Abstract
To determine an optimal cut-off value for distinguishing early and late recurrence in patients with laryngeal cancer after initial surgery and to evaluate the risk factors for early recurrence. This retrospective study included 328 patients with laryngeal cancer who underwent initial resection in our hospital from January 2014 to April 2018. A minimum P-value approach was used to determine the optimal cut-off value to divide patients into early and late recurrence groups. The clinicopathological characteristics were compared between the two groups. The risk factors for early recurrence were evaluated using logistic regression analysis. The optimal cut-off value to identify between early recurrence (n = 51, 50.5%) and late recurrence (n = 50, 49.5%) was 17 months (p < 1e−17). The overall survival of the late recurrence group (48.36 ± 16.02 months) was longer than the early recurrence group (32.61 ± 19.65 months) significantly (p < 0.001). Lymphovascular invasion (p = 0.038), patients without adjuvant radiotherapy (p = 0.043), advanced tumor, node, metastasis (TNM) stage (p = 0.035), and positive surgical margins (p = 0.045)
were independent risk factors for early recurrence. The best cut-off value to identify early recurrence after initial surgery for laryngeal cancer was 17 months. Intensive follow-up and adjuvant radiotherapy may be beneficial for patients with risk factors for early recurrence.
Similar content being viewed by others
Introduction
Laryngeal squamous cell carcinoma (LSCC) is a common malignant tumor of the head and neck originating from the laryngeal mucosal epithelium, with a higher incidence in males than in females as reported in 2020 (160,265 versus 24,350)1. Worldwide, an estimated 184,615 new laryngeal cancer cases occurred, and approximately 99,840 people died from laryngeal cancer in 20201. Although several studies2,3,4 have shown that radiotherapy has the advantage of organ preservation and shows no differences in survival compared with surgery for local advanced LSCC, surgery has historically been the mainstay treatment for laryngeal cancer and remains irreplaceable to date. Despite significant advances in the treatment of laryngeal cancer in the last decade, the recurrence of tumors after surgery remains a great challenge for surgeons.
Previous studies have shown that the time interval between primary surgery and recurrence is related to the survival of patients in many malignancies, such as pancreatic cancer5, lung cancer6, rectal cancer7, gastric cancer8, and liver cancer9, and have clearly defined “early recurrence”, which is considered to be associated with poorer survival. However, to the best of our knowledge, the association between recurrence interval and survival in LSCC has been rarely evaluated, and the “early recurrence” of LSCC has not been defined. This study aimed to determine an optimal cut-off value for distinguishing early and late recurrence in patients with laryngeal cancer after initial surgery and to evaluate the risk factors for early recurrence.
Materials and methods
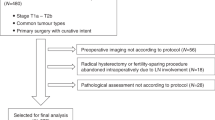
Patients and strategy of adjuvant therapy
The medical records of 377 patients with laryngeal cancer who underwent curative resection without induction chemotherapy in our hospital from January 2014 to April 2018 were retrospectively reviewed. The eligibility criteria were: (1) completion of curative resection; (2) without an invagination of the common artery or internal carotid artery or mediastinum; and (3) without distant metastases. The exclusion criteria were: (1) histologically confirmed non-squamous cell carcinoma (n = 2); (2) concomitant other malignancies at diagnosis (n = 25); (3) incomplete medical data (n = 4); and (4) received chemotherapy or radiotherapy as initial treatment (n = 18). Finally, a total of 328 patients were included in our study.
The indication for surgery as initial treatment was based on NCCN (National Comprehensive Cancer Network) guidelines for laryngeal cancer10, all diseases included were resectable. Surgery was not the initial treatment for patients with distant metastases (stage IVC), an invagination of the common artery or internal carotid artery or mediastinum, and those who requested non-surgical treatment in our hospital. We performed lymph node dissection for all supraglottic diseases, T3-T4 diseases, and T1-T2 diseases with suspected neck metastases based on CT/MRI. Besides, we performed bilateral cervical lymph node dissection for all supraglottic diseases, and other subsites of tumor were selected for unilateral or bilateral lymph node dissection based on CT/MRI examination.
Patients were recommended to adjuvant radiotherapy 4–6 weeks after surgery based on final pathologic risk factors assessment (perineural or lymphovascular invasion, positive margins, subglottic extension over 1 cm, T3-T4 disease with bone invasion, and N2-N3 disease), and total treatment dose for postoperative beds and areas at high risk of recurrence was 60–66 Gy. Concurrent platinum-based chemotherapy was recommended for these patients every 3 weeks for 2–4 cycles unless they had a contraindication to or cannot tolerate chemotherapy.
Follow-up
All patients were followed up every three to six months in the first five years after surgery and annually after five years and had been strongly encouraged to quit smoking and alcohol. Physical examinations, laryngoscope examination, and neck computed tomography (CT) or magnetic resonance imaging (MRI) scans were performed at each follow-up. Chest CT was performed annually. If tumor recurrence was suspected, a positron emission tomography (PET) scan was performed to localize the sites of recurrence, and patients were treated based on multidisciplinary assessment and their consent. Salvage surgery or chemoradiotherapy was recommended for patients without distant metastasis based on the extent of local recurrence, lymph node metastasis, and strategy of initial treatment, palliative chemotherapy was recommended for patients with distant metastasis.
Definition
The tumor staging was classified according to the American Joint Committee on Cancer (AJCC) eighth edition criteria11. The positive margins were defined as the presence of high-grade intraepithelial neoplasia (HGN) or invasive carcinoma at the resection margins on the final pathologic assessment. Residual disease refers to a manifestation of disease within 6 months after surgery, and recurrence is defined as local recurrence, lymph node metastasis, and distant metastasis presented after 6 months of surgery. Overall survival (OS) was calculated from the date of surgery to the date of death or the final follow-up. Recurrence-free survival (RFS) was calculated from the date of surgery to the date of recurrence or last follow-up.
Statistical analysis
The statistical analyses were conducted with SPSS 23.0 (IBM, USA) and software R (version 4.2.1). Normally distributed continuous data parameters were presented as mean ± standard deviation and were compared using the Student t-test. The Fisher test or chi-square test was used for comparing categorical variables. Ordered variables were compared using the Mann-Whitney test was used. The survival rate was calculated by the Kaplan–Meier method and survival curves were compared with the log-rank test. Univariable and multivariable logistic regression models were used to determine factors associated with early recurrence. A minimum p-value approach5,12 (R package survminer: https://CRAN.R-project.org/package=survminer) was used to determine the optimal cut-off value to divide patients into early and late recurrence groups based on overall survival. p < 0.05 was considered statistically significant.
Results
Optimal cut-off value to define early and late recurrence
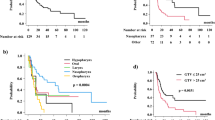
A total of 101 (30.8%) patients experienced tumor recurrence after primary surgery. The best cut-off value to categorize patients into early recurrence (ER) group (n = 51, 50.5%) and late recurrence (LR) group (n = 50, 49.5%) based on OS was 17 months (p < 1e−17) (Table 1; Fig. 1), the c-index was 0.730. The OS of the LR group (48.36 ± 16.02 months) was longer than the ER group (32.61 ± 19.65 months) significantly (p < 0.001). The median RFS was 29 months and 11 months in the LR group and ER group respectively.
The clinicopathological characteristics of included patients
Kaplan-Meier survival curves showed that patients with tumor recurrence had worse OS than those without recurrence, with 5-year OS rates of 28.7% and 92.3%, respectively (p < 0.001) (Fig. 2a). Patients who experienced recurrence were associated with lymph node metastasis (p < 0.001), absence of radiotherapy (p < 0.001), perineural invasion (p < 0.001), lymphovascular invasion (p < 0.001), positive surgical margins (p < 0.001), surgical approaches (p = 0.006), poorer differentiation (p < 0.001), advanced tumor classification (p < 0.001), and advanced tumor, node, metastasis (TNM) stage (p < 0.001) compared with no recurrence. However, there were no significant differences regarding age, gender, tobacco addiction, alcohol addiction, and subsites of tumor (Table 2).
Comparison of early and late recurrence
The 5-year OS rate of included patients was 66.2%, and the 5-year OS rate in patients with ER (21.6%) was worse than those in patients with LR (36.9%) and no recurrence (92.3%) (Fig. 2b). Patients who experienced ER were associated with perineural invasion (p = 0.022), absence of radiotherapy (p = 0.034), lymphovascular invasion (p = 0.032), positive surgical margins (p = 0.006), and advanced TNM stage (p = 0.044) compared with LR (Table 3). In the early recurrence group, 15 (29.4%) patients refused salvage therapy, 9 (17.6%) patients received palliative chemotherapy, 11 (21.6%) patients received chemoradiotherapy, and 16 (31.4%) patients received salvage surgery. In the late recurrence group, 13 (26%) patients refused salvage therapy, 8 (16.0%) patients received palliative chemotherapy, 10 (20.0%) patients received chemoradiotherapy, and 19 (38.0%) patients received salvage surgery. A total of 90 deaths were due to tumor-related factors in the recurrence group, and we found the OS of patients with salvage therapy (37.53 ± 19.56) was better than those without salvage therapy (19.20 ± 7.01) in the early recurrence group (p = 0.001), and the OS of patients with salvage therapy (47.05 ± 13.65) was better than those without salvage therapy (37.77 ± 6.66) in the late recurrence group (p = 0.003). Local recurrence was the most common recurrence site in ER group (72.5%) and LR group (66.0%) (p = 0.48), and the lungs were the most common site of distant metastases in ER group (19.6%) and LR group (22.0%) (p = 0.77).
Risk factors for early recurrence
Univariate analysis showed that perineural invasion, lymphovascular invasion, patients without adjuvant radiotherapy, advanced TNM stage, and positive surgical margins were risk factors for ER. Multivariate analysis showed that lymphovascular invasion (odds ratio: 2.81, 95% confidence interval: 1.06–7.43, p = 0.038), patients without adjuvant radiotherapy (odds ratio: 3.12, 95% confidence interval: 1.04–9.39, p = 0.043), advanced TNM stage (odds ratio: 1.96, 95% confidence interval: 1.05–3.66, p = 0.035), and positive surgical margins (odds ratio: 3.03, 95% confidence interval: 1.02–8.92, p = 0.045) were independent risk factors for ER (Table 4).
The benefit of adjuvant radiotherapy
In the recurrence group, 56 patients were recommended adjuvant radiotherapy based on final pathologic risk factors assessment, 16(28.6%, 11 in the ER group and 5 in the LR group) patients refused radiotherapy due to financial reasons or personal intentions, and 11(68.75%) patients suffered early recurrence, and we found patients who refused radiotherapy were more likely to have early recurrence compared with those who received radiotherapy as we recommended (p = 0.034). We found the overall survival (OS) of lymphovascular invasion group with adjuvant radiotherapy (38.30 ± 16.73) was better than those without radiotherapy (31.27 ± 18.23) (p = 0.028), the OS of positive surgical margins group with adjuvant radiotherapy (38.31 ± 19.71) was better than those without radiotherapy (29.20 ± 14.10) (p = 0.034), and the OS of stage III and IV with adjuvant radiotherapy (37.27 ± 15.79) was better than those without radiotherapy (30.08 ± 15.08) (p = 0.048).
Discussion
Despite considerable achievements have been made in the surgical management of tumors in recent years, postoperative tumor recurrence remains a significant concern for surgeons, and early recurrence (ER) has been reported as a risk factor for survival in many tumors6,7,9. Studies have shown that approximately 30% of patients with LSCC experienced recurrence after treatment13,14, however, the association between recurrence interval and prognosis in LSCC has been rarely evaluated and the ER of LSCC has not been defined. Philippe et al.15 reported that the time to locoregional recurrence in laryngeal cancer was a prognostic factor correlated with post-recurrence survival, and recurrence within 12 months was significantly associated with poorer survival regardless of primary treatment. However, patients with distant metastases were excluded and the 12-month recurrence interval had not been defined in this study. Our study was the first study to define ER and LR of LSCC after surgery, we found 17 months was the best cut-off value to distinguish ER and LR. Besides, we evaluated all recurrence patterns of laryngeal cancer including distant metastasis compared with Philippe Gorphe’s study. Consistently, we found patients with ER had worse OS than those with LR. In our opinion, recurrence-free survival (RFS) is associated with the biological behavior of tumors, poor tumor biology may result in shorter RFS and quick progression to death, and patients with better tumor biological behavior are more likely to have better RFS and overall survival.
The standard of care for patients with laryngeal cancer remains controversial. Previous studies2,16,17have found that there is no difference in survival between surgery and radiation therapy for early-stage LSCC. However, other studies14,18,19showed that patients with advanced LSCC who underwent surgery had better overall survival than those who received radiotherapy or chemoradiotherapy. Additionally, salvage surgery is the only standard of care for patients with recurrence cancer after non-surgical treatment20,21. Nowadays, larynx preservation surgery has become the main approach for surgical treatment of laryngeal cancer. Steven M Sperry et al.22 suggested that supracricoid partial laryngectomy (SCPL) seemed to be a feasible option for patients with advanced LSCC, even after the failure of radiation therapy, Xin Xia et al.23 found SCPL could be used to avoid total laryngectomy in some patients with advanced LSCC, and Vincent Vander Poorten et al.20 indicated that transoral laser surgery (TLS) could be selected in recurrence LSCC cases with limited localized lesions. Similarly, we found surgical approaches were not a risk factor for ER. TLS or partial laryngectomy can be performed to preserve the larynx on the premise of following indications strictly.
Recurrence of tumors is associated with poor prognosis, it is essential to identify the recurrence pattern of tumors for more targeted follow-up. In the present study, we have found local recurrence is the most common recurrence site, similar results have been reported in other studies14,24,25, the possible reason is nodal and distant spread are limited by the cartilage barrier and lack of lymphatic drainage in the glottic region. Besides, we have found lungs are the most common site of distant metastases in both ER group and LR group, which is consistent with Huang et al.26. Therefore, in addition to laryngoscopy and cervical CT or MRI, chest CT is essential for postoperative follow-up.
Lymphovascular invasion refers to lymphatic or blood arteries invaded by tumors, which is related to the recurrence and prognosis of tumors. Studies27,28 reported that lymphovascular invasion increased the risk of local recurrence in patients with laryngeal cancer significantly. Positive surgical margins imply that the margins of resection are insufficient, which may lead to early recurrence. Tassone P et al.29reported that positive surgical margins were associated with recurrence of LSCC and poorer survival. Radiotherapy plays an integral role in the treatment of laryngeal cancers, adjuvant radiotherapy for patients with high-risk postoperative features may achieve better local control and reduce the risk of recurrence30,31. TNM stage represents the invasiveness of the tumors, which has been reported as an independent risk factor for disease-free survival in many multivariate analyses32,33. Similarly, we found lymphovascular invasion, patients without adjuvant radiotherapy, advanced TNM stage, and positive surgical margins were independent risk factors for early recurrence in our study, and adjuvant radiotherapy improved the overall survival even when patients were exposed to other risk factors. Consequently, adjuvant radiotherapy is recommended for this high-risk population.
Salvage therapy is critical for recurrent laryngeal cancer. Salvage surgery is the standard treatment for laryngeal cancer after failure of initial radiotherapy, and total laryngectomy is the classical salvage approach. Recent studies20,34,35 have shown that partial laryngectomy also can be used to treat limited localized disease after radiotherapy failure with a comparable survival rate and preserve laryngeal function. Sati Akbaba et al.36 reported that salvage radiotherapy for recurrent laryngeal cancer after first-line treatment with surgery alone improved the local progression-free survival rate. Similarly, we found salvage total laryngectomy and lymph node dissection for limited localized disease and chemoradiotherapy for those who underwent surgery alone prolonged the survival of patients. Consequently, intensive follow-up is recommended for this high-risk population and salvage therapy is required once tumor recurrence is detected.
Perineural invasion, lymph node metastasis, and nodal extracapsular extension are common negative prognostic factors, perineural invasion correlates with tumor recurrence and spread and predicts poor survival in head and neck carcinomas, including LSCC37. Jacques Bernier et al.38 found that nodal extracapsular spread was the most significant prognostic factor for poor outcomes in patients with laryngeal cancer. In our study, perineural invasion and lymph node metastasis were not independent risk factors for early recurrence, the possible reason may be selection bias caused by single-institution retrospective studies and many patients with T1-T2 glottic disease who underwent transoral surgery without lymph node dissection. Nevertheless, we found that perineural invasion and lymph node metastasis were significantly associated with the recurrence of LSCC (p < 0.001). The nodal extracapsular extension has not been included in our study, because only 8 patients with extracapsular extension received initial surgery instead of neoadjuvant chemotherapy.
The present study has some limitations. First, this study is subject to the limitations of retrospective studies. Second, this single-institution study may lead to a selection bias. Finally, the nodal extracapsular extension has not been included in our study. Therefore, multicenter prospective studies are needed to validate our results.
Conclusion
The best cut-off value to distinguish early and late recurrence after laryngeal cancer surgery was 17 months, and more intensive follow-up and adjuvant radiotherapy for the high-risk population may be beneficial.
Data availability
Data is available upon reasonable request, and Desheng Wang should be contacted if someone wants to request the data from this study.
References
Sung, H., Ferlay, J. & Siegel, R. L. Global Cancer statistics 2020: GLOBOCAN estimates of incidence and Mortality Worldwide for 36 cancers in 185 countries. Cancer J. Clin. 71, 209–249 (2021).
Zhang, H., Travis, L. B. & Chen, R. Impact of radiotherapy on laryngeal cancer survival: a population-based study of 13,808 US patients. Cancer 118, 1276–1287 (2012).
Lefebvre, J. L. & Rolland, F. Tesselaar Met al. Phase 3 randomized trial on larynx preservation comparing sequential vs alternating chemotherapy and radiotherapy. J. Natl Cancer Inst. 101, 142–152 (2009).
Wolf, G. T., Fisher, S. G. & Hong, W. K. Induction chemotherapy plus radiation compared with surgery plus radiation in patients with advanced laryngeal cancer. N. Engl. J. Med. 324, 1685–1690 (1991).
Yamamoto, Y., Ikoma, H. & Morimura, R. Optimal duration of the early and late recurrence of pancreatic cancer after pancreatectomy based on the difference in the prognosis. Pancreatology: Official J. Int. Association Pancreatology (IAP) [et al]. 14, 524–529 (2014).
Kiankhooy, A. & Taylor, M. D. LaPar DJet al. Predictors of early recurrence for node-negative t1 to t2b non-small cell lung cancer. Ann. Thorac. Surg. 98, 1175–1183 (2014).
Zheng, Z. et al. Defining and predicting early recurrence in patients with locally advanced rectal cancer treated with neoadjuvant chemoradiotherapy. Eur. J. Surg. Oncology: J. Eur. Soc. Surg. Oncol. Br. Association Surg. Oncol. 46, 2057–2063 (2020).
Xu, B. B., Lu, J. & Zheng, Z. F. The predictive value of the preoperative C-reactive protein-albumin ratio for early recurrence and chemotherapy benefit in patients with gastric cancer after radical gastrectomy: using randomized phase III trial data. Gastric cancer: Official J. Int. Gastric Cancer Association Japanese Gastric Cancer Association. 22, 1016–1028 (2019).
Yamamoto, Y., Ikoma, H. & Morimura, R. Optimal duration of the early and late recurrence of hepatocellular carcinoma after hepatectomy. World J. Gastroenterol. 21, 1207–1215 (2015).
Caudell, J. J. & Gillison, M. L. Maghami eet al. NCCN Guidelines® insights: Head and Neck cancers, Version 1.2022. J. Natl. Compr. Cancer Network: JNCCN. 20, 224–234 (2022).
Ho, A. S., Kim, S. & Tighiouart, M. Association of Quantitative Metastatic Lymph Node Burden with Survival in Hypopharyngeal and Laryngeal Cancer. JAMA Oncol. 4, 985–989 (2018).
Altman, D. G., Lausen, B., Sauerbrei, W. & Schumacher, M. Dangers of using optimal cutpoints in the evaluation of prognostic factors. J. Natl Cancer Inst. 86, 829–835 (1994).
Haapaniemi, A., Koivunen, P. & Saarilahti, K. Laryngeal cancer in Finland: a 5-year follow-up study of 366 patients. Head neck. 38, 36–43 (2016).
Haapaniemi, A. et al. Predictive factors and treatment outcome of laryngeal carcinoma recurrence. Head neck. 39, 555–563 (2017).
Gorphe, P., Tao, Y. & Blanchard, P. Relationship between the time to locoregional recurrence and survival in laryngeal squamous-cell carcinoma. European archives of oto-rhino-laryngology: official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : affiliated with the German society for Oto-Rhino-Laryngology -. Head Neck Surg. 274, 2267–2271 (2017).
Hinerman, R. W., Mendenhall, W. M., Amdur, R. J., Villaret, D. B. & Robbins, K. T. Early laryngeal cancer. Curr. Treat. Options Oncol. 3, 3–9 (2002).
Wang, W. L., Zheng, H. W., Zhang, L. H. & Yu, L. S. Effect of treatment modality on the long-term survival of patients with early glottic squamous cancer: a retrospective cohort study based on the SEER database. Annals Translational Med. 10, 440 (2022).
Timmermans, A. J., de Gooijer, C. J., Hamming-Vrieze, O., Hilgers, F. J. & van den Brekel, M. W. T3-T4 laryngeal cancer in the Netherlands Cancer Institute; 10-year results of the consistent application of an organ-preserving/-sacrificing protocol. Head neck. 37, 1495–1503 (2015).
Dziegielewski, P. T. et al. Klein M Primary total laryngectomy versus organ preservation for T3/T4a laryngeal cancer: a population-based analysis of survival. Journal of otolaryngology - headneck surgery = Le Journal d’oto-rhino-laryngologie et de chirurgie cervico-faciale ; 41 Suppl 1:S56-64. (2012).
Vander Poorten, V., Meulemans, J. & Beitler, J. J. Salvage surgery for residual or recurrent laryngeal squamous cell carcinoma after (Chemo)radiotherapy: oncological outcomes and prognostic factors. Eur. J. Surg. Oncology: J. Eur. Soc. Surg. Oncol. Br. Association Surg. Oncol. 47, 2711–2721 (2021).
Steuer, C. E., El-Deiry, M., Parks, J. R., Higgins, K. A. & Saba, N. F. An update on larynx cancer. Cancer J. Clin. 67, 31–50 (2017).
Sperry, S. M., Rassekh, C. H., Laccourreye, O. & Weinstein, G. S. Supracricoid partial laryngectomy for primary and recurrent laryngeal cancer. JAMA otolaryngology– head neck Surg. 139, 1226–1235 (2013).
Xia, X., Zhu, Y. Y. & Diao, W. W. Matched-pair analysis of survival in the patients with T3 laryngeal squamous cell carcinoma treated with supracricoid partial laryngectomy or total laryngectomy. OncoTargets Therapy. 11, 7947–7953 (2018).
Ho, A. S. et al. Decision making in the management of recurrent head and neck cancer. Head neck. 36, 144–151 (2014).
Sandulache, V. C., Vandelaar, L. J. & Skinner, H. D. Salvage total laryngectomy after external-beam radiotherapy: a 20-year experience. Head neck. 38 (Suppl 1), E1962–1968 (2016).
Huang, X. W. et al. Effects of anesthetic technique on postoperative pulmonary metastasis in patients undergoing laryngectomy. Cancer Manage. Res. 12, 5515–5525 (2020).
Tsai, M. H., Chuang, H. C. & Lin, Y. T. al. Survival outcomes and predictors for patients who failed Chemoradiotherapy/Radiotherapy and Underwent Salvage Total Laryngectomy. Int. J. Environ. Res. Public Health ; 18. (2021).
Yilmaz, T., Hosal, A. S., Gedikoğlu, G., Onerci, M. & Gürsel, B. Prognostic significance of vascular and perineural invasion in cancer of the larynx. Am. J. Otolaryngol. 19, 83–88 (1998).
Tassone, P., Savard, C. & Topf, M. C. Association of Positive Initial margins with survival among patients with squamous cell carcinoma treated with total laryngectomy. JAMA otolaryngology– head neck Surg. 144, 1030–1036 (2018).
Mattioli, F. et al. The role of adjuvant therapy in pT4N0 laryngectomized patients: multicentric observational study. Head neck. 45, 197–206 (2023).
De Stefani, A., Magnano, M. & Cavalot, A. Adjuvant radiotherapy influences the survival of patients with squamous carcinoma of the head and neck who have poor prognoses. Otolaryngology–head neck Surgery: Official J. Am. Acad. Otolaryngology-Head Neck Surg. 123, 630–636 (2000).
Lin, Q., Lin, S. & Chen, W. Controlling Nutritional Status (CONUT) score is a prognostic marker for laryngeal cancer patients with curative resection. Head neck. 44, 2834–2841 (2022).
Zhang, S. Y., Lu, Z. M. & Luo, X. N. Retrospective analysis of prognostic factors in 205 patients with laryngeal squamous cell carcinoma who underwent surgical treatment. PloS One. 8, e60157 (2013).
Marioni, G., Marchese-Ragona, R., Lucioni, M. & Staffieri, A. Organ-preservation surgery following failed radiotherapy for laryngeal cancer. Evaluation, patient selection, functional outcome and survival. Curr. Opin. Otolaryngol. Head Neck Surg. 16, 141–146 (2008).
Russo, E., Costantino, A. & Veneroni, M. V. Transoral Laser Microsurgery in recurrent laryngeal Cancer: a systematic review and Meta-analysis. Laryngoscope 133, 1425–1433 (2023).
Akbaba, S., Held, T. & Lang, K. Salvage radiotherapy for recurrent hypopharyngeal and laryngeal squamous cell carcinoma (SCC) after first-line treatment with surgery alone: a 10-year single-centre experience. Radiation Oncol. (London England). 14, 34 (2019).
Scanlon, C. S., Banerjee, R. & Inglehart, R. C. Galanin modulates the neural niche to favour perineural invasion in head and neck cancer. Nat. Commun. 6, 6885 (2015).
Bernier, J., Cooper, J. S. & Pajak, T. F. Defining risk levels in locally advanced head and neck cancers: a comparative analysis of concurrent postoperative radiation plus chemotherapy trials of the EORTC (#22931) and RTOG (# 9501). Head neck. 27, 843–850 (2005).
Acknowledgements
None.
Funding
Special Finance Project of Fujian Province [Grant numbers: 2019B022].
Author information
Authors and Affiliations
Contributions
Longxiang Zheng designed the work and acquired and analyzed data, Qin Lin wrote and drafted it, Xiaoqiang Chen revised the manuscript, and Desheng Wang approved the manuscript and agreed to be accountable for all aspects of the work. Qin Lin analyzed data, responded to reviewers, revised this manuscript, and drafted the revised manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical statement
This study was performed following the principles of the Declaration of Helsinki and its amendments and was approved by the Ethics Committee of Fujian Medical University Union Hospital (ethical approval code: 2023KY127). Informed consent from participants was waived by the Fujian Medical University Union Hospital ethical committee because this was a retrospective study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lin, Q., Zheng, L., Chen, X. et al. Definition and risk factors for early recurrence in patients with laryngeal cancer after initial surgery. Sci Rep 15, 13033 (2025). https://doi.org/10.1038/s41598-025-89223-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-89223-6