Abstract
Bone defects pose a significant risk to human health. Medical polyetheretherketone (PEEK) is an excellent implant material for bone defect repair, but it faces the challenge of bone osteoconduction and osseointegration. Osteoconduction describes the process by which bone grows on the surface of the implant, while osseointegration is the stable anchoring of the implant achieved by direct contact between the bone and the implant. Bone defects repair depends on the implant’s three-dimensional spatial structure, including pore size, porosity, and interconnections to a great extent. However, it is challenging to fabricate the porous structures to meet specific requirements and to characterize them without causing damage. In this study, we designed and fabricated sandwich-like PEEK implants mimicking the three-layer structures of the skull, whose defects imposes a significant burden on young adulthood and paediatric populations, and performed in-line phase-contrast synchrotron X-ray microtomography to non-destructively investigate the internal porous microstructures. The sandwich-like three-layer microstructure, comprising a dense layer, a loose layer and a dense layer in succession, exhibits structural similarity to that in a natural skull. This work demonstrated the fabrication of the sandwich-like PEEK implant that could potentially enhance osteoconduction and osseointegration. Furthermore, the interior structures and residual porogen sodium chloride particles were observed within the PEEK implant, which cannot be realized by other microscopic methods without destroying the sample. It highlights the advantages and potential of using synchrotron X-ray microtomography to analyze the structure of biomedical materials. This study provides theoretical guidance for the further design and fabrication of PEEK bone repair materials and will advance the clinical application of innovative bioactive bone repair materials.
Similar content being viewed by others
Introduction
Bone tissue defects threaten human health and life seriously1,2. Skull defects, for example, are a global health concern often resulting from road accidents, tumor resections, and vascular injuries3,4,5. These defects can lead to both physical and psychological distress, particularly in young adults and children6,7. Therefore, there is an urgent need to develop bone repair materials to improve people’s health and quality of life. Various materials, including metal implants, ceramics and bioactive glass, have been developed and used in clinical practice5,8,9,10,11.
Among these bone repair materials, medical polyetheretherketone (PEEK) has great potentials to meet the critical clinical needs12,13. PEEK is a high-performance thermoplastic polymer with mechanical properties, chemical stability, biocompatibility, and radiation transmittance. It has been widely used in biomedical fields such as intercolumnar fusion, hip repair, and skull reconstruction14,15,16. Medical PEEK is considered as the best long-term bone graft material17. However, PEEK shows poor osteoconduction and osseointegration16. When PEEK is implanted into an organism, fibrous tissue grows around it. No new bone tissue grows. The new implant cannot be tightly integrated with the surrounding bone tissue, leading to bone loosening and nonunion14,18,19. Improving the osteoconduction and osseointegration of PEEK is an urgent issue that needs to be addressed.
To develop bioactive PEEK bone repair materials, it is necessary to explore material modification methods based on the bone repair mechanism1,13,20,21,22. Bone repair materials are used as implants during bone regeneration, providing a three-dimensional microenvironment for the adhesion, proliferation, and differentiation of osteogenic-related cells23,24. This structure guides the growth and formation of blood vessels and other related tissues25,26. It also acts as a carrier of active protein factors and other drugs to regulate the formation of new bone27. Bone repair using conduction materials depends on their three-dimensional spatial structure, including pore size, porosity, and inter-hole communication1,26,28. PEEK engineering for bone repair involves extrusion molding and 3D printing to construct porous materials with three-dimensional microstructures15,29,30. These structures can be built on the surface or inside the material, improving the osteoconductivity of PEEK and achieving effective bone repair.
Modifying the microstructure of PEEK to imitate that of natural bone is an important approach to enhancing its biological activity13,15,16,30,31. However, the microstructure and regulatory mechanisms of PEEK are not fully understood. This challenge stems from the complexity inherent in biomimetic bone repair materials, which are characterized by multi-scale structures31,32. Pore structures range from hundreds of microns to sub-micron and nanometer scales33,34. Employing innovative microscopic imaging techniques is essential. This understanding will help clarify microstructure formation mechanisms and aid in developing improved bone repair materials.
X-ray tomography is an invaluable tool for non-destructive, three-dimensional structural analysis of biomedical materials35,36,37,38,39. This technique allows for multiscale resolutions, without damaging to the samples due to the high penetration power and short wavelength of X-rays37,38,40,41. It has been employed to investigate the microstructure of bone repair materials and dental materials35,42,43,44,45,46. X-rays allow imaging of bone repair materials of various sizes without sectioning the sample, unlike electron microscopy47,48,49,50. Furthermore, X-rays have a shorter wavelength than visible light, allowing for higher spatial resolution imaging than optical microscopy. Synchrotron radiation light sources have expanded the applications of X-ray microscopy in material science, biology, and industry51,52,53,54,55,56. Various phase-contrast imaging techniques, such as in-line phase-contrast imaging, interferometry, grating-based imaging, and analyzer-based imaging, have been developed to enhance image contrast57,58. In-line phase-contrast X-ray imaging is suitable for various applications because of its simplicity in the experimental setup, in which no optical elements are used other than the coherent X-ray beam59,60. A coherent beam at an appropriate sample-to-detector distance provides phase-contrast information without extra optical components, such as gratings for grating based X-ray phase contrast imaging, diffuser for speckle-based phase contrast imaging and analyzer crystals for analyzer-based phase contrast imaging36,40,41,51.
In this study, we designed and fabricated a sandwich-like PEEK implant mimicking the three-layer structure of the skull to improve the osteoconduction and osseointegration, and performed in-line phase-contrast synchrotron X-ray microtomography to non-destructively investigate the internal porous microstructures. The three-layer structures are sandwich-like structures, following the sequence of dense layer, loose layer, and dense layer. The interior porous microstructures of the implant were successfully observed. The middle layer’s microstructure resembles the cancellous bone of a natural skull, displaying typical connected pore structures. This study provides theoretical guidance for the further design and fabrication of PEEK bone repair materials and highlights the advantages of using synchrotron X-ray microtomography in biomedical field.
Experimental
Sample preparation
Analytical grade polyether ether ketone (PEEK) powder was sourced from Jilin Zhongyan High Performance Plastic Co., Ltd for our study. As depicted in Fig. 1, porous PEEK samples with three distinct layers were fabricated using a salt fractionation technique12. The size of the sodium chloride used was 500–600 μm. The process was repeated multiple times to ensure the reliability and consistency of this approach. Initially, the dense layer was formed from PEEK powder. The loose layer was created using a blend of PEEK and sodium chloride powders in a volume ratio of 1:9. Subsequently, the powder mixture was compressed layer by layer at a pressure of 20 MPa which is a balance between the consolidation of the material and the retention of the desired porous structure, which is critical for the performance of the implants, following the sequence of dense layer, loose layer, and dense layer. The resulting sheet was then fused and heated at 400℃ for 2 h. Afterward, the blank was rapidly transferred to a press machine where it underwent repeated compression at 20 MPa for 30 min before being positioned on the demolding seat for separation. Finally, the entire template, containing both PEEK and sodium chloride, was soaked in deionized water at 60℃ for 48 h to eliminate the sodium chloride pore-forming agent. The sample was then dried at 60℃ for 6 h. For each of the subsequent tests, a minimum of three samples were meticulously prepared to ensure the robustness and reproducibility of our findings.
Sample characterization
The surface morphology of the samples was analyzed using a field emission scanning electron microscope (FE-SEM, JSM-7610 F) equipped with an X-ray energy dispersive spectrometer (EDS, X-Max) at an accelerating voltage of 15 kV. The phase composition of the samples was determined through X-ray diffraction (XRD, Bruker D8 Advance, λ = 1.5418 Å,) utilizing Cu Kα radiation. The data were recorded over a diffraction angle (2θ) range of 10° to 60°, using a scanning speed of 4° per minute. The functional groups of the samples were identified using Fourier Transform Infrared Spectroscopy (FTIR, Nicolet IS50), with spectra recorded in the range of 750 to 2000 cm− 1.
Synchrotron X-ray microtomography
The synchrotron X-ray microtomography study on PEEK was carried out at the Shanghai Synchrotron Radiation Facility (SSRF)57,61. The schematic layout of the in-line phase contrast x-ray microscopy is shown in Fig. 2. A collimated X-ray beam, with the X-ray energy set to 15 KeV to optimize edge enhancement and transmission rate, was monochromatized using a double Si (311) crystal system. As the X-ray beam passed through the sample, the exiting beam carried both absorption and phase shift information. After propagating for 20 cm, the phase shifts were converted into measurable intensity variations by Fresnel diffraction. The distance was determined to obtain optimal image contrast (Fig. 2), in which the term “distance” refers to the distance between the sample and the detector. When the distance is 0, i.e. Detector position I, the imaging technique is absorption contrast; conversely, when the distance is 20, i.e. Detector position II, the imaging technique is phase contrast. Phase contrast is achieved through the propagation of high-coherence synchrotron X-rays. The absorption contrast at the position I can be selected, while the image contrast is at a minimum for materials with similar absorption coefficients. During the experiment, the detector was moved to position II to increase the image contrast. The resulting images are a hybrid of the absorption information and the phase shift information.
Schematic layout of the synchrotron X-ray microtomography41. The X-ray beam at 15 KeV is monochromatized using a double Si (311) crystal system. A shutter is used to regulate the radiation dose by allowing the beam to pass only when the image forms on the CCD detector. Absorption contrast can be achieved at position I, while materials with similar absorption coefficients have minimum image contrast. To increase image contrast, the detector was moved to position II during the experiment. After propagating for 20 cm, the phase shifts were converted into measurable intensity variations through Fresnel diffraction.
The beam was captured as an image using a CCD detector with a resolution of 2048 × 2048 pixels and pixel size of 3.25 μm × 3.25 μm. The sample was glued directly on a rotary stage that was precisely calibrated to align with the CCD detector. The rotary stage was rotated 180° during data acquisition. The detector collected 1800 projections from 0° to 180° with 0.01° rotation interval and 50 ms exposure time per projection. Two flat images were taken every 100 projections to calibrate the background. There were no samples in the beam path. In addition, five dark images with no X-rays in the beam path were taken to eliminate CCD dark noise.
Tomographic Reconstruction and 3D volume rendering
The tomographic reconstruction was performed using CT software developed at the SSRF End station, which includes background correction, rotation axis position correction and filtered back projection (FBP) reconstruction57. Amira software was used to render the three-dimensional images of the specimen62,63.
Results and discussion
Synthesis and phase characterizations
We have successfully fabricated biomimetic porous PEEK implants. The implants exhibit structures analogous to the human skull, featuring two dense outer layers akin to cortical bones, with a less compact central region representative of the trabecular space (Fig. 3). As shown in the optical image, the implant ‘s diameter measures approximately 30 mm with a thickness of 3 mm. The dense (red arrows in Fig. 3) and porous layers (green arrow in Fig. 3) can be distinguished by looking at the sides. The dense part is about 0.5 mm thick, while the porous part is about 2 mm thick. The density of the sample measured by Archimedes principle is 1.09 g/cm3. However, the pore information is not available due to the limited spatial resolution of the optical image. Moreover, only the surface information such as the 3D morphology, shape, and porous surface structures are observed while the interior microstructures cannot be observed because the implant is non-transparent.
Optical image of the PEEK implant. The implant has a sandwich structure, consisting of two dense outer layers and a less compact central region. The diameter is approximately 30 mm. The thickness is 3 mm. The dense and porous layers can be distinguished by observing the sides. The dense layer is 0.5 mm thick, the porous layer 2 mm.
Herein the PEEK implant was fabricated using the salting-out technique, which is a simple method compared to other techniques. Several techniques have been developed to fabricate the desired bone repair implants, such as additive manufacturing and 3D printing28,30. Three-dimensional (3D) printing technology such as stereolithography (SLA), selective laser sintering (SLS), fused deposition modeling (FDM), and ink-jet 3D printing have the potential to integrate diverse cellular types within 3D biomaterial constructs, comprising conventional micro- and nanoscale biomaterials, to develop an artificial bone graft capable of regenerating damaged tissues64. In these fabrication methods, the bone implants are designed and fabricated by mimicking the target bone tissue. In the process, information about the shape and microstructure, such as internal pores and interconnecting channels, is essential. However, this information is difficult to obtain, making these methods complicated. Moreover, the intricate design specifications impose constraints on the effectiveness of the currently available methodologies, particularly when attempting to restore clinically relevant injuries to their original size65. While the salt out method used in this work has several advantages, including ease of operation and a controllable structure, which has been verified in our previous work12. It allows the size, layer thickness and pore size to be controlled, with the possibility of creating additional sizes as required. In addition, this method has the advantage of allowing simple parameter adjustments for easy preparation and mass production.
Phase characterizations
X-Ray Powder Diffraction (XRD) was used to investigate the phase of the PEEK implants. The focus point of XRD is selected on the layer with planar structure. Figure 4a shows the XRD pattern of the samples. The intensity peaks at 2θ angles of 18.7°, 20.6°, 22.4°, and 28.6° correspond to the characteristic planes of PEEK with (110), (111), (200), and (211) crystalline planes, belonging to the orthorhombic crystal system and the Pbcn space group66. It indicates that there is no change in the crystal structure during the sample preparation process.
Fourier transform infrared spectroscopy (FTIR) was used to investigate the functional group. The FTIR pattern of the samples is shown in Fig. 4b. The peak at 1644 cm− 1 corresponds to the aromatic C = O carbonyl stretching vibration67. The peaks at 1591 cm− 1 and 1486 cm− 1 are from the in-plane vibration band of benzene, while the peak at 1225 cm− 1 corresponds to the stretching vibration of C-O-C67,68. The peaks at 831 cm− 1 and 763 cm− 1 correspond to the out-of-plane bending vibration absorption of benzene’s C-H vibration69. These peaks are all characteristic of PEEK. The FTIR result confirms that the sample is PEEK phase.
XRD and FTIR confirm the stable chemical structure of PEEK, which is consistent with literature reports15,16,70. The stable property is determined by the chemical structures of PEEK. This stable property determines the major advantages of the material as a bone implant material, including chemical stability and non-toxicity. PEEK could be a superior choice compared to metal and other bone implant materials. In addition, no trace of NaCl phase was detected on the dense surface of the samples, indicating that the pore-forming agent did not migrate into the dense layer during the salt-bath process. While the XRD and FTIR were performed on the PEEK implant surface, the NaCl particles in the internal microstructure need further investigation.
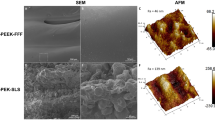
SEM and EDS characterization
Figure 5 shows the field emission scanning electron microscopy (FE-SEM) images and energy-dispersive X-ray spectroscopy (EDS) mapping of PEEK implants. The FE-SEM images indicate that the PEEK samples comprise of three distinct layers, with a porous layer located in the middle (Fig. 5a-b). A closer examination of the central layer reveals an average pore size ranging from 500 to 600 micrometers (Fig. 5c-d). Fig. S1 shows the distribution frequency of pore size in the central layer with a mean calculated pore size of 549 μm. The EDS mapping indicates the presence of carbon (C) and oxygen (O) elements in PEEK (Fig. 5e-f), which agrees with the observed X-ray diffraction (XRD) pattern.
FE-SEM images and EDS mapping of the PEEK implant. (a) the microstructure of the PEEK samples with three layers; (b) high magnification of FE-SEM image in a; (c) the microstructure in the porous layer; (d) the microstructure of an integrated pore in the porous layer; (e) mapping of C element, and (f) mapping of O element.
In this case, the pore size is consistent with the size of the pore-forming agent used in the experiments (Fig. S2 in the Supporting Information). Based on the pore size characteristics of cancellous bone, as referenced in literature71, it is possible to further refine the experimental parameters to achieve a pore size distribution similar to that of natural bone. According to the mechanisms of bone repair and regeneration, the pore size should be at least 300 μm to 500 μm with good interconnectivity1,22. Our current fabrication process for PEEK implants yields a pore size distribution from 500 μm to 600 μm, which, while slightly exceeding the lower limit, still meets the functional requirements. The structures could facility the ingrowth and formation of new bone by providing a porous implant material that creates a three-dimensional microenvironment for the adhesion, proliferation and differentiation of osteogenic-related cells during bone regeneration.
The pore size in PEEK implants is primarily determined by the size of the NaCl particles used as porogens. By controlling the size of these particles, it is possible to tailor the pore dimensions to meet specific requirements. This research will be instrumental in optimizing our fabrication techniques to achieve a pore size distribution that closely mirrors the natural cancellous bone, thereby enhancing the efficacy of our implants in bone regeneration therapies. Future studies will further be investigated on the relationship between NaCl particle size and resulting pore dimensions in PEEK implants.
Synchrotron X-ray tomography of PEEK implants
To visualize the 3D interior microstructures of the PEEK implant, synchrotron X-ray tomographic microscopy based on in-line phase contrast was performed. Due to the limited field of view, we selected a cubic section for the experiment. The field of view is limited by the size of the X-ray beam. At 3.25 μm detector pixel size, the field of view is 6.656 mm (horizontal) by 1.95 mm (vertical). In the experiment three samples were checked by using X-ray projections (Fig. S5 in Supporting Information, ). Yet only one sample was reconstructed and analyzed in fine detail. The CT projection reveals dense structures on both sides, with a porous structure in the middle (Fig. 6, green arrows). It is evident that the middle layer exhibits a 3D porous structure. The dense part is about 0.5 mm thick, while the porous part is about 2 mm thick. The internal ultrastructure is visible, with the dark dots corresponding to porogen sodium chloride particles, which is not observed in the optical image (Fig. 3). These particles are not discernible using optical or electron microscopy unless the sample is destroyed. The size of the porous structures should be calculated after CT reconstruction because the 3D structures overlap to 2D projections.
The issue of radiation damage during X-ray imaging is of significant importance. In particular, when working with radiation-sensitive samples, such as biomaterials, the application of X-rays can lead to structural damage if the radiation dose surpasses a certain threshold. In the case of PEEK, however, the material demonstrates a notable resistance to radiation-induced deterioration. Moreover, the irradiation dose employed in the experiment is minimal (The total X-ray exposure time is just 90 s.), resulting in structural alterations, if any, that are essentially inconsequential in comparison to the porous structure of the sample, which measures in the few hundred micrometers range.
Two-dimensional (2D) X-ray projection at (a) 0° (b) 90° and (c) 180° viewed by Image Pro Plus 6.0. The projections show that the PEEK implant has sandwich-like structures. It has dense structures on both sides and porous structures in the middle. The dense part is about 0.5 mm thick, while the porous part is 2 mm thick. The internal ultrastructure is visible and the dark dots (red arrows) correspond to porogen sodium chloride particles.
After the tomographic reconstruction, the 3D virtual microstructure was obtained and the virtual sample can be rotated along any axis. Figure 7a displays the 3D morphology of the selected cubic PEEK implant from three orthometric viewpoints. Figure 7b shows the overview, where the sample width was measured to be approximately 3 mm. The thickness of the porous part of the implant was measured to be approximately 2 mm from the side view obtained by rotating the virtual sample 90◦ (Fig. 7c).
The 3D microstructure of the porous PEEK implant was reconstructed by X-ray tomography. In comparison with the histological methods that are often technically difficult and labor-intensive, X-ray tomography shows high efficiency and high precision in noninvasive structural analysis72. To investigate the interior structures, the sample was virtually analyzed slice by slice. We also performed the 3D segment of the pores. (Fig. S6 in the Supporting Information). Figure 8 displays the intermediate layer obtained after CT reconstruction. The middle layer of the sample exhibits a 3D porous structure, enabling three-dimensional measurements. Figure 8a-d show four representative slices spaced 65 μm apart with a thickness of 3.25 μm, clearly displaying the sandwich-like structure and connectivity of the porous material. The pore size ranges from 500 μm to 600 μm, which corresponds to the particle size distribution of the porogen sodium chloride particles (Fig. S2 in the Supporting Information). Upon cutting the sample for further analysis, we employed EDS mapping to examine the elemental composition. This technique revealed the presence of Na and chlorine Cl elements within the sample, as depicted in Fig. S3 of the Supporting Information.
Slice by slice analysis of the PEEK implant by X-ray tomography. (a-d) Four representative slices spaced 65 μm apart perpendicular to the X-ray beam direction. The slices clearly display the sandwich-like structure and connectivity of the porous material (yellow arrows). The residual porogen sodium chloride particles (i.e. NaCl) are also observed (red arrows).
What’s more, the residual porogen sodium chloride particles (i.e. NaCl) were observed within the PEEK implant (Fig. 8, red arrows), which cannot be realized by other microscopic methods without destroying the sample. The residual NaCl particles is far away from other ones and led to the formation of closed pores. The closed pores are unfavorable which hinder the growth and formation of blood vessels and other related tissues. Ultimately it will influence the osteoconduction and osseointegration. In the following work, we will further optimize the fabricate procedures to eliminate the closed pores.
The internal porous microstructures of the sandwich-like PEEK implant were investigated by in-line phase contrast microtomography. In the representative tomographic slices, the edge of neighboring pores was clearly observed (Fig. 8, the ___location of the slices in the 3D volume is in Fig. S4 in Supporting Information). The edge enhancement is due to the phase shift after the X-ray passes through the sample. Phase contrast based on phase shift is much more sensitive than absorption contrast based on X-ray intensity change11,49,58. And the in-line phase contrast microscopy in the study has a simple setup (Fig. 2). No optical element is used other than the highly coherent X-ray beam. With the development of synchrotron light source, high-coherent X-ray light source is much easier to get73. The method will have wider application, especially for biological applications. Yet the experimental time of synchrotron radiation facility is limited, laboratory X-ray tomography also should be applied and could provide valuable structural information. Laboratory X-ray CT imaging is a particularly significant technique, and for the examination of holes measuring a few hundred micrometers can yield results comparable to those obtained with synchrotron light sources. However, in contrast to synchrotron light sources, laboratory X-ray light sources are characterized by low brightness, resulting in prolonged data acquisition times, comparatively projections with low signal-to-noise ratios. These attributes represent some of the inherent limitations of this technology. One advantage of this approach is that it allows for easy access and unlimited experimental time. A comparison of synchrotron radiation and laboratory X-ray tomography will be performed in the future work.
Additionally, the work demonstrate that X-ray tomography is an ideal method for imaging intact specimens nondestructively due to the long penetration depth of X-rays. The selected PEEK implant is a cubic sample with size of 3 mm by 3 mm by 3 mm. It is not necessary to cut the sample usually performed in optical microscopy and electron microscopy to obtain the 3D structure information of the sample. By using larger CCD detector, much larger samples could be investigated potentially.
X-ray tomography and SEM each show distinct advantages. In the present study, two distinct imaging techniques were employed: SEM and X-ray computed tomography (X-ray CT). Scanning electron microscopy allows for the acquisition of high-resolution images and elemental-resolution information (Fig. 5), which is a significant advantage of this technique. If focused ion beam-scanning electron microscopy (FIB-SEM) is employed to facilitate real-time observation of the electron beam and ion beam cutting or micromachining. While X-ray CT technology enables the acquisition of non-destructive three-dimensional structural information and the execution of statistical analyses of pore structures, among other capabilities (Fig. 8). The combination of these two methods facilitates a more comprehensive and multi-scale structural analysis45,74.
In addition, the triple-layered structures are very similar to those found in natural skulls3. The bionic natural bone is also characterized by a three-layer structure, consisting of dense layers on either side and a sparse, porous layer in the middle. The typical well-connected porous structures are shown (Fig. 8, marked with yellow arrows). The microstructure of PEEK imitates that of natural bone15. The porous structure of PEEK implants allows for enhanced osteoconduction and osseointegration. The porous structure provides space for cells to adhere and grow, facilitating the formation of a strong bond between the implant and bone tissue. This structure can provide a growing environment for new bone to form and maintain good mechanical properties. In the following work, the pore size and interconnectivity will be optimized to have gradient and multiscale structures similar to skull bones. Herein the physical structures of the PEEK implants have been modified. Furthermore, the chemical composition will be modified by adding bioactive materials16,31. The incorporation of bioactive materials into PEEK will enhance its bioactivity, thereby increasing the likelihood of cellular growth and subsequent promotion of osteoconduction and osteointegration Combining structural and chemical modifications, we will enhance the bone repair capabilities of PEEK and address the issue of bone defects, ultimately improving people’s quality of life.
Conclusions
In summary, we successfully designed and fabricated a bionic sandwich-like PEEK implant. Synchrotron X-ray in-line phase contrast microtomography was employed to nondestructively observe the interior porous microstructures. The microstructure of the three layers resembles the cancellous bone of a natural skull, exhibiting typical pore structures such as pore size and shapes. Additionally, residual porogen sodium chloride particles within the PEEK implants were observed, which highlights the advantages and potential of synchrotron X-ray microtomography for structural analysis of biomedical materials. This study offers theoretical guidance for further designing and preparing PEEK bone repair materials, and will advance the clinical application of innovative bioactive bone repair materials.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Taylor, D., Hazenberg, J. G. & Lee, T. C. Living with cracks: damage and repair in human bone. Nat. Mater. 6, 263–268. https://doi.org/10.1038/nmat1866 (2007).
Rodan, G. A. & Martin, T. J. Therapeutic approaches to bone diseases. Science 289, 1508–1514 (2000).
Wilkie, A. O. et al. Functional haploinsufficiency of the human homeobox gene MSX2 causes defects in skull ossification. Nat. Genet. 24, 387–390 (2000).
Mavrogiannis, L. A. et al. Haploinsufficiency of the human homeobox gene ALX4 causes skull ossification defects. Nat. Genet. 27, 17–18 (2001).
Goiato, M. C., Anchieta, R. B. & Pita, M. S. Dos Santos, D. M. Reconstruction of skull defects: currently available materials. J. Craniofac. Surg. 20, 1512–1518 (2009).
Yu, M. et al. Cranial suture regeneration mitigates skull and neurocognitive defects in craniosynostosis. Cell 184, 243–256 (2021).
Posnick, J. C., Goldstein, J. A., Armstrong, D. & Rutka, J. T. Reconstruction of skull defects in children and adolescents by the use of fixed cranial bone grafts: long-term results. Neurosurgery 32, 785–791 (1993).
Jeong, J., Kim, J. H., Shim, J. H., Hwang, N. S. & Heo, C. Y. Bioactive calcium phosphate materials and applications in bone regeneration. Biomaterials Res. 23, 1–11 (2019).
Chang, J., Zhang, X. & Dai, K. Bioactive Materials for bone Regeneration. Academic Press. (2020).
Li, T. et al. Bioinspired Biomaterials with a Brick-and‐Mortar Microstructure combining mechanical and biological performance. Adv. Healthc. Mater. 9, 1901211 (2020).
Stevens, M. M. Biomaterials for bone tissue engineering. Mater. Today. 11, 18–25 (2008).
Zhang, M. et al. Integrated porous polyetheretherketone implants for treating skull defect. J. Mater. Res. Technol. 22, 728–734 (2023).
Li, M. et al. Rational integration of defense and repair synergy on PEEK osteoimplants via biomimetic peptide clicking strategy. Bioact Mater. 8, 309–324. https://doi.org/10.1016/j.bioactmat.2021.07.002 (2022).
Chen, Z., Chen, Y., Ding, J. & Yu, L. Blending strategy to modify PEEK-based orthopedic implants. Compos. Part. B: Eng. 250, 110427. https://doi.org/10.1016/j.compositesb.2022.110427 (2023).
Saad, A. et al. Biomimetic Strategy to enhance epithelial cell viability and spreading on PEEK implants. ACS Biomater. Sci. Eng. 8, 5129–5144. https://doi.org/10.1021/acsbiomaterials.2c00764 (2022).
Wei, X. et al. Magnesium surface-activated 3D printed porous PEEK scaffolds for in vivo osseointegration by promoting angiogenesis and osteogenesis. Bioactive Mater. 20, 16–28 (2023).
Verma, S., Sharma, N., Kango, S. & Sharma, S. Developments of PEEK (polyetheretherketone) as a biomedical material: a focused review. Eur. Polymer J. 147, 110295 (2021).
Yin, W. et al. Recent advances in orthopedic polyetheretherketone biomaterials: material fabrication and biofunction establishment. Smart Mater. Med. 3, 20–36. https://doi.org/10.1016/j.smaim.2021.11.005 (2022).
Hao, Z. et al. The scaffold microenvironment for stem cell based bone tissue engineering. Biomater. Sci. 5, 1382–1392. https://doi.org/10.1039/c7bm00146k (2017).
Yuan, Z. et al. 3D printed porous sulfonated polyetheretherketone scaffold for cartilage repair: potential and limitation. J. Orthop. Translation. 33, 90–106 (2022).
Salhotra, A., Shah, H. N., Levi, B. & Longaker, M. T. Mechanisms of bone development and repair. Nat. Rev. Mol. Cell. Bio. 21, 696–711 (2020).
Deschaseaux, F., Sensébé, L. & Heymann, D. Mechanisms of bone repair and regeneration. Trends Mol. Med. 15, 417–429 (2009).
Zhang, M. et al. 3D printing of haversian bone–mimicking scaffolds for multicellular delivery in bone regeneration. Sci. Adv. 6, eaaz6725 (2020).
Burg, K. J., Porter, S. & Kellam, J. F. Biomaterial developments for bone tissue engineering. Biomaterials 21, 2347–2359 (2000).
Kim, H. D. et al. Biomimetic materials and fabrication approaches for bone tissue engineering. Adv. Healthc. Mater. 6, 1700612 (2017).
Wang, L. et al. Biomimetic scaffolds with programmable pore structures for minimum invasive bone repair. Nanoscale 13, 16680–16689 (2021).
Huang, L. et al. Propelling Multi-modal therapeutics of PEEK implants through the power of NO evolving Covalent Organic frameworks (COFs). Small 20, 2306508 (2024).
Liu, X. et al. 3D-printed bioactive ceramic scaffolds with biomimetic micro/nano-HAp surfaces mediated cell fate and promoted bone augmentation of the bone–implant interface in vivo. Bioactive Mater. 12, 120–132 (2022).
Liu, Z. et al. 3D-printed porous PEEK scaffold combined with CSMA/POSS bioactive surface: a strategy for enhancing osseointegration of PEEK implants. Compos. Part. B: Eng. 230, 109512 (2022).
Wubneh, A., Tsekoura, E. K., Ayranci, C. & Uludağ, H. Current state of fabrication technologies and materials for bone tissue engineering. Acta Biomater. 80, 1–30. https://doi.org/10.1016/j.actbio.2018.09.031 (2018).
Zhao, R. et al. Osteoporotic bone recovery by a bamboo-structured bioceramic with controlled release of hydroxyapatite nanoparticles. Bioact Mater. 17, 379–393. https://doi.org/10.1016/j.bioactmat.2022.01.007 (2022).
Xie, C. et al. Advanced strategies of Biomimetic tissue-Engineered grafts for bone regeneration. Adv. Healthc. Mater. 10, e2100408. https://doi.org/10.1002/adhm.202100408 (2021).
Koons, G. L., Diba, M. & Mikos, A. G. Materials design for bone-tissue engineering. Nat. Reviews Mater. 5, 584–603. https://doi.org/10.1038/s41578-020-0204-2 (2020).
Deng, C. et al. Micro/nanometer-structured scaffolds for regeneration of both cartilage and subchondral bone. Adv. Funct. Mater. 29, 1806068 (2019).
Walsh, C. L. et al. Imaging intact human organs with local resolution of cellular structures using hierarchical phase-contrast tomography. Nat. Methods. 18, 1532–1541. https://doi.org/10.1038/s41592-021-01317-x (2021).
Tao, Q. & Luo, S. Investigation of gastric cancers in nude mice using X-ray in-line phase contrast imaging. Biomed. Eng. Online. 13, 101. https://doi.org/10.1186/1475-925X-13-101 (2014).
Zhao, Y. et al. High-resolution, low-dose phase contrast X-ray tomography for 3D diagnosis of human breast cancers. Proc. Natl. Acad. Sci. U.S.A. 109, 18290–18294. https://doi.org/10.1073/pnas.1204460109 (2012).
Zanette, I. et al. X-ray microtomography using correlation of near-field speckles for material characterization. Proc. Natl. Acad. Sci. U.S.A. 112, 12569–12573. https://doi.org/10.1073/pnas.1502828112 (2015).
Westneat, M. W. et al. Tracheal respiration in insects visualized with synchrotron x-ray imaging. Science 299, 558–560. https://doi.org/10.1126/science.1078008 (2003).
Zhu, P. et al. Low-dose, simple, and fast grating-based X-ray phase-contrast imaging. Proc. Natl. Acad. Sci. U.S.A. 107, 13576–13581. https://doi.org/10.1073/pnas.1003198107 (2010).
Yao, S. et al. Equally sloped X-ray microtomography of living insects with low radiation dose and improved resolution capability. Appl. Phys. Lett. 108, 123702. https://doi.org/10.1063/1.4944727 (2016).
Akhter, M. & Recker, R. High resolution imaging in bone tissue research-review. Bone 143, 115620 (2021).
Zhai, X. et al. High-speed X-ray visualization of dynamic crack initiation and propagation in bone. Acta Biomater. 90, 278–286 (2019).
Yu, B., Pacureanu, A., Olivier, C., Cloetens, P. & Peyrin, F. Quantification of the bone lacunocanalicular network from 3D X-ray phase nanotomography images. J. Microsc. 282, 30–44. https://doi.org/10.1111/jmi.12973 (2021).
Besnard, C. et al. Hierarchical 2D to 3D micro/nano-histology of human dental caries lesions using light, X-ray and electron microscopy. Mater. Design. 220, 110829. https://doi.org/10.1016/j.matdes.2022.110829 (2022).
Neldam, C. A. et al. Application of high resolution synchrotron micro-CT radiation in dental implant osseointegration. J. Cranio-Maxillofacial Surg. 43, 682–687. https://doi.org/10.1016/j.jcms.2015.03.012 (2015).
Kourkoutis, L. F., Plitzko, J. M. & Baumeister, W. Electron Microscopy of Biological materials at the nanometer scale. Annu. Rev. Mater. Res. 42, 33–58. https://doi.org/10.1146/annurev-matsci-070511-155004 (2012).
Peña Fernández, M. et al. In situ synchrotron radiation µCT indentation of cortical bone: anisotropic crack propagation, local deformation, and fracture. Acta Biomater. 167, 83–99. https://doi.org/10.1016/j.actbio.2023.04.038 (2023).
Obata, Y. et al. Quantitative and qualitative bone imaging: a review of synchrotron radiation microtomography analysis in bone research. J. Mech. Behav. Biomed. Mater. 110, 103887. https://doi.org/10.1016/j.jmbbm.2020.103887 (2020).
Muller, R. Hierarchical microimaging of bone structure and function. Nat. Rev. Rheumatol. 5, 373–381. https://doi.org/10.1038/nrrheum.2009.107 (2009).
Matsumoto, T., Shimizu, R. & Uesugi, K. In vivo monitoring of bone microstructure by propagation-based phase-contrast computed tomography using monochromatic synchrotron light. Lab. Invest. 100, 72–83. https://doi.org/10.1038/s41374-019-0337-3 (2020).
Cedola, A. et al. Three dimensional visualization of engineered bone and soft tissue by combined x-ray micro-diffraction and phase contrast tomography. Phys. Med. Biol. 59, 189 (2013).
Weiss, P. et al. Synchrotron X-ray microtomography (on a micron scale) provides three-dimensional imaging representation of bone ingrowth in calcium phosphate biomaterials. Biomaterials 24, 4591–4601. https://doi.org/10.1016/s0142-9612(03)00335-1 (2003).
Giuliani, A. et al. Synchrotron phase tomography: an emerging imaging method for microvessel detection in engineered bone of craniofacial districts. Front. Physiol. 8, 769 (2017).
Obata, Y. et al. Quantitative and qualitative bone imaging: a review of synchrotron radiation microtomography analysis in bone research. J. Mech. Behav. Biomed. Mater. 110, 103887. https://doi.org/10.1016/j.jmbbm.2020.103887 (2020).
Besnard, C. et al. Synchrotron X-ray studies of the structural and functional hierarchies in Mineralised Human Dental Enamel: a state-of-the-art review. Dentistry J. 11, 98 (2023).
Ji, J. F. et al. The new X-ray imaging and biomedical application beamline BL13HB at SSRF. Nucl. Sci. Tech. 34 https://doi.org/10.1007/s41365-023-01349-2 (2023).
Davis, T. J., Gao, D., Gureyev, T. E., Stevenson, A. W. & Wilkins, S. W. Phase-contrast imaging of weakly absorbing materials using hard X-Rays. Nature 373, 595–598. https://doi.org/10.1038/373595a0 (1995).
Kok, J. et al. Analysis of Bone-Implant Integration with Synchrotron X-ray Tomography. Quantitative Musculoskeletal Imaging (QMSKI) 2022 &. (2022).
Peña Fernández, M. et al. Time-resolved in situ synchrotron-microCT: 4D deformation of bone and bone analogues using digital volume correlation. Acta Biomater. 131, 424–439. https://doi.org/10.1016/j.actbio.2021.06.014 (2021).
Yao, S. K. et al. Nondestructive structural investigation of Yttria-stabilized Zirconia Fiber Insulation Tile by Synchrotron X-ray In-Line phase-contrast Microtomography. Photonics 8 (8), 338. https://doi.org/10.3390/photonics8080338 (2021).
Zhao, Y., Sun, Y., Yuan, L. & Xu, Q. Impact of nanopore structure on coal strength: a study based on synchrotron radiation nano-CT. Results Phys. 17, 103029. https://doi.org/10.1016/j.rinp.2020.103029 (2020).
Besnard, C. et al. 3D analysis of enamel demineralisation in human dental caries using high-resolution, large field of view synchrotron X-ray micro-computed tomography. Mater. Today Commun. 27, 102418. https://doi.org/10.1016/j.mtcomm.2021.102418 (2021).
Cheng, L. et al. 3D printing of micro-and nanoscale bone substitutes: a review on technical and translational perspectives. Int. J. Nanomed., 4289–4319 (2021).
Zhang, C., Wang, L., Kang, J., Fuentes, O. M. & Li, D. Bionic design and verification of 3D printed PEEK costal cartilage prosthesis. J. Mech. Behav. Biomed. Mater. 103, 103561 (2020).
Xie, M., Xiao, G., Song, Z. & Lu, Y. The formation process and mechanism of the 3D Porous Network on the Sulfonated PEEK Surface. ACS Appl. Mater. Interfaces. 16, 13585–13596. https://doi.org/10.1021/acsami.4c00055 (2024).
Al Lafi, A. G. The sulfonation of poly (ether ether ketone) as investigated by two-dimensional FTIR correlation spectroscopy. J. Appl. Polym. Sci. 132 (2015).
Wang, W., Luo, C., Huang, J. & Edirisinghe, M. PEEK surface modification by fast ambient-temperature sulfonation for bone implant applications. J. Royal Soc. Interface. 16, 20180955 (2019).
Li, S. et al. Porous polyetheretherketone-hydroxyapatite composite: a candidate material for orthopedic implant. Compos. Commun. 28, 100908 (2021).
Kurtz, S. M. & Devine, J. N. PEEK biomaterials in trauma, orthopedic, and spinal implants. Biomaterials 28 32, 4845–4869 (2007).
Li, J., Li, S., Blitterswijk, C. V. & Groot, K. d. cancellous bone from porous T {i} 6Al4V by multiple coating technique. J. Mater. Science: Mater. Med. 17, 179–185 (2006).
Otto, R. et al. Synchrotron µ-CT-based morphological characterization of additively manufactured open porous structures. Additive Manuf. 55, 102874. https://doi.org/10.1016/j.addma.2022.102874 (2022).
Xu, J. Q. et al. Advances in X-ray neuroimaging: bridging scales from molecular to organ architectures. Trac-Trend Anal. Chem. 171, 117513. https://doi.org/10.1016/j.trac.2023.117513 (2024).
Yuchen, F. & Keyu, L. Large-volume FIB-SEM 3D reconstruction: an effective method for characterizing pore space of lacustrine shales. Front. Earth Sci. 10, 1046927 (2023).
Acknowledgements
This work was supported by Young Talent of Lifting Engineering for Science and Technology in Shandong, China (SDAST2021qt05) and Shandong Provincial Natural Science Foundation (ZR2020QA076 and ZR2020QE070). We thank Dr. Jianhua Zhang, Dr. Difei Zhang and the staffs of beamline 13HB at Shanghai Synchrotron Radiation Facility for assistance with data acquisition.
Author information
Authors and Affiliations
Contributions
S. Y. and H. Z. designed the research; M. Q., M. L. ,E.S. and K. Y. performed the experiment; M. Q. and S. Y. prepared the figures; M. Q. and S. Y. write the draft; All the authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Qi, Ml., Li, M., Yuan, K. et al. Fabrication and X-ray microtomography of sandwich-structured PEEK implants for skull defect repair. Sci Rep 14, 28585 (2024). https://doi.org/10.1038/s41598-024-80103-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-80103-z