Abstract
Objective: To investigate the predictive ability of the MRI-based vertebral bone quality (VBQ) score for pedicle screw loosening following instrumented transforaminal lumbar interbody fusion (TLIF). Methods: Data from patients who have received one or two-level instrumented TLIF from February 2014 to March 2015 were retrospectively collected. Pedicle screw loosening was diagnosed when the radiolucent zone around the screw exceeded 1 mm in plain radiographs. The T1-weighted MRI sagittal images were used for calculation of the VBQ score. The score was calculated with the median signal intensity value of L1 to L4 divided by the signal intensity value of cerebrospinal fluid at the L3 level. Univariate analysis and multivariate binary logistic regression analysis were performed. Receiver operating characteristic curve analysis assessed the predictive ability of the VBQ score on screw loosening. Results: Among the included 211 patients, 75 of them (35.55%) had pedicle screw loosening at the 24 month follow-up. Multivariable logistic regression analyses demonstrated that higher VBQ score (OR: 27.887 ± 0.514 ,95% CI: 10.189–76.326), male sex (female to male 0.323 ± 0.483, 0.126–0.833), and longer fusion length (2.578 ± 0.545, 1.166–5.701) were significant influencing factors for pedicle screw loosening. The VBQ score significantly predicted screw loosening with an accuracy of 78.9%. Conclusions: A higher VBQ score was an independent risk factor for pedicle screw loosening following instrumented TLIF. The MRI-based VBQ score showed good predictive ability for screw loosening and could be used as an alternative option for preoperative bone quality evaluation.
Similar content being viewed by others
Introduction
Transforaminal lumbar interbody fusion (TLIF) combined with pedicle screw instrumentation is an effective treatment for patients with degenerative lumbar spine diseases1. However, perioperative and postoperative complications can occur after TLIF. A recognized complication of TLIF is pedicle screw loosening, which may lead to a resultant high pseudoarthrosis rate, affecting the patient’s quality of life, preventing successful fusion, and leading to screw breakage, nonunion, and progressive kyphosis which may all be attributed to an incorrect, failing loading scenario after surgery2,3,4.
Previous reports indicated a very wide range of failure rates, ranging from less than 1 to 15% in non-osteoporotic patients treated with rigid systems and even up to 60% in osteoporotic subjects5. If predictors of screw loosening are obvious before surgery, the choice of proper augmentation or fused segments may be optimized. Among the risk factors associated with pedicle screw loosening, low bone density has been considered to be one of the main risk factors6,7.
Decreased bone mineral density (BMD) could be measured by dual energy X-ray absorptiometry(DEXA). However, the majority of patients do not have DEXA measurements available. A novel magnetic resonance imaging (MRI)-based vertebral bone quality (VBQ) score has emerged as an alternative for bone quality evaluation. Prior reports demonstrated that the VBQ score is an independent predictor of normal BMD versus osteopenic/osteoporotic BMD based on DEXA with an accuracy of 81%.8 Another study showed that there was a moderate correlation between the VBQ score and the BMD measured by quantitative computed tomography8.
To the best of our knowledge, the relationship between the VBQ score and pedicle screw loosening has yet to be determined. The purpose of this study was to clarify the following: (1) What is the ability of the VBQ score to predict pedicle screw (PS) loosening following TLIF? (2) What are the risk factors related to pedicle screw (PS) loosening following TLIF?
Materials and methods
Patients
This study was approved by the Institutional Review Board of our institution before the data collection and analyses (IRB202100894B0). The study was performed in accordance with relevant guidelines/regulations and the need of informed consent was waived by the committee due to its retrospective nature. Patients who were surgically treated by the spine surgeon group in our department from February 2014 to March 2015 were included in this study. The included patients were required met the following criteria: (1) age more than 18 years; (2) history of one or two-level TLIF with bilateral pedicle screw instrumentation to treat degenerative lumbar spinal diseases; (3) adequate lumbar spine T1-weighted MRI without inversion recovery or contrast obtained within 1 year prior to surgery; (4) failure of conservative treatment for more than 6 months; and (5) a follow-up including plain radiographs for more than 2 years. Exclusion criteria were the following: (1) presence of spinal tumors, fractures, or infections, (2) history of prior spinal surgery, (3) occurrence of screw malposition or redirection, and (4) history of reoperation within 2 years after the initial surgery for reasons other than screw loosening.
Surgical technique
All surgeries were performed through a midline posterior open approach by the same group ofspine surgeons who were trained by the same senior surgeon. The patients underwent bilateral pedicle screw instrumentation and transforaminal interbody fusion. The starting point for pedicle screw was the intersection between the midpoint of the transverse process and the lateral margin of the superior facet, and the orientation of screw insertion was determined by preoperative and intraoperative radiographs. The inserted screw diameter was 6.0–6.5 mm for the lumbar vertebrae, and 6.5–7.0 mm for S1, and the length was 4.5–5.0 cm for the lumbar vertebrae, and 4.0–4.5 cm for S1. After pedicle screw placement, decompression with laminectomy and bilateral medial facetectomies was then performed. Polyetheretherketone (PEEK) cages were used for interbody fusion, which were chosen for insertion on the side with the major neurological symptoms. After discectomy and disc preparation, the milled autologous bone graft from decompression along with calcium phosphate bone substitute was packed into the disc space. The cage filled with the autologous bone graft was then inserted.
The patients were instructed to walk by themselves with the support of lumbar braces after 1–2 days after the surgeries. We asked the patients to wear braces until 3 months postoperatively. Physical therapy such as straight leg raise and ankle pump exercise was started at the first day after the surgery. Only essential daily activities were allowed during the first 3 months after the operation.
Data collection and radiographic assessment
General patient information was collected and recorded, including age, sex, body mass index (BMI), diabetes, history of smoking, anti-osteoporotic drug usage for 2 years perioperatively, and chronic steroid usage. The outcome of the operation was assessed preoperatively and at 2 years postoperatively by the Oswestry Disability Index (ODI) and the visual analog scale (VAS) for back and leg pain.
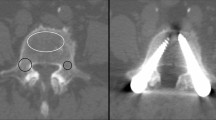
All included patients completed lumbar radiographic examination at 24 months postoperatively. Two experienced spine surgeon (Y.Y. and M.H.) independently evaluated pedicle screw loosening, relative pedicle screw length and the bone fusion status. The final result of assessment was made by consensus after discussion on cases with divergent results between two assessors. Screw loosening was diagnosed when the radiolucent zone around the screw exceeded 1 mm. To analyze the relative screw length, we divided the vertebral body into four parts from anterior to posterior and calculated the mean depth of all screws. (Fig. 1) The fusion status was evaluated by anteroposterior and lateral dynamic radiographs at 2 years after the initial operation. Nonunion was diagnosed when (1) more than 3 degrees of angular motion or (2) more than 3 mm of segmental translation, or (3) absence of bone fusion mass across any fusion segment was observed in the radiographs9.
Calculation of the vertebral bone quality score
The calculation of the VBQ score was performed with T1-weighted MRI of the lumbar spine without inversion recovery or contrast as previously reported8. By placing regions of interest (ROIs) within the medullary portions of the L1-L4 vertebral bodies and the cerebrospinal fluid (CSF) space at the level of L3 in the midsagittal cut of the lumbar image, the average signal intensity (SI) values were obtained. The VBQ score was calculated as the median SI value of the L1-L4 vertebral body divided by the SI of the CSF (Fig. 2). Parasagittal cuts were used instead for patients with conditions preventing ROI measurement on the midsagittal slice (e.g. scoliotic change, hemangioma, venous plexus). If the abnormal condition invaded all sagittal cuts of the vertebral body, this body was excluded from the calculation, and the VBQ score was derived from the remaining vertebrae. In some cases for which the CSF space at L3 was obstructed by descending roots, the CSF space ROI at L2 or L4 was used instead for the calculation to fully reflect the SI of CSF. VBQ scores in this study were measured by two trained independent researchers (Y.H. and J.C.) who were blinded to the clinical and radiographic outcomes, and the mean VBQ of the two measurement sets was used in this analysis.
Data analysis
Continuous variables were analyzed by an independent t test. The chi-square test and Fisher’s exact test were used for categorical comparisons. Variables deemed as potential risk factors were included in a multivariate logistic regression model.
A receiver operating characteristic (ROC) curve was used to identify cutoff values by the Youden index and the area under the curve (AUC) of the VBQ score as a predictor of the presence of pedicle screw loosening. Interrater reliability was assessed using the intraclass correlation coefficient (ICC). SPSS statistical software version 20 (IBM Corporation, Armonk, NY, USA) was used to perform the statistical analyses. Differences were deemed significant if the p value was < 0.05.
Results
A total 211 patients were included into the final analysis, the mean age was 63.70 ± 12.69 years and the mean BMI was 25.07 ± 5.67. The mean fusion length was 1.52 level, and 53 patients (25.11%) had the lowest instrumented vertebrae (LIV) at S1. The mean VBQ score of the included patients was 3.20 ± 0.71, and the interrater reliability between the two independent researchers was good (ICC: 0.824, 95% CI 0.76–0.89). The detailed demographic data of the included patients are listed in Table 1.
Among the included patients, 75 of them (35.55%) had pedicle screw loosening at the 24-month follow-up. Comparing the loosening and the nonloosening group, the loosening group was significantly older (67.67 ± 12.08 vs. 61.51 ± 12.52). The loosening group was also found to have a longer fusion length (1.61 ± 0.49 vs. 1.46 ± 0.50), and a higher VBQ score was found in the loosening group. The fusion rate in the postoperative 24-month follow-up was lower in the loosening group. The sex, BMI, screw depth, and percentage of LIV at S1 showed no significant between-group differences. Table 2.
All clinically relevant factors were entered into the multiple logistic regression model, and the multivariate analysis showed that higher VBQ score (odds ratio: 27.887 ± 0.514 ,95% CI: 10.189–76.326), male sex (female to male 0.323 ± 0.483, 0.126–0.833), and longer fusion length (2.578 ± 0.545, 1.166–5.701) were significant influencing factors for pedicle screw loosening. To further investigate the effect of VBQ score increase on the risk of screw loosening, we multiplied the VBQ score by 10 and re-entered it into the regression mode. The odds ratio turned out to be 1.382, indication that the risk of screw loosening increases by 1.382 times as the VBQ screw increases by 0.1 (Table 3).
A receiver operating characteristic curve was created for the VBQ score to assess the predictive ability for the presence of pedicle screw loosening, and the AUC was 0.789 The cutoff value was 3.097, which was determined by the Youden index, indicating the most sensitive and specific value for screw loosening risk. (Fig. 3).
The patient-reported outcomes showed that the loosening group had less back pain improvement in the 2-year postoperative follow-up (back pain vas: 3.40 vs. 2.29, p < 0.05). The postoperative ODI and leg pain VAS scores showed no significant difference between the loosening and the nonloosening groups. Table 4.
Of all included patients, 4 cases developed posterior cage migration along with screw loosening, and 2 of them underwent reoperation. One patient underwent revision surgery due to pseudoarthrosis and screw loosening, and six patients underwent revision surgery because of adjacent segment disease.
Discussion
In this study, we included 211 patients who have received 1- or 2-level instrumented TLIF to investigate the risk factors for pedicle screw loosening. We utilized the novel MRI-based VBQ score to evaluate bone quality, and the results of multivariable analysis demonstrated that a higher VBQ score, longer fusion length, and male sex were significant risk factors for this complication. The VBQ score was also found to be a predictor of pedicle screw loosening with an accuracy of 78.9%.
Lower BMD measured by DEXA was shown to be associated with pedicle screw loosening in prior clinical study5. A biomechanical study from Wiser et al. also demonstrated less pedicle screw stability in specimens with lower bone mineral density10. Further studies investigated the potential of the Hounsfield unit measured in computed tomography images in predicting pedicle screw loosening. Both the Hounsfield unit of the L1-L4 vertebral bodies and the screw trajectory have been reported to predict pedicle screw loosening with good accuracy3,11,12. However, neither DEXA nor computed tomography is obtained as a part of the standard workup for patients with degenerative spine disease. It would be helpful to develop a simple, accurate tool that is derived from images of routine preoperative examinations, such as MRI.
The VBQ score was presented by Ehresman et al. as an innovative MRI-based method for bone quality quantification, and it was reported to be a predictor of osteopenia and osteoporosis, fragility fracture, and vertebral compression fracture in patients with spine metastases13,14,15. The vertebral bone quality score was based on the finding that the adipose tissue content increased as the vertebral body became osteoporotic16. The signal intensity of the vertebral body measured on the T1-weighted image increased as the fat infiltration increased, thus reflecting the bone quality of the medullary portion of the vertebral body. Further studies have demonstrated that the VBQ score had moderate correlation with BMD measured by quantitative computed tomography8,17. The VBQ score was also shown to predict cage subsidence following TLIF and standalone lateral lumbar interbody fusion18,19,20. In terms of the detecting power of the VBQ score on pedicle screw loosening, several studies have been published. A study by Li et al. utilized another MRI-based method to obtain the “pedicle bone quality (PBQ)” score which was calculated by dividing the median signal intensity value of the L1 to L4 pedicles with the signal intensity value of CSF around the L3. The PBQ score was shown to predict pedicle screw loosening well with ROC analysis showing AUC to be 0.75121. Another study Li et al. investigated the predictive value of MRI- based S1 bone quality score on screw loosening after degenerative scoliosis surgery. In patient with severe scoliosis, the rotated vertebrae may bring difficulties in measuring the L1 ~ L4 signal intensity in the sagittal images. Therefore, they focused on measuring the signal intensity value at S1 instead of measuring from L1 to L4 in our study. The result was also promising, showing the predictive accuracy to be 74.6%, and the threshold determined Youden Index was 3.17522. In this study, we utilized the general vertebral bone quality evaluation method covering from L1 to L4 and found it be to have good predicting power with 78.9% accuracy. All these studies demonstrated legitimate predicting accuracy despite different measuring methods, indicating the reliability of MRI based bone quality assessment is promising. However, there is still lack of data between the difference of these different methods, further study will be needed to address this issue.
Pedicle screw loosening is one of the most common complications following lumbar spine surgery. Various detection methods via CT, MRI or plain radiographs have been reported23. In this study, we used the radiolucent zone around the screw as the criterion for loosening. Previous studies reported that if the radiolucent zone around the screw exceeded 1 mm, the sensitivity was 24%~54% and the specificity was 89%~98% for the diagnosis of pedicle screw loosening23,24. In our cases, we found the screw loosening rate was 35.55% in the postoperative 2-year follow-up. Previous reports have demonstrated that a wide range of screw loosening incidences, different primary diseases, surgical methods, follow-up times, patient age and fixation lengths could alter the results. It could range as low as 7.4% for one-level fixation, and over 60% in elderly osteoporotic patients with multilevel fixation7,25. Reports from Xu et al. showed the screw loosening rate at L3 was 20.3% from 143 patients receiving L3-L5 fusion26. In this study, it was deemed as loosened if any one screw of the whole construct had radiolucent zone > 1 mm, which is probably why the loosening rate is relatively higher in our study.
In addition to the VBQ score, male sex, and fixation length were other independent risk factors for pedicle screw loosening found in our patients. Although female patients usually have lower BMD than male patients, we still found male sex to be associated with a greater risk of developing screw loosening. We speculated that male patients may have more manual labor and more intense physical activity after the operation, resulting in more stress on the fixation construct. Prior studies also had found male sex to be an independent risk factor in multivariable analysis3,27. The length of fixation was frequently mentioned as a predictor of pedicle screw loosening. Reports from Kim et al. showed that the loosening rate was 2.0% for one-level fusion, and 50.0% for 4-level fusion28. Zou et al., observed similar results and reported the screw loosening rate to be 4.1%, 33.3%, 53.3%, and 78.8% for 1-level, 2-level, 3-level, and 4-level fixation constructs, respectively3. Our data showed that a longer fixation length was associated with higher incidence of pedicle screw loosening, which was compatible with the results of previous studies.
In the present study, patients in the loosening group were found to have less postoperative back pain improvement and higher incidence of pseudoarthrosis. A higher fusion failure rate was also observed by Tokuhashi et al., and a report from Zou et al. showed a 43.0% pseudoarthrosis rate in the loosening group3,25. A higher postoperative back pain VAS was observed in the loosening group according to Zou et al.3 The loosened fixation construct may lead to an unstable environment for fusion union, and possibly cause postoperative back discomfort. From the above results, screw loosening is correlated to fusion failure and poor clinical results.
The present study has the following limitations. First, it is a retrospectively designed study. Second, the DEXA T score data were not available in all the included patients. Last, the screw loosening and pseudoarthrosis were determined by plain radiographs instead of CT scans, which may underestimate the loosening and the fusion failure rates.
Conclusion
This is the a study to demontstrate the significant predictive ability of the MRI-based VBQ score for pedicle screw loosening following instrumented TLIF. We found the score to be an independent predictor of screw loosening with an accuracy of 78.9%. The complication was found be to correlated with fusion failure and postoperative back pain. For posterior instrumentation, surgeons could consider the VBQ score for preoperative bone quality evaluation.
Data availability
The authors are unable to share the raw dataset, which contained detailed patients’ record. The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
References
Harms, J. & Rolinger, H. A one-stager procedure in operative treatment of spondylolistheses: Dorsal traction-reposition and anterior fusion (author’s transl). Z. Orthop. Ihre Grenzgeb. 120 (3), 343–347. https://doi.org/10.1055/s-2008-1051624 (1982) (die operative Behandlung der Spondylolisthese durch dorsale Aufrichtung und ventrale Verblockung).
Berjano, P. et al. Failures and revisions in surgery for sagittal imbalance: Analysis of factors influencing failure. Eur. Spine J. 22 (S6), 853–858. https://doi.org/10.1007/s00586-013-3024-x (2013).
Zou, D. et al. Computed tomography Hounsfield unit-based prediction of pedicle screw loosening after surgery for degenerative lumbar spine disease. J. Neurosurg. Spine 3, 1–6. https://doi.org/10.3171/2019.11.Spine19868 (2020).
McLain, R. F., Sparling, E. & Benson, D. R. Early failure of short-segment pedicle instrumentation for thoracolumbar fractures. A preliminary report. J. Bone Jt. Surg. Am. . 75 (2), 162–167. https://doi.org/10.2106/00004623-199302000-00002 (1993).
Okuyama, K. et al. Influence of bone mineral density on pedicle screw fixation: A study of pedicle screw fixation augmenting posterior lumbar interbody fusion in elderly patients. Spine J. 1 (6), 402–407. https://doi.org/10.1016/s1529-9430(01)00078-x (2001).
Ponnusamy, K. E., Iyer, S., Gupta, G. & Khanna, A. J. Instrumentation of the osteoporotic spine: Biomechanical and clinical considerations. Spine J. Jan. 11 (1), 54–63. https://doi.org/10.1016/j.spinee.2010.09.024 (2011).
El Saman, A. et al. Reduced loosening rate and loss of correction following posterior stabilization with or without PMMA augmentation of pedicle screws in vertebral fractures in the elderly. Eur. J. Trauma. Emerg. Surg. Oct. 39 (5), 455–460. https://doi.org/10.1007/s00068-013-0310-6 (2013).
Salzmann, S. N. et al. Preoperative MRI-based vertebral bone quality (VBQ) score assessment in patients undergoing lumbar spinal fusion. Spine J. Aug. 22 (8), 1301–1308. https://doi.org/10.1016/j.spinee.2022.03.006 (2022).
Ito, Z. et al. Bone union rate with autologous iliac bone versus local bone graft in posterior lumbar interbody fusion. Spine (Phila Pa) 35(21), E1101-5 (1976). https://doi.org/10.1097/BRS.0b013e3181de4f2e.
Weiser, L. et al. Insufficient stability of pedicle screws in osteoporotic vertebrae: Biomechanical correlation of bone mineral density and pedicle screw fixation strength. Eur. Spine J. 26 (11), 2891–2897. https://doi.org/10.1007/s00586-017-5091-x (2017).
Xu, F. et al. Hounsfield units of the vertebral body and pedicle as predictors of pedicle screw loosening after degenerative lumbar spine surgery. NeuroSurg. Focus. 49 (2), E10. https://doi.org/10.3171/2020.5.focus20249 (2020).
Zou, D., Sun, Z., Zhou, S., Zhong, W. & Li, W. Hounsfield units value is a better predictor of pedicle screw loosening than the T-score of DXA in patients with lumbar degenerative diseases. Eur. Spine J. 29 (5), 1105–1111. https://doi.org/10.1007/s00586-020-06386-8 (2020).
Ehresman, J. et al. Novel MRI-based score for assessment of bone density in operative spine patients. Spine J. 20 (4), 556–562. https://doi.org/10.1016/j.spinee.2019.10.018 (2020).
Ehresman, J. et al. A novel MRI-based score assessing trabecular bone quality to predict vertebral compression fractures in patients with spinal metastasis. J. Neurosurg. Spine 20, 1–8. https://doi.org/10.3171/2019.9.Spine19954 ( 2019).
Ehresman, J. et al. Vertebral bone quality score predicts fragility fractures independently of bone mineral density. Spine J. 21 (1), 20–27. https://doi.org/10.1016/j.spinee.2020.05.540 (2021).
Meunier, P., Aaron, J., Edouard, C. & Vignon, G. Osteoporosis and the replacement of cell populations of the marrow by adipose tissue. A quantitative study of 84 iliac bone biopsies. Clin. Orthop. Relat. Res. 80, 147–154. https://doi.org/10.1097/00003086-197110000-00021 (1971).
Haffer, H. et al. Bone quality in patients with osteoporosis undergoing lumbar fusion surgery: Analysis of the MRI-based vertebral bone quality score and the bone microstructure derived from microcomputed tomography. Spine J. 22 (10), 1642–1650. https://doi.org/10.1016/j.spinee.2022.05.008 (2022).
Hu, Y. H. et al. Novel MRI-based vertebral bone quality score as a predictor of cage subsidence following transforaminal lumbar interbody fusion. J. Neurosurg. Spine 13, 1–9. https://doi.org/10.3171/2022.3.Spine211489 (2022).
Soliman, M. A. R. et al. Vertebral bone quality score independently predicts cage subsidence following transforaminal lumbar interbody fusion. Spine J. . 10 https://doi.org/10.1016/j.spinee.2022.08.002 (2022).
Jones, C. et al. The predictive value of a novel site-specific MRI-based bone quality assessment, end plate bone quality (EBQ), for severe cage subsidence among patients undergoing standalone lateral lumbar interbody fusion. Spine J.. 15 https://doi.org/10.1016/j.spinee.2022.07.085 (2022).
Li, Q. et al. Novel MRI-Based pedicle bone quality score independently predicts pedicle screw loosening after degenerative lumbar Fusion surgery. Orthop. Surg. 16 (10), 2372–2379. https://doi.org/10.1111/os.14146 (2024).
Li, Q. et al. S1 vertebral bone quality score independently predicts pedicle screw loosening following surgery in patients with adult degenerative scoliosis. Spine J. 24 (8), 1443–1450. https://doi.org/10.1016/j.spinee.2024.04.020 (2024).
Spirig, J. M., Sutter, R., Götschi, T., Farshad-Amacker, N. A. & Farshad, M. Value of standard radiographs, computed tomography, and magnetic resonance imaging of the lumbar spine in detection of intraoperatively confirmed pedicle screw loosening—A prospective clinical trial. Spine J. 19 (3), 461–468. https://doi.org/10.1016/j.spinee.2018.06.345 (2019).
Wu, X. et al. Pedicle screw loosening: The value of radiological imagings and the identification of risk factors assessed by extraction torque during screw removal surgery. J. Orthop. Surg, Res. 14 (1). https://doi.org/10.1186/s13018-018-1046-0 (2019).
Tokuhashi, Y., Matsuzaki, H., Oda, H. & Uei, H. Clinical course and significance of the clear zone around the pedicle screws in the lumbar degenerative disease. Spine (Phila Pa) 33(8), 903-908 (1976). https://doi.org/10.1097/BRS.0b013e31816b1eff
Xu, F. et al. Hounsfield units of the vertebral body and pedicle as predictors of pedicle screw loosening after degenerative lumbar spine surgery. Neurosurg. Focus 49 (2), E10. https://doi.org/10.3171/2020.5.Focus20249 (2020).
Sakai, Y. et al. Hounsfield unit of screw trajectory as a predictor of pedicle screw loosening after single level lumbar interbody fusion. J. Orthop. Sci. 23 (5), 734–738. https://doi.org/10.1016/j.jos.2018.04.006 (2018).
Kim, J-B. et al. The effects of spinopelvic parameters and paraspinal muscle degeneration on S1 screw loosening. J. Korean Neurosurg. Soc. 58 (4), 357. https://doi.org/10.3340/jkns.2015.58.4.357 (2015).
Acknowledgements
The authors thank the Biostatistical Center for Clinical Research, Chang Gung Memorial Hospital at Linkou, for statistical consultation.
Funding
This study was supported by Grant CORPG3L0211 from Chang Gung Memorial Hospital.
Author information
Authors and Affiliations
Contributions
Y.H. and J.C. wrote the main manuscript text. Y.Y, Y.H. and M.H. participated in data collection and analysis. T.T. and C.N. prepared the tables and figures. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of Chang Gung Memorial Hospital at Linkou, Taoyuan, Taiwan. The need for patient consent was waived by the committee. (IRB: IRB202100894B0)
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Hu, YH., Chou, JH., Yeh, YC. et al. The MRI-based vertebral bone quality score is a predictor of pedicle screw loosening following instrumented posterior lumbar fusion. Sci Rep 15, 1696 (2025). https://doi.org/10.1038/s41598-025-85625-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-85625-8





