Abstract
This study aimed to evaluate the effectiveness of combining initial hemoglobin levels with the shock index for predicting the need for life-saving interventions (LSI) in pediatric patients with blunt liver and spleen injuries (BLSI), specifically tailored to different age groups. This was a multicenter retrospective cohort study of pediatric patients with BLSI in Japan. The area under the receiver operating characteristic curve (AUROC) were used to assess predictive accuracy. The study included 1,370 patients. LSI was required in 59 of 247 (23.9%) aged 1 to 6 years, 100 of 402 (24.9%) aged 7 to 12 years, and 125 of 297 (42.1%) patients aged 13 to 16 years. Within each specific age group, the predictability was categorized as fair and appeared higher than that of the entire cohort or when using either parameter alone. Notably, in the 1 to 6-year age group, the combined values showed the highest predictability, which was statistically superior to the shock index alone (AUROC of 0.770 vs. 0.671, P = 0.025). Tailoring initial hemoglobin levels and shock index to specific age groups enhances predictability of LSI in pediatric BLSI, showing a fair level of predictive accuracy.
Similar content being viewed by others
Introduction
Abdominal injuries represent about 25% of major trauma incidents in pediatric patients. The majority of these abdominal traumas are of a blunt nature, predominantly affecting the liver and spleen1,2. Delayed intervention may lead to fatal consequences. Therefore, it is critical to identify simple, reliable, and objective predictors that can be used for the early identification of patients who will most benefit from timely and effective management3,4.
An earlier study suggested that a lower initial hematocrit was associated with intra-abdominal injuries following pediatric blunt trauma5. A recent large study also emphasized that initial low hemoglobin level was linked to failure of non-operative management, as well as the need for blood transfusions, in pediatric patients with blunt liver and spleen injuries (BLSI)6. Importantly, normal hemoglobin values vary across different age groups, necessitating the evaluation of hemoglobin based on specific age categories7.
The shock index, defined as the heart rate to systolic blood pressure ratio, is commonly employed as a predictor of mortality in trauma patients. In pediatric trauma cases, the shock index pediatric age-adjusted (SIPA) has proven to be superior to shock index unadjusted for age in identifying severely injured children who require early transfusion, emergency surgery, or are at risk for death8,9. Of note, SIPA has been demonstrated to be useful in the management of children with BLSI10. Considering age-related variations in shock index is crucial for a more accurate assessment in pediatric trauma care, especially in predicting need for urgent interventions.
Given these findings, we hypothesized that the combination of hemoglobin levels and shock index in age-specific groups would be more useful in predicting the need for life-saving interventions (LSI) in pediatric BLSI.
Accordingly, we seek to analyze the utility of initial hemoglobin levels in conjunction with the shock index based on age-specific categories, as predictors for LSI, using a cohort study of pediatric BLSI cases in Japan.
Methods
Study design
This was a pre-planned sub-analysis of the SHIPPs (Splenic and Hepatic Injury in Pediatric Patients) study, which was a multicenter retrospective cohort study. The SHIPPs study involved 83 institutions and included 1,462 pediatric patients (≤ 16 years of age) with BLSI from 2008 to 2019 in Japan11. The SHIPPs study included patients admitted to an emergency care setting with at least an Abbreviated Injury Scale (AIS) grade ≥ I BLSI, as detected by any imaging method or operative findings. This study conforms to the principles outlined in the Declaration of Helsinki. Okayama University Hospital Ethics Committee approved the study on December 23, 2022. The approval was for the study titled ‘Age-specific assessment of initial hemoglobin levels and shock index for predicting life-saving interventions in pediatric blunt liver and spleen injuries’, under Study ID: K2302-006. Furthermore, the committee waived the requirement for written informed consent. The study followed the Standards for Reporting of Diagnostic Accuracy (STARD) reporting guidelines for diagnostic accuracy studies12.
Study participants
Among the study candidates, we excluded those who had duplicated records due to inter-hospital transfers, as well as cases with an AIS of 6 in any body region or treatment limitations due to severe traumatic brain injury (TBI), defined as a head AIS ≥ 511 we further excluded patients who were younger than 1 year old because the SIPA was not defined for this age group13. Additionally, we excluded those with missing data on systolic blood pressure, heart rate at arrival, or initial hemoglobin levels.
Grouping and definitions
Patients were divided into three age-groups based on previous studies regarding SIPA: 1 to 6 years old, 7–12 years old, and 13 to 16 years old8,9,13,14,15. Abnormal SIPA was defined as greater than 1.2 for the 1 to 6-year-old age group, greater than 1.0 for the 7 to 12-year-old age group, and greater than 0.9 for the 13 to 16-year-old age group, based on these studies. In cases where patients were transferred from another hospital, their vital signs and laboratory data from the first-visit facility were used if available.
Outcomes
Our primary outcome was the necessity for LSI. LSI was defined as the requirement for any component of blood transfusion or the need for transcatheter arterial embolization or laparotomy due to bleeding from BLSI10,14,16. Blood transfusion components included packed red blood cells, fresh frozen plasma, platelets, cryoprecipitate, or fibrinogen administered within 24 h of hospital arrival, regardless of BLSI severity. We examined two secondary outcomes: 1) hemostatic interventions for bleeding due to BLSI including transcatheter arterial embolization or laparotomy, and 2) blood transfusions within 24 h of hospital arrival.
Statistical analysis
Continuous variables are shown as median and interquartile range values, unless otherwise described. Categorical variables are presented as frequencies and percentages. Comparisons between two groups were made using the Mann–Whitney U test for continuous variables and chi-square test for categorical variables. We evaluated the predictability of the need for LSI by analyzing initial hemoglobin levels and shock index values for all ages and across three age groups. The predictive accuracy in each of these categories was determined using the area under the receiver operating characteristic curve (AUROC). The cut-off value for prediction was established using the Youden index. Next, we performed a binary logistic regression analysis with the need for LSI as the dependent variable and initial hemoglobin levels and shock index as covariates. This analysis yielded predicted probabilities, from which we derived the AUROC to assess the combined predictability of initial hemoglobin levels and the shock index for determining the need for LSI. To interpret the AUROC values, we adopted the following standard categorical ratings: 0.5 to 0.6 as failed, 0.6 to 0.7 as poor, 0.7 to 0.8 as fair, 0.8 to 0.9 as good, and 0.9 to 1.0 as excellent17,18. When evaluating the performance of two or more diagnostic tests, a higher AUROC value generally indicates better diagnostic accuracy18. To conduct statistical comparisons between the AUROCs of different models within the same cohort, we employed the Z statistic for pairwise comparisons, thereby determining any significant differences in their diagnostic accuracy19.
As sensitivity analyses, we excluded patients transferred to or from other hospitals. Additionally, we conducted another sensitivity analysis excluding those who had severe TBI, defined as a head Abbreviated Injury Scale score of 4 or 5, which can potentially affect the shock index20.
All tests were two-tailed, and a P value of < 0.05 was considered statistically significant. We performed all statistical analysis using IBM SPSS Statistics 26 (IBM SPSS, Chicago, IL), Prism 10.0.3 (GraphPad, San Diego, CA), and Microsoft Excel for Mac Version 16.79.2.
Results
Among 1,462 patients registered in the SHIPPs study, 1,370 were included in the final analysis as shown in Fig. 1. Of these, 365 were aged 1 to 6 years, 619 were aged 7 to 12 years, and 386 were aged 13 to 16 years.
Patient characteristics
The baseline characteristics of each age category patient cohort are presented in Table 1 and Table S1. Initial hemoglobin levels were significantly lower in the LSI group compared to the no LSI group: 10.7 vs. 12.1 g/dL in the 1 to 6-year age group; 11.8 vs. 12.6 g/dL in the 7 to 12-year age group; and 12.9 vs. 13.6 g/dL in the 13 to 16-year age group, with P < 0.001 for each comparison, respectively. Meanwhile, the shock index was significantly higher in the LSI group: 1.27 vs. 1.10 in the 1 to 6-year age group; 0.96 vs. 0.85 in the 7 to 12-year age group; and 0.83 vs. 0.69 in the 13 to 16-year age group, with P < 0.001 for each comparison, respectively. There were no patients who died from hemorrhagic shock due to BLSI without receiving any LSI.
Outcomes
Table 2 presents the outcomes for specific age groups. LSI were required in 92 out of 365 patients (25.2%) aged 1 to 6 years, 139 out of 619 patients (22.5%) aged 7 to 12 years, and 154 out of 386 patients (39.9%) aged 13 to 16 years, respectively. In terms of hemostatic procedures, transcatheter arterial embolization was more commonly performed than laparotomy across all age groups. A majority of patients in each group received blood transfusions within 24 h of hospital arrival.
Primary outcome
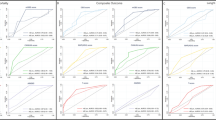
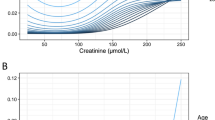
Table 3 shows the predictability for all ages and for specific age groups of hemoglobin levels, shock index values, and their combination in predicting the need for LSI. The ROC curves for hemoglobin, shock index, and their combination for the entire cohort and age-specific groups are illustrated in Fig. 2. Both initial hemoglobin levels and shock index demonstrated improved predictive performance for LSI in age-specific groups compared to the entire cohort encompassing all ages. Cut-off values for hemoglobin, determined by the Youden index, were 10.8 g/dL for the 1 to 6-year age group, 11.9 g/dL for the 7 to 12-year age group, and 12.1 g/dL for the 13 to 16-year age group. Similarly, cut-off values for the shock index were 1.20 for the 1 to 6-year age group, 1.03 for the 7 to 12-year age group, and 0.93 for the 13 to 16-year age group. When combining hemoglobin levels and the shock index, the predictability for the entire cohort was categorized as poor, with an AUROC of 0.665 (95% CI, 0.630 to 0.700). In contrast, predictability was categorized as fair within each specific age group. In the 1 to 6-year age group, the shock index in conjunction with the initial hemoglobin levels demonstrated statistically superior predictive performance compared to the shock index alone (AUROC of 0.770 vs. 0.671, P = 0.025; Z = 2.245).
Secondary outcomes
As for the secondary outcomes, hemostatic interventions including transcatheter arterial embolization or laparotomy due to BLSI was required in 61/365 (16.7%) for the 1 to 6-year age group, 110/619 (17.8%) for the 7 to 12-year age group, and 110/386 (28.5%) for the 13 to 16-year age group. While any blood transfusions within 24 h of hospital arrival was required in 75/365 (20.5%) for the 1 to 6-year age group, 84/619 (13.6%) for the 7 to 12-year age group, and 99/386 (25.6%) for the 13 to 16-year age group. The AUROC appeared to decrease when utilized to predict the need for hemostatic interventions including transcatheter arterial embolization or laparotomy for BLSI, in comparison to predicting the need for LSI (Table S2 & Figure S1). Conversely, the AUROC appeared to increase when predicting the necessity for blood transfusions within 24 h of hospital arrival, in comparison to predicting the need for LSI (Table S3 & Figure S2).
Sensitivity analysis
A sensitivity analysis is presented in Table S4 and Figure S3, where patients transferred to or from other hospitals were excluded. Another sensitivity analysis, which excluded patients with severe TBI, are detailed in Table S5 and Figure S4. Similar results were obtained: combined variables, categorized by age, improved predictive performance for LSI compared to either parameter alone or a combined assessment in the entire cohort.
Discussion
In this multicenter retrospective cohort study, we found that the combined use of initial hemoglobin levels and the shock index, when tailored to specific age groups, consistently yielded a fair level of predictive performance. This was in contrast to the lower predictive accuracy observed when applying either parameter alone or a combined assessment to the entire cohort for determining the need for LSI in pediatric patients with BLSI. Specifically, the predictability of combined values significantly improved in the 1 to 6-year age group compared to the shock index alone. The utility of this approach is highlighted by our findings that hemoglobin levels and shock index cutoff values vary among different age groups. These variations enhance the predictability of the need for LSI in these diverse pediatric populations.
Although normal hemoglobin levels vary among different races/ethnicities and regions21, in general, pediatric populations tend to have lower normal hemoglobin values that increase with age: approximately 12.5 g/dL for ages 2 to 6 years; 13.5 g/dL for 6 to 12 years; and 14.5 g/dL for males and 14.0 g/dL for females between 12 to 18 years7. The observation that the highest predictive performance for the need for LSI is found in the 1 to 6-year age group suggests that children in this age group may reach critical thresholds more rapidly in the event of trauma, likely due to their generally lower hemoglobin levels. The cut-off values we obtained for the shock index are in near-perfect alignment with those previously suggested by SIPA: > 1.2 for the 1 to 6-year-old age group, > 1.0 for the 7 to 12-year-old age group, and > 0.9 for the 13 to 16-year-old age group8,9,13,15,22. In the 1 to 6-year age group, the potential reason that combined variables are statistically superior to shock index alone could be that tachycardia in younger children is more frequently induced by factors such as pain and agitation, rather than solely by hypovolemic shock23. The variation in AUROC across different age groups may be in part attributed to the fact that injury patterns differ among these groups. Analysis of baseline characteristics reveals significant demographic variability across age groups, as demonstrated in previous studies24,25, which could markedly affect the AUROC. For instance, injury due to falls from height exhibit distinct patterns in various age cohorts. The proportion of pedestrian injuries is higher among younger children.
In our secondary outcome analyses, we observed a variation in the AUROC when predicting different outcomes: the combined AUROC of hemoglobin and shock index appeared higher for predicting the necessity of blood transfusions within 24 h of hospital arrival compared to the need for hemostatic interventions across any age-specific group. This may be due to the direct relationship between hemoglobin levels and the decision to administer blood transfusions. Our findings remained consistent even after excluding patients who were transferred between hospitals or those with severe TBI, indicating the robustness and validity of our results.
Our analysis revealed that the combination of initial hemoglobin levels and shock index, categorized by age, enhances predictive performance rather than applying either parameter alone or even a combined assessment in the entire cohort, aligning with our hypothesis. Although it is important to acknowledge that these two parameters alone cannot perfectly discriminate the need for LSI, their combined use considering age-specific groups and being readily and rapidly available, could aid physicians in making determinations and thereby enhance prompt management in pediatric BLSI patients.
This study has several limitations. First, the study cohort is restricted to pediatric patients with BLSI. While liver and spleen injuries are common in blunt abdominal trauma, our findings cannot be directly applied to all patients presenting to the emergency department with blunt abdominal injuries. Second, the decision regarding the timing and choice of LSI, such as transcatheter arterial embolization or laparotomy, was entirely at the discretion of the attending physician or institution. This variability could introduce a degree of bias and inconsistency in the treatment approach, potentially affecting the generalizability of our findings. Third, although prehospital fluid resuscitation for pediatric trauma patients is relatively uncommon in Japan26, we lacked data on whether the patients received fluid resuscitation in the prehospital setting. This could affect the initial hemoglobin levels and vital signs27, which are crucial parameters in our study. Additionally, nearly 30% of the study cohort were transferred from other hospitals. Although we used the vital signs and laboratory data from the original facility where available, the exact proportion of patients with original versus transfer-time data is unknown. Such data could differ significantly due to initial treatments such as fluid administration. Nonetheless, our results remained robust even after excluding patients who were transferred between hospitals. Fourth, the number of patients registered varied significantly across institutions, which could affect robustness (Figure S5). Moreover, this study included patients with BLSI of any severity, from minor to critical injuries, as identified through imaging or operative findings. However, the higher-than-expected rate of LSI may be explained by differences in practice patterns between Japan and the United States, where significantly fewer angiographic procedures are performed28. Lastly, we did not perform external validation with other datasets, which may limit the applicability of our findings in other clinical settings.
Despite these limitations, our study, using a large cohort, provides important insights into the specific needs for LSI in pediatric BLSI patients. It emphasizes the usefulness of utilizing a combined approach of initial hemoglobin levels and shock index, especially considering their variability across different age groups. While the identified SIPA and hemoglobin cut-off values provide objective reference points, they should be interpreted alongside clinical assessment rather than used in isolation. These values may help clinicians rapidly identify pediatric patients with BLSI at risk for LSI; however, real-time decision-making should remain multifactorial, incorporating additional clinical parameters and assessments.
Conclusions
This multicenter retrospective study revealed that an age-specific approach, combining initial hemoglobin levels with the shock index, consistently improves the predictability of LSI to a fair level in pediatric patients with BLSI, compared to using each parameter independently or a general assessment across the entire cohort. Notably, this combined approach showed statistical superiority over the shock index alone, particularly in the 1 to 6-year age group. These findings suggest that our method is a more useful tool for physicians, facilitating timely and accurate decision-making, and thus may enhance the management of pediatric BLSI.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Gaines, B. A. Intra-abdominal solid organ injury in children: Diagnosis and treatment. J. Trauma 67(2 Suppl), S135–S139. https://doi.org/10.1097/TA.0b013e3181adc17a (2009).
Lynch, T., Kilgar, J. & Al, S. A. Pediatric abdominal trauma. Curr. Pediatr. Rev. 14(1), 59–63. https://doi.org/10.2174/1573396313666170815100547 (2018).
Poletti, P. A. et al. Blunt abdominal trauma patients: can organ injury be excluded without performing computed tomography?. J. Trauma 57(5), 1072–1081. https://doi.org/10.1097/01.ta.0000092680.73274.e1 (2004).
Cook, S. H., Fielding, J. R. & Phillips, J. D. Repeat abdominal computed tomography scans after pediatric blunt abdominal trauma: Missed injuries, extra costs, and unnecessary radiation exposure. J. Pediatr. Surg. 45(10), 2019–2024. https://doi.org/10.1016/j.jpedsurg.2010.06.007 (2010).
Holmes, J. F. et al. Identification of children with intra-abdominal injuries after blunt trauma. Annals Emerg. Med. 39(5), 500–509. https://doi.org/10.1067/mem.2002.122900 (2002).
Stottlemyre, R. L. et al. Hemodilution in pediatric trauma: Defining the expected hemoglobin changes in patients with liver and/or spleen injury: An ATOMAC+ secondary analysis. J. Surg. 58(2), 325–329. https://doi.org/10.1016/j.jpedsurg.2022.10.044 (2023).
Janus, J. & MOERSCHEL SK.,. Evaluation of anemia in children. Am. Fam. Physician. 81(12), 1462–1471 (2018).
Acker, S. N. et al. Shock index, pediatric age-adjusted (SIPA) is more accurate than age-adjusted hypotension for trauma team activation. Surgery. 161(3), 803–807. https://doi.org/10.1016/j.surg.2016.08.050 (2017).
Reppucci, M. L. et al. Pediatric age-adjusted shock index as a tool for predicting outcomes in children with or without traumatic brain injury. J. Trauma & Acute Care Surg.. 91(5), 856–860. https://doi.org/10.1097/TA.0000000000003208 (2021).
Linnaus, M. E. et al. Prospective validation of the shock index pediatric-adjusted (SIPA) in blunt liver and spleen trauma: An ATOMAC + study. J. Pediatr. Surg. 52(2), 340–344. https://doi.org/10.1016/J.JPEDSURG.2016.09.060 (2017).
Katsura, M. et al. Therapeutic strategies for pseudoaneurysm following blunt liver and spleen injuries: A multicenter cohort study in the pediatric population. J. Trauma & Acute Care Surg. 94(3), 433–442. https://doi.org/10.1097/TA.0000000000003813 (2023).
Bossuyt, P. M. et al. STARD 2015: An updated list of essential items for reporting diagnostic accuracy studies. BMJ. 351(October), 1–9. https://doi.org/10.1136/bmj.h5527 (2015).
Cuenca, C. M., Borgman, M. A., April, M. D., Fisher, A. D. & Schauer, S. G. Validation of the age-adjusted shock index for pediatric casualties in Iraq and Afghanistan. Mil. Med. Res. 7(1), 1–7. https://doi.org/10.1186/s40779-020-00262-8 (2020).
Acker, S. N., Ross, J. T., Partrick, D. A., Tong, S. & Bensard, D. D. Pediatric specific shock index accurately identifies severely injured children. J. Pediatr. Surg. 50(2), 331–334. https://doi.org/10.1016/j.jpedsurg.2014.08.009 (2015).
Gandhi, G. et al. Predictive value of the shock index (SI) compared to the age-adjusted pediatric shock index (SIPA) for identifying children that needed the highest-level trauma activation based on the presence of consensus criteria. J. Pediatr. Surg. 55(9), 1761–1765. https://doi.org/10.1016/j.jpedsurg.2019.09.032 (2020).
Stevens, J. et al. Novel tool (BIS) heralds the need for blood transfusion and/or failure of non-operative management in pediatric blunt liver and spleen injuries. J. Pediatr. Surg. 57(9), 202–207. https://doi.org/10.1016/j.jpedsurg.2021.09.043 (2022).
Metz, C. E. Basic principles of ROC analysis. Semin. Nucl. Med. 8(4), 283–298. https://doi.org/10.1016/S0001-2998(78)80014-2 (1978).
Nahm, F. S. Receiver operating characteristic curve: overview and practical use for clinicians. Korean J. Anesthesiol. 75(1), 25–36. https://doi.org/10.4097/kja.21209 (2022).
Hanley, J. A. & McNeil, B. J. A method of comparing the areas under receiver operating characteristic curves derived from the same cases. Radiology. 148(3), 839–843. https://doi.org/10.1148/radiology.148.3.6878708 (1983).
Yumoto, T. et al. Cushing’s sign and severe traumatic brain injury in children after blunt trauma: A nationwide retrospective cohort study in Japan. BMJ Open https://doi.org/10.1136/bmjopen-2017-020781s (2018).
Addo, O. Y. et al. Evaluation of hemoglobin cutoff levels to define anemia among healthy individuals. JAMA Netw. Open. 4(8), 1–13. https://doi.org/10.1001/jamanetworkopen.2021.19123 (2021).
Huang, K. C. et al. Shock index, pediatric age-adjusted predicts morbidity and mortality in children admitted to the intensive care unit. Front. Pediatr. 9(September), 1–8. https://doi.org/10.3389/fped.2021.727466 (2021).
Mendelson, J. Emergency department management of pediatric shock. Emerg. Med. Clin. N. Am. 36(2), 427–440. https://doi.org/10.1016/J.EMC.2017.12.010 (2018).
Tracy, E. T. et al. Pediatric injury patterns by year of age. J. Pediatr. Surg. 48(6), 1384–1388. https://doi.org/10.1016/j.jpedsurg.2013.03.041 (2013).
Aoki, M., Abe, T., Saitoh, D. & Oshima, K. Epidemiology, patterns of treatment, and mortality of pediatric trauma patients in Japan. Sci. Rep. 9(1), 1–7. https://doi.org/10.1038/s41598-018-37579-3 (2019).
Ishihara, T., Kondo, Y. & Tanaka, H. Efficacy of venous access placement at a pre-hospital scene in severe paediatric trauma patients: A retrospective cohort study. Sci. Rep. 10(1), 1–6. https://doi.org/10.1038/s41598-020-63564-w (2020).
Figueiredo, S. et al. How useful are hemoglobin concentration and its variations to predict significsant hemorrhage in the early phase of trauma?. A multicentric. cohort study Ann. Intensive Care. 8, 1. https://doi.org/10.1186/s13613-018-0420-8 (2018).
Swendiman, R. A., Goldshore, M. A., Allukian, M., Nace, G. W. & Nance, M. L. In reply to “abdominal angiography is associated with reduced in-hospital mortality among pediatric patients with blunt splenic and hepatic injury: A propensity-score-matching study from the national trauma registry in Japan”. J. Pediatr. Surg. 56(5), 1088–1089. https://doi.org/10.1016/j.jpedsurg.2021.03.014 (2021).
Acknowledgements
The authors thank collaborators of SHIPPs (Splenic and Hepatic Injury in Pediatric Patients) Study Group.
Author information
Authors and Affiliations
Consortia
Contributions
TYu, TO, TH, AI, KT, HN, and AN conceived and designed the study. TYu, TO, and TH analyzed the data. TYu prepared the first draft. MK, YK, HY, and SK participated in data collection and interpretation. TYo provided statistical advice on study design. All authors contributed substantially to its critical revision and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yumoto, T., Obara, T., Hongo, T. et al. Age-specific assessment of initial hemoglobin levels and shock index for predicting life-saving interventions in pediatric blunt liver and spleen injuries. Sci Rep 15, 8502 (2025). https://doi.org/10.1038/s41598-025-92673-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-92673-7