months after the initiation of targeted therapy. The multivariate accelerated failure time (AFT) model revealed that, compared to chemotherapy-based regimens group, the combined targeted therapy group (p < 0.001) and the combined local treatment group for oligo-progression (p < 0.001) significantly extended patient survival. In contrast, continuing the original signaling pathway's targeted monotherapy was associated with shorter survival (p = 0.034). The median global OS for each treatment group was as follows: chemotherapy-based regimens group, 45 months; combined targeted therapy group, 59 months; combined local treatment group for patients with oligo-progression, 46 months; and targeted monotherapy group, 36 months. Study results indicate that the combination targeted therapy group (including TKIs, BRAF inhibitors, and/or MEK inhibitors) and the localized treatment group are more effective than traditional chemotherapy-based regimens in improving survival. Additionally, continuing targeted monotherapy along the original signaling pathway proves less effective than chemotherapy-based regimens.
Similar content being viewed by others
Introduction
TKIs have improved survival for patients with advanced NSCLC harboring driver mutations. However, resistance to targeted therapies is inevitable. Currently, the mechanisms of acquired resistance to TKIs, primarily involve the activation of pathways dependent on or independent of driver genes, as well as histological transformation1,2. Advances in genomic testing have made it easier to detect variations in the BRAF gene. However, the clinical significance of acquired BRAF variations remains unclear due to their low incidence. Only 1%-7% of NSCLC patients with resistance to EGFR TKIs exhibit acquired BRAF variations3,4. The BRAF gene, part of the RAF serine/threonine kinase family, encodes a kinase that regulates cell growth and differentiation by activating the downstream RAS-MAPK pathway. BRAF variations, including mutations and fusions, activate downstream pathways via bypass signaling, driving uncontrolled cell proliferation and resistance. BRAF mutations are categorized into BRAF V600 and BRAF Non-V600 mutations. BRAFV600 mutations continuously activate the MEK/ERK signaling pathway through their monomeric protein form, while BRAF Non-V600 mutations activate downstream pathways by dimerizing with CRAF or wild-type BRAF. BRAF fusions result in the loss of the auto-inhibitory ___domain, leading to the formation of constitutive dimers that continuously activate downstream pathways5,6. Research on subsequent treatments for these patients mainly consists of case reports and in vitro studies, and the best treatment strategy post-resistance remains controversial. Therefore, we conducted a retrospective study to explore the clinical and genetic characteristics of patients with driver gene-positive (EGFR/ALK/ROS1) advanced NSCLC who developed BRAF variations after resistance to targeted therapies, as well as the impact of different treatment strategies on their survival. This study aims to provide clinical insights into the characteristics and treatment options for patients with acquired resistance due to secondary BRAF variations.
Methods
Study subjects and data collection
We retrospectively reviewed the medical records of patients with driver gene-positive NSCLC who received TKIs therapy at Zhejiang Cancer Hospital between May 2016 and December 2023. Among a cohort of 3,150 patients, we identified 27 patients who developed secondary BRAF variations following resistance to TKIs therapy. These patients were subsequently included in our study. For these patients, samples of tumor tissue or body fluids (including pleural effusion, plasma, or cerebrospinal fluid) were collected at the initial diagnosis or during disease progression. These samples were subjected to panel NGS, encompassing 139, 168, 425 or 437 cancer-associated genes. In this study, we focused on analyzing 67 genes that were consistently evaluated across all four panels7,8. The primary aim of the study was to describe the clinical and genetic characteristics of these patients and to examine the impact of various treatment strategies on their prognosis. Clinical data were sourced from the electronic medical records at Zhejiang Cancer Hospital. Inclusion criteria were as follows: (I) patients histologically or cytologically diagnosed with NSCLC; (II) patients with a history of treatment with TKIs for driver mutations recommended by national comprehensive cancer network(NCCN) guidelines (e.g., EGFR, ALK, ROS1) prior to the detection of BRAF alterations; (III) patients who had new BRAF variations detected by NGS after developing resistance to TKIs. Exclusion criteria were as follows: (I) patients with mixed small cell lung cancer components; (II) patients with concurrent BRAF variations at the initial diagnosis of EGFR/ALK/ROS1 mutations; (III) patients with incomplete survival follow-up information. This study was approved by the Ethics Committee of Zhejiang Cancer Hospital (approval number IRB-2020–324). All participants signed informed consent forms, and the study adhered to the ethical principles of the Declaration of Helsinki.
Treatment and assessments
The definitive treatment strategies utilized in this study are as follows. The first treatment strategy refers to combined targeted therapy incorporating TKIs and/or BRAF inhibitors and/or MEK inhibitors, such as the third-generation TKIs (osimertinib or furmonertinib) combined with dabrafenib, with or without trametinib. The second treatment strategy involves the continuation of current TKIs combined with local treatment (stereotactic body radiotherapy) for patients with oligo-progression, specifically using the third-generation TKIs (osimertinib or furmonertinib) or the second-generation TKIs (afatinib).The third treatment strategy refers to chemotherapy-based regimens such as pemetrexed plus carboplatin plus bevacizumab or PD-1 inhibitor. The fourth treatment strategy involves the continuation of single-agent TKIs along the original ALK or EGFR signaling pathway, specifically including the first-generation TKIs (crizotinib or icotinib) or the third-generation TKIs (osimertinib). The above-mentioned medications were derived from the electronic medical records of 27 patients. Using the Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1, disease severity was assessed with the Eastern Cooperative Oncology Group (ECOG) performance status. Progression-free survival (PFS) was defined as the time from the start of treatment to disease progression or death from any cause, whichever occurred first. Overall survival (OS) was defined as the time from the confirmation of BRAF variations to death due to any cause. Global OS was defined as the time from the initial diagnosis to death from any cause.
Statistical analysis
Categorical variables were compared using the chi-square test or Fisher's exact test in this study. The non-parametric test used was the rank-sum test. A preliminary Cox proportional hazards analysis indicated that the model violated the proportional hazards assumption. Trends in Schoenfeld residual plots also indicate changes in covariates over time. Consequently, we employed a Weibull-based accelerated failure time (AFT) model to estimate the time ratio (TR) for global OS and its 95% confidence interval (CI). In the multivariate AFT model, results were reported as TR rather than hazard ratios (HR). A TR greater than 1 indicates slower progression to endpoints such as death or disease progression, while a TR less than 1 signifies accelerated time to these endpoints. Survival among groups was analyzed using Kaplan–Meier curves and the log-rank test. Statistical significance was defined as a p-value of less than 0.05. All statistical and graphical analyses were conducted using R software version 4.3.3.
Results
Clinical characteristics of driver-positive NSCLC with concomitant BRAF variations
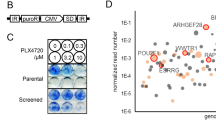
We retrospectively identified 27 cases of advanced NSCLC with secondary BRAF variations. Baseline characteristics of the patients are listed in Table 1. The median time from initial targeted therapy to acquisition of BRAF variations was 28 months (95% CI: 19–32 months). The three BRAF subtypes (V600E, Non-V600E, and fusion) appeared at similar times: 25, 30.5, and 32 months, respectively (p = 0.47; Fig. 1A). All patients exhibited BRAF mutations upon disease progression. BRAF variations occurred in 55.6% (15/27) of patients following the failure of second-line or later treatments. Clinically significant BRAF mutations or fusions were observed in 23 patients (Supplementary Table 1). The clinical relevance of BRAF mutations or fusions aligns with the entries in OncoKB (https://www.oncokb.org/), a database of human genetic variants that is acknowledged by the Food and Drug Administration (FDA) and accessible to the public9. Variants in Tier I and II are recognized as having clinical importance10. Prior to the detection of BRAF mutations, the most common treatment regimen involved initially using gefitinib, erlotinib or icotinib, followed by a switch to osimertinib upon developing resistance. This approach accounted for 44.4% in our study (Fig. 1B). Among all patients, 55.6% (15/27) developed BRAF mutations after treatment with osimertinib, including four cases where third-generation TKIs were used as first-line therapy. BRAF variants include V600E (48.2%, 13/27), Non-V600E (37%, 10/27), and fusions (14.8%, 4/27). Of these, 82.6% (19/23) of the mutations occurred in the tyrosine kinase ___domain (Fig. 1C).The median global OS for all patients was 41 months (95% CI: 0.36–0.75). The median OS from the detection of BRAF mutations for all patients was 7 months (95% CI: 0.35–0.74). Patients with BRAF fusions had a longer median global OS compared to those with V600E and Non-V600E mutations, at 61 months, 34 months, and 49 months, respectively (p = 0.13). Median OS for patients with BRAF fusions was also longer, at 28 months compared to 11 months and 6.5 months for V600E and Non-V600E mutations, respectively (p = 0.28).The median time from diagnosis to last follow-up for each patient was 42 months.
(A)Time from initial diagnosis to acquisition of BRAF variants.(B) The TKIs sequences before acquisition of BRAF variants: 1, 2, and 3 indicate the first-generation TKIs, second-generation TKIs, and third-generation TKIs, respectively.(C) the distribution of BRAF mutations.(D) The mutation counts in the overall population and patients of different BRAF subtypes.
Molecular Characteristics of Driver-Positive NSCLC with Concomitant BRAF Variations
A total of 27 patients underwent NGS testing before the emergence of BRAF Variations (Supplementary Fig. 1). With the acquisition of BRAF Variations, the frequency of TP53 and LRP1B mutations increased. The median Variations count for all patients with acquired BRAF Variations was 6 (95% CI: 5–8; Fig. 1D), with significant differences observed between variant types (V600E vs. Non-V600E vs. Fusion: 5,8.5, 7; p = 0.047).Beyond BRAF variants, variations in TP53, T790M, LRP1B, DNMT3A, RB1, CDKN2, AKT, KRAS, and NTRK were observed with frequencies exceeding 5% (Fig. 2). Consequently, frequencies of variations in the cell cycle/p53 pathway (TP53, RB1, MYC, CDKN2A), EGFR downstream pathway (KRAS), and bypass pathways (MET, NTRK) also exceeded 5%. In the chi-square analysis, TP53 mutations were significantly enriched in patients with V600E mutations (p = 0.03; Supplementary Table 2), while other mutations showed no significant association with BRAF type.
Targeted combination therapy can prolong survival outcomes
We identified 27 patients who developed secondary BRAF variations following TKIs treatment resistance and analyzed the impact of various treatment strategies on their survival (Fig. 3A). Treatment distributions: chemotherapy-based regimens group (37%, 10/27); targeted monotherapy group (29.6%, 8/27); combined targeted therapy group (18.5%, 5/27); combined local treatment group (14.9%, 4/27). Objective response rate (ORR) of the different treatment groups was as follows: chemotherapy-based regimens group, 30%; combined targeted therapy group, 40%; targeted monotherapy group, 12.5%; combined local treatment group, 0%. Disease control rate (DCR) of the different treatment groups was as follows: chemotherapy-based regimens group, 60%; combined targeted therapy group, 60%; targeted monotherapy group, 37.5%; combined local treatment group, 100%. Median PFS of the different treatment groups was as follows: chemotherapy-based regimens group, 4 months; combined targeted therapy group, 3 months; targeted monotherapy group, 1.5 months; combined local treatment group, 8 months (Supplementary Fig. 2). Notably, PFS was significantly longer in the combined local treatment group compared to the targeted monotherapy group (p = 0.024). Median global OS (Fig. 3B) of the different treatment groups was as follows: chemotherapy-based regimens group, 45 months; combined targeted therapy group, 59 months; targeted monotherapy group, 36 months; Across median PFS and global OS, a consistent finding emerges: the targeted monotherapy group has the poorest prognosis, while prognosis significantly improves in the combined targeted therapy group and the combined local treatment group. Similar trends were confirmed by the multivariate AFT model Combined targeted therapy (TR = 1.96; [1.43, 2.68]; p < 0.001) and combined local therapy (TR = 2.42; [1.71, 3.44]; p < 0.001) significantly extended global OS compared to chemotherapy-based regimens alone (Supplementary Table 3). However, Continuing the original signaling pathway targeted monotherapy significantly reduced global OS (TR = 0.76; [0.59, 0.98]; p = 0.034) and PFS (TR = 0.28; [0.13, 0.61]; p = 0.002). No significant differences in PFS were observed for the other covariates in the multivariate AFT analysis (Supplementary Table 4).Additionally, previous treatment lines (≥ 2 vs 1: TR = 0.70; [0.50, 0.98]; p = 0.035), TP53 mutations (TR = 1.63; [1.22, 2.18]; p = 0.001), and the duration of targeted therapy prior to secondary BRAF variations (TR = 1.01; [1.00, 1.01]; p = 0.036) were significantly associated with global OS.
(A) The efficacies of various treatment strategies for patients with secondary BRAF variants following resistance to prior TKIs. Chemotherapy-based regimens are shown by the red bar; Multi-target combination therapy is indicated by the blue bar. Continuing current targeted therapy is indicated by the green bar. Targeted therapy combined with local therapy is indicated by the purple bar. 1 represents the use of first-generation targeted drugs. 2 represents the use of second-generation targeted drugs. 3 represents the use of third-generation targeted drugs.1/2 is indicated by the orange bar. 3 is indicated by the yellow bar. PD, progressive disease; PR, partial response; SD, stable disease; The texts on the side of the figure represent types of BRAF variations. (B) Kaplan–Meier survival curves and At-Risk Table for global OS after treatment for NSCLC patients with secondary BRAF alterations by group.
Discussion
Understanding of the clinical characteristics, subsequent treatment options, and efficacy for NSCLC patients with BRAF variations following TKIs resistance remains limited, primarily due to the low incidence of BRAF variations in NSCLC. Fang et al. conducted a retrospective study on the molecular characteristics and response to combined targeted therapy in NSCLC patients with BRAF variations following EGFR TKIs resistance. In this study, only 4.3% (71/1637) of NSCLC patients resistant to EGFR TKIs exhibited acquired BRAF variations4. In our study, 74.1% of the advanced NSCLC patients with secondary BRAF variations were Non-smokers, and 63% were female. Research indicates a correlation between BRAF mutations and smoking in NSCLC. A study on the clinical characteristics of advanced lung adenocarcinoma with primary BRAF mutations found that these mutations were more common in current or former smokers compared to other mutation types: BRAF vs EGFR/ALK/other mutations, 82% vs 36%/39%/49%11. However, the situation is reversed in patients with acquired BRAF variations. Marchetti et al. noted that BRAF mutations predominantly occur in females and Non-smokers12. Ding et al.'s study indicates that in China, BRAF mutations are more prevalent among Non-smokers13. Furthermore, Sheikine et al. conducted a study on BRAF variation characteristics in advanced lung cancer, finding that 78.5% (788/1004) occurred in adenocarcinoma patients, 3.2% (32/1004) in squamous cell carcinoma, and the remaining 18.3% in other types of NSCLC14. In our study, all 27 patients had the adenocarcinoma subtype, reflecting that acquired BRAF mutations predominantly occur in adenocarcinomas. These clinical characteristics are consistent with aforementioned studies and other real-world cases. Notably, our data reveal that 85.2% (23/27) of patients developed secondary BRAF variations after treatment with first- or second-generation TKIs. Although Fang et al. reported that the incidence of secondary BRAF variations was 3% among patients treated with first- or second-generation TKIs and 7% among those treated with osimertinib4. However, osimertinib has now become the standard first-line treatment for advanced EGFR-mutated NSCLC15. Therefore, confirming whether acquired BRAF mutations are more prevalent in patients treated with third-generation TKIs necessitates broader data statistics and deeper molecular studies.
Although the incidence of secondary BRAF variations is low (4.3%)4, the co-mutation rate in BRAF-mutated NSCLC is relatively high (14%-16%)11,12,13 Peng et al. provided a detailed report on co-mutations of various BRAF subtypes with EGFR, including V600E and Non-V600E mutations. In addition, they analyzed the association of BRAF subtypes with EGFR mutant subtypes and found that NSCLC patients with EGFR exon 19 deletion were more likely to have acquired BRAF fusions (P = 0.015)16. However, in our samples and in the study by Wei et al., no significant associations were observed between different BRAF subtypes and primary driver genes. In our study, all patients with acquired BRAF variations also exhibited co-mutations in other genes, with TP53 mutations being the most common (81%). This finding is closely aligned with the results reported by Fang et al. (74.6%) and Wei et al. (75.4%). However, there are differences between studies: Fang et al. found that aside from EGFR and TP53, the most common co-mutations among 71 patients with acquired BRAF mutations were in RB1 and MET. Wei et al. additionally identified PIK3CA as a common co-mutation, along with RB1 and MET. They also reported some benign co-mutations that appeared to have a minimal impact on subsequent treatments4,17. These differences may arise from variations in our study populations: our cohort included patients with ALK and ROS1 rearrangements, whereas their cohorts were limited to those with EGFR mutations. Furthermore, due to limited sample sizes, the characteristics of co-mutations and their impacts on treatment require analysis in larger samples. Overall, our statistical analysis of the clinical characteristics and genetic features of these patients partially concurs with existing literature.
In a preclinical study, Class I BRAF mutants (BRAF V600) demonstrated sensitivity to FDA-approved inhibitors such as dabrafenib and vemurafenib (Fig. 4). Conversely, Class II and III mutants, which utilize RAF dimer signaling, are theoretically resistant to clinically approved monomeric BRAF inhibitors5,6. However, sensitivity to BRAF inhibitors in BRAF V600E mutants was inconsistent, as shown in Sun et al.'s case studies with vemurafenib and Shi et al.'s in vitro research18,19. In our study, secondary BRAF V600E and Non-V600 mutation carriers exhibited distinct genetic characteristics. Although these differences were mostly not statistically significant, the genetic background of the BRAF V600E group was relatively more homogenous. Thus, BRAF V600E may confer a high level of resistance to TKIs. Furthermore, we found that TP53 mutations were more likely to be enriched in patients with the BRAF V600 variant (p = 0.03). This may explain the ineffective response to BRAF inhibitors in some patients with the BRAF V600 mutation. However, Wei et al. found that RB1 and TP53 mutations were more common in patients with BRAF Non-V600 mutations (p < 0.04, p < 0.09)17. Therefore, larger-scale, multicenter studies are needed to further validate the genetic characteristics of NSCLC patients with secondary BRAF mutations. Nevertheless, BRAF V600 mutations were the most common acquired mutations in both our study and that of Wei et al. These characteristics underscore that combined targeted therapy or pan-RAF inhibitors may be the optimal choice for these patients.
(A) Signaling downstream affected by various BRAF mutants. (a). Class I mutations activate MEK/ERK via monomeric BRAF with sustained signaling. (b). Class II mutants form dimers through BRAF and/or CRAF, activating the MAPK pathway. (c). Class III BRAF mutants display minimal or no kinase activity. Despite this, they increase interactions with RAS, leading to the activation of subsequent signaling pathway via dimer formation. (B) BRAF gene fusions lead to the loss of serine/threonine kinase domains while preserving the conserved region 3 (CR3) of the N-terminal ___domain. The absence of the N-terminal structural domains CR1 and CR2 is often offset by the presence of fusion partners, such as KIAA 1549. Truncation of the CR1 auto-inhibitory ___domain leads to the formation of constitutively active BRAF dimers and subsequently activate downstream signalling pathways.
Besides comparing characteristics of NSCLC patients with secondary BRAF variations, our study identified duration of targeted therapy and number of treatment lines as independent predictors of global OS using a multivariate AFT model. Later occurrence of BRAF mutations was associated with a favorable prognosis for global OS. A higher number of treatment lines negatively predicted global OS. Additionally, continuing the original signaling pathway targeted monotherapy was negatively associated with global OS. In contrast, both the combined targeted therapy group and the combined local therapy group (for patients of oligo-progression) showed positive correlations. Our findings are consistent with other real-world case reports and in vitro studies, indicating that combination targeted therapy regimens can prolong survival. According to existing case reports and in vitro studies (Table 2), chemotherapy, immunotherapy, and continued monotherapy targeting the original pathway had poor efficacy, with 0% of DCR18,19,23,24,27,32,34. However, the combination therapies showed improved outcomes. In dual-targeted therapy, DCR was 85.7% (6/7) and ORR was 42.9% (3/7)18,21,22,28,33. In triple-targeted therapy, excluding one case with unreported efficacy, DCR reached 100% and ORR was 66.7% (6/9)20,21,26,27,28,29,35. Despite case reports indicating poor outcomes for chemotherapy-based regimens, research by Wei et al. on patients with advanced EGFR-mutated NSCLC carrying acquired BRAF variations demonstrated an ORR of 14.3%, a DCR of 57.1%, and a median PFS of 3.5 months. In our study, the chemotherapy-based regimens group also achieved an ORR of 30%, a DCR of 60%, and a median PFS of 4 months. However, patients continuing with original pathway targeted monotherapy (TR = 0.76; p = 0.034) had significantly shorter survival, only 76% of the chemotherapy-based regimens group. These findings suggest that continuing with monotherapy targeting the original pathway is less effective than chemotherapy-based regimens. chemotherapy-based regimen remain a viable treatment option.
In the multivariate AFT model, combination targeted therapy (TR = 1.96; p < 0.001) and targeted monotherapy combined with local therapy (TR = 2.42; p < 0.001) had superior treatment outcomes. Their global OS were 1.96 and 2.42 times those of the chemotherapy-based regimens group, respectively. Current research also indicates that localized treatment can improve survival for patients with oligo-progression in advanced NSCLC36. Therefore, based on our study and existing researches, we recommend prioritizing combination therapy with TKIs and/or BRAF inhibitors and/or MEK inhibitors over monotherapy targeting the original pathway for NSCLC patients with TKIs-resistant secondary BRAF variations. Although the multivariable AFT model showed no significant associations between covariates and PFS, the Kaplan–Meier curves revealed significant differences in PFS between treatment regimens (P = 0.018). Log-rank tests showed that PFS for patients receiving localized treatment combined with original targeting was significantly better than for those receiving monotherapy targeting the original pathway alone (p = 0.024), with no significant differences in PFS among other treatment groups. Therefore, for patients with oligo-progression, we recommend continuing targeted monotherapy along the original signaling pathway and combining it with local therapy. Although TP53 co-mutations are generally associated with poorer clinical outcomes, our study found that patients carrying TP53 mutations exhibited better prognosis (TR = 1.63; p = 0.001)37. We believe this outcome may be due to the majority of patients undergoing combined targeted and localized treatment (77.8%) carrying TP53 co-mutations and demonstrating good efficacy, compounded by a limited sample size. Additionally, our findings suggest that shorter durations of targeted therapy prior to the emergence of BRAF variations (median onset time: 28 months) are associated with shorter global OS (TR = 1.01; p = 0.036). Therefore, considering these findings, continued development of new TKIs to extend disease control duration, delay the onset of secondary BRAF variations, and further investigate treatment strategies for NSCLC patients with secondary BRAF variations holds significant potential.
Our study has several limitations. Firstly, since we used only samples from a single institution at our center and the sample size was limited, there may be sampling bias. Secondly, the study did not differentiate the efficacy between dual-targeted and triple-targeted combination therapies, and the safety of these therapies still requires further validation. Consequently, due to the lack of a clear consensus, it is currently impossible to provide final recommendations for the use of combined targeted therapy in NSCLC patients with resistant secondary BRAF variations. Thirdly, constrained by the sample size, our analysis included five patients with acquired BRAF variations of unclear clinical significance. Although these five patients did not receive combined targeted therapy, limiting the analysis to those with clinically significant acquired BRAF variations yielded more reliable comparative results. Fourthly, as this study was retrospective, the conclusions can only suggest associations, not establish causality.
In conclusion, our findings suggest that combination targeted therapy may provide survival benefits to NSCLC patients with BRAF variations arising after resistance to TKIs. Further exploration through larger, multicenter prospective studies and clinical trials is warranted.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- TKIs:
-
Tyrosine kinase inhibitors
- AFT:
-
Accelerated failure time
- TR:
-
Time ratio
- PFS:
-
Progression-free survival
- OS:
-
Overall survival
- CI:
-
Confidence interval
- PR:
-
Partial response
- SD:
-
Stable disease
- PD:
-
Progressive disease
- ORR:
-
Objective response rate
- DCR:
-
Disease control rate
- NCCN:
-
National comprehensive cancer network
- FDA:
-
Food and drug administration
References
Ho, C.-C. et al. Acquired BRAF V600E mutation as resistant mechanism after treatment with osimertinib. J. Thorac. Oncol. 12(3), 567–572. https://doi.org/10.1016/j.jtho.2016.11.2231 (2017).
Mu, Y. et al. Acquired resistance to osimertinib in patients with non-small-cell lung cancer: Mechanisms and clinical outcomes. J. Cancer Res. Clin. Oncol. 146(9), 2427–2433. https://doi.org/10.1007/s00432-020-03239-1 (2020).
Westover, D., Zugazagoitia, J., Cho, B. C., Lovly, C. M. & Paz-Ares, L. Mechanisms of acquired resistance to first- and second-generation EGFR tyrosine kinase inhibitors. Annal. Oncol. https://doi.org/10.1093/annonc/mdx703 (2018).
Fang, W. et al. Molecular characteristics of BRAF mutations in EGFR mutant NSCLC after progression on EGFR TKIs and response to combination targeted therapy. J. Thoracic Oncol. https://doi.org/10.1016/j.jtho.2021.01.1147 (2021).
Dankner, M., Rose, A. A. N., Rajkumar, S., Siegel, P. M. & Watson, I. R. Classifying BRAF alterations in cancer: New rational therapeutic strategies for actionable mutations. https://doi.org/10.1038/s41388-018-0171-x.
Yao, Z. et al. Tumours with class 3 BRAF mutants are sensitive to the inhibition of activated RAS. Nature 548(7666), 234–238. https://doi.org/10.1038/nature23291 (2017).
Li, Y. S. et al. Unique genetic profiles from cerebrospinal fluid cell-free DNA in leptomeningeal metastases of EGFR-mutant non-small-cell lung cancer: A new medium of liquid biopsy. Ann. Oncol. 29(4), 945–952. https://doi.org/10.1093/annonc/mdy009 (2018).
Zhang, Y.-C. et al. Analysis of resistance mechanisms to abivertinib, a third-generation EGFR tyrosine kinase inhibitor, in patients with EGFR T790M-positive non-small cell lung cancer from a phase I trial. EBioMedicine 43, 180–187. https://doi.org/10.1016/j.ebiom.2019.04.030 (2019).
Chakravarty, D. et al. OncoKB: A precision oncology knowledge base. JCO Precision Oncol. 1, 1–16. https://doi.org/10.1200/PO.17.00011 (2017).
Li, M. M. et al. Standards and guidelines for the interpretation and reporting of sequence variants in cancer: A joint consensus recommendation of the association for molecular pathology, American society of clinical oncology, and College of American pathologists. J. Mol. Diagn. 19, 4–23. https://doi.org/10.1016/j.jmoldx.2016.10.002 (2017).
Villaruz, L. C. et al. Clinicopathologic features and outcomes of patients with lung adenocarcinomas harboring BRAF mutations in the LUng CAncer Mutation Consortium. Cancer 121(3), 448–456. https://doi.org/10.1002/cncr.29042 (2015).
Marchetti, A. et al. Clinical features and outcome of patients with non–small-cell lung cancer harboring BRAF mutations. JCO 29(26), 3574–3579. https://doi.org/10.1200/JCO.2011.35.9638 (2011).
Ding, X. et al. Clinicopathologic characteristics and outcomes of Chinese patients with non-small-cell lung cancer and BRAF mutation. Cancer Med. 6(3), 555–562. https://doi.org/10.1002/cam4.1014 (2017).
Sheikine, Y. et al. BRAF in lung cancers: Analysis of patient cases reveals recurrent BRAF mutations, fusions, kinase duplications, and concurrent alterations. JCO Precis. Oncol. 2, 1–15. https://doi.org/10.1200/PO.17.00172 (2018).
Soria, J.-C. et al. Osimertinib in untreated EGFR-mutated advanced non-small-cell lung cancer. N. Engl. J. Med. 378(2), 113–125. https://doi.org/10.1056/NEJMoa1713137 (2018).
Peng, P. et al. Co-mutations of epidermal growth factor receptor and BRAF in Chinese non-small cell lung cancer patients. Ann. Transl. Med. 9(16), 1321–1321. https://doi.org/10.21037/atm-21-3570 (2021).
Wei, X.-W. et al. Characteristics of and treatment strategies for advanced EGFR-mutant NSCLC with concomitant BRAF variations. JTO Clin. Res. Rep. https://doi.org/10.1016/j.jtocrr.2022.100348 (2022).
Sun, M. et al. Combined targeting of EGFR and BRAF triggers regression of osimertinib resistance by using osimertinib and vemurafenib concurrently in a patient with heterogeneity between different lesions. Thoracic Cancer 13(3), 514–516. https://doi.org/10.1111/1759-7714.14295 (2022).
Shi, R. et al. BRAF V600E mutation and MET amplification as resistance pathways of the second-generation anaplastic lymphoma kinase (ALK) inhibitor alectinib in lung cancer. Lung Cancer 146, 78–85. https://doi.org/10.1016/j.lungcan.2020.05.018 (2020).
Vojnic, M. et al. Acquired BRAF rrearrangements induce secondary resistance to EGFR therapy in EGFR-mutated lung cancers. J. Thor. Oncol. 14(5), 802–815. https://doi.org/10.1016/j.jtho.2018.12.038 (2019).
Kong, W.-M., Guo, Y.-J., Ma, J. & Shi, C. BTN2A1-BRAF fusion may be a novel mechanism of resistance to osimertinib in lung adenocarcinoma: A case report. Transl. Cancer Res. 12(1), 186–193. https://doi.org/10.21037/tcr-22-2060 (2023).
Kian, W. et al. Overcoming CEP85L-ROS1, MKRN1-BRAF and MET amplification as rare, acquired resistance mutations to osimertinib. Front. Oncol. 13, 1124949. https://doi.org/10.3389/fonc.2023.1124949 (2023).
Sui, A. et al. BRAF V600E mutation as a novel mechanism of acquired resistance to ALK inhibition in ALK-rearranged lung adenocarcinoma: A case report. Medicine https://doi.org/10.1097/MD.0000000000024917 (2021).
Ren, S. et al. Crizotinib resistance conferred by BRAF V600E mutation in non-small cell lung cancer harboring an oncogenic ROS1 fusion. Cancer Treat. Res. Commun. https://doi.org/10.1016/j.ctarc.2021.100377 (2021).
Giustini, N. P. et al. Resistance to EGFR tyrosine kinase inhibitor therapy in non–small-cell lung cancer via newly acquired targetable oncogenic driver alterations with an emphasis on BRAF: Case series and literature review of treatment. JCO Precisio. Oncolog. https://doi.org/10.1200/PO.21.00551 (2022).
Liu, Y. et al. Acquired BRAF N581S mutation mediated resistance to gefitinib and responded to dabrafenib plus trametinib. Lung Cancer 146, 355–357. https://doi.org/10.1016/j.lungcan.2020.06.004 (2020).
Mauclet, C., Collard, P., Ghaye, B., Hoton, D. & Nana, F. A. Tumor response to EGFR/BRAF/MEK co-inhibition in a patient with EGFR mutated lung adenocarcinoma developing a BRAFV600 mutation as an acquired resistance mechanism. Lung Cancer. 159, 42–44. https://doi.org/10.1016/j.lungcan.2021.06.025 (2021).
Li, J., Wang, Q., Ge, J., Tian, Y. & Yao, W. BRAF V600E mediates crizotinib resistance and responds to dabrafenib and trametinib in a ROS1-rearranged non-small cell lung cancer: A case report. Oncol. 26(12), e2115–e2119. https://doi.org/10.1002/onco.13979 (2021).
Zhou, F., Zhao, W., Chen, X., Zhang, J. & Zhou, C. Response to the combination of dabrafenib, trametinib and osimertinib in a patient with EGFR-mutant NSCLC harboring an acquired BRAFV600E mutation. Lung Cancer 139, 219–220. https://doi.org/10.1016/j.lungcan.2019.10.014 (2020).
Zeng, R. et al. EGFR/BRAF/MEK Co-Inhibition for EGFR-Mutated Lung Adenocarcinoma Patients with an Acquired BRAFV600E Mutation: A Case Report and Review of Literature. CDR 2021. https://doi.org/10.20517/cdr.2021.98 (2021).
Valet, O. et al. Response to the combination of osimertinib, dabrafenib, and trametinib in leptomeningitis from EGFR-mutant NSCLC with acquired BRAF V600E mutation: A case report. JTO Clin. Res. Rep. https://doi.org/10.1016/j.jtocrr.2021.100192 (2021).
Li, D. et al. Combined lorlatinib, dabrafenib, and trametinib treatment for ROS1-rearranged advanced non-small-cell lung cancer with a lorlatinib-induced BRAF V600E mutation: A case report. CMAR 14, 3175–3179. https://doi.org/10.2147/CMAR.S387211 (2022).
Tsai, C. J. et al. Standard-of-care systemic therapy with or without stereotactic body radiotherapy in patients with oligoprogressive breast cancer or non-small-cell lung cancer (consolidative use of radiotherapy to block [CURB] oligoprogression): An open-label, randomised, controlled, phase 2 study. Lancet, 403(10422), 171–182. https://doi.org/10.1016/S0140-6736(23)01857-3 (2024).
Labbé, C. et al. Prognostic and predictive effects of TP53 co-mutation in patients with EGFR-mutated non-small cell lung cancer (NSCLC). Lung Cancer 111, 23–29. https://doi.org/10.1016/j.lungcan.2017.06.014 (2017).
Li, S., Lin, X., Sun, S., Li, S. & Zhou, C. Response to osimertinib plus trametinib in a heavily treated epidermal growth factor receptor (EGFR)-positive NSCLC harboring a rare, acquired rapidly accelerated fibrosarcoma B-Type (BRAF) p.D594N mutation: A case report. Anti-Cancer Drugs 33(9), 963–965 (2022).
Bearz, A., De Carlo, E., Doliana, R. & Schiappacassi, M. Acquired BRAF V600E mutation as resistant mechanism after treatment with third-generation EGFR tyrosine kinase inhibitor. J. Thoracic Oncol. 12(11), e181–e182. https://doi.org/10.1016/j.jtho.2017.07.017 (2017).
Dagogo-Jack, I. Durable response to Dabrafenib combined with trametinib in a patient with NSCLC harboring a BRAF G469A mutation. J. Thoracic Oncol. 15(10), e174–e176. https://doi.org/10.1016/j.jtho.2020.07.007 (2020).
Acknowledgements
The authors thank the patients and their families for participating in this study.
Funding
This study was supported by the Natural Scientific Foundation of Zhejiang Province, China (Grant No.LTGY23H160007).
Author information
Authors and Affiliations
Contributions
DuJiang Liu: Visualization, Writing—original draft, and Writing—review & editing. KaiBo Ding: Validation, Writing—original draft. KaiLai Ying: Methodology. ZhongSheng Peng: Software. Xinyue Li: Investigation. Yang Pan: Investigation. XuanHong Jin: Formal analysis. YanJun Xu: Conceptualization, Data curation, Funding acquisition, Project administration, Resources; Supervision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Zhejiang Cancer Hospital (approval number IRB-2020–324). All participants signed informed consent forms, and the study adhered to the ethical principles of the Declaration of Helsinki.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, D., Ding, K., Yin, K. et al. A real world analysis of secondary BRAF variations after targeted therapy resistance in driver gene positive NSCLC. Sci Rep 14, 20302 (2024). https://doi.org/10.1038/s41598-024-71143-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-71143-6